User login
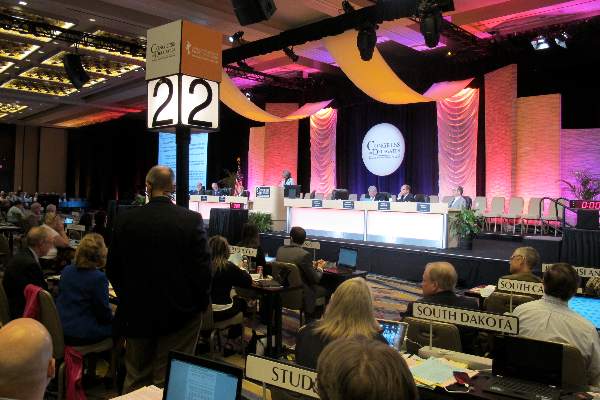
American Academy of Family Physicians (AAFP): Congress of Delegates
New AAFP mission: No more Dr. Nice Guy
WASHINGTON – The American Academy of Family Physicians installed a new president and elected four* new board members and a president-elect, as all promised to take family medicine into a new, more focused, and more aggressive era.
The election results were announced Oct. 22 on the eve of the unveiling of a major new AAFP initiative, “Health is Primary,” which will seek to put family physicians at the forefront of the transformation of the health care system.
The details will be publicly released on Oct. 23, but in discussing the campaign with the Congress of Delegates, Dr. Glen R. Stream, a former AAFP president, said, “It is not self-serving to stand up and say the health care system needs solid primary care that’s well compensated to deliver that care in a medical home model.”
That goal “serves our patients and our country,” said Dr. Stream, who is in private practice in La Quinta, Calif. “We have got to get over ‘Family Medicine Nice.’ ”
Dr. Robert L. Wergin, who took over the helm as AAFP president, promised delegates that he would help them manage the challenges of the rapidly changing health care system and asked for their help. “We’ll finish this together and be winners in this health care delivery race,” he said.
Dr. Wergin, an AAFP member since 1982, practices in the town where he was born and raised – Milford, Neb. He’s chairman of the Milford public schools foundation board, and a team physician for the school district, and medical director of the town volunteer fire department. He was named Nebraska family physician of the year in 2002 and the state’s nursing home medical director of the year in 2012.
The new president-elect is Dr. Wanda Filer, a current AAFP board member who practices in York, Pa. She said that the new AAFP direction was “a completely new story.”
It will require the “mobilization of American family medicine,” with everyone coming to the table to explain why they are best positioned to lower costs, and improve access and quality, said Dr. Filer. In the next 3 to 5 years, “the message can be transformational for the American health care system.” New board member Dr. Lynne Lillie, said that she was ready to be a strong advocate for family medicine. “We as family practice physicians are overregulated, undercompensated, overburdened, and undervalued,” said Dr. Lillie, who is in private practice in Red Wing, Minn.
Noting a high level of burnout, a loss of job satisfaction, and declining empathy toward patients, she said,“This is not okay.”
Family physicians “deserve better and our patients deserve better,” said Dr. Lillie.
The Congress of Delegates also elected Dr. John S. Cullen of Valdez, Alaska, and Dr. Mott Blair, of Wallace, N.C., to full 3-year terms as directors. Dr. Cullen is the emergency medical services director for the Alaska Avalanche Information Center. Dr. Blair used to accompany his father, a family physician, on house calls, often into very rural areas. There, he learned “don’t step on a stick that moves,” he said.
The path ahead for family medicine is tricky – and may have sticks that move – but he said he was prepared to take on the challenges.
Dr. Carl Olden of Yakima, Wash., was the final new board member, and will serve the remainder of an expiring 1-year term and then be eligible to run again in 2015. Dr. Olden was born and raised in Toppenish, Wash., on the Yakima Indian Reservation.
After his residency, he went back to the reservation and practiced with the Indian Health Services from 1984 to 1995.
On Twitter @aliciaault
*Correction, 10/24/2014: An earlier version of this story misstated the number of new AAFP board members elected.
WASHINGTON – The American Academy of Family Physicians installed a new president and elected four* new board members and a president-elect, as all promised to take family medicine into a new, more focused, and more aggressive era.
The election results were announced Oct. 22 on the eve of the unveiling of a major new AAFP initiative, “Health is Primary,” which will seek to put family physicians at the forefront of the transformation of the health care system.
The details will be publicly released on Oct. 23, but in discussing the campaign with the Congress of Delegates, Dr. Glen R. Stream, a former AAFP president, said, “It is not self-serving to stand up and say the health care system needs solid primary care that’s well compensated to deliver that care in a medical home model.”
That goal “serves our patients and our country,” said Dr. Stream, who is in private practice in La Quinta, Calif. “We have got to get over ‘Family Medicine Nice.’ ”
Dr. Robert L. Wergin, who took over the helm as AAFP president, promised delegates that he would help them manage the challenges of the rapidly changing health care system and asked for their help. “We’ll finish this together and be winners in this health care delivery race,” he said.
Dr. Wergin, an AAFP member since 1982, practices in the town where he was born and raised – Milford, Neb. He’s chairman of the Milford public schools foundation board, and a team physician for the school district, and medical director of the town volunteer fire department. He was named Nebraska family physician of the year in 2002 and the state’s nursing home medical director of the year in 2012.
The new president-elect is Dr. Wanda Filer, a current AAFP board member who practices in York, Pa. She said that the new AAFP direction was “a completely new story.”
It will require the “mobilization of American family medicine,” with everyone coming to the table to explain why they are best positioned to lower costs, and improve access and quality, said Dr. Filer. In the next 3 to 5 years, “the message can be transformational for the American health care system.” New board member Dr. Lynne Lillie, said that she was ready to be a strong advocate for family medicine. “We as family practice physicians are overregulated, undercompensated, overburdened, and undervalued,” said Dr. Lillie, who is in private practice in Red Wing, Minn.
Noting a high level of burnout, a loss of job satisfaction, and declining empathy toward patients, she said,“This is not okay.”
Family physicians “deserve better and our patients deserve better,” said Dr. Lillie.
The Congress of Delegates also elected Dr. John S. Cullen of Valdez, Alaska, and Dr. Mott Blair, of Wallace, N.C., to full 3-year terms as directors. Dr. Cullen is the emergency medical services director for the Alaska Avalanche Information Center. Dr. Blair used to accompany his father, a family physician, on house calls, often into very rural areas. There, he learned “don’t step on a stick that moves,” he said.
The path ahead for family medicine is tricky – and may have sticks that move – but he said he was prepared to take on the challenges.
Dr. Carl Olden of Yakima, Wash., was the final new board member, and will serve the remainder of an expiring 1-year term and then be eligible to run again in 2015. Dr. Olden was born and raised in Toppenish, Wash., on the Yakima Indian Reservation.
