User login
Study offers snapshot of common MS comorbidities
NEW ORLEANS – Comorbidities such as hyperlipidemia, hypertension, gastrointestinal disorders, and depression are significantly more common among patients with multiple sclerosis, compared with patients who do not have the condition.
The findings, based on a large analysis of national claims data that was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers, may better inform physicians and patients about potential comorbidities in patients with MS, lead study author Kiren Kresa-Reahl, MD, said in an interview. “The challenge is, what is the underlying problem?” she asked. “Is it the chicken or the egg? It may be that MS lesions on the brain and microvascular disease look similar, so it’s hard to know. There are also conditions that are caused by MS, such as depression. Is it caused by MS the disease or is it a comorbidity with MS? That’s hard to know.”
In an effort to compare the prevalence of comorbidities in patients with and without MS, Dr. Kresa-Reahl and her associates retrospectively evaluated IMS Health Real World Data Adjudicated Claims-U.S. data between Jan. 1, 2011, and Sept. 30, 2015. The database includes about 150 million patients with a medical benefit and a subset of 95 million patients with both medical and pharmacy benefits. MS patients were required to have at least two claims with an ICD-9 diagnosis of MS 30 days apart and to be between the ages of 18 and 65.
The researchers drew from a systematic review of the 10 most common comorbidities in MS (Mult Scler. 2015;21[3]:263-81) and then matched 69,550 MS patients to a pool of 3,129,573 patients without MS by age group, gender, geographic region, and index quarter year. This left 66,616 patients in each cohort. Their mean age was 46 years, 76% were female, and the majority had commercial health insurance (97% of MS patients and 95% of those without the condition).
Of the 10 common comorbidities, eight occurred significantly more frequently among MS patients, compared with those without the condition (P less than .0001 for all). These included hyperlipidemia (27.76% vs. 24.57%, respectively), hypertension (26.91% vs. 23.50%), GI disorders (18.02% vs. 13.84%), depression (16.12% vs. 9.62%), thyroid disease (15.77% vs. 12.05%), anxiety (12.27% vs. 9.32%), and chronic obstructive pulmonary disease (10.39% vs. 9.52%).
Dr. Kresa-Reahl, a neurologist at the Providence Multiple Sclerosis Center in Portland, Ore., and her associates also found that patients with MS had a significantly lower prevalence of alcohol abuse, AIDS, mild liver disease, and moderate liver disease than did patients without MS (P less than .05 for all). There were no differences between groups in the prevalence of diabetes without complications or in metastatic tumor (P greater than .05).
She acknowledged certain limitations of the study, including the potential for missing information and the inability of the researchers to determine which form of MS the patients had. “It might be that if we looked at just Medicare and Medicaid patients, these diagnoses would be a little bit different,” Dr. Kresa-Reahl added. “Maybe they would have more disability or more depression or more limited mobility. It’s hard to know, but this is a snapshot of people who have commercial insurance, so maybe they would be more likely to be employed.”
The study was sponsored by EMD Serono. Dr. Kresa-Reahl disclosed that she has received consulting fees from Biogen and EMD Serono; speakers fees and honoraria from Biogen, EMD Serono, Genzyme, Mallinckrodt, Novartis, and Teva; and grant/research support from Biogen, Genentech, Genzyme, Mallinckrodt, and Novartis.
NEW ORLEANS – Comorbidities such as hyperlipidemia, hypertension, gastrointestinal disorders, and depression are significantly more common among patients with multiple sclerosis, compared with patients who do not have the condition.
The findings, based on a large analysis of national claims data that was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers, may better inform physicians and patients about potential comorbidities in patients with MS, lead study author Kiren Kresa-Reahl, MD, said in an interview. “The challenge is, what is the underlying problem?” she asked. “Is it the chicken or the egg? It may be that MS lesions on the brain and microvascular disease look similar, so it’s hard to know. There are also conditions that are caused by MS, such as depression. Is it caused by MS the disease or is it a comorbidity with MS? That’s hard to know.”
In an effort to compare the prevalence of comorbidities in patients with and without MS, Dr. Kresa-Reahl and her associates retrospectively evaluated IMS Health Real World Data Adjudicated Claims-U.S. data between Jan. 1, 2011, and Sept. 30, 2015. The database includes about 150 million patients with a medical benefit and a subset of 95 million patients with both medical and pharmacy benefits. MS patients were required to have at least two claims with an ICD-9 diagnosis of MS 30 days apart and to be between the ages of 18 and 65.
The researchers drew from a systematic review of the 10 most common comorbidities in MS (Mult Scler. 2015;21[3]:263-81) and then matched 69,550 MS patients to a pool of 3,129,573 patients without MS by age group, gender, geographic region, and index quarter year. This left 66,616 patients in each cohort. Their mean age was 46 years, 76% were female, and the majority had commercial health insurance (97% of MS patients and 95% of those without the condition).
Of the 10 common comorbidities, eight occurred significantly more frequently among MS patients, compared with those without the condition (P less than .0001 for all). These included hyperlipidemia (27.76% vs. 24.57%, respectively), hypertension (26.91% vs. 23.50%), GI disorders (18.02% vs. 13.84%), depression (16.12% vs. 9.62%), thyroid disease (15.77% vs. 12.05%), anxiety (12.27% vs. 9.32%), and chronic obstructive pulmonary disease (10.39% vs. 9.52%).
Dr. Kresa-Reahl, a neurologist at the Providence Multiple Sclerosis Center in Portland, Ore., and her associates also found that patients with MS had a significantly lower prevalence of alcohol abuse, AIDS, mild liver disease, and moderate liver disease than did patients without MS (P less than .05 for all). There were no differences between groups in the prevalence of diabetes without complications or in metastatic tumor (P greater than .05).
She acknowledged certain limitations of the study, including the potential for missing information and the inability of the researchers to determine which form of MS the patients had. “It might be that if we looked at just Medicare and Medicaid patients, these diagnoses would be a little bit different,” Dr. Kresa-Reahl added. “Maybe they would have more disability or more depression or more limited mobility. It’s hard to know, but this is a snapshot of people who have commercial insurance, so maybe they would be more likely to be employed.”
The study was sponsored by EMD Serono. Dr. Kresa-Reahl disclosed that she has received consulting fees from Biogen and EMD Serono; speakers fees and honoraria from Biogen, EMD Serono, Genzyme, Mallinckrodt, Novartis, and Teva; and grant/research support from Biogen, Genentech, Genzyme, Mallinckrodt, and Novartis.
NEW ORLEANS – Comorbidities such as hyperlipidemia, hypertension, gastrointestinal disorders, and depression are significantly more common among patients with multiple sclerosis, compared with patients who do not have the condition.
The findings, based on a large analysis of national claims data that was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers, may better inform physicians and patients about potential comorbidities in patients with MS, lead study author Kiren Kresa-Reahl, MD, said in an interview. “The challenge is, what is the underlying problem?” she asked. “Is it the chicken or the egg? It may be that MS lesions on the brain and microvascular disease look similar, so it’s hard to know. There are also conditions that are caused by MS, such as depression. Is it caused by MS the disease or is it a comorbidity with MS? That’s hard to know.”
In an effort to compare the prevalence of comorbidities in patients with and without MS, Dr. Kresa-Reahl and her associates retrospectively evaluated IMS Health Real World Data Adjudicated Claims-U.S. data between Jan. 1, 2011, and Sept. 30, 2015. The database includes about 150 million patients with a medical benefit and a subset of 95 million patients with both medical and pharmacy benefits. MS patients were required to have at least two claims with an ICD-9 diagnosis of MS 30 days apart and to be between the ages of 18 and 65.
The researchers drew from a systematic review of the 10 most common comorbidities in MS (Mult Scler. 2015;21[3]:263-81) and then matched 69,550 MS patients to a pool of 3,129,573 patients without MS by age group, gender, geographic region, and index quarter year. This left 66,616 patients in each cohort. Their mean age was 46 years, 76% were female, and the majority had commercial health insurance (97% of MS patients and 95% of those without the condition).
Of the 10 common comorbidities, eight occurred significantly more frequently among MS patients, compared with those without the condition (P less than .0001 for all). These included hyperlipidemia (27.76% vs. 24.57%, respectively), hypertension (26.91% vs. 23.50%), GI disorders (18.02% vs. 13.84%), depression (16.12% vs. 9.62%), thyroid disease (15.77% vs. 12.05%), anxiety (12.27% vs. 9.32%), and chronic obstructive pulmonary disease (10.39% vs. 9.52%).
Dr. Kresa-Reahl, a neurologist at the Providence Multiple Sclerosis Center in Portland, Ore., and her associates also found that patients with MS had a significantly lower prevalence of alcohol abuse, AIDS, mild liver disease, and moderate liver disease than did patients without MS (P less than .05 for all). There were no differences between groups in the prevalence of diabetes without complications or in metastatic tumor (P greater than .05).
She acknowledged certain limitations of the study, including the potential for missing information and the inability of the researchers to determine which form of MS the patients had. “It might be that if we looked at just Medicare and Medicaid patients, these diagnoses would be a little bit different,” Dr. Kresa-Reahl added. “Maybe they would have more disability or more depression or more limited mobility. It’s hard to know, but this is a snapshot of people who have commercial insurance, so maybe they would be more likely to be employed.”
The study was sponsored by EMD Serono. Dr. Kresa-Reahl disclosed that she has received consulting fees from Biogen and EMD Serono; speakers fees and honoraria from Biogen, EMD Serono, Genzyme, Mallinckrodt, Novartis, and Teva; and grant/research support from Biogen, Genentech, Genzyme, Mallinckrodt, and Novartis.
AT THE CMSC ANNUAL MEETING
Key clinical point:
Major finding: Of 10 common comorbidities, eight occurred significantly more frequently among MS patients, compared with those without the condition (P less than .0001 for all).
Data source: A retrospective analysis of claims data from 66,616 MS patients and 66,616 patients without the condition.
Disclosures: The study was sponsored by EMD Serono. Dr. Kresa-Reahl disclosed that she has received consulting fees from Biogen and EMD Serono; speakers fees and honoraria from Biogen, EMD Serono, Genzyme, Mallinckrodt, Novartis, and Teva; and grant/research support from Biogen, Genentech, Genzyme, Mallinckrodt, and Novartis.
