User login
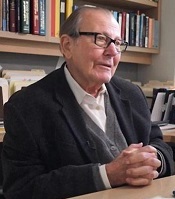
Leading researcher in genetics, hematology dies at 84
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
Avapritinib produces durable responses in SM
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
T-cell therapy induced CMRs with no CRS
CHICAGO—A novel CD19-targeted T-cell therapy induced complete metabolic responses (CMRs) and no cytokine release syndrome (CRS) in patients with B-cell lymphomas in a first-in-human clinical study.
All subjects achieving CMR at the 1-month safety and efficacy assessment continued to show CMR at 3 months, investigators reported at the 2018 ASCO Annual Meeting (abstract 3049*).
The therapy is built on a novel platform, ARTEMIS, designed to match the potency of chimeric antigen receptor (CAR) T-cell therapy but trigger less cytokine release when the target is engaged, investigators explained.
That platform is “potentially a major improvement” over existing CAR-T cell therapy, said Zhi Tao Ying, MD, of Peking University Cancer Hospital & Institute in Beijing, China, and coauthors in a poster presented at ASCO.
The treatment, called ET190L1-ARTEMIS, utilizes the T-cell receptor platform and a proprietary human anti-CD19 antibody to target CD19-positive malignancies.
The investigators reported on 21 adults with CD-19 positive relapsed and refractory B-cell lymphomas who had received a median of 4 lines of previous therapy.
Patients received autologous ET190L1-ARTEMIS T cells in 1 of 3 dosing cohorts: 3 patients at 1 x 106/kg, 13 at 3 x 106/kg, and 5 at 6 x 106/kg.
Of 17 patients completing a first-month efficacy assessment, 11 (65%) responded, including 7 CMRs and 3 partial responses. One patient had stable disease.
Seven of the 11 responders completed a third-month efficacy assessment, as of this analysis. Of 5 patients with CMR at month 1, all 5 maintained CMR at month 3. Likewise, 1 patient in partial response and 1 with stable disease at month 1 had the same response status at month 3.
There were no cases of CRS or neurotoxicity in 17 patients who completed the 1-month safety and efficacy assessment reported at ASCO. Grade 3 or greater adverse events in those subjects included lymphopenia in 17 (100%) and neutropenia in 5 (29%).
Eureka Therapeutics Inc., of Emeryville, California, is developing ET190L1-ARTEMIS. Co-investigators in this trial were from Eureka, Xi-An Jiaotong University in China, and Duke University School of Medicine in Durham, North Carolina.
A phase 1 trial of ET190L1-ARTEMIS in patients with relapsed and refractory non-Hodgkin lymphoma has been initiated at Duke University, and investigators say another US phase 1 trial including relapsed and refractory pediatric acute lymphoblastic leukemia patients will begin later this year.
Data in the abstract differ from that presented in the poster.
CHICAGO—A novel CD19-targeted T-cell therapy induced complete metabolic responses (CMRs) and no cytokine release syndrome (CRS) in patients with B-cell lymphomas in a first-in-human clinical study.
All subjects achieving CMR at the 1-month safety and efficacy assessment continued to show CMR at 3 months, investigators reported at the 2018 ASCO Annual Meeting (abstract 3049*).
The therapy is built on a novel platform, ARTEMIS, designed to match the potency of chimeric antigen receptor (CAR) T-cell therapy but trigger less cytokine release when the target is engaged, investigators explained.
That platform is “potentially a major improvement” over existing CAR-T cell therapy, said Zhi Tao Ying, MD, of Peking University Cancer Hospital & Institute in Beijing, China, and coauthors in a poster presented at ASCO.
The treatment, called ET190L1-ARTEMIS, utilizes the T-cell receptor platform and a proprietary human anti-CD19 antibody to target CD19-positive malignancies.
The investigators reported on 21 adults with CD-19 positive relapsed and refractory B-cell lymphomas who had received a median of 4 lines of previous therapy.
Patients received autologous ET190L1-ARTEMIS T cells in 1 of 3 dosing cohorts: 3 patients at 1 x 106/kg, 13 at 3 x 106/kg, and 5 at 6 x 106/kg.
Of 17 patients completing a first-month efficacy assessment, 11 (65%) responded, including 7 CMRs and 3 partial responses. One patient had stable disease.
Seven of the 11 responders completed a third-month efficacy assessment, as of this analysis. Of 5 patients with CMR at month 1, all 5 maintained CMR at month 3. Likewise, 1 patient in partial response and 1 with stable disease at month 1 had the same response status at month 3.
There were no cases of CRS or neurotoxicity in 17 patients who completed the 1-month safety and efficacy assessment reported at ASCO. Grade 3 or greater adverse events in those subjects included lymphopenia in 17 (100%) and neutropenia in 5 (29%).
Eureka Therapeutics Inc., of Emeryville, California, is developing ET190L1-ARTEMIS. Co-investigators in this trial were from Eureka, Xi-An Jiaotong University in China, and Duke University School of Medicine in Durham, North Carolina.
A phase 1 trial of ET190L1-ARTEMIS in patients with relapsed and refractory non-Hodgkin lymphoma has been initiated at Duke University, and investigators say another US phase 1 trial including relapsed and refractory pediatric acute lymphoblastic leukemia patients will begin later this year.
Data in the abstract differ from that presented in the poster.
CHICAGO—A novel CD19-targeted T-cell therapy induced complete metabolic responses (CMRs) and no cytokine release syndrome (CRS) in patients with B-cell lymphomas in a first-in-human clinical study.
All subjects achieving CMR at the 1-month safety and efficacy assessment continued to show CMR at 3 months, investigators reported at the 2018 ASCO Annual Meeting (abstract 3049*).
The therapy is built on a novel platform, ARTEMIS, designed to match the potency of chimeric antigen receptor (CAR) T-cell therapy but trigger less cytokine release when the target is engaged, investigators explained.
That platform is “potentially a major improvement” over existing CAR-T cell therapy, said Zhi Tao Ying, MD, of Peking University Cancer Hospital & Institute in Beijing, China, and coauthors in a poster presented at ASCO.
The treatment, called ET190L1-ARTEMIS, utilizes the T-cell receptor platform and a proprietary human anti-CD19 antibody to target CD19-positive malignancies.
The investigators reported on 21 adults with CD-19 positive relapsed and refractory B-cell lymphomas who had received a median of 4 lines of previous therapy.
Patients received autologous ET190L1-ARTEMIS T cells in 1 of 3 dosing cohorts: 3 patients at 1 x 106/kg, 13 at 3 x 106/kg, and 5 at 6 x 106/kg.
Of 17 patients completing a first-month efficacy assessment, 11 (65%) responded, including 7 CMRs and 3 partial responses. One patient had stable disease.
Seven of the 11 responders completed a third-month efficacy assessment, as of this analysis. Of 5 patients with CMR at month 1, all 5 maintained CMR at month 3. Likewise, 1 patient in partial response and 1 with stable disease at month 1 had the same response status at month 3.
There were no cases of CRS or neurotoxicity in 17 patients who completed the 1-month safety and efficacy assessment reported at ASCO. Grade 3 or greater adverse events in those subjects included lymphopenia in 17 (100%) and neutropenia in 5 (29%).
Eureka Therapeutics Inc., of Emeryville, California, is developing ET190L1-ARTEMIS. Co-investigators in this trial were from Eureka, Xi-An Jiaotong University in China, and Duke University School of Medicine in Durham, North Carolina.
A phase 1 trial of ET190L1-ARTEMIS in patients with relapsed and refractory non-Hodgkin lymphoma has been initiated at Duke University, and investigators say another US phase 1 trial including relapsed and refractory pediatric acute lymphoblastic leukemia patients will begin later this year.
Data in the abstract differ from that presented in the poster.
Survey reveals patient perceptions of ITP
STOCKHOLM—A new survey has revealed patients’ perceptions of immune thrombocytopenia (ITP) and how the condition impacts their quality of life (QOL).
Patients reported delays in diagnosis, lack of support, severe fatigue, and impacts on both emotional well-being and their ability to work.