After his residency, he went back to the reservation and practiced with the Indian Health Services from 1984 to 1995.
On Twitter @aliciaault
*Correction, 10/24/2014: An earlier version of this story misstated the number of new AAFP board members elected.
WASHINGTON – The American Academy of Family Physicians installed a new president and elected four* new board members and a president-elect, as all promised to take family medicine into a new, more focused, and more aggressive era.
The election results were announced Oct. 22 on the eve of the unveiling of a major new AAFP initiative, “Health is Primary,” which will seek to put family physicians at the forefront of the transformation of the health care system.
The details will be publicly released on Oct. 23, but in discussing the campaign with the Congress of Delegates, Dr. Glen R. Stream, a former AAFP president, said, “It is not self-serving to stand up and say the health care system needs solid primary care that’s well compensated to deliver that care in a medical home model.”
That goal “serves our patients and our country,” said Dr. Stream, who is in private practice in La Quinta, Calif. “We have got to get over ‘Family Medicine Nice.’ ”
Dr. Robert L. Wergin, who took over the helm as AAFP president, promised delegates that he would help them manage the challenges of the rapidly changing health care system and asked for their help. “We’ll finish this together and be winners in this health care delivery race,” he said.
Dr. Wergin, an AAFP member since 1982, practices in the town where he was born and raised – Milford, Neb. He’s chairman of the Milford public schools foundation board, and a team physician for the school district, and medical director of the town volunteer fire department. He was named Nebraska family physician of the year in 2002 and the state’s nursing home medical director of the year in 2012.
The new president-elect is Dr. Wanda Filer, a current AAFP board member who practices in York, Pa. She said that the new AAFP direction was “a completely new story.”
It will require the “mobilization of American family medicine,” with everyone coming to the table to explain why they are best positioned to lower costs, and improve access and quality, said Dr. Filer. In the next 3 to 5 years, “the message can be transformational for the American health care system.” New board member Dr. Lynne Lillie, said that she was ready to be a strong advocate for family medicine. “We as family practice physicians are overregulated, undercompensated, overburdened, and undervalued,” said Dr. Lillie, who is in private practice in Red Wing, Minn.
Noting a high level of burnout, a loss of job satisfaction, and declining empathy toward patients, she said,“This is not okay.”
Family physicians “deserve better and our patients deserve better,” said Dr. Lillie.
The Congress of Delegates also elected Dr. John S. Cullen of Valdez, Alaska, and Dr. Mott Blair, of Wallace, N.C., to full 3-year terms as directors. Dr. Cullen is the emergency medical services director for the Alaska Avalanche Information Center. Dr. Blair used to accompany his father, a family physician, on house calls, often into very rural areas. There, he learned “don’t step on a stick that moves,” he said.
The path ahead for family medicine is tricky – and may have sticks that move – but he said he was prepared to take on the challenges.
Dr. Carl Olden of Yakima, Wash., was the final new board member, and will serve the remainder of an expiring 1-year term and then be eligible to run again in 2015. Dr. Olden was born and raised in Toppenish, Wash., on the Yakima Indian Reservation.
After his residency, he went back to the reservation and practiced with the Indian Health Services from 1984 to 1995.
On Twitter @aliciaault
*Correction, 10/24/2014: An earlier version of this story misstated the number of new AAFP board members elected.
AT THE AAFP CONGRESS OF DELEGATES
AAFP delegates want Medicare pay for vaccines, insulin pens
WASHINGTON– Medicare Part B should pay physicians to administer vaccines in their offices, according to resolutions passed at the annual Congress of Delegates of the American Academy of Family Physicians.
The AAFP’s policymaking body voted to advocate that the Centers for Medicare & Medicaid Services pay physicians under Medicare Part B to administer the shingles vaccine and all other vaccines recommended by the Advisory Committee on Immunization Practices. Payment should be retroactive to when the ACIP first recommends a particular vaccine, according to a resolution introduced by the New York State chapter.
The Mississippi delegation urged the delegates to approve a resolution to have Medicare pay for the cost of insulin pens, as many patients with diabetes and vision issues cannot appropriately use vials and syringes, which are covered by Medicare. The AAFP Congress backed this resolution, also.
A hotly contested resolution called for the AAFP to advocate for a ban on diagnostic testing by pharmacists. An initiative in Michigan is allowing pharmacists to test for conditions like strep and then prescribe appropriate medications. The Michigan chapter urged the Congress to take a strong stand against this expansion of scope-of-practice for pharmacists, saying that it would likely spread to other states.
Many delegates said that pharmacists did not have extensive clinical training and that patient safety could be jeopardized. Others said that they did not want to be viewed as engaging in a turf battle against pharmacists.
Ultimately, the Congress referred the proposal to the AAFP board for study.
The Congress also voted against advocating for a single-payer health care system, and referred to the AAFP board a proposal to rescind the marketing approval of the long-acting opioid Zohydro.
The New York and Rhode Island chapters asked the AAFP to lobby the U.S. Congress to pass a law to treat electronic cigarettes the same as tobacco products, and that the minimum age for purchase be made the same as well. That resolution was accepted by the delegates.
The AAFP Congress also adopted a resolution that urged the federal government to end the mandatory 30-day waiting period between when informed consent is given and when Medicaid will cover a voluntary sterilization procedure. Delegates also backed a proposal to urge coverage of vasectomy and male contraceptive services as a preventive care service – that is, a cost-free service – under the Affordable Care Act.
On Twitter @aliciaault
WASHINGTON– Medicare Part B should pay physicians to administer vaccines in their offices, according to resolutions passed at the annual Congress of Delegates of the American Academy of Family Physicians.
The AAFP’s policymaking body voted to advocate that the Centers for Medicare & Medicaid Services pay physicians under Medicare Part B to administer the shingles vaccine and all other vaccines recommended by the Advisory Committee on Immunization Practices. Payment should be retroactive to when the ACIP first recommends a particular vaccine, according to a resolution introduced by the New York State chapter.
The Mississippi delegation urged the delegates to approve a resolution to have Medicare pay for the cost of insulin pens, as many patients with diabetes and vision issues cannot appropriately use vials and syringes, which are covered by Medicare. The AAFP Congress backed this resolution, also.
A hotly contested resolution called for the AAFP to advocate for a ban on diagnostic testing by pharmacists. An initiative in Michigan is allowing pharmacists to test for conditions like strep and then prescribe appropriate medications. The Michigan chapter urged the Congress to take a strong stand against this expansion of scope-of-practice for pharmacists, saying that it would likely spread to other states.
Many delegates said that pharmacists did not have extensive clinical training and that patient safety could be jeopardized. Others said that they did not want to be viewed as engaging in a turf battle against pharmacists.