Effective monitoring of DMTs for multiple sclerosis can be tricky
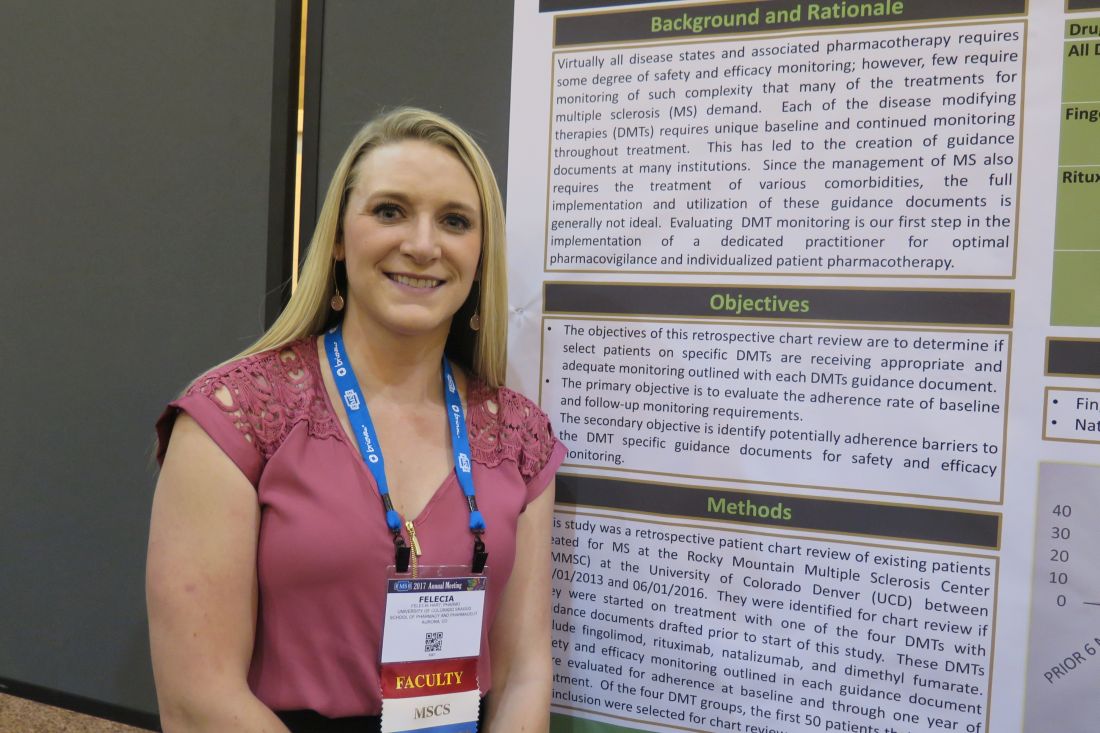
NEW ORLEANS – Safety and efficacy laboratory monitoring of adherence to disease-modifying therapies for multiple sclerosis remains challenging, results from a small pilot study showed.
In an effort to determine if select patients on specific DMTs are receiving appropriate and adequate monitoring as outlined by each DMT’s internal guidance document, Felecia Hart, PharmD, and her associates retrospectively reviewed existing patients treated for MS at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado, Denver, between June 1, 2013, and June 1, 2016.
“What we wanted to know was, if patients are getting their infusions or lab work done elsewhere, are we properly documenting it and keeping track of it?” Dr. Hart said in an interview at the meeting. “We’re not looking for core outcomes yet.”
Dr. Hart, a clinical pharmacy neurology fellow at the Skaggs School of Pharmacy and Pharmaceutical Sciences on the University of Colorado Anschutz Medical Campus, reported preliminary results from 50 patients treated with natalizumab and 50 treated with fingolimod. Among those treated with natalizumab, 49 had vitamin D measured within 6 months of drug initiation, 49 had a complete blood count measured within 1 year of drug initiation, and 49 had a comprehensive metabolic panel (CMP) measured within 1 year of drug initiation. “Interestingly, the absent CBC and CMP were from different patients,” she said.
Among patients treated with fingolimod, all had CBC/CMP measured within 1 year of drug initiation, 48 had vitamin D measured within 6 months of drug initiation, and 47 had documented macular optical coherence tomography at baseline, but the proportion of patients who had adequate documentation for other recommended assessments declined significantly. For example, only 19 of 50 had a documented repeat echocardiography within 3 months of drug initiation. Also, several baseline measurements required prior to drug initiation were documented poorly or in an untimely manner. Four patients had their HIV-1 and -2 antibody measured after drug initiation, three had hepatitis B virus surface antigen measured after drug initiation, and three had varicella measured after drug initiation.
Even though the MS center has an electronic medical record system, Dr. Hart and her associates found it difficult to obtain and monitor the parameters of interest. “I’ve been working with our EMR for 6 years, so I know how to navigate it well,” she said. “But I found it difficult to do a simple chart review and find what I wanted to. We have a labs tab in our chart, but the difficulty became including patients who were coming from outside of our center. The lab and the order were referenced in a note but there was never any documentation after that. There are too many holes in getting it documented correctly.”
The findings suggest that having a dedicated clinician such as a clinical pharmacist to oversee pharmacovigilance may improve patient outcomes and ensure that safety and efficacy monitoring doesn’t inadvertently get overlooked because of difficulties with adequate documentation. “That would be ideal,” Dr. Hart said.
She reported having no financial disclosures.
NEW ORLEANS – Safety and efficacy laboratory monitoring of adherence to disease-modifying therapies for multiple sclerosis remains challenging, results from a small pilot study showed.
In an effort to determine if select patients on specific DMTs are receiving appropriate and adequate monitoring as outlined by each DMT’s internal guidance document, Felecia Hart, PharmD, and her associates retrospectively reviewed existing patients treated for MS at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado, Denver, between June 1, 2013, and June 1, 2016.
“What we wanted to know was, if patients are getting their infusions or lab work done elsewhere, are we properly documenting it and keeping track of it?” Dr. Hart said in an interview at the meeting. “We’re not looking for core outcomes yet.”
Dr. Hart, a clinical pharmacy neurology fellow at the Skaggs School of Pharmacy and Pharmaceutical Sciences on the University of Colorado Anschutz Medical Campus, reported preliminary results from 50 patients treated with natalizumab and 50 treated with fingolimod. Among those treated with natalizumab, 49 had vitamin D measured within 6 months of drug initiation, 49 had a complete blood count measured within 1 year of drug initiation, and 49 had a comprehensive metabolic panel (CMP) measured within 1 year of drug initiation. “Interestingly, the absent CBC and CMP were from different patients,” she said.
Among patients treated with fingolimod, all had CBC/CMP measured within 1 year of drug initiation, 48 had vitamin D measured within 6 months of drug initiation, and 47 had documented macular optical coherence tomography at baseline, but the proportion of patients who had adequate documentation for other recommended assessments declined significantly. For example, only 19 of 50 had a documented repeat echocardiography within 3 months of drug initiation. Also, several baseline measurements required prior to drug initiation were documented poorly or in an untimely manner. Four patients had their HIV-1 and -2 antibody measured after drug initiation, three had hepatitis B virus surface antigen measured after drug initiation, and three had varicella measured after drug initiation.
Even though the MS center has an electronic medical record system, Dr. Hart and her associates found it difficult to obtain and monitor the parameters of interest. “I’ve been working with our EMR for 6 years, so I know how to navigate it well,” she said. “But I found it difficult to do a simple chart review and find what I wanted to. We have a labs tab in our chart, but the difficulty became including patients who were coming from outside of our center. The lab and the order were referenced in a note but there was never any documentation after that. There are too many holes in getting it documented correctly.”
The findings suggest that having a dedicated clinician such as a clinical pharmacist to oversee pharmacovigilance may improve patient outcomes and ensure that safety and efficacy monitoring doesn’t inadvertently get overlooked because of difficulties with adequate documentation. “That would be ideal,” Dr. Hart said.
She reported having no financial disclosures.
NEW ORLEANS – Safety and efficacy laboratory monitoring of adherence to disease-modifying therapies for multiple sclerosis remains challenging, results from a small pilot study showed.
In an effort to determine if select patients on specific DMTs are receiving appropriate and adequate monitoring as outlined by each DMT’s internal guidance document, Felecia Hart, PharmD, and her associates retrospectively reviewed existing patients treated for MS at the Rocky Mountain Multiple Sclerosis Center at the University of Colorado, Denver, between June 1, 2013, and June 1, 2016.
“What we wanted to know was, if patients are getting their infusions or lab work done elsewhere, are we properly documenting it and keeping track of it?” Dr. Hart said in an interview at the meeting. “We’re not looking for core outcomes yet.”
Dr. Hart, a clinical pharmacy neurology fellow at the Skaggs School of Pharmacy and Pharmaceutical Sciences on the University of Colorado Anschutz Medical Campus, reported preliminary results from 50 patients treated with natalizumab and 50 treated with fingolimod. Among those treated with natalizumab, 49 had vitamin D measured within 6 months of drug initiation, 49 had a complete blood count measured within 1 year of drug initiation, and 49 had a comprehensive metabolic panel (CMP) measured within 1 year of drug initiation. “Interestingly, the absent CBC and CMP were from different patients,” she said.
Among patients treated with fingolimod, all had CBC/CMP measured within 1 year of drug initiation, 48 had vitamin D measured within 6 months of drug initiation, and 47 had documented macular optical coherence tomography at baseline, but the proportion of patients who had adequate documentation for other recommended assessments declined significantly. For example, only 19 of 50 had a documented repeat echocardiography within 3 months of drug initiation. Also, several baseline measurements required prior to drug initiation were documented poorly or in an untimely manner. Four patients had their HIV-1 and -2 antibody measured after drug initiation, three had hepatitis B virus surface antigen measured after drug initiation, and three had varicella measured after drug initiation.
Even though the MS center has an electronic medical record system, Dr. Hart and her associates found it difficult to obtain and monitor the parameters of interest. “I’ve been working with our EMR for 6 years, so I know how to navigate it well,” she said. “But I found it difficult to do a simple chart review and find what I wanted to. We have a labs tab in our chart, but the difficulty became including patients who were coming from outside of our center. The lab and the order were referenced in a note but there was never any documentation after that. There are too many holes in getting it documented correctly.”
The findings suggest that having a dedicated clinician such as a clinical pharmacist to oversee pharmacovigilance may improve patient outcomes and ensure that safety and efficacy monitoring doesn’t inadvertently get overlooked because of difficulties with adequate documentation. “That would be ideal,” Dr. Hart said.
She reported having no financial disclosures.
