User login
Liquid biopsy may help guide treatment decisions in prostate cancer
Analysis of the phenotypic and genotypic profile of circulating tumor cells (CTCs) – a so-called liquid biopsy – may help guide treatment decisions in men with castration-resistant metastatic prostate cancer, according to a cohort study being reported at the Genitourinary Cancers Symposium.
Investigators analyzed CTCs in 221 blood samples from 179 patients with metastatic prostate cancer about to begin either hormonal therapy (enzalutamide or abiraterone) or chemotherapy based on a taxane (docetaxel or cabazitaxel).
Among patients given hormonal therapy, those whose CTCs exhibited high versus low scores for phenotypic heterogeneity had poorer radiographic progression-free survival (5 months vs. 17 months) and overall survival (9 months vs. not reached), first author Dr. Howard I. Scher reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
In contrast, among those given chemotherapy, heterogeneity score did not affect these outcomes.
In other key findings, the heterogeneity score increased with each additional line of therapy patients received in the metastatic setting.
“We were able to show that single cell morphology, protein, and genomic characterization is feasible and can be used to assess tumor heterogeneity,” commented Dr. Scher of the Genitourinary Oncology Service at the Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “For characterizing disease at the point of decision making, a noninvasive liquid biopsy that enables the characterization of individual cells from a patient with metastatic prostate cancer can be used to guide treatment selection. Clinical trials to validate these findings are currently in development.”
He speculated that CTC heterogeneity was important only for hormonal therapy because it is a targeted therapy; as the disease becomes more diverse, essentially evolving into multiple diseases, this therapy is less likely to be effective. “The mechanism of taxanes is more general and not quite as targeted as these specific agents, which is why we believe they are more effective in a more diverse population,” he explained.
ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal, commented, “This is really fascinating work. We’ve always relied on a patient’s tumor to get genetic information, but that can be incredibly complicated for a number of reasons.” Among them, metastases may be located in hard-to-biopsy locations, and it is not practical to repeatedly perform needle biopsies over time.
The new findings show that “prostate cancer appears to get more complex over time as the disease evolves. The genetic diversity, quote unquote, increases, potentially suggesting that the cancer cell is crafting machinery to resist treatment,” he said.
From the clinical perspective, the ability to link CTC characteristics to response or lack thereof to a given therapy “is of incredible value,” according to Dr. Pal of the City of Hope, Duarte, Calif. “We have a number of new treatments for advanced prostate cancer and right now, we have little means of personalizing them and offering the right treatment to the right patient. With the studies that Dr. Scher has proposed to potentially validate this modality, we would have this personalized selection tool in our hands.”
Giving some background to the research, Dr. Scher noted, “Tissues are composed of a mixture of cells that differ morphologically and biologically. The result is diversity at single sites and multiple sites, broadly termed heterogeneity, so that we are not treating a single disease but a collection of diseases, and that is one reason we have difficulty achieving cures.”
“One could think of the blood as sampling, at least in theory, from all of the metastatic sites that are present. And we think you’ll have a greater chance of getting a more relevant characterization of the disease as a whole, in particular, by looking at the individual cells,” he further noted.
In the study, the investigators collected CTCs from blood samples, deposited them onto slides, stained them with DAPI and for various proteins (cytokeratin, androgen receptor, and CD45), and then scanned them, using a commercial platform (Epic Sciences).
They analyzed morphologic and phenotypic features of 9,225 single CTCs, splitting them into 15 distinct subtypes. They also performed whole-genome sequencing in a subset of 741 CTCs to assess copy number variation, clonality, and gene amplifications and deletions.
“The samples can be run quickly, and you can get results within 48 hours, which is important if you are trying to make a treatment decision,” Dr. Scher noted.
Findings showed that among patients given hormonal therapy, a high versus low CTC heterogeneity score was associated with much greater risks of radiographic progression-free survival events (hazard ratio, 2.2; P = .00182) and death (HR, 5.5; P less than .0001). In contrast, among patients who received taxane-based chemotherapy, CTC heterogeneity did not significantly affect either outcome.
Analysis of the phenotypic and genotypic profile of circulating tumor cells (CTCs) – a so-called liquid biopsy – may help guide treatment decisions in men with castration-resistant metastatic prostate cancer, according to a cohort study being reported at the Genitourinary Cancers Symposium.
Investigators analyzed CTCs in 221 blood samples from 179 patients with metastatic prostate cancer about to begin either hormonal therapy (enzalutamide or abiraterone) or chemotherapy based on a taxane (docetaxel or cabazitaxel).
Among patients given hormonal therapy, those whose CTCs exhibited high versus low scores for phenotypic heterogeneity had poorer radiographic progression-free survival (5 months vs. 17 months) and overall survival (9 months vs. not reached), first author Dr. Howard I. Scher reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
In contrast, among those given chemotherapy, heterogeneity score did not affect these outcomes.
In other key findings, the heterogeneity score increased with each additional line of therapy patients received in the metastatic setting.