Ultimately, the Congress referred the proposal to the AAFP board for study.
The Congress also voted against advocating for a single-payer health care system, and referred to the AAFP board a proposal to rescind the marketing approval of the long-acting opioid Zohydro.
The New York and Rhode Island chapters asked the AAFP to lobby the U.S. Congress to pass a law to treat electronic cigarettes the same as tobacco products, and that the minimum age for purchase be made the same as well. That resolution was accepted by the delegates.
The AAFP Congress also adopted a resolution that urged the federal government to end the mandatory 30-day waiting period between when informed consent is given and when Medicaid will cover a voluntary sterilization procedure. Delegates also backed a proposal to urge coverage of vasectomy and male contraceptive services as a preventive care service – that is, a cost-free service – under the Affordable Care Act.
On Twitter @aliciaault
WASHINGTON– Medicare Part B should pay physicians to administer vaccines in their offices, according to resolutions passed at the annual Congress of Delegates of the American Academy of Family Physicians.
The AAFP’s policymaking body voted to advocate that the Centers for Medicare & Medicaid Services pay physicians under Medicare Part B to administer the shingles vaccine and all other vaccines recommended by the Advisory Committee on Immunization Practices. Payment should be retroactive to when the ACIP first recommends a particular vaccine, according to a resolution introduced by the New York State chapter.
The Mississippi delegation urged the delegates to approve a resolution to have Medicare pay for the cost of insulin pens, as many patients with diabetes and vision issues cannot appropriately use vials and syringes, which are covered by Medicare. The AAFP Congress backed this resolution, also.
A hotly contested resolution called for the AAFP to advocate for a ban on diagnostic testing by pharmacists. An initiative in Michigan is allowing pharmacists to test for conditions like strep and then prescribe appropriate medications. The Michigan chapter urged the Congress to take a strong stand against this expansion of scope-of-practice for pharmacists, saying that it would likely spread to other states.
Many delegates said that pharmacists did not have extensive clinical training and that patient safety could be jeopardized. Others said that they did not want to be viewed as engaging in a turf battle against pharmacists.
Ultimately, the Congress referred the proposal to the AAFP board for study.
The Congress also voted against advocating for a single-payer health care system, and referred to the AAFP board a proposal to rescind the marketing approval of the long-acting opioid Zohydro.
The New York and Rhode Island chapters asked the AAFP to lobby the U.S. Congress to pass a law to treat electronic cigarettes the same as tobacco products, and that the minimum age for purchase be made the same as well. That resolution was accepted by the delegates.
The AAFP Congress also adopted a resolution that urged the federal government to end the mandatory 30-day waiting period between when informed consent is given and when Medicaid will cover a voluntary sterilization procedure. Delegates also backed a proposal to urge coverage of vasectomy and male contraceptive services as a preventive care service – that is, a cost-free service – under the Affordable Care Act.
On Twitter @aliciaault
AT THE AAFP CONGRESS OF DELEGATES 2014
AAFP Congress votes to keep Coke alliance
WASHINGTON – Family doctors who do not support the alliance between the American Academy of Family Physicians and the Coca-Cola Company were unable to convince their peers to break up that union.
The final vote on the resolution introduced by the Maryland and Rhode Island chapters was 72-20 in favor of the academy considering a renewal of the relationship in late 2015.
Dr. Robert E. Reneker Jr., a delegate from Michigan, said that he was voting in favor of the relationship based on its financial benefits. However, he added, “the board, our leadership, should understand this: You need to extract us from Coke as soon as it is financially viable and actually actively work to do that. I will vote against this resolution this year, but I am not going to keep giving you a pass on this. Get us out of Coke.”
Delegates voted by consent to accept a number of committee recommendations, including not adopting resolutions on forming a task force to examine proportional representation within the Congress of Delegates; that family medicine physicians be referred to as physicians and not health care providers; and changes to awarding a title of fellow that would recognize a student’s medical school membership toward the 6-year requirement.
Delegates referred for further investigation resolutions examining the language of the oath of AAFP fellows, specifically the clause to placing patient “welfare above all else” and that the AAFP use the International System of Units throughout its journals, publications, and clinical communications and present a similar resolution to the American Medical Association.
WASHINGTON – Family doctors who do not support the alliance between the American Academy of Family Physicians and the Coca-Cola Company were unable to convince their peers to break up that union.
The final vote on the resolution introduced by the Maryland and Rhode Island chapters was 72-20 in favor of the academy considering a renewal of the relationship in late 2015.
Dr. Robert E. Reneker Jr., a delegate from Michigan, said that he was voting in favor of the relationship based on its financial benefits. However, he added, “the board, our leadership, should understand this: You need to extract us from Coke as soon as it is financially viable and actually actively work to do that. I will vote against this resolution this year, but I am not going to keep giving you a pass on this. Get us out of Coke.”
Delegates voted by consent to accept a number of committee recommendations, including not adopting resolutions on forming a task force to examine proportional representation within the Congress of Delegates; that family medicine physicians be referred to as physicians and not health care providers; and changes to awarding a title of fellow that would recognize a student’s medical school membership toward the 6-year requirement.
Delegates referred for further investigation resolutions examining the language of the oath of AAFP fellows, specifically the clause to placing patient “welfare above all else” and that the AAFP use the International System of Units throughout its journals, publications, and clinical communications and present a similar resolution to the American Medical Association.
WASHINGTON – Family doctors who do not support the alliance between the American Academy of Family Physicians and the Coca-Cola Company were unable to convince their peers to break up that union.
The final vote on the resolution introduced by the Maryland and Rhode Island chapters was 72-20 in favor of the academy considering a renewal of the relationship in late 2015.
Dr. Robert E. Reneker Jr., a delegate from Michigan, said that he was voting in favor of the relationship based on its financial benefits. However, he added, “the board, our leadership, should understand this: You need to extract us from Coke as soon as it is financially viable and actually actively work to do that. I will vote against this resolution this year, but I am not going to keep giving you a pass on this. Get us out of Coke.”
Delegates voted by consent to accept a number of committee recommendations, including not adopting resolutions on forming a task force to examine proportional representation within the Congress of Delegates; that family medicine physicians be referred to as physicians and not health care providers; and changes to awarding a title of fellow that would recognize a student’s medical school membership toward the 6-year requirement.
Delegates referred for further investigation resolutions examining the language of the oath of AAFP fellows, specifically the clause to placing patient “welfare above all else” and that the AAFP use the International System of Units throughout its journals, publications, and clinical communications and present a similar resolution to the American Medical Association.
AAFP Congress to push for ending of tobacco sales at pharmacies
WASHINGTON – The American Academy of Family Physicians voiced its support for ending of tobacco sales at pharmacies and for developing end-of-life registries.
