User login
Does Medicare Enrollment Raise Diabetes Medication Costs?
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Light During Nighttime Linked to Diabetes Risk
Concerned about your patient’s type 2 diabetes risk? Along with the usual preventive strategies — like diet and exercise and, when appropriate, glucagon-like peptide 1 (GLP-1) agonists — there’s another simple, no-risk strategy that just might help: Turning off the light at night.
A study in The Lancet found that people who were exposed to the most light between 12:30 a.m. and 6 a.m. were 1.5 times more likely to develop diabetes than those who remained in darkness during that time frame.
The study builds on growing evidence linking nighttime light exposure to type 2 diabetes risk. But unlike previous large studies that relied on satellite data of outdoor light levels (an indirect measure of light exposure), the recent study looked at personal light exposure — that is, light measured directly on individuals — as recorded by a wrist-worn sensor.
“Those previous studies likely underestimated the effect,” said study author Andrew Phillips, PhD, professor of sleep health at Flinders University in Adelaide, Australia, “since they did not capture indoor light environments.”
Using data from 85,000 participants from the UK Biobank, the recent study is the largest to date linking diabetes risk to personal light exposure at night.
“This is really a phenomenal study,” said Courtney Peterson, PhD, a scientist at the University of Alabama at Birmingham’s Diabetes Research Center, who was not involved in the study. “This is the first large-scale study we have looking at people’s light exposure patterns and linking it to their long-term health.”
What the Study Showed
The participants wore the light sensors for a week, recording day and night light from all sources — whether from sunlight, lamps, streetlights, or digital screens. The researchers then tracked participants for 8 years.
“About half of the people that we looked at had very dim levels of light at night, so less than 1 lux — that basically means less than candlelight,” said Dr. Phillips. “They were the people who were protected against type 2 diabetes.”
Participants in the top 10% of light exposure — who were exposed to about 48 lux , or the equivalent of relatively dim overhead lighting — were 1.5 times more likely to develop diabetes than those in the dark. That’s about the risk increase you’d get from having a family history of type 2 diabetes, the researchers said.
Even when they controlled for factors like socioeconomic status, smoking, diet, exercise, and shift work, “we still found there was this very strong relationship between light exposure and risk of type 2 diabetes,” said Dr. Phillips.
How Light at Night May Increase Diabetes Risk
The results are not entirely surprising, said endocrinologist Susanne Miedlich, MD, a professor at the University of Rochester Medical Center, Rochester, New York, who was not involved in the study.
Light at night can disrupt the circadian rhythm, or your body’s internal 24-hour cycle. And scientists have long known that circadian rhythm is important for all kinds of biologic processes, including how the body manages blood sugar.
One’s internal clock regulates food intake, sugar absorption, and the release of insulin. Dysregulation in the circadian rhythm is associated with insulin resistance, a precursor to type 2 diabetes.
Dr. Phillips speculated that the sleep hormone melatonin also plays a role.
“Melatonin does a lot of things, but one of the things that it does is it manages our glucose and our insulin responses,” Dr. Phillips said. “So if you’re chronically getting light exposure at night, that’s reducing a level of melatonin that, in the long term, could lead to poor metabolic outcomes.”
Previous studies have explored melatonin supplementation to help manage diabetes. “However, while melatonin clearly regulates circadian rhythms, its utility as a drug to prevent diabetes has not really panned out thus far,” Dr. Miedlich said.
Takeaways
Interventional studies are needed to confirm whether strategies like powering down screens, turning off lights, or using blackout curtains could reduce diabetes risk.
That said, “there’s no reason not to tell people to get healthy light exposure patterns and sleep, especially in the context of diabetes,” said Dr. Phillips.
Other known strategies for reducing diabetes risk include intensive lifestyle programs, which reduce risk by up to 58%, and GLP-1 agonists.
“Probably a GLP-1 agonist is going to be more effective,” Dr. Peterson said. “But this is still a fairly large effect without having to go through the expense of buying a GLP-1 or losing a lot of weight or making a big lifestyle change.”
A version of this article first appeared on Medscape.com.
Concerned about your patient’s type 2 diabetes risk? Along with the usual preventive strategies — like diet and exercise and, when appropriate, glucagon-like peptide 1 (GLP-1) agonists — there’s another simple, no-risk strategy that just might help: Turning off the light at night.
A study in The Lancet found that people who were exposed to the most light between 12:30 a.m. and 6 a.m. were 1.5 times more likely to develop diabetes than those who remained in darkness during that time frame.
The study builds on growing evidence linking nighttime light exposure to type 2 diabetes risk. But unlike previous large studies that relied on satellite data of outdoor light levels (an indirect measure of light exposure), the recent study looked at personal light exposure — that is, light measured directly on individuals — as recorded by a wrist-worn sensor.
“Those previous studies likely underestimated the effect,” said study author Andrew Phillips, PhD, professor of sleep health at Flinders University in Adelaide, Australia, “since they did not capture indoor light environments.”
Using data from 85,000 participants from the UK Biobank, the recent study is the largest to date linking diabetes risk to personal light exposure at night.
“This is really a phenomenal study,” said Courtney Peterson, PhD, a scientist at the University of Alabama at Birmingham’s Diabetes Research Center, who was not involved in the study. “This is the first large-scale study we have looking at people’s light exposure patterns and linking it to their long-term health.”
What the Study Showed
The participants wore the light sensors for a week, recording day and night light from all sources — whether from sunlight, lamps, streetlights, or digital screens. The researchers then tracked participants for 8 years.
“About half of the people that we looked at had very dim levels of light at night, so less than 1 lux — that basically means less than candlelight,” said Dr. Phillips. “They were the people who were protected against type 2 diabetes.”
Participants in the top 10% of light exposure — who were exposed to about 48 lux , or the equivalent of relatively dim overhead lighting — were 1.5 times more likely to develop diabetes than those in the dark. That’s about the risk increase you’d get from having a family history of type 2 diabetes, the researchers said.
Even when they controlled for factors like socioeconomic status, smoking, diet, exercise, and shift work, “we still found there was this very strong relationship between light exposure and risk of type 2 diabetes,” said Dr. Phillips.
How Light at Night May Increase Diabetes Risk
The results are not entirely surprising, said endocrinologist Susanne Miedlich, MD, a professor at the University of Rochester Medical Center, Rochester, New York, who was not involved in the study.
Light at night can disrupt the circadian rhythm, or your body’s internal 24-hour cycle. And scientists have long known that circadian rhythm is important for all kinds of biologic processes, including how the body manages blood sugar.
One’s internal clock regulates food intake, sugar absorption, and the release of insulin. Dysregulation in the circadian rhythm is associated with insulin resistance, a precursor to type 2 diabetes.
Dr. Phillips speculated that the sleep hormone melatonin also plays a role.
“Melatonin does a lot of things, but one of the things that it does is it manages our glucose and our insulin responses,” Dr. Phillips said. “So if you’re chronically getting light exposure at night, that’s reducing a level of melatonin that, in the long term, could lead to poor metabolic outcomes.”
Previous studies have explored melatonin supplementation to help manage diabetes. “However, while melatonin clearly regulates circadian rhythms, its utility as a drug to prevent diabetes has not really panned out thus far,” Dr. Miedlich said.
Takeaways
Interventional studies are needed to confirm whether strategies like powering down screens, turning off lights, or using blackout curtains could reduce diabetes risk.
That said, “there’s no reason not to tell people to get healthy light exposure patterns and sleep, especially in the context of diabetes,” said Dr. Phillips.
Other known strategies for reducing diabetes risk include intensive lifestyle programs, which reduce risk by up to 58%, and GLP-1 agonists.
“Probably a GLP-1 agonist is going to be more effective,” Dr. Peterson said. “But this is still a fairly large effect without having to go through the expense of buying a GLP-1 or losing a lot of weight or making a big lifestyle change.”
A version of this article first appeared on Medscape.com.
Concerned about your patient’s type 2 diabetes risk? Along with the usual preventive strategies — like diet and exercise and, when appropriate, glucagon-like peptide 1 (GLP-1) agonists — there’s another simple, no-risk strategy that just might help: Turning off the light at night.
A study in The Lancet found that people who were exposed to the most light between 12:30 a.m. and 6 a.m. were 1.5 times more likely to develop diabetes than those who remained in darkness during that time frame.
The study builds on growing evidence linking nighttime light exposure to type 2 diabetes risk. But unlike previous large studies that relied on satellite data of outdoor light levels (an indirect measure of light exposure), the recent study looked at personal light exposure — that is, light measured directly on individuals — as recorded by a wrist-worn sensor.
“Those previous studies likely underestimated the effect,” said study author Andrew Phillips, PhD, professor of sleep health at Flinders University in Adelaide, Australia, “since they did not capture indoor light environments.”
Using data from 85,000 participants from the UK Biobank, the recent study is the largest to date linking diabetes risk to personal light exposure at night.
“This is really a phenomenal study,” said Courtney Peterson, PhD, a scientist at the University of Alabama at Birmingham’s Diabetes Research Center, who was not involved in the study. “This is the first large-scale study we have looking at people’s light exposure patterns and linking it to their long-term health.”
What the Study Showed
The participants wore the light sensors for a week, recording day and night light from all sources — whether from sunlight, lamps, streetlights, or digital screens. The researchers then tracked participants for 8 years.
“About half of the people that we looked at had very dim levels of light at night, so less than 1 lux — that basically means less than candlelight,” said Dr. Phillips. “They were the people who were protected against type 2 diabetes.”
Participants in the top 10% of light exposure — who were exposed to about 48 lux , or the equivalent of relatively dim overhead lighting — were 1.5 times more likely to develop diabetes than those in the dark. That’s about the risk increase you’d get from having a family history of type 2 diabetes, the researchers said.
Even when they controlled for factors like socioeconomic status, smoking, diet, exercise, and shift work, “we still found there was this very strong relationship between light exposure and risk of type 2 diabetes,” said Dr. Phillips.
How Light at Night May Increase Diabetes Risk
The results are not entirely surprising, said endocrinologist Susanne Miedlich, MD, a professor at the University of Rochester Medical Center, Rochester, New York, who was not involved in the study.
Light at night can disrupt the circadian rhythm, or your body’s internal 24-hour cycle. And scientists have long known that circadian rhythm is important for all kinds of biologic processes, including how the body manages blood sugar.
One’s internal clock regulates food intake, sugar absorption, and the release of insulin. Dysregulation in the circadian rhythm is associated with insulin resistance, a precursor to type 2 diabetes.
Dr. Phillips speculated that the sleep hormone melatonin also plays a role.
“Melatonin does a lot of things, but one of the things that it does is it manages our glucose and our insulin responses,” Dr. Phillips said. “So if you’re chronically getting light exposure at night, that’s reducing a level of melatonin that, in the long term, could lead to poor metabolic outcomes.”
Previous studies have explored melatonin supplementation to help manage diabetes. “However, while melatonin clearly regulates circadian rhythms, its utility as a drug to prevent diabetes has not really panned out thus far,” Dr. Miedlich said.
Takeaways
Interventional studies are needed to confirm whether strategies like powering down screens, turning off lights, or using blackout curtains could reduce diabetes risk.
That said, “there’s no reason not to tell people to get healthy light exposure patterns and sleep, especially in the context of diabetes,” said Dr. Phillips.
Other known strategies for reducing diabetes risk include intensive lifestyle programs, which reduce risk by up to 58%, and GLP-1 agonists.
“Probably a GLP-1 agonist is going to be more effective,” Dr. Peterson said. “But this is still a fairly large effect without having to go through the expense of buying a GLP-1 or losing a lot of weight or making a big lifestyle change.”
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Whether GLP-1 RAs Significantly Delay Gastric Emptying Called into Question
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Semaglutide May Increase Risk of Disease Causing Vision Loss
TOPLINE:
Patients with type 2 diabetes, overweight, or obesity taking the glucagon-like peptide receptor agonist (GLP-1 RA) semaglutide appear to have an increased risk for an uncommon condition that can cause vision loss.
METHODOLOGY:
- Researchers conducted a retrospective study of 16,827 patients at Massachusetts Eye and Ear in Boston.
- Their analysis focused on 710 patients with type 2 diabetes (194 of whom had been prescribed semaglutide) and 979 patients with overweight or obesity (361 prescribed semaglutide).
- The researchers compared patients prescribed semaglutide with those prescribed a medication other than a GLP-1 agent. They matched patients by factors such as age and sex and whether they had hypertension, obstructive sleep apnea, or coronary artery disease.
- They assessed the cumulative incidence of nonarteritic anterior ischemic optic neuropathy (NAION) during 36 months of follow-up.
TAKEAWAY:
- Semaglutide use was associated with a higher risk for NAION in patients with type 2 diabetes (hazard ratio [HR], 4.28; 95% CI, 1.62-11.29).
- In patients with overweight or obesity, semaglutide again was linked to a higher risk for NAION (HR, 7.64; 95% CI, 2.21-26.36).
- Among patients with type 2 diabetes, the cumulative incidence of NAION over 36 months was 8.9% for those prescribed semaglutide vs 1.8% among those taking non–GLP-1 medications.
IN PRACTICE:
Semaglutide has “provided very significant benefits in many ways, but future discussions between a patient and their physician should include NAION as a potential risk,” study leader Joseph Rizzo, MD, with Mass Eye and Ear and Harvard Medical School, said in a news release about the findings. “It is important to appreciate, however, that the increased risk relates to a disorder that is relatively uncommon.”
“Given the numbers of participants who have been recruited to clinical trials and the large number of people globally who use GLP-1 RAs, we should be confident that if corroborated, the absolute risk of developing NAION in direct relation to taking semaglutide must indeed be rare,” Susan P. Mollan, MBcHB, of University Hospitals Birmingham NHS Foundation Trust, in England, wrote in a commentary published with the study.
SOURCE:
The study was published online on July 3 in JAMA Ophthalmology.
LIMITATIONS:
The patients were seen at a hospital that specializes in ophthalmology and has a specialized neuro-ophthalmology service, so the results may not fully apply to other settings. The results were driven by a relatively small number of NAION cases in the patients exposed to semaglutide. The study does not establish that semaglutide directly causes NAION, the researchers noted. “The best approaches to confirm, refute, or refine our findings would be to conduct a much larger, retrospective, multicenter population-based cohort study; a prospective, randomized clinical study; or a postmarket analysis of all GLP-1 RA drugs,” they wrote.
DISCLOSURES:
The study was supported by a grant from Research to Prevent Blindness.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Patients with type 2 diabetes, overweight, or obesity taking the glucagon-like peptide receptor agonist (GLP-1 RA) semaglutide appear to have an increased risk for an uncommon condition that can cause vision loss.
METHODOLOGY:
- Researchers conducted a retrospective study of 16,827 patients at Massachusetts Eye and Ear in Boston.
- Their analysis focused on 710 patients with type 2 diabetes (194 of whom had been prescribed semaglutide) and 979 patients with overweight or obesity (361 prescribed semaglutide).
- The researchers compared patients prescribed semaglutide with those prescribed a medication other than a GLP-1 agent. They matched patients by factors such as age and sex and whether they had hypertension, obstructive sleep apnea, or coronary artery disease.
- They assessed the cumulative incidence of nonarteritic anterior ischemic optic neuropathy (NAION) during 36 months of follow-up.
TAKEAWAY:
- Semaglutide use was associated with a higher risk for NAION in patients with type 2 diabetes (hazard ratio [HR], 4.28; 95% CI, 1.62-11.29).
- In patients with overweight or obesity, semaglutide again was linked to a higher risk for NAION (HR, 7.64; 95% CI, 2.21-26.36).
- Among patients with type 2 diabetes, the cumulative incidence of NAION over 36 months was 8.9% for those prescribed semaglutide vs 1.8% among those taking non–GLP-1 medications.
IN PRACTICE:
Semaglutide has “provided very significant benefits in many ways, but future discussions between a patient and their physician should include NAION as a potential risk,” study leader Joseph Rizzo, MD, with Mass Eye and Ear and Harvard Medical School, said in a news release about the findings. “It is important to appreciate, however, that the increased risk relates to a disorder that is relatively uncommon.”
“Given the numbers of participants who have been recruited to clinical trials and the large number of people globally who use GLP-1 RAs, we should be confident that if corroborated, the absolute risk of developing NAION in direct relation to taking semaglutide must indeed be rare,” Susan P. Mollan, MBcHB, of University Hospitals Birmingham NHS Foundation Trust, in England, wrote in a commentary published with the study.
SOURCE:
The study was published online on July 3 in JAMA Ophthalmology.