“We were able to show that single cell morphology, protein, and genomic characterization is feasible and can be used to assess tumor heterogeneity,” commented Dr. Scher of the Genitourinary Oncology Service at the Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “For characterizing disease at the point of decision making, a noninvasive liquid biopsy that enables the characterization of individual cells from a patient with metastatic prostate cancer can be used to guide treatment selection. Clinical trials to validate these findings are currently in development.”
He speculated that CTC heterogeneity was important only for hormonal therapy because it is a targeted therapy; as the disease becomes more diverse, essentially evolving into multiple diseases, this therapy is less likely to be effective. “The mechanism of taxanes is more general and not quite as targeted as these specific agents, which is why we believe they are more effective in a more diverse population,” he explained.
ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal, commented, “This is really fascinating work. We’ve always relied on a patient’s tumor to get genetic information, but that can be incredibly complicated for a number of reasons.” Among them, metastases may be located in hard-to-biopsy locations, and it is not practical to repeatedly perform needle biopsies over time.
The new findings show that “prostate cancer appears to get more complex over time as the disease evolves. The genetic diversity, quote unquote, increases, potentially suggesting that the cancer cell is crafting machinery to resist treatment,” he said.
From the clinical perspective, the ability to link CTC characteristics to response or lack thereof to a given therapy “is of incredible value,” according to Dr. Pal of the City of Hope, Duarte, Calif. “We have a number of new treatments for advanced prostate cancer and right now, we have little means of personalizing them and offering the right treatment to the right patient. With the studies that Dr. Scher has proposed to potentially validate this modality, we would have this personalized selection tool in our hands.”
Giving some background to the research, Dr. Scher noted, “Tissues are composed of a mixture of cells that differ morphologically and biologically. The result is diversity at single sites and multiple sites, broadly termed heterogeneity, so that we are not treating a single disease but a collection of diseases, and that is one reason we have difficulty achieving cures.”
“One could think of the blood as sampling, at least in theory, from all of the metastatic sites that are present. And we think you’ll have a greater chance of getting a more relevant characterization of the disease as a whole, in particular, by looking at the individual cells,” he further noted.
In the study, the investigators collected CTCs from blood samples, deposited them onto slides, stained them with DAPI and for various proteins (cytokeratin, androgen receptor, and CD45), and then scanned them, using a commercial platform (Epic Sciences).
They analyzed morphologic and phenotypic features of 9,225 single CTCs, splitting them into 15 distinct subtypes. They also performed whole-genome sequencing in a subset of 741 CTCs to assess copy number variation, clonality, and gene amplifications and deletions.
“The samples can be run quickly, and you can get results within 48 hours, which is important if you are trying to make a treatment decision,” Dr. Scher noted.
Findings showed that among patients given hormonal therapy, a high versus low CTC heterogeneity score was associated with much greater risks of radiographic progression-free survival events (hazard ratio, 2.2; P = .00182) and death (HR, 5.5; P less than .0001). In contrast, among patients who received taxane-based chemotherapy, CTC heterogeneity did not significantly affect either outcome.
Analysis of the phenotypic and genotypic profile of circulating tumor cells (CTCs) – a so-called liquid biopsy – may help guide treatment decisions in men with castration-resistant metastatic prostate cancer, according to a cohort study being reported at the Genitourinary Cancers Symposium.
Investigators analyzed CTCs in 221 blood samples from 179 patients with metastatic prostate cancer about to begin either hormonal therapy (enzalutamide or abiraterone) or chemotherapy based on a taxane (docetaxel or cabazitaxel).
Among patients given hormonal therapy, those whose CTCs exhibited high versus low scores for phenotypic heterogeneity had poorer radiographic progression-free survival (5 months vs. 17 months) and overall survival (9 months vs. not reached), first author Dr. Howard I. Scher reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
In contrast, among those given chemotherapy, heterogeneity score did not affect these outcomes.
In other key findings, the heterogeneity score increased with each additional line of therapy patients received in the metastatic setting.
“We were able to show that single cell morphology, protein, and genomic characterization is feasible and can be used to assess tumor heterogeneity,” commented Dr. Scher of the Genitourinary Oncology Service at the Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “For characterizing disease at the point of decision making, a noninvasive liquid biopsy that enables the characterization of individual cells from a patient with metastatic prostate cancer can be used to guide treatment selection. Clinical trials to validate these findings are currently in development.”
He speculated that CTC heterogeneity was important only for hormonal therapy because it is a targeted therapy; as the disease becomes more diverse, essentially evolving into multiple diseases, this therapy is less likely to be effective. “The mechanism of taxanes is more general and not quite as targeted as these specific agents, which is why we believe they are more effective in a more diverse population,” he explained.
ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal, commented, “This is really fascinating work. We’ve always relied on a patient’s tumor to get genetic information, but that can be incredibly complicated for a number of reasons.” Among them, metastases may be located in hard-to-biopsy locations, and it is not practical to repeatedly perform needle biopsies over time.
The new findings show that “prostate cancer appears to get more complex over time as the disease evolves. The genetic diversity, quote unquote, increases, potentially suggesting that the cancer cell is crafting machinery to resist treatment,” he said.
