User login
Ivosidenib active in R/R IDH1-mutated AML patients
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
FDA grants pembrolizumab accelerated approval for PMBCL
The US Food and Drug Administration (FDA) granted accelerated approval to the anti-PD-1 therapy pembrolizumab (Keytruda) for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL).
The indication also includes patients who have relapsed after 2 or more prior lines of therapy.
Pembrolizumab had received priority review for PMBCL late last year and also has orphan drug designation and breakthrough therapy designation for this indication.
The FDA based its approval on data from the KEYNOTE-170 (NCT02576990 ) trial.
Investigators enrolled 53 patients onto the multicenter, open-label, single-arm trial. Patients received pembrolizumab 200 mg intravenously every 3 weeks until unacceptable toxicity or documented disease progression.
Patients whose disease did not progress received the drug for up to 24 months.
Patient characteristics
Patients were a median age of 33 years (range, 20 – 61), 43% were male, 92% white, 43% had an ECOG performance status of 0, and 57% had an ECOG performance status of 1.
Almost half (49%) had relapsed disease, and 36% had primary refractory disease.
About a quarter (26%) had undergone prior autologous hematopoietic stem cell transplant, and 32% had prior radiation therapy.
All patients had received prior rituximab.
Results
At a median follow-up of 9.7 months, the overall response rate was 45% (24 responders), including 11% complete responses and 34% partial responses.
The median duration of response was not reached during the follow-up period and ranged from a median 1.1 to 19.2 months.
Median time to first objective response was 2.8 months (range, 2.1 – 8.5). Accordingly, investigators do not recommend pembrolizumab for PMBCL patients who require urgent cytoreductive therapy.
Safety
The most common adverse events occurring in 10% or more of patients were musculoskeletal pain (30%), upper respiratory tract infection (28%), pyrexia (28%), fatigue (23%), cough (26%), dyspnea (21%), diarrhea (13%), abdominal pain (13%), nausea (11%), arrhythmia (11%), and headache (11%).
Eight percent of patients discontinued treatment, and 15% interrupted treatment due to adverse reactions.
Adverse events requiring systemic corticosteroid therapy occurred in 25% of patients.
Serious adverse events occurred in 26% and included arrhythmia (4 %), cardiac tamponade (2%), myocardial infarction (2%), pericardial effusion (2%), and pericarditis (2%).
Six (11%) patients died within 30 days of start of treatment.
The recommended pembrolizumab dose for treatment of adults with PMBCL is 200 mg every 3 weeks. The recommended dose in pediatric patients is 2 mg/kg (up to a maximum of 200 mg) every 3 weeks.
Additional indications for pembrolizumab include melanoma, non-small cell lung cancer, head and neck squamous cell cancer, classical Hodgkin lymphoma, urothelial carcinoma, microsatellite instability-high cancer, gastric cancer, and cervical cancer.
The full prescribing information is available on the FDA website.
Pembrolizumab (Keytruda) is a product of Merck & Co, Inc.
The US Food and Drug Administration (FDA) granted accelerated approval to the anti-PD-1 therapy pembrolizumab (Keytruda) for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL).
The indication also includes patients who have relapsed after 2 or more prior lines of therapy.
Pembrolizumab had received priority review for PMBCL late last year and also has orphan drug designation and breakthrough therapy designation for this indication.
The FDA based its approval on data from the KEYNOTE-170 (NCT02576990 ) trial.
Investigators enrolled 53 patients onto the multicenter, open-label, single-arm trial. Patients received pembrolizumab 200 mg intravenously every 3 weeks until unacceptable toxicity or documented disease progression.
Patients whose disease did not progress received the drug for up to 24 months.
Patient characteristics
Patients were a median age of 33 years (range, 20 – 61), 43% were male, 92% white, 43% had an ECOG performance status of 0, and 57% had an ECOG performance status of 1.
Almost half (49%) had relapsed disease, and 36% had primary refractory disease.
About a quarter (26%) had undergone prior autologous hematopoietic stem cell transplant, and 32% had prior radiation therapy.
All patients had received prior rituximab.
Results
At a median follow-up of 9.7 months, the overall response rate was 45% (24 responders), including 11% complete responses and 34% partial responses.
The median duration of response was not reached during the follow-up period and ranged from a median 1.1 to 19.2 months.
Median time to first objective response was 2.8 months (range, 2.1 – 8.5). Accordingly, investigators do not recommend pembrolizumab for PMBCL patients who require urgent cytoreductive therapy.
Safety
The most common adverse events occurring in 10% or more of patients were musculoskeletal pain (30%), upper respiratory tract infection (28%), pyrexia (28%), fatigue (23%), cough (26%), dyspnea (21%), diarrhea (13%), abdominal pain (13%), nausea (11%), arrhythmia (11%), and headache (11%).
Eight percent of patients discontinued treatment, and 15% interrupted treatment due to adverse reactions.
Adverse events requiring systemic corticosteroid therapy occurred in 25% of patients.
Serious adverse events occurred in 26% and included arrhythmia (4 %), cardiac tamponade (2%), myocardial infarction (2%), pericardial effusion (2%), and pericarditis (2%).
Six (11%) patients died within 30 days of start of treatment.
The recommended pembrolizumab dose for treatment of adults with PMBCL is 200 mg every 3 weeks. The recommended dose in pediatric patients is 2 mg/kg (up to a maximum of 200 mg) every 3 weeks.
Additional indications for pembrolizumab include melanoma, non-small cell lung cancer, head and neck squamous cell cancer, classical Hodgkin lymphoma, urothelial carcinoma, microsatellite instability-high cancer, gastric cancer, and cervical cancer.
The full prescribing information is available on the FDA website.
Pembrolizumab (Keytruda) is a product of Merck & Co, Inc.
The US Food and Drug Administration (FDA) granted accelerated approval to the anti-PD-1 therapy pembrolizumab (Keytruda) for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL).
The indication also includes patients who have relapsed after 2 or more prior lines of therapy.
Pembrolizumab had received priority review for PMBCL late last year and also has orphan drug designation and breakthrough therapy designation for this indication.
The FDA based its approval on data from the KEYNOTE-170 (NCT02576990 ) trial.
Investigators enrolled 53 patients onto the multicenter, open-label, single-arm trial. Patients received pembrolizumab 200 mg intravenously every 3 weeks until unacceptable toxicity or documented disease progression.
Patients whose disease did not progress received the drug for up to 24 months.
Patient characteristics
Patients were a median age of 33 years (range, 20 – 61), 43% were male, 92% white, 43% had an ECOG performance status of 0, and 57% had an ECOG performance status of 1.
Almost half (49%) had relapsed disease, and 36% had primary refractory disease.
About a quarter (26%) had undergone prior autologous hematopoietic stem cell transplant, and 32% had prior radiation therapy.
All patients had received prior rituximab.
Results
At a median follow-up of 9.7 months, the overall response rate was 45% (24 responders), including 11% complete responses and 34% partial responses.
The median duration of response was not reached during the follow-up period and ranged from a median 1.1 to 19.2 months.
Median time to first objective response was 2.8 months (range, 2.1 – 8.5). Accordingly, investigators do not recommend pembrolizumab for PMBCL patients who require urgent cytoreductive therapy.
Safety
The most common adverse events occurring in 10% or more of patients were musculoskeletal pain (30%), upper respiratory tract infection (28%), pyrexia (28%), fatigue (23%), cough (26%), dyspnea (21%), diarrhea (13%), abdominal pain (13%), nausea (11%), arrhythmia (11%), and headache (11%).
Eight percent of patients discontinued treatment, and 15% interrupted treatment due to adverse reactions.
Adverse events requiring systemic corticosteroid therapy occurred in 25% of patients.
Serious adverse events occurred in 26% and included arrhythmia (4 %), cardiac tamponade (2%), myocardial infarction (2%), pericardial effusion (2%), and pericarditis (2%).
Six (11%) patients died within 30 days of start of treatment.
The recommended pembrolizumab dose for treatment of adults with PMBCL is 200 mg every 3 weeks. The recommended dose in pediatric patients is 2 mg/kg (up to a maximum of 200 mg) every 3 weeks.
Additional indications for pembrolizumab include melanoma, non-small cell lung cancer, head and neck squamous cell cancer, classical Hodgkin lymphoma, urothelial carcinoma, microsatellite instability-high cancer, gastric cancer, and cervical cancer.
The full prescribing information is available on the FDA website.
Pembrolizumab (Keytruda) is a product of Merck & Co, Inc.
Ibrutinib and venetoclax combo promising in frontline CLL
CHICAGO—Ibrutinib combined with venetoclax is showing promising clinical activity in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to investigators for the CAPTIVATE study.
In the first 30 patients, 77% of treatment-naïve patients had undetected minimal residual disease (MRD; <10-4 cells) in the blood and 86% showed a similar response in the bone marrow.
The overall response rate (ORR) was 100% in 11 evaluable patients. The investigators reported this initial data at the 2018 Annual Meeting of the American Society of Clinical Oncology (abstract 7502).