Interim results of this survey, the ITP World Impact Survey (I-WISh), were presented in a poster (abstract PF654) at the 23rd Congress of the European Hematology Association (EHA).
I-WISh is a cross-sectional survey of ITP patients developed by global ITP experts, patient groups, and Novartis.
Interim results of the survey included patients from 12 countries (Canada, China, Colombia, France, Germany, Italy, India, Japan, Spain, Turkey, UK, and US) who completed an online questionnaire beginning in January 2018.
As of May 14, 2018, 1400 adults (age 18 and older) had completed the survey. Sixty-five percent were female, and they had a mean age of 47.1 years. The patients’ mean length of time with ITP was 110 months.
Most patients (63%) reported a high score for their current health state (5 to 7 on the Likert scale), but 15% reported a low score (1-3).
Most patients were working full-time (45%) or part-time (16%) at the time of the survey. Nineteen percent were retired, 6% were homemakers, 4% were students, and 10% were not seeking employment, on long-term sick leave or disability, or “other.”
Diagnosis
Twenty-two percent of all patients (307/1400) felt they had a delay in their ITP diagnosis caused by waiting for additional tests (49%, 150/307) or referral to a specialist (37%, 114/307).
Three-quarters of patients with a perceived delay (229/307) were anxious throughout diagnosis.
And 66% of all patients (927/1400) wanted more support during their diagnosis.
Symptoms
Patients reported fatigue as one of the most severe symptoms at diagnosis (75%, 627/839) and at survey completion (66%, 480/722).
The other “most severe” symptoms at diagnosis were heavy menstrual bleeding (85%, 353/416) and anxiety surrounding unstable platelet count (78%, 382/487). The other “most severe” symptoms at survey completion were thrombosis (73%, 24/33) and anxiety surrounding unstable platelet count (66%, 284/431).
“Severe fatigue, in particular, was reported by many patients as the most difficult-to-manage symptom of ITP,” said study investigator Nichola Cooper, MD, of Hammersmith Hospital, Imperial College London, in the UK.
“This is an important message for healthcare providers treating patients with this rare disease. ITP is about more than bruising and risk of bleeding.”
QOL
Forty-four percent of respondents (611/1398) said ITP impacted their energy levels more than half the time, and 36% (501/1398) said ITP had a negative impact on their normal capacity to exercise more than half the time.
Half of all patients (697/1400) said ITP had a high impact on their emotional well-being.
Eighty-three percent (1157/1400) said they felt a stable and safe platelet count was important, 64% (900/1400) worried that their condition will get worse, and 63% (888/1400) were concerned that their platelet count changes for no apparent reason.
Thirty-seven percent of all patients (511/1400) had reduced their work hours because of ITP, 37% (522/1400) seriously considered reducing their hours, and 21% (294/1400) considered terminating their employment.
Thirty-five percent of patients (491/1400) said obtaining healthy blood counts was their most important treatment goal. Twenty-one percent (299/1400) said increasing their energy levels was most important, and 15% (203/1400) said reducing spontaneous bleeds/bruising was most important.
STOCKHOLM—A new survey has revealed patients’ perceptions of immune thrombocytopenia (ITP) and how the condition impacts their quality of life (QOL).
Patients reported delays in diagnosis, lack of support, severe fatigue, and impacts on both emotional well-being and their ability to work.
Interim results of this survey, the ITP World Impact Survey (I-WISh), were presented in a poster (abstract PF654) at the 23rd Congress of the European Hematology Association (EHA).
I-WISh is a cross-sectional survey of ITP patients developed by global ITP experts, patient groups, and Novartis.
Interim results of the survey included patients from 12 countries (Canada, China, Colombia, France, Germany, Italy, India, Japan, Spain, Turkey, UK, and US) who completed an online questionnaire beginning in January 2018.
As of May 14, 2018, 1400 adults (age 18 and older) had completed the survey. Sixty-five percent were female, and they had a mean age of 47.1 years. The patients’ mean length of time with ITP was 110 months.
Most patients (63%) reported a high score for their current health state (5 to 7 on the Likert scale), but 15% reported a low score (1-3).
Most patients were working full-time (45%) or part-time (16%) at the time of the survey. Nineteen percent were retired, 6% were homemakers, 4% were students, and 10% were not seeking employment, on long-term sick leave or disability, or “other.”
Diagnosis
Twenty-two percent of all patients (307/1400) felt they had a delay in their ITP diagnosis caused by waiting for additional tests (49%, 150/307) or referral to a specialist (37%, 114/307).
Three-quarters of patients with a perceived delay (229/307) were anxious throughout diagnosis.
And 66% of all patients (927/1400) wanted more support during their diagnosis.
Symptoms
Patients reported fatigue as one of the most severe symptoms at diagnosis (75%, 627/839) and at survey completion (66%, 480/722).
The other “most severe” symptoms at diagnosis were heavy menstrual bleeding (85%, 353/416) and anxiety surrounding unstable platelet count (78%, 382/487). The other “most severe” symptoms at survey completion were thrombosis (73%, 24/33) and anxiety surrounding unstable platelet count (66%, 284/431).
“Severe fatigue, in particular, was reported by many patients as the most difficult-to-manage symptom of ITP,” said study investigator Nichola Cooper, MD, of Hammersmith Hospital, Imperial College London, in the UK.
“This is an important message for healthcare providers treating patients with this rare disease. ITP is about more than bruising and risk of bleeding.”
QOL
Forty-four percent of respondents (611/1398) said ITP impacted their energy levels more than half the time, and 36% (501/1398) said ITP had a negative impact on their normal capacity to exercise more than half the time.
Half of all patients (697/1400) said ITP had a high impact on their emotional well-being.
Eighty-three percent (1157/1400) said they felt a stable and safe platelet count was important, 64% (900/1400) worried that their condition will get worse, and 63% (888/1400) were concerned that their platelet count changes for no apparent reason.
Thirty-seven percent of all patients (511/1400) had reduced their work hours because of ITP, 37% (522/1400) seriously considered reducing their hours, and 21% (294/1400) considered terminating their employment.
Thirty-five percent of patients (491/1400) said obtaining healthy blood counts was their most important treatment goal. Twenty-one percent (299/1400) said increasing their energy levels was most important, and 15% (203/1400) said reducing spontaneous bleeds/bruising was most important.
STOCKHOLM—A new survey has revealed patients’ perceptions of immune thrombocytopenia (ITP) and how the condition impacts their quality of life (QOL).
Patients reported delays in diagnosis, lack of support, severe fatigue, and impacts on both emotional well-being and their ability to work.
Interim results of this survey, the ITP World Impact Survey (I-WISh), were presented in a poster (abstract PF654) at the 23rd Congress of the European Hematology Association (EHA).
I-WISh is a cross-sectional survey of ITP patients developed by global ITP experts, patient groups, and Novartis.
Interim results of the survey included patients from 12 countries (Canada, China, Colombia, France, Germany, Italy, India, Japan, Spain, Turkey, UK, and US) who completed an online questionnaire beginning in January 2018.
As of May 14, 2018, 1400 adults (age 18 and older) had completed the survey. Sixty-five percent were female, and they had a mean age of 47.1 years. The patients’ mean length of time with ITP was 110 months.
Most patients (63%) reported a high score for their current health state (5 to 7 on the Likert scale), but 15% reported a low score (1-3).
Most patients were working full-time (45%) or part-time (16%) at the time of the survey. Nineteen percent were retired, 6% were homemakers, 4% were students, and 10% were not seeking employment, on long-term sick leave or disability, or “other.”
Diagnosis
Twenty-two percent of all patients (307/1400) felt they had a delay in their ITP diagnosis caused by waiting for additional tests (49%, 150/307) or referral to a specialist (37%, 114/307).
Three-quarters of patients with a perceived delay (229/307) were anxious throughout diagnosis.
And 66% of all patients (927/1400) wanted more support during their diagnosis.
Symptoms
Patients reported fatigue as one of the most severe symptoms at diagnosis (75%, 627/839) and at survey completion (66%, 480/722).
The other “most severe” symptoms at diagnosis were heavy menstrual bleeding (85%, 353/416) and anxiety surrounding unstable platelet count (78%, 382/487). The other “most severe” symptoms at survey completion were thrombosis (73%, 24/33) and anxiety surrounding unstable platelet count (66%, 284/431).
