User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
‘Dr. Caveman’ had a leg up on amputation
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
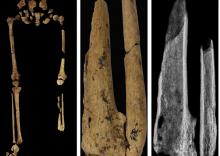
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
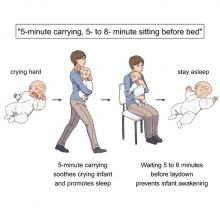
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
AMA joins in lawsuit accusing Cigna of underpaying physicians
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
Flashy, blingy doc sabotages his own malpractice trial in rural farm town
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
FDA warns of clip lock malfunctions with MitraClip devices
The Food and Drug Administration is alerting health care providers about the potential for clip lock malfunctions with Abbott’s MitraClip’s delivery system.
“These events appear to occur in approximately 1.3% of MitraClip procedures and have been observed with all device models,” the FDA says in a letter posted on its website.
The MitraClip device was approved in 2013 for patients with symptomatic, degenerative mitral regurgitation (MR) deemed high risk for mitral-valve surgery.
In its own “urgent medical device correction letter” to providers, Abbott reports a recent increase in reports of the clips failing to “establish final arm angle (EFAA)” and of “clip opening while locked (COWL)” events.
During device preparation and prior to clip deployment, the operator intentionally attempts to open a locked clip to verify that the locking mechanism is engaged.
COWL describes when the clip arm angle increases postdeployment. “In these cases, users observe a slippage in the lock, resulting in an arm angle greater than 10 degrees from the angle observed at deployment,” which can be identified through fluoroscopy, Abbott says.
From February 2021 to January 2022, the EFAA failure rate was 0.51% and COWL rate 0.28%, increasing to 0.80% and 0.50%, respectively, from February 2022 to July 2022, according to the company.
Despite the increase in reports, the acute procedural success rate remains consistent with historical data, according to Abbott. “Further, EFAA failure or COWL most often results in no adverse patient outcomes. COWL may lead to less MR reduction, which is often treated with the use of one or more additional clips.”
Abbott says there is also a “low incidence” of required additional interventions. No immediate open surgical conversions have occurred as a result of EFAA/COWL events, whereas 0.53% of such events have resulted in nonurgent surgical conversions.
“In any case where significant residual MR is observed after clip deployment, a second clip should be considered and implanted in accordance with the IFU [instructions for use],” it advises.
Abbott says that a “change in the material properties of one of the clip locking components” has been identified as a contributing cause of EFAA/COWL events. It is working on producing new lots with updated manufacturing processing and raw material to mitigate the risk.
Certain use conditions can also contribute to EFAA/COWL events, and are referenced in the IFU, Appendix A, it notes.
The FDA is working with Abbott and recommends that health care providers do the following:
- Review the recall notice from Abbott for all MitraClip Clip Delivery Systems.
- Be aware of the potential for clip lock malfunctions before or after deployment with this device.
- Read and carefully follow the instructions for use and the recommendations provided in the recall notice to help minimize the chance of the clip failing to lock. These include recommendations about procedural steps for implant positioning, locking sequences, establishing clip arm angle, preparation for clip release, and avoiding excessive force and manipulation when unlocking the clip during device preparation and during the procedure.
Health care professionals can also report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration is alerting health care providers about the potential for clip lock malfunctions with Abbott’s MitraClip’s delivery system.
“These events appear to occur in approximately 1.3% of MitraClip procedures and have been observed with all device models,” the FDA says in a letter posted on its website.
The MitraClip device was approved in 2013 for patients with symptomatic, degenerative mitral regurgitation (MR) deemed high risk for mitral-valve surgery.
In its own “urgent medical device correction letter” to providers, Abbott reports a recent increase in reports of the clips failing to “establish final arm angle (EFAA)” and of “clip opening while locked (COWL)” events.
During device preparation and prior to clip deployment, the operator intentionally attempts to open a locked clip to verify that the locking mechanism is engaged.
COWL describes when the clip arm angle increases postdeployment. “In these cases, users observe a slippage in the lock, resulting in an arm angle greater than 10 degrees from the angle observed at deployment,” which can be identified through fluoroscopy, Abbott says.
From February 2021 to January 2022, the EFAA failure rate was 0.51% and COWL rate 0.28%, increasing to 0.80% and 0.50%, respectively, from February 2022 to July 2022, according to the company.
Despite the increase in reports, the acute procedural success rate remains consistent with historical data, according to Abbott. “Further, EFAA failure or COWL most often results in no adverse patient outcomes. COWL may lead to less MR reduction, which is often treated with the use of one or more additional clips.”
Abbott says there is also a “low incidence” of required additional interventions. No immediate open surgical conversions have occurred as a result of EFAA/COWL events, whereas 0.53% of such events have resulted in nonurgent surgical conversions.
“In any case where significant residual MR is observed after clip deployment, a second clip should be considered and implanted in accordance with the IFU [instructions for use],” it advises.
Abbott says that a “change in the material properties of one of the clip locking components” has been identified as a contributing cause of EFAA/COWL events. It is working on producing new lots with updated manufacturing processing and raw material to mitigate the risk.
Certain use conditions can also contribute to EFAA/COWL events, and are referenced in the IFU, Appendix A, it notes.
The FDA is working with Abbott and recommends that health care providers do the following:
- Review the recall notice from Abbott for all MitraClip Clip Delivery Systems.
- Be aware of the potential for clip lock malfunctions before or after deployment with this device.
- Read and carefully follow the instructions for use and the recommendations provided in the recall notice to help minimize the chance of the clip failing to lock. These include recommendations about procedural steps for implant positioning, locking sequences, establishing clip arm angle, preparation for clip release, and avoiding excessive force and manipulation when unlocking the clip during device preparation and during the procedure.
Health care professionals can also report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration is alerting health care providers about the potential for clip lock malfunctions with Abbott’s MitraClip’s delivery system.
“These events appear to occur in approximately 1.3% of MitraClip procedures and have been observed with all device models,” the FDA says in a letter posted on its website.
The MitraClip device was approved in 2013 for patients with symptomatic, degenerative mitral regurgitation (MR) deemed high risk for mitral-valve surgery.
In its own “urgent medical device correction letter” to providers, Abbott reports a recent increase in reports of the clips failing to “establish final arm angle (EFAA)” and of “clip opening while locked (COWL)” events.
During device preparation and prior to clip deployment, the operator intentionally attempts to open a locked clip to verify that the locking mechanism is engaged.
COWL describes when the clip arm angle increases postdeployment. “In these cases, users observe a slippage in the lock, resulting in an arm angle greater than 10 degrees from the angle observed at deployment,” which can be identified through fluoroscopy, Abbott says.
From February 2021 to January 2022, the EFAA failure rate was 0.51% and COWL rate 0.28%, increasing to 0.80% and 0.50%, respectively, from February 2022 to July 2022, according to the company.