AT THE CMSC ANNUAL MEETING
Key clinical point:
Major finding: Among patients treated with fingolimod, only 19 of 50 had a documented repeat ECG within 3 months of drug initiation. Also, several baseline measurements required prior to drug initiation were documented poorly or in an untimely manner.
Data source: Preliminary results from a retrospective review of 50 patients treated with natalizumab and 50 treated with fingolimod.
Disclosures: Dr. Hart reported having no financial disclosures.
Phase II Data Show Safety and Efficacy of Ozanimod for Relapsing MS
NEW ORLEANS—Ozanimod demonstrated durable efficacy with a favorable safety profile in patients continuing ozanimod for 120 weeks or switching from placebo to ozanimod for 96 weeks, according to results of a phase II study presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “These data support the ongoing RADIANCE and SUNBEAM phase III studies,” said Brett E. Skolnick, PhD, on behalf of his study collaborators. Dr. Skolnick is an employee of Receptos, a wholly owned subsidiary of Celgene, in San Diego.
Ozanimod, an oral, once-daily immunomodulator selectively targeting sphingosine 1-phosphate (S1P) receptor-1 and -5 , is in development for relapsing multiple sclerosis (MS). “The increased receptor selectivity of ozanimod and additional pharmaceutical properties may result in a more favorable safety profile versus other nonselective and selective S1P receptor modulators,” said Dr. Skolnick.
In the completed RADIANCE Part A phase II trial, patients with relapsing MS were randomized (1:1:1) to once-daily ozanimod 0.5 mg or 1.0 mg or to placebo for 24 weeks. At week 24, patients could enter a 96-week, blinded extension phase. Patients randomized to ozanimod continued their assigned dose; 85 patients received 0.5 mg, and 81 patients received 1.0 mg. Patients administered placebo were re-randomized (1:1) to ozanimod 0.5 mg (n = 41) or 1.0 mg (n = 42). Ozanimod was dose-escalated over seven days to attenuate first-dose effects.
A total of 89% of patients taking the 0.5 mg dose and 90% of patients taking the 1.0 mg dose completed the extension study. At week 120, 89% to 91% of patients were free of gadolinium-enhancing lesions. Unadjusted annualized relapse rates were 0.31 in the 0.5 mg group and 0.18 in the 1.0 mg group. One or more treatment-emergent adverse events were seen in 79% of patients taking the 0.5 mg dose and in 76% of those taking the 1.0 mg dose. The most common adverse events were increased alanine aminotransferases, nasopharyngitis, and upper respiratory tract infection. Serious treatment-emergent adverse events were seen in 12 patients in the 0.5 mg group and in nine patients in the 1.0 mg group. Mild blunting of the normal diurnal heart rate was observed. The largest mean decrease in heart rate relative to pre-dose was 3.5 bpm at hour 6 on day 1, with no associated symptoms. No type II or 2:1 atrioventricular block was reported.
At week 120, alanine aminotransferase (ALT) levels were three or more times upper limit of normal in 6% of the 0.5 mg group and in 7% of the 1.0 mg group. In the 0.5 mg group, 2% of patients discontinued ozanimod due to increased liver transaminases. Less than 1% of patients in the 1.0 mg group discontinued ozanimod for the same reason. Between baseline and week 120, three patients in the 1.0 mg group had absolute lymphocyte counts below 200 cells/μL; none was associated with severe or serious infection. There were no notable cases of pulmonary adverse events and no cases of macular edema, malignancy-related adverse events, or serious opportunistic infections.
This study was supported by Celgene.
Suggested Reading
Cohen JA, Arnold DL, Comi G, et al. Safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ozanimod in relapsing multiple sclerosis (RADIANCE): a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(4):373-381.
NEW ORLEANS—Ozanimod demonstrated durable efficacy with a favorable safety profile in patients continuing ozanimod for 120 weeks or switching from placebo to ozanimod for 96 weeks, according to results of a phase II study presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “These data support the ongoing RADIANCE and SUNBEAM phase III studies,” said Brett E. Skolnick, PhD, on behalf of his study collaborators. Dr. Skolnick is an employee of Receptos, a wholly owned subsidiary of Celgene, in San Diego.
Ozanimod, an oral, once-daily immunomodulator selectively targeting sphingosine 1-phosphate (S1P) receptor-1 and -5 , is in development for relapsing multiple sclerosis (MS). “The increased receptor selectivity of ozanimod and additional pharmaceutical properties may result in a more favorable safety profile versus other nonselective and selective S1P receptor modulators,” said Dr. Skolnick.
In the completed RADIANCE Part A phase II trial, patients with relapsing MS were randomized (1:1:1) to once-daily ozanimod 0.5 mg or 1.0 mg or to placebo for 24 weeks. At week 24, patients could enter a 96-week, blinded extension phase. Patients randomized to ozanimod continued their assigned dose; 85 patients received 0.5 mg, and 81 patients received 1.0 mg. Patients administered placebo were re-randomized (1:1) to ozanimod 0.5 mg (n = 41) or 1.0 mg (n = 42). Ozanimod was dose-escalated over seven days to attenuate first-dose effects.
A total of 89% of patients taking the 0.5 mg dose and 90% of patients taking the 1.0 mg dose completed the extension study. At week 120, 89% to 91% of patients were free of gadolinium-enhancing lesions. Unadjusted annualized relapse rates were 0.31 in the 0.5 mg group and 0.18 in the 1.0 mg group. One or more treatment-emergent adverse events were seen in 79% of patients taking the 0.5 mg dose and in 76% of those taking the 1.0 mg dose. The most common adverse events were increased alanine aminotransferases, nasopharyngitis, and upper respiratory tract infection. Serious treatment-emergent adverse events were seen in 12 patients in the 0.5 mg group and in nine patients in the 1.0 mg group. Mild blunting of the normal diurnal heart rate was observed. The largest mean decrease in heart rate relative to pre-dose was 3.5 bpm at hour 6 on day 1, with no associated symptoms. No type II or 2:1 atrioventricular block was reported.
At week 120, alanine aminotransferase (ALT) levels were three or more times upper limit of normal in 6% of the 0.5 mg group and in 7% of the 1.0 mg group. In the 0.5 mg group, 2% of patients discontinued ozanimod due to increased liver transaminases. Less than 1% of patients in the 1.0 mg group discontinued ozanimod for the same reason. Between baseline and week 120, three patients in the 1.0 mg group had absolute lymphocyte counts below 200 cells/μL; none was associated with severe or serious infection. There were no notable cases of pulmonary adverse events and no cases of macular edema, malignancy-related adverse events, or serious opportunistic infections.
This study was supported by Celgene.
Suggested Reading
Cohen JA, Arnold DL, Comi G, et al. Safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ozanimod in relapsing multiple sclerosis (RADIANCE): a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(4):373-381.
NEW ORLEANS—Ozanimod demonstrated durable efficacy with a favorable safety profile in patients continuing ozanimod for 120 weeks or switching from placebo to ozanimod for 96 weeks, according to results of a phase II study presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “These data support the ongoing RADIANCE and SUNBEAM phase III studies,” said Brett E. Skolnick, PhD, on behalf of his study collaborators. Dr. Skolnick is an employee of Receptos, a wholly owned subsidiary of Celgene, in San Diego.
Ozanimod, an oral, once-daily immunomodulator selectively targeting sphingosine 1-phosphate (S1P) receptor-1 and -5 , is in development for relapsing multiple sclerosis (MS). “The increased receptor selectivity of ozanimod and additional pharmaceutical properties may result in a more favorable safety profile versus other nonselective and selective S1P receptor modulators,” said Dr. Skolnick.
In the completed RADIANCE Part A phase II trial, patients with relapsing MS were randomized (1:1:1) to once-daily ozanimod 0.5 mg or 1.0 mg or to placebo for 24 weeks. At week 24, patients could enter a 96-week, blinded extension phase. Patients randomized to ozanimod continued their assigned dose; 85 patients received 0.5 mg, and 81 patients received 1.0 mg. Patients administered placebo were re-randomized (1:1) to ozanimod 0.5 mg (n = 41) or 1.0 mg (n = 42). Ozanimod was dose-escalated over seven days to attenuate first-dose effects.
A total of 89% of patients taking the 0.5 mg dose and 90% of patients taking the 1.0 mg dose completed the extension study. At week 120, 89% to 91% of patients were free of gadolinium-enhancing lesions. Unadjusted annualized relapse rates were 0.31 in the 0.5 mg group and 0.18 in the 1.0 mg group. One or more treatment-emergent adverse events were seen in 79% of patients taking the 0.5 mg dose and in 76% of those taking the 1.0 mg dose. The most common adverse events were increased alanine aminotransferases, nasopharyngitis, and upper respiratory tract infection. Serious treatment-emergent adverse events were seen in 12 patients in the 0.5 mg group and in nine patients in the 1.0 mg group. Mild blunting of the normal diurnal heart rate was observed. The largest mean decrease in heart rate relative to pre-dose was 3.5 bpm at hour 6 on day 1, with no associated symptoms. No type II or 2:1 atrioventricular block was reported.
At week 120, alanine aminotransferase (ALT) levels were three or more times upper limit of normal in 6% of the 0.5 mg group and in 7% of the 1.0 mg group. In the 0.5 mg group, 2% of patients discontinued ozanimod due to increased liver transaminases. Less than 1% of patients in the 1.0 mg group discontinued ozanimod for the same reason. Between baseline and week 120, three patients in the 1.0 mg group had absolute lymphocyte counts below 200 cells/μL; none was associated with severe or serious infection. There were no notable cases of pulmonary adverse events and no cases of macular edema, malignancy-related adverse events, or serious opportunistic infections.
This study was supported by Celgene.
Suggested Reading
Cohen JA, Arnold DL, Comi G, et al. Safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ozanimod in relapsing multiple sclerosis (RADIANCE): a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(4):373-381.
Risk tolerance to MS therapies varies widely
NEW ORLEANS – Risk tolerance to current disease modifying therapies by patients with multiple sclerosis varies widely, results from a large national survey demonstrated.
“We have therapies available with a wide range of risks,” study author Sneha Natarajan, PhD, said in an interview at the annual meeting of the Consortium of Multiple Sclerosis Centers. “Some of the risks are relatively minor like injection site reactions or flu-like symptoms and some are as bad as PML [progressive multifocal leukoencephalopathy], which can be fatal. We don’t know what kind of risks people tolerate.”