LIMITATIONS:
The patients were seen at a hospital that specializes in ophthalmology and has a specialized neuro-ophthalmology service, so the results may not fully apply to other settings. The results were driven by a relatively small number of NAION cases in the patients exposed to semaglutide. The study does not establish that semaglutide directly causes NAION, the researchers noted. “The best approaches to confirm, refute, or refine our findings would be to conduct a much larger, retrospective, multicenter population-based cohort study; a prospective, randomized clinical study; or a postmarket analysis of all GLP-1 RA drugs,” they wrote.
DISCLOSURES:
The study was supported by a grant from Research to Prevent Blindness.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Patients with type 2 diabetes, overweight, or obesity taking the glucagon-like peptide receptor agonist (GLP-1 RA) semaglutide appear to have an increased risk for an uncommon condition that can cause vision loss.
METHODOLOGY:
- Researchers conducted a retrospective study of 16,827 patients at Massachusetts Eye and Ear in Boston.
- Their analysis focused on 710 patients with type 2 diabetes (194 of whom had been prescribed semaglutide) and 979 patients with overweight or obesity (361 prescribed semaglutide).
- The researchers compared patients prescribed semaglutide with those prescribed a medication other than a GLP-1 agent. They matched patients by factors such as age and sex and whether they had hypertension, obstructive sleep apnea, or coronary artery disease.
- They assessed the cumulative incidence of nonarteritic anterior ischemic optic neuropathy (NAION) during 36 months of follow-up.
TAKEAWAY:
- Semaglutide use was associated with a higher risk for NAION in patients with type 2 diabetes (hazard ratio [HR], 4.28; 95% CI, 1.62-11.29).
- In patients with overweight or obesity, semaglutide again was linked to a higher risk for NAION (HR, 7.64; 95% CI, 2.21-26.36).
- Among patients with type 2 diabetes, the cumulative incidence of NAION over 36 months was 8.9% for those prescribed semaglutide vs 1.8% among those taking non–GLP-1 medications.
IN PRACTICE:
Semaglutide has “provided very significant benefits in many ways, but future discussions between a patient and their physician should include NAION as a potential risk,” study leader Joseph Rizzo, MD, with Mass Eye and Ear and Harvard Medical School, said in a news release about the findings. “It is important to appreciate, however, that the increased risk relates to a disorder that is relatively uncommon.”
“Given the numbers of participants who have been recruited to clinical trials and the large number of people globally who use GLP-1 RAs, we should be confident that if corroborated, the absolute risk of developing NAION in direct relation to taking semaglutide must indeed be rare,” Susan P. Mollan, MBcHB, of University Hospitals Birmingham NHS Foundation Trust, in England, wrote in a commentary published with the study.
SOURCE:
The study was published online on July 3 in JAMA Ophthalmology.
LIMITATIONS:
The patients were seen at a hospital that specializes in ophthalmology and has a specialized neuro-ophthalmology service, so the results may not fully apply to other settings. The results were driven by a relatively small number of NAION cases in the patients exposed to semaglutide. The study does not establish that semaglutide directly causes NAION, the researchers noted. “The best approaches to confirm, refute, or refine our findings would be to conduct a much larger, retrospective, multicenter population-based cohort study; a prospective, randomized clinical study; or a postmarket analysis of all GLP-1 RA drugs,” they wrote.
DISCLOSURES:
The study was supported by a grant from Research to Prevent Blindness.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Weight Loss Drugs Cut Cancer Risk in Diabetes Patients
Recent research on popular weight loss drugs has uncovered surprising benefits beyond their intended use, like lowering the risk of fatal heart attacks. And now there may be another unforeseen advantage:
That’s according to a study published July 5 in JAMA Network Open where researchers studied glucagon-like peptide receptor agonists (known as GLP-1RAs), a class of drugs used to treat diabetes and obesity. Ozempic, Wegovy, Mounjaro, and Zepbound, which have become well-known recently because they are linked to rapid weight loss, contain GLP-1RAs.
For the study, they looked at electronic health records of 1.7 million patients who had type 2 diabetes, no prior diagnosis of obesity-related cancers, and had been prescribed GLP-1RAs, insulins, or metformin from March 2005 to November 2018.
The scientists found that compared to patients who took insulin, people who took GLP-1RAs had a “significant risk reduction” in 10 of 13 obesity-related cancers. Those 10 cancers were esophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancers, as well as meningioma and multiple myeloma.
Compared with patients taking insulin, patients taking GLP-1RAs showed no statistically significant reduction in stomach cancer and no reduced risk of breast and thyroid cancers, the study said.
But the study found no decrease in cancer risk with GLP-1RAs compared with metformin.
While the study results suggest that these drugs may reduce the risk of certain obesity-related cancers better than insulins, more research is needed, they said.
A version of this article appeared on WebMD.com.
Recent research on popular weight loss drugs has uncovered surprising benefits beyond their intended use, like lowering the risk of fatal heart attacks. And now there may be another unforeseen advantage:
That’s according to a study published July 5 in JAMA Network Open where researchers studied glucagon-like peptide receptor agonists (known as GLP-1RAs), a class of drugs used to treat diabetes and obesity. Ozempic, Wegovy, Mounjaro, and Zepbound, which have become well-known recently because they are linked to rapid weight loss, contain GLP-1RAs.
For the study, they looked at electronic health records of 1.7 million patients who had type 2 diabetes, no prior diagnosis of obesity-related cancers, and had been prescribed GLP-1RAs, insulins, or metformin from March 2005 to November 2018.
The scientists found that compared to patients who took insulin, people who took GLP-1RAs had a “significant risk reduction” in 10 of 13 obesity-related cancers. Those 10 cancers were esophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancers, as well as meningioma and multiple myeloma.
Compared with patients taking insulin, patients taking GLP-1RAs showed no statistically significant reduction in stomach cancer and no reduced risk of breast and thyroid cancers, the study said.
But the study found no decrease in cancer risk with GLP-1RAs compared with metformin.
While the study results suggest that these drugs may reduce the risk of certain obesity-related cancers better than insulins, more research is needed, they said.
A version of this article appeared on WebMD.com.
Recent research on popular weight loss drugs has uncovered surprising benefits beyond their intended use, like lowering the risk of fatal heart attacks. And now there may be another unforeseen advantage:
That’s according to a study published July 5 in JAMA Network Open where researchers studied glucagon-like peptide receptor agonists (known as GLP-1RAs), a class of drugs used to treat diabetes and obesity. Ozempic, Wegovy, Mounjaro, and Zepbound, which have become well-known recently because they are linked to rapid weight loss, contain GLP-1RAs.
For the study, they looked at electronic health records of 1.7 million patients who had type 2 diabetes, no prior diagnosis of obesity-related cancers, and had been prescribed GLP-1RAs, insulins, or metformin from March 2005 to November 2018.
The scientists found that compared to patients who took insulin, people who took GLP-1RAs had a “significant risk reduction” in 10 of 13 obesity-related cancers. Those 10 cancers were esophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancers, as well as meningioma and multiple myeloma.
Compared with patients taking insulin, patients taking GLP-1RAs showed no statistically significant reduction in stomach cancer and no reduced risk of breast and thyroid cancers, the study said.
But the study found no decrease in cancer risk with GLP-1RAs compared with metformin.
While the study results suggest that these drugs may reduce the risk of certain obesity-related cancers better than insulins, more research is needed, they said.
A version of this article appeared on WebMD.com.
Can Cannabis Help to Reduce Diabetes Risk?
ORLANDO, FLORIDA — , ongoing research suggests.
In the findings from the SONIC trial, Angela Bryan, PhD, professor and codirector of CUChange at the University of Colorado, Boulder, and colleagues hypothesized that “those inflammatory profiles would improve over the course of 4 weeks, particularly for those using a CBD [cannabidiol] as opposed to a THC [tetrahydrocannabinol] product.”
She presented the findings at the American Diabetes Association (ADA) 84th Scientific Sessions.
Other recent work by Dr. Bryan and her colleagues focused on the public health implications of cannabis legalization. One study examined the acute effects of legal-market cannabis on regular users’ subjective responses while running and found that cannabis use prior to exercise may lead to more enjoyment and runner’s high symptoms, although it also led to feelings of greater exertion. The positive effects could make exercise more appealing to individuals — including those with or at risk for diabetes — who might not otherwise engage in it, Bryan suggested.
Another study found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
‘Complicated’ Connection to Diabetes
In the SONIC study, participants who were regular cannabis users had an average age of 30 years and had body mass index (BMI) in the healthy range; 86% were White individuals, and 59% were men. They were matched with a similar group of individuals who had not used cannabis for at least a year. At baseline, participants’ NSDR Healthy Eating Index score overall was 51.24, showing a “need for improvement/poor diet.”
“Folks were maybe not killing it in the dietary domain,” Dr. Bryan acknowledged. “However, they were absolutely killing it in the physical activity domain.”
The researchers did oral glucose tolerance tests to calculate participants’ Matsuda index of insulin sensitivity and measured inflammatory markers, including tumor necrosis factor alpha, interleukin 6 (IL6), IL1 beta, IL12, interferon gamma, IL4, and monocyte chemoattractant protein 1 (MCP-1). In a “randomized encouragement” design, users were assigned to purchase and use a flower product for 4 weeks, however much they wanted. They completed daily assessments of their cannabis use, alcohol use, diet, and physical activity.
Between-group eating patterns were similar over the 4 weeks, with cannabis users reporting “marginally” more servings of salty snacks and food relative to nonusers. None of the daily associations were moderated by which cannabis product was used.
At 4 weeks, the team repeated the tests and, surprisingly, found no change in participants’ inflammatory markers. But what “popped out,” she said, was the “stark difference” between users and nonusers, with users having significantly lower levels of inflammatory biomarkers, circulating cytokines than the nonusers.
An exception were levels of MCP-1, which increased over time in the users but didn’t change in nonusers. Bryan said the finding is “perplexing” and asked the audience for thoughts, especially given that MCP-1 levels are positively associated with diabetes.
After controlling for BMI and inflammation, “we saw absolutely no effects of group or group by time interaction on the Matsuda index of insulin sensitivity,” she said. “Seemingly, there are no chronic effects of cannabis use on insulin sensitivity.”
Regarding limitations, Dr. Bryan acknowledged that the study is being conducted with “a very healthy sample of individuals who exercise a lot, and that might be factoring into our results, especially on insulin sensitivity.” The team could not use “gold standard” randomization because of the schedule-1 status of CannaVan cannabis, and the MCP-1 findings are difficult to interpret.
Furthermore, she noted, “our day-to-day level data show only slight differences in behavior between those who use cannabis and those who don’t and also very slight differences between users’ behavior on days that they use vs days that they don’t.
“I think all of this put together shows us that the relationship between cannabis use and potential implications for diabetes is a lot more complicated than just couch to couchlock [very deep relaxation/sedation] or runner’s high,” she said.
Bring On the CannaVan
The team’s next step, currently underway, is to get an acute response to cannabis with an oral glucose tolerance test that’s done immediately after the participant uses a product. Since cannabis is a schedule-1 drug, it can’t be taken into the laboratory. Therefore, the researchers are using a CannaVan — a mobile lab. “We drive it to their homes, they come out, we draw blood, and we send them back into their homes to use as much of their product as they want,” Bryan explained. “They come back out to the van. They do all the follow-up assessments. We take blood again to verify their exposure. And that’s how we collect those data.”
“Invite me back next year, and I will tell you what we found,” she quipped.
Dr. Bryan had no disclosures to report.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — , ongoing research suggests.
In the findings from the SONIC trial, Angela Bryan, PhD, professor and codirector of CUChange at the University of Colorado, Boulder, and colleagues hypothesized that “those inflammatory profiles would improve over the course of 4 weeks, particularly for those using a CBD [cannabidiol] as opposed to a THC [tetrahydrocannabinol] product.”
She presented the findings at the American Diabetes Association (ADA) 84th Scientific Sessions.
Other recent work by Dr. Bryan and her colleagues focused on the public health implications of cannabis legalization. One study examined the acute effects of legal-market cannabis on regular users’ subjective responses while running and found that cannabis use prior to exercise may lead to more enjoyment and runner’s high symptoms, although it also led to feelings of greater exertion. The positive effects could make exercise more appealing to individuals — including those with or at risk for diabetes — who might not otherwise engage in it, Bryan suggested.
Another study found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
‘Complicated’ Connection to Diabetes
In the SONIC study, participants who were regular cannabis users had an average age of 30 years and had body mass index (BMI) in the healthy range; 86% were White individuals, and 59% were men. They were matched with a similar group of individuals who had not used cannabis for at least a year. At baseline, participants’ NSDR Healthy Eating Index score overall was 51.24, showing a “need for improvement/poor diet.”
“Folks were maybe not killing it in the dietary domain,” Dr. Bryan acknowledged. “However, they were absolutely killing it in the physical activity domain.”
The researchers did oral glucose tolerance tests to calculate participants’ Matsuda index of insulin sensitivity and measured inflammatory markers, including tumor necrosis factor alpha, interleukin 6 (IL6), IL1 beta, IL12, interferon gamma, IL4, and monocyte chemoattractant protein 1 (MCP-1). In a “randomized encouragement” design, users were assigned to purchase and use a flower product for 4 weeks, however much they wanted. They completed daily assessments of their cannabis use, alcohol use, diet, and physical activity.
Between-group eating patterns were similar over the 4 weeks, with cannabis users reporting “marginally” more servings of salty snacks and food relative to nonusers. None of the daily associations were moderated by which cannabis product was used.
At 4 weeks, the team repeated the tests and, surprisingly, found no change in participants’ inflammatory markers. But what “popped out,” she said, was the “stark difference” between users and nonusers, with users having significantly lower levels of inflammatory biomarkers, circulating cytokines than the nonusers.
An exception were levels of MCP-1, which increased over time in the users but didn’t change in nonusers. Bryan said the finding is “perplexing” and asked the audience for thoughts, especially given that MCP-1 levels are positively associated with diabetes.
After controlling for BMI and inflammation, “we saw absolutely no effects of group or group by time interaction on the Matsuda index of insulin sensitivity,” she said. “Seemingly, there are no chronic effects of cannabis use on insulin sensitivity.”
Regarding limitations, Dr. Bryan acknowledged that the study is being conducted with “a very healthy sample of individuals who exercise a lot, and that might be factoring into our results, especially on insulin sensitivity.” The team could not use “gold standard” randomization because of the schedule-1 status of CannaVan cannabis, and the MCP-1 findings are difficult to interpret.
Furthermore, she noted, “our day-to-day level data show only slight differences in behavior between those who use cannabis and those who don’t and also very slight differences between users’ behavior on days that they use vs days that they don’t.
“I think all of this put together shows us that the relationship between cannabis use and potential implications for diabetes is a lot more complicated than just couch to couchlock [very deep relaxation/sedation] or runner’s high,” she said.
Bring On the CannaVan
The team’s next step, currently underway, is to get an acute response to cannabis with an oral glucose tolerance test that’s done immediately after the participant uses a product. Since cannabis is a schedule-1 drug, it can’t be taken into the laboratory. Therefore, the researchers are using a CannaVan — a mobile lab. “We drive it to their homes, they come out, we draw blood, and we send them back into their homes to use as much of their product as they want,” Bryan explained. “They come back out to the van. They do all the follow-up assessments. We take blood again to verify their exposure. And that’s how we collect those data.”
“Invite me back next year, and I will tell you what we found,” she quipped.
Dr. Bryan had no disclosures to report.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — , ongoing research suggests.
In the findings from the SONIC trial, Angela Bryan, PhD, professor and codirector of CUChange at the University of Colorado, Boulder, and colleagues hypothesized that “those inflammatory profiles would improve over the course of 4 weeks, particularly for those using a CBD [cannabidiol] as opposed to a THC [tetrahydrocannabinol] product.”
She presented the findings at the American Diabetes Association (ADA) 84th Scientific Sessions.
Other recent work by Dr. Bryan and her colleagues focused on the public health implications of cannabis legalization. One study examined the acute effects of legal-market cannabis on regular users’ subjective responses while running and found that cannabis use prior to exercise may lead to more enjoyment and runner’s high symptoms, although it also led to feelings of greater exertion. The positive effects could make exercise more appealing to individuals — including those with or at risk for diabetes — who might not otherwise engage in it, Bryan suggested.
Another study found that CBD-dominant forms of cannabis were associated with acute tension reduction, which might lead to longer-term reductions in anxiety. Bryan said the findings could be relevant in the context of diabetes distress.