Despite the increase in reports, the acute procedural success rate remains consistent with historical data, according to Abbott. “Further, EFAA failure or COWL most often results in no adverse patient outcomes. COWL may lead to less MR reduction, which is often treated with the use of one or more additional clips.”
Abbott says there is also a “low incidence” of required additional interventions. No immediate open surgical conversions have occurred as a result of EFAA/COWL events, whereas 0.53% of such events have resulted in nonurgent surgical conversions.
“In any case where significant residual MR is observed after clip deployment, a second clip should be considered and implanted in accordance with the IFU [instructions for use],” it advises.
Abbott says that a “change in the material properties of one of the clip locking components” has been identified as a contributing cause of EFAA/COWL events. It is working on producing new lots with updated manufacturing processing and raw material to mitigate the risk.
Certain use conditions can also contribute to EFAA/COWL events, and are referenced in the IFU, Appendix A, it notes.
The FDA is working with Abbott and recommends that health care providers do the following:
- Review the recall notice from Abbott for all MitraClip Clip Delivery Systems.
- Be aware of the potential for clip lock malfunctions before or after deployment with this device.
- Read and carefully follow the instructions for use and the recommendations provided in the recall notice to help minimize the chance of the clip failing to lock. These include recommendations about procedural steps for implant positioning, locking sequences, establishing clip arm angle, preparation for clip release, and avoiding excessive force and manipulation when unlocking the clip during device preparation and during the procedure.
Health care professionals can also report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
One fish, two fish, are good fish for you ... fish
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Real medical news: Many teens trust fake medical news
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
Living-donor liver transplants linked with substantial survival benefit
Living-donor liver transplant recipients gained an additional 13-17 years of life, compared with patients who remained on the wait list, according to a retrospective case-control study.
The data suggest that the life-years gained are comparable to or greater than those conferred by either other lifesaving procedures or liver transplant from a deceased donor, wrote the researchers, led by Whitney Jackson, MD, assistant professor of gastroenterology and medical director of living-donor liver transplantation at the University of Colorado Anschutz Medical Campus.
“Despite the acceptance of living-donor liver transplant as a lifesaving procedure for end-stage liver disease, it remains underused in the United States,” the authors wrote in JAMA Surgery. “This study’s findings challenge current perceptions regarding when the survival benefit of a living-donor transplant occurs.”
Dr. Jackson and colleagues conducted a retrospective, secondary analysis of the Scientific Registry of Transplant Recipients database for 119,275 U.S. liver transplant candidates and recipients from January 2012 to September 2021. They assessed the survival benefit, life-years saved, and the Model for End-Stage Liver Disease incorporating sodium levels (MELD-Na) score at which the survival benefit was obtained, compared with those who remained on the wait list.
The research team included 116,455 liver transplant candidates who were 18 and older and assigned to the wait list, as well as 2,820 patients who received a living-donor liver transplant. Patients listed for retransplant or multiorgan transplant were excluded, as were those with prior kidney or liver transplants.
The mean age of the study participants was 55 years, and 63% were men. Overall, 70.2% were White, 15.8% were Hispanic or Latinx, 8.2% were Black or African American, 4.3% were Asian, 0.9% were American Indian or Alaska Native, and 0.2% were Native Hawaiian or Pacific Islander. The most common etiologies were alcoholic cirrhosis (23.8%) and nonalcoholic steatohepatitis (15.9%).
Compared with patients on the wait list, recipients of a living-donor liver transplant were younger, more often women, more educated, and more often White. A greater proportion of transplant recipients had a primary etiology of nonalcoholic steatohepatitis (19.8%) and cholestatic liver disease (24.1%). At wait list placement, one-third of candidates had a MELD-Na score of 14 or higher.
The research team found a significant survival benefit for patients receiving a living-donor liver transplant based on mortality risk and survival scores. The survival benefit was significant at a MELD-Na score as low as 11, with a 34% decrease(95% confidence interval [CI], 17.4%-52.0%) in mortality compared with the wait list. In addition, mortality risk models confirmed a survival benefit for patients with a MELD-Na score of 11 or higher at 1 year after transplant (adjusted hazard ratio, 0.64; 95% CI, 0.47-0.88; P = .006). At a MELD-Na score of 14-16, mortality decreased by about 50% (aHR, 0.47; 95% CI, 0.34-0.66; P < .001).
The probability of death from a living-donor liver transplant for patients with very low MELD-Na scores (between 6 and 10) was greater than that for patients on the wait list for the first 259 days, at which point the risk of death for both groups was equal. At 471 days, the probability of survival in both groups was equal. As the MELD-Na score increased, both the time to equal risk of death and the time to equal survival decreased, demonstrating that the survival benefit occurs much earlier for patients with a higher MELD-Na score.
Analysis of life-years from transplant showed living-donor transplant recipients gained 13-17 life-years compared to those who didn’t receive one.
“Living-donor liver transplantation is a valuable yet underutilized strategy to address the significant organ shortage and long waiting times on the transplant list in the U.S.,” said Renu Dhanasekaran, MD, PhD, assistant professor of gastroenterology and hepatology at Stanford (Calif.) University.
Dr. Dhanasekaran, who wasn’t involved with this study, also welcomed the finding that living-donor liver transplantation can benefit patients with low MELD-Na scores, even below the expected cutoff at 15. According to the study authors, previous research had suggested benefit would be seen only at MELD-Na 15 and above.
“In my practice, I have several patients whose symptoms are out of proportion to their MELD score, and data like this will convince them and their potential donors to avail a transplant at an earlier stage,” she said.
The findings challenge the current paradigm around the timing of referral for a liver transplant and may have ramifications for allocation policies for deceased donors, the study authors wrote. The data can also help to contextualize risk-benefit discussions for donors and recipients.
“Donating a part of one’s liver to save a patient suffering from end-stage liver disease is an incredible act of selfless love,” Dr. Dhanasekaran said. “I hope strong positive data from studies like this one encourage more donors, patients, and transplant centers to expand the use of [living-donor liver transplant].”
The authors reported no grant support or funding sources for this study. One author disclosed being married to the current chair of the United Network for Organ Sharing’s Liver and Intestinal Organ Transplantation Committee. No other conflicts of interest were reported. Dr. Dhanasekaran reported no relevant disclosures.
Living-donor liver transplant recipients gained an additional 13-17 years of life, compared with patients who remained on the wait list, according to a retrospective case-control study.
The data suggest that the life-years gained are comparable to or greater than those conferred by either other lifesaving procedures or liver transplant from a deceased donor, wrote the researchers, led by Whitney Jackson, MD, assistant professor of gastroenterology and medical director of living-donor liver transplantation at the University of Colorado Anschutz Medical Campus.