Dr. Natarajan, research coordinator at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, reported results from 3,371 survey respondents. Their mean age was 55 years, 93% were white, 61% had the relapsing-remitting form of MS, and 53% were currently taking a DMT. Overall, respondents reported the highest risk tolerance for infection or thyroid risks (1:1,000 for both) and lowest risk tolerance for PML and kidney injury risks (1:1,000,000 for both). Males reported a higher risk tolerance to all six risks (P less than .0001 for all). Females reported a risk tolerance to skin rash that was similar to kidney injury and PML.
“There is a pattern to the risks that our patients accept,” Dr. Natarajan said. “I don’t think a doctor would not recommend a therapy benefit because of a skin rash [risk], but he may need to address the concerns of the patient upfront and have a talk with the patient.”
The researchers also found that current DMT users expressed increased risk tolerance for all outcomes, compared with those not using any DMT (P less than .001). Higher risk tolerance was also expressed by respondents who were older, more disabled, and by those taking infusion therapies.
The National Multiple Sclerosis Society funded the study. Dr. Natarajan reported having no financial disclosures.
NEW ORLEANS – Risk tolerance to current disease modifying therapies by patients with multiple sclerosis varies widely, results from a large national survey demonstrated.
“We have therapies available with a wide range of risks,” study author Sneha Natarajan, PhD, said in an interview at the annual meeting of the Consortium of Multiple Sclerosis Centers. “Some of the risks are relatively minor like injection site reactions or flu-like symptoms and some are as bad as PML [progressive multifocal leukoencephalopathy], which can be fatal. We don’t know what kind of risks people tolerate.”
Dr. Natarajan, research coordinator at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, reported results from 3,371 survey respondents. Their mean age was 55 years, 93% were white, 61% had the relapsing-remitting form of MS, and 53% were currently taking a DMT. Overall, respondents reported the highest risk tolerance for infection or thyroid risks (1:1,000 for both) and lowest risk tolerance for PML and kidney injury risks (1:1,000,000 for both). Males reported a higher risk tolerance to all six risks (P less than .0001 for all). Females reported a risk tolerance to skin rash that was similar to kidney injury and PML.
“There is a pattern to the risks that our patients accept,” Dr. Natarajan said. “I don’t think a doctor would not recommend a therapy benefit because of a skin rash [risk], but he may need to address the concerns of the patient upfront and have a talk with the patient.”
The researchers also found that current DMT users expressed increased risk tolerance for all outcomes, compared with those not using any DMT (P less than .001). Higher risk tolerance was also expressed by respondents who were older, more disabled, and by those taking infusion therapies.
The National Multiple Sclerosis Society funded the study. Dr. Natarajan reported having no financial disclosures.
NEW ORLEANS – Risk tolerance to current disease modifying therapies by patients with multiple sclerosis varies widely, results from a large national survey demonstrated.
“We have therapies available with a wide range of risks,” study author Sneha Natarajan, PhD, said in an interview at the annual meeting of the Consortium of Multiple Sclerosis Centers. “Some of the risks are relatively minor like injection site reactions or flu-like symptoms and some are as bad as PML [progressive multifocal leukoencephalopathy], which can be fatal. We don’t know what kind of risks people tolerate.”
Dr. Natarajan, research coordinator at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, reported results from 3,371 survey respondents. Their mean age was 55 years, 93% were white, 61% had the relapsing-remitting form of MS, and 53% were currently taking a DMT. Overall, respondents reported the highest risk tolerance for infection or thyroid risks (1:1,000 for both) and lowest risk tolerance for PML and kidney injury risks (1:1,000,000 for both). Males reported a higher risk tolerance to all six risks (P less than .0001 for all). Females reported a risk tolerance to skin rash that was similar to kidney injury and PML.
“There is a pattern to the risks that our patients accept,” Dr. Natarajan said. “I don’t think a doctor would not recommend a therapy benefit because of a skin rash [risk], but he may need to address the concerns of the patient upfront and have a talk with the patient.”
The researchers also found that current DMT users expressed increased risk tolerance for all outcomes, compared with those not using any DMT (P less than .001). Higher risk tolerance was also expressed by respondents who were older, more disabled, and by those taking infusion therapies.
The National Multiple Sclerosis Society funded the study. Dr. Natarajan reported having no financial disclosures.
AT THE CMSC ANNUAL MEETING
Key clinical point:
Major finding: Survey respondents reported the highest risk tolerance for infection or thyroid risks (1:1,000 for both) and lowest risk tolerance for PML and kidney injury risks (1:1,000,000 for both).
Data source: A survey of 3,371 people who reported having MS.
Disclosures: The National Multiple Sclerosis Society funded the study. Dr. Natarajan reported having no financial disclosures.
Alemtuzumab May Prevent MRI Lesions for Six Years in Patients With Highly Active Disease
NEW ORLEANS—Most patients with relapsing-remitting multiple sclerosis (MS) with highly active disease remain free of new MRI activity for six years after receiving alemtuzumab, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers. The durable effects may result from the distinct pattern of lymphocyte repopulation following treatment with alemtuzumab, which may lead to a rebalancing of the immune system, said Anthony Traboulsee, MD, Associate Professor of Neurology at the University of British Columbia in Vancouver. Additional mechanistic studies are needed to establish this hypothesis, the authors said.
To evaluate six-year MRI and brain volume loss outcomes in a subset of patient with highly active disease at baseline who were treated with alemtuzumab, Dr. Traboulsee and colleagues analyzed data from the CARE-MS I trial. In that trial, researchers randomized patients with active relapsing-remitting MS who were drug-naïve at baseline to alemtuzumab or interferon beta-1a. After two years, patients who received alemtuzumab had improved clinical and MRI outcomes, including brain loss volume, compared with patients who received interferon beta-1a. In addition, significantly more of these patients had no evidence of disease activity, compared with patients treated with interferon beta1-a.
In an extension study, patients could receive additional treatment with alemtuzumab (12 mg/day on three consecutive days one year or more after the most recent course) as needed for relapse or radiologic activity. During the extension, patients also could receive treatment with other licensed disease-modifying therapies at an investigator’s discretion. Retreatment criteria included one or more relapse, two or more new or enlarging T2 hyperintense lesions, or new gadolinium-enhancing T1 brain or spinal cord lesions on MRI. Researchers defined highly active disease as two or more relapses a year prior to randomization and one or more gadolinium-enhancing T1 lesion at core study baseline.
The researchers obtained MRI scans at baseline and yearly thereafter. Experts masked to patients’ original treatment group assignment analyzed the MRI scans. Investigators assessed the proportion of patients free of MRI disease activity (ie, no new or enlarging T2 hyperintense lesions or new gadolinium-enhancing T1 lesions) and the proportion of patients free of new non-enhancing T1 lesions. Brain volume loss was derived by brain parenchymal fraction change.
Of 376 patients who received alemtuzumab in the CARE-MS I trial, 105 met the criteria for highly active disease at core study baseline. Of these 105 patients, 99 remained in the study through Year 6. Through six years, 63% of patients did not receive additional treatment with alemtuzumab or another disease-modifying therapy. In each year through Year 6, a majority of patients were free of MRI disease activity (61 % at Year 6), free of new gadolinium-enhancing T1 lesions (83% at Year 6), and free of new or enlarging T2 hyperintense lesions (62% at Year 6). The investigators also observed that annually in Years 2 through 6, high proportions of patients had no new non-enhancing T1 hypointense lesions.
“These findings, along with long-term clinical efficacy, suggest that alemtuzumab may provide a unique treatment approach for relapsing-remitting MS patients with highly active disease, offering durable efficacy in the absence of continuous treatment,” said Dr. Traboulsee and colleagues.
NEW ORLEANS—Most patients with relapsing-remitting multiple sclerosis (MS) with highly active disease remain free of new MRI activity for six years after receiving alemtuzumab, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers. The durable effects may result from the distinct pattern of lymphocyte repopulation following treatment with alemtuzumab, which may lead to a rebalancing of the immune system, said Anthony Traboulsee, MD, Associate Professor of Neurology at the University of British Columbia in Vancouver. Additional mechanistic studies are needed to establish this hypothesis, the authors said.
To evaluate six-year MRI and brain volume loss outcomes in a subset of patient with highly active disease at baseline who were treated with alemtuzumab, Dr. Traboulsee and colleagues analyzed data from the CARE-MS I trial. In that trial, researchers randomized patients with active relapsing-remitting MS who were drug-naïve at baseline to alemtuzumab or interferon beta-1a. After two years, patients who received alemtuzumab had improved clinical and MRI outcomes, including brain loss volume, compared with patients who received interferon beta-1a. In addition, significantly more of these patients had no evidence of disease activity, compared with patients treated with interferon beta1-a.
In an extension study, patients could receive additional treatment with alemtuzumab (12 mg/day on three consecutive days one year or more after the most recent course) as needed for relapse or radiologic activity. During the extension, patients also could receive treatment with other licensed disease-modifying therapies at an investigator’s discretion. Retreatment criteria included one or more relapse, two or more new or enlarging T2 hyperintense lesions, or new gadolinium-enhancing T1 brain or spinal cord lesions on MRI. Researchers defined highly active disease as two or more relapses a year prior to randomization and one or more gadolinium-enhancing T1 lesion at core study baseline.
The researchers obtained MRI scans at baseline and yearly thereafter. Experts masked to patients’ original treatment group assignment analyzed the MRI scans. Investigators assessed the proportion of patients free of MRI disease activity (ie, no new or enlarging T2 hyperintense lesions or new gadolinium-enhancing T1 lesions) and the proportion of patients free of new non-enhancing T1 lesions. Brain volume loss was derived by brain parenchymal fraction change.
Of 376 patients who received alemtuzumab in the CARE-MS I trial, 105 met the criteria for highly active disease at core study baseline. Of these 105 patients, 99 remained in the study through Year 6. Through six years, 63% of patients did not receive additional treatment with alemtuzumab or another disease-modifying therapy. In each year through Year 6, a majority of patients were free of MRI disease activity (61 % at Year 6), free of new gadolinium-enhancing T1 lesions (83% at Year 6), and free of new or enlarging T2 hyperintense lesions (62% at Year 6). The investigators also observed that annually in Years 2 through 6, high proportions of patients had no new non-enhancing T1 hypointense lesions.
“These findings, along with long-term clinical efficacy, suggest that alemtuzumab may provide a unique treatment approach for relapsing-remitting MS patients with highly active disease, offering durable efficacy in the absence of continuous treatment,” said Dr. Traboulsee and colleagues.