‘Complicated’ Connection to Diabetes
In the SONIC study, participants who were regular cannabis users had an average age of 30 years and had body mass index (BMI) in the healthy range; 86% were White individuals, and 59% were men. They were matched with a similar group of individuals who had not used cannabis for at least a year. At baseline, participants’ NSDR Healthy Eating Index score overall was 51.24, showing a “need for improvement/poor diet.”
“Folks were maybe not killing it in the dietary domain,” Dr. Bryan acknowledged. “However, they were absolutely killing it in the physical activity domain.”
The researchers did oral glucose tolerance tests to calculate participants’ Matsuda index of insulin sensitivity and measured inflammatory markers, including tumor necrosis factor alpha, interleukin 6 (IL6), IL1 beta, IL12, interferon gamma, IL4, and monocyte chemoattractant protein 1 (MCP-1). In a “randomized encouragement” design, users were assigned to purchase and use a flower product for 4 weeks, however much they wanted. They completed daily assessments of their cannabis use, alcohol use, diet, and physical activity.
Between-group eating patterns were similar over the 4 weeks, with cannabis users reporting “marginally” more servings of salty snacks and food relative to nonusers. None of the daily associations were moderated by which cannabis product was used.
At 4 weeks, the team repeated the tests and, surprisingly, found no change in participants’ inflammatory markers. But what “popped out,” she said, was the “stark difference” between users and nonusers, with users having significantly lower levels of inflammatory biomarkers, circulating cytokines than the nonusers.
An exception were levels of MCP-1, which increased over time in the users but didn’t change in nonusers. Bryan said the finding is “perplexing” and asked the audience for thoughts, especially given that MCP-1 levels are positively associated with diabetes.
After controlling for BMI and inflammation, “we saw absolutely no effects of group or group by time interaction on the Matsuda index of insulin sensitivity,” she said. “Seemingly, there are no chronic effects of cannabis use on insulin sensitivity.”
Regarding limitations, Dr. Bryan acknowledged that the study is being conducted with “a very healthy sample of individuals who exercise a lot, and that might be factoring into our results, especially on insulin sensitivity.” The team could not use “gold standard” randomization because of the schedule-1 status of CannaVan cannabis, and the MCP-1 findings are difficult to interpret.
Furthermore, she noted, “our day-to-day level data show only slight differences in behavior between those who use cannabis and those who don’t and also very slight differences between users’ behavior on days that they use vs days that they don’t.
“I think all of this put together shows us that the relationship between cannabis use and potential implications for diabetes is a lot more complicated than just couch to couchlock [very deep relaxation/sedation] or runner’s high,” she said.
Bring On the CannaVan
The team’s next step, currently underway, is to get an acute response to cannabis with an oral glucose tolerance test that’s done immediately after the participant uses a product. Since cannabis is a schedule-1 drug, it can’t be taken into the laboratory. Therefore, the researchers are using a CannaVan — a mobile lab. “We drive it to their homes, they come out, we draw blood, and we send them back into their homes to use as much of their product as they want,” Bryan explained. “They come back out to the van. They do all the follow-up assessments. We take blood again to verify their exposure. And that’s how we collect those data.”
“Invite me back next year, and I will tell you what we found,” she quipped.
Dr. Bryan had no disclosures to report.
A version of this article first appeared on Medscape.com.
FROM ADA 2024
Can Response to Semaglutide Be Predicted With a Genetic Test?
ORLANDO, FLORIDA — An analysis of data from 137 patients suggested testing whether people have a trait known as abnormal postprandial satiety (APS), or hungry gut, can predict how well they may respond to the obesity drug semaglutide, although it failed to establish this link for the somewhat similar tirzepatide.
At the American Diabetes Association (ADA) Scientific Sessions, Maria Daniela Hurtado Andrade, MD, PhD, of the Mayo Clinic, Jacksonville, Florida, presented results of a study using the MyPhenome Hungry Gut test, which was developed through machine learning, a form of artificial intelligence.
The test is part of the MyPhenome obesity phenotyping portfolio from Phenomix Sciences, a company founded by Mayo Clinic physicians, scientists, and researchers Andres Acosta, MD, PhD, and Michael Camilleri, MD, DSc.
At the ADA meeting, Dr. Hurtado Andrade discussed a test of 137 adults: 91 were considered to have a positive biomarker for abnormal postprandial satiety (APS+), and 46 who did not have it were classified as APS−. These were patients of the Mayo Clinic who were already taking obesity drugs and agreed to phenotyping. Of this group, 113 were on semaglutide and 24 on tirzepatide.
, with a mean 19.4% body weight loss in the APS+ group and a mean loss of 22.1% in the APS− group.
Further studies are warranted to assess the clinical utility of these biomarkers, Dr. Hurtado Andrade said. But these findings do support “the use of precision medicine for obesity based on an individual’s genetic background,” she said.
Dr. Hurtado Andrade’s presentation impressed fellow researchers who noted it as an early step toward the long-sought goal of more personalized medicine.
Daniel S. Hsia, MD, of Emory University, Atlanta, who led the ADA session at which Dr. Hurtado Andrade presented, said it was good to see new information being presented about using genetic risk scoring in obesity.
“The numbers were very small for the tirzepatide group as compared to the semaglutide group, so it’s a little hard to really come to any significant conclusions,” Dr. Hsia said in an interview.
At the ADA meeting, Ajay D. Rao, MD, MMSc, of Temple University, Philadelphia, said clinicians are excited about the idea of having biomarkers to aid in decisions about approaches to obesity.
In a follow-up interview with this news organization, Dr. Rao said he too is looking to see more testing of this approach to care, while describing Hurtado Andrade’s work as a “very well-done study.”
“We still need to see more large-scale studies of responsiveness to certain interventions,” he said.
Dr. Hurtado Andrade noted that researchers at academic centers such as Mayo can try to hone in the combination of genetic and other factors that led to obesity, such as emotional eating patterns and abnormal postprandial satiety.
But this approach is not widely scalable, as it demands resources of time and staffing that not all clinicians and patients enjoy.
“To overcome this challenge, our team has been working on developing biomarkers” such as the machine-learning gene risk score used to predict abnormal postprandial satiety, she said.
Findings for a related project were presented in May at Digestive Disease Week, as this news organization reported earlier. In that study, researchers calculated the genetic risk score for 84 adults undergoing weight loss interventions at Mayo Clinic who were prescribed the glucagon-like peptide 1 receptor agonist semaglutide.
This news organization separately asked Phenomix about the sales of MyPhenome Test kits. These cost $499, and about 500 tests have been sold since commercialization started last year, a spokesperson said.
The study was funded by Phenomix Sciences. Separately, Dr. Hurtado Andrade has worked as a consultant for Novo Nordisk and received research support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — An analysis of data from 137 patients suggested testing whether people have a trait known as abnormal postprandial satiety (APS), or hungry gut, can predict how well they may respond to the obesity drug semaglutide, although it failed to establish this link for the somewhat similar tirzepatide.
At the American Diabetes Association (ADA) Scientific Sessions, Maria Daniela Hurtado Andrade, MD, PhD, of the Mayo Clinic, Jacksonville, Florida, presented results of a study using the MyPhenome Hungry Gut test, which was developed through machine learning, a form of artificial intelligence.
The test is part of the MyPhenome obesity phenotyping portfolio from Phenomix Sciences, a company founded by Mayo Clinic physicians, scientists, and researchers Andres Acosta, MD, PhD, and Michael Camilleri, MD, DSc.
At the ADA meeting, Dr. Hurtado Andrade discussed a test of 137 adults: 91 were considered to have a positive biomarker for abnormal postprandial satiety (APS+), and 46 who did not have it were classified as APS−. These were patients of the Mayo Clinic who were already taking obesity drugs and agreed to phenotyping. Of this group, 113 were on semaglutide and 24 on tirzepatide.
, with a mean 19.4% body weight loss in the APS+ group and a mean loss of 22.1% in the APS− group.
Further studies are warranted to assess the clinical utility of these biomarkers, Dr. Hurtado Andrade said. But these findings do support “the use of precision medicine for obesity based on an individual’s genetic background,” she said.
Dr. Hurtado Andrade’s presentation impressed fellow researchers who noted it as an early step toward the long-sought goal of more personalized medicine.
Daniel S. Hsia, MD, of Emory University, Atlanta, who led the ADA session at which Dr. Hurtado Andrade presented, said it was good to see new information being presented about using genetic risk scoring in obesity.
“The numbers were very small for the tirzepatide group as compared to the semaglutide group, so it’s a little hard to really come to any significant conclusions,” Dr. Hsia said in an interview.
At the ADA meeting, Ajay D. Rao, MD, MMSc, of Temple University, Philadelphia, said clinicians are excited about the idea of having biomarkers to aid in decisions about approaches to obesity.
In a follow-up interview with this news organization, Dr. Rao said he too is looking to see more testing of this approach to care, while describing Hurtado Andrade’s work as a “very well-done study.”
“We still need to see more large-scale studies of responsiveness to certain interventions,” he said.
Dr. Hurtado Andrade noted that researchers at academic centers such as Mayo can try to hone in the combination of genetic and other factors that led to obesity, such as emotional eating patterns and abnormal postprandial satiety.
But this approach is not widely scalable, as it demands resources of time and staffing that not all clinicians and patients enjoy.
“To overcome this challenge, our team has been working on developing biomarkers” such as the machine-learning gene risk score used to predict abnormal postprandial satiety, she said.
Findings for a related project were presented in May at Digestive Disease Week, as this news organization reported earlier. In that study, researchers calculated the genetic risk score for 84 adults undergoing weight loss interventions at Mayo Clinic who were prescribed the glucagon-like peptide 1 receptor agonist semaglutide.
This news organization separately asked Phenomix about the sales of MyPhenome Test kits. These cost $499, and about 500 tests have been sold since commercialization started last year, a spokesperson said.
The study was funded by Phenomix Sciences. Separately, Dr. Hurtado Andrade has worked as a consultant for Novo Nordisk and received research support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — An analysis of data from 137 patients suggested testing whether people have a trait known as abnormal postprandial satiety (APS), or hungry gut, can predict how well they may respond to the obesity drug semaglutide, although it failed to establish this link for the somewhat similar tirzepatide.
At the American Diabetes Association (ADA) Scientific Sessions, Maria Daniela Hurtado Andrade, MD, PhD, of the Mayo Clinic, Jacksonville, Florida, presented results of a study using the MyPhenome Hungry Gut test, which was developed through machine learning, a form of artificial intelligence.
The test is part of the MyPhenome obesity phenotyping portfolio from Phenomix Sciences, a company founded by Mayo Clinic physicians, scientists, and researchers Andres Acosta, MD, PhD, and Michael Camilleri, MD, DSc.
At the ADA meeting, Dr. Hurtado Andrade discussed a test of 137 adults: 91 were considered to have a positive biomarker for abnormal postprandial satiety (APS+), and 46 who did not have it were classified as APS−. These were patients of the Mayo Clinic who were already taking obesity drugs and agreed to phenotyping. Of this group, 113 were on semaglutide and 24 on tirzepatide.
, with a mean 19.4% body weight loss in the APS+ group and a mean loss of 22.1% in the APS− group.
Further studies are warranted to assess the clinical utility of these biomarkers, Dr. Hurtado Andrade said. But these findings do support “the use of precision medicine for obesity based on an individual’s genetic background,” she said.
Dr. Hurtado Andrade’s presentation impressed fellow researchers who noted it as an early step toward the long-sought goal of more personalized medicine.
Daniel S. Hsia, MD, of Emory University, Atlanta, who led the ADA session at which Dr. Hurtado Andrade presented, said it was good to see new information being presented about using genetic risk scoring in obesity.
“The numbers were very small for the tirzepatide group as compared to the semaglutide group, so it’s a little hard to really come to any significant conclusions,” Dr. Hsia said in an interview.
At the ADA meeting, Ajay D. Rao, MD, MMSc, of Temple University, Philadelphia, said clinicians are excited about the idea of having biomarkers to aid in decisions about approaches to obesity.
In a follow-up interview with this news organization, Dr. Rao said he too is looking to see more testing of this approach to care, while describing Hurtado Andrade’s work as a “very well-done study.”
“We still need to see more large-scale studies of responsiveness to certain interventions,” he said.
Dr. Hurtado Andrade noted that researchers at academic centers such as Mayo can try to hone in the combination of genetic and other factors that led to obesity, such as emotional eating patterns and abnormal postprandial satiety.
But this approach is not widely scalable, as it demands resources of time and staffing that not all clinicians and patients enjoy.
“To overcome this challenge, our team has been working on developing biomarkers” such as the machine-learning gene risk score used to predict abnormal postprandial satiety, she said.
Findings for a related project were presented in May at Digestive Disease Week, as this news organization reported earlier. In that study, researchers calculated the genetic risk score for 84 adults undergoing weight loss interventions at Mayo Clinic who were prescribed the glucagon-like peptide 1 receptor agonist semaglutide.
This news organization separately asked Phenomix about the sales of MyPhenome Test kits. These cost $499, and about 500 tests have been sold since commercialization started last year, a spokesperson said.
The study was funded by Phenomix Sciences. Separately, Dr. Hurtado Andrade has worked as a consultant for Novo Nordisk and received research support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM ADA 2024
GLP-1 Thyroid Warning Could Increase Overdiagnosis
ORLANDO, Florida — Clinicians should keep in mind concerns about overdiagnosis of thyroid cancer when prescribing glucagon-like peptide 1 (GLP-1) drugs, as the US boxed warning about this risk for this class of medicines for certain tumors in mice could trigger excess screening, an expert endocrinologist said.
Speaking at the annual American Diabetes Association (ADA) 84th Scientific Sessions, Elizabeth N. Pearce, MD, MSc, a professor of medicine at Boston University, Boston, reviewed the different approaches US and European regulators have taken for the GLP-1 drugs. She also explained the current concerns about the wide use of thyroid screening in general and how these intersect with the rapid uptake of the GLP-1 drugs.
said Dr. Pearce, who is also a former board president of the American Thyroid Association (ATA). “We do not want to contribute to this epidemic of overdiagnosis of thyroid cancer.”
The ATA and the US Preventive Services Task Force (USPSTF) are among the health organizations that have in recent years sought to boost public awareness of the potential risks for excess screening of thyroid nodules. In 2017, the USPSTF, which influences insurance coverage, recommended against routine screening for thyroid cancer in asymptomatic adults. At that time, the incidence of thyroid cancer detection had increased by 4.5% per year over a decade, faster than for any other cancer, but without a corresponding change in the mortality rate, USPSTF said.
“Unequivocally, the thyroid cancer mortality has not kept pace with thyroid cancer detection,” Dr. Pearce said at the ADA meeting. “We’ve been diagnosing a lot of small thyroid cancers that people would otherwise have been destined to die with and not die of.”
Dr. Pearce said clinicians should be careful not to overly restrict access to GLP-1 drugs due to concerns about thyroid cancer — and they should use care in screening nodules.
It’s possible that the weight loss experienced by people taking GLP-1 drugs may make preexisting thyroid nodules more prominent, Dr. Pearce said. It’s also likely that the US boxed warning on thyroid risk on GLP-1 drugs makes clinicians and patients more likely to look for these kinds of growths.
Dr. Pearce urged adherence to guidelines such as the ones the ATA published in 2015 for assessing nodules.
In an interview with this news organization, Dr. Pearce noted the frequency of CT scans in US medical practice in turning up many incidental thyroid nodules, a finding that can cause some panic for patients and their clinicians.
But it helps to put these findings in context, as by the age of 50, about 40% of women will have at least one thyroid nodule, making this a very common finding, she said.
“The vast majority are not malignant,” Dr. Pearce said. “When you explain this to patients, it alleviates anxiety.”
The US, European Union Differences
In the United States, the label for GLP-1 drugs starts with a boxed warning about thyroid C-cell tumors seen in rodents given these medicines in testing.
It’s unknown if the medicines could cause medullary thyroid carcinoma (MTC) in humans, the label adds. The drug is contraindicated in patients with a personal or family history of MTC or multiple endocrine neoplasia syndrome 2, the boxed warning says. This is based largely on data seen in laboratory rats.
“It’s a big black box warning that gets people’s attention,” Dr. Pearce said. “Important to note that if you practice in Europe, you will not be familiar with this labeling because it doesn’t exist there. They’ve never had this warning on the European package.”
The European Medicines Agency (EMA) does include information about the results of rodent studies as part of the discussion of known and potential risks for GLP-1 drugs but has not emphasized it in the same way as the US drug labels do.