“Despite the acceptance of living-donor liver transplant as a lifesaving procedure for end-stage liver disease, it remains underused in the United States,” the authors wrote in JAMA Surgery. “This study’s findings challenge current perceptions regarding when the survival benefit of a living-donor transplant occurs.”
Dr. Jackson and colleagues conducted a retrospective, secondary analysis of the Scientific Registry of Transplant Recipients database for 119,275 U.S. liver transplant candidates and recipients from January 2012 to September 2021. They assessed the survival benefit, life-years saved, and the Model for End-Stage Liver Disease incorporating sodium levels (MELD-Na) score at which the survival benefit was obtained, compared with those who remained on the wait list.
The research team included 116,455 liver transplant candidates who were 18 and older and assigned to the wait list, as well as 2,820 patients who received a living-donor liver transplant. Patients listed for retransplant or multiorgan transplant were excluded, as were those with prior kidney or liver transplants.
The mean age of the study participants was 55 years, and 63% were men. Overall, 70.2% were White, 15.8% were Hispanic or Latinx, 8.2% were Black or African American, 4.3% were Asian, 0.9% were American Indian or Alaska Native, and 0.2% were Native Hawaiian or Pacific Islander. The most common etiologies were alcoholic cirrhosis (23.8%) and nonalcoholic steatohepatitis (15.9%).
Compared with patients on the wait list, recipients of a living-donor liver transplant were younger, more often women, more educated, and more often White. A greater proportion of transplant recipients had a primary etiology of nonalcoholic steatohepatitis (19.8%) and cholestatic liver disease (24.1%). At wait list placement, one-third of candidates had a MELD-Na score of 14 or higher.
The research team found a significant survival benefit for patients receiving a living-donor liver transplant based on mortality risk and survival scores. The survival benefit was significant at a MELD-Na score as low as 11, with a 34% decrease(95% confidence interval [CI], 17.4%-52.0%) in mortality compared with the wait list. In addition, mortality risk models confirmed a survival benefit for patients with a MELD-Na score of 11 or higher at 1 year after transplant (adjusted hazard ratio, 0.64; 95% CI, 0.47-0.88; P = .006). At a MELD-Na score of 14-16, mortality decreased by about 50% (aHR, 0.47; 95% CI, 0.34-0.66; P < .001).
The probability of death from a living-donor liver transplant for patients with very low MELD-Na scores (between 6 and 10) was greater than that for patients on the wait list for the first 259 days, at which point the risk of death for both groups was equal. At 471 days, the probability of survival in both groups was equal. As the MELD-Na score increased, both the time to equal risk of death and the time to equal survival decreased, demonstrating that the survival benefit occurs much earlier for patients with a higher MELD-Na score.
Analysis of life-years from transplant showed living-donor transplant recipients gained 13-17 life-years compared to those who didn’t receive one.
“Living-donor liver transplantation is a valuable yet underutilized strategy to address the significant organ shortage and long waiting times on the transplant list in the U.S.,” said Renu Dhanasekaran, MD, PhD, assistant professor of gastroenterology and hepatology at Stanford (Calif.) University.
Dr. Dhanasekaran, who wasn’t involved with this study, also welcomed the finding that living-donor liver transplantation can benefit patients with low MELD-Na scores, even below the expected cutoff at 15. According to the study authors, previous research had suggested benefit would be seen only at MELD-Na 15 and above.
“In my practice, I have several patients whose symptoms are out of proportion to their MELD score, and data like this will convince them and their potential donors to avail a transplant at an earlier stage,” she said.
The findings challenge the current paradigm around the timing of referral for a liver transplant and may have ramifications for allocation policies for deceased donors, the study authors wrote. The data can also help to contextualize risk-benefit discussions for donors and recipients.
“Donating a part of one’s liver to save a patient suffering from end-stage liver disease is an incredible act of selfless love,” Dr. Dhanasekaran said. “I hope strong positive data from studies like this one encourage more donors, patients, and transplant centers to expand the use of [living-donor liver transplant].”
The authors reported no grant support or funding sources for this study. One author disclosed being married to the current chair of the United Network for Organ Sharing’s Liver and Intestinal Organ Transplantation Committee. No other conflicts of interest were reported. Dr. Dhanasekaran reported no relevant disclosures.
Living-donor liver transplant recipients gained an additional 13-17 years of life, compared with patients who remained on the wait list, according to a retrospective case-control study.
The data suggest that the life-years gained are comparable to or greater than those conferred by either other lifesaving procedures or liver transplant from a deceased donor, wrote the researchers, led by Whitney Jackson, MD, assistant professor of gastroenterology and medical director of living-donor liver transplantation at the University of Colorado Anschutz Medical Campus.
“Despite the acceptance of living-donor liver transplant as a lifesaving procedure for end-stage liver disease, it remains underused in the United States,” the authors wrote in JAMA Surgery. “This study’s findings challenge current perceptions regarding when the survival benefit of a living-donor transplant occurs.”
Dr. Jackson and colleagues conducted a retrospective, secondary analysis of the Scientific Registry of Transplant Recipients database for 119,275 U.S. liver transplant candidates and recipients from January 2012 to September 2021. They assessed the survival benefit, life-years saved, and the Model for End-Stage Liver Disease incorporating sodium levels (MELD-Na) score at which the survival benefit was obtained, compared with those who remained on the wait list.
The research team included 116,455 liver transplant candidates who were 18 and older and assigned to the wait list, as well as 2,820 patients who received a living-donor liver transplant. Patients listed for retransplant or multiorgan transplant were excluded, as were those with prior kidney or liver transplants.
The mean age of the study participants was 55 years, and 63% were men. Overall, 70.2% were White, 15.8% were Hispanic or Latinx, 8.2% were Black or African American, 4.3% were Asian, 0.9% were American Indian or Alaska Native, and 0.2% were Native Hawaiian or Pacific Islander. The most common etiologies were alcoholic cirrhosis (23.8%) and nonalcoholic steatohepatitis (15.9%).
Compared with patients on the wait list, recipients of a living-donor liver transplant were younger, more often women, more educated, and more often White. A greater proportion of transplant recipients had a primary etiology of nonalcoholic steatohepatitis (19.8%) and cholestatic liver disease (24.1%). At wait list placement, one-third of candidates had a MELD-Na score of 14 or higher.
The research team found a significant survival benefit for patients receiving a living-donor liver transplant based on mortality risk and survival scores. The survival benefit was significant at a MELD-Na score as low as 11, with a 34% decrease(95% confidence interval [CI], 17.4%-52.0%) in mortality compared with the wait list. In addition, mortality risk models confirmed a survival benefit for patients with a MELD-Na score of 11 or higher at 1 year after transplant (adjusted hazard ratio, 0.64; 95% CI, 0.47-0.88; P = .006). At a MELD-Na score of 14-16, mortality decreased by about 50% (aHR, 0.47; 95% CI, 0.34-0.66; P < .001).