From the clinical perspective, the ability to link CTC characteristics to response or lack thereof to a given therapy “is of incredible value,” according to Dr. Pal of the City of Hope, Duarte, Calif. “We have a number of new treatments for advanced prostate cancer and right now, we have little means of personalizing them and offering the right treatment to the right patient. With the studies that Dr. Scher has proposed to potentially validate this modality, we would have this personalized selection tool in our hands.”
Giving some background to the research, Dr. Scher noted, “Tissues are composed of a mixture of cells that differ morphologically and biologically. The result is diversity at single sites and multiple sites, broadly termed heterogeneity, so that we are not treating a single disease but a collection of diseases, and that is one reason we have difficulty achieving cures.”
“One could think of the blood as sampling, at least in theory, from all of the metastatic sites that are present. And we think you’ll have a greater chance of getting a more relevant characterization of the disease as a whole, in particular, by looking at the individual cells,” he further noted.
In the study, the investigators collected CTCs from blood samples, deposited them onto slides, stained them with DAPI and for various proteins (cytokeratin, androgen receptor, and CD45), and then scanned them, using a commercial platform (Epic Sciences).
They analyzed morphologic and phenotypic features of 9,225 single CTCs, splitting them into 15 distinct subtypes. They also performed whole-genome sequencing in a subset of 741 CTCs to assess copy number variation, clonality, and gene amplifications and deletions.
“The samples can be run quickly, and you can get results within 48 hours, which is important if you are trying to make a treatment decision,” Dr. Scher noted.
Findings showed that among patients given hormonal therapy, a high versus low CTC heterogeneity score was associated with much greater risks of radiographic progression-free survival events (hazard ratio, 2.2; P = .00182) and death (HR, 5.5; P less than .0001). In contrast, among patients who received taxane-based chemotherapy, CTC heterogeneity did not significantly affect either outcome.
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: In patients with castration-resistant metastatic prostate cancer, CTC heterogeneity affects the response to hormonal therapy but not to chemotherapy.
Major finding: A high vs. low CTC heterogeneity score was associated with shorter median progression-free survival (5 vs. 17 months) and overall survival (9 months vs. not reached) with hormonal therapy but did not affect these outcomes with chemotherapy.
Data source: A cohort study of 179 patients with castration-resistant metastatic prostate cancer about to begin either hormonal therapy or taxane-based chemotherapy.
Disclosures: Dr. Scher disclosed that he has a consulting or advisory role, and receives travel, accommodations, and/or expenses from numerous pharmaceutical companies. He receives research funding (institutional) from BIND Biosciences, Exelixis, Janssen Pharmaceuticals, Medivation, Janssen Diagnostics, and Innocrin Pharmaceuticals. The study received funding from the Prostate Cancer Foundation, MSKCC SPORE, and MSKCC Core Grant. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.
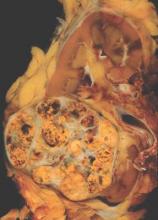
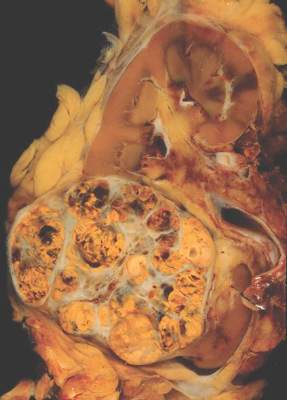
METEOR: Cabozantinib bests everolimus across renal cancer subgroups
The oral multitargeted tyrosine kinase inhibitor cabozantinib is more efficacious than everolimus as therapy for advanced renal cell carcinoma across a wide range of patients, suggests a subgroup analysis of the phase III METEOR trial being reported at the genitourinary cancers symposium.
Trial participants were 658 patients with advanced renal cell carcinoma and clear cell histology who had experienced progression on a tyrosine kinase inhibitor targeting the vascular endothelial growth factor receptor (VEGFR). There was no limit on the number of prior therapies.
The patients were randomized evenly to cabozantinib (Cometriq), which inhibits the VEGFR, MET, and AXL tyrosine kinases – all of which are up-regulated in this cancer – or to everolimus (Afinitor), an inhibitor of the mammalian target of rapamycin that is considered a standard of care. (At present, cabozantinib is approved by the Food and Drug Administration for the treatment of medullary thyroid cancer.)
Results for the entire trial population showed that patients in the cabozantinib group were about half as likely as were their counterparts in the everolimus group to experience progression-free survival events, lead author Dr. Bernard Escudier reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology. All patients appeared to derive benefit, with the reduction in risk ranging from 16% to 78% depending on the specific subgroup.
“Cabozantinib improved progression-free survival, compared to one of our standard therapies, everolimus, in advanced renal cell carcinoma,” concluded Dr. Escudier, who is chair of the Genitourinary Oncology Committee at the Institut Gustave Roussy in Villejuif, France. “Benefit was observed across prespecified subgroups,” including a small subgroup who had previously received immunotherapies targeting the programmed death 1 (PD-1) signaling pathway.