For example, the public assessment report posted on the EMA website for semaglutide (Ozempic, Novo Nordisk) notes that nonlethal thyroid C-cell tumors “observed in rodents are a class effect for GLP-1 receptor agonists.” It’s possible that these may be due to a particular sensitivity in rodents, the report said.
“The relevance for humans is considered to be low but cannot be completely excluded,” the EMA report said in the product information section of the report.
There has been ongoing interest in the issue.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) in October concluded that the available evidence does not support a causal association between GLP-1 receptor agonists and thyroid cancer.
The EMA’s PRAC safety committee said it began assessing the evidence about a possible connection following the publication of a study in 2022 in the journal Diabetes Care. That paper reported on an analysis that suggested increased risk for all thyroid cancer and medullary thyroid cancer with the use of GLP-1 drugs, particularly after 1-3 years of treatment.
The EMA’s PRAC said that in making its decision, it also considered other published papers on this topic as well as clinical and postmarketing data on GLP-1 drugs.
In an email interview, Jean-Luc Faillie, MD, PhD, corresponding author of the Diabetes Care paper, called for continued “vigilance and prudence in clinical practice” with GLP-1 drugs.
His paper reported on a case-control analysis on the basis of reports from the French national healthcare insurance system database, looking at people who had taken GLP-1 drugs and similar people who had not.
Due to a lack of a specific diagnostic code for medullary thyroid cancers, the researchers used a composite definition combining thyroid cancer diagnosis with several calcitonin tests, a carcinoembryonic antigen test, or a specific treatment (vandetanib) to identify potential cases of this cancer.
It’s possible that this method could have led to overestimation of MTC among the cases of thyroid cancer, wrote Dr. Faillie, who is a professor at France’s Université de Montpellier, Montpellier, France, and part of its pharmacological vigilance service.
“Nevertheless, it’s crucial to emphasize that any potential overestimation of MTC cases would likely apply equally to both GLP-1 receptor agonist–exposed and unexposed groups,” Dr. Faillie wrote. “Therefore, it should not significantly impact our main findings regarding the suggested increased risk associated with GLP-1 receptor agonist use.”
Dr. Pearce disclosed honoraria for speaking at the Merck China Forum. Dr. Faille and his coauthors reported no conflicts of interest in the publication of their study. Their research was supported by the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des Produits de Santé, grant 2019S015) in the context of a partnership with the Health Product Epidemiology Scientific Interest Group (EPI-PHARE). The study was part of France’s Drugs Systematized Assessment in Real-Life Environment (DRUGS-SAFEr) research program.
A version of this article first appeared on Medscape.com.
ORLANDO, Florida — Clinicians should keep in mind concerns about overdiagnosis of thyroid cancer when prescribing glucagon-like peptide 1 (GLP-1) drugs, as the US boxed warning about this risk for this class of medicines for certain tumors in mice could trigger excess screening, an expert endocrinologist said.
Speaking at the annual American Diabetes Association (ADA) 84th Scientific Sessions, Elizabeth N. Pearce, MD, MSc, a professor of medicine at Boston University, Boston, reviewed the different approaches US and European regulators have taken for the GLP-1 drugs. She also explained the current concerns about the wide use of thyroid screening in general and how these intersect with the rapid uptake of the GLP-1 drugs.
said Dr. Pearce, who is also a former board president of the American Thyroid Association (ATA). “We do not want to contribute to this epidemic of overdiagnosis of thyroid cancer.”
The ATA and the US Preventive Services Task Force (USPSTF) are among the health organizations that have in recent years sought to boost public awareness of the potential risks for excess screening of thyroid nodules. In 2017, the USPSTF, which influences insurance coverage, recommended against routine screening for thyroid cancer in asymptomatic adults. At that time, the incidence of thyroid cancer detection had increased by 4.5% per year over a decade, faster than for any other cancer, but without a corresponding change in the mortality rate, USPSTF said.
“Unequivocally, the thyroid cancer mortality has not kept pace with thyroid cancer detection,” Dr. Pearce said at the ADA meeting. “We’ve been diagnosing a lot of small thyroid cancers that people would otherwise have been destined to die with and not die of.”
Dr. Pearce said clinicians should be careful not to overly restrict access to GLP-1 drugs due to concerns about thyroid cancer — and they should use care in screening nodules.
It’s possible that the weight loss experienced by people taking GLP-1 drugs may make preexisting thyroid nodules more prominent, Dr. Pearce said. It’s also likely that the US boxed warning on thyroid risk on GLP-1 drugs makes clinicians and patients more likely to look for these kinds of growths.
Dr. Pearce urged adherence to guidelines such as the ones the ATA published in 2015 for assessing nodules.
In an interview with this news organization, Dr. Pearce noted the frequency of CT scans in US medical practice in turning up many incidental thyroid nodules, a finding that can cause some panic for patients and their clinicians.
But it helps to put these findings in context, as by the age of 50, about 40% of women will have at least one thyroid nodule, making this a very common finding, she said.
“The vast majority are not malignant,” Dr. Pearce said. “When you explain this to patients, it alleviates anxiety.”
The US, European Union Differences
In the United States, the label for GLP-1 drugs starts with a boxed warning about thyroid C-cell tumors seen in rodents given these medicines in testing.
It’s unknown if the medicines could cause medullary thyroid carcinoma (MTC) in humans, the label adds. The drug is contraindicated in patients with a personal or family history of MTC or multiple endocrine neoplasia syndrome 2, the boxed warning says. This is based largely on data seen in laboratory rats.
“It’s a big black box warning that gets people’s attention,” Dr. Pearce said. “Important to note that if you practice in Europe, you will not be familiar with this labeling because it doesn’t exist there. They’ve never had this warning on the European package.”
The European Medicines Agency (EMA) does include information about the results of rodent studies as part of the discussion of known and potential risks for GLP-1 drugs but has not emphasized it in the same way as the US drug labels do.
For example, the public assessment report posted on the EMA website for semaglutide (Ozempic, Novo Nordisk) notes that nonlethal thyroid C-cell tumors “observed in rodents are a class effect for GLP-1 receptor agonists.” It’s possible that these may be due to a particular sensitivity in rodents, the report said.
“The relevance for humans is considered to be low but cannot be completely excluded,” the EMA report said in the product information section of the report.
There has been ongoing interest in the issue.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) in October concluded that the available evidence does not support a causal association between GLP-1 receptor agonists and thyroid cancer.
The EMA’s PRAC safety committee said it began assessing the evidence about a possible connection following the publication of a study in 2022 in the journal Diabetes Care. That paper reported on an analysis that suggested increased risk for all thyroid cancer and medullary thyroid cancer with the use of GLP-1 drugs, particularly after 1-3 years of treatment.
The EMA’s PRAC said that in making its decision, it also considered other published papers on this topic as well as clinical and postmarketing data on GLP-1 drugs.
In an email interview, Jean-Luc Faillie, MD, PhD, corresponding author of the Diabetes Care paper, called for continued “vigilance and prudence in clinical practice” with GLP-1 drugs.
His paper reported on a case-control analysis on the basis of reports from the French national healthcare insurance system database, looking at people who had taken GLP-1 drugs and similar people who had not.
Due to a lack of a specific diagnostic code for medullary thyroid cancers, the researchers used a composite definition combining thyroid cancer diagnosis with several calcitonin tests, a carcinoembryonic antigen test, or a specific treatment (vandetanib) to identify potential cases of this cancer.
It’s possible that this method could have led to overestimation of MTC among the cases of thyroid cancer, wrote Dr. Faillie, who is a professor at France’s Université de Montpellier, Montpellier, France, and part of its pharmacological vigilance service.
“Nevertheless, it’s crucial to emphasize that any potential overestimation of MTC cases would likely apply equally to both GLP-1 receptor agonist–exposed and unexposed groups,” Dr. Faillie wrote. “Therefore, it should not significantly impact our main findings regarding the suggested increased risk associated with GLP-1 receptor agonist use.”
Dr. Pearce disclosed honoraria for speaking at the Merck China Forum. Dr. Faille and his coauthors reported no conflicts of interest in the publication of their study. Their research was supported by the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des Produits de Santé, grant 2019S015) in the context of a partnership with the Health Product Epidemiology Scientific Interest Group (EPI-PHARE). The study was part of France’s Drugs Systematized Assessment in Real-Life Environment (DRUGS-SAFEr) research program.
A version of this article first appeared on Medscape.com.
ORLANDO, Florida — Clinicians should keep in mind concerns about overdiagnosis of thyroid cancer when prescribing glucagon-like peptide 1 (GLP-1) drugs, as the US boxed warning about this risk for this class of medicines for certain tumors in mice could trigger excess screening, an expert endocrinologist said.
Speaking at the annual American Diabetes Association (ADA) 84th Scientific Sessions, Elizabeth N. Pearce, MD, MSc, a professor of medicine at Boston University, Boston, reviewed the different approaches US and European regulators have taken for the GLP-1 drugs. She also explained the current concerns about the wide use of thyroid screening in general and how these intersect with the rapid uptake of the GLP-1 drugs.
said Dr. Pearce, who is also a former board president of the American Thyroid Association (ATA). “We do not want to contribute to this epidemic of overdiagnosis of thyroid cancer.”
The ATA and the US Preventive Services Task Force (USPSTF) are among the health organizations that have in recent years sought to boost public awareness of the potential risks for excess screening of thyroid nodules. In 2017, the USPSTF, which influences insurance coverage, recommended against routine screening for thyroid cancer in asymptomatic adults. At that time, the incidence of thyroid cancer detection had increased by 4.5% per year over a decade, faster than for any other cancer, but without a corresponding change in the mortality rate, USPSTF said.
“Unequivocally, the thyroid cancer mortality has not kept pace with thyroid cancer detection,” Dr. Pearce said at the ADA meeting. “We’ve been diagnosing a lot of small thyroid cancers that people would otherwise have been destined to die with and not die of.”
Dr. Pearce said clinicians should be careful not to overly restrict access to GLP-1 drugs due to concerns about thyroid cancer — and they should use care in screening nodules.
It’s possible that the weight loss experienced by people taking GLP-1 drugs may make preexisting thyroid nodules more prominent, Dr. Pearce said. It’s also likely that the US boxed warning on thyroid risk on GLP-1 drugs makes clinicians and patients more likely to look for these kinds of growths.
Dr. Pearce urged adherence to guidelines such as the ones the ATA published in 2015 for assessing nodules.
In an interview with this news organization, Dr. Pearce noted the frequency of CT scans in US medical practice in turning up many incidental thyroid nodules, a finding that can cause some panic for patients and their clinicians.
But it helps to put these findings in context, as by the age of 50, about 40% of women will have at least one thyroid nodule, making this a very common finding, she said.
“The vast majority are not malignant,” Dr. Pearce said. “When you explain this to patients, it alleviates anxiety.”
The US, European Union Differences
In the United States, the label for GLP-1 drugs starts with a boxed warning about thyroid C-cell tumors seen in rodents given these medicines in testing.
It’s unknown if the medicines could cause medullary thyroid carcinoma (MTC) in humans, the label adds. The drug is contraindicated in patients with a personal or family history of MTC or multiple endocrine neoplasia syndrome 2, the boxed warning says. This is based largely on data seen in laboratory rats.
“It’s a big black box warning that gets people’s attention,” Dr. Pearce said. “Important to note that if you practice in Europe, you will not be familiar with this labeling because it doesn’t exist there. They’ve never had this warning on the European package.”
The European Medicines Agency (EMA) does include information about the results of rodent studies as part of the discussion of known and potential risks for GLP-1 drugs but has not emphasized it in the same way as the US drug labels do.
For example, the public assessment report posted on the EMA website for semaglutide (Ozempic, Novo Nordisk) notes that nonlethal thyroid C-cell tumors “observed in rodents are a class effect for GLP-1 receptor agonists.” It’s possible that these may be due to a particular sensitivity in rodents, the report said.
“The relevance for humans is considered to be low but cannot be completely excluded,” the EMA report said in the product information section of the report.
There has been ongoing interest in the issue.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) in October concluded that the available evidence does not support a causal association between GLP-1 receptor agonists and thyroid cancer.
The EMA’s PRAC safety committee said it began assessing the evidence about a possible connection following the publication of a study in 2022 in the journal Diabetes Care. That paper reported on an analysis that suggested increased risk for all thyroid cancer and medullary thyroid cancer with the use of GLP-1 drugs, particularly after 1-3 years of treatment.
The EMA’s PRAC said that in making its decision, it also considered other published papers on this topic as well as clinical and postmarketing data on GLP-1 drugs.
In an email interview, Jean-Luc Faillie, MD, PhD, corresponding author of the Diabetes Care paper, called for continued “vigilance and prudence in clinical practice” with GLP-1 drugs.
His paper reported on a case-control analysis on the basis of reports from the French national healthcare insurance system database, looking at people who had taken GLP-1 drugs and similar people who had not.
Due to a lack of a specific diagnostic code for medullary thyroid cancers, the researchers used a composite definition combining thyroid cancer diagnosis with several calcitonin tests, a carcinoembryonic antigen test, or a specific treatment (vandetanib) to identify potential cases of this cancer.
It’s possible that this method could have led to overestimation of MTC among the cases of thyroid cancer, wrote Dr. Faillie, who is a professor at France’s Université de Montpellier, Montpellier, France, and part of its pharmacological vigilance service.
“Nevertheless, it’s crucial to emphasize that any potential overestimation of MTC cases would likely apply equally to both GLP-1 receptor agonist–exposed and unexposed groups,” Dr. Faillie wrote. “Therefore, it should not significantly impact our main findings regarding the suggested increased risk associated with GLP-1 receptor agonist use.”
Dr. Pearce disclosed honoraria for speaking at the Merck China Forum. Dr. Faille and his coauthors reported no conflicts of interest in the publication of their study. Their research was supported by the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des Produits de Santé, grant 2019S015) in the context of a partnership with the Health Product Epidemiology Scientific Interest Group (EPI-PHARE). The study was part of France’s Drugs Systematized Assessment in Real-Life Environment (DRUGS-SAFEr) research program.
A version of this article first appeared on Medscape.com.