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” said William G. Wierda, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, who presented the findings at ASCO.
Ibrutinib, a Bruton-kinase inhibitor, has already been approved for the treatment of CLL and venetoclax, a Bcl-2 inhibitor, is currently used to treat relapsed del 17p CLL.
Venetoclax in combination with rituximab was recently approved by the US Food and Drug Administration to treat patients with CLL or small lymphocytic lymphoma whether or not patients have del 17p.
With complementary mechanisms of action and preclinical studies suggesting synergy with the combination, CAPTIVATE was designed to test the efficacy of the oral combination given for 12 cycles.
Study design
CAPTIVATE (NCT02910583) is an ongoing phase 2 study that enrolled 164 patients with treatment-naïve CLL. Patients first received 3 cycles of ibrutinib monotherapy at the standard dose. This was intended to debulk the disease and reduce risk for venetoclax-associated tumor lysis syndrome (TLS).
Venetoclax 400 mg was initiated at cycle 4. After 12 cycles of the combination, patients with confirmed MRD negativity were randomized to receive ibrutinib with a placebo or to continue with the combination therapy.
In this initial report, Dr Wierda highlighted safety data for all 164 enrolled patients and efficacy data for the first 30 patients who had 6 cycles of combination therapy (MRD assessment cohort).
Dr Wierda also reported bone marrow data for the first 14 patients, who received a total of 12 cycles of the combination and represent the safety run-in cohort.
Ibrutinib and venetoclax show promising activity
Median age of patients was 58 years; about 2/3 of patients had unmutated IGHV and 1/3 had a creatine clearance of <80 mL/min.
Of 164 patients, 95% remain on therapy, with discontinuations reported for adverse events; one patient had disease progression to Richter’s transformation.
For the MRD evaluation, all 30 patients had 6 months of combination therapy and continue on treatment.
As expected, lead-in with ibrutinib monotherapy debulked the disease.
Investigators observed a reduction in the proportion of patients at high risk for TLS (24% to 3%) and an increase in the proportion of patients at low risk for TLS (12% to 29%).
A similar picture emerged for debulking of lymph node disease. No patient developed clinical TLS.
Other adverse events were consistent with the safety profile of single-agent ibrutinib and venetoclax. No new safety signals were seen.
After 6 cycles of the combination, blood MRD negativity was reported in 77% of the patients in the MRD assessment cohort.
In the safety-run in cohort of 14 patients, blood MRD negativity was reported in 86% of patients after 12 cycles and 93% of patients after 15 cycles of the combination. In these patients, bone marrow MRD negativity was achieved in 86%.
After 12 cycles of combination therapy, the objective response rate was 100% for 11 of the 14 evaluable patients from the safety run-in cohort: 6 patients showed complete remission (CR) or CR with incomplete blood count recovery (CRi) for a CR/CRi of 55%. All patients had confirmed undetectable MRD.
Investigators considered these responses promising and an assessment of the full treatment plan and durability of response are awaited.
The study was sponsored by Pharmacyclics.
CHICAGO—Ibrutinib combined with venetoclax is showing promising clinical activity in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to investigators for the CAPTIVATE study.
In the first 30 patients, 77% of treatment-naïve patients had undetected minimal residual disease (MRD; <10-4 cells) in the blood and 86% showed a similar response in the bone marrow.
The overall response rate (ORR) was 100% in 11 evaluable patients. The investigators reported this initial data at the 2018 Annual Meeting of the American Society of Clinical Oncology (abstract 7502).
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” said William G. Wierda, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, who presented the findings at ASCO.
Ibrutinib, a Bruton-kinase inhibitor, has already been approved for the treatment of CLL and venetoclax, a Bcl-2 inhibitor, is currently used to treat relapsed del 17p CLL.
Venetoclax in combination with rituximab was recently approved by the US Food and Drug Administration to treat patients with CLL or small lymphocytic lymphoma whether or not patients have del 17p.
With complementary mechanisms of action and preclinical studies suggesting synergy with the combination, CAPTIVATE was designed to test the efficacy of the oral combination given for 12 cycles.
Study design
CAPTIVATE (NCT02910583) is an ongoing phase 2 study that enrolled 164 patients with treatment-naïve CLL. Patients first received 3 cycles of ibrutinib monotherapy at the standard dose. This was intended to debulk the disease and reduce risk for venetoclax-associated tumor lysis syndrome (TLS).
Venetoclax 400 mg was initiated at cycle 4. After 12 cycles of the combination, patients with confirmed MRD negativity were randomized to receive ibrutinib with a placebo or to continue with the combination therapy.
In this initial report, Dr Wierda highlighted safety data for all 164 enrolled patients and efficacy data for the first 30 patients who had 6 cycles of combination therapy (MRD assessment cohort).
Dr Wierda also reported bone marrow data for the first 14 patients, who received a total of 12 cycles of the combination and represent the safety run-in cohort.
Ibrutinib and venetoclax show promising activity
Median age of patients was 58 years; about 2/3 of patients had unmutated IGHV and 1/3 had a creatine clearance of <80 mL/min.
Of 164 patients, 95% remain on therapy, with discontinuations reported for adverse events; one patient had disease progression to Richter’s transformation.
For the MRD evaluation, all 30 patients had 6 months of combination therapy and continue on treatment.
As expected, lead-in with ibrutinib monotherapy debulked the disease.
Investigators observed a reduction in the proportion of patients at high risk for TLS (24% to 3%) and an increase in the proportion of patients at low risk for TLS (12% to 29%).
A similar picture emerged for debulking of lymph node disease. No patient developed clinical TLS.
Other adverse events were consistent with the safety profile of single-agent ibrutinib and venetoclax. No new safety signals were seen.
After 6 cycles of the combination, blood MRD negativity was reported in 77% of the patients in the MRD assessment cohort.
In the safety-run in cohort of 14 patients, blood MRD negativity was reported in 86% of patients after 12 cycles and 93% of patients after 15 cycles of the combination. In these patients, bone marrow MRD negativity was achieved in 86%.
After 12 cycles of combination therapy, the objective response rate was 100% for 11 of the 14 evaluable patients from the safety run-in cohort: 6 patients showed complete remission (CR) or CR with incomplete blood count recovery (CRi) for a CR/CRi of 55%. All patients had confirmed undetectable MRD.
Investigators considered these responses promising and an assessment of the full treatment plan and durability of response are awaited.
The study was sponsored by Pharmacyclics.
CHICAGO—Ibrutinib combined with venetoclax is showing promising clinical activity in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to investigators for the CAPTIVATE study.
In the first 30 patients, 77% of treatment-naïve patients had undetected minimal residual disease (MRD; <10-4 cells) in the blood and 86% showed a similar response in the bone marrow.
The overall response rate (ORR) was 100% in 11 evaluable patients. The investigators reported this initial data at the 2018 Annual Meeting of the American Society of Clinical Oncology (abstract 7502).
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” said William G. Wierda, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, who presented the findings at ASCO.
Ibrutinib, a Bruton-kinase inhibitor, has already been approved for the treatment of CLL and venetoclax, a Bcl-2 inhibitor, is currently used to treat relapsed del 17p CLL.
Venetoclax in combination with rituximab was recently approved by the US Food and Drug Administration to treat patients with CLL or small lymphocytic lymphoma whether or not patients have del 17p.
With complementary mechanisms of action and preclinical studies suggesting synergy with the combination, CAPTIVATE was designed to test the efficacy of the oral combination given for 12 cycles.
Study design
CAPTIVATE (NCT02910583) is an ongoing phase 2 study that enrolled 164 patients with treatment-naïve CLL. Patients first received 3 cycles of ibrutinib monotherapy at the standard dose. This was intended to debulk the disease and reduce risk for venetoclax-associated tumor lysis syndrome (TLS).
Venetoclax 400 mg was initiated at cycle 4. After 12 cycles of the combination, patients with confirmed MRD negativity were randomized to receive ibrutinib with a placebo or to continue with the combination therapy.
In this initial report, Dr Wierda highlighted safety data for all 164 enrolled patients and efficacy data for the first 30 patients who had 6 cycles of combination therapy (MRD assessment cohort).
Dr Wierda also reported bone marrow data for the first 14 patients, who received a total of 12 cycles of the combination and represent the safety run-in cohort.
Ibrutinib and venetoclax show promising activity
Median age of patients was 58 years; about 2/3 of patients had unmutated IGHV and 1/3 had a creatine clearance of <80 mL/min.
Of 164 patients, 95% remain on therapy, with discontinuations reported for adverse events; one patient had disease progression to Richter’s transformation.
For the MRD evaluation, all 30 patients had 6 months of combination therapy and continue on treatment.
As expected, lead-in with ibrutinib monotherapy debulked the disease.
Investigators observed a reduction in the proportion of patients at high risk for TLS (24% to 3%) and an increase in the proportion of patients at low risk for TLS (12% to 29%).
A similar picture emerged for debulking of lymph node disease. No patient developed clinical TLS.
Other adverse events were consistent with the safety profile of single-agent ibrutinib and venetoclax. No new safety signals were seen.