The probability of death from a living-donor liver transplant for patients with very low MELD-Na scores (between 6 and 10) was greater than that for patients on the wait list for the first 259 days, at which point the risk of death for both groups was equal. At 471 days, the probability of survival in both groups was equal. As the MELD-Na score increased, both the time to equal risk of death and the time to equal survival decreased, demonstrating that the survival benefit occurs much earlier for patients with a higher MELD-Na score.
Analysis of life-years from transplant showed living-donor transplant recipients gained 13-17 life-years compared to those who didn’t receive one.
“Living-donor liver transplantation is a valuable yet underutilized strategy to address the significant organ shortage and long waiting times on the transplant list in the U.S.,” said Renu Dhanasekaran, MD, PhD, assistant professor of gastroenterology and hepatology at Stanford (Calif.) University.
Dr. Dhanasekaran, who wasn’t involved with this study, also welcomed the finding that living-donor liver transplantation can benefit patients with low MELD-Na scores, even below the expected cutoff at 15. According to the study authors, previous research had suggested benefit would be seen only at MELD-Na 15 and above.
“In my practice, I have several patients whose symptoms are out of proportion to their MELD score, and data like this will convince them and their potential donors to avail a transplant at an earlier stage,” she said.
The findings challenge the current paradigm around the timing of referral for a liver transplant and may have ramifications for allocation policies for deceased donors, the study authors wrote. The data can also help to contextualize risk-benefit discussions for donors and recipients.
“Donating a part of one’s liver to save a patient suffering from end-stage liver disease is an incredible act of selfless love,” Dr. Dhanasekaran said. “I hope strong positive data from studies like this one encourage more donors, patients, and transplant centers to expand the use of [living-donor liver transplant].”
The authors reported no grant support or funding sources for this study. One author disclosed being married to the current chair of the United Network for Organ Sharing’s Liver and Intestinal Organ Transplantation Committee. No other conflicts of interest were reported. Dr. Dhanasekaran reported no relevant disclosures.
FROM JAMA SURGERY
ARBs, beta-blockers independently inhibit Marfan syndrome progression
Early start might delay surgery
Beta-blockers have long been recommended to prevent aortic dissection associated with Marfan syndrome despite limited evidence, but a new analysis also supports a benefit from angiotensin receptors blockers (ARBs) and further suggests that beta-blockers and ARBs exert independent effects.
For the endpoint of inhibition of growth of the aortic root, “there is no evidence of any interaction between the effects of ARBs with beta-blockers, and so we think that the treatment effects are likely to be additive,” reported Alex Pitcher, BMBCh, DPhil, Oxford (England) University Hospitals, NHS Trust.
Based on these data, Dr. Pitcher recommended considering ARBs and beta-blockers together soon after the diagnosis of Marfan syndrome. This includes young children.
“We think that medical treatments can delay surgery and dissection substantially if given for a number of years,” he added.
In this study, undertaken by the Marfan Treatment Trialists (MTT) collaboration, data were available from 1,442 Marfan syndrome patients participating in seven treatment trials. The primary outcome was aortic root enlargement, a predictor of life-threatening aortic dissection and rupture. Rather than a meta-analysis of the pooled data, the meta-analysis was conducted with individual patient data that involved collaboration with the original trialists.
Four of the studies with 746 patients compared ARBs to placebo or a control medication. A second group of three trials with 766 patients compared ARBs to beta-blockers.
From the two sets of data, a calculation of the effect of beta-blockers was indirectly estimated.
ARBs slow annualized aortic growth rate significantly
In the first set of trials, the analysis showed a significantly slower annualized aortic root growth rate for those treated with ARBs relative to controls (0.07 vs. 0.13), producing a statistically significant absolute difference (0.7%; P = .01) in favor of the ARB.
“In other words, the rate of growth was nearly double in the control arm,” Dr. Pitcher said.
In the three trials comparing ARBs to beta-blockers, the annualized growth rate among those taking an ARB was similar (0.8%) to that seen in the previous set of controlled trials. This rate of annualized growth was not significantly different from the 0.11% annualized rate of growth in patients receiving beta-blockers. When an analysis of the impact of beta-blockers was conducted by indirectly evaluating the change in growth relative to controls, the estimated impact was an annualized growth rate of 0.9% (P = .042).
A second set of data provided the basis for suggesting that the effects of beta ARBs and beta-blockers are independent and potentially additive.
“We were able to look at subgroups of patients in the ARB trials that were broken down by whether they were or were not on beta-blockers at baseline, and so by doing able to estimate independent effects,” Dr. Pitcher said. The lack of any interactions led Dr. Pitcher to conclude that benefits are likely additive.
Of patients genotyped in the ARB studies, more than 80% had the FBN1 pathogenic variant of Marfan syndrome. When the data were analyzed by subgroups, including age or blood pressure, there were no differences in treatment effect except for those with the FBN1 mutation in whom the benefit of ARB therapy was greater relative to those without.
As FBN1 is one of the most common genetic signatures of Marfan syndrome, the “greater effect of ARBs in this group makes it more plausible that the effect is real,” Dr. Pitcher said.
Results could change treatment guidelines
Current guidelines recommend beta-blockers in Marfan syndrome prior to a dilatation size of 4.5 to 5 cm when surgery is indicated, according to Dr. Pitcher, but he said these data might change guidelines. While reinforcing the benefit of beta-blockers, this analysis suggests ARBs should also be considered, possibly in combination with beta-blockers.
“What I hope this meta-analysis does is add substantially to the certainty with which physicians can discuss treatments with patients.”
As for the mechanism, it is reasonable to speculate the antihypertensive effect of both medications is relevant, but each has plausible independent activities that might contribute to modifying aortic growth, according to Roland R.J. van Kimmenade, MD, PhD, a specialist in aortic diseases and heart failure at Raboud University Medical Center, Nijmegan, the Netherlands.
Citing several studies, he suggested that the benefit of beta-blockers could also stem from their ability to reduce heart rate and aortic stiffness while ARBs are likely to inhibit the interaction between the renin-angiotensin system (RAS) and TGF-beta pathway. Each of these might participate in risk of aortic root growth, according to Dr. van Kimmenade, who was invited by ESC to discuss this study.
On the basis of these data as well as past studies, he agreed that the combination of beta-blockers and ARBs might not just be additive but “even a little bit synergistic.”
While Dr. Pitcher suggested that the evidence supports starting both beta-blockers and ARBs soon after the diagnosis, Dr. van Kimmenade said, “I don’t like using beta-blockers in young patients, but ARBs are now shown to be an excellent alternative.”