FROM ADA 2024
Facial Temperature Can Reveal Age and Disease
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.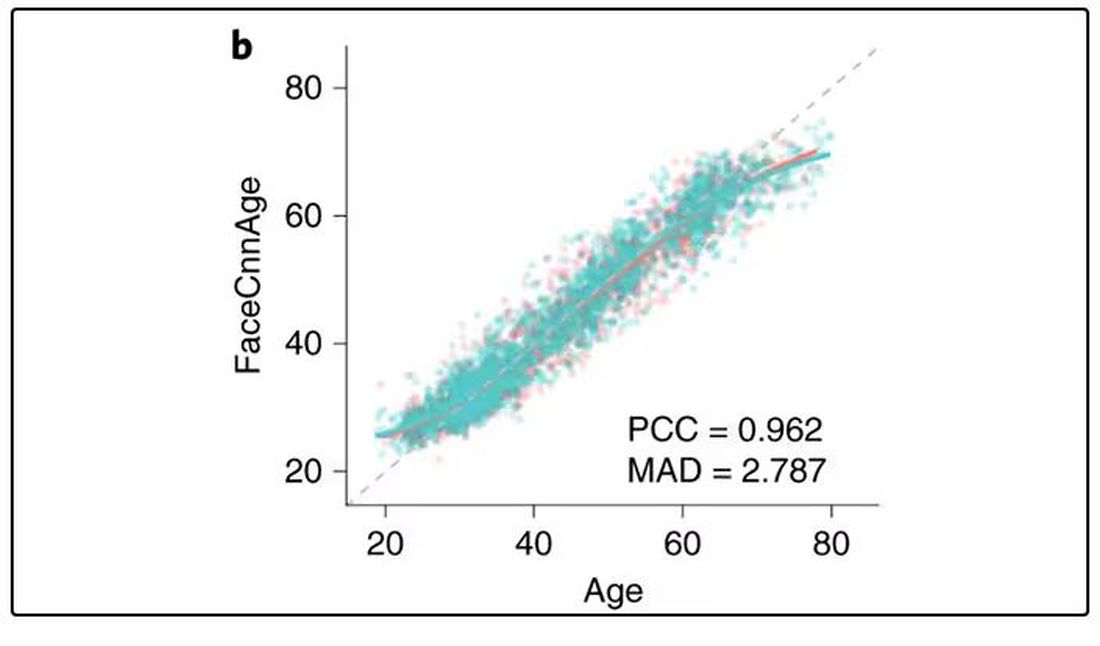
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 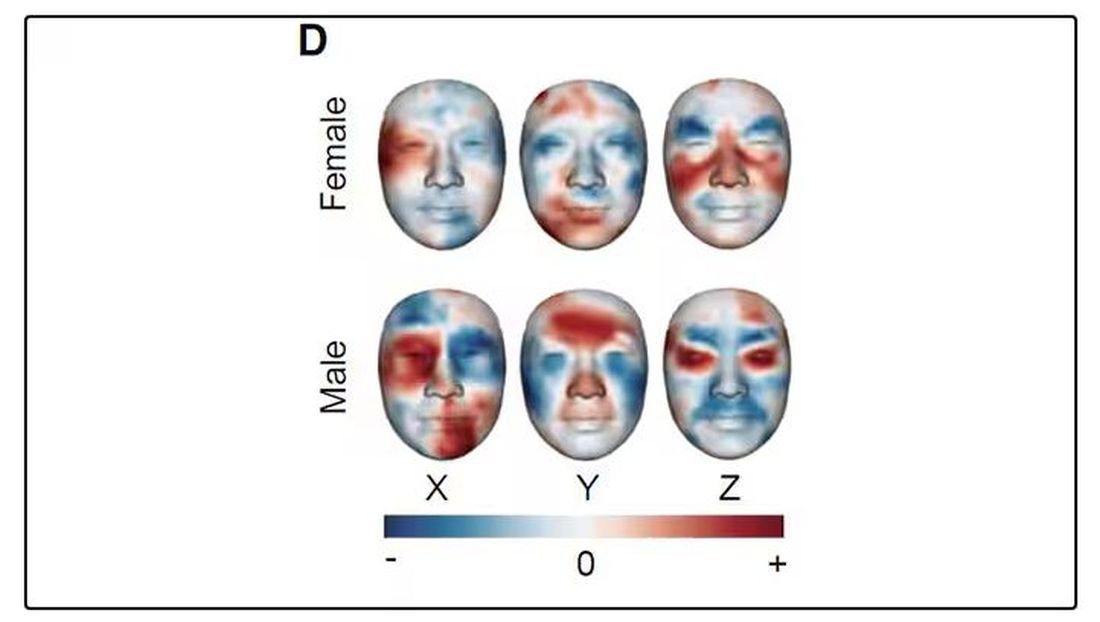
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.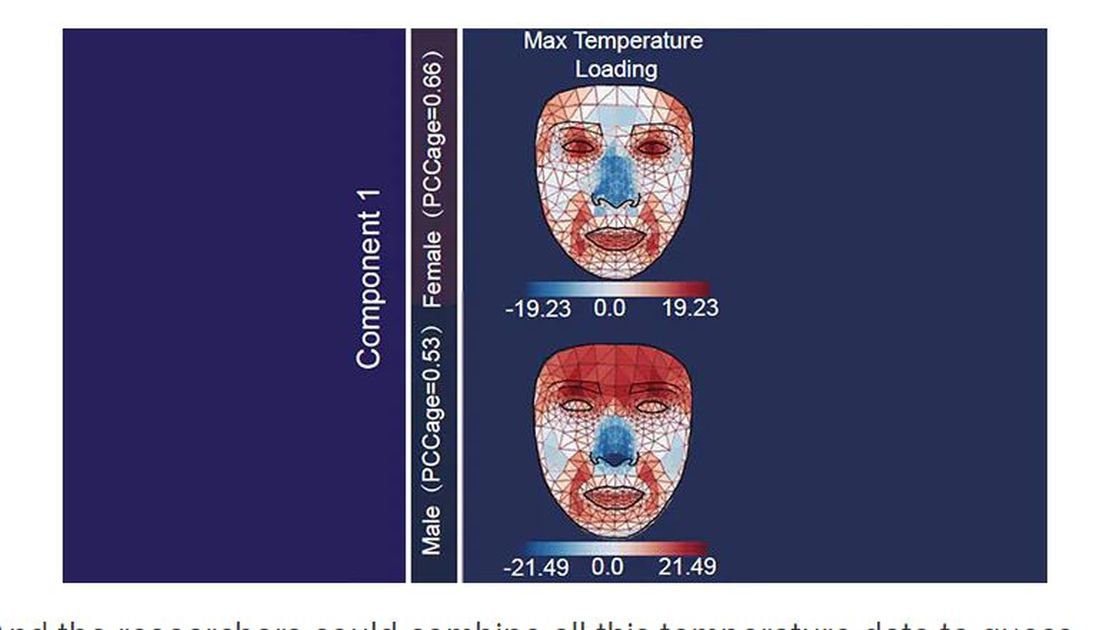
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.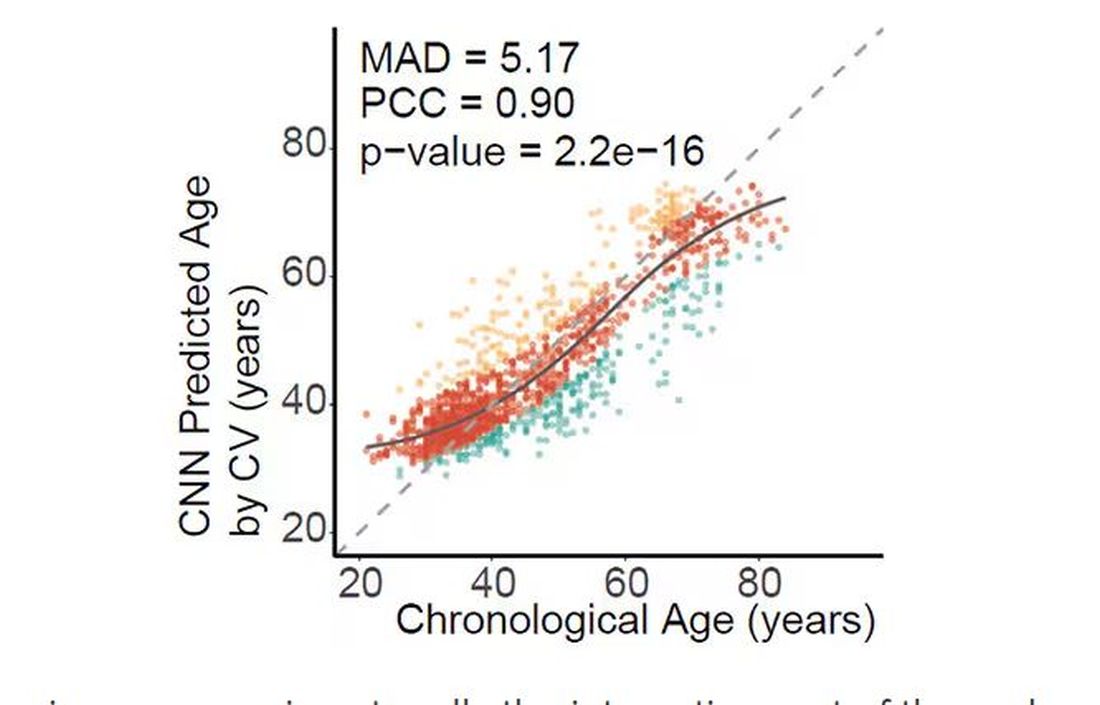
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.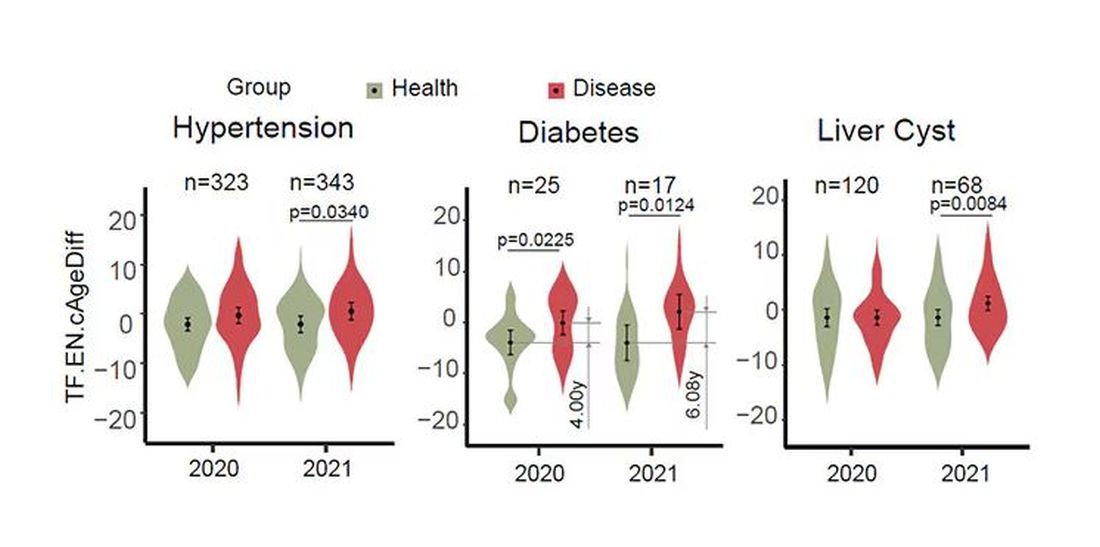
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.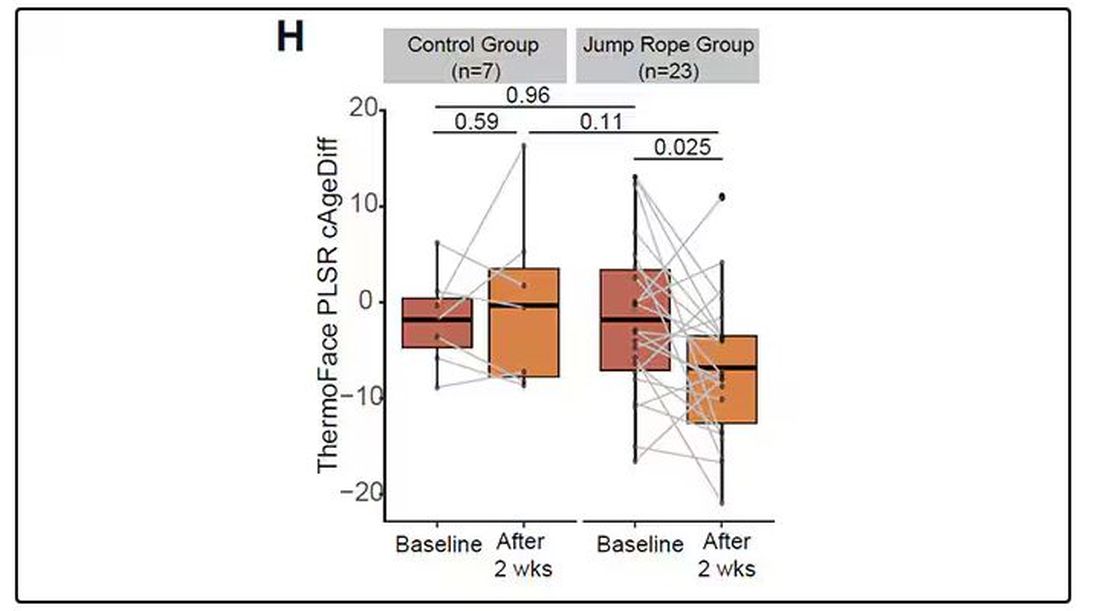
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 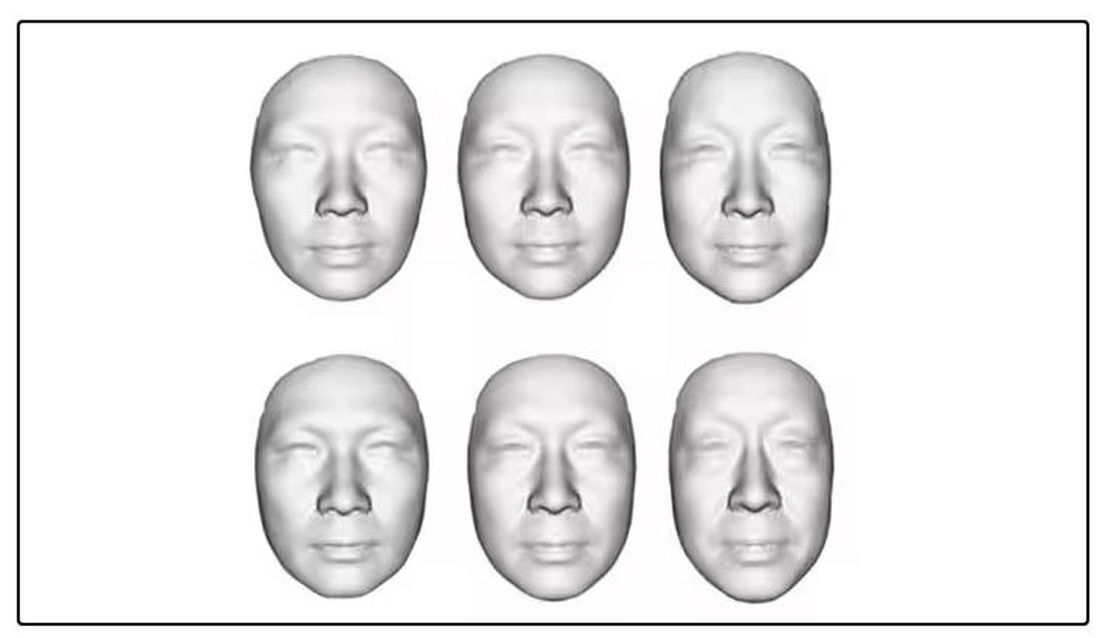
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.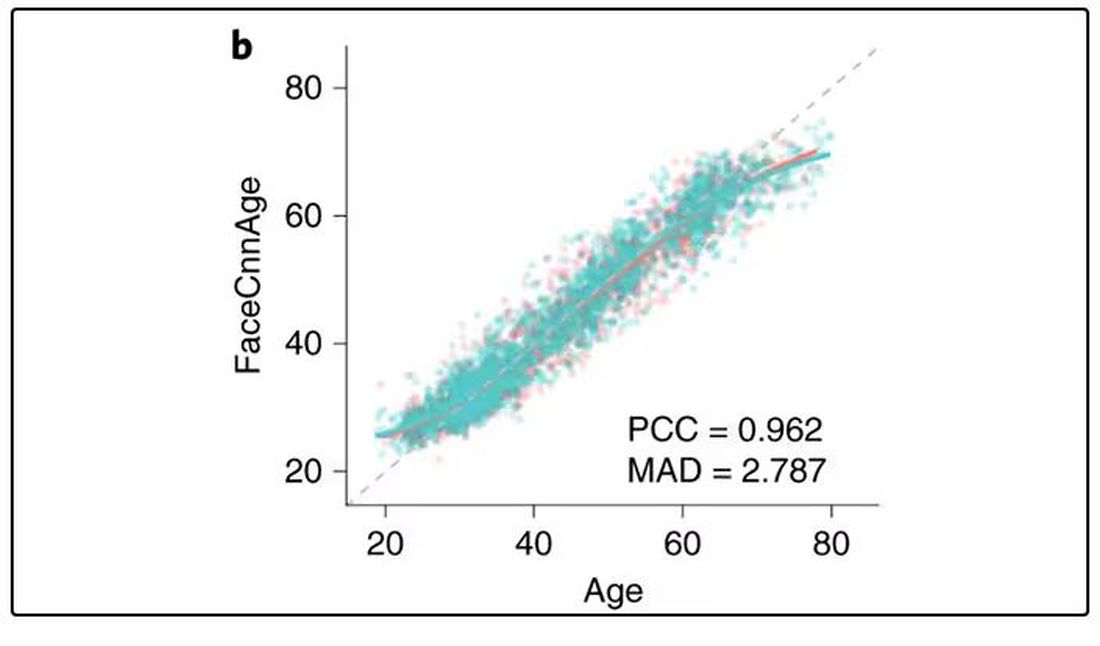
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 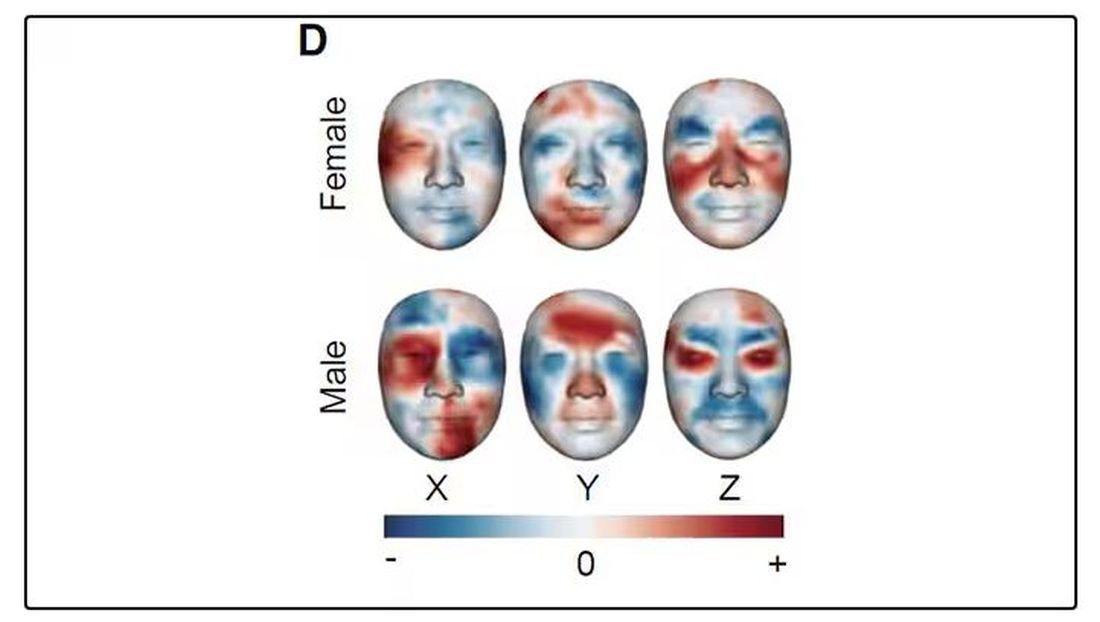
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.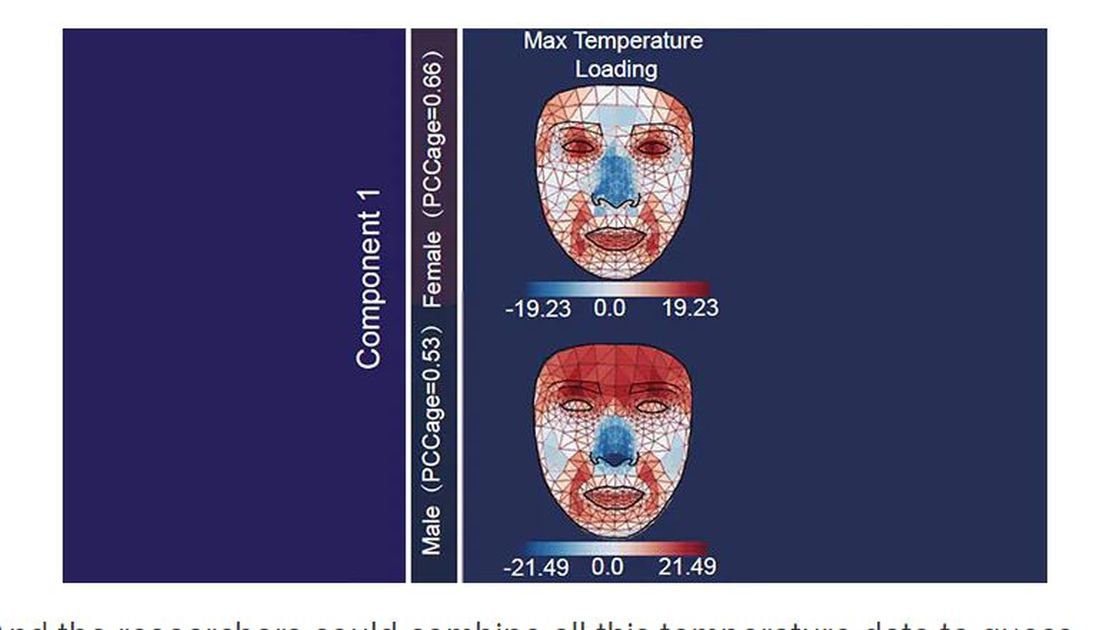
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.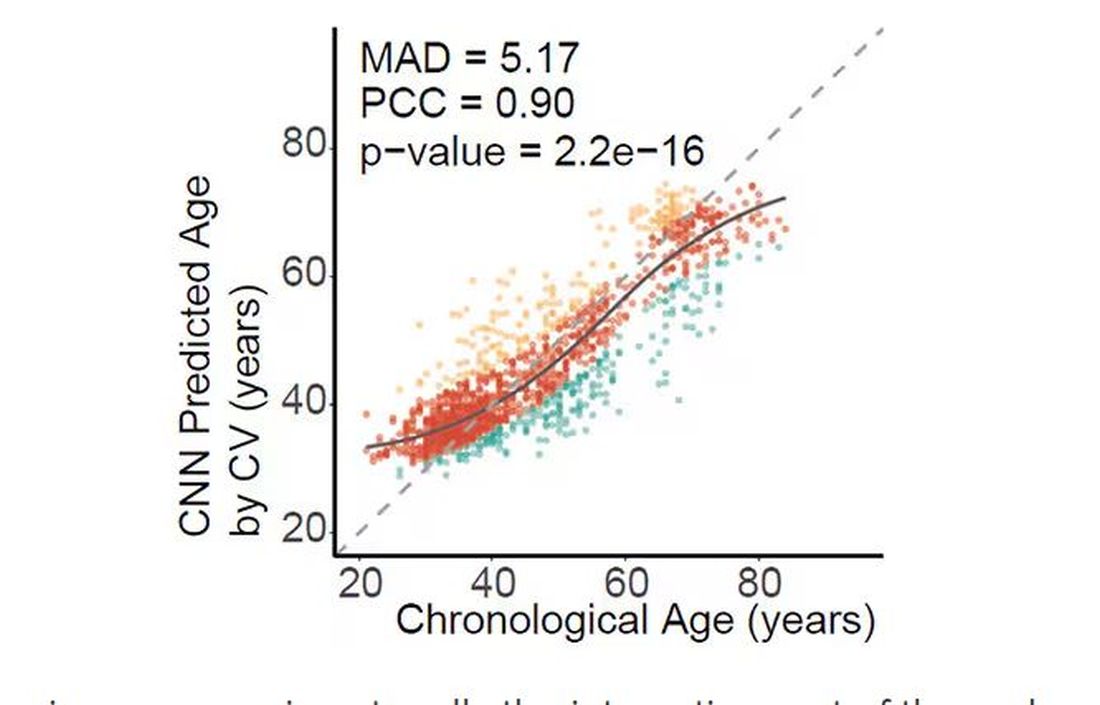
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.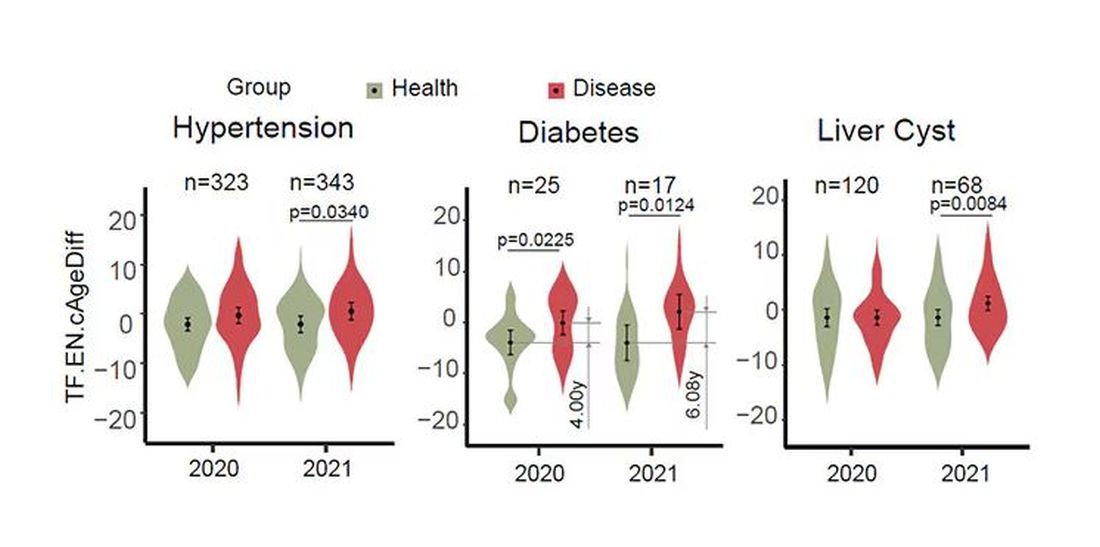
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.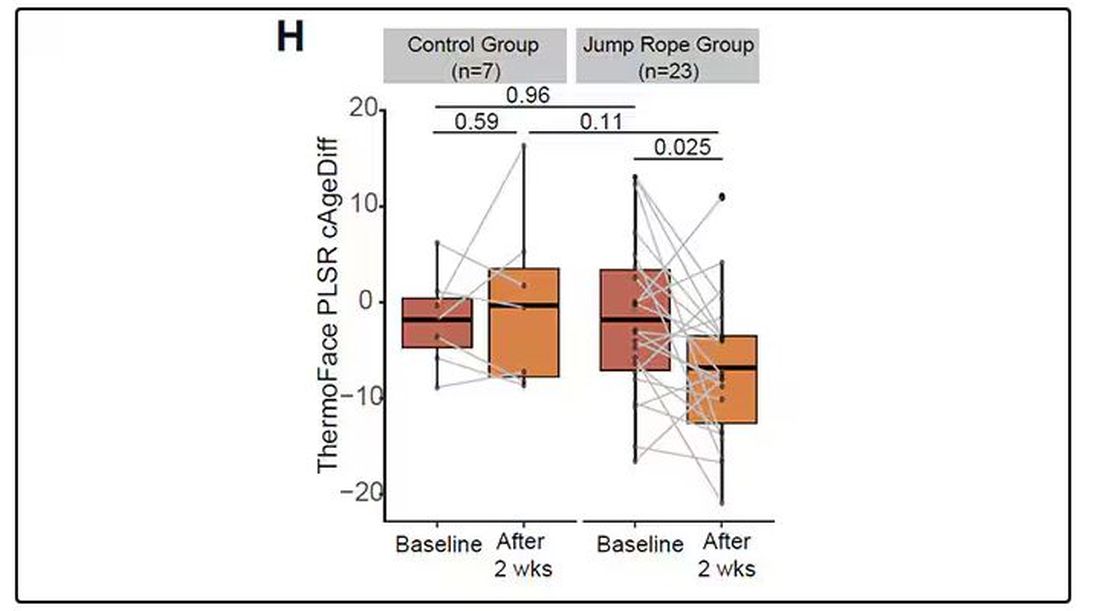
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.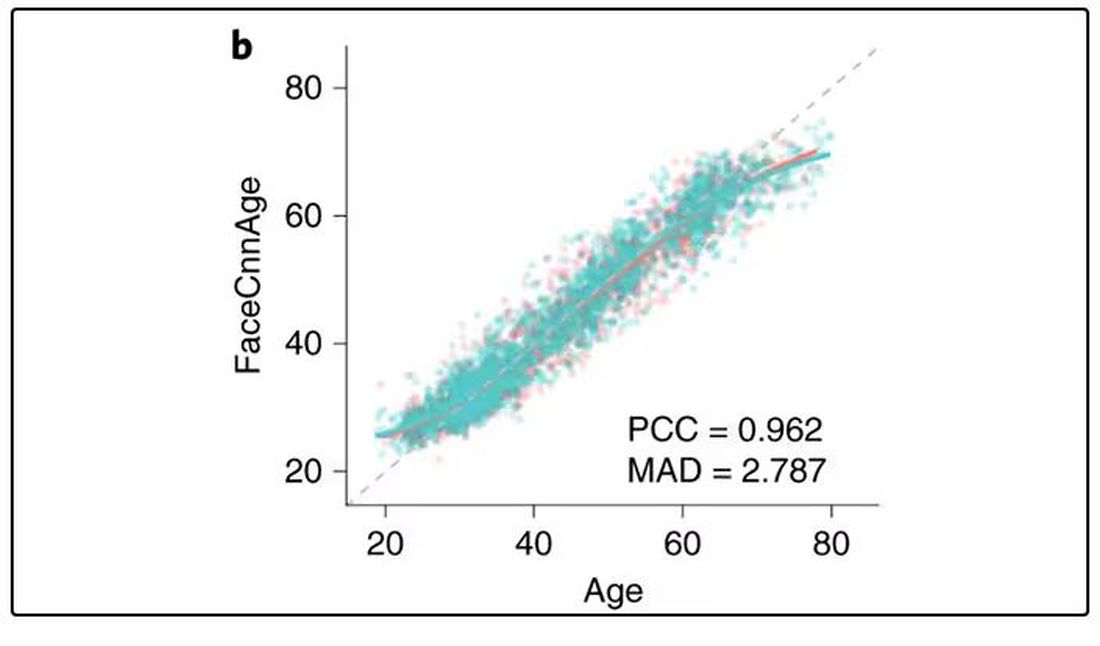
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 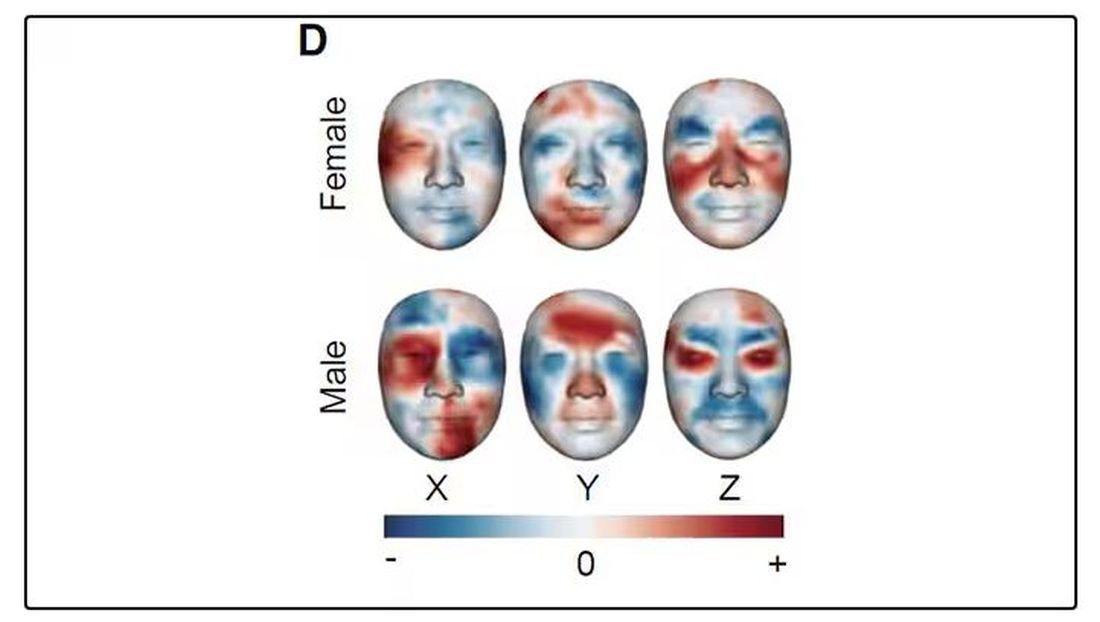
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.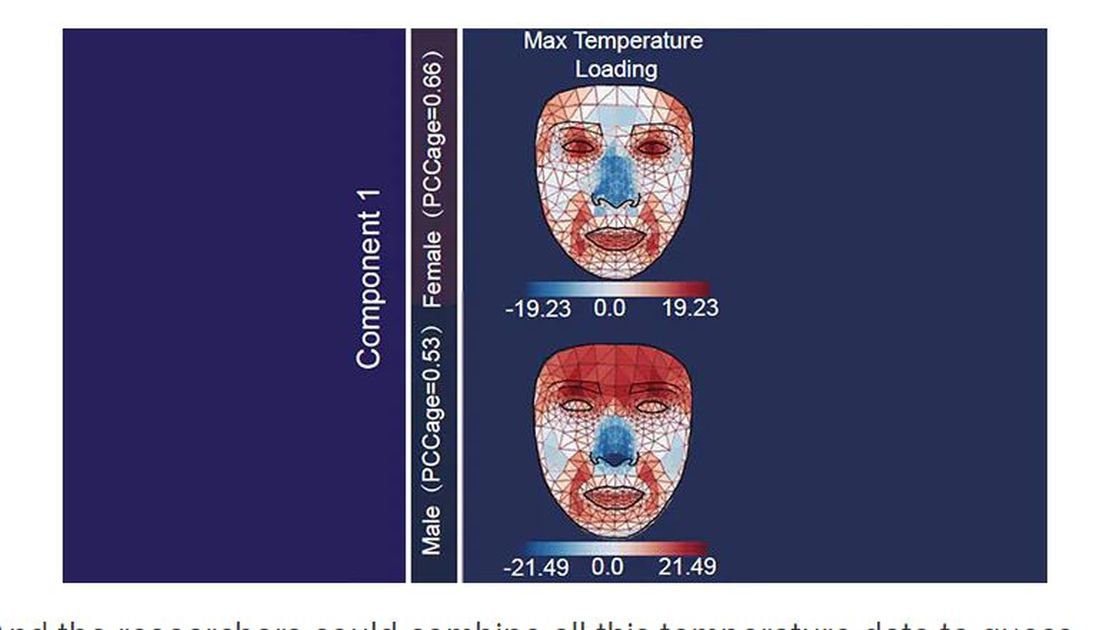
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.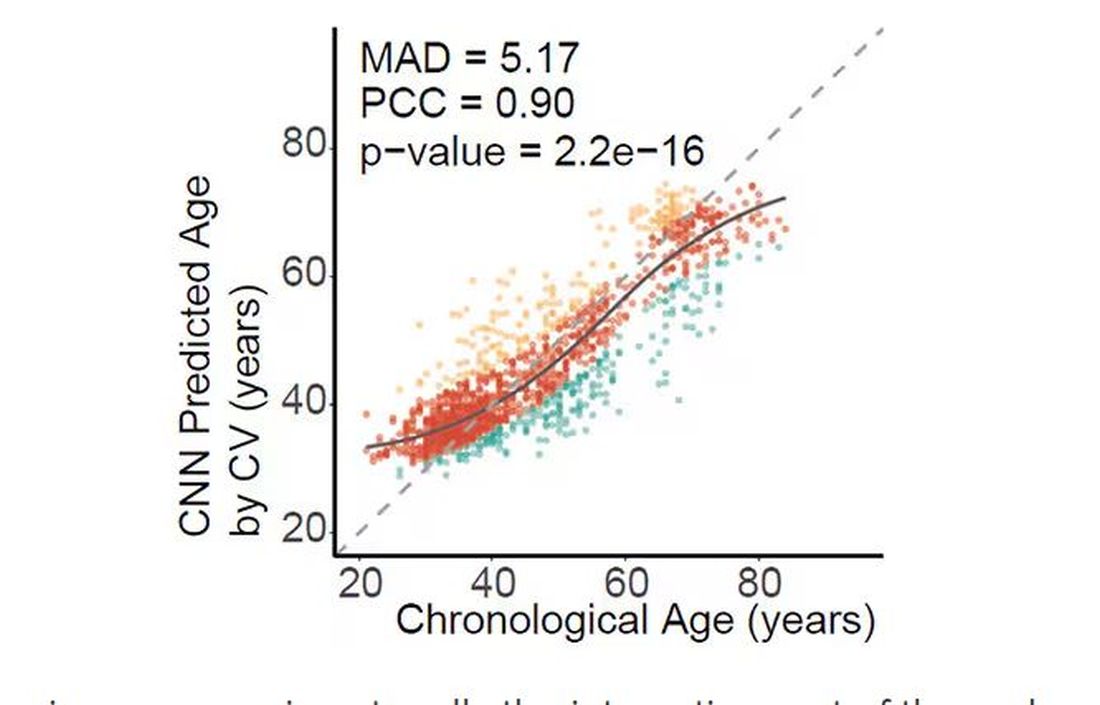
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.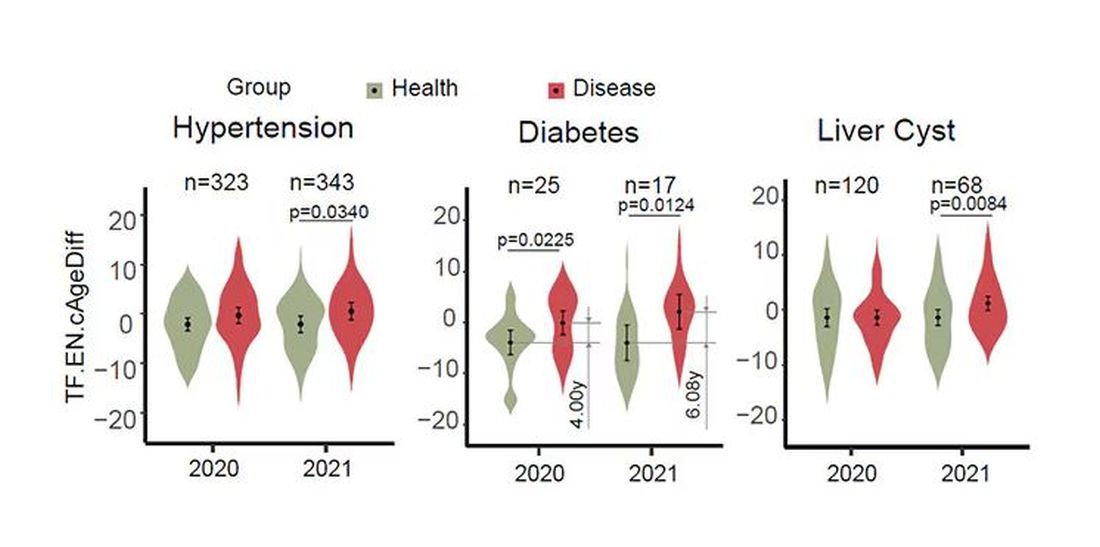
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.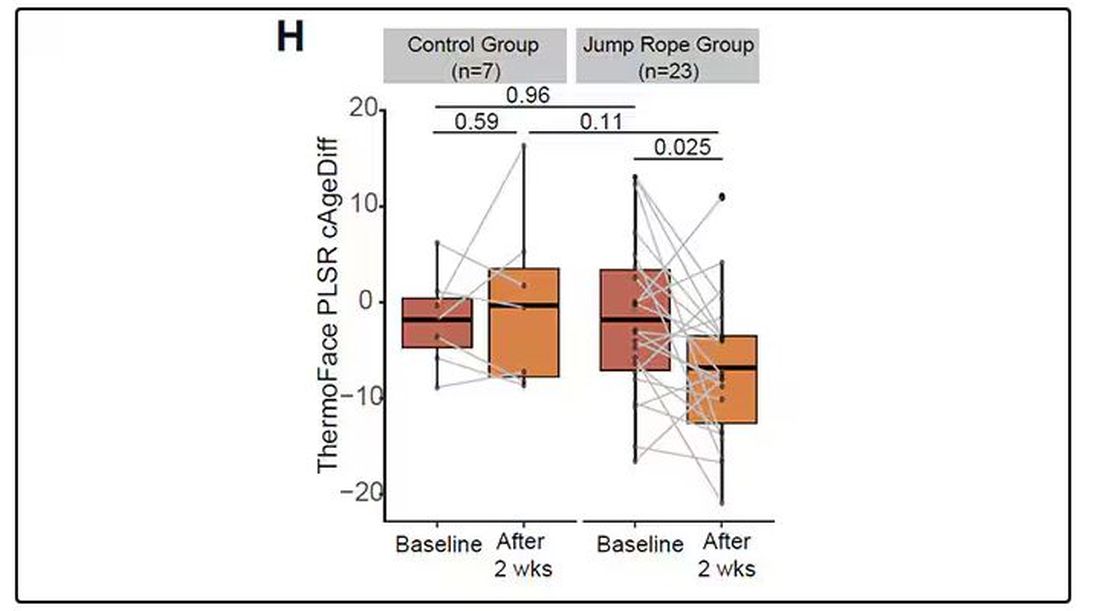
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
What Should Be Prioritized in Managing Early Diabetes?
ORLANDO, FLORIDA — What to prioritize first in managing early diabetes? That was the question debated on an expert panel at the American Diabetes Association (ADA) 84th Scientific Sessions, with impassioned responses ranging from a plea to “treat obesity first,” to a James Carville–inspired counterpoint of “it’s the glucose, stupid.”
With a focus on preventing complications and inducing remission rounding out the four positions argued,
“In clinical decision-making [for early diabetes], we are faced with weighing each of these variables for the individual patient, and while all are good options, strong arguments can be made for prioritizing each — with the potential of each choice to influence or improve all of the others,” Dr. Retnakaran told this news organization.
Which to Prioritize First?
Making the obesity first argument, Ania M. Jastreboff, MD, PhD, associate professor and director of the Yale Obesity Research Center at Yale School of Medicine, New Haven, Connecticut, noted the striking statistic that nearly 90% of people with type 2 diabetes have overweight or obesity and discussed the ever-expanding data showing the benefits of drugs including glucagon-like peptide 1 (GLP-1) receptor agonists not just in weight loss but also in kidney, cardiovascular, and, as presented at the meeting, sleep apnea improvement.
She contrasted the experiences of two patients with obesity: One treated for the obesity upon type 2 diagnosis — who had a quick normalization of lipids and hypertension soon after the obesity treatment — and the other presenting after 10 years with type 2 diabetes — who was on therapy for hypertension and hyperlipidemia but not for obesity and whose diseases were not as easily treated by that point.
“Why are we treating all the downstream effects and we’re not treating the disease that is potentially the root cause of all these other diseases?” Dr. Jastreboff said.
Complications?
Arguing in favor of focusing on complications, Roopa Mehta, MD, PhD, with the department of endocrinology and metabolism at Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), Mexico City, made the case that stakes don’t get any higher in diabetes than when it comes the looming threat of potentially fatal complications.