“Severe fatigue, in particular, was reported by many patients as the most difficult-to-manage symptom of ITP,” said study investigator Nichola Cooper, MD, of Hammersmith Hospital, Imperial College London, in the UK.
“This is an important message for healthcare providers treating patients with this rare disease. ITP is about more than bruising and risk of bleeding.”
QOL
Forty-four percent of respondents (611/1398) said ITP impacted their energy levels more than half the time, and 36% (501/1398) said ITP had a negative impact on their normal capacity to exercise more than half the time.
Half of all patients (697/1400) said ITP had a high impact on their emotional well-being.
Eighty-three percent (1157/1400) said they felt a stable and safe platelet count was important, 64% (900/1400) worried that their condition will get worse, and 63% (888/1400) were concerned that their platelet count changes for no apparent reason.
Thirty-seven percent of all patients (511/1400) had reduced their work hours because of ITP, 37% (522/1400) seriously considered reducing their hours, and 21% (294/1400) considered terminating their employment.
Thirty-five percent of patients (491/1400) said obtaining healthy blood counts was their most important treatment goal. Twenty-one percent (299/1400) said increasing their energy levels was most important, and 15% (203/1400) said reducing spontaneous bleeds/bruising was most important.
Drug is convenient alternative for PNH, doc says
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
Inhibitor elicits responses in cGVHD
STOCKHOLM—The ROCK2 inhibitor KD025 produced responses in about two-thirds of patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2 trial.
KD025 elicited improvements in Lee Symptom Scale score, and patients were able to reduce doses of corticosteroids and other immunosuppressants.
There were no serious adverse events (AEs) related to KD025 and no apparent increased risk of infection with the drug.
Amandeep Salhotra, MD, of City of Hope in Duarte, California, presented these results at the 23rd Congress of the European Hematology Association (EHA) as abstract S873. The research was sponsored by Kadmon Holdings, Inc.
This ongoing phase 2 trial has enrolled 48 adults with steroid-dependent or steroid-refractory cGVHD and active disease.
The patients were divided into 3 cohorts, in which they received different dose levels of KD025—200 mg daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg daily (cohort 3).
Dr Salhotra presented results in cohorts 1 (n=17) and 2 (n=16). These patients had cGVHD for a median of 18.9 months before enrollment and had received a median of 3 prior lines of cGVHD therapy. They had cGVHD involvement across all organ systems.
The median age was 50 (range, 20-63) in cohort 1 and 55 (range, 30-75) in cohort 2. The median time to cGHVD diagnosis was 9.1 months in cohort 1 and 7.7 months in cohort 2. The median time from cGVHD diagnosis to enrollment was 25.9 months and 15.8 months, respectively.
All patients in cohort 1 had at least 2 organs involved, as did 94% of patients in cohort 2. Forty-seven percent and 69%, respectively, had at least 4 organs involved.
Treatment duration
The median treatment duration was 37 weeks in cohort 1 and 33 weeks in cohort 2. Four patients in cohort 1 had cGVHD progression, as did 8 patients in cohort 2.
Seven patients in cohort 1 withdrew from the study—2 due to cancer relapse, 2 due to AEs (headache and diarrhea), 1 due to investigator decision, and 2 due to voluntary withdrawal. Three patients in cohort 2 withdrew—1 due to investigator decision and 2 due to voluntary withdrawal.
Six patients are still active in cohort 1, with a median treatment duration of 70 weeks. Five patients are still active in cohort 2, with a median treatment duration of 58 weeks.
Safety
“The adverse events were, overall, consistent with those expected in patients with chronic GVHD receiving corticosteroids,” Dr Salhotra said. “There were no treatment-related serious adverse events, and there was no increased signal of infection.”
Ninety-four percent of patients in both cohorts had AEs. Thirty-five percent of patients in cohort 1 and 63% in cohort 2 had treatment-related AEs. Twelve percent and 31%, respectively, had grade 3 or higher related AEs. Twelve percent of patients in cohort 1 had a related AE leading to discontinuation (2 events, headache and diarrhea).
Commonly reported AEs (in cohorts 1 and 2, respectively) included ALT/AST elevation (35% and 25%), upper respiratory tract infection (24% and 38%), anemia (29% and 25%), gamma-glutamyltransferase elevation (24% and 31%), diarrhea (35% and 13%), and nausea (35% and 13%).
Response
The overall response rate (ORR) was 65% (11/17) in cohort 1 and 69% (11/16) in cohort 2.
In patients with at least 2 prior lines of systemic therapy, the ORR was 65% (11/17) in cohort 1 and 64% (9/14) in cohort 2. In patients with severe cGVHD, the ORR was 67% (8/12) in cohort 1 and 64% (9/14) in cohort 2.
“Responses were rapid,” Dr Salhotra noted. “Seventy-seven percent of the responders achieved a response by the time of first assessment, which was at 8 weeks.”
“These responses were durable. Seventy-three percent (8/11) of responders in cohort 1 and 55% (6/11) of responders in cohort 2 have sustained responses for more than 20 weeks. At the 32-week endpoint, there were 45% (5/11) responders in cohort 1 and 18% (2/11) in cohort 2.”
Dr Salhotra added that responses were observed across all affected organ systems, including complete responses in upper and lower gastrointestinal systems, mouth, joints/fascia, skin, eyes, and liver.
Of the 13 responders in cohorts 1 and 2 with at least 4 organs involved, 46% (n=6) achieved responses in 4 or more organs.
In cohort 1, 73% (8/11) of responders and 83% (5/6) of non-responders had corticosteroid dose reductions. In cohort 2, 55% (6/11) of responders and 60% (3/5) of non-responders had dose reductions.
Five patients have completely discontinued steroids—4 (24%) in cohort 1 and 1 (6%) in cohort 2.
There were 6 patients each in cohorts 1 and 2 who were receiving tacrolimus. Each cohort had 5 patients (83%) who had tacrolimus dose reductions on KD025. One patient completely discontinued tacrolimus.
Sixty-five percent of patients in cohort 1 and 44% in cohort 2 had a clinically meaningful improvement in cGVHD symptoms, which was defined as at least a 7-point decrease in the Lee Symptom Scale score. Both responders and non-responders had such improvements.
Based on these results, Kadmon Holdings, Inc., is planning a pivotal study of KD025 in cGVHD, which is expected to begin in the third quarter of 2018.
Dr Salhotra said the study will enroll adults who have received at least 2 prior lines of systemic therapy for cGVHD. Patients will be randomized to receive KD025 at 200 mg daily or 200 mg twice daily. The primary endpoint will be ORR.
STOCKHOLM—The ROCK2 inhibitor KD025 produced responses in about two-thirds of patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2 trial.
KD025 elicited improvements in Lee Symptom Scale score, and patients were able to reduce doses of corticosteroids and other immunosuppressants.
There were no serious adverse events (AEs) related to KD025 and no apparent increased risk of infection with the drug.
Amandeep Salhotra, MD, of City of Hope in Duarte, California, presented these results at the 23rd Congress of the European Hematology Association (EHA) as abstract S873. The research was sponsored by Kadmon Holdings, Inc.
This ongoing phase 2 trial has enrolled 48 adults with steroid-dependent or steroid-refractory cGVHD and active disease.
The patients were divided into 3 cohorts, in which they received different dose levels of KD025—200 mg daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg daily (cohort 3).
Dr Salhotra presented results in cohorts 1 (n=17) and 2 (n=16). These patients had cGVHD for a median of 18.9 months before enrollment and had received a median of 3 prior lines of cGVHD therapy. They had cGVHD involvement across all organ systems.
The median age was 50 (range, 20-63) in cohort 1 and 55 (range, 30-75) in cohort 2. The median time to cGHVD diagnosis was 9.1 months in cohort 1 and 7.7 months in cohort 2. The median time from cGVHD diagnosis to enrollment was 25.9 months and 15.8 months, respectively.
All patients in cohort 1 had at least 2 organs involved, as did 94% of patients in cohort 2. Forty-seven percent and 69%, respectively, had at least 4 organs involved.