Ultimately, “the prescription pencil will not replace the surgical knife” in a disease that is likely to eventually require surgery to prevent life-threatening events, according to Dr. van Kimmenade, but he agreed that these data provide more certainty about the value of beta-blockers and ARBs for slowing progression.
Dr. Pitcher reports no potential conflicts of interest. Dr. van Kimmenade has financial relationships with Bayer and Novartis.
Early start might delay surgery
Early start might delay surgery
Beta-blockers have long been recommended to prevent aortic dissection associated with Marfan syndrome despite limited evidence, but a new analysis also supports a benefit from angiotensin receptors blockers (ARBs) and further suggests that beta-blockers and ARBs exert independent effects.
For the endpoint of inhibition of growth of the aortic root, “there is no evidence of any interaction between the effects of ARBs with beta-blockers, and so we think that the treatment effects are likely to be additive,” reported Alex Pitcher, BMBCh, DPhil, Oxford (England) University Hospitals, NHS Trust.
Based on these data, Dr. Pitcher recommended considering ARBs and beta-blockers together soon after the diagnosis of Marfan syndrome. This includes young children.
“We think that medical treatments can delay surgery and dissection substantially if given for a number of years,” he added.
In this study, undertaken by the Marfan Treatment Trialists (MTT) collaboration, data were available from 1,442 Marfan syndrome patients participating in seven treatment trials. The primary outcome was aortic root enlargement, a predictor of life-threatening aortic dissection and rupture. Rather than a meta-analysis of the pooled data, the meta-analysis was conducted with individual patient data that involved collaboration with the original trialists.
Four of the studies with 746 patients compared ARBs to placebo or a control medication. A second group of three trials with 766 patients compared ARBs to beta-blockers.
From the two sets of data, a calculation of the effect of beta-blockers was indirectly estimated.
ARBs slow annualized aortic growth rate significantly
In the first set of trials, the analysis showed a significantly slower annualized aortic root growth rate for those treated with ARBs relative to controls (0.07 vs. 0.13), producing a statistically significant absolute difference (0.7%; P = .01) in favor of the ARB.
“In other words, the rate of growth was nearly double in the control arm,” Dr. Pitcher said.
In the three trials comparing ARBs to beta-blockers, the annualized growth rate among those taking an ARB was similar (0.8%) to that seen in the previous set of controlled trials. This rate of annualized growth was not significantly different from the 0.11% annualized rate of growth in patients receiving beta-blockers. When an analysis of the impact of beta-blockers was conducted by indirectly evaluating the change in growth relative to controls, the estimated impact was an annualized growth rate of 0.9% (P = .042).
A second set of data provided the basis for suggesting that the effects of beta ARBs and beta-blockers are independent and potentially additive.
“We were able to look at subgroups of patients in the ARB trials that were broken down by whether they were or were not on beta-blockers at baseline, and so by doing able to estimate independent effects,” Dr. Pitcher said. The lack of any interactions led Dr. Pitcher to conclude that benefits are likely additive.
Of patients genotyped in the ARB studies, more than 80% had the FBN1 pathogenic variant of Marfan syndrome. When the data were analyzed by subgroups, including age or blood pressure, there were no differences in treatment effect except for those with the FBN1 mutation in whom the benefit of ARB therapy was greater relative to those without.
As FBN1 is one of the most common genetic signatures of Marfan syndrome, the “greater effect of ARBs in this group makes it more plausible that the effect is real,” Dr. Pitcher said.
Results could change treatment guidelines
Current guidelines recommend beta-blockers in Marfan syndrome prior to a dilatation size of 4.5 to 5 cm when surgery is indicated, according to Dr. Pitcher, but he said these data might change guidelines. While reinforcing the benefit of beta-blockers, this analysis suggests ARBs should also be considered, possibly in combination with beta-blockers.
“What I hope this meta-analysis does is add substantially to the certainty with which physicians can discuss treatments with patients.”
As for the mechanism, it is reasonable to speculate the antihypertensive effect of both medications is relevant, but each has plausible independent activities that might contribute to modifying aortic growth, according to Roland R.J. van Kimmenade, MD, PhD, a specialist in aortic diseases and heart failure at Raboud University Medical Center, Nijmegan, the Netherlands.
Citing several studies, he suggested that the benefit of beta-blockers could also stem from their ability to reduce heart rate and aortic stiffness while ARBs are likely to inhibit the interaction between the renin-angiotensin system (RAS) and TGF-beta pathway. Each of these might participate in risk of aortic root growth, according to Dr. van Kimmenade, who was invited by ESC to discuss this study.
On the basis of these data as well as past studies, he agreed that the combination of beta-blockers and ARBs might not just be additive but “even a little bit synergistic.”
While Dr. Pitcher suggested that the evidence supports starting both beta-blockers and ARBs soon after the diagnosis, Dr. van Kimmenade said, “I don’t like using beta-blockers in young patients, but ARBs are now shown to be an excellent alternative.”
Ultimately, “the prescription pencil will not replace the surgical knife” in a disease that is likely to eventually require surgery to prevent life-threatening events, according to Dr. van Kimmenade, but he agreed that these data provide more certainty about the value of beta-blockers and ARBs for slowing progression.
Dr. Pitcher reports no potential conflicts of interest. Dr. van Kimmenade has financial relationships with Bayer and Novartis.
Beta-blockers have long been recommended to prevent aortic dissection associated with Marfan syndrome despite limited evidence, but a new analysis also supports a benefit from angiotensin receptors blockers (ARBs) and further suggests that beta-blockers and ARBs exert independent effects.
For the endpoint of inhibition of growth of the aortic root, “there is no evidence of any interaction between the effects of ARBs with beta-blockers, and so we think that the treatment effects are likely to be additive,” reported Alex Pitcher, BMBCh, DPhil, Oxford (England) University Hospitals, NHS Trust.
Based on these data, Dr. Pitcher recommended considering ARBs and beta-blockers together soon after the diagnosis of Marfan syndrome. This includes young children.
“We think that medical treatments can delay surgery and dissection substantially if given for a number of years,” he added.
In this study, undertaken by the Marfan Treatment Trialists (MTT) collaboration, data were available from 1,442 Marfan syndrome patients participating in seven treatment trials. The primary outcome was aortic root enlargement, a predictor of life-threatening aortic dissection and rupture. Rather than a meta-analysis of the pooled data, the meta-analysis was conducted with individual patient data that involved collaboration with the original trialists.
Four of the studies with 746 patients compared ARBs to placebo or a control medication. A second group of three trials with 766 patients compared ARBs to beta-blockers.
From the two sets of data, a calculation of the effect of beta-blockers was indirectly estimated.
ARBs slow annualized aortic growth rate significantly
In the first set of trials, the analysis showed a significantly slower annualized aortic root growth rate for those treated with ARBs relative to controls (0.07 vs. 0.13), producing a statistically significant absolute difference (0.7%; P = .01) in favor of the ARB.