Resolutions from the Reference Committee on Health of the Public & Science were adopted by consent without debate Oct. 21 during a session of the full Congress of Delegates, with a number being referred back to the board of directors for further investigation.
During an Oct. 20 session to present the resolutions, all testimony provided by delegates was in support of a resolution introduced by the New York State, Pennsylvania, and Rhode Island chapters directing AAFP to “support ending the sale of tobacco products in all pharmacies and stores that contain a pharmacy department,” and to work with various pharmacy and pharmacist associations to push for the prohibition of sale of tobacco products at pharmacies.
The move comes in the wake of CVS/Caremark announcing that it will charge higher copays at pharmacies that also sell tobacco products, a move that could be designed to drive business to CVS/pharmacies, which no longer sells tobacco products in the retail portion of its stores.
An end-of-life planning resolution offered by the Michigan chapter also received support, though specific concerns were voiced during the Oct. 20 reference committee session.
The resolution directs AAFP to support the implementation of centralized registries, similar to Michigan’s “Peace of Mind Registry” that offers a central repository housing a patient’s end-of-life care preferences. It also calls for support of mechanisms that encourage the uploading of durable powers of attorney, physician order scope of treatment forms, and do-not-resuscitate orders into the registry, advocates for the development of centralized HIPAA registries of an individual’s preferences for end-of-life care, and supports mechanisms that allow for the registries to be readily accessible and routinely used by medical professionals.
Delegates generally supported the resolution during the Oct. 20 session, though some concerns regarding its implementation were raised, including wording that was eventually dropped regarding how public the information would be.
Other concerns included understanding how the registries would be updated as patient preferences changed.
Dr. Dale Ragle, president of the Texas delegation, offered his support of the spirit of the resolution, asked for wording to be included specifically on who could access such registries, similar to wording that is used to determine access to prescription drug–monitoring programs, including patients and their families as well as physicians.
“What happens if the wishes or the conditions of the patient changes?” Dr. Ragle asked. “Perhaps there should be some sort of mechanism in place or some sort of assurances that would be ... reviewed and updated periodically as the conditions may change. Also maybe put wording in there that a physician could override the database ... at the wishes of the patients that they verbally express them ... or if the physician has reliable information that perhaps the patient’s wishes have changed or the condition has changed.”
Florida delegate Dr. Dennis Saver also noted that access when a patient travels outside of his home state also need to be addressed.
Integrating information into electronic health records also was raised as a need from multiple delegates voicing support for the resolution.
Other resolutions adopted relate to addressing disparities and discrimination in immigrant populations and support for the Center for the Study of Tobacco and Society.
One resolution that received strong support from delegates at the reference committee meeting but ultimately was referred to the board for further study was the development of educational materials regarding the recreational use of marijuana, particularly as states begin to legalize it for that purpose.
Dr Elizabeth Snyder, the Oregon delegate, noted that family physicians are “going to have a different kind of counseling that we need to do and even without it becoming legal, we find ourselves with a paucity of useful, valid scientific information that we can use to educate our patients, both young and older, about marijuana use and its risks. We would therefore encourage the academy to help develop high-quality educational materials as it has done for many other substances that people use or medical conditions that we can reliably use in our practices.”
Other resolutions referred back to the board for further investigation addressed a vaccination personal belief exemption policy, support of the One Health Initiative, expansion of venues for peer-reviewed family medicine research, support of the prohibition of sale/distribution of raw or unpasteurized milk or milk products and support of the ban on nontherapeutic antibiotic use in farm animals.
WASHINGTON – The American Academy of Family Physicians voiced its support for ending of tobacco sales at pharmacies and for developing end-of-life registries.
Resolutions from the Reference Committee on Health of the Public & Science were adopted by consent without debate Oct. 21 during a session of the full Congress of Delegates, with a number being referred back to the board of directors for further investigation.
During an Oct. 20 session to present the resolutions, all testimony provided by delegates was in support of a resolution introduced by the New York State, Pennsylvania, and Rhode Island chapters directing AAFP to “support ending the sale of tobacco products in all pharmacies and stores that contain a pharmacy department,” and to work with various pharmacy and pharmacist associations to push for the prohibition of sale of tobacco products at pharmacies.
The move comes in the wake of CVS/Caremark announcing that it will charge higher copays at pharmacies that also sell tobacco products, a move that could be designed to drive business to CVS/pharmacies, which no longer sells tobacco products in the retail portion of its stores.
An end-of-life planning resolution offered by the Michigan chapter also received support, though specific concerns were voiced during the Oct. 20 reference committee session.
The resolution directs AAFP to support the implementation of centralized registries, similar to Michigan’s “Peace of Mind Registry” that offers a central repository housing a patient’s end-of-life care preferences. It also calls for support of mechanisms that encourage the uploading of durable powers of attorney, physician order scope of treatment forms, and do-not-resuscitate orders into the registry, advocates for the development of centralized HIPAA registries of an individual’s preferences for end-of-life care, and supports mechanisms that allow for the registries to be readily accessible and routinely used by medical professionals.
Delegates generally supported the resolution during the Oct. 20 session, though some concerns regarding its implementation were raised, including wording that was eventually dropped regarding how public the information would be.
Other concerns included understanding how the registries would be updated as patient preferences changed.
Dr. Dale Ragle, president of the Texas delegation, offered his support of the spirit of the resolution, asked for wording to be included specifically on who could access such registries, similar to wording that is used to determine access to prescription drug–monitoring programs, including patients and their families as well as physicians.
“What happens if the wishes or the conditions of the patient changes?” Dr. Ragle asked. “Perhaps there should be some sort of mechanism in place or some sort of assurances that would be ... reviewed and updated periodically as the conditions may change. Also maybe put wording in there that a physician could override the database ... at the wishes of the patients that they verbally express them ... or if the physician has reliable information that perhaps the patient’s wishes have changed or the condition has changed.”
Florida delegate Dr. Dennis Saver also noted that access when a patient travels outside of his home state also need to be addressed.
Integrating information into electronic health records also was raised as a need from multiple delegates voicing support for the resolution.
Other resolutions adopted relate to addressing disparities and discrimination in immigrant populations and support for the Center for the Study of Tobacco and Society.
One resolution that received strong support from delegates at the reference committee meeting but ultimately was referred to the board for further study was the development of educational materials regarding the recreational use of marijuana, particularly as states begin to legalize it for that purpose.
Dr Elizabeth Snyder, the Oregon delegate, noted that family physicians are “going to have a different kind of counseling that we need to do and even without it becoming legal, we find ourselves with a paucity of useful, valid scientific information that we can use to educate our patients, both young and older, about marijuana use and its risks. We would therefore encourage the academy to help develop high-quality educational materials as it has done for many other substances that people use or medical conditions that we can reliably use in our practices.”