Acute myocardial infarction, stroke, amputation, and end-stage renal disease are all on the list of unwanted outcomes and need to be considered even in the earliest stages, as data show early onset type 2 diabetes is linked to life expectancy.
“The main goal of management has always been to prevent complications,” she noted. Citing ADA guidelines, Dr. Mehta underscored the benefits of first- and second-line therapy of metformin, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and GLP-1 receptor agonists for most patients.
Remission?
Discussing the priority of putting patients into disease remission, Roy Taylor, MD, professor of medicine and metabolism at Newcastle University and Newcastle Hospitals NHS in Newcastle upon Tyne, England, and author of the book Life Without Diabetes, focused on an evidence-based alternative to achieving remission — a nonpharmacologic approach that avoids costly and sometimes inaccessible drugs.
In the intervention, described in the DiRECT randomized trial and subsequently in the UK National Health Service Type 2 Diabetes Path to Remission Program, patients with overweight or obesity were placed on a highly restrictive diet of just 800-900 calories a day for 12-20 weeks, followed by maintenance for 12 months, and they not only achieved weight loss but also achieved diabetes remission, in some cases long term.
Acknowledging that “this is not for everyone,” Dr. Taylor asserted that “we have to realize there is a substantial minority of people who want to be healthy but who don’t want to be medicalized,” he said.
“They want their health, and they can do extremely well.”
Glucose?
In taking his self-titled “it’s the glucose, stupid” stand, David M. Nathan, MD, of the Diabetes Center, Massachusetts General Hospital, Harvard Medical School, in Boston, cited extensive evidence showing that early intensive blood glucose control with treatment including sulfonylureas, insulin, or metformin significantly reduced the risk for complications in type 2 diabetes 15 or more years later, including renal failure, blindness, amputation, and myocardial infarctions, in addition to a reduction in diabetes-related death.
“In many of these studies, you saw the benefit even in the setting of weight-gain,” Dr. Nathan underscored.
He further noted the “sobering” findings of the Look AHEAD study, which had to be stopped due to futility when an intensive lifestyle/weight loss intervention showed no significant benefits in terms of cardiovascular disease in people with type 2 diabetes at a median follow-up of 9.6 years.
Ultimately, “diabetes, type 1 and type 2, remains a gluco-centric disease,” Dr. Nathan asserted. “Hyperglycemia is the only universal link between all forms of diabetes and mortality, and the long-term complications of diabetes are intimately associated with hyperglycemia.”
Tackling the Caveats
The ensuing panel discussion did not fail to deliver in delving into key areas of contention, particularly in terms of GLP-1 treatment.
Regarding a lack of data on the potential long-term effects of GLP-1s: “Yes, there are a huge number of studies [on GLP-1 receptor agonists], but they are, in general, over short periods of time and driven by pharma, who get in and get out as quickly as they can and have little in the way of interest to do comparative effectiveness studies,” Dr. Nathan argued.
“Meanwhile, this is like the crack cocaine of medications — patients have to stay on it for a lifetime or they will regain the weight — are you concerned at all about a lifetime of exposure to GLP-1 [drugs]?” he asked the panel.
Dr. Jastreboff responded that the first GLP-1 receptor agonist medications were approved in 2005, nearly 20 years ago, by the US Food and Drug Administration.
“Do I think we need long-term lifetime data? Absolutely,” she said. “We need to do our due diligence, we need to be careful, we need to monitor patients, and when and if there are signals, we need to follow them.”
What about the notorious gastrointestinal side effects of the drugs? “A majority of them are mitigated by slow up-titration,” Dr. Jastreboff noted.