Toxicity was somewhat problematic with cabozantinib, despite starting the drug at a lower dose than has typically been used in the past, he acknowledged. The most common side effects were diarrhea, fatigue, nausea, decreased appetite, and hand-foot syndrome, and they often necessitated further dose reductions.
“Benefit with cabozantinib treatment is supported by a trend in overall survival, and hopefully, we will give this final overall survival analysis at ASCO this year,” Dr. Escudier added. Findings of an interim analysis reported last year were very promising with respect to this outcome (hazard ratio, 0.67; P = .005) (N Engl J Med. 2015 Nov 5;373:1814-23).
“This study is unique compared to others in that it allowed a broad range of patients: Patients could have had spread of cancer to the brain, they could have received any number of prior therapies, and they could have been exposed to immune-based treatments,” commented ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal. “The magnitude of benefit that patients got from cabozantinib far exceeds, in my opinion, what we have seen to date in this setting in terms of both delay in tumor growth and improving survival.”
In fact, for some oncologists, the findings may be strong enough to prompt use of cabozantinib as second-line therapy, according to Dr. Pal, who is a medical oncologist at the City of Hope in Duarte, Calif.
“Given the fact that cabozantinib has a very compelling benefit in terms of both delay in tumor growth and a hint toward a benefit in terms of overall survival, I would perhaps tend to favor that as a second-line option as compared to other comparators, such as nivolumab (Opdivo), in that setting,” he said, referring to an antibody that targets the cell surface receptor PD-1. “Now that’s a personal opinion. I certainly think there are some merits with nivolumab, such as the toxicity profile. But, in broad terms, patients are very focused on clinical efficacy, and with that in mind, the data for cabozantinib truly speaks for itself.”
But Dr. Escudier offered a more-reserved perspective. “I think what people are going to do will be to use nivolumab as second-line [therapy] in most patients and keep cabozantinib for nivolumab failure,” he predicted. “Based on that, this subgroup, although small, is of importance. I don’t think it’s good enough to say we should use cabozantinib or nivolumab in second line based on the subgroup analyses we have.”
The eagerly awaited overall survival results will also help determine cabozantinib’s position in treatment sequence, he added. “If we get a survival advantage [that] is the same magnitude that we have with nivolumab, with such an impressive improvement in progression-free survival, maybe despite the toxicity with cabozantinib, people will be willing to use cabozantinib early on.”
In the new analysis, median progression-free survival in the entire trial population was 7.4 months with cabozantinib and 3.9 months with everolimus, translating to a near halving of the risk of events (hazard ratio, 0.52; P less than .001).
Subgroup analyses showed that patients in the cabozantinib group consistently had a lower risk of events, with hazard ratios ranging from 0.22 to 0.84, regardless of their Memorial Sloan Kettering Cancer Center risk group, number of organs with metastases, presence of both visceral and bone metastases, number of prior VEGFR tyrosine kinase inhibitors, the specific VEGFR tyrosine kinase inhibitor in patients who had received only one, and prior immunotherapy targeting the programmed death pathway.
The 42 patients who had previously received immunotherapy targeting that pathway were among those seeming to derive most benefit, Dr. Escudier reported. “Of course, this is a small number, but certainly an observation [of interest] when many patients are going to receive nivolumab as second-line in kidney cancer. This drug is still very active after PD-1 or PD-L1 antibodies.”
The oral multitargeted tyrosine kinase inhibitor cabozantinib is more efficacious than everolimus as therapy for advanced renal cell carcinoma across a wide range of patients, suggests a subgroup analysis of the phase III METEOR trial being reported at the genitourinary cancers symposium.
Trial participants were 658 patients with advanced renal cell carcinoma and clear cell histology who had experienced progression on a tyrosine kinase inhibitor targeting the vascular endothelial growth factor receptor (VEGFR). There was no limit on the number of prior therapies.
The patients were randomized evenly to cabozantinib (Cometriq), which inhibits the VEGFR, MET, and AXL tyrosine kinases – all of which are up-regulated in this cancer – or to everolimus (Afinitor), an inhibitor of the mammalian target of rapamycin that is considered a standard of care. (At present, cabozantinib is approved by the Food and Drug Administration for the treatment of medullary thyroid cancer.)
Results for the entire trial population showed that patients in the cabozantinib group were about half as likely as were their counterparts in the everolimus group to experience progression-free survival events, lead author Dr. Bernard Escudier reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology. All patients appeared to derive benefit, with the reduction in risk ranging from 16% to 78% depending on the specific subgroup.
“Cabozantinib improved progression-free survival, compared to one of our standard therapies, everolimus, in advanced renal cell carcinoma,” concluded Dr. Escudier, who is chair of the Genitourinary Oncology Committee at the Institut Gustave Roussy in Villejuif, France. “Benefit was observed across prespecified subgroups,” including a small subgroup who had previously received immunotherapies targeting the programmed death 1 (PD-1) signaling pathway.