NEW ORLEANS—Most patients with relapsing-remitting multiple sclerosis (MS) with highly active disease remain free of new MRI activity for six years after receiving alemtuzumab, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers. The durable effects may result from the distinct pattern of lymphocyte repopulation following treatment with alemtuzumab, which may lead to a rebalancing of the immune system, said Anthony Traboulsee, MD, Associate Professor of Neurology at the University of British Columbia in Vancouver. Additional mechanistic studies are needed to establish this hypothesis, the authors said.
To evaluate six-year MRI and brain volume loss outcomes in a subset of patient with highly active disease at baseline who were treated with alemtuzumab, Dr. Traboulsee and colleagues analyzed data from the CARE-MS I trial. In that trial, researchers randomized patients with active relapsing-remitting MS who were drug-naïve at baseline to alemtuzumab or interferon beta-1a. After two years, patients who received alemtuzumab had improved clinical and MRI outcomes, including brain loss volume, compared with patients who received interferon beta-1a. In addition, significantly more of these patients had no evidence of disease activity, compared with patients treated with interferon beta1-a.
In an extension study, patients could receive additional treatment with alemtuzumab (12 mg/day on three consecutive days one year or more after the most recent course) as needed for relapse or radiologic activity. During the extension, patients also could receive treatment with other licensed disease-modifying therapies at an investigator’s discretion. Retreatment criteria included one or more relapse, two or more new or enlarging T2 hyperintense lesions, or new gadolinium-enhancing T1 brain or spinal cord lesions on MRI. Researchers defined highly active disease as two or more relapses a year prior to randomization and one or more gadolinium-enhancing T1 lesion at core study baseline.
The researchers obtained MRI scans at baseline and yearly thereafter. Experts masked to patients’ original treatment group assignment analyzed the MRI scans. Investigators assessed the proportion of patients free of MRI disease activity (ie, no new or enlarging T2 hyperintense lesions or new gadolinium-enhancing T1 lesions) and the proportion of patients free of new non-enhancing T1 lesions. Brain volume loss was derived by brain parenchymal fraction change.
Of 376 patients who received alemtuzumab in the CARE-MS I trial, 105 met the criteria for highly active disease at core study baseline. Of these 105 patients, 99 remained in the study through Year 6. Through six years, 63% of patients did not receive additional treatment with alemtuzumab or another disease-modifying therapy. In each year through Year 6, a majority of patients were free of MRI disease activity (61 % at Year 6), free of new gadolinium-enhancing T1 lesions (83% at Year 6), and free of new or enlarging T2 hyperintense lesions (62% at Year 6). The investigators also observed that annually in Years 2 through 6, high proportions of patients had no new non-enhancing T1 hypointense lesions.
“These findings, along with long-term clinical efficacy, suggest that alemtuzumab may provide a unique treatment approach for relapsing-remitting MS patients with highly active disease, offering durable efficacy in the absence of continuous treatment,” said Dr. Traboulsee and colleagues.
What Are Patients With MS Saying About Day-to-Day Life and Treatment?
NEW ORLEANS—Two studies presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis (MS) Centers examined the impact of MS and treatment among patients who are members of an online social network. Researchers found that, among patients who were taking oral disease-modifying treatments (DMTs), how the drug was taken was the most important factor in selecting the therapy (36% of patients) almost as often as the doctor’s recommendation (40% of patients), according to the results of a patient survey. In a separate study that analyzed comments made on the social network, researchers found that adverse events were the most commonly stated reason for stopping a treatment (56%).
In one study, Terrie Livingston, PharmD, an employee of Biogen in Weston, Massachusetts, and colleagues conducted a patient survey to assess the impact of MS on day-to-day life, self-reported symptoms, patient descriptions of disability progression, trade-offs when deciding which DMT to take, and what health care providers should know to better manage MS.
In November 2014, researchers sent an email invitation to the entire MyMSTeam community, a social network of approximately 25,000 people (currently more than 75,000 people) diagnosed with MS. In all, 1,107 members responded to the survey.
Overall, the most commonly reported symptoms were fatigue (82% of patients), problems with mobility (64%), and poor balance (64%). In addition, weakness, cognitive issues, and depression were common. The respondents defined disability progression as increased limitations on their ability to get around, having to sacrifice normal daily activities, and losing their ability to be independent. Patients measured the efficacy of DMTs by evaluating the treatments’ ability to slow progression, prevent further physical disability, prevent new lesions, and improve quality of life.
In a separate study, Dr. Livingston and colleagues conducted an analysis of organic discussions within MyMSTeam from January 2015 to April 2016. Researchers anonymized, coded, categorized, and analyzed 3,300 verbatim comments by key themes. The analysis focused on 12 DMTs. Discussions were overlaid with patient self-reported data on gender, age, date of diagnosis, MS type, current DMT, and effectiveness ratings.
Common discussion topics included side effects experienced; reasons for stopping treatment; perceived efficacy; questions, hopes, and concerns about starting a new DMT; rituals to mitigate side effects; and insurance or financial hurdles to getting on or staying on treatment.
Discussions about infusion therapies tended to focus on receiving treatment and issues related to progressive multifocal leukoencephalopathy.
When discussing Tysabri (natalizumab), patients most commonly discussed elevated energy levels post infusion around day 14. Patients also reported increased fatigue in the days prior to the next infusion and extreme fatigue on the day of treatment. In addition, patients shared their experiences with managing tolerability issues, most commonly flu-like symptoms with interferons and gastrointestinal effects with Tecfidera (dimethyl fumarate).
Dr. Livingston and colleagues said that their research “will better allow medical professionals to treat the individual holistically, and not just the disease itself. Additionally, helping patients understand MS progression will allow specialists to set realistic expectations for treating the disease and to help their patients better prepare for the future.”
NEW ORLEANS—Two studies presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis (MS) Centers examined the impact of MS and treatment among patients who are members of an online social network. Researchers found that, among patients who were taking oral disease-modifying treatments (DMTs), how the drug was taken was the most important factor in selecting the therapy (36% of patients) almost as often as the doctor’s recommendation (40% of patients), according to the results of a patient survey. In a separate study that analyzed comments made on the social network, researchers found that adverse events were the most commonly stated reason for stopping a treatment (56%).
In one study, Terrie Livingston, PharmD, an employee of Biogen in Weston, Massachusetts, and colleagues conducted a patient survey to assess the impact of MS on day-to-day life, self-reported symptoms, patient descriptions of disability progression, trade-offs when deciding which DMT to take, and what health care providers should know to better manage MS.
In November 2014, researchers sent an email invitation to the entire MyMSTeam community, a social network of approximately 25,000 people (currently more than 75,000 people) diagnosed with MS. In all, 1,107 members responded to the survey.
Overall, the most commonly reported symptoms were fatigue (82% of patients), problems with mobility (64%), and poor balance (64%). In addition, weakness, cognitive issues, and depression were common. The respondents defined disability progression as increased limitations on their ability to get around, having to sacrifice normal daily activities, and losing their ability to be independent. Patients measured the efficacy of DMTs by evaluating the treatments’ ability to slow progression, prevent further physical disability, prevent new lesions, and improve quality of life.
In a separate study, Dr. Livingston and colleagues conducted an analysis of organic discussions within MyMSTeam from January 2015 to April 2016. Researchers anonymized, coded, categorized, and analyzed 3,300 verbatim comments by key themes. The analysis focused on 12 DMTs. Discussions were overlaid with patient self-reported data on gender, age, date of diagnosis, MS type, current DMT, and effectiveness ratings.
Common discussion topics included side effects experienced; reasons for stopping treatment; perceived efficacy; questions, hopes, and concerns about starting a new DMT; rituals to mitigate side effects; and insurance or financial hurdles to getting on or staying on treatment.
Discussions about infusion therapies tended to focus on receiving treatment and issues related to progressive multifocal leukoencephalopathy.
When discussing Tysabri (natalizumab), patients most commonly discussed elevated energy levels post infusion around day 14. Patients also reported increased fatigue in the days prior to the next infusion and extreme fatigue on the day of treatment. In addition, patients shared their experiences with managing tolerability issues, most commonly flu-like symptoms with interferons and gastrointestinal effects with Tecfidera (dimethyl fumarate).
Dr. Livingston and colleagues said that their research “will better allow medical professionals to treat the individual holistically, and not just the disease itself. Additionally, helping patients understand MS progression will allow specialists to set realistic expectations for treating the disease and to help their patients better prepare for the future.”
NEW ORLEANS—Two studies presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis (MS) Centers examined the impact of MS and treatment among patients who are members of an online social network. Researchers found that, among patients who were taking oral disease-modifying treatments (DMTs), how the drug was taken was the most important factor in selecting the therapy (36% of patients) almost as often as the doctor’s recommendation (40% of patients), according to the results of a patient survey. In a separate study that analyzed comments made on the social network, researchers found that adverse events were the most commonly stated reason for stopping a treatment (56%).
In one study, Terrie Livingston, PharmD, an employee of Biogen in Weston, Massachusetts, and colleagues conducted a patient survey to assess the impact of MS on day-to-day life, self-reported symptoms, patient descriptions of disability progression, trade-offs when deciding which DMT to take, and what health care providers should know to better manage MS.
In November 2014, researchers sent an email invitation to the entire MyMSTeam community, a social network of approximately 25,000 people (currently more than 75,000 people) diagnosed with MS. In all, 1,107 members responded to the survey.
Overall, the most commonly reported symptoms were fatigue (82% of patients), problems with mobility (64%), and poor balance (64%). In addition, weakness, cognitive issues, and depression were common. The respondents defined disability progression as increased limitations on their ability to get around, having to sacrifice normal daily activities, and losing their ability to be independent. Patients measured the efficacy of DMTs by evaluating the treatments’ ability to slow progression, prevent further physical disability, prevent new lesions, and improve quality of life.
In a separate study, Dr. Livingston and colleagues conducted an analysis of organic discussions within MyMSTeam from January 2015 to April 2016. Researchers anonymized, coded, categorized, and analyzed 3,300 verbatim comments by key themes. The analysis focused on 12 DMTs. Discussions were overlaid with patient self-reported data on gender, age, date of diagnosis, MS type, current DMT, and effectiveness ratings.
Common discussion topics included side effects experienced; reasons for stopping treatment; perceived efficacy; questions, hopes, and concerns about starting a new DMT; rituals to mitigate side effects; and insurance or financial hurdles to getting on or staying on treatment.
Discussions about infusion therapies tended to focus on receiving treatment and issues related to progressive multifocal leukoencephalopathy.