Treatment duration
The median treatment duration was 37 weeks in cohort 1 and 33 weeks in cohort 2. Four patients in cohort 1 had cGVHD progression, as did 8 patients in cohort 2.
Seven patients in cohort 1 withdrew from the study—2 due to cancer relapse, 2 due to AEs (headache and diarrhea), 1 due to investigator decision, and 2 due to voluntary withdrawal. Three patients in cohort 2 withdrew—1 due to investigator decision and 2 due to voluntary withdrawal.
Six patients are still active in cohort 1, with a median treatment duration of 70 weeks. Five patients are still active in cohort 2, with a median treatment duration of 58 weeks.
Safety
“The adverse events were, overall, consistent with those expected in patients with chronic GVHD receiving corticosteroids,” Dr Salhotra said. “There were no treatment-related serious adverse events, and there was no increased signal of infection.”
Ninety-four percent of patients in both cohorts had AEs. Thirty-five percent of patients in cohort 1 and 63% in cohort 2 had treatment-related AEs. Twelve percent and 31%, respectively, had grade 3 or higher related AEs. Twelve percent of patients in cohort 1 had a related AE leading to discontinuation (2 events, headache and diarrhea).
Commonly reported AEs (in cohorts 1 and 2, respectively) included ALT/AST elevation (35% and 25%), upper respiratory tract infection (24% and 38%), anemia (29% and 25%), gamma-glutamyltransferase elevation (24% and 31%), diarrhea (35% and 13%), and nausea (35% and 13%).
Response
The overall response rate (ORR) was 65% (11/17) in cohort 1 and 69% (11/16) in cohort 2.
In patients with at least 2 prior lines of systemic therapy, the ORR was 65% (11/17) in cohort 1 and 64% (9/14) in cohort 2. In patients with severe cGVHD, the ORR was 67% (8/12) in cohort 1 and 64% (9/14) in cohort 2.
“Responses were rapid,” Dr Salhotra noted. “Seventy-seven percent of the responders achieved a response by the time of first assessment, which was at 8 weeks.”
“These responses were durable. Seventy-three percent (8/11) of responders in cohort 1 and 55% (6/11) of responders in cohort 2 have sustained responses for more than 20 weeks. At the 32-week endpoint, there were 45% (5/11) responders in cohort 1 and 18% (2/11) in cohort 2.”
Dr Salhotra added that responses were observed across all affected organ systems, including complete responses in upper and lower gastrointestinal systems, mouth, joints/fascia, skin, eyes, and liver.
Of the 13 responders in cohorts 1 and 2 with at least 4 organs involved, 46% (n=6) achieved responses in 4 or more organs.
In cohort 1, 73% (8/11) of responders and 83% (5/6) of non-responders had corticosteroid dose reductions. In cohort 2, 55% (6/11) of responders and 60% (3/5) of non-responders had dose reductions.
Five patients have completely discontinued steroids—4 (24%) in cohort 1 and 1 (6%) in cohort 2.
There were 6 patients each in cohorts 1 and 2 who were receiving tacrolimus. Each cohort had 5 patients (83%) who had tacrolimus dose reductions on KD025. One patient completely discontinued tacrolimus.
Sixty-five percent of patients in cohort 1 and 44% in cohort 2 had a clinically meaningful improvement in cGVHD symptoms, which was defined as at least a 7-point decrease in the Lee Symptom Scale score. Both responders and non-responders had such improvements.
Based on these results, Kadmon Holdings, Inc., is planning a pivotal study of KD025 in cGVHD, which is expected to begin in the third quarter of 2018.
Dr Salhotra said the study will enroll adults who have received at least 2 prior lines of systemic therapy for cGVHD. Patients will be randomized to receive KD025 at 200 mg daily or 200 mg twice daily. The primary endpoint will be ORR.
STOCKHOLM—The ROCK2 inhibitor KD025 produced responses in about two-thirds of patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2 trial.
KD025 elicited improvements in Lee Symptom Scale score, and patients were able to reduce doses of corticosteroids and other immunosuppressants.
There were no serious adverse events (AEs) related to KD025 and no apparent increased risk of infection with the drug.
Amandeep Salhotra, MD, of City of Hope in Duarte, California, presented these results at the 23rd Congress of the European Hematology Association (EHA) as abstract S873. The research was sponsored by Kadmon Holdings, Inc.
This ongoing phase 2 trial has enrolled 48 adults with steroid-dependent or steroid-refractory cGVHD and active disease.
The patients were divided into 3 cohorts, in which they received different dose levels of KD025—200 mg daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg daily (cohort 3).
Dr Salhotra presented results in cohorts 1 (n=17) and 2 (n=16). These patients had cGVHD for a median of 18.9 months before enrollment and had received a median of 3 prior lines of cGVHD therapy. They had cGVHD involvement across all organ systems.
The median age was 50 (range, 20-63) in cohort 1 and 55 (range, 30-75) in cohort 2. The median time to cGHVD diagnosis was 9.1 months in cohort 1 and 7.7 months in cohort 2. The median time from cGVHD diagnosis to enrollment was 25.9 months and 15.8 months, respectively.
All patients in cohort 1 had at least 2 organs involved, as did 94% of patients in cohort 2. Forty-seven percent and 69%, respectively, had at least 4 organs involved.
Treatment duration
The median treatment duration was 37 weeks in cohort 1 and 33 weeks in cohort 2. Four patients in cohort 1 had cGVHD progression, as did 8 patients in cohort 2.
Seven patients in cohort 1 withdrew from the study—2 due to cancer relapse, 2 due to AEs (headache and diarrhea), 1 due to investigator decision, and 2 due to voluntary withdrawal. Three patients in cohort 2 withdrew—1 due to investigator decision and 2 due to voluntary withdrawal.
Six patients are still active in cohort 1, with a median treatment duration of 70 weeks. Five patients are still active in cohort 2, with a median treatment duration of 58 weeks.
Safety
“The adverse events were, overall, consistent with those expected in patients with chronic GVHD receiving corticosteroids,” Dr Salhotra said. “There were no treatment-related serious adverse events, and there was no increased signal of infection.”
Ninety-four percent of patients in both cohorts had AEs. Thirty-five percent of patients in cohort 1 and 63% in cohort 2 had treatment-related AEs. Twelve percent and 31%, respectively, had grade 3 or higher related AEs. Twelve percent of patients in cohort 1 had a related AE leading to discontinuation (2 events, headache and diarrhea).
Commonly reported AEs (in cohorts 1 and 2, respectively) included ALT/AST elevation (35% and 25%), upper respiratory tract infection (24% and 38%), anemia (29% and 25%), gamma-glutamyltransferase elevation (24% and 31%), diarrhea (35% and 13%), and nausea (35% and 13%).
Response
The overall response rate (ORR) was 65% (11/17) in cohort 1 and 69% (11/16) in cohort 2.
In patients with at least 2 prior lines of systemic therapy, the ORR was 65% (11/17) in cohort 1 and 64% (9/14) in cohort 2. In patients with severe cGVHD, the ORR was 67% (8/12) in cohort 1 and 64% (9/14) in cohort 2.
“Responses were rapid,” Dr Salhotra noted. “Seventy-seven percent of the responders achieved a response by the time of first assessment, which was at 8 weeks.”
“These responses were durable. Seventy-three percent (8/11) of responders in cohort 1 and 55% (6/11) of responders in cohort 2 have sustained responses for more than 20 weeks. At the 32-week endpoint, there were 45% (5/11) responders in cohort 1 and 18% (2/11) in cohort 2.”
Dr Salhotra added that responses were observed across all affected organ systems, including complete responses in upper and lower gastrointestinal systems, mouth, joints/fascia, skin, eyes, and liver.
Of the 13 responders in cohorts 1 and 2 with at least 4 organs involved, 46% (n=6) achieved responses in 4 or more organs.
In cohort 1, 73% (8/11) of responders and 83% (5/6) of non-responders had corticosteroid dose reductions. In cohort 2, 55% (6/11) of responders and 60% (3/5) of non-responders had dose reductions.