After 6 cycles of the combination, blood MRD negativity was reported in 77% of the patients in the MRD assessment cohort.
In the safety-run in cohort of 14 patients, blood MRD negativity was reported in 86% of patients after 12 cycles and 93% of patients after 15 cycles of the combination. In these patients, bone marrow MRD negativity was achieved in 86%.
After 12 cycles of combination therapy, the objective response rate was 100% for 11 of the 14 evaluable patients from the safety run-in cohort: 6 patients showed complete remission (CR) or CR with incomplete blood count recovery (CRi) for a CR/CRi of 55%. All patients had confirmed undetectable MRD.
Investigators considered these responses promising and an assessment of the full treatment plan and durability of response are awaited.
The study was sponsored by Pharmacyclics.
Mircera approved for anemia in pediatric patients with CKD
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
Chemo-free combo provides potential first-line option for FL
CHICAGO—A chemotherapy-free combination of lenalidomide plus rituximab shows similar efficacy and a different safety profile to chemotherapy plus rituximab (R-chemo) followed by rituximab maintenance in patients with previously untreated follicular lymphoma (FL).
According to investigators, the multicenter, international phase 3 RELEVANCE trial is the first to evaluate the chemo-free combination against the standard of care, R-chemo with rituximab maintenance.
“These results show that lenalidomide plus rituximab, a novel immunomodulatory approach, is a potential first-line option for patients with FL requiring treatment,” said investigator Nathan H. Fowler, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr Fowler presented the results of the study at the 2018 ASCO Annual Meeting (abstract 7500).
The current standard of care in previously untreated symptomatic FL is immunochemotherapy induction followed by rituximab maintenance.
The immunomodulatory agent lenalidomide has complementary mechanisms with rituximab. Phase 2 studies of combined immunotherapy with lenalidomide and rituximab demonstrated 3-year progression-free survival (PFS) of 79%-81% in previously untreated FL, Dr Fowler said.
Phase 3 RELEVANCE trial (NCT01650701)
Investigators evaluated 1030 previously untreated grade 1-3a FL patients who required therapy.
Patients in the lenalidomide-rituximab group (n=513) received lenalidomide doses of 20 mg per day on days 2 to 22 and 28 for 6 to 12 cycles. Responders continued on therapy at 10 mg per day for a total of 18 cycles.
The rituximab dose was 375 mg/m2 weekly in cycle 1 and day 1 in cycles 2 to 6 and continued in responders for 12 additional cycles.
Patients in the R-chemo arm (n=517) received the investigator’s choice of standard rituximab-CHOP, rituximab-bendamustine, or rituximab-CVP, followed by 12 cycles of rituximab.
Most patients (72%) in the R-chemo arm received R-CHOP.
Baseline characteristics were similar in both groups, Dr Fowler said.
Co-primary endpoints were complete remission/complete remission unconfirmed (CR/Cru) at 120 weeks and PFS.
Results
At a median follow-up of 37.9 months, the superiority for lenalidomide and rituximab over rituximab-chemotherapy was not established.
For the lenalidomide-rituximab patients, the CR/Cru was 48% and 3-year PFS was 77% as compared to 53% and 78%, respectively, for rituximab-chemotherapy patients, as assessed by an independent review committee.
Overall survival was 94% in both groups.
Safety
“Important differences in safety profiles were observed between the arms,” Dr Fowler said.
Rituximab-chemotherapy patients had more frequent neutropenia, febrile neutropenia, growth factor usage, nausea, vomiting, neuropathy, and alopecia.
Lenalidomide and rituximab showed more cutaneous reactions, tumor flare, and diarrhea.
Toxicity profiles differed, with higher grade 4 neutropenia (31% vs 8%) and febrile neutropenia (7% vs 2%) with rituximab-chemotherapy compared with lenalidomide-rituximab, respectively.
More patients experienced grade 3/4 cutaneous events (7% vs 1%) with lenalidomide-rituximab.
Second primary malignancies were slightly higher with rituximab-chemotherapy (10%) than with lenalidomide-rituximab (7%). Grade 5 adverse events were 1% in both groups.
About 70% of patients completed treatment in both groups.
“Lenalidomide and rituximab was not superior to rituximab-chemotherapy based on mature CR/Cru at 120 weeks and interim PFS,” Dr Fowler said. “Both treatments showed similar efficacy results. Treatment effects on PFS were consistent across pre-specified subgroups.”
Dr Fowler presented data as of May 31, 2017. Continued follow-up on PFS and OS is ongoing.
The study is sponsored by Celgene Corporation and the Lymphoma Academic Research Organisation (LYSARC).
CHICAGO—A chemotherapy-free combination of lenalidomide plus rituximab shows similar efficacy and a different safety profile to chemotherapy plus rituximab (R-chemo) followed by rituximab maintenance in patients with previously untreated follicular lymphoma (FL).
According to investigators, the multicenter, international phase 3 RELEVANCE trial is the first to evaluate the chemo-free combination against the standard of care, R-chemo with rituximab maintenance.
“These results show that lenalidomide plus rituximab, a novel immunomodulatory approach, is a potential first-line option for patients with FL requiring treatment,” said investigator Nathan H. Fowler, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr Fowler presented the results of the study at the 2018 ASCO Annual Meeting (abstract 7500).
The current standard of care in previously untreated symptomatic FL is immunochemotherapy induction followed by rituximab maintenance.
The immunomodulatory agent lenalidomide has complementary mechanisms with rituximab. Phase 2 studies of combined immunotherapy with lenalidomide and rituximab demonstrated 3-year progression-free survival (PFS) of 79%-81% in previously untreated FL, Dr Fowler said.
Phase 3 RELEVANCE trial (NCT01650701)
Investigators evaluated 1030 previously untreated grade 1-3a FL patients who required therapy.
Patients in the lenalidomide-rituximab group (n=513) received lenalidomide doses of 20 mg per day on days 2 to 22 and 28 for 6 to 12 cycles. Responders continued on therapy at 10 mg per day for a total of 18 cycles.
The rituximab dose was 375 mg/m2 weekly in cycle 1 and day 1 in cycles 2 to 6 and continued in responders for 12 additional cycles.
Patients in the R-chemo arm (n=517) received the investigator’s choice of standard rituximab-CHOP, rituximab-bendamustine, or rituximab-CVP, followed by 12 cycles of rituximab.
Most patients (72%) in the R-chemo arm received R-CHOP.
Baseline characteristics were similar in both groups, Dr Fowler said.
Co-primary endpoints were complete remission/complete remission unconfirmed (CR/Cru) at 120 weeks and PFS.
Results
At a median follow-up of 37.9 months, the superiority for lenalidomide and rituximab over rituximab-chemotherapy was not established.
For the lenalidomide-rituximab patients, the CR/Cru was 48% and 3-year PFS was 77% as compared to 53% and 78%, respectively, for rituximab-chemotherapy patients, as assessed by an independent review committee.
Overall survival was 94% in both groups.
Safety
“Important differences in safety profiles were observed between the arms,” Dr Fowler said.
Rituximab-chemotherapy patients had more frequent neutropenia, febrile neutropenia, growth factor usage, nausea, vomiting, neuropathy, and alopecia.
Lenalidomide and rituximab showed more cutaneous reactions, tumor flare, and diarrhea.
Toxicity profiles differed, with higher grade 4 neutropenia (31% vs 8%) and febrile neutropenia (7% vs 2%) with rituximab-chemotherapy compared with lenalidomide-rituximab, respectively.
More patients experienced grade 3/4 cutaneous events (7% vs 1%) with lenalidomide-rituximab.
Second primary malignancies were slightly higher with rituximab-chemotherapy (10%) than with lenalidomide-rituximab (7%). Grade 5 adverse events were 1% in both groups.
About 70% of patients completed treatment in both groups.
“Lenalidomide and rituximab was not superior to rituximab-chemotherapy based on mature CR/Cru at 120 weeks and interim PFS,” Dr Fowler said. “Both treatments showed similar efficacy results. Treatment effects on PFS were consistent across pre-specified subgroups.”
Dr Fowler presented data as of May 31, 2017. Continued follow-up on PFS and OS is ongoing.
The study is sponsored by Celgene Corporation and the Lymphoma Academic Research Organisation (LYSARC).
CHICAGO—A chemotherapy-free combination of lenalidomide plus rituximab shows similar efficacy and a different safety profile to chemotherapy plus rituximab (R-chemo) followed by rituximab maintenance in patients with previously untreated follicular lymphoma (FL).
According to investigators, the multicenter, international phase 3 RELEVANCE trial is the first to evaluate the chemo-free combination against the standard of care, R-chemo with rituximab maintenance.
“These results show that lenalidomide plus rituximab, a novel immunomodulatory approach, is a potential first-line option for patients with FL requiring treatment,” said investigator Nathan H. Fowler, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr Fowler presented the results of the study at the 2018 ASCO Annual Meeting (abstract 7500).
The current standard of care in previously untreated symptomatic FL is immunochemotherapy induction followed by rituximab maintenance.