When discussing Tysabri (natalizumab), patients most commonly discussed elevated energy levels post infusion around day 14. Patients also reported increased fatigue in the days prior to the next infusion and extreme fatigue on the day of treatment. In addition, patients shared their experiences with managing tolerability issues, most commonly flu-like symptoms with interferons and gastrointestinal effects with Tecfidera (dimethyl fumarate).
Dr. Livingston and colleagues said that their research “will better allow medical professionals to treat the individual holistically, and not just the disease itself. Additionally, helping patients understand MS progression will allow specialists to set realistic expectations for treating the disease and to help their patients better prepare for the future.”
Should Patients on B Cell–Depleting Therapies Be Immunized Against Influenza?
NEW ORLEANS—Immunizing patients on B cell–depleting therapies against influenza using the inactivated virus vaccine may be beneficial, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Creating virus-specific T cell immunity and boosting highly cross-reactive memory T cells from prior exposures to influenza are valuable in reducing the severity of the infection,” said Elena Grebenciucova, MD, and Eric Williamson, MD, of the Multiple Sclerosis Division of the Perelman Center for Advanced Medicine at the University of Pennsylvania in Philadelphia.
The use of B cell–depleting therapies in patients with multiple sclerosis, neuromyelitis optica, and other inflammatory disorders raises a clinical dilemma. Given that the ability to generate an adequate protective antibody response is severely impaired due to B-cell depletion, is it still beneficial to immunize patients using the inactivated influenza vaccine? The practice of vaccinating patients on B cell–depleting therapies is not universal among neurologists. Many assume that the practice has no benefit and choose not to vaccinate their patients. However, antibody-mediated immune responses are not the only part of the immune system that helps control influenza infection. T cell–mediated immunity, although affected by the absence of B cells in many complex ways, is not abolished, and may offer protection, limit severity of the disease, and reduce influenza-associated morbidity.
Drs. Grebenciucova and Williamson conducted a literature review and analysis to provide a mechanistic rationale for immunizing against influenza in patients on B cell–depleting therapies.
In 2008, Stambas et al reported that virus-specific CD8+ T effector cells are important in clearing influenza infection. They also found that CD4+ T memory cells are critical in maintaining virus-specific CD8+ memory responses. Influenza vaccine helps prime naïve T cells and generates virus-specific T cells. Vaccinating also can boost pre-existent influenza-specific memory T cells, which, unlike the specific antibodies, are effective against various strains of the virus.
Dolphi et al. showed that memory T cell CD8+ and CD4+ epitopes cross-react with internal viral protein sequences (matrix [M] and nucleoprotein [NP]) that are highly conserved among various influenza strains, and thus may offer protection even when the antibody response is either inadequate or directed against the wrong strain of the virus.
A study by Sridhar et al conducted in the setting of the 2009 H1N1 pandemic highlighted the importance of cross-reactive cellular immunity by evaluating CD8+ T cell responses prior to, during, and after the influenza infection and showed that those with pre-existent CD8+ T cells specific for highly conserved internal viral proteins experienced a less severe illness, despite the absence of neutralizing antibodies.
Wilkinson et al and McElhaney et al also showed that even in the setting of inadequate antibody responses, virus-specific T cell–mediated immunity against influenza virus offers protection and may reduce morbidity.
Suggested Reading
McElhaney JE, Kuchel GA, Zhou X, et al. T-cell immunity to influenza in older adults: a pathophysiological framework for development of more effective vaccines. Front Immunol. 2016;7:41.
Sridhar S, Begom S, Bermingham A, et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat Med. 2013;19(10):1305-1312.
Stambas J, Guillonneau C, Kedzierska K, et al. Killer T cells in influenza. Pharmacol Ther. 2008;120(2):186-196.
Wilkinson TM, Li CK, Chui CS, et al. Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans. Nat Med. 2012;18(2):274-280.
NEW ORLEANS—Immunizing patients on B cell–depleting therapies against influenza using the inactivated virus vaccine may be beneficial, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Creating virus-specific T cell immunity and boosting highly cross-reactive memory T cells from prior exposures to influenza are valuable in reducing the severity of the infection,” said Elena Grebenciucova, MD, and Eric Williamson, MD, of the Multiple Sclerosis Division of the Perelman Center for Advanced Medicine at the University of Pennsylvania in Philadelphia.
The use of B cell–depleting therapies in patients with multiple sclerosis, neuromyelitis optica, and other inflammatory disorders raises a clinical dilemma. Given that the ability to generate an adequate protective antibody response is severely impaired due to B-cell depletion, is it still beneficial to immunize patients using the inactivated influenza vaccine? The practice of vaccinating patients on B cell–depleting therapies is not universal among neurologists. Many assume that the practice has no benefit and choose not to vaccinate their patients. However, antibody-mediated immune responses are not the only part of the immune system that helps control influenza infection. T cell–mediated immunity, although affected by the absence of B cells in many complex ways, is not abolished, and may offer protection, limit severity of the disease, and reduce influenza-associated morbidity.
Drs. Grebenciucova and Williamson conducted a literature review and analysis to provide a mechanistic rationale for immunizing against influenza in patients on B cell–depleting therapies.
In 2008, Stambas et al reported that virus-specific CD8+ T effector cells are important in clearing influenza infection. They also found that CD4+ T memory cells are critical in maintaining virus-specific CD8+ memory responses. Influenza vaccine helps prime naïve T cells and generates virus-specific T cells. Vaccinating also can boost pre-existent influenza-specific memory T cells, which, unlike the specific antibodies, are effective against various strains of the virus.
Dolphi et al. showed that memory T cell CD8+ and CD4+ epitopes cross-react with internal viral protein sequences (matrix [M] and nucleoprotein [NP]) that are highly conserved among various influenza strains, and thus may offer protection even when the antibody response is either inadequate or directed against the wrong strain of the virus.
A study by Sridhar et al conducted in the setting of the 2009 H1N1 pandemic highlighted the importance of cross-reactive cellular immunity by evaluating CD8+ T cell responses prior to, during, and after the influenza infection and showed that those with pre-existent CD8+ T cells specific for highly conserved internal viral proteins experienced a less severe illness, despite the absence of neutralizing antibodies.
Wilkinson et al and McElhaney et al also showed that even in the setting of inadequate antibody responses, virus-specific T cell–mediated immunity against influenza virus offers protection and may reduce morbidity.
Suggested Reading
McElhaney JE, Kuchel GA, Zhou X, et al. T-cell immunity to influenza in older adults: a pathophysiological framework for development of more effective vaccines. Front Immunol. 2016;7:41.
Sridhar S, Begom S, Bermingham A, et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat Med. 2013;19(10):1305-1312.
Stambas J, Guillonneau C, Kedzierska K, et al. Killer T cells in influenza. Pharmacol Ther. 2008;120(2):186-196.
Wilkinson TM, Li CK, Chui CS, et al. Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans. Nat Med. 2012;18(2):274-280.
NEW ORLEANS—Immunizing patients on B cell–depleting therapies against influenza using the inactivated virus vaccine may be beneficial, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Creating virus-specific T cell immunity and boosting highly cross-reactive memory T cells from prior exposures to influenza are valuable in reducing the severity of the infection,” said Elena Grebenciucova, MD, and Eric Williamson, MD, of the Multiple Sclerosis Division of the Perelman Center for Advanced Medicine at the University of Pennsylvania in Philadelphia.
The use of B cell–depleting therapies in patients with multiple sclerosis, neuromyelitis optica, and other inflammatory disorders raises a clinical dilemma. Given that the ability to generate an adequate protective antibody response is severely impaired due to B-cell depletion, is it still beneficial to immunize patients using the inactivated influenza vaccine? The practice of vaccinating patients on B cell–depleting therapies is not universal among neurologists. Many assume that the practice has no benefit and choose not to vaccinate their patients. However, antibody-mediated immune responses are not the only part of the immune system that helps control influenza infection. T cell–mediated immunity, although affected by the absence of B cells in many complex ways, is not abolished, and may offer protection, limit severity of the disease, and reduce influenza-associated morbidity.
Drs. Grebenciucova and Williamson conducted a literature review and analysis to provide a mechanistic rationale for immunizing against influenza in patients on B cell–depleting therapies.
In 2008, Stambas et al reported that virus-specific CD8+ T effector cells are important in clearing influenza infection. They also found that CD4+ T memory cells are critical in maintaining virus-specific CD8+ memory responses. Influenza vaccine helps prime naïve T cells and generates virus-specific T cells. Vaccinating also can boost pre-existent influenza-specific memory T cells, which, unlike the specific antibodies, are effective against various strains of the virus.
Dolphi et al. showed that memory T cell CD8+ and CD4+ epitopes cross-react with internal viral protein sequences (matrix [M] and nucleoprotein [NP]) that are highly conserved among various influenza strains, and thus may offer protection even when the antibody response is either inadequate or directed against the wrong strain of the virus.
A study by Sridhar et al conducted in the setting of the 2009 H1N1 pandemic highlighted the importance of cross-reactive cellular immunity by evaluating CD8+ T cell responses prior to, during, and after the influenza infection and showed that those with pre-existent CD8+ T cells specific for highly conserved internal viral proteins experienced a less severe illness, despite the absence of neutralizing antibodies.
Wilkinson et al and McElhaney et al also showed that even in the setting of inadequate antibody responses, virus-specific T cell–mediated immunity against influenza virus offers protection and may reduce morbidity.
Suggested Reading
McElhaney JE, Kuchel GA, Zhou X, et al. T-cell immunity to influenza in older adults: a pathophysiological framework for development of more effective vaccines. Front Immunol. 2016;7:41.
Sridhar S, Begom S, Bermingham A, et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat Med. 2013;19(10):1305-1312.
Stambas J, Guillonneau C, Kedzierska K, et al. Killer T cells in influenza. Pharmacol Ther. 2008;120(2):186-196.
Wilkinson TM, Li CK, Chui CS, et al. Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans. Nat Med. 2012;18(2):274-280.
Does a High-Quality Diet Affect Disability Status in Patients With MS?
NEW ORLEANS—A diet high in fruits, vegetables, legumes, and whole grains and low in sugar and red meat is associated with less disability and fewer depressive symptoms in patients with multiple sclerosis (MS), according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Our findings suggest that people with MS who have a healthier diet have less disability, and that a generally healthy lifestyle is associated with a lower burden of severe depression, pain, fatigue, and cognitive problems. Therefore, modifying diet may offer a way of improving symptoms,” said Ruth Ann Marrie, MD, PhD, Associate Professor of Neurology and Director of the MS Clinic at the University of Manitoba in Winnipeg, Canada.