“If patients have nausea, I do not go up [in dose]. I invite patients to tell me if they’re having vomiting because I don’t want anybody to have it, and I can count on one hand how many of my patients do.”
Dr. Mehta added the concern that as the drugs’ popularity soars, “a lot of doctors don’t know when they need to put the brakes on [weight coming off too quickly].”
She underscored that “we are not treating obesity for weight loss or for cosmetic reasons — this is about optimizing health.”
Dr. Jastreboff noted that in her practice, “I down-titrate if they’re losing weight too quickly.”
“If the patient is losing more than 1% per week of their body weight, then I slow down to make sure they’re getting the nutrients that they need, that they have enough energy to exercise, and that they’re prioritizing protein and fruits and vegetables in their diet.
“We just need to go slow, and yes, we need to follow them long term,” she said.
Chiming in from the audience, Julio Rosenstock, MD, a recognized thought leader in type 2 diabetes, offered his own take on the issues, describing Dr. Taylor’s very low–calorie diet suggestion as “not realistic” and Dr. Nathan’s glucose-first argument to be “stuck in the past.”
Based on modern-day evidence, “there is no reason on earth to start [diabetes treatment] with only metformin,” asserted Dr. Rosenstock, director of the Velocity Clinical Research center at Medical City and clinical professor of medicine at the University of Texas Southwestern Medical Center, Dallas.
“We need to start at the very least with metformin and a sodium-glucose cotransporter 2 (SGLT2) inhibitor from day 1, and then, if it’s affordable and there is access, with a GLP-1 receptor agonist,” he said.
“There is nothing better these days than those agents that consistently have shown a reduction of cardiovascular events and slowing of kidney disease progression.”
Overall, however, “I think you are all right,” he added, a sentiment shared by most.
Noting that the discussion as a whole represents a virtual sea change from the evidence-based options that would have been discussed only a decade ago, Dr. Retnakaran summed up his take-home message: “Stay tuned.
“You could easily see things changing in the next decade to come as we get more data and evidence to support what we ultimately should prioritize an early type 2 diabetes, so this is an exciting time.”
Dr. Retnakaran disclosed ties with Novo Nordisk, Boehringer Ingelheim, Novartis, Sanofi, and Eli Lilly. Dr. Jastreboff disclosed ties with Amgen, AstraZeneca, Boehringer Ingelheim, Biohaven, Eli Lilly, Intellihealth, Novo Nordisk, Pfizer, Regeneron, Scholar Rock, Structure Therapeutics, Terms Pharmaceutical, Weight Watchers, and Zealand Pharmaceuticals. Dr. Roopa had relationships with Novo Nordisk, Boehringer Ingelheim, Amgen, AstraZeneca, Eli Lilly, Silanes, and Sanofi. Dr. Taylor received lecture fees from Novartis, Lilly, Abbott, and Nestle Health and research funding from Diabetes UK and is an advisor to Fast800. Dr. Rosenstock reported relationships with Applied Therapeutics, AstraZeneca, Biomea Fusion, Boehringer Ingelheim, Eli Lilly and Company, Hanmi, Merck, Oramed, Structure Therapeutics, Novartis, Novo Nordisk, Pfizer, Ragor, and Sanofi. Dr. Nathan had no disclosures to report.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — What to prioritize first in managing early diabetes? That was the question debated on an expert panel at the American Diabetes Association (ADA) 84th Scientific Sessions, with impassioned responses ranging from a plea to “treat obesity first,” to a James Carville–inspired counterpoint of “it’s the glucose, stupid.”
With a focus on preventing complications and inducing remission rounding out the four positions argued,
“In clinical decision-making [for early diabetes], we are faced with weighing each of these variables for the individual patient, and while all are good options, strong arguments can be made for prioritizing each — with the potential of each choice to influence or improve all of the others,” Dr. Retnakaran told this news organization.