“In other words, the rate of growth was nearly double in the control arm,” Dr. Pitcher said.
In the three trials comparing ARBs to beta-blockers, the annualized growth rate among those taking an ARB was similar (0.8%) to that seen in the previous set of controlled trials. This rate of annualized growth was not significantly different from the 0.11% annualized rate of growth in patients receiving beta-blockers. When an analysis of the impact of beta-blockers was conducted by indirectly evaluating the change in growth relative to controls, the estimated impact was an annualized growth rate of 0.9% (P = .042).
A second set of data provided the basis for suggesting that the effects of beta ARBs and beta-blockers are independent and potentially additive.
“We were able to look at subgroups of patients in the ARB trials that were broken down by whether they were or were not on beta-blockers at baseline, and so by doing able to estimate independent effects,” Dr. Pitcher said. The lack of any interactions led Dr. Pitcher to conclude that benefits are likely additive.
Of patients genotyped in the ARB studies, more than 80% had the FBN1 pathogenic variant of Marfan syndrome. When the data were analyzed by subgroups, including age or blood pressure, there were no differences in treatment effect except for those with the FBN1 mutation in whom the benefit of ARB therapy was greater relative to those without.
As FBN1 is one of the most common genetic signatures of Marfan syndrome, the “greater effect of ARBs in this group makes it more plausible that the effect is real,” Dr. Pitcher said.
Results could change treatment guidelines
Current guidelines recommend beta-blockers in Marfan syndrome prior to a dilatation size of 4.5 to 5 cm when surgery is indicated, according to Dr. Pitcher, but he said these data might change guidelines. While reinforcing the benefit of beta-blockers, this analysis suggests ARBs should also be considered, possibly in combination with beta-blockers.
“What I hope this meta-analysis does is add substantially to the certainty with which physicians can discuss treatments with patients.”
As for the mechanism, it is reasonable to speculate the antihypertensive effect of both medications is relevant, but each has plausible independent activities that might contribute to modifying aortic growth, according to Roland R.J. van Kimmenade, MD, PhD, a specialist in aortic diseases and heart failure at Raboud University Medical Center, Nijmegan, the Netherlands.
Citing several studies, he suggested that the benefit of beta-blockers could also stem from their ability to reduce heart rate and aortic stiffness while ARBs are likely to inhibit the interaction between the renin-angiotensin system (RAS) and TGF-beta pathway. Each of these might participate in risk of aortic root growth, according to Dr. van Kimmenade, who was invited by ESC to discuss this study.
On the basis of these data as well as past studies, he agreed that the combination of beta-blockers and ARBs might not just be additive but “even a little bit synergistic.”
While Dr. Pitcher suggested that the evidence supports starting both beta-blockers and ARBs soon after the diagnosis, Dr. van Kimmenade said, “I don’t like using beta-blockers in young patients, but ARBs are now shown to be an excellent alternative.”
Ultimately, “the prescription pencil will not replace the surgical knife” in a disease that is likely to eventually require surgery to prevent life-threatening events, according to Dr. van Kimmenade, but he agreed that these data provide more certainty about the value of beta-blockers and ARBs for slowing progression.
Dr. Pitcher reports no potential conflicts of interest. Dr. van Kimmenade has financial relationships with Bayer and Novartis.
FROM ESC CONGRESS 2022
Increased risk of dyspareunia following cesarean section
There is no evidence to support postulated associations between mode of delivery and subsequent maternal sexual enjoyment or frequency of intercourse, according to a new study from the University of Bristol (England). However, cesarean section was shown to be associated with a 74% increased risk of dyspareunia, and this was not necessarily due to abdominal scarring, the researchers said.
A team from the University of Bristol and the Karolinska Institutet in Sweden used data from participants in the Avon Longitudinal Study of Parents and Children, a prospective longitudinal birth cohort study also dubbed “Children of the 90s” and involving more than 14,000 women in the United Kingdom who were pregnant in 1991 and 1992. The study has been following the health and development of the parents, their children, and now their grandchildren in detail ever since.
The new study, published in BJOG, aimed to assess whether cesarean section maintains sexual well-being compared with vaginal delivery, as has been suggested to occur because of the reduced risk of genital damage – less chance of tearing – and the maintenance of vaginal tone. There is some evidence that cesarean section is associated with an increased risk of sexual problems such as dyspareunia, but few studies have looked at the postbirth period long term.
Mode of delivery was abstracted from routine obstetric records and recorded as one of either spontaneous vaginal delivery (SVD), cesarean section, assisted breech, breech extraction, forceps, or vacuum extraction. Women whose records showed “other” as mode of delivery or whose notes contained conflicting modes of delivery were excluded.
Self-reported questionnaires asking about general health and lifestyle and including questions relating to sexual enjoyment and frequency were collected at 33 months and at 5, 12, and 18 years postpartum. Women were asked if they enjoyed sexual intercourse, with possible responses of:
- Yes, very much.
- Yes, somewhat.
- No, not a lot.
- No, not at all.
- No sex at the moment.
Possible sexual frequency responses were:
- Not at all.
- Less than once a month.
- 1-3 times a month.
- About once a week.
- 2-4 times a week.
- 5 or more times a week.
First study to look at sexual frequency
The team noted that theirs is the first study investigating the association of mode of delivery with sexual frequency. “Although it may be less important for well-being than sexual enjoyment or sex-related pain, it is an important measure to observe alongside other sexual outcomes,” they said.
Separately, sex-related pain, in the vagina during sex or elsewhere after sex, was assessed once, at 11 years post partum.
The data showed that women who had a cesarean section (11% of the sample) tended to be older than those who had vaginal delivery, with a higher mean body mass index (24.2 versus 22.8 kg/m2), and were more likely to be nulliparous at the time of the index pregnancy (54% versus 44%).
There was no significant difference between cesarean section and vaginal delivery in terms of responses for sexual enjoyment or frequency at any time after childbirth, the authors said. Nor, in adjusted models, was there evidence of associations between the type of vaginal delivery and sexual enjoyment or frequency outcomes.
Pain during sex increased more than a decade after cesarean
However, while the majority of respondents reported no intercourse-related pain, those who delivered via cesarean were more likely than those who gave birth vaginally to report sex-related pain at 11 years post partum. This was specifically an elevated incidence of pain in the vagina during sex, with an odds ratio of 1.74 (95% confidence interval, 1.46-2.08) in the adjusted model. This finding was consistent for emergency and elective cesarean section separately – both types were associated with increased dyspareunia, compared with vaginal delivery.
The dataset did not include measures of individual prenatal sex-related pain and, therefore, “it is unknown from this study whether Caesarean section causes sex-related pain, as suggested by the findings, or whether prenatal sex-related pain predicts both Caesarean section and postnatal sex-related pain,” the researchers said.