Five patients have completely discontinued steroids—4 (24%) in cohort 1 and 1 (6%) in cohort 2.
There were 6 patients each in cohorts 1 and 2 who were receiving tacrolimus. Each cohort had 5 patients (83%) who had tacrolimus dose reductions on KD025. One patient completely discontinued tacrolimus.
Sixty-five percent of patients in cohort 1 and 44% in cohort 2 had a clinically meaningful improvement in cGVHD symptoms, which was defined as at least a 7-point decrease in the Lee Symptom Scale score. Both responders and non-responders had such improvements.
Based on these results, Kadmon Holdings, Inc., is planning a pivotal study of KD025 in cGVHD, which is expected to begin in the third quarter of 2018.
Dr Salhotra said the study will enroll adults who have received at least 2 prior lines of systemic therapy for cGVHD. Patients will be randomized to receive KD025 at 200 mg daily or 200 mg twice daily. The primary endpoint will be ORR.
FDA approves 2 blood screening assays
The US Food and Drug Administration (FDA) has approved 2 Grifols blood screening assays—Procleix Ultrio Elite and Procleix WNV.
Procleix WNV is a qualitative in vitro nucleic acid assay for the detection of West Nile virus RNA in plasma and serum of human blood donors.
Procleix Ultrio Elite is a blood screening assay that delivers simultaneous results for human immunodeficiency virus type 1, hepatitis C virus, and hepatitis B virus. It also detects human immunodeficiency virus type 2.
Procleix Ultrio Elite can be used to test pools of plasma composed of up to 96 individual donations from donors of source plasma.
Grifols will begin commercializing the Procleix Ultrio Elite and Procleix WNV assays in the US later this year.
“These FDA approvals demonstrate our ongoing commitment to expand Grifols comprehensive nucleic acid testing (NAT) solutions portfolio to help labs administer NAT,” said Carsten Schroeder, president of Grifols’s Diagnostic Division.
Procleix Ultrio Elite and Procleix WNV will run on the fully automated NAT blood screening platform Procleix Panther system. The device is an integrated NAT system that fully automates all necessary steps to perform Procleix assays, from sample processing through amplification, detection, and data reduction.
“The addition of the Procleix Panther system with these assays will allow blood centers to efficiently screen for infectious diseases on one simple, automated platform while adapting to changes in donation volume and regulatory requirements,” Schroeder said.
The US Food and Drug Administration (FDA) has approved 2 Grifols blood screening assays—Procleix Ultrio Elite and Procleix WNV.
Procleix WNV is a qualitative in vitro nucleic acid assay for the detection of West Nile virus RNA in plasma and serum of human blood donors.
Procleix Ultrio Elite is a blood screening assay that delivers simultaneous results for human immunodeficiency virus type 1, hepatitis C virus, and hepatitis B virus. It also detects human immunodeficiency virus type 2.
Procleix Ultrio Elite can be used to test pools of plasma composed of up to 96 individual donations from donors of source plasma.
Grifols will begin commercializing the Procleix Ultrio Elite and Procleix WNV assays in the US later this year.
“These FDA approvals demonstrate our ongoing commitment to expand Grifols comprehensive nucleic acid testing (NAT) solutions portfolio to help labs administer NAT,” said Carsten Schroeder, president of Grifols’s Diagnostic Division.
Procleix Ultrio Elite and Procleix WNV will run on the fully automated NAT blood screening platform Procleix Panther system. The device is an integrated NAT system that fully automates all necessary steps to perform Procleix assays, from sample processing through amplification, detection, and data reduction.
“The addition of the Procleix Panther system with these assays will allow blood centers to efficiently screen for infectious diseases on one simple, automated platform while adapting to changes in donation volume and regulatory requirements,” Schroeder said.
The US Food and Drug Administration (FDA) has approved 2 Grifols blood screening assays—Procleix Ultrio Elite and Procleix WNV.
Procleix WNV is a qualitative in vitro nucleic acid assay for the detection of West Nile virus RNA in plasma and serum of human blood donors.
Procleix Ultrio Elite is a blood screening assay that delivers simultaneous results for human immunodeficiency virus type 1, hepatitis C virus, and hepatitis B virus. It also detects human immunodeficiency virus type 2.
Procleix Ultrio Elite can be used to test pools of plasma composed of up to 96 individual donations from donors of source plasma.
Grifols will begin commercializing the Procleix Ultrio Elite and Procleix WNV assays in the US later this year.
“These FDA approvals demonstrate our ongoing commitment to expand Grifols comprehensive nucleic acid testing (NAT) solutions portfolio to help labs administer NAT,” said Carsten Schroeder, president of Grifols’s Diagnostic Division.
Procleix Ultrio Elite and Procleix WNV will run on the fully automated NAT blood screening platform Procleix Panther system. The device is an integrated NAT system that fully automates all necessary steps to perform Procleix assays, from sample processing through amplification, detection, and data reduction.
“The addition of the Procleix Panther system with these assays will allow blood centers to efficiently screen for infectious diseases on one simple, automated platform while adapting to changes in donation volume and regulatory requirements,” Schroeder said.
MAb doubles ORR, PFS in rel/ref MM
STOCKHOLM—Adding elotuzumab (E) to treatment with pomalidomide (P) and low-dose dexamethasone (d) can produce “clinically meaningful” results in patients with relapsed/refractory multiple myeloma (MM), according to an investigator for the ELOQUENT-3 trial.
In this phase 2 trial, patients who received EPd had double the overall response rate (ORR) and median progression-free survival (PFS) of patients who received Pd.
Additionally, adverse events (AEs) were comparable between the treatment arms.
Meletios Dimopoulos, MD, of National and Kapodistrian University of Athens in Greece, presented these results as a late-breaking abstract (LB2606) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Bristol-Myers Squibb.
The ELOQUENT-3 trial enrolled MM patients who had refractory or relapsed and refractory MM. They had to have received lenalidomide and a proteasome inhibitor (PI).
The patients were randomized to receive EPd (n=60) or Pd (n=57) in 28-day cycles until disease progression or unacceptable toxicity.
Pomalidomide was given orally at 4 mg on days 1 to 21 of each cycle. In the Pd arm, dexamethasone was given as a 20 mg (for patients older than 75) or 40 mg (75 and younger) tablet weekly.
In the EPd arm, dexamethasone was split between oral (8 mg, 20 mg, or 40 mg tablets) and intravenous doses (8 mg or 28 mg).
Elotuzumab was given at 10 mg/kg intravenously weekly for the first 2 cycles and 20 mg/kg monthly from cycle 3 on.
Patient characteristics
The patients’ median age was 69 (range, 43-81) in the EPd arm and 66 (range, 36-81) in the Pd arm. They were a median of 4.8 years (EPd) or 4.4 years (Pd) from diagnosis.
The median number of prior therapies was 3 (range, 2-8) in both groups.
Ninety percent of patients in the EPd arm and 84% of those in the Pd arm were refractory to lenalidomide. Seventy-eight percent and 82%, respectively, were refractory to a PI. And 68% and 72%, respectively, were refractory to both lenalidomide and a PI.
Treatment duration
Dr Dimopoulos noted that twice as many patients remained on treatment with EPd compared to Pd at the time of database lock (February 21, 2018). Forty percent of EPd patients (n=24) and 20% of Pd patients (n=11) were still on treatment at that time.
Patients’ primary reason for treatment discontinuation was disease progression—43% of EPd recipients and 56% of Pd recipients. Two percent of EPd recipients and 4% of Pd recipients withdrew due to treatment-related toxicity. Four percent of patients in the Pd arm (and none in the EPd arm) withdrew due to maximum clinical benefit.
The median number of treatment cycles was 9 (range, 4-13) in the EPd arm and 5 (range, 3-10) in the Pd arm.
Efficacy
The ORR was 53% in the EPd arm and 26% in the Pd arm. The odds ratio was 3.25 (P=0.0029).
Eight percent of patients in the EPd arm had a complete response or stringent complete response, as did 2% of patients in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and has not been reached in the EPd arm.
“Elotuzumab with pomalidomide and dexamethasone showed a significant and clinically meaningful 46% reduction in the risk of progression or death,” Dr Dimopoulos said.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.0078).