Toxicity was somewhat problematic with cabozantinib, despite starting the drug at a lower dose than has typically been used in the past, he acknowledged. The most common side effects were diarrhea, fatigue, nausea, decreased appetite, and hand-foot syndrome, and they often necessitated further dose reductions.
“Benefit with cabozantinib treatment is supported by a trend in overall survival, and hopefully, we will give this final overall survival analysis at ASCO this year,” Dr. Escudier added. Findings of an interim analysis reported last year were very promising with respect to this outcome (hazard ratio, 0.67; P = .005) (N Engl J Med. 2015 Nov 5;373:1814-23).
“This study is unique compared to others in that it allowed a broad range of patients: Patients could have had spread of cancer to the brain, they could have received any number of prior therapies, and they could have been exposed to immune-based treatments,” commented ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal. “The magnitude of benefit that patients got from cabozantinib far exceeds, in my opinion, what we have seen to date in this setting in terms of both delay in tumor growth and improving survival.”
In fact, for some oncologists, the findings may be strong enough to prompt use of cabozantinib as second-line therapy, according to Dr. Pal, who is a medical oncologist at the City of Hope in Duarte, Calif.
“Given the fact that cabozantinib has a very compelling benefit in terms of both delay in tumor growth and a hint toward a benefit in terms of overall survival, I would perhaps tend to favor that as a second-line option as compared to other comparators, such as nivolumab (Opdivo), in that setting,” he said, referring to an antibody that targets the cell surface receptor PD-1. “Now that’s a personal opinion. I certainly think there are some merits with nivolumab, such as the toxicity profile. But, in broad terms, patients are very focused on clinical efficacy, and with that in mind, the data for cabozantinib truly speaks for itself.”
But Dr. Escudier offered a more-reserved perspective. “I think what people are going to do will be to use nivolumab as second-line [therapy] in most patients and keep cabozantinib for nivolumab failure,” he predicted. “Based on that, this subgroup, although small, is of importance. I don’t think it’s good enough to say we should use cabozantinib or nivolumab in second line based on the subgroup analyses we have.”
The eagerly awaited overall survival results will also help determine cabozantinib’s position in treatment sequence, he added. “If we get a survival advantage [that] is the same magnitude that we have with nivolumab, with such an impressive improvement in progression-free survival, maybe despite the toxicity with cabozantinib, people will be willing to use cabozantinib early on.”
In the new analysis, median progression-free survival in the entire trial population was 7.4 months with cabozantinib and 3.9 months with everolimus, translating to a near halving of the risk of events (hazard ratio, 0.52; P less than .001).
Subgroup analyses showed that patients in the cabozantinib group consistently had a lower risk of events, with hazard ratios ranging from 0.22 to 0.84, regardless of their Memorial Sloan Kettering Cancer Center risk group, number of organs with metastases, presence of both visceral and bone metastases, number of prior VEGFR tyrosine kinase inhibitors, the specific VEGFR tyrosine kinase inhibitor in patients who had received only one, and prior immunotherapy targeting the programmed death pathway.
The 42 patients who had previously received immunotherapy targeting that pathway were among those seeming to derive most benefit, Dr. Escudier reported. “Of course, this is a small number, but certainly an observation [of interest] when many patients are going to receive nivolumab as second-line in kidney cancer. This drug is still very active after PD-1 or PD-L1 antibodies.”
The oral multitargeted tyrosine kinase inhibitor cabozantinib is more efficacious than everolimus as therapy for advanced renal cell carcinoma across a wide range of patients, suggests a subgroup analysis of the phase III METEOR trial being reported at the genitourinary cancers symposium.
Trial participants were 658 patients with advanced renal cell carcinoma and clear cell histology who had experienced progression on a tyrosine kinase inhibitor targeting the vascular endothelial growth factor receptor (VEGFR). There was no limit on the number of prior therapies.
The patients were randomized evenly to cabozantinib (Cometriq), which inhibits the VEGFR, MET, and AXL tyrosine kinases – all of which are up-regulated in this cancer – or to everolimus (Afinitor), an inhibitor of the mammalian target of rapamycin that is considered a standard of care. (At present, cabozantinib is approved by the Food and Drug Administration for the treatment of medullary thyroid cancer.)
Results for the entire trial population showed that patients in the cabozantinib group were about half as likely as were their counterparts in the everolimus group to experience progression-free survival events, lead author Dr. Bernard Escudier reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology. All patients appeared to derive benefit, with the reduction in risk ranging from 16% to 78% depending on the specific subgroup.
“Cabozantinib improved progression-free survival, compared to one of our standard therapies, everolimus, in advanced renal cell carcinoma,” concluded Dr. Escudier, who is chair of the Genitourinary Oncology Committee at the Institut Gustave Roussy in Villejuif, France. “Benefit was observed across prespecified subgroups,” including a small subgroup who had previously received immunotherapies targeting the programmed death 1 (PD-1) signaling pathway.
