User login
Treatments, disease affect spermatogonia in boys
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
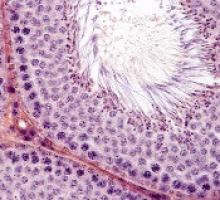
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Fitness trackers help monitor cancer patients
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
NIH aims to improve access to cloud computing
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
Drug approved for radical cure of P vivax malaria
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
Team finds potential therapeutic targets for T-ALL
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
GPS receives fast track designation for MM
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
FDA approves drug for IDH1-mutated AML
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
FDA approves biosimilar filgrastim
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
Tool may reveal optimal time for SCT in MF
A new tool can help patients with myelofibrosis (MF) decide when to pursue stem cell transplant (SCT), according to the MPN Research Foundation.
The SCT Spectrum Transplant Timing tool (SSTT) is an online MF risk calculator.
It is designed to inform patients of their risk status in a timely manner so they can be proactive in speaking to their doctors about SCT.
“There is an optimal time to start SCT, simply because the odds of success soar in our favor when we start early rather than late in the game,” said Zhenya Senyak, editor of MPN Forum, an MF patient, and creator of the SSTT.
“The SCT Spectrum Timing Tool can help inform the timing of that decision.”
The SSTT incorporates the Dynamic International Prognostic Scoring System (DIPSS), asking patients about their age, white blood cell count, hemoglobin level, peripheral blood blast percentage, and constitutional symptoms.
Patients’ answers are used to create a color signal that indicates their current MF risk level. Accompanying information explains what the risk level means, provides median survival times for that level, and alerts patients of the relative urgency of SCT.
Patients can review these results with their hematologist to ensure accuracy and incorporate risk factors not measured by the SSTT.
The SSTT also includes resources to support SCT discussions between patients and hematologists.
Senyak created SSTT with help from the MPN SCT Transplantation Timing Taskforce, a group of 18 MPN and transplant specialists, patient advocates, and SCT survivors. The work was sponsored by the MPN Research Foundation.
“The decision of whether or not to pursue a stem cell transplant is incredibly fraught for any person,” said Ruben Mesa, MD, a member of the MPN SCT Transplantation Timing Taskforce.
“Our hope in assisting with this effort is to lend our knowledge and experience to create a guide to assist with patient-doctor communication around this very complicated issue.”
A new tool can help patients with myelofibrosis (MF) decide when to pursue stem cell transplant (SCT), according to the MPN Research Foundation.
The SCT Spectrum Transplant Timing tool (SSTT) is an online MF risk calculator.
It is designed to inform patients of their risk status in a timely manner so they can be proactive in speaking to their doctors about SCT.
“There is an optimal time to start SCT, simply because the odds of success soar in our favor when we start early rather than late in the game,” said Zhenya Senyak, editor of MPN Forum, an MF patient, and creator of the SSTT.
“The SCT Spectrum Timing Tool can help inform the timing of that decision.”
The SSTT incorporates the Dynamic International Prognostic Scoring System (DIPSS), asking patients about their age, white blood cell count, hemoglobin level, peripheral blood blast percentage, and constitutional symptoms.
Patients’ answers are used to create a color signal that indicates their current MF risk level. Accompanying information explains what the risk level means, provides median survival times for that level, and alerts patients of the relative urgency of SCT.
Patients can review these results with their hematologist to ensure accuracy and incorporate risk factors not measured by the SSTT.
The SSTT also includes resources to support SCT discussions between patients and hematologists.
Senyak created SSTT with help from the MPN SCT Transplantation Timing Taskforce, a group of 18 MPN and transplant specialists, patient advocates, and SCT survivors. The work was sponsored by the MPN Research Foundation.
“The decision of whether or not to pursue a stem cell transplant is incredibly fraught for any person,” said Ruben Mesa, MD, a member of the MPN SCT Transplantation Timing Taskforce.
“Our hope in assisting with this effort is to lend our knowledge and experience to create a guide to assist with patient-doctor communication around this very complicated issue.”
A new tool can help patients with myelofibrosis (MF) decide when to pursue stem cell transplant (SCT), according to the MPN Research Foundation.
The SCT Spectrum Transplant Timing tool (SSTT) is an online MF risk calculator.
It is designed to inform patients of their risk status in a timely manner so they can be proactive in speaking to their doctors about SCT.
“There is an optimal time to start SCT, simply because the odds of success soar in our favor when we start early rather than late in the game,” said Zhenya Senyak, editor of MPN Forum, an MF patient, and creator of the SSTT.
“The SCT Spectrum Timing Tool can help inform the timing of that decision.”
The SSTT incorporates the Dynamic International Prognostic Scoring System (DIPSS), asking patients about their age, white blood cell count, hemoglobin level, peripheral blood blast percentage, and constitutional symptoms.
Patients’ answers are used to create a color signal that indicates their current MF risk level. Accompanying information explains what the risk level means, provides median survival times for that level, and alerts patients of the relative urgency of SCT.
Patients can review these results with their hematologist to ensure accuracy and incorporate risk factors not measured by the SSTT.
The SSTT also includes resources to support SCT discussions between patients and hematologists.
Senyak created SSTT with help from the MPN SCT Transplantation Timing Taskforce, a group of 18 MPN and transplant specialists, patient advocates, and SCT survivors. The work was sponsored by the MPN Research Foundation.
“The decision of whether or not to pursue a stem cell transplant is incredibly fraught for any person,” said Ruben Mesa, MD, a member of the MPN SCT Transplantation Timing Taskforce.
“Our hope in assisting with this effort is to lend our knowledge and experience to create a guide to assist with patient-doctor communication around this very complicated issue.”
Kinase may be therapeutic target for hemoglobinopathies
A kinase called heme-regulated inhibitor (HRI) could be a therapeutic target for sickle cell disease (SCD) and some forms of β-thalassemia, according to researchers.
The team found that reducing the activity of HRI (also known as EIF2AK1) can boost the production of fetal hemoglobin (HbF).
Gerd Blobel MD