Although overall survival data are not yet mature, there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 deaths in the Pd arm.
Safety
Dr Dimopoulos said AEs were comparable between the treatment arms. He pointed out that neutropenia was less common with EPd compared to Pd, despite similar pomalidomide dose intensity. And exposure-adjusted hematologic AEs and infections were lower with EPd than with Pd.
Ninety-seven percent of patients in the EPd arm and 95% in the Pd arm had at least 1 AE.
Grade 3-4 nonhematologic AEs (in the EPd and Pd arms, respectively) included constipation (2% and 0%), hyperglycemia (8% and 7%), bone pain (3% and 0%), dyspnea (3% and 2%), fatigue (0% and 4%), respiratory tract infection (0% and 2%), and upper respiratory tract infection (0% and 2%).
Grade 3-4 hematologic AEs (in the EPd and Pd arms, respectively) included anemia (10% and 20%), neutropenia (13% and 27%), thrombocytopenia (8% and 5%), and lymphopenia (8% and 2%).
Grade 3-4 AEs of special interest (in the EPd and Pd arms, respectively) included infections (13% and 22%), vascular disorders (3% and 0%), cardiac disorders (7% and 4%), and neoplasms (2% and 11%).
There were 5 grade 5 AEs in the EPd arm and 8 in the Pd arm.
In the EPd arm, grade 5 AEs included infection (n=3), cardiac failure, and general physical health deterioration.
In the Pd arm, grade 5 AEs included malignant neoplasm progression (n=4), infection, multiple organ failure and infection, myocardial infarction, and plasma cell myeloma.
STOCKHOLM—Adding elotuzumab (E) to treatment with pomalidomide (P) and low-dose dexamethasone (d) can produce “clinically meaningful” results in patients with relapsed/refractory multiple myeloma (MM), according to an investigator for the ELOQUENT-3 trial.
In this phase 2 trial, patients who received EPd had double the overall response rate (ORR) and median progression-free survival (PFS) of patients who received Pd.
Additionally, adverse events (AEs) were comparable between the treatment arms.
Meletios Dimopoulos, MD, of National and Kapodistrian University of Athens in Greece, presented these results as a late-breaking abstract (LB2606) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Bristol-Myers Squibb.
The ELOQUENT-3 trial enrolled MM patients who had refractory or relapsed and refractory MM. They had to have received lenalidomide and a proteasome inhibitor (PI).
The patients were randomized to receive EPd (n=60) or Pd (n=57) in 28-day cycles until disease progression or unacceptable toxicity.
Pomalidomide was given orally at 4 mg on days 1 to 21 of each cycle. In the Pd arm, dexamethasone was given as a 20 mg (for patients older than 75) or 40 mg (75 and younger) tablet weekly.
In the EPd arm, dexamethasone was split between oral (8 mg, 20 mg, or 40 mg tablets) and intravenous doses (8 mg or 28 mg).
Elotuzumab was given at 10 mg/kg intravenously weekly for the first 2 cycles and 20 mg/kg monthly from cycle 3 on.
Patient characteristics
The patients’ median age was 69 (range, 43-81) in the EPd arm and 66 (range, 36-81) in the Pd arm. They were a median of 4.8 years (EPd) or 4.4 years (Pd) from diagnosis.
The median number of prior therapies was 3 (range, 2-8) in both groups.
Ninety percent of patients in the EPd arm and 84% of those in the Pd arm were refractory to lenalidomide. Seventy-eight percent and 82%, respectively, were refractory to a PI. And 68% and 72%, respectively, were refractory to both lenalidomide and a PI.
Treatment duration
Dr Dimopoulos noted that twice as many patients remained on treatment with EPd compared to Pd at the time of database lock (February 21, 2018). Forty percent of EPd patients (n=24) and 20% of Pd patients (n=11) were still on treatment at that time.
Patients’ primary reason for treatment discontinuation was disease progression—43% of EPd recipients and 56% of Pd recipients. Two percent of EPd recipients and 4% of Pd recipients withdrew due to treatment-related toxicity. Four percent of patients in the Pd arm (and none in the EPd arm) withdrew due to maximum clinical benefit.
The median number of treatment cycles was 9 (range, 4-13) in the EPd arm and 5 (range, 3-10) in the Pd arm.
Efficacy
The ORR was 53% in the EPd arm and 26% in the Pd arm. The odds ratio was 3.25 (P=0.0029).
Eight percent of patients in the EPd arm had a complete response or stringent complete response, as did 2% of patients in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and has not been reached in the EPd arm.
“Elotuzumab with pomalidomide and dexamethasone showed a significant and clinically meaningful 46% reduction in the risk of progression or death,” Dr Dimopoulos said.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.0078).
Although overall survival data are not yet mature, there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 deaths in the Pd arm.
Safety
Dr Dimopoulos said AEs were comparable between the treatment arms. He pointed out that neutropenia was less common with EPd compared to Pd, despite similar pomalidomide dose intensity. And exposure-adjusted hematologic AEs and infections were lower with EPd than with Pd.
Ninety-seven percent of patients in the EPd arm and 95% in the Pd arm had at least 1 AE.
Grade 3-4 nonhematologic AEs (in the EPd and Pd arms, respectively) included constipation (2% and 0%), hyperglycemia (8% and 7%), bone pain (3% and 0%), dyspnea (3% and 2%), fatigue (0% and 4%), respiratory tract infection (0% and 2%), and upper respiratory tract infection (0% and 2%).
Grade 3-4 hematologic AEs (in the EPd and Pd arms, respectively) included anemia (10% and 20%), neutropenia (13% and 27%), thrombocytopenia (8% and 5%), and lymphopenia (8% and 2%).
Grade 3-4 AEs of special interest (in the EPd and Pd arms, respectively) included infections (13% and 22%), vascular disorders (3% and 0%), cardiac disorders (7% and 4%), and neoplasms (2% and 11%).
There were 5 grade 5 AEs in the EPd arm and 8 in the Pd arm.
In the EPd arm, grade 5 AEs included infection (n=3), cardiac failure, and general physical health deterioration.
In the Pd arm, grade 5 AEs included malignant neoplasm progression (n=4), infection, multiple organ failure and infection, myocardial infarction, and plasma cell myeloma.
STOCKHOLM—Adding elotuzumab (E) to treatment with pomalidomide (P) and low-dose dexamethasone (d) can produce “clinically meaningful” results in patients with relapsed/refractory multiple myeloma (MM), according to an investigator for the ELOQUENT-3 trial.
In this phase 2 trial, patients who received EPd had double the overall response rate (ORR) and median progression-free survival (PFS) of patients who received Pd.
Additionally, adverse events (AEs) were comparable between the treatment arms.
Meletios Dimopoulos, MD, of National and Kapodistrian University of Athens in Greece, presented these results as a late-breaking abstract (LB2606) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Bristol-Myers Squibb.
The ELOQUENT-3 trial enrolled MM patients who had refractory or relapsed and refractory MM. They had to have received lenalidomide and a proteasome inhibitor (PI).
The patients were randomized to receive EPd (n=60) or Pd (n=57) in 28-day cycles until disease progression or unacceptable toxicity.
Pomalidomide was given orally at 4 mg on days 1 to 21 of each cycle. In the Pd arm, dexamethasone was given as a 20 mg (for patients older than 75) or 40 mg (75 and younger) tablet weekly.
In the EPd arm, dexamethasone was split between oral (8 mg, 20 mg, or 40 mg tablets) and intravenous doses (8 mg or 28 mg).
Elotuzumab was given at 10 mg/kg intravenously weekly for the first 2 cycles and 20 mg/kg monthly from cycle 3 on.
Patient characteristics
The patients’ median age was 69 (range, 43-81) in the EPd arm and 66 (range, 36-81) in the Pd arm. They were a median of 4.8 years (EPd) or 4.4 years (Pd) from diagnosis.
The median number of prior therapies was 3 (range, 2-8) in both groups.
Ninety percent of patients in the EPd arm and 84% of those in the Pd arm were refractory to lenalidomide. Seventy-eight percent and 82%, respectively, were refractory to a PI. And 68% and 72%, respectively, were refractory to both lenalidomide and a PI.