Toxicity was somewhat problematic with cabozantinib, despite starting the drug at a lower dose than has typically been used in the past, he acknowledged. The most common side effects were diarrhea, fatigue, nausea, decreased appetite, and hand-foot syndrome, and they often necessitated further dose reductions.
“Benefit with cabozantinib treatment is supported by a trend in overall survival, and hopefully, we will give this final overall survival analysis at ASCO this year,” Dr. Escudier added. Findings of an interim analysis reported last year were very promising with respect to this outcome (hazard ratio, 0.67; P = .005) (N Engl J Med. 2015 Nov 5;373:1814-23).
“This study is unique compared to others in that it allowed a broad range of patients: Patients could have had spread of cancer to the brain, they could have received any number of prior therapies, and they could have been exposed to immune-based treatments,” commented ASCO spokesperson and moderator of the press briefing Dr. Sumanta K. Pal. “The magnitude of benefit that patients got from cabozantinib far exceeds, in my opinion, what we have seen to date in this setting in terms of both delay in tumor growth and improving survival.”
In fact, for some oncologists, the findings may be strong enough to prompt use of cabozantinib as second-line therapy, according to Dr. Pal, who is a medical oncologist at the City of Hope in Duarte, Calif.
“Given the fact that cabozantinib has a very compelling benefit in terms of both delay in tumor growth and a hint toward a benefit in terms of overall survival, I would perhaps tend to favor that as a second-line option as compared to other comparators, such as nivolumab (Opdivo), in that setting,” he said, referring to an antibody that targets the cell surface receptor PD-1. “Now that’s a personal opinion. I certainly think there are some merits with nivolumab, such as the toxicity profile. But, in broad terms, patients are very focused on clinical efficacy, and with that in mind, the data for cabozantinib truly speaks for itself.”
But Dr. Escudier offered a more-reserved perspective. “I think what people are going to do will be to use nivolumab as second-line [therapy] in most patients and keep cabozantinib for nivolumab failure,” he predicted. “Based on that, this subgroup, although small, is of importance. I don’t think it’s good enough to say we should use cabozantinib or nivolumab in second line based on the subgroup analyses we have.”
The eagerly awaited overall survival results will also help determine cabozantinib’s position in treatment sequence, he added. “If we get a survival advantage [that] is the same magnitude that we have with nivolumab, with such an impressive improvement in progression-free survival, maybe despite the toxicity with cabozantinib, people will be willing to use cabozantinib early on.”
In the new analysis, median progression-free survival in the entire trial population was 7.4 months with cabozantinib and 3.9 months with everolimus, translating to a near halving of the risk of events (hazard ratio, 0.52; P less than .001).
Subgroup analyses showed that patients in the cabozantinib group consistently had a lower risk of events, with hazard ratios ranging from 0.22 to 0.84, regardless of their Memorial Sloan Kettering Cancer Center risk group, number of organs with metastases, presence of both visceral and bone metastases, number of prior VEGFR tyrosine kinase inhibitors, the specific VEGFR tyrosine kinase inhibitor in patients who had received only one, and prior immunotherapy targeting the programmed death pathway.
The 42 patients who had previously received immunotherapy targeting that pathway were among those seeming to derive most benefit, Dr. Escudier reported. “Of course, this is a small number, but certainly an observation [of interest] when many patients are going to receive nivolumab as second-line in kidney cancer. This drug is still very active after PD-1 or PD-L1 antibodies.”
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: Cabozantinib appears more efficacious than does everolimus for a wide range of patients.
Major finding: Progression-free survival was better with cabozantinib than with everolimus across subgroups (hazard ratios, 0.22-0.84).
Data source: A subgroup analysis of 658 patients with previously treated advanced renal cell carcinoma in a randomized phase III trial (METEOR).
Disclosures: Dr. Escudier disclosed that he has a consulting or advisory role with Bayer, GlaxoSmithKline, Novartis, Pfizer, Exelixis, Bristol-Myers Squibb, and that he receives honoraria from Pfizer, Novartis, GlaxoSmithKline, and Bayer. The study was funded in part by Exelixis. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.
Risk of lethal prostate cancer is lower for regular aspirin users
Regular aspirin use appears to protect against the development of metastatic and fatal prostate cancer, according to an analysis of the Physicians’ Health Study.
Investigators led by Dr. Christopher Brian Allard analyzed data from 22,071 male physicians who were initially free of prostate cancer and were prospectively followed from 1982 through 2009.
Results showed that after adjustment for age, race, body mass index, and smoking status, men who took aspirin regularly (more than three tablets a week) were 24% less likely to develop lethal prostate cancer, which was defined in the study as metastatic disease or death from prostate cancer, Dr. Allard reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
However, regular aspirin use did not reduce the risk of prostate cancer overall, of high-grade prostate cancer, or of locally advanced prostate cancer.
Further analyses restricted to the men who developed prostate cancer showed that regular aspirin use after diagnosis was associated with a 39% lower risk of dying from the disease. In contrast, use before diagnosis did not have a protective effect.