“Longitudinal data on sex-related pain need to be collected both before and after parturition,” they recommend, to clarify the direction of a possible effect between cesarean section and dyspareunia.
Cesarean does not protect against sexual dysfunction
Meanwhile, “For women considering a planned Caesarean section in an uncomplicated pregnancy, evidence suggesting that Caesarean section may not protect against sexual dysfunction may help inform their decision-making in the antenatal period.”
Lead author Flo Martin, a PhD student in epidemiology at the University of Bristol, said: “Rates of Caesarean section have been rising over the last 20 years due to many contributing factors and, importantly, it has been suggested that Caesarean section maintains sexual wellbeing compared with vaginal delivery. It is crucial that a whole range of maternal and foetal outcomes following Caesarean section are investigated, including sexual wellbeing, to appropriately inform decision-making both pre- and postnatally.
“This research provides expectant mothers, as well as women who have given birth, with really important information and demonstrates that there was no difference in sexual enjoyment or sexual frequency at any time point postpartum between women who gave birth via Caesarean section and those who delivered vaginally. It also suggests that Caesarean section may not help protect against sexual dysfunction, as previously thought, where sex-related pain was higher among women who gave birth via Caesarean section more than 10 years postpartum.”
Asked to comment on the research, Dr. Leila Frodsham, consultant gynecologist and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “Sexual pain disorders affect 7.5% of women of all ages, but there are peaks: during the start of sexual activity, if subfertility is an issue, after childbirth, and in the peri/menopause. It can be up to three times more prevalent at these peak times.
“Many women with sexual pain are worried when they consider starting a family and request a Caesarean birth to reduce risk of worsening their pain. However, this study has demonstrated that a Caesarean birth is associated with increased sexual pain longer term, which is very useful for helping women to plan their births.
“While more research about postpartum sexual wellbeing is needed, the findings of this study are reassuring to those who are pregnant as it found no difference in the enjoyment or frequency of sex in the years after a vaginal or a Caesarean birth.
“Most women in the U.K. recover well whether they have a vaginal or a Caesarean birth. Women should be supported to make informed decisions about how they plan to give birth, and it is vital that health care professionals respect their preferences.”
A version of this article first appeared on Medscape UK.
There is no evidence to support postulated associations between mode of delivery and subsequent maternal sexual enjoyment or frequency of intercourse, according to a new study from the University of Bristol (England). However, cesarean section was shown to be associated with a 74% increased risk of dyspareunia, and this was not necessarily due to abdominal scarring, the researchers said.
A team from the University of Bristol and the Karolinska Institutet in Sweden used data from participants in the Avon Longitudinal Study of Parents and Children, a prospective longitudinal birth cohort study also dubbed “Children of the 90s” and involving more than 14,000 women in the United Kingdom who were pregnant in 1991 and 1992. The study has been following the health and development of the parents, their children, and now their grandchildren in detail ever since.
The new study, published in BJOG, aimed to assess whether cesarean section maintains sexual well-being compared with vaginal delivery, as has been suggested to occur because of the reduced risk of genital damage – less chance of tearing – and the maintenance of vaginal tone. There is some evidence that cesarean section is associated with an increased risk of sexual problems such as dyspareunia, but few studies have looked at the postbirth period long term.
Mode of delivery was abstracted from routine obstetric records and recorded as one of either spontaneous vaginal delivery (SVD), cesarean section, assisted breech, breech extraction, forceps, or vacuum extraction. Women whose records showed “other” as mode of delivery or whose notes contained conflicting modes of delivery were excluded.
Self-reported questionnaires asking about general health and lifestyle and including questions relating to sexual enjoyment and frequency were collected at 33 months and at 5, 12, and 18 years postpartum. Women were asked if they enjoyed sexual intercourse, with possible responses of:
- Yes, very much.
- Yes, somewhat.
- No, not a lot.
- No, not at all.
- No sex at the moment.
Possible sexual frequency responses were:
- Not at all.
- Less than once a month.
- 1-3 times a month.
- About once a week.
- 2-4 times a week.
- 5 or more times a week.
First study to look at sexual frequency
The team noted that theirs is the first study investigating the association of mode of delivery with sexual frequency. “Although it may be less important for well-being than sexual enjoyment or sex-related pain, it is an important measure to observe alongside other sexual outcomes,” they said.
Separately, sex-related pain, in the vagina during sex or elsewhere after sex, was assessed once, at 11 years post partum.
The data showed that women who had a cesarean section (11% of the sample) tended to be older than those who had vaginal delivery, with a higher mean body mass index (24.2 versus 22.8 kg/m2), and were more likely to be nulliparous at the time of the index pregnancy (54% versus 44%).
There was no significant difference between cesarean section and vaginal delivery in terms of responses for sexual enjoyment or frequency at any time after childbirth, the authors said. Nor, in adjusted models, was there evidence of associations between the type of vaginal delivery and sexual enjoyment or frequency outcomes.
Pain during sex increased more than a decade after cesarean
However, while the majority of respondents reported no intercourse-related pain, those who delivered via cesarean were more likely than those who gave birth vaginally to report sex-related pain at 11 years post partum. This was specifically an elevated incidence of pain in the vagina during sex, with an odds ratio of 1.74 (95% confidence interval, 1.46-2.08) in the adjusted model. This finding was consistent for emergency and elective cesarean section separately – both types were associated with increased dyspareunia, compared with vaginal delivery.
The dataset did not include measures of individual prenatal sex-related pain and, therefore, “it is unknown from this study whether Caesarean section causes sex-related pain, as suggested by the findings, or whether prenatal sex-related pain predicts both Caesarean section and postnatal sex-related pain,” the researchers said.
“Longitudinal data on sex-related pain need to be collected both before and after parturition,” they recommend, to clarify the direction of a possible effect between cesarean section and dyspareunia.
Cesarean does not protect against sexual dysfunction
Meanwhile, “For women considering a planned Caesarean section in an uncomplicated pregnancy, evidence suggesting that Caesarean section may not protect against sexual dysfunction may help inform their decision-making in the antenatal period.”
Lead author Flo Martin, a PhD student in epidemiology at the University of Bristol, said: “Rates of Caesarean section have been rising over the last 20 years due to many contributing factors and, importantly, it has been suggested that Caesarean section maintains sexual wellbeing compared with vaginal delivery. It is crucial that a whole range of maternal and foetal outcomes following Caesarean section are investigated, including sexual wellbeing, to appropriately inform decision-making both pre- and postnatally.
“This research provides expectant mothers, as well as women who have given birth, with really important information and demonstrates that there was no difference in sexual enjoyment or sexual frequency at any time point postpartum between women who gave birth via Caesarean section and those who delivered vaginally. It also suggests that Caesarean section may not help protect against sexual dysfunction, as previously thought, where sex-related pain was higher among women who gave birth via Caesarean section more than 10 years postpartum.”