Other resolutions referred back to the board for further investigation addressed a vaccination personal belief exemption policy, support of the One Health Initiative, expansion of venues for peer-reviewed family medicine research, support of the prohibition of sale/distribution of raw or unpasteurized milk or milk products and support of the ban on nontherapeutic antibiotic use in farm animals.
WASHINGTON – The American Academy of Family Physicians voiced its support for ending of tobacco sales at pharmacies and for developing end-of-life registries.
Resolutions from the Reference Committee on Health of the Public & Science were adopted by consent without debate Oct. 21 during a session of the full Congress of Delegates, with a number being referred back to the board of directors for further investigation.
During an Oct. 20 session to present the resolutions, all testimony provided by delegates was in support of a resolution introduced by the New York State, Pennsylvania, and Rhode Island chapters directing AAFP to “support ending the sale of tobacco products in all pharmacies and stores that contain a pharmacy department,” and to work with various pharmacy and pharmacist associations to push for the prohibition of sale of tobacco products at pharmacies.
The move comes in the wake of CVS/Caremark announcing that it will charge higher copays at pharmacies that also sell tobacco products, a move that could be designed to drive business to CVS/pharmacies, which no longer sells tobacco products in the retail portion of its stores.
An end-of-life planning resolution offered by the Michigan chapter also received support, though specific concerns were voiced during the Oct. 20 reference committee session.
The resolution directs AAFP to support the implementation of centralized registries, similar to Michigan’s “Peace of Mind Registry” that offers a central repository housing a patient’s end-of-life care preferences. It also calls for support of mechanisms that encourage the uploading of durable powers of attorney, physician order scope of treatment forms, and do-not-resuscitate orders into the registry, advocates for the development of centralized HIPAA registries of an individual’s preferences for end-of-life care, and supports mechanisms that allow for the registries to be readily accessible and routinely used by medical professionals.
Delegates generally supported the resolution during the Oct. 20 session, though some concerns regarding its implementation were raised, including wording that was eventually dropped regarding how public the information would be.
Other concerns included understanding how the registries would be updated as patient preferences changed.
Dr. Dale Ragle, president of the Texas delegation, offered his support of the spirit of the resolution, asked for wording to be included specifically on who could access such registries, similar to wording that is used to determine access to prescription drug–monitoring programs, including patients and their families as well as physicians.
“What happens if the wishes or the conditions of the patient changes?” Dr. Ragle asked. “Perhaps there should be some sort of mechanism in place or some sort of assurances that would be ... reviewed and updated periodically as the conditions may change. Also maybe put wording in there that a physician could override the database ... at the wishes of the patients that they verbally express them ... or if the physician has reliable information that perhaps the patient’s wishes have changed or the condition has changed.”
Florida delegate Dr. Dennis Saver also noted that access when a patient travels outside of his home state also need to be addressed.
Integrating information into electronic health records also was raised as a need from multiple delegates voicing support for the resolution.
Other resolutions adopted relate to addressing disparities and discrimination in immigrant populations and support for the Center for the Study of Tobacco and Society.
One resolution that received strong support from delegates at the reference committee meeting but ultimately was referred to the board for further study was the development of educational materials regarding the recreational use of marijuana, particularly as states begin to legalize it for that purpose.
Dr Elizabeth Snyder, the Oregon delegate, noted that family physicians are “going to have a different kind of counseling that we need to do and even without it becoming legal, we find ourselves with a paucity of useful, valid scientific information that we can use to educate our patients, both young and older, about marijuana use and its risks. We would therefore encourage the academy to help develop high-quality educational materials as it has done for many other substances that people use or medical conditions that we can reliably use in our practices.”
Other resolutions referred back to the board for further investigation addressed a vaccination personal belief exemption policy, support of the One Health Initiative, expansion of venues for peer-reviewed family medicine research, support of the prohibition of sale/distribution of raw or unpasteurized milk or milk products and support of the ban on nontherapeutic antibiotic use in farm animals.
AT THE AAFP CONGRESS OF DELEGATES
AAFP Congress: Delegates remain divided on Coca-Cola alliance
WASHINGTON – The controversial alliance between the American Academy of Family Physicians and the Coca-Cola Company took center stage during preliminary discussions Oct. 20 at the AAFP Congress of Delegates.
The congress’s Reference Committee on Organization and Finance addressed a resolution offered by the Maryland and Rhode Island chapters that calls on AAFP to not engage in discussions to renew the alliance when the time comes in November 2015.
Public perception of the partnership dominated those who opposed the renewing alliance as sugary drinks come under public scrutiny for their role in the growing obesity problem, despite positive steps the Coca-Cola Co. has taken to encourage healthier behavior.
A delegate from New York, who admitted to being a Coke drinker, said that the organization “shouldn’t underestimate how negatively that AAFP is looked upon for its link to this company where most of their products are not health choices for their patients. As a group that is trying to promote health, I would say we shouldn’t be linked or taking large amounts of sponsorship from them.”
A renewed relationship with Coca-Cola could bring the AAFP more than $1 million over 2 years, according to the resolution.
Another delegate noted recent evidence suggesting that artificial sweeteners could be contributing to metabolic disorders, making it more difficult to promote diet soft drinks as an alternative.
In support of the alliance, a delegate from Texas noted that many AAFP member benefits, including offering continuing medical education credits and political advocacy, “cost money. You do have to look at this [alliance] with eyes open and sometimes have to look at both sides. ... Sometimes we have to make difficult compromises to support our overall mission.”
Dr. Lori J. Heim, AAFP president from 2009-2010, also spoke in support of the alliance.
Dr. Heim noted that the company has sought out not only AAFP, but also other medical specialty societies representing cardiologists, pediatricians, and sports medicine specialties, as well as representatives from groups representing nutritionists and nurses, to solicit feedback on becoming a better corporate citizen.
And while the changes that have come from this have not gone far enough, Dr. Heim said, there has been progress, such as the smaller cans and clearly displayed calorie information to help patients make better choices.
“This is pretty much unheard of,” said Dr. Heim, who was AAFP president when the alliance was formed. “Have there been monumental changes? No. Have they gone as far as I would have liked them to go? No. Have we seen changes though? Yes.”
And those steps of progress go well beyond the initial intent of the alliance, which Dr. Heim reminded reference committee members was to help promote FamilyDoctor.org.
As for the perception issue, while many delegates felt that the alliance put them in an awkward position to have to defend it to their patients, Dr. Reid Blackwelder suggested the perception issue may be more individualized rather than widespread.
“I will assure you our reputation is strong and our voice is heard,” said Dr. Blackwelder, who completes his term as AAFP president on Oct. 22. “And even though you will hear stories of how folks are having to justify the relationship, as your face and voice this past year, I can promise you I have not done a single media interview or question about this issue. You can argue whether that should or should not be the case but many other issues are where I am being asked for input and not for this one.”