“Our study demonstrates that regular aspirin intake may inhibit lethal prostate cancer, probably by preventing cancer progression,” said Dr. Allard, a urologic oncology fellow at Brigham and Women’s Hospital and Massachusetts General Hospital, both in Boston. Also, “men with prostate cancer who took aspirin regularly after diagnosis had a significantly reduced risk of death.”
Although aspirin’s exact mechanism in preventing lethal disease is unknown, preclinical data have implicated its antiplatelet action, which is consistent with evidence suggesting that circulating cancer cells may use platelets to escape immune detection, he said. “That would explain why there is no effect on the local cancer, but it is preventing deposition of metastases into metastatic environments.”
The main shortcoming of the research was the lack of information on aspirin dose, Dr. Allard acknowledged. Although the Physicians’ Health Study began as a randomized trial in 1982 testing 325 mg of the drug every other day, it was formally stopped 5 years later after cardiovascular benefit was established, and participants were free to take any dose thereafter. “We think most men started at 325 [mg] but then 81 mg did become a popular dose, and we really don’t know what they were taking,” he said.
“More work is needed to identify particular subsets of men most likely to benefit from aspirin and to determine the optimal aspirin dose,” Dr. Allard said.
In terms of applying the findings to clinical care, he recommended an individualized approach. “The main thing to keep in mind is that although aspirin is over the counter, there are side effects and potential harms. That being said, we don’t have the results of a randomized clinical trial looking at aspirin for prostate cancer survival yet,” he said. So men who are interested in aspirin for prevention of lethal prostate cancer should talk to their physicians, he added, “and look at their personal risks of side effects and harms from aspirin, as well as their benefits in terms of both prostate cancer and also potential cardiovascular benefits. It needs to be a personalized decision for every individual patient.”
Dr. Sumanta Pal, ASCO spokesperson and moderator of the press briefing, agreed that the trial left unanswered some critical questions and that clinicians must weigh the potential harms of aspirin therapy against the observed benefits.
“While this work is provocative, it’s important to keep in mind that the findings were from an observational study in which surveys and a review of hospital records were used to obtain information,” added Dr. Pal, a medical oncologist at City of Hope in Duarte, Calif. “These studies are certainly thought provoking but are perhaps best followed by formal clinical trials where we compare use of aspirin either to no treatment or perhaps to placebo.”
Dr. Allard disclosed that he had no conflicts of interests. The Prostate Cancer Foundation and the National Institutes of Health/National Cancer Institute funded the trial. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.
*This article was updated 1/6/2015.
Regular aspirin use appears to protect against the development of metastatic and fatal prostate cancer, according to an analysis of the Physicians’ Health Study.
Investigators led by Dr. Christopher Brian Allard analyzed data from 22,071 male physicians who were initially free of prostate cancer and were prospectively followed from 1982 through 2009.
Results showed that after adjustment for age, race, body mass index, and smoking status, men who took aspirin regularly (more than three tablets a week) were 24% less likely to develop lethal prostate cancer, which was defined in the study as metastatic disease or death from prostate cancer, Dr. Allard reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
However, regular aspirin use did not reduce the risk of prostate cancer overall, of high-grade prostate cancer, or of locally advanced prostate cancer.
Further analyses restricted to the men who developed prostate cancer showed that regular aspirin use after diagnosis was associated with a 39% lower risk of dying from the disease. In contrast, use before diagnosis did not have a protective effect.
“Our study demonstrates that regular aspirin intake may inhibit lethal prostate cancer, probably by preventing cancer progression,” said Dr. Allard, a urologic oncology fellow at Brigham and Women’s Hospital and Massachusetts General Hospital, both in Boston. Also, “men with prostate cancer who took aspirin regularly after diagnosis had a significantly reduced risk of death.”
Although aspirin’s exact mechanism in preventing lethal disease is unknown, preclinical data have implicated its antiplatelet action, which is consistent with evidence suggesting that circulating cancer cells may use platelets to escape immune detection, he said. “That would explain why there is no effect on the local cancer, but it is preventing deposition of metastases into metastatic environments.”
The main shortcoming of the research was the lack of information on aspirin dose, Dr. Allard acknowledged. Although the Physicians’ Health Study began as a randomized trial in 1982 testing 325 mg of the drug every other day, it was formally stopped 5 years later after cardiovascular benefit was established, and participants were free to take any dose thereafter. “We think most men started at 325 [mg] but then 81 mg did become a popular dose, and we really don’t know what they were taking,” he said.
“More work is needed to identify particular subsets of men most likely to benefit from aspirin and to determine the optimal aspirin dose,” Dr. Allard said.
In terms of applying the findings to clinical care, he recommended an individualized approach. “The main thing to keep in mind is that although aspirin is over the counter, there are side effects and potential harms. That being said, we don’t have the results of a randomized clinical trial looking at aspirin for prostate cancer survival yet,” he said. So men who are interested in aspirin for prevention of lethal prostate cancer should talk to their physicians, he added, “and look at their personal risks of side effects and harms from aspirin, as well as their benefits in terms of both prostate cancer and also potential cardiovascular benefits. It needs to be a personalized decision for every individual patient.”