The immunomodulatory agent lenalidomide has complementary mechanisms with rituximab. Phase 2 studies of combined immunotherapy with lenalidomide and rituximab demonstrated 3-year progression-free survival (PFS) of 79%-81% in previously untreated FL, Dr Fowler said.
Phase 3 RELEVANCE trial (NCT01650701)
Investigators evaluated 1030 previously untreated grade 1-3a FL patients who required therapy.
Patients in the lenalidomide-rituximab group (n=513) received lenalidomide doses of 20 mg per day on days 2 to 22 and 28 for 6 to 12 cycles. Responders continued on therapy at 10 mg per day for a total of 18 cycles.
The rituximab dose was 375 mg/m2 weekly in cycle 1 and day 1 in cycles 2 to 6 and continued in responders for 12 additional cycles.
Patients in the R-chemo arm (n=517) received the investigator’s choice of standard rituximab-CHOP, rituximab-bendamustine, or rituximab-CVP, followed by 12 cycles of rituximab.
Most patients (72%) in the R-chemo arm received R-CHOP.
Baseline characteristics were similar in both groups, Dr Fowler said.
Co-primary endpoints were complete remission/complete remission unconfirmed (CR/Cru) at 120 weeks and PFS.
Results
At a median follow-up of 37.9 months, the superiority for lenalidomide and rituximab over rituximab-chemotherapy was not established.
For the lenalidomide-rituximab patients, the CR/Cru was 48% and 3-year PFS was 77% as compared to 53% and 78%, respectively, for rituximab-chemotherapy patients, as assessed by an independent review committee.
Overall survival was 94% in both groups.
Safety
“Important differences in safety profiles were observed between the arms,” Dr Fowler said.
Rituximab-chemotherapy patients had more frequent neutropenia, febrile neutropenia, growth factor usage, nausea, vomiting, neuropathy, and alopecia.
Lenalidomide and rituximab showed more cutaneous reactions, tumor flare, and diarrhea.
Toxicity profiles differed, with higher grade 4 neutropenia (31% vs 8%) and febrile neutropenia (7% vs 2%) with rituximab-chemotherapy compared with lenalidomide-rituximab, respectively.
More patients experienced grade 3/4 cutaneous events (7% vs 1%) with lenalidomide-rituximab.
Second primary malignancies were slightly higher with rituximab-chemotherapy (10%) than with lenalidomide-rituximab (7%). Grade 5 adverse events were 1% in both groups.
About 70% of patients completed treatment in both groups.
“Lenalidomide and rituximab was not superior to rituximab-chemotherapy based on mature CR/Cru at 120 weeks and interim PFS,” Dr Fowler said. “Both treatments showed similar efficacy results. Treatment effects on PFS were consistent across pre-specified subgroups.”
Dr Fowler presented data as of May 31, 2017. Continued follow-up on PFS and OS is ongoing.
The study is sponsored by Celgene Corporation and the Lymphoma Academic Research Organisation (LYSARC).
bb2121 demonstrates durable responses, manageable toxicity in MM
CHICAGO—bb2121, the anti-BCMA chimeric antigen receptor (CAR) T-cell therapy, induced deep and durable ongoing responses in heavily pretreated multiple myeloma (MM) patients, updated results of a phase 1 study show.
At active doses (≥150 x 108 CAR+ T cells), the B-cell maturation antigen (BCMA)-targeted therapy produced an overall response rate of 95.5%, including a 50% rate of complete response (CR) or stringent CR, with a median duration of response of 10.8 months.
Median progression-free survival (PFS) was 11.8 months in the dose-escalation cohort.
Noopur S. Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston, reported these results at the 2018 ASCO Annual Meeting (abstract 8007*). The study is sponsored by Celgene Corporation and bluebird bio.
To date, bb2121 has been manageable for patients at doses as high as 800 x 108 CAR T cells, Dr Raje noted.
She updated the findings of CRB-401 (NCT02658929), which included 43 patients with relapsed/refractory MM, including 21 in a dose-escalation (DE) cohort and 22 in a dose-expansion (Exp) cohort.
Patients received one infusion of bb2121 anti-BCMA CAR T cells after a lymphodepleting conditioning regimen including fludarabine and cyclophosphamide.
Patients were a median age of 58 (range, 37 – 74) and 65 (range, 44 – 75) in the DE and Exp cohorts, respectively.
Eight patients (38%) in the DE cohort and 9 (41%) in the Exp cohort had high-risk cytogenetics and had received a median of 7 (range, 3 – 14) and 8 (range, 3 – 23) prior regimens, respectively.
All patients in the DE cohort and 86% in the Exp cohort had a prior autologous stem cell transplant (ASCT), and 29% and 23% in each cohort, respectively, had more than one ASCT.
Results
Patients in the DE cohort had a median PFS of 11.8 months at active doses.
All 16 responding patients who were evaluable for minimal residual disease (MRD) achieved MRD negativity and had a median PFS of 17.7 months.
The investigators observed a dose-response relationship across the active dose ranges and higher peak CAR T expansion in responding patients compared with those who did not respond.
The investigators also noted that the tumor response was independent of tumor BCMA expression.
bb2121 persisted for 6 months or longer in 44% of responding patients.
“This should be tested a little bit earlier now, because what we’ve done here is show the proof of concept, and really treated these very end-stage myeloma patients,” Dr Raje observed.
Adverse events of interest
“We found that this product is extremely well tolerated,” Dr Raje said. “We saw, certainly, cytokine release syndrome (CRS) in over 60% of patients, but most of the CRS was managed, and it was grade 1 and 2 with very little grade 3 CRS. [W]e just had 1 patient with grade 4 neurotoxicity who is now completely recovered.”
The 2 grade 3 CRS events observed in this study resolved in 24 hours, Dr Raje noted.
Infused patients (n=43) also experienced neutropenia (81%), thrombocytopenia (61%), and anemia (56%).
Thirty-one of 40 patients (78%) recovered their absolute neutrophil count to 1000/μL or greater by day 32, and 22 of 40 (55%) patients recovered their platelet counts to 50,000/μL or greater by day 32.
Commentary
BCMA is the “latest promising target” in MM, said Parameswaran Hari, MD, of the Medical College of Wisconsin in Milwaukee, and this bb2121 data represents the largest and most mature experience with the CAR T approach in the disease.
However, patients are still relapsing, and the meaning of MRD negativity is unclear in this setting, Dr Parameswaran said in a presentation referencing the results of the study.
“Unfortunately, this is not yet a cure, so I’m going advise my patients who are in stringent CR and on maintenance not to go for CAR T cells unless they relapse,” he said.
An ongoing global trial of bb2121, known as KarMMa, is open for enrollment in North America and Europe, and additional studies are planned in earlier lines of myeloma.
*Data presented at the meeting differ from the abstract.
CHICAGO—bb2121, the anti-BCMA chimeric antigen receptor (CAR) T-cell therapy, induced deep and durable ongoing responses in heavily pretreated multiple myeloma (MM) patients, updated results of a phase 1 study show.
At active doses (≥150 x 108 CAR+ T cells), the B-cell maturation antigen (BCMA)-targeted therapy produced an overall response rate of 95.5%, including a 50% rate of complete response (CR) or stringent CR, with a median duration of response of 10.8 months.
Median progression-free survival (PFS) was 11.8 months in the dose-escalation cohort.
Noopur S. Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston, reported these results at the 2018 ASCO Annual Meeting (abstract 8007*). The study is sponsored by Celgene Corporation and bluebird bio.
To date, bb2121 has been manageable for patients at doses as high as 800 x 108 CAR T cells, Dr Raje noted.
She updated the findings of CRB-401 (NCT02658929), which included 43 patients with relapsed/refractory MM, including 21 in a dose-escalation (DE) cohort and 22 in a dose-expansion (Exp) cohort.
Patients received one infusion of bb2121 anti-BCMA CAR T cells after a lymphodepleting conditioning regimen including fludarabine and cyclophosphamide.
Patients were a median age of 58 (range, 37 – 74) and 65 (range, 44 – 75) in the DE and Exp cohorts, respectively.
Eight patients (38%) in the DE cohort and 9 (41%) in the Exp cohort had high-risk cytogenetics and had received a median of 7 (range, 3 – 14) and 8 (range, 3 – 23) prior regimens, respectively.
All patients in the DE cohort and 86% in the Exp cohort had a prior autologous stem cell transplant (ASCT), and 29% and 23% in each cohort, respectively, had more than one ASCT.
Results
Patients in the DE cohort had a median PFS of 11.8 months at active doses.
All 16 responding patients who were evaluable for minimal residual disease (MRD) achieved MRD negativity and had a median PFS of 17.7 months.
The investigators observed a dose-response relationship across the active dose ranges and higher peak CAR T expansion in responding patients compared with those who did not respond.
The investigators also noted that the tumor response was independent of tumor BCMA expression.
bb2121 persisted for 6 months or longer in 44% of responding patients.