Many patients with MS ask whether their diet could influence their disease status. To address this question, Dr. Marrie and colleagues assessed the association between overall diet quality and disability and physical and mental functioning in a large cohort of people with MS. They conducted a cross-sectional study of North American Research Committee on MS (NARCOMS) registry participants who had completed a dietary screener questionnaire. The questionnaire, created by the National Health and Nutrition Examination Survey, provides an assessment of diet composition when full information on diet is unavailable. The survey estimates intake of fruits, vegetables and legumes, whole grains, added sugars, and red and processed meats.
The researchers constructed an overall diet-quality score based on responses to the questionnaire and assigned participants to sex-specific quintiles of each of the questionnaire’s five food groups. They then assigned scores for fruits, vegetables, legumes, and whole grains based on the patient’s quintile ranking. The investigators inverted scores for red and processed meats and added sugar. The researchers summed individual food-group scores to obtain an overall diet score, ranging from 4 (poor quality) to 20 (high quality).
Dr. Marrie and colleagues assessed the association between diet quality and disability status (using the Patient-Determined Disease Steps) and mental and physical functioning (ie, depression, fatigue, cognition, mobility, vision, pain, spasticity, tremor, and sensory function) using proportional odds models adjusting for age, gender, income, BMI, smoking status, and disease duration.
In all, 7,418 responders had an average quality-diet score of 11.9. Patients with higher scores tended to be older, leaner, and nonsmokers. People with diet-quality scores in the top quintile had lower levels of disability and lower depression scores. Diet-quality scores were not associated with other physical or mental functioning scores, however.
A lack of details about potentially important dietary factors, such as types of fat, is one limitation of the study, said Dr. Marrie.
“While our study does not prove that diet change will improve symptoms, a high-quality diet that emphasizes intake of fruits, vegetables, and whole grains, and lower intake of red meat, can be encouraged, given the known benefits for general health,” said Dr. Marrie. “Future studies should look at the relationship between diet and disability, as well as symptoms over time, so that we can establish whether changing diet will improve outcomes in MS. These studies should also look at diet in more detail.”
The National MS Society supported this study.
—Erica Tricarico
NEW ORLEANS—A diet high in fruits, vegetables, legumes, and whole grains and low in sugar and red meat is associated with less disability and fewer depressive symptoms in patients with multiple sclerosis (MS), according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Our findings suggest that people with MS who have a healthier diet have less disability, and that a generally healthy lifestyle is associated with a lower burden of severe depression, pain, fatigue, and cognitive problems. Therefore, modifying diet may offer a way of improving symptoms,” said Ruth Ann Marrie, MD, PhD, Associate Professor of Neurology and Director of the MS Clinic at the University of Manitoba in Winnipeg, Canada.
Many patients with MS ask whether their diet could influence their disease status. To address this question, Dr. Marrie and colleagues assessed the association between overall diet quality and disability and physical and mental functioning in a large cohort of people with MS. They conducted a cross-sectional study of North American Research Committee on MS (NARCOMS) registry participants who had completed a dietary screener questionnaire. The questionnaire, created by the National Health and Nutrition Examination Survey, provides an assessment of diet composition when full information on diet is unavailable. The survey estimates intake of fruits, vegetables and legumes, whole grains, added sugars, and red and processed meats.
The researchers constructed an overall diet-quality score based on responses to the questionnaire and assigned participants to sex-specific quintiles of each of the questionnaire’s five food groups. They then assigned scores for fruits, vegetables, legumes, and whole grains based on the patient’s quintile ranking. The investigators inverted scores for red and processed meats and added sugar. The researchers summed individual food-group scores to obtain an overall diet score, ranging from 4 (poor quality) to 20 (high quality).
Dr. Marrie and colleagues assessed the association between diet quality and disability status (using the Patient-Determined Disease Steps) and mental and physical functioning (ie, depression, fatigue, cognition, mobility, vision, pain, spasticity, tremor, and sensory function) using proportional odds models adjusting for age, gender, income, BMI, smoking status, and disease duration.
In all, 7,418 responders had an average quality-diet score of 11.9. Patients with higher scores tended to be older, leaner, and nonsmokers. People with diet-quality scores in the top quintile had lower levels of disability and lower depression scores. Diet-quality scores were not associated with other physical or mental functioning scores, however.
A lack of details about potentially important dietary factors, such as types of fat, is one limitation of the study, said Dr. Marrie.
“While our study does not prove that diet change will improve symptoms, a high-quality diet that emphasizes intake of fruits, vegetables, and whole grains, and lower intake of red meat, can be encouraged, given the known benefits for general health,” said Dr. Marrie. “Future studies should look at the relationship between diet and disability, as well as symptoms over time, so that we can establish whether changing diet will improve outcomes in MS. These studies should also look at diet in more detail.”
The National MS Society supported this study.
—Erica Tricarico
NEW ORLEANS—A diet high in fruits, vegetables, legumes, and whole grains and low in sugar and red meat is associated with less disability and fewer depressive symptoms in patients with multiple sclerosis (MS), according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Our findings suggest that people with MS who have a healthier diet have less disability, and that a generally healthy lifestyle is associated with a lower burden of severe depression, pain, fatigue, and cognitive problems. Therefore, modifying diet may offer a way of improving symptoms,” said Ruth Ann Marrie, MD, PhD, Associate Professor of Neurology and Director of the MS Clinic at the University of Manitoba in Winnipeg, Canada.
Many patients with MS ask whether their diet could influence their disease status. To address this question, Dr. Marrie and colleagues assessed the association between overall diet quality and disability and physical and mental functioning in a large cohort of people with MS. They conducted a cross-sectional study of North American Research Committee on MS (NARCOMS) registry participants who had completed a dietary screener questionnaire. The questionnaire, created by the National Health and Nutrition Examination Survey, provides an assessment of diet composition when full information on diet is unavailable. The survey estimates intake of fruits, vegetables and legumes, whole grains, added sugars, and red and processed meats.
The researchers constructed an overall diet-quality score based on responses to the questionnaire and assigned participants to sex-specific quintiles of each of the questionnaire’s five food groups. They then assigned scores for fruits, vegetables, legumes, and whole grains based on the patient’s quintile ranking. The investigators inverted scores for red and processed meats and added sugar. The researchers summed individual food-group scores to obtain an overall diet score, ranging from 4 (poor quality) to 20 (high quality).
Dr. Marrie and colleagues assessed the association between diet quality and disability status (using the Patient-Determined Disease Steps) and mental and physical functioning (ie, depression, fatigue, cognition, mobility, vision, pain, spasticity, tremor, and sensory function) using proportional odds models adjusting for age, gender, income, BMI, smoking status, and disease duration.
In all, 7,418 responders had an average quality-diet score of 11.9. Patients with higher scores tended to be older, leaner, and nonsmokers. People with diet-quality scores in the top quintile had lower levels of disability and lower depression scores. Diet-quality scores were not associated with other physical or mental functioning scores, however.
A lack of details about potentially important dietary factors, such as types of fat, is one limitation of the study, said Dr. Marrie.
“While our study does not prove that diet change will improve symptoms, a high-quality diet that emphasizes intake of fruits, vegetables, and whole grains, and lower intake of red meat, can be encouraged, given the known benefits for general health,” said Dr. Marrie. “Future studies should look at the relationship between diet and disability, as well as symptoms over time, so that we can establish whether changing diet will improve outcomes in MS. These studies should also look at diet in more detail.”
The National MS Society supported this study.
—Erica Tricarico
Light Physical Activity May Improve Physical Function in Older Patients With MS
NEW ORLEANS—Older adults with multiple sclerosis (MS) who engaged more in light physical activity demonstrated better physical function independent of sedentary behavior and moderate-to-vigorous activity, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Such results might underscore light physical activity as a suitable target of future rehabilitative interventions for improving physical function in older adults with MS,” said Katie L.J. Cederberg, a doctoral student at the University of Alabama at Birmingham.
Rate and pattern of participation in physical activity and sedentary behavior might be associated with a reduction of physical function among older adults with MS. Ms. Cederberg conducted a study that examined the associations among levels of light and moderate-to-vigorous physical activity, sedentary behavior, and physical function in older adults with MS.
Ms. Cederberg’s study sample included 40 older adults with MS with a median age of 60. Participants wore an accelerometer during the waking hours of a seven-day period. In addition, Ms. Cederberg used cut-points for MS to process data for time spent in moderate-to-vigorous physical activity, light physical activity, and sedentary behavior. Finally, patients completed the Short Physical Performance Battery (SPPB), the Six-Minute Walk Test, and the Timed 25-Foot Walk.
The median scores for time spent in moderate-to-vigorous physical activity and light physical activity were lower, and sedentary behavior was significantly greater, than those reported for older adults in the general population.
In addition, bivariate correlation analyses suggested that light physical activity and moderate to vigorous physical activity were associated with SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores, but the association was stronger for light physical activity. Regression analyses yielded significant associations between light physical activity, but not moderate-to-vigorous physical activity or sedentary behavior, and SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores.
NEW ORLEANS—Older adults with multiple sclerosis (MS) who engaged more in light physical activity demonstrated better physical function independent of sedentary behavior and moderate-to-vigorous activity, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Such results might underscore light physical activity as a suitable target of future rehabilitative interventions for improving physical function in older adults with MS,” said Katie L.J. Cederberg, a doctoral student at the University of Alabama at Birmingham.
Rate and pattern of participation in physical activity and sedentary behavior might be associated with a reduction of physical function among older adults with MS. Ms. Cederberg conducted a study that examined the associations among levels of light and moderate-to-vigorous physical activity, sedentary behavior, and physical function in older adults with MS.
Ms. Cederberg’s study sample included 40 older adults with MS with a median age of 60. Participants wore an accelerometer during the waking hours of a seven-day period. In addition, Ms. Cederberg used cut-points for MS to process data for time spent in moderate-to-vigorous physical activity, light physical activity, and sedentary behavior. Finally, patients completed the Short Physical Performance Battery (SPPB), the Six-Minute Walk Test, and the Timed 25-Foot Walk.
The median scores for time spent in moderate-to-vigorous physical activity and light physical activity were lower, and sedentary behavior was significantly greater, than those reported for older adults in the general population.
In addition, bivariate correlation analyses suggested that light physical activity and moderate to vigorous physical activity were associated with SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores, but the association was stronger for light physical activity. Regression analyses yielded significant associations between light physical activity, but not moderate-to-vigorous physical activity or sedentary behavior, and SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores.