Dr. Sumanta Pal, ASCO spokesperson and moderator of the press briefing, agreed that the trial left unanswered some critical questions and that clinicians must weigh the potential harms of aspirin therapy against the observed benefits.
“While this work is provocative, it’s important to keep in mind that the findings were from an observational study in which surveys and a review of hospital records were used to obtain information,” added Dr. Pal, a medical oncologist at City of Hope in Duarte, Calif. “These studies are certainly thought provoking but are perhaps best followed by formal clinical trials where we compare use of aspirin either to no treatment or perhaps to placebo.”
Dr. Allard disclosed that he had no conflicts of interests. The Prostate Cancer Foundation and the National Institutes of Health/National Cancer Institute funded the trial. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.
*This article was updated 1/6/2015.
Regular aspirin use appears to protect against the development of metastatic and fatal prostate cancer, according to an analysis of the Physicians’ Health Study.
Investigators led by Dr. Christopher Brian Allard analyzed data from 22,071 male physicians who were initially free of prostate cancer and were prospectively followed from 1982 through 2009.
Results showed that after adjustment for age, race, body mass index, and smoking status, men who took aspirin regularly (more than three tablets a week) were 24% less likely to develop lethal prostate cancer, which was defined in the study as metastatic disease or death from prostate cancer, Dr. Allard reported in a press briefing held before the 2016 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
However, regular aspirin use did not reduce the risk of prostate cancer overall, of high-grade prostate cancer, or of locally advanced prostate cancer.
Further analyses restricted to the men who developed prostate cancer showed that regular aspirin use after diagnosis was associated with a 39% lower risk of dying from the disease. In contrast, use before diagnosis did not have a protective effect.
“Our study demonstrates that regular aspirin intake may inhibit lethal prostate cancer, probably by preventing cancer progression,” said Dr. Allard, a urologic oncology fellow at Brigham and Women’s Hospital and Massachusetts General Hospital, both in Boston. Also, “men with prostate cancer who took aspirin regularly after diagnosis had a significantly reduced risk of death.”
Although aspirin’s exact mechanism in preventing lethal disease is unknown, preclinical data have implicated its antiplatelet action, which is consistent with evidence suggesting that circulating cancer cells may use platelets to escape immune detection, he said. “That would explain why there is no effect on the local cancer, but it is preventing deposition of metastases into metastatic environments.”
The main shortcoming of the research was the lack of information on aspirin dose, Dr. Allard acknowledged. Although the Physicians’ Health Study began as a randomized trial in 1982 testing 325 mg of the drug every other day, it was formally stopped 5 years later after cardiovascular benefit was established, and participants were free to take any dose thereafter. “We think most men started at 325 [mg] but then 81 mg did become a popular dose, and we really don’t know what they were taking,” he said.
“More work is needed to identify particular subsets of men most likely to benefit from aspirin and to determine the optimal aspirin dose,” Dr. Allard said.
In terms of applying the findings to clinical care, he recommended an individualized approach. “The main thing to keep in mind is that although aspirin is over the counter, there are side effects and potential harms. That being said, we don’t have the results of a randomized clinical trial looking at aspirin for prostate cancer survival yet,” he said. So men who are interested in aspirin for prevention of lethal prostate cancer should talk to their physicians, he added, “and look at their personal risks of side effects and harms from aspirin, as well as their benefits in terms of both prostate cancer and also potential cardiovascular benefits. It needs to be a personalized decision for every individual patient.”
Dr. Sumanta Pal, ASCO spokesperson and moderator of the press briefing, agreed that the trial left unanswered some critical questions and that clinicians must weigh the potential harms of aspirin therapy against the observed benefits.
“While this work is provocative, it’s important to keep in mind that the findings were from an observational study in which surveys and a review of hospital records were used to obtain information,” added Dr. Pal, a medical oncologist at City of Hope in Duarte, Calif. “These studies are certainly thought provoking but are perhaps best followed by formal clinical trials where we compare use of aspirin either to no treatment or perhaps to placebo.”
Dr. Allard disclosed that he had no conflicts of interests. The Prostate Cancer Foundation and the National Institutes of Health/National Cancer Institute funded the trial. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.
*This article was updated 1/6/2015.
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: Regular aspirin use may reduce the risk of developing advanced prostate cancer and dying from the disease.
Major finding: Men who regularly took aspirin had a 24% lower risk of developing lethal prostate cancer and, among all who developed the disease, a 39% lower risk of dying from it.
Data source: A prospective cohort study of 22,071 men from the Physicians’ Health Study followed up for 27 years.
Disclosures: Dr. Allard disclosed that he had no conflicts of interests. The Prostate Cancer Foundation and the National Institutes of Health/National Cancer Institute funded the trial. Dr. Pal disclosed that he receives honoraria from Astellas Pharma, Medivation, and Novartis; that he has a consulting or advisory role with Aveo, Genentech, Myriad Pharmaceuticals, Novartis, and Pfizer; and that he receives research funding from Medivation.