“This should be tested a little bit earlier now, because what we’ve done here is show the proof of concept, and really treated these very end-stage myeloma patients,” Dr Raje observed.
Adverse events of interest
“We found that this product is extremely well tolerated,” Dr Raje said. “We saw, certainly, cytokine release syndrome (CRS) in over 60% of patients, but most of the CRS was managed, and it was grade 1 and 2 with very little grade 3 CRS. [W]e just had 1 patient with grade 4 neurotoxicity who is now completely recovered.”
The 2 grade 3 CRS events observed in this study resolved in 24 hours, Dr Raje noted.
Infused patients (n=43) also experienced neutropenia (81%), thrombocytopenia (61%), and anemia (56%).
Thirty-one of 40 patients (78%) recovered their absolute neutrophil count to 1000/μL or greater by day 32, and 22 of 40 (55%) patients recovered their platelet counts to 50,000/μL or greater by day 32.
Commentary
BCMA is the “latest promising target” in MM, said Parameswaran Hari, MD, of the Medical College of Wisconsin in Milwaukee, and this bb2121 data represents the largest and most mature experience with the CAR T approach in the disease.
However, patients are still relapsing, and the meaning of MRD negativity is unclear in this setting, Dr Parameswaran said in a presentation referencing the results of the study.
“Unfortunately, this is not yet a cure, so I’m going advise my patients who are in stringent CR and on maintenance not to go for CAR T cells unless they relapse,” he said.
An ongoing global trial of bb2121, known as KarMMa, is open for enrollment in North America and Europe, and additional studies are planned in earlier lines of myeloma.
*Data presented at the meeting differ from the abstract.
CHICAGO—bb2121, the anti-BCMA chimeric antigen receptor (CAR) T-cell therapy, induced deep and durable ongoing responses in heavily pretreated multiple myeloma (MM) patients, updated results of a phase 1 study show.
At active doses (≥150 x 108 CAR+ T cells), the B-cell maturation antigen (BCMA)-targeted therapy produced an overall response rate of 95.5%, including a 50% rate of complete response (CR) or stringent CR, with a median duration of response of 10.8 months.
Median progression-free survival (PFS) was 11.8 months in the dose-escalation cohort.
Noopur S. Raje, MD, of the Massachusetts General Hospital Cancer Center in Boston, reported these results at the 2018 ASCO Annual Meeting (abstract 8007*). The study is sponsored by Celgene Corporation and bluebird bio.
To date, bb2121 has been manageable for patients at doses as high as 800 x 108 CAR T cells, Dr Raje noted.
She updated the findings of CRB-401 (NCT02658929), which included 43 patients with relapsed/refractory MM, including 21 in a dose-escalation (DE) cohort and 22 in a dose-expansion (Exp) cohort.
Patients received one infusion of bb2121 anti-BCMA CAR T cells after a lymphodepleting conditioning regimen including fludarabine and cyclophosphamide.
Patients were a median age of 58 (range, 37 – 74) and 65 (range, 44 – 75) in the DE and Exp cohorts, respectively.
Eight patients (38%) in the DE cohort and 9 (41%) in the Exp cohort had high-risk cytogenetics and had received a median of 7 (range, 3 – 14) and 8 (range, 3 – 23) prior regimens, respectively.
All patients in the DE cohort and 86% in the Exp cohort had a prior autologous stem cell transplant (ASCT), and 29% and 23% in each cohort, respectively, had more than one ASCT.
Results
Patients in the DE cohort had a median PFS of 11.8 months at active doses.
All 16 responding patients who were evaluable for minimal residual disease (MRD) achieved MRD negativity and had a median PFS of 17.7 months.
The investigators observed a dose-response relationship across the active dose ranges and higher peak CAR T expansion in responding patients compared with those who did not respond.
The investigators also noted that the tumor response was independent of tumor BCMA expression.
bb2121 persisted for 6 months or longer in 44% of responding patients.
“This should be tested a little bit earlier now, because what we’ve done here is show the proof of concept, and really treated these very end-stage myeloma patients,” Dr Raje observed.
Adverse events of interest
“We found that this product is extremely well tolerated,” Dr Raje said. “We saw, certainly, cytokine release syndrome (CRS) in over 60% of patients, but most of the CRS was managed, and it was grade 1 and 2 with very little grade 3 CRS. [W]e just had 1 patient with grade 4 neurotoxicity who is now completely recovered.”
The 2 grade 3 CRS events observed in this study resolved in 24 hours, Dr Raje noted.
Infused patients (n=43) also experienced neutropenia (81%), thrombocytopenia (61%), and anemia (56%).
Thirty-one of 40 patients (78%) recovered their absolute neutrophil count to 1000/μL or greater by day 32, and 22 of 40 (55%) patients recovered their platelet counts to 50,000/μL or greater by day 32.
Commentary
BCMA is the “latest promising target” in MM, said Parameswaran Hari, MD, of the Medical College of Wisconsin in Milwaukee, and this bb2121 data represents the largest and most mature experience with the CAR T approach in the disease.
However, patients are still relapsing, and the meaning of MRD negativity is unclear in this setting, Dr Parameswaran said in a presentation referencing the results of the study.
“Unfortunately, this is not yet a cure, so I’m going advise my patients who are in stringent CR and on maintenance not to go for CAR T cells unless they relapse,” he said.
An ongoing global trial of bb2121, known as KarMMa, is open for enrollment in North America and Europe, and additional studies are planned in earlier lines of myeloma.
*Data presented at the meeting differ from the abstract.
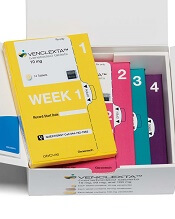
FDA approves venetoclax for CLL/SLL with or without del 17p
The US Food and Drug Administration (FDA) has approved venetoclax tablets (Venclexta ®) in combination with rituximab to treat patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who have received 1 prior therapy.
The combination is approved for patients with or without deletion of 17p (del 17p).
The FDA based its approval on the phase 3 MURANO trial, in which venetoclax in combination with rituximab (VEN+R) significantly improved progression-free survival (PFS) in relapsed or refractory CLL patients compared to the chemoimmunotherapy regimen of bendamustine plus rituximab(B+R).
This approval, according to the drug’s developers, makes venetoclax plus rituximab the first oral-based, chemotherapy-free combination with a fixed treatment duration for CLL.
The FDA has also converted venetoclax's accelerated approval to a full approval. The drug was previously granted accelerated approval as a single agent for the treatment of people with CLL with 17p deletion.
Venetoclax is being developed by AbbVie and Roche and jointly commercialized by AbbVie and Genentech in the US and by AbbVie outside the US.
Phase 3 MURANO trial (NCT02005471)
The multicenter, open-label trial randomized 389 patients to VEN+R (194 patients) or B+R (195 patients). Median age of the patients was 65 years (range, 22 – 85).
Patients in the VEN+R arm completed a 5-week ramp-up of venetoclax followed by venetoclax 400 mg once daily for 24 months measured from the rituximab start date.
Tumor lysis syndrome (TLS), caused by a rapid reduction in tumor volume, is an identified risk with venetoclax treatment. The dose ramp-up was intended to mitigate this risk.
Rituximab was initiated after venetoclax ramp-up and given for 6 cycles (375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 intravenously on day 1 of cycles 2-6, with a 28-day cycle length).
Patients in the B+R arm received 6 cycles of B+R (bendamustine 70 mg/m2 on days 1 and 2 of each 28-day cycle and rituximab at the above described dose and schedule).
Efficacy was based on PFS as assessed by an independent review committee.
After a median follow-up of 23 months, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (P<0.0001).
The overall response rate was 92% for patients treated with VEN+R compared to 72% for those treated with B+R.
Safety
The most common adverse events (AEs) in the VEN+R arms that occurred in 20% or more patients were neutropenia (65%), diarrhea (40%), upper respiratory tract infection (39%), fatigue (22%), cough (22%), and nausea (21%).
Grade 3 or 4 neutropenia developed in 64% of patients, and grade 4 neutropenia in 31%.
Serious adverse events (SAEs) developed in 46% of patients and serious infections in 21%, consisting most frequently of pneumonia (9%).
The incidence of TLS was 3%, occurring in 6 of 194 patients.
In the VEN+R arm, discontinuations due to any AEs occurred in 16% of patients, dose reductions in 15%, and dose interruptions in 71%.
Neutropenia led to dose interruptions in 46% of patients and discontinuations in 3%. Thrombocytopenia led to discontinuations in 3% of patients.
Fatal AEs that occurred in the absence of disease progression and within 30 days of the last VEN+R treatment and/or 90 days of the last rituximab infusion were reported in 2% (4/194) of patients.
In the B+R arm, AEs led to treatment discontinuations in 10% of patients, dose reductions in 15%, and dose interruptions in 40 %.
Investigators previously reported data from the phase 3 MURANO study as a late-breaking abstract at the 2017 ASH Annual Meeting and published the findings in NEJM.
John Seymour, MBBS, PhD, lead investigator of the MURANO study, said in the corporate release, the approval "validates the results seen in the phase 3 trial, including the significant improvement in progression-free survival over a standard of care comparator arm."