Which to Prioritize First?
Making the obesity first argument, Ania M. Jastreboff, MD, PhD, associate professor and director of the Yale Obesity Research Center at Yale School of Medicine, New Haven, Connecticut, noted the striking statistic that nearly 90% of people with type 2 diabetes have overweight or obesity and discussed the ever-expanding data showing the benefits of drugs including glucagon-like peptide 1 (GLP-1) receptor agonists not just in weight loss but also in kidney, cardiovascular, and, as presented at the meeting, sleep apnea improvement.
She contrasted the experiences of two patients with obesity: One treated for the obesity upon type 2 diagnosis — who had a quick normalization of lipids and hypertension soon after the obesity treatment — and the other presenting after 10 years with type 2 diabetes — who was on therapy for hypertension and hyperlipidemia but not for obesity and whose diseases were not as easily treated by that point.
“Why are we treating all the downstream effects and we’re not treating the disease that is potentially the root cause of all these other diseases?” Dr. Jastreboff said.
Complications?
Arguing in favor of focusing on complications, Roopa Mehta, MD, PhD, with the department of endocrinology and metabolism at Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), Mexico City, made the case that stakes don’t get any higher in diabetes than when it comes the looming threat of potentially fatal complications.
Acute myocardial infarction, stroke, amputation, and end-stage renal disease are all on the list of unwanted outcomes and need to be considered even in the earliest stages, as data show early onset type 2 diabetes is linked to life expectancy.
“The main goal of management has always been to prevent complications,” she noted. Citing ADA guidelines, Dr. Mehta underscored the benefits of first- and second-line therapy of metformin, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and GLP-1 receptor agonists for most patients.
Remission?
Discussing the priority of putting patients into disease remission, Roy Taylor, MD, professor of medicine and metabolism at Newcastle University and Newcastle Hospitals NHS in Newcastle upon Tyne, England, and author of the book Life Without Diabetes, focused on an evidence-based alternative to achieving remission — a nonpharmacologic approach that avoids costly and sometimes inaccessible drugs.
In the intervention, described in the DiRECT randomized trial and subsequently in the UK National Health Service Type 2 Diabetes Path to Remission Program, patients with overweight or obesity were placed on a highly restrictive diet of just 800-900 calories a day for 12-20 weeks, followed by maintenance for 12 months, and they not only achieved weight loss but also achieved diabetes remission, in some cases long term.
Acknowledging that “this is not for everyone,” Dr. Taylor asserted that “we have to realize there is a substantial minority of people who want to be healthy but who don’t want to be medicalized,” he said.
“They want their health, and they can do extremely well.”
Glucose?
In taking his self-titled “it’s the glucose, stupid” stand, David M. Nathan, MD, of the Diabetes Center, Massachusetts General Hospital, Harvard Medical School, in Boston, cited extensive evidence showing that early intensive blood glucose control with treatment including sulfonylureas, insulin, or metformin significantly reduced the risk for complications in type 2 diabetes 15 or more years later, including renal failure, blindness, amputation, and myocardial infarctions, in addition to a reduction in diabetes-related death.
“In many of these studies, you saw the benefit even in the setting of weight-gain,” Dr. Nathan underscored.
He further noted the “sobering” findings of the Look AHEAD study, which had to be stopped due to futility when an intensive lifestyle/weight loss intervention showed no significant benefits in terms of cardiovascular disease in people with type 2 diabetes at a median follow-up of 9.6 years.
Ultimately, “diabetes, type 1 and type 2, remains a gluco-centric disease,” Dr. Nathan asserted. “Hyperglycemia is the only universal link between all forms of diabetes and mortality, and the long-term complications of diabetes are intimately associated with hyperglycemia.”
Tackling the Caveats
The ensuing panel discussion did not fail to deliver in delving into key areas of contention, particularly in terms of GLP-1 treatment.
Regarding a lack of data on the potential long-term effects of GLP-1s: “Yes, there are a huge number of studies [on GLP-1 receptor agonists], but they are, in general, over short periods of time and driven by pharma, who get in and get out as quickly as they can and have little in the way of interest to do comparative effectiveness studies,” Dr. Nathan argued.
“Meanwhile, this is like the crack cocaine of medications — patients have to stay on it for a lifetime or they will regain the weight — are you concerned at all about a lifetime of exposure to GLP-1 [drugs]?” he asked the panel.
Dr. Jastreboff responded that the first GLP-1 receptor agonist medications were approved in 2005, nearly 20 years ago, by the US Food and Drug Administration.
“Do I think we need long-term lifetime data? Absolutely,” she said. “We need to do our due diligence, we need to be careful, we need to monitor patients, and when and if there are signals, we need to follow them.”
What about the notorious gastrointestinal side effects of the drugs? “A majority of them are mitigated by slow up-titration,” Dr. Jastreboff noted.
“If patients have nausea, I do not go up [in dose]. I invite patients to tell me if they’re having vomiting because I don’t want anybody to have it, and I can count on one hand how many of my patients do.”
Dr. Mehta added the concern that as the drugs’ popularity soars, “a lot of doctors don’t know when they need to put the brakes on [weight coming off too quickly].”
She underscored that “we are not treating obesity for weight loss or for cosmetic reasons — this is about optimizing health.”
Dr. Jastreboff noted that in her practice, “I down-titrate if they’re losing weight too quickly.”
“If the patient is losing more than 1% per week of their body weight, then I slow down to make sure they’re getting the nutrients that they need, that they have enough energy to exercise, and that they’re prioritizing protein and fruits and vegetables in their diet.
“We just need to go slow, and yes, we need to follow them long term,” she said.
Chiming in from the audience, Julio Rosenstock, MD, a recognized thought leader in type 2 diabetes, offered his own take on the issues, describing Dr. Taylor’s very low–calorie diet suggestion as “not realistic” and Dr. Nathan’s glucose-first argument to be “stuck in the past.”
Based on modern-day evidence, “there is no reason on earth to start [diabetes treatment] with only metformin,” asserted Dr. Rosenstock, director of the Velocity Clinical Research center at Medical City and clinical professor of medicine at the University of Texas Southwestern Medical Center, Dallas.
“We need to start at the very least with metformin and a sodium-glucose cotransporter 2 (SGLT2) inhibitor from day 1, and then, if it’s affordable and there is access, with a GLP-1 receptor agonist,” he said.
“There is nothing better these days than those agents that consistently have shown a reduction of cardiovascular events and slowing of kidney disease progression.”
Overall, however, “I think you are all right,” he added, a sentiment shared by most.
Noting that the discussion as a whole represents a virtual sea change from the evidence-based options that would have been discussed only a decade ago, Dr. Retnakaran summed up his take-home message: “Stay tuned.
“You could easily see things changing in the next decade to come as we get more data and evidence to support what we ultimately should prioritize an early type 2 diabetes, so this is an exciting time.”
Dr. Retnakaran disclosed ties with Novo Nordisk, Boehringer Ingelheim, Novartis, Sanofi, and Eli Lilly. Dr. Jastreboff disclosed ties with Amgen, AstraZeneca, Boehringer Ingelheim, Biohaven, Eli Lilly, Intellihealth, Novo Nordisk, Pfizer, Regeneron, Scholar Rock, Structure Therapeutics, Terms Pharmaceutical, Weight Watchers, and Zealand Pharmaceuticals. Dr. Roopa had relationships with Novo Nordisk, Boehringer Ingelheim, Amgen, AstraZeneca, Eli Lilly, Silanes, and Sanofi. Dr. Taylor received lecture fees from Novartis, Lilly, Abbott, and Nestle Health and research funding from Diabetes UK and is an advisor to Fast800. Dr. Rosenstock reported relationships with Applied Therapeutics, AstraZeneca, Biomea Fusion, Boehringer Ingelheim, Eli Lilly and Company, Hanmi, Merck, Oramed, Structure Therapeutics, Novartis, Novo Nordisk, Pfizer, Ragor, and Sanofi. Dr. Nathan had no disclosures to report.
A version of this article first appeared on Medscape.com.
ORLANDO, FLORIDA — What to prioritize first in managing early diabetes? That was the question debated on an expert panel at the American Diabetes Association (ADA) 84th Scientific Sessions, with impassioned responses ranging from a plea to “treat obesity first,” to a James Carville–inspired counterpoint of “it’s the glucose, stupid.”
With a focus on preventing complications and inducing remission rounding out the four positions argued,
“In clinical decision-making [for early diabetes], we are faced with weighing each of these variables for the individual patient, and while all are good options, strong arguments can be made for prioritizing each — with the potential of each choice to influence or improve all of the others,” Dr. Retnakaran told this news organization.
Which to Prioritize First?
Making the obesity first argument, Ania M. Jastreboff, MD, PhD, associate professor and director of the Yale Obesity Research Center at Yale School of Medicine, New Haven, Connecticut, noted the striking statistic that nearly 90% of people with type 2 diabetes have overweight or obesity and discussed the ever-expanding data showing the benefits of drugs including glucagon-like peptide 1 (GLP-1) receptor agonists not just in weight loss but also in kidney, cardiovascular, and, as presented at the meeting, sleep apnea improvement.
She contrasted the experiences of two patients with obesity: One treated for the obesity upon type 2 diagnosis — who had a quick normalization of lipids and hypertension soon after the obesity treatment — and the other presenting after 10 years with type 2 diabetes — who was on therapy for hypertension and hyperlipidemia but not for obesity and whose diseases were not as easily treated by that point.
“Why are we treating all the downstream effects and we’re not treating the disease that is potentially the root cause of all these other diseases?” Dr. Jastreboff said.
Complications?
Arguing in favor of focusing on complications, Roopa Mehta, MD, PhD, with the department of endocrinology and metabolism at Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), Mexico City, made the case that stakes don’t get any higher in diabetes than when it comes the looming threat of potentially fatal complications.
Acute myocardial infarction, stroke, amputation, and end-stage renal disease are all on the list of unwanted outcomes and need to be considered even in the earliest stages, as data show early onset type 2 diabetes is linked to life expectancy.
“The main goal of management has always been to prevent complications,” she noted. Citing ADA guidelines, Dr. Mehta underscored the benefits of first- and second-line therapy of metformin, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and GLP-1 receptor agonists for most patients.
Remission?
Discussing the priority of putting patients into disease remission, Roy Taylor, MD, professor of medicine and metabolism at Newcastle University and Newcastle Hospitals NHS in Newcastle upon Tyne, England, and author of the book Life Without Diabetes, focused on an evidence-based alternative to achieving remission — a nonpharmacologic approach that avoids costly and sometimes inaccessible drugs.
In the intervention, described in the DiRECT randomized trial and subsequently in the UK National Health Service Type 2 Diabetes Path to Remission Program, patients with overweight or obesity were placed on a highly restrictive diet of just 800-900 calories a day for 12-20 weeks, followed by maintenance for 12 months, and they not only achieved weight loss but also achieved diabetes remission, in some cases long term.
Acknowledging that “this is not for everyone,” Dr. Taylor asserted that “we have to realize there is a substantial minority of people who want to be healthy but who don’t want to be medicalized,” he said.
“They want their health, and they can do extremely well.”
Glucose?
In taking his self-titled “it’s the glucose, stupid” stand, David M. Nathan, MD, of the Diabetes Center, Massachusetts General Hospital, Harvard Medical School, in Boston, cited extensive evidence showing that early intensive blood glucose control with treatment including sulfonylureas, insulin, or metformin significantly reduced the risk for complications in type 2 diabetes 15 or more years later, including renal failure, blindness, amputation, and myocardial infarctions, in addition to a reduction in diabetes-related death.
“In many of these studies, you saw the benefit even in the setting of weight-gain,” Dr. Nathan underscored.
He further noted the “sobering” findings of the Look AHEAD study, which had to be stopped due to futility when an intensive lifestyle/weight loss intervention showed no significant benefits in terms of cardiovascular disease in people with type 2 diabetes at a median follow-up of 9.6 years.
Ultimately, “diabetes, type 1 and type 2, remains a gluco-centric disease,” Dr. Nathan asserted. “Hyperglycemia is the only universal link between all forms of diabetes and mortality, and the long-term complications of diabetes are intimately associated with hyperglycemia.”
Tackling the Caveats
The ensuing panel discussion did not fail to deliver in delving into key areas of contention, particularly in terms of GLP-1 treatment.
Regarding a lack of data on the potential long-term effects of GLP-1s: “Yes, there are a huge number of studies [on GLP-1 receptor agonists], but they are, in general, over short periods of time and driven by pharma, who get in and get out as quickly as they can and have little in the way of interest to do comparative effectiveness studies,” Dr. Nathan argued.
“Meanwhile, this is like the crack cocaine of medications — patients have to stay on it for a lifetime or they will regain the weight — are you concerned at all about a lifetime of exposure to GLP-1 [drugs]?” he asked the panel.
Dr. Jastreboff responded that the first GLP-1 receptor agonist medications were approved in 2005, nearly 20 years ago, by the US Food and Drug Administration.
“Do I think we need long-term lifetime data? Absolutely,” she said. “We need to do our due diligence, we need to be careful, we need to monitor patients, and when and if there are signals, we need to follow them.”
What about the notorious gastrointestinal side effects of the drugs? “A majority of them are mitigated by slow up-titration,” Dr. Jastreboff noted.
“If patients have nausea, I do not go up [in dose]. I invite patients to tell me if they’re having vomiting because I don’t want anybody to have it, and I can count on one hand how many of my patients do.”
Dr. Mehta added the concern that as the drugs’ popularity soars, “a lot of doctors don’t know when they need to put the brakes on [weight coming off too quickly].”
She underscored that “we are not treating obesity for weight loss or for cosmetic reasons — this is about optimizing health.”
Dr. Jastreboff noted that in her practice, “I down-titrate if they’re losing weight too quickly.”
“If the patient is losing more than 1% per week of their body weight, then I slow down to make sure they’re getting the nutrients that they need, that they have enough energy to exercise, and that they’re prioritizing protein and fruits and vegetables in their diet.
“We just need to go slow, and yes, we need to follow them long term,” she said.
Chiming in from the audience, Julio Rosenstock, MD, a recognized thought leader in type 2 diabetes, offered his own take on the issues, describing Dr. Taylor’s very low–calorie diet suggestion as “not realistic” and Dr. Nathan’s glucose-first argument to be “stuck in the past.”
Based on modern-day evidence, “there is no reason on earth to start [diabetes treatment] with only metformin,” asserted Dr. Rosenstock, director of the Velocity Clinical Research center at Medical City and clinical professor of medicine at the University of Texas Southwestern Medical Center, Dallas.
“We need to start at the very least with metformin and a sodium-glucose cotransporter 2 (SGLT2) inhibitor from day 1, and then, if it’s affordable and there is access, with a GLP-1 receptor agonist,” he said.
“There is nothing better these days than those agents that consistently have shown a reduction of cardiovascular events and slowing of kidney disease progression.”
Overall, however, “I think you are all right,” he added, a sentiment shared by most.
Noting that the discussion as a whole represents a virtual sea change from the evidence-based options that would have been discussed only a decade ago, Dr. Retnakaran summed up his take-home message: “Stay tuned.
“You could easily see things changing in the next decade to come as we get more data and evidence to support what we ultimately should prioritize an early type 2 diabetes, so this is an exciting time.”
Dr. Retnakaran disclosed ties with Novo Nordisk, Boehringer Ingelheim, Novartis, Sanofi, and Eli Lilly. Dr. Jastreboff disclosed ties with Amgen, AstraZeneca, Boehringer Ingelheim, Biohaven, Eli Lilly, Intellihealth, Novo Nordisk, Pfizer, Regeneron, Scholar Rock, Structure Therapeutics, Terms Pharmaceutical, Weight Watchers, and Zealand Pharmaceuticals. Dr. Roopa had relationships with Novo Nordisk, Boehringer Ingelheim, Amgen, AstraZeneca, Eli Lilly, Silanes, and Sanofi. Dr. Taylor received lecture fees from Novartis, Lilly, Abbott, and Nestle Health and research funding from Diabetes UK and is an advisor to Fast800. Dr. Rosenstock reported relationships with Applied Therapeutics, AstraZeneca, Biomea Fusion, Boehringer Ingelheim, Eli Lilly and Company, Hanmi, Merck, Oramed, Structure Therapeutics, Novartis, Novo Nordisk, Pfizer, Ragor, and Sanofi. Dr. Nathan had no disclosures to report.
A version of this article first appeared on Medscape.com.