NEW ORLEANS—Older adults with multiple sclerosis (MS) who engaged more in light physical activity demonstrated better physical function independent of sedentary behavior and moderate-to-vigorous activity, according to research presented at the 31st Annual Meeting of the Consortium of MS Centers.
“Such results might underscore light physical activity as a suitable target of future rehabilitative interventions for improving physical function in older adults with MS,” said Katie L.J. Cederberg, a doctoral student at the University of Alabama at Birmingham.
Rate and pattern of participation in physical activity and sedentary behavior might be associated with a reduction of physical function among older adults with MS. Ms. Cederberg conducted a study that examined the associations among levels of light and moderate-to-vigorous physical activity, sedentary behavior, and physical function in older adults with MS.
Ms. Cederberg’s study sample included 40 older adults with MS with a median age of 60. Participants wore an accelerometer during the waking hours of a seven-day period. In addition, Ms. Cederberg used cut-points for MS to process data for time spent in moderate-to-vigorous physical activity, light physical activity, and sedentary behavior. Finally, patients completed the Short Physical Performance Battery (SPPB), the Six-Minute Walk Test, and the Timed 25-Foot Walk.
The median scores for time spent in moderate-to-vigorous physical activity and light physical activity were lower, and sedentary behavior was significantly greater, than those reported for older adults in the general population.
In addition, bivariate correlation analyses suggested that light physical activity and moderate to vigorous physical activity were associated with SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores, but the association was stronger for light physical activity. Regression analyses yielded significant associations between light physical activity, but not moderate-to-vigorous physical activity or sedentary behavior, and SPPB, Six-Minute Walk Test, and Timed 25-Foot Walk scores.
Number Needed to Treat Analyses Comparing Alemtuzumab With Ocrelizumab
NEW ORLEANS—Two-year analyses show that fewer patients required treatment with alemtuzumab than ocrelizumab to prevent one relapse, to prevent relapse in one patient, and to prevent six-month confirmed disability worsening in one patient versus subcutaneous interferon beta-1a, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers.
In the absence of head-to-head trials, researchers can use the number needed to treat to indirectly assess the comparative efficacy of disease-modifying therapies. Aaron L. Boster, MD, and colleagues analyzed the number needed to treat to prevent clinical disease events in studies of alemtuzumab and ocrelizumab in relapsing-remitting multiple sclerosis (MS). Dr. Boster is a clinical neuroimmunologist at the OhioHealth MS Clinic in Columbus.
Number needed to treat values were derived from post hoc analyses of two-year data from studies of alemtuzumab (12 mg) and ocrelizumab (600 mg). Alemtuzumab data were of pooled treatment-naive patients from the CAMMS223 and CARE-MS I studies (n = 786), and separately, patients with inadequate response to prior therapy from CARE-MS II (n = 628). Ocrelizumab data were derived from the OPERA I and II studies (n = 821 and n = 835, respectively). Alemtuzumab was administered as two annual courses; ocrelizumab was administered at baseline and weeks 24, 48, and 72. Number needed to treat was based on inverse of absolute risk differences versus subcutaneous interferon beta-1a 44 μg three times per week (common comparator) for annualized relapse rate and proportion of patients experiencing relapse, and the Altman method for six-month confirmed disability worsening. Lower number needed to treat values reflect greater efficacy.
Baseline mean Expanded Disability Status Scale (EDSS) scores were 2.0 for CAMMS223 and CARE-MS I, 2.7 for CARE-MS II, 2.9 for OPERA I, and 2.8 for OPERA II. Mean MS duration was 1.9 years in CAMMS223 and CARE-MS I, 4.5 years in CARE-MS II, and 6.7 years in OPERA I and II. Mean number of relapses in the previous two years was 2.5 for CAMMS223 and CARE-MS I, 2.8 for CARE-MS II, and 1.8 in OPERA I and II.
Alemtuzumab and ocrelizumab significantly reduced annualized relapse rates and confirmed disability worsening versus subcutaneous interferon beta-1a. Number needed to treat values to prevent one relapse versus subcutaneous interferon beta-1a were lower with alemtuzumab (CAMMS223/CARE-MS I: five; CARE-MS II: four) than with ocrelizumab (OPERA I/II: eight in each study), as were number needed to treat values to prevent one patient from experiencing relapse (CAMMS223/CARE-MS I and CARE-MS II: six in each study; OPERA I and II: eight in each study), and to prevent one patient from experiencing six-month confirmed disability worsening (CAMMS223/CARE-MS I: 15; CARE-MS II: 13; OPERA I: 23; OPERA II: 21).
Although the populations in the available datasets differ, these findings suggest a benefit of alemtuzumab over ocrelizumab.
This study was supported by Sanofi Genzyme.
NEW ORLEANS—Two-year analyses show that fewer patients required treatment with alemtuzumab than ocrelizumab to prevent one relapse, to prevent relapse in one patient, and to prevent six-month confirmed disability worsening in one patient versus subcutaneous interferon beta-1a, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers.
In the absence of head-to-head trials, researchers can use the number needed to treat to indirectly assess the comparative efficacy of disease-modifying therapies. Aaron L. Boster, MD, and colleagues analyzed the number needed to treat to prevent clinical disease events in studies of alemtuzumab and ocrelizumab in relapsing-remitting multiple sclerosis (MS). Dr. Boster is a clinical neuroimmunologist at the OhioHealth MS Clinic in Columbus.
Number needed to treat values were derived from post hoc analyses of two-year data from studies of alemtuzumab (12 mg) and ocrelizumab (600 mg). Alemtuzumab data were of pooled treatment-naive patients from the CAMMS223 and CARE-MS I studies (n = 786), and separately, patients with inadequate response to prior therapy from CARE-MS II (n = 628). Ocrelizumab data were derived from the OPERA I and II studies (n = 821 and n = 835, respectively). Alemtuzumab was administered as two annual courses; ocrelizumab was administered at baseline and weeks 24, 48, and 72. Number needed to treat was based on inverse of absolute risk differences versus subcutaneous interferon beta-1a 44 μg three times per week (common comparator) for annualized relapse rate and proportion of patients experiencing relapse, and the Altman method for six-month confirmed disability worsening. Lower number needed to treat values reflect greater efficacy.
Baseline mean Expanded Disability Status Scale (EDSS) scores were 2.0 for CAMMS223 and CARE-MS I, 2.7 for CARE-MS II, 2.9 for OPERA I, and 2.8 for OPERA II. Mean MS duration was 1.9 years in CAMMS223 and CARE-MS I, 4.5 years in CARE-MS II, and 6.7 years in OPERA I and II. Mean number of relapses in the previous two years was 2.5 for CAMMS223 and CARE-MS I, 2.8 for CARE-MS II, and 1.8 in OPERA I and II.
Alemtuzumab and ocrelizumab significantly reduced annualized relapse rates and confirmed disability worsening versus subcutaneous interferon beta-1a. Number needed to treat values to prevent one relapse versus subcutaneous interferon beta-1a were lower with alemtuzumab (CAMMS223/CARE-MS I: five; CARE-MS II: four) than with ocrelizumab (OPERA I/II: eight in each study), as were number needed to treat values to prevent one patient from experiencing relapse (CAMMS223/CARE-MS I and CARE-MS II: six in each study; OPERA I and II: eight in each study), and to prevent one patient from experiencing six-month confirmed disability worsening (CAMMS223/CARE-MS I: 15; CARE-MS II: 13; OPERA I: 23; OPERA II: 21).
Although the populations in the available datasets differ, these findings suggest a benefit of alemtuzumab over ocrelizumab.
This study was supported by Sanofi Genzyme.
NEW ORLEANS—Two-year analyses show that fewer patients required treatment with alemtuzumab than ocrelizumab to prevent one relapse, to prevent relapse in one patient, and to prevent six-month confirmed disability worsening in one patient versus subcutaneous interferon beta-1a, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers.
In the absence of head-to-head trials, researchers can use the number needed to treat to indirectly assess the comparative efficacy of disease-modifying therapies. Aaron L. Boster, MD, and colleagues analyzed the number needed to treat to prevent clinical disease events in studies of alemtuzumab and ocrelizumab in relapsing-remitting multiple sclerosis (MS). Dr. Boster is a clinical neuroimmunologist at the OhioHealth MS Clinic in Columbus.
Number needed to treat values were derived from post hoc analyses of two-year data from studies of alemtuzumab (12 mg) and ocrelizumab (600 mg). Alemtuzumab data were of pooled treatment-naive patients from the CAMMS223 and CARE-MS I studies (n = 786), and separately, patients with inadequate response to prior therapy from CARE-MS II (n = 628). Ocrelizumab data were derived from the OPERA I and II studies (n = 821 and n = 835, respectively). Alemtuzumab was administered as two annual courses; ocrelizumab was administered at baseline and weeks 24, 48, and 72. Number needed to treat was based on inverse of absolute risk differences versus subcutaneous interferon beta-1a 44 μg three times per week (common comparator) for annualized relapse rate and proportion of patients experiencing relapse, and the Altman method for six-month confirmed disability worsening. Lower number needed to treat values reflect greater efficacy.
Baseline mean Expanded Disability Status Scale (EDSS) scores were 2.0 for CAMMS223 and CARE-MS I, 2.7 for CARE-MS II, 2.9 for OPERA I, and 2.8 for OPERA II. Mean MS duration was 1.9 years in CAMMS223 and CARE-MS I, 4.5 years in CARE-MS II, and 6.7 years in OPERA I and II. Mean number of relapses in the previous two years was 2.5 for CAMMS223 and CARE-MS I, 2.8 for CARE-MS II, and 1.8 in OPERA I and II.
Alemtuzumab and ocrelizumab significantly reduced annualized relapse rates and confirmed disability worsening versus subcutaneous interferon beta-1a. Number needed to treat values to prevent one relapse versus subcutaneous interferon beta-1a were lower with alemtuzumab (CAMMS223/CARE-MS I: five; CARE-MS II: four) than with ocrelizumab (OPERA I/II: eight in each study), as were number needed to treat values to prevent one patient from experiencing relapse (CAMMS223/CARE-MS I and CARE-MS II: six in each study; OPERA I and II: eight in each study), and to prevent one patient from experiencing six-month confirmed disability worsening (CAMMS223/CARE-MS I: 15; CARE-MS II: 13; OPERA I: 23; OPERA II: 21).
Although the populations in the available datasets differ, these findings suggest a benefit of alemtuzumab over ocrelizumab.
This study was supported by Sanofi Genzyme.