"Progression-free survival is considered a gold standard for demonstrating clinical benefit in oncology," he added.
Full prescribing information for venetoclax is available here.
The US Food and Drug Administration (FDA) has approved venetoclax tablets (Venclexta ®) in combination with rituximab to treat patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who have received 1 prior therapy.
The combination is approved for patients with or without deletion of 17p (del 17p).
The FDA based its approval on the phase 3 MURANO trial, in which venetoclax in combination with rituximab (VEN+R) significantly improved progression-free survival (PFS) in relapsed or refractory CLL patients compared to the chemoimmunotherapy regimen of bendamustine plus rituximab(B+R).
This approval, according to the drug’s developers, makes venetoclax plus rituximab the first oral-based, chemotherapy-free combination with a fixed treatment duration for CLL.
The FDA has also converted venetoclax's accelerated approval to a full approval. The drug was previously granted accelerated approval as a single agent for the treatment of people with CLL with 17p deletion.
Venetoclax is being developed by AbbVie and Roche and jointly commercialized by AbbVie and Genentech in the US and by AbbVie outside the US.
Phase 3 MURANO trial (NCT02005471)
The multicenter, open-label trial randomized 389 patients to VEN+R (194 patients) or B+R (195 patients). Median age of the patients was 65 years (range, 22 – 85).
Patients in the VEN+R arm completed a 5-week ramp-up of venetoclax followed by venetoclax 400 mg once daily for 24 months measured from the rituximab start date.
Tumor lysis syndrome (TLS), caused by a rapid reduction in tumor volume, is an identified risk with venetoclax treatment. The dose ramp-up was intended to mitigate this risk.
Rituximab was initiated after venetoclax ramp-up and given for 6 cycles (375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 intravenously on day 1 of cycles 2-6, with a 28-day cycle length).
Patients in the B+R arm received 6 cycles of B+R (bendamustine 70 mg/m2 on days 1 and 2 of each 28-day cycle and rituximab at the above described dose and schedule).
Efficacy was based on PFS as assessed by an independent review committee.
After a median follow-up of 23 months, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (P<0.0001).
The overall response rate was 92% for patients treated with VEN+R compared to 72% for those treated with B+R.
Safety
The most common adverse events (AEs) in the VEN+R arms that occurred in 20% or more patients were neutropenia (65%), diarrhea (40%), upper respiratory tract infection (39%), fatigue (22%), cough (22%), and nausea (21%).
Grade 3 or 4 neutropenia developed in 64% of patients, and grade 4 neutropenia in 31%.
Serious adverse events (SAEs) developed in 46% of patients and serious infections in 21%, consisting most frequently of pneumonia (9%).
The incidence of TLS was 3%, occurring in 6 of 194 patients.
In the VEN+R arm, discontinuations due to any AEs occurred in 16% of patients, dose reductions in 15%, and dose interruptions in 71%.
Neutropenia led to dose interruptions in 46% of patients and discontinuations in 3%. Thrombocytopenia led to discontinuations in 3% of patients.
Fatal AEs that occurred in the absence of disease progression and within 30 days of the last VEN+R treatment and/or 90 days of the last rituximab infusion were reported in 2% (4/194) of patients.
In the B+R arm, AEs led to treatment discontinuations in 10% of patients, dose reductions in 15%, and dose interruptions in 40 %.
Investigators previously reported data from the phase 3 MURANO study as a late-breaking abstract at the 2017 ASH Annual Meeting and published the findings in NEJM.
John Seymour, MBBS, PhD, lead investigator of the MURANO study, said in the corporate release, the approval "validates the results seen in the phase 3 trial, including the significant improvement in progression-free survival over a standard of care comparator arm."
"Progression-free survival is considered a gold standard for demonstrating clinical benefit in oncology," he added.
Full prescribing information for venetoclax is available here.
The US Food and Drug Administration (FDA) has approved venetoclax tablets (Venclexta ®) in combination with rituximab to treat patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who have received 1 prior therapy.
The combination is approved for patients with or without deletion of 17p (del 17p).
The FDA based its approval on the phase 3 MURANO trial, in which venetoclax in combination with rituximab (VEN+R) significantly improved progression-free survival (PFS) in relapsed or refractory CLL patients compared to the chemoimmunotherapy regimen of bendamustine plus rituximab(B+R).
This approval, according to the drug’s developers, makes venetoclax plus rituximab the first oral-based, chemotherapy-free combination with a fixed treatment duration for CLL.
The FDA has also converted venetoclax's accelerated approval to a full approval. The drug was previously granted accelerated approval as a single agent for the treatment of people with CLL with 17p deletion.
Venetoclax is being developed by AbbVie and Roche and jointly commercialized by AbbVie and Genentech in the US and by AbbVie outside the US.
Phase 3 MURANO trial (NCT02005471)
The multicenter, open-label trial randomized 389 patients to VEN+R (194 patients) or B+R (195 patients). Median age of the patients was 65 years (range, 22 – 85).
Patients in the VEN+R arm completed a 5-week ramp-up of venetoclax followed by venetoclax 400 mg once daily for 24 months measured from the rituximab start date.
Tumor lysis syndrome (TLS), caused by a rapid reduction in tumor volume, is an identified risk with venetoclax treatment. The dose ramp-up was intended to mitigate this risk.
Rituximab was initiated after venetoclax ramp-up and given for 6 cycles (375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 intravenously on day 1 of cycles 2-6, with a 28-day cycle length).
Patients in the B+R arm received 6 cycles of B+R (bendamustine 70 mg/m2 on days 1 and 2 of each 28-day cycle and rituximab at the above described dose and schedule).
Efficacy was based on PFS as assessed by an independent review committee.
After a median follow-up of 23 months, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (P<0.0001).
The overall response rate was 92% for patients treated with VEN+R compared to 72% for those treated with B+R.
Safety
The most common adverse events (AEs) in the VEN+R arms that occurred in 20% or more patients were neutropenia (65%), diarrhea (40%), upper respiratory tract infection (39%), fatigue (22%), cough (22%), and nausea (21%).
Grade 3 or 4 neutropenia developed in 64% of patients, and grade 4 neutropenia in 31%.
Serious adverse events (SAEs) developed in 46% of patients and serious infections in 21%, consisting most frequently of pneumonia (9%).
The incidence of TLS was 3%, occurring in 6 of 194 patients.
In the VEN+R arm, discontinuations due to any AEs occurred in 16% of patients, dose reductions in 15%, and dose interruptions in 71%.
Neutropenia led to dose interruptions in 46% of patients and discontinuations in 3%. Thrombocytopenia led to discontinuations in 3% of patients.
Fatal AEs that occurred in the absence of disease progression and within 30 days of the last VEN+R treatment and/or 90 days of the last rituximab infusion were reported in 2% (4/194) of patients.
In the B+R arm, AEs led to treatment discontinuations in 10% of patients, dose reductions in 15%, and dose interruptions in 40 %.
Investigators previously reported data from the phase 3 MURANO study as a late-breaking abstract at the 2017 ASH Annual Meeting and published the findings in NEJM.
John Seymour, MBBS, PhD, lead investigator of the MURANO study, said in the corporate release, the approval "validates the results seen in the phase 3 trial, including the significant improvement in progression-free survival over a standard of care comparator arm."
"Progression-free survival is considered a gold standard for demonstrating clinical benefit in oncology," he added.
Full prescribing information for venetoclax is available here.
Dasatinib outcomes similar to imatinib in pediatric Ph+ ALL
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Pomalidomide triplet significantly extends PFS in R/R MM
CHICAGO—The addition of pomalidomide to bortezomib and low‐dose dexamethasone (PVd) significantly improves progression-free survival (PFS) in lenalidomide-exposed patients with relapsed or refractory (R/R) multiple myeloma (MM), a new study reveals.
Up until now, pomalidomide and dexamethasone (Pd) had been the only therapy investigated exclusively after lenalidomide therapy, according to Paul G. Richardson, MD.
Now, he said, “a triple combination of PVd demonstrated promising activity in early phase clinical trials of lenalidomide-refractory patients.”
Dr Richardson, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presented the findings of the phase 3 OPTIMISMM trial (abstract 8001) at the 2018 ASCO Annual Meeting.
The oral immunomodulatory agent pomalidomide, a standard-of-care treatment in R/R MM, has demonstrated synergistic anti-myeloma activity with dexamethasone and proteasome inhibitors.
A combination of pomalidomide and dexamethasone is indicated for MM patients after 2 or more prior therapies, including lenalidomide and a proteasome inhibitor.
“Lenalidomide is an established therapy in newly diagnosed multiple myeloma,” Dr Richardson explained. “Therefore, patients for whom lenalidomide is no longer a treatment option represent a clinically relevant population with unmet need.”
Phase 3 OPTIMISMM trial (NCT01734928)
Dr Richardson reported the final PFS and safety data from the first phase 3 pomalidomide triplet trial comparing PVd against bortezomib and dexamethasone (Vd) in an entirely post-lenalidomide treated population.