Other resolutions addressed at the reference committee meeting included:
• A resolution from the Tennessee delegation to modify the oath of AAFP Fellows. The resolution would strike a clause about patients and “placing their welfare above all else” and replace it with language that better supports work/life balance.
• A resolution from the Texas delegation that would shift the composition of the AAFP Congress of Delegates away from a senatorial style makeup (two delegates and an alternate from each state chapter) and instead compose the body on a more proportional basis.
WASHINGTON – The controversial alliance between the American Academy of Family Physicians and the Coca-Cola Company took center stage during preliminary discussions Oct. 20 at the AAFP Congress of Delegates.
The congress’s Reference Committee on Organization and Finance addressed a resolution offered by the Maryland and Rhode Island chapters that calls on AAFP to not engage in discussions to renew the alliance when the time comes in November 2015.
Public perception of the partnership dominated those who opposed the renewing alliance as sugary drinks come under public scrutiny for their role in the growing obesity problem, despite positive steps the Coca-Cola Co. has taken to encourage healthier behavior.
A delegate from New York, who admitted to being a Coke drinker, said that the organization “shouldn’t underestimate how negatively that AAFP is looked upon for its link to this company where most of their products are not health choices for their patients. As a group that is trying to promote health, I would say we shouldn’t be linked or taking large amounts of sponsorship from them.”
A renewed relationship with Coca-Cola could bring the AAFP more than $1 million over 2 years, according to the resolution.
Another delegate noted recent evidence suggesting that artificial sweeteners could be contributing to metabolic disorders, making it more difficult to promote diet soft drinks as an alternative.
In support of the alliance, a delegate from Texas noted that many AAFP member benefits, including offering continuing medical education credits and political advocacy, “cost money. You do have to look at this [alliance] with eyes open and sometimes have to look at both sides. ... Sometimes we have to make difficult compromises to support our overall mission.”
Dr. Lori J. Heim, AAFP president from 2009-2010, also spoke in support of the alliance.
Dr. Heim noted that the company has sought out not only AAFP, but also other medical specialty societies representing cardiologists, pediatricians, and sports medicine specialties, as well as representatives from groups representing nutritionists and nurses, to solicit feedback on becoming a better corporate citizen.
And while the changes that have come from this have not gone far enough, Dr. Heim said, there has been progress, such as the smaller cans and clearly displayed calorie information to help patients make better choices.
“This is pretty much unheard of,” said Dr. Heim, who was AAFP president when the alliance was formed. “Have there been monumental changes? No. Have they gone as far as I would have liked them to go? No. Have we seen changes though? Yes.”
And those steps of progress go well beyond the initial intent of the alliance, which Dr. Heim reminded reference committee members was to help promote FamilyDoctor.org.
As for the perception issue, while many delegates felt that the alliance put them in an awkward position to have to defend it to their patients, Dr. Reid Blackwelder suggested the perception issue may be more individualized rather than widespread.
“I will assure you our reputation is strong and our voice is heard,” said Dr. Blackwelder, who completes his term as AAFP president on Oct. 22. “And even though you will hear stories of how folks are having to justify the relationship, as your face and voice this past year, I can promise you I have not done a single media interview or question about this issue. You can argue whether that should or should not be the case but many other issues are where I am being asked for input and not for this one.”
Other resolutions addressed at the reference committee meeting included:
• A resolution from the Tennessee delegation to modify the oath of AAFP Fellows. The resolution would strike a clause about patients and “placing their welfare above all else” and replace it with language that better supports work/life balance.
• A resolution from the Texas delegation that would shift the composition of the AAFP Congress of Delegates away from a senatorial style makeup (two delegates and an alternate from each state chapter) and instead compose the body on a more proportional basis.
WASHINGTON – The controversial alliance between the American Academy of Family Physicians and the Coca-Cola Company took center stage during preliminary discussions Oct. 20 at the AAFP Congress of Delegates.
The congress’s Reference Committee on Organization and Finance addressed a resolution offered by the Maryland and Rhode Island chapters that calls on AAFP to not engage in discussions to renew the alliance when the time comes in November 2015.
Public perception of the partnership dominated those who opposed the renewing alliance as sugary drinks come under public scrutiny for their role in the growing obesity problem, despite positive steps the Coca-Cola Co. has taken to encourage healthier behavior.
A delegate from New York, who admitted to being a Coke drinker, said that the organization “shouldn’t underestimate how negatively that AAFP is looked upon for its link to this company where most of their products are not health choices for their patients. As a group that is trying to promote health, I would say we shouldn’t be linked or taking large amounts of sponsorship from them.”
A renewed relationship with Coca-Cola could bring the AAFP more than $1 million over 2 years, according to the resolution.
Another delegate noted recent evidence suggesting that artificial sweeteners could be contributing to metabolic disorders, making it more difficult to promote diet soft drinks as an alternative.
In support of the alliance, a delegate from Texas noted that many AAFP member benefits, including offering continuing medical education credits and political advocacy, “cost money. You do have to look at this [alliance] with eyes open and sometimes have to look at both sides. ... Sometimes we have to make difficult compromises to support our overall mission.”
Dr. Lori J. Heim, AAFP president from 2009-2010, also spoke in support of the alliance.
Dr. Heim noted that the company has sought out not only AAFP, but also other medical specialty societies representing cardiologists, pediatricians, and sports medicine specialties, as well as representatives from groups representing nutritionists and nurses, to solicit feedback on becoming a better corporate citizen.
And while the changes that have come from this have not gone far enough, Dr. Heim said, there has been progress, such as the smaller cans and clearly displayed calorie information to help patients make better choices.
“This is pretty much unheard of,” said Dr. Heim, who was AAFP president when the alliance was formed. “Have there been monumental changes? No. Have they gone as far as I would have liked them to go? No. Have we seen changes though? Yes.”
And those steps of progress go well beyond the initial intent of the alliance, which Dr. Heim reminded reference committee members was to help promote FamilyDoctor.org.
As for the perception issue, while many delegates felt that the alliance put them in an awkward position to have to defend it to their patients, Dr. Reid Blackwelder suggested the perception issue may be more individualized rather than widespread.
“I will assure you our reputation is strong and our voice is heard,” said Dr. Blackwelder, who completes his term as AAFP president on Oct. 22. “And even though you will hear stories of how folks are having to justify the relationship, as your face and voice this past year, I can promise you I have not done a single media interview or question about this issue. You can argue whether that should or should not be the case but many other issues are where I am being asked for input and not for this one.”
Other resolutions addressed at the reference committee meeting included:
• A resolution from the Tennessee delegation to modify the oath of AAFP Fellows. The resolution would strike a clause about patients and “placing their welfare above all else” and replace it with language that better supports work/life balance.