Treatment duration
Dr Dimopoulos noted that twice as many patients remained on treatment with EPd compared to Pd at the time of database lock (February 21, 2018). Forty percent of EPd patients (n=24) and 20% of Pd patients (n=11) were still on treatment at that time.
Patients’ primary reason for treatment discontinuation was disease progression—43% of EPd recipients and 56% of Pd recipients. Two percent of EPd recipients and 4% of Pd recipients withdrew due to treatment-related toxicity. Four percent of patients in the Pd arm (and none in the EPd arm) withdrew due to maximum clinical benefit.
The median number of treatment cycles was 9 (range, 4-13) in the EPd arm and 5 (range, 3-10) in the Pd arm.
Efficacy
The ORR was 53% in the EPd arm and 26% in the Pd arm. The odds ratio was 3.25 (P=0.0029).
Eight percent of patients in the EPd arm had a complete response or stringent complete response, as did 2% of patients in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and has not been reached in the EPd arm.
“Elotuzumab with pomalidomide and dexamethasone showed a significant and clinically meaningful 46% reduction in the risk of progression or death,” Dr Dimopoulos said.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.0078).
Although overall survival data are not yet mature, there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 deaths in the Pd arm.
Safety
Dr Dimopoulos said AEs were comparable between the treatment arms. He pointed out that neutropenia was less common with EPd compared to Pd, despite similar pomalidomide dose intensity. And exposure-adjusted hematologic AEs and infections were lower with EPd than with Pd.
Ninety-seven percent of patients in the EPd arm and 95% in the Pd arm had at least 1 AE.
Grade 3-4 nonhematologic AEs (in the EPd and Pd arms, respectively) included constipation (2% and 0%), hyperglycemia (8% and 7%), bone pain (3% and 0%), dyspnea (3% and 2%), fatigue (0% and 4%), respiratory tract infection (0% and 2%), and upper respiratory tract infection (0% and 2%).
Grade 3-4 hematologic AEs (in the EPd and Pd arms, respectively) included anemia (10% and 20%), neutropenia (13% and 27%), thrombocytopenia (8% and 5%), and lymphopenia (8% and 2%).
Grade 3-4 AEs of special interest (in the EPd and Pd arms, respectively) included infections (13% and 22%), vascular disorders (3% and 0%), cardiac disorders (7% and 4%), and neoplasms (2% and 11%).
There were 5 grade 5 AEs in the EPd arm and 8 in the Pd arm.
In the EPd arm, grade 5 AEs included infection (n=3), cardiac failure, and general physical health deterioration.
In the Pd arm, grade 5 AEs included malignant neoplasm progression (n=4), infection, multiple organ failure and infection, myocardial infarction, and plasma cell myeloma.
Inhibitor exhibits activity in B- and T-cell NHLs
STOCKHOLM—The dual SYK/JAK inhibitor cerdulatinib has demonstrated efficacy in a phase 2 trial of patients with heavily pretreated B- and T-cell non-Hodgkin lymphomas (NHLs).
There were a few deaths due to sepsis or septic shock that were considered related to cerdulatinib, but investigators have taken steps to prevent additional deaths.
Cerdulatinib produced responses in patients with peripheral T-cell lymphoma (PTCL), cutaneous T-cell lymphoma (CTCL), chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other NHLs.
The 5 deaths due to sepsis or septic shock (3 concomitant with pneumonia) occurred early on in the trial, and dose reductions, monitoring, and antibiotic prophylaxis appeared to be effective in preventing additional deaths.
Results from this trial were presented in a poster (abstract PF437) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Portola Pharmaceuticals, Inc.
The trial enrolled 114 patients. They had FL (grade 1-3A; n=39), PTCL (n=25), CTCL (n=5), CLL/SLL (n=28), other indolent NHLs (Waldenstrom’s macroglobulinemia and marginal zone lymphoma; n=12), or aggressive NHL (defined as diffuse large B-cell lymphoma [DLBCL], grade 3B FL, mantle cell lymphoma, and transformed NHL with relapsed disease; n=5).
The patients’ median age was 68 (range, 34-93), and 59% were male. The median number of prior treatment regimens was 3 (range, 1-13), and 37% of patients had refractory disease.
Patients received cerdulatinib at 25, 30, or 35 mg twice daily (BID). A total of 101 patients were evaluable as of May 4, 2018.
Response
The objective response rate (ORR) was 47% in the entire population. Thirteen patients achieved a complete response (CR), and 34 had a partial response (PR). Thirty-four patients remained on cerdulatinib at the data cut-off.
The ORR was 46% in the FL patients, with 3 patients achieving a CR and 13 achieving a PR. Thirteen FL patients remained on cerdulatinib.
In the CLL/SLL patients, the ORR was 61%. Two patients had a CR, and 15 had a PR. Four CLL/SLL patients remained on cerdulatinib.
In PTCL, the ORR was 35%. All 7 responders had a CR. Eleven PTCL patients remained on cerdulatinib.
Only 1 CTCL patient was evaluable, but this patient achieved a CR and remained on cerdulatinib.
The ORR was 42% for patients with other indolent NHLs, with 5 PRs and no CRs. Only 1 patient in this group remained on cerdulatinib.
For aggressive NHL, the ORR was 20%, with 1 PR and no CRs. None of the patients in this group stayed on cerdulatinib.
“Cerdulatinib continues to demonstrate promising results across a wide range of B- and T-cell malignancies, including early indications of the potential for durable responses,” said study investigator Paul Hamlin, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“The new signals in relapsed/refractory PTCL and CTCL are particularly compelling when you consider the limited treatment options for patients that fail frontline therapy.”
Safety
Grade 3 or higher adverse events included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
The 5 deaths due to sepsis or septic shock (3 of which were concomitant with pneumonia) were considered related to cerdulatinib. Three of the deaths occurred in patients with CLL, 1 in a DLBCL patient, and 1 in an FL patient.
“One of the things we have seen [with CLL patients] is the background infection rate is quite a bit higher,” said John T. Curnutte, MD, PhD, interim co-president and head of research and development at Portola Pharmaceuticals.
“You see this with multiple other agents, so we were not particularly surprised to see [sepsis/septic shock in CLL].”
Dr Curnutte noted that grade 5 sepsis/septic shock tended to occur in patients who were pre-colonized and/or had high plasma levels of cerdulatinib.
So, to prevent these adverse events, the starting dose of cerdulatinib was lowered, investigators began monitoring patients’ plasma levels, and all patients began receiving antibiotic prophylaxis. (Previously, only CLL patients had received this prophylaxis.)
The investigators found that lowering the starting dose from 35 mg BID to 30 mg or even 25 mg BID reduced plasma levels.
“At the 35 mg dose, 1 out of every 4 patients showed accumulation of the drug,” Dr Curnutte said. “In general, the use of the 30 mg BID or step-down 25 mg BID did not result in accumulation of drug.”
Dr Curnutte also noted that enrollment of CLL/SLL patients is complete, and investigators would be “very careful” if the study were to be re-opened to these patients.
For now, Portola is focused on completing enrollment in other patient groups on this phase 2 trial. The company is also hoping to conduct a phase 3 trial of cerdulatinib in PTCL that could begin as early as the end of this year.
STOCKHOLM—The dual SYK/JAK inhibitor cerdulatinib has demonstrated efficacy in a phase 2 trial of patients with heavily pretreated B- and T-cell non-Hodgkin lymphomas (NHLs).
There were a few deaths due to sepsis or septic shock that were considered related to cerdulatinib, but investigators have taken steps to prevent additional deaths.
Cerdulatinib produced responses in patients with peripheral T-cell lymphoma (PTCL), cutaneous T-cell lymphoma (CTCL), chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other NHLs.
The 5 deaths due to sepsis or septic shock (3 concomitant with pneumonia) occurred early on in the trial, and dose reductions, monitoring, and antibiotic prophylaxis appeared to be effective in preventing additional deaths.
Results from this trial were presented in a poster (abstract PF437) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Portola Pharmaceuticals, Inc.