The 559 patients had 1 to 3 prior lines of therapy and 2 or more cycles of prior lenalidomide. They were randomized to receive PVd (281 patients, median age 67 years) or Vd (278 patients, median age 68 years).
In 21-day cycles, patients received pomalidomide 4 mg per day on days 1-14 (PVd arm only); bortezomib 1.3 mg/m² on days 1, 4, 8, and 11 of cycles 1-8 and on day 1 and 8 of cycles 9 and higher; and dexamethasone 20 mg per day (10 mg for those over age 75) on the days of and after bortezomib.
The primary endpoint was PFS.
Results
After a median follow-up of 16 months, “PVd reduced the risk of progression or death by 39% compared with Vd,” Dr Richardson said.
Median PFS was 11.2 months in the PVd group and 7.1 months in the Vd group. Overall survival data are not mature.
The overall response rate was significantly higher with PVd (82.2%) vs Vd (50%).
And the overall response rate was even higher in patients with only 1 prior line of therapy (90.1% vs 54.8%, respectively).
“PVd led to deeper responses with higher stringent complete response/complete response and more very good partial responses than Vd,” Dr Richardson noted.
“PFS was improved with PVd vs Vd across patient subgroups and regardless of lenalidomide refractoriness. The PFS benefit with PVd was maintained through the next line of therapy.”
He reported longer treatment duration and exposure with PVd compared with Vd.
Safety
The safety profile was consistent with known toxicities associated with pomalidomide and low-dose dexamethasone, he said.
Most common grade 3/4 treatment-emergent adverse events were higher with PVd than Vd, including neutropenia (42% vs 9%) and infections (31% vs 18%).
In conclusion, Dr Richardson said, “These results support the use of PVd in first relapse in patients with relapsed/refractory multiple myeloma and prior exposure to lenalidomide.”
Future analyses of the data will include correlatives, minimal residual disease, and quality of life, he said.
The trial was sponsored by Celgene.
CHICAGO—The addition of pomalidomide to bortezomib and low‐dose dexamethasone (PVd) significantly improves progression-free survival (PFS) in lenalidomide-exposed patients with relapsed or refractory (R/R) multiple myeloma (MM), a new study reveals.
Up until now, pomalidomide and dexamethasone (Pd) had been the only therapy investigated exclusively after lenalidomide therapy, according to Paul G. Richardson, MD.
Now, he said, “a triple combination of PVd demonstrated promising activity in early phase clinical trials of lenalidomide-refractory patients.”
Dr Richardson, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presented the findings of the phase 3 OPTIMISMM trial (abstract 8001) at the 2018 ASCO Annual Meeting.
The oral immunomodulatory agent pomalidomide, a standard-of-care treatment in R/R MM, has demonstrated synergistic anti-myeloma activity with dexamethasone and proteasome inhibitors.
A combination of pomalidomide and dexamethasone is indicated for MM patients after 2 or more prior therapies, including lenalidomide and a proteasome inhibitor.
“Lenalidomide is an established therapy in newly diagnosed multiple myeloma,” Dr Richardson explained. “Therefore, patients for whom lenalidomide is no longer a treatment option represent a clinically relevant population with unmet need.”
Phase 3 OPTIMISMM trial (NCT01734928)
Dr Richardson reported the final PFS and safety data from the first phase 3 pomalidomide triplet trial comparing PVd against bortezomib and dexamethasone (Vd) in an entirely post-lenalidomide treated population.
The 559 patients had 1 to 3 prior lines of therapy and 2 or more cycles of prior lenalidomide. They were randomized to receive PVd (281 patients, median age 67 years) or Vd (278 patients, median age 68 years).
In 21-day cycles, patients received pomalidomide 4 mg per day on days 1-14 (PVd arm only); bortezomib 1.3 mg/m² on days 1, 4, 8, and 11 of cycles 1-8 and on day 1 and 8 of cycles 9 and higher; and dexamethasone 20 mg per day (10 mg for those over age 75) on the days of and after bortezomib.
The primary endpoint was PFS.
Results
After a median follow-up of 16 months, “PVd reduced the risk of progression or death by 39% compared with Vd,” Dr Richardson said.
Median PFS was 11.2 months in the PVd group and 7.1 months in the Vd group. Overall survival data are not mature.
The overall response rate was significantly higher with PVd (82.2%) vs Vd (50%).
And the overall response rate was even higher in patients with only 1 prior line of therapy (90.1% vs 54.8%, respectively).
“PVd led to deeper responses with higher stringent complete response/complete response and more very good partial responses than Vd,” Dr Richardson noted.
“PFS was improved with PVd vs Vd across patient subgroups and regardless of lenalidomide refractoriness. The PFS benefit with PVd was maintained through the next line of therapy.”
He reported longer treatment duration and exposure with PVd compared with Vd.
Safety
The safety profile was consistent with known toxicities associated with pomalidomide and low-dose dexamethasone, he said.
Most common grade 3/4 treatment-emergent adverse events were higher with PVd than Vd, including neutropenia (42% vs 9%) and infections (31% vs 18%).
In conclusion, Dr Richardson said, “These results support the use of PVd in first relapse in patients with relapsed/refractory multiple myeloma and prior exposure to lenalidomide.”
Future analyses of the data will include correlatives, minimal residual disease, and quality of life, he said.
The trial was sponsored by Celgene.
CHICAGO—The addition of pomalidomide to bortezomib and low‐dose dexamethasone (PVd) significantly improves progression-free survival (PFS) in lenalidomide-exposed patients with relapsed or refractory (R/R) multiple myeloma (MM), a new study reveals.
Up until now, pomalidomide and dexamethasone (Pd) had been the only therapy investigated exclusively after lenalidomide therapy, according to Paul G. Richardson, MD.
Now, he said, “a triple combination of PVd demonstrated promising activity in early phase clinical trials of lenalidomide-refractory patients.”
Dr Richardson, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presented the findings of the phase 3 OPTIMISMM trial (abstract 8001) at the 2018 ASCO Annual Meeting.
The oral immunomodulatory agent pomalidomide, a standard-of-care treatment in R/R MM, has demonstrated synergistic anti-myeloma activity with dexamethasone and proteasome inhibitors.
A combination of pomalidomide and dexamethasone is indicated for MM patients after 2 or more prior therapies, including lenalidomide and a proteasome inhibitor.
“Lenalidomide is an established therapy in newly diagnosed multiple myeloma,” Dr Richardson explained. “Therefore, patients for whom lenalidomide is no longer a treatment option represent a clinically relevant population with unmet need.”
Phase 3 OPTIMISMM trial (NCT01734928)
Dr Richardson reported the final PFS and safety data from the first phase 3 pomalidomide triplet trial comparing PVd against bortezomib and dexamethasone (Vd) in an entirely post-lenalidomide treated population.
The 559 patients had 1 to 3 prior lines of therapy and 2 or more cycles of prior lenalidomide. They were randomized to receive PVd (281 patients, median age 67 years) or Vd (278 patients, median age 68 years).
In 21-day cycles, patients received pomalidomide 4 mg per day on days 1-14 (PVd arm only); bortezomib 1.3 mg/m² on days 1, 4, 8, and 11 of cycles 1-8 and on day 1 and 8 of cycles 9 and higher; and dexamethasone 20 mg per day (10 mg for those over age 75) on the days of and after bortezomib.
The primary endpoint was PFS.
Results
After a median follow-up of 16 months, “PVd reduced the risk of progression or death by 39% compared with Vd,” Dr Richardson said.
Median PFS was 11.2 months in the PVd group and 7.1 months in the Vd group. Overall survival data are not mature.
The overall response rate was significantly higher with PVd (82.2%) vs Vd (50%).
And the overall response rate was even higher in patients with only 1 prior line of therapy (90.1% vs 54.8%, respectively).
“PVd led to deeper responses with higher stringent complete response/complete response and more very good partial responses than Vd,” Dr Richardson noted.
“PFS was improved with PVd vs Vd across patient subgroups and regardless of lenalidomide refractoriness. The PFS benefit with PVd was maintained through the next line of therapy.”
He reported longer treatment duration and exposure with PVd compared with Vd.
Safety
The safety profile was consistent with known toxicities associated with pomalidomide and low-dose dexamethasone, he said.
Most common grade 3/4 treatment-emergent adverse events were higher with PVd than Vd, including neutropenia (42% vs 9%) and infections (31% vs 18%).
In conclusion, Dr Richardson said, “These results support the use of PVd in first relapse in patients with relapsed/refractory multiple myeloma and prior exposure to lenalidomide.”
Future analyses of the data will include correlatives, minimal residual disease, and quality of life, he said.
The trial was sponsored by Celgene.
Polatuzumab plus BR improves efficacy in DLBCL
CHICAGO—Polatuzumab vedotin, when added to bendamustine (B) and rituximab (R), significantly improved response and survival rates in a cohort of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a phase 2 study.