• A resolution from the Texas delegation that would shift the composition of the AAFP Congress of Delegates away from a senatorial style makeup (two delegates and an alternate from each state chapter) and instead compose the body on a more proportional basis.
AT THE AAFP CONGRESS OF DELEGATES
Family medicine is ascendant, says AAFP’s Cain
WASHINGTON – Family medicine has gone from the brink of collapse to a rising specialty, American Academy of Family Physicians Board Chair Jeffrey Cain said Oct. 20 in a speech capping his service on the academy leadership team.
Dr. Cain noted that he began his run as an AAFP officer in 2007, a time when the “impending collapse” description had been bestowed upon family medicine by the Institute of Medicine. “For family medicine, it really was a time of crisis,” he said at the annual Congress of Delegates of the American Academy of Family Physicians.
Payments were low, there was little student interest in the specialty, and some 47 million Americans were uninsured, he said.
“We’ve actually stopped that free fall of [family medicine] and we are now rising,” said Dr. Cain, who completes his term as board chair at the meeting.
Six years ago, insurers, payers, and employers did not see the value of primary care, but now, the adoption of the patient-centered medical home “has proven in the real world that we are the key to the triple aim” of increasing access, increasing quality, and reducing cost, Dr. Cain said.
Medicare is also paying for value, in part through grants from the Center for Medicare and Medicaid Innovation, he said.
Even President Obama has spoken publicly “about the need to make family medicine the hub of patient-centered care,” Dr. Cain said. “We have not arrived, but we’re on our way.”
In 2007, family medicine had the lowest match rate ever recorded, but the number of matches has increased each year for the past 5 years. There are now 26,000 student members of the AAFP today – one in four U.S. medical students, Dr. Cain said.
Access to primary care has increased as well, he said. Six years ago, there were some 47 million uninsured Americans. The push for the Affordable Care Act “unleashed a political firestorm,” nationally and within the AAFP membership, Dr. Cain said.
The uninsured rate has dropped from 18% to about 13% currently, he said.
“Today I stand before you a witness to what I see as the rebirth of family medicine,” Dr. Cain said.
On Twitter @aliciaault
WASHINGTON – Family medicine has gone from the brink of collapse to a rising specialty, American Academy of Family Physicians Board Chair Jeffrey Cain said Oct. 20 in a speech capping his service on the academy leadership team.
Dr. Cain noted that he began his run as an AAFP officer in 2007, a time when the “impending collapse” description had been bestowed upon family medicine by the Institute of Medicine. “For family medicine, it really was a time of crisis,” he said at the annual Congress of Delegates of the American Academy of Family Physicians.
Payments were low, there was little student interest in the specialty, and some 47 million Americans were uninsured, he said.
“We’ve actually stopped that free fall of [family medicine] and we are now rising,” said Dr. Cain, who completes his term as board chair at the meeting.
Six years ago, insurers, payers, and employers did not see the value of primary care, but now, the adoption of the patient-centered medical home “has proven in the real world that we are the key to the triple aim” of increasing access, increasing quality, and reducing cost, Dr. Cain said.
Medicare is also paying for value, in part through grants from the Center for Medicare and Medicaid Innovation, he said.
Even President Obama has spoken publicly “about the need to make family medicine the hub of patient-centered care,” Dr. Cain said. “We have not arrived, but we’re on our way.”
In 2007, family medicine had the lowest match rate ever recorded, but the number of matches has increased each year for the past 5 years. There are now 26,000 student members of the AAFP today – one in four U.S. medical students, Dr. Cain said.
Access to primary care has increased as well, he said. Six years ago, there were some 47 million uninsured Americans. The push for the Affordable Care Act “unleashed a political firestorm,” nationally and within the AAFP membership, Dr. Cain said.
The uninsured rate has dropped from 18% to about 13% currently, he said.
“Today I stand before you a witness to what I see as the rebirth of family medicine,” Dr. Cain said.
On Twitter @aliciaault
WASHINGTON – Family medicine has gone from the brink of collapse to a rising specialty, American Academy of Family Physicians Board Chair Jeffrey Cain said Oct. 20 in a speech capping his service on the academy leadership team.
Dr. Cain noted that he began his run as an AAFP officer in 2007, a time when the “impending collapse” description had been bestowed upon family medicine by the Institute of Medicine. “For family medicine, it really was a time of crisis,” he said at the annual Congress of Delegates of the American Academy of Family Physicians.
Payments were low, there was little student interest in the specialty, and some 47 million Americans were uninsured, he said.
“We’ve actually stopped that free fall of [family medicine] and we are now rising,” said Dr. Cain, who completes his term as board chair at the meeting.
Six years ago, insurers, payers, and employers did not see the value of primary care, but now, the adoption of the patient-centered medical home “has proven in the real world that we are the key to the triple aim” of increasing access, increasing quality, and reducing cost, Dr. Cain said.
Medicare is also paying for value, in part through grants from the Center for Medicare and Medicaid Innovation, he said.
Even President Obama has spoken publicly “about the need to make family medicine the hub of patient-centered care,” Dr. Cain said. “We have not arrived, but we’re on our way.”
In 2007, family medicine had the lowest match rate ever recorded, but the number of matches has increased each year for the past 5 years. There are now 26,000 student members of the AAFP today – one in four U.S. medical students, Dr. Cain said.
Access to primary care has increased as well, he said. Six years ago, there were some 47 million uninsured Americans. The push for the Affordable Care Act “unleashed a political firestorm,” nationally and within the AAFP membership, Dr. Cain said.
The uninsured rate has dropped from 18% to about 13% currently, he said.
“Today I stand before you a witness to what I see as the rebirth of family medicine,” Dr. Cain said.
On Twitter @aliciaault
AT THE AAFP CONGRESS OF DELEGATES 2014
Family docs mull abortion, EHRs, gun safety at AAFP Congress
WASHINGTON – Resolutions to end restrictions on abortion providers and to encourage discussion of gun safety predictably elicited significant debate during reference committee discussions at the American Academy of Family Physicians’ annual policy-making meeting.
The Reference Committee on Advocacy considered two abortion-related proposals submitted by the New York State chapter, both aimed at removing state-imposed restrictions on providers, such as requiring physicians who provide the services to have admitting privileges at a nearby hospital.
Currently, 27 states have laws that restrict abortion providers, said Dr. Cathleen London of Weill Cornell Physicians, N.Y., an author of the two resolutions. The statutes interfere with access to care, and do not add protections for patients, she said.
“Regardless of where you stand on this issue, making abortion difficult or illegal means that we’ll see abortions performed unsafely,” Dr. London said. “It will not stop them.”
Dr. Reid B. Blackwelder, AAFP president, urged the committee to forward the resolutions to the board of directors for study rather than vote on them directly. “We’d also like to note that the AAFP has adopted a neutral position on abortion,” said Dr. Blackwelder.