The trial enrolled 114 patients. They had FL (grade 1-3A; n=39), PTCL (n=25), CTCL (n=5), CLL/SLL (n=28), other indolent NHLs (Waldenstrom’s macroglobulinemia and marginal zone lymphoma; n=12), or aggressive NHL (defined as diffuse large B-cell lymphoma [DLBCL], grade 3B FL, mantle cell lymphoma, and transformed NHL with relapsed disease; n=5).
The patients’ median age was 68 (range, 34-93), and 59% were male. The median number of prior treatment regimens was 3 (range, 1-13), and 37% of patients had refractory disease.
Patients received cerdulatinib at 25, 30, or 35 mg twice daily (BID). A total of 101 patients were evaluable as of May 4, 2018.
Response
The objective response rate (ORR) was 47% in the entire population. Thirteen patients achieved a complete response (CR), and 34 had a partial response (PR). Thirty-four patients remained on cerdulatinib at the data cut-off.
The ORR was 46% in the FL patients, with 3 patients achieving a CR and 13 achieving a PR. Thirteen FL patients remained on cerdulatinib.
In the CLL/SLL patients, the ORR was 61%. Two patients had a CR, and 15 had a PR. Four CLL/SLL patients remained on cerdulatinib.
In PTCL, the ORR was 35%. All 7 responders had a CR. Eleven PTCL patients remained on cerdulatinib.
Only 1 CTCL patient was evaluable, but this patient achieved a CR and remained on cerdulatinib.
The ORR was 42% for patients with other indolent NHLs, with 5 PRs and no CRs. Only 1 patient in this group remained on cerdulatinib.
For aggressive NHL, the ORR was 20%, with 1 PR and no CRs. None of the patients in this group stayed on cerdulatinib.
“Cerdulatinib continues to demonstrate promising results across a wide range of B- and T-cell malignancies, including early indications of the potential for durable responses,” said study investigator Paul Hamlin, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“The new signals in relapsed/refractory PTCL and CTCL are particularly compelling when you consider the limited treatment options for patients that fail frontline therapy.”
Safety
Grade 3 or higher adverse events included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
The 5 deaths due to sepsis or septic shock (3 of which were concomitant with pneumonia) were considered related to cerdulatinib. Three of the deaths occurred in patients with CLL, 1 in a DLBCL patient, and 1 in an FL patient.
“One of the things we have seen [with CLL patients] is the background infection rate is quite a bit higher,” said John T. Curnutte, MD, PhD, interim co-president and head of research and development at Portola Pharmaceuticals.
“You see this with multiple other agents, so we were not particularly surprised to see [sepsis/septic shock in CLL].”
Dr Curnutte noted that grade 5 sepsis/septic shock tended to occur in patients who were pre-colonized and/or had high plasma levels of cerdulatinib.
So, to prevent these adverse events, the starting dose of cerdulatinib was lowered, investigators began monitoring patients’ plasma levels, and all patients began receiving antibiotic prophylaxis. (Previously, only CLL patients had received this prophylaxis.)
The investigators found that lowering the starting dose from 35 mg BID to 30 mg or even 25 mg BID reduced plasma levels.
“At the 35 mg dose, 1 out of every 4 patients showed accumulation of the drug,” Dr Curnutte said. “In general, the use of the 30 mg BID or step-down 25 mg BID did not result in accumulation of drug.”
Dr Curnutte also noted that enrollment of CLL/SLL patients is complete, and investigators would be “very careful” if the study were to be re-opened to these patients.
For now, Portola is focused on completing enrollment in other patient groups on this phase 2 trial. The company is also hoping to conduct a phase 3 trial of cerdulatinib in PTCL that could begin as early as the end of this year.
STOCKHOLM—The dual SYK/JAK inhibitor cerdulatinib has demonstrated efficacy in a phase 2 trial of patients with heavily pretreated B- and T-cell non-Hodgkin lymphomas (NHLs).
There were a few deaths due to sepsis or septic shock that were considered related to cerdulatinib, but investigators have taken steps to prevent additional deaths.
Cerdulatinib produced responses in patients with peripheral T-cell lymphoma (PTCL), cutaneous T-cell lymphoma (CTCL), chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other NHLs.
The 5 deaths due to sepsis or septic shock (3 concomitant with pneumonia) occurred early on in the trial, and dose reductions, monitoring, and antibiotic prophylaxis appeared to be effective in preventing additional deaths.
Results from this trial were presented in a poster (abstract PF437) at the 23rd Congress of the European Hematology Association (EHA).
The research was sponsored by Portola Pharmaceuticals, Inc.
The trial enrolled 114 patients. They had FL (grade 1-3A; n=39), PTCL (n=25), CTCL (n=5), CLL/SLL (n=28), other indolent NHLs (Waldenstrom’s macroglobulinemia and marginal zone lymphoma; n=12), or aggressive NHL (defined as diffuse large B-cell lymphoma [DLBCL], grade 3B FL, mantle cell lymphoma, and transformed NHL with relapsed disease; n=5).
The patients’ median age was 68 (range, 34-93), and 59% were male. The median number of prior treatment regimens was 3 (range, 1-13), and 37% of patients had refractory disease.
Patients received cerdulatinib at 25, 30, or 35 mg twice daily (BID). A total of 101 patients were evaluable as of May 4, 2018.
Response
The objective response rate (ORR) was 47% in the entire population. Thirteen patients achieved a complete response (CR), and 34 had a partial response (PR). Thirty-four patients remained on cerdulatinib at the data cut-off.
The ORR was 46% in the FL patients, with 3 patients achieving a CR and 13 achieving a PR. Thirteen FL patients remained on cerdulatinib.
In the CLL/SLL patients, the ORR was 61%. Two patients had a CR, and 15 had a PR. Four CLL/SLL patients remained on cerdulatinib.
In PTCL, the ORR was 35%. All 7 responders had a CR. Eleven PTCL patients remained on cerdulatinib.
Only 1 CTCL patient was evaluable, but this patient achieved a CR and remained on cerdulatinib.
The ORR was 42% for patients with other indolent NHLs, with 5 PRs and no CRs. Only 1 patient in this group remained on cerdulatinib.
For aggressive NHL, the ORR was 20%, with 1 PR and no CRs. None of the patients in this group stayed on cerdulatinib.
“Cerdulatinib continues to demonstrate promising results across a wide range of B- and T-cell malignancies, including early indications of the potential for durable responses,” said study investigator Paul Hamlin, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“The new signals in relapsed/refractory PTCL and CTCL are particularly compelling when you consider the limited treatment options for patients that fail frontline therapy.”
Safety
Grade 3 or higher adverse events included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
The 5 deaths due to sepsis or septic shock (3 of which were concomitant with pneumonia) were considered related to cerdulatinib. Three of the deaths occurred in patients with CLL, 1 in a DLBCL patient, and 1 in an FL patient.
“One of the things we have seen [with CLL patients] is the background infection rate is quite a bit higher,” said John T. Curnutte, MD, PhD, interim co-president and head of research and development at Portola Pharmaceuticals.
“You see this with multiple other agents, so we were not particularly surprised to see [sepsis/septic shock in CLL].”
Dr Curnutte noted that grade 5 sepsis/septic shock tended to occur in patients who were pre-colonized and/or had high plasma levels of cerdulatinib.
So, to prevent these adverse events, the starting dose of cerdulatinib was lowered, investigators began monitoring patients’ plasma levels, and all patients began receiving antibiotic prophylaxis. (Previously, only CLL patients had received this prophylaxis.)
The investigators found that lowering the starting dose from 35 mg BID to 30 mg or even 25 mg BID reduced plasma levels.
“At the 35 mg dose, 1 out of every 4 patients showed accumulation of the drug,” Dr Curnutte said. “In general, the use of the 30 mg BID or step-down 25 mg BID did not result in accumulation of drug.”
Dr Curnutte also noted that enrollment of CLL/SLL patients is complete, and investigators would be “very careful” if the study were to be re-opened to these patients.
For now, Portola is focused on completing enrollment in other patient groups on this phase 2 trial. The company is also hoping to conduct a phase 3 trial of cerdulatinib in PTCL that could begin as early as the end of this year.
EC grants blinatumomab full approval
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.