By contrast, there were no such improvements in a cohort of follicular lymphoma (FL) patients, at least in short-term follow-up, investigator Laurie Helen Sehn, MD, of the BC Cancer Agency in Vancouver, Canada, said at the 2018 ASCO Annual Meeting.
However, the improvement in overall survival in DLBCL patients is “remarkable,” Dr Sehn affirmed in an oral presentation (abstract 7507).
“Based on these encouraging results, polatuzumab vedotin has received breakthrough therapy designation and priority medicines designation by the FDA and EMA for patients with relapsed or refractory DLBCL,” she said.
Polatuzumab-BR study (NCT02257567)
The study by Dr Sehn and colleagues included a cohort of 80 DLBCL patients randomized to BR or polatuzumab-BR for 6 planned 21-day cycles.
Investigators randomized another cohort of 80 FL patients to BR or polatuzumab-BR for 6 planned 28-day cycles.
The primary endpoint was complete response (CR) assessed by fluorodeoxyglucose positron emission tomography (FDG-PET) at 6 to 8 weeks after the end of treatment.
DLBCL patients
A total of 40% of polatuzumab-BR-treated DLBCL patients achieved CR at the end of treatment, versus 15% of BR-treated patients (P=0.012).
That CR improvement translated into a significantly higher progression-free survival (PFS) (6.7 months for polatuzumab-BR vs 2.0 months for BR, P<0.0001) and overall survival (11.8 months versus 4.7 months, P=0.0008), according to Dr Sehn.
The FDG-PET CR rates were higher in the polatuzumab-BR arm regardless of the number of prior lines of treatment for DLBCL, and regardless of relapsed versus refractory status, Dr. Sehn added.
FL patients
By contrast, in the FL cohort, the FDG-PET CR rate was high for both arms, at 69% for polatuzumab-BR and 63% for BR.
And there was no significant difference in progression-free survival (P=0.58) with “relatively short-term follow-up,” she said.
Adverse events
The most common grades 3 – 5 adverse events for both DLBCL and FL patients were higher in the polatuzumab-BR arm than the BR arm and included cytopenias, febrile neutropenia, and infections.
Serious AEs were also higher in the polatuzumab-BR arm and included febrile neutropenia for both FL and DLBCL patients and infection for FL patients.
Five percent of FL patients and 18% of DLBCL had a grade 5 event.
Commentary
Whether polatuzumab vedotin will change treatment paradigms for DLBCL patients may be answered by the ongoing POLARIX study, according to Alison Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, NY.
The randomized phase 3 POLARIX study (abstract TPS7589) is comparing polatuzumab plus R-CHP to R-CHOP in patients with previously untreated DLBCL.
“Certainly, there are patients who do very well with R-CHOP chemotherapy alone, and so we need to learn whether this is necessary for all patients, or only the high-risk patients,” Dr Moskowitz said in a talk at ASCO commenting on the results of the polatuzumab-BR study.
Hoffman-LaRoche is the sponsor of the study.
CHICAGO—Polatuzumab vedotin, when added to bendamustine (B) and rituximab (R), significantly improved response and survival rates in a cohort of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a phase 2 study.
By contrast, there were no such improvements in a cohort of follicular lymphoma (FL) patients, at least in short-term follow-up, investigator Laurie Helen Sehn, MD, of the BC Cancer Agency in Vancouver, Canada, said at the 2018 ASCO Annual Meeting.
However, the improvement in overall survival in DLBCL patients is “remarkable,” Dr Sehn affirmed in an oral presentation (abstract 7507).
“Based on these encouraging results, polatuzumab vedotin has received breakthrough therapy designation and priority medicines designation by the FDA and EMA for patients with relapsed or refractory DLBCL,” she said.
Polatuzumab-BR study (NCT02257567)
The study by Dr Sehn and colleagues included a cohort of 80 DLBCL patients randomized to BR or polatuzumab-BR for 6 planned 21-day cycles.
Investigators randomized another cohort of 80 FL patients to BR or polatuzumab-BR for 6 planned 28-day cycles.
The primary endpoint was complete response (CR) assessed by fluorodeoxyglucose positron emission tomography (FDG-PET) at 6 to 8 weeks after the end of treatment.
DLBCL patients
A total of 40% of polatuzumab-BR-treated DLBCL patients achieved CR at the end of treatment, versus 15% of BR-treated patients (P=0.012).
That CR improvement translated into a significantly higher progression-free survival (PFS) (6.7 months for polatuzumab-BR vs 2.0 months for BR, P<0.0001) and overall survival (11.8 months versus 4.7 months, P=0.0008), according to Dr Sehn.
The FDG-PET CR rates were higher in the polatuzumab-BR arm regardless of the number of prior lines of treatment for DLBCL, and regardless of relapsed versus refractory status, Dr. Sehn added.
FL patients
By contrast, in the FL cohort, the FDG-PET CR rate was high for both arms, at 69% for polatuzumab-BR and 63% for BR.
And there was no significant difference in progression-free survival (P=0.58) with “relatively short-term follow-up,” she said.
Adverse events
The most common grades 3 – 5 adverse events for both DLBCL and FL patients were higher in the polatuzumab-BR arm than the BR arm and included cytopenias, febrile neutropenia, and infections.
Serious AEs were also higher in the polatuzumab-BR arm and included febrile neutropenia for both FL and DLBCL patients and infection for FL patients.
Five percent of FL patients and 18% of DLBCL had a grade 5 event.
Commentary
Whether polatuzumab vedotin will change treatment paradigms for DLBCL patients may be answered by the ongoing POLARIX study, according to Alison Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, NY.
The randomized phase 3 POLARIX study (abstract TPS7589) is comparing polatuzumab plus R-CHP to R-CHOP in patients with previously untreated DLBCL.
“Certainly, there are patients who do very well with R-CHOP chemotherapy alone, and so we need to learn whether this is necessary for all patients, or only the high-risk patients,” Dr Moskowitz said in a talk at ASCO commenting on the results of the polatuzumab-BR study.
Hoffman-LaRoche is the sponsor of the study.
CHICAGO—Polatuzumab vedotin, when added to bendamustine (B) and rituximab (R), significantly improved response and survival rates in a cohort of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a phase 2 study.
By contrast, there were no such improvements in a cohort of follicular lymphoma (FL) patients, at least in short-term follow-up, investigator Laurie Helen Sehn, MD, of the BC Cancer Agency in Vancouver, Canada, said at the 2018 ASCO Annual Meeting.
However, the improvement in overall survival in DLBCL patients is “remarkable,” Dr Sehn affirmed in an oral presentation (abstract 7507).
“Based on these encouraging results, polatuzumab vedotin has received breakthrough therapy designation and priority medicines designation by the FDA and EMA for patients with relapsed or refractory DLBCL,” she said.
Polatuzumab-BR study (NCT02257567)
The study by Dr Sehn and colleagues included a cohort of 80 DLBCL patients randomized to BR or polatuzumab-BR for 6 planned 21-day cycles.
Investigators randomized another cohort of 80 FL patients to BR or polatuzumab-BR for 6 planned 28-day cycles.
The primary endpoint was complete response (CR) assessed by fluorodeoxyglucose positron emission tomography (FDG-PET) at 6 to 8 weeks after the end of treatment.
DLBCL patients
A total of 40% of polatuzumab-BR-treated DLBCL patients achieved CR at the end of treatment, versus 15% of BR-treated patients (P=0.012).
That CR improvement translated into a significantly higher progression-free survival (PFS) (6.7 months for polatuzumab-BR vs 2.0 months for BR, P<0.0001) and overall survival (11.8 months versus 4.7 months, P=0.0008), according to Dr Sehn.
The FDG-PET CR rates were higher in the polatuzumab-BR arm regardless of the number of prior lines of treatment for DLBCL, and regardless of relapsed versus refractory status, Dr. Sehn added.
FL patients
By contrast, in the FL cohort, the FDG-PET CR rate was high for both arms, at 69% for polatuzumab-BR and 63% for BR.
And there was no significant difference in progression-free survival (P=0.58) with “relatively short-term follow-up,” she said.
Adverse events
The most common grades 3 – 5 adverse events for both DLBCL and FL patients were higher in the polatuzumab-BR arm than the BR arm and included cytopenias, febrile neutropenia, and infections.
Serious AEs were also higher in the polatuzumab-BR arm and included febrile neutropenia for both FL and DLBCL patients and infection for FL patients.
Five percent of FL patients and 18% of DLBCL had a grade 5 event.
Commentary
Whether polatuzumab vedotin will change treatment paradigms for DLBCL patients may be answered by the ongoing POLARIX study, according to Alison Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, NY.
The randomized phase 3 POLARIX study (abstract TPS7589) is comparing polatuzumab plus R-CHP to R-CHOP in patients with previously untreated DLBCL.
“Certainly, there are patients who do very well with R-CHOP chemotherapy alone, and so we need to learn whether this is necessary for all patients, or only the high-risk patients,” Dr Moskowitz said in a talk at ASCO commenting on the results of the polatuzumab-BR study.
Hoffman-LaRoche is the sponsor of the study.