Asked to comment on the research, Dr. Leila Frodsham, consultant gynecologist and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “Sexual pain disorders affect 7.5% of women of all ages, but there are peaks: during the start of sexual activity, if subfertility is an issue, after childbirth, and in the peri/menopause. It can be up to three times more prevalent at these peak times.
“Many women with sexual pain are worried when they consider starting a family and request a Caesarean birth to reduce risk of worsening their pain. However, this study has demonstrated that a Caesarean birth is associated with increased sexual pain longer term, which is very useful for helping women to plan their births.
“While more research about postpartum sexual wellbeing is needed, the findings of this study are reassuring to those who are pregnant as it found no difference in the enjoyment or frequency of sex in the years after a vaginal or a Caesarean birth.
“Most women in the U.K. recover well whether they have a vaginal or a Caesarean birth. Women should be supported to make informed decisions about how they plan to give birth, and it is vital that health care professionals respect their preferences.”
A version of this article first appeared on Medscape UK.
There is no evidence to support postulated associations between mode of delivery and subsequent maternal sexual enjoyment or frequency of intercourse, according to a new study from the University of Bristol (England). However, cesarean section was shown to be associated with a 74% increased risk of dyspareunia, and this was not necessarily due to abdominal scarring, the researchers said.
A team from the University of Bristol and the Karolinska Institutet in Sweden used data from participants in the Avon Longitudinal Study of Parents and Children, a prospective longitudinal birth cohort study also dubbed “Children of the 90s” and involving more than 14,000 women in the United Kingdom who were pregnant in 1991 and 1992. The study has been following the health and development of the parents, their children, and now their grandchildren in detail ever since.
The new study, published in BJOG, aimed to assess whether cesarean section maintains sexual well-being compared with vaginal delivery, as has been suggested to occur because of the reduced risk of genital damage – less chance of tearing – and the maintenance of vaginal tone. There is some evidence that cesarean section is associated with an increased risk of sexual problems such as dyspareunia, but few studies have looked at the postbirth period long term.
Mode of delivery was abstracted from routine obstetric records and recorded as one of either spontaneous vaginal delivery (SVD), cesarean section, assisted breech, breech extraction, forceps, or vacuum extraction. Women whose records showed “other” as mode of delivery or whose notes contained conflicting modes of delivery were excluded.
Self-reported questionnaires asking about general health and lifestyle and including questions relating to sexual enjoyment and frequency were collected at 33 months and at 5, 12, and 18 years postpartum. Women were asked if they enjoyed sexual intercourse, with possible responses of:
- Yes, very much.
- Yes, somewhat.
- No, not a lot.
- No, not at all.
- No sex at the moment.
Possible sexual frequency responses were:
- Not at all.
- Less than once a month.
- 1-3 times a month.
- About once a week.
- 2-4 times a week.
- 5 or more times a week.
First study to look at sexual frequency
The team noted that theirs is the first study investigating the association of mode of delivery with sexual frequency. “Although it may be less important for well-being than sexual enjoyment or sex-related pain, it is an important measure to observe alongside other sexual outcomes,” they said.
Separately, sex-related pain, in the vagina during sex or elsewhere after sex, was assessed once, at 11 years post partum.
The data showed that women who had a cesarean section (11% of the sample) tended to be older than those who had vaginal delivery, with a higher mean body mass index (24.2 versus 22.8 kg/m2), and were more likely to be nulliparous at the time of the index pregnancy (54% versus 44%).
There was no significant difference between cesarean section and vaginal delivery in terms of responses for sexual enjoyment or frequency at any time after childbirth, the authors said. Nor, in adjusted models, was there evidence of associations between the type of vaginal delivery and sexual enjoyment or frequency outcomes.
Pain during sex increased more than a decade after cesarean
However, while the majority of respondents reported no intercourse-related pain, those who delivered via cesarean were more likely than those who gave birth vaginally to report sex-related pain at 11 years post partum. This was specifically an elevated incidence of pain in the vagina during sex, with an odds ratio of 1.74 (95% confidence interval, 1.46-2.08) in the adjusted model. This finding was consistent for emergency and elective cesarean section separately – both types were associated with increased dyspareunia, compared with vaginal delivery.
The dataset did not include measures of individual prenatal sex-related pain and, therefore, “it is unknown from this study whether Caesarean section causes sex-related pain, as suggested by the findings, or whether prenatal sex-related pain predicts both Caesarean section and postnatal sex-related pain,” the researchers said.
“Longitudinal data on sex-related pain need to be collected both before and after parturition,” they recommend, to clarify the direction of a possible effect between cesarean section and dyspareunia.
Cesarean does not protect against sexual dysfunction
Meanwhile, “For women considering a planned Caesarean section in an uncomplicated pregnancy, evidence suggesting that Caesarean section may not protect against sexual dysfunction may help inform their decision-making in the antenatal period.”
Lead author Flo Martin, a PhD student in epidemiology at the University of Bristol, said: “Rates of Caesarean section have been rising over the last 20 years due to many contributing factors and, importantly, it has been suggested that Caesarean section maintains sexual wellbeing compared with vaginal delivery. It is crucial that a whole range of maternal and foetal outcomes following Caesarean section are investigated, including sexual wellbeing, to appropriately inform decision-making both pre- and postnatally.
“This research provides expectant mothers, as well as women who have given birth, with really important information and demonstrates that there was no difference in sexual enjoyment or sexual frequency at any time point postpartum between women who gave birth via Caesarean section and those who delivered vaginally. It also suggests that Caesarean section may not help protect against sexual dysfunction, as previously thought, where sex-related pain was higher among women who gave birth via Caesarean section more than 10 years postpartum.”
Asked to comment on the research, Dr. Leila Frodsham, consultant gynecologist and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “Sexual pain disorders affect 7.5% of women of all ages, but there are peaks: during the start of sexual activity, if subfertility is an issue, after childbirth, and in the peri/menopause. It can be up to three times more prevalent at these peak times.
“Many women with sexual pain are worried when they consider starting a family and request a Caesarean birth to reduce risk of worsening their pain. However, this study has demonstrated that a Caesarean birth is associated with increased sexual pain longer term, which is very useful for helping women to plan their births.
“While more research about postpartum sexual wellbeing is needed, the findings of this study are reassuring to those who are pregnant as it found no difference in the enjoyment or frequency of sex in the years after a vaginal or a Caesarean birth.
“Most women in the U.K. recover well whether they have a vaginal or a Caesarean birth. Women should be supported to make informed decisions about how they plan to give birth, and it is vital that health care professionals respect their preferences.”
A version of this article first appeared on Medscape UK.
COVID-19 vaccine safe in patients with heart failure
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022