But Dr. Robert Reneker of Mercy Health in Grand Rapids, Mich., supported the organization’s neutral position. “To get mixed up in this debate on abortion, and to get off the fence, serves no purpose in furthering some of our other goals,” Dr. Reneker said.
A resolution introduced by the Michigan chapter urges the AAFP to be more outspoken on gun safety. Many delegates supported the resolution’s call for the academy to advocate for legislation that would call for safe gun storage in the home, while others objected to a provision that would allow health insurers in the Affordable Care Act’s health exchanges to collect data about guns in the home.
An opioid-related resolution from the New York State chapter urged the Food and Drug Administration to rescind approval of the long-acting hydrocodone formulation Zohydro. The drug has been viewed by many as highly abusable, but some palliative care and hospice specialists told the reference committee that it was a necessary therapy for their patients.
Delegates also vented about electronic health records. A late resolution introduced by Dr. Leonard Finn of Wellesley, Mass., laid out a wish list of improvements that he said AAFP should advocate, including interoperability.
EHRs “fail to help us do what we want to do – provide excellent care for our patients,” Dr. Finn told the Reference Committee on Practice Enhancement, adding, “No bank, no airline system would tolerate the quality of the software we have to work with.”
Dr. Cecil Bennett of Peachtree City, Ga., also expressed his frustration with current state of EHRs. “I don’t want to tweak the current system, I want to blow it up,” said Dr. Bennett.
The full Congress of Delegates will hear all of the resolutions and vote on them on Oct. 21 and Oct. 22.
On Twitter @aliciaault
WASHINGTON – Resolutions to end restrictions on abortion providers and to encourage discussion of gun safety predictably elicited significant debate during reference committee discussions at the American Academy of Family Physicians’ annual policy-making meeting.
The Reference Committee on Advocacy considered two abortion-related proposals submitted by the New York State chapter, both aimed at removing state-imposed restrictions on providers, such as requiring physicians who provide the services to have admitting privileges at a nearby hospital.
Currently, 27 states have laws that restrict abortion providers, said Dr. Cathleen London of Weill Cornell Physicians, N.Y., an author of the two resolutions. The statutes interfere with access to care, and do not add protections for patients, she said.
“Regardless of where you stand on this issue, making abortion difficult or illegal means that we’ll see abortions performed unsafely,” Dr. London said. “It will not stop them.”
Dr. Reid B. Blackwelder, AAFP president, urged the committee to forward the resolutions to the board of directors for study rather than vote on them directly. “We’d also like to note that the AAFP has adopted a neutral position on abortion,” said Dr. Blackwelder.
But Dr. Robert Reneker of Mercy Health in Grand Rapids, Mich., supported the organization’s neutral position. “To get mixed up in this debate on abortion, and to get off the fence, serves no purpose in furthering some of our other goals,” Dr. Reneker said.
A resolution introduced by the Michigan chapter urges the AAFP to be more outspoken on gun safety. Many delegates supported the resolution’s call for the academy to advocate for legislation that would call for safe gun storage in the home, while others objected to a provision that would allow health insurers in the Affordable Care Act’s health exchanges to collect data about guns in the home.
An opioid-related resolution from the New York State chapter urged the Food and Drug Administration to rescind approval of the long-acting hydrocodone formulation Zohydro. The drug has been viewed by many as highly abusable, but some palliative care and hospice specialists told the reference committee that it was a necessary therapy for their patients.
Delegates also vented about electronic health records. A late resolution introduced by Dr. Leonard Finn of Wellesley, Mass., laid out a wish list of improvements that he said AAFP should advocate, including interoperability.
EHRs “fail to help us do what we want to do – provide excellent care for our patients,” Dr. Finn told the Reference Committee on Practice Enhancement, adding, “No bank, no airline system would tolerate the quality of the software we have to work with.”
Dr. Cecil Bennett of Peachtree City, Ga., also expressed his frustration with current state of EHRs. “I don’t want to tweak the current system, I want to blow it up,” said Dr. Bennett.
The full Congress of Delegates will hear all of the resolutions and vote on them on Oct. 21 and Oct. 22.
On Twitter @aliciaault
WASHINGTON – Resolutions to end restrictions on abortion providers and to encourage discussion of gun safety predictably elicited significant debate during reference committee discussions at the American Academy of Family Physicians’ annual policy-making meeting.
The Reference Committee on Advocacy considered two abortion-related proposals submitted by the New York State chapter, both aimed at removing state-imposed restrictions on providers, such as requiring physicians who provide the services to have admitting privileges at a nearby hospital.
Currently, 27 states have laws that restrict abortion providers, said Dr. Cathleen London of Weill Cornell Physicians, N.Y., an author of the two resolutions. The statutes interfere with access to care, and do not add protections for patients, she said.
“Regardless of where you stand on this issue, making abortion difficult or illegal means that we’ll see abortions performed unsafely,” Dr. London said. “It will not stop them.”
Dr. Reid B. Blackwelder, AAFP president, urged the committee to forward the resolutions to the board of directors for study rather than vote on them directly. “We’d also like to note that the AAFP has adopted a neutral position on abortion,” said Dr. Blackwelder.
But Dr. Robert Reneker of Mercy Health in Grand Rapids, Mich., supported the organization’s neutral position. “To get mixed up in this debate on abortion, and to get off the fence, serves no purpose in furthering some of our other goals,” Dr. Reneker said.
A resolution introduced by the Michigan chapter urges the AAFP to be more outspoken on gun safety. Many delegates supported the resolution’s call for the academy to advocate for legislation that would call for safe gun storage in the home, while others objected to a provision that would allow health insurers in the Affordable Care Act’s health exchanges to collect data about guns in the home.
An opioid-related resolution from the New York State chapter urged the Food and Drug Administration to rescind approval of the long-acting hydrocodone formulation Zohydro. The drug has been viewed by many as highly abusable, but some palliative care and hospice specialists told the reference committee that it was a necessary therapy for their patients.
Delegates also vented about electronic health records. A late resolution introduced by Dr. Leonard Finn of Wellesley, Mass., laid out a wish list of improvements that he said AAFP should advocate, including interoperability.
EHRs “fail to help us do what we want to do – provide excellent care for our patients,” Dr. Finn told the Reference Committee on Practice Enhancement, adding, “No bank, no airline system would tolerate the quality of the software we have to work with.”
Dr. Cecil Bennett of Peachtree City, Ga., also expressed his frustration with current state of EHRs. “I don’t want to tweak the current system, I want to blow it up,” said Dr. Bennett.
The full Congress of Delegates will hear all of the resolutions and vote on them on Oct. 21 and Oct. 22.
On Twitter @aliciaault
AT THE AAFP CONGRESS OF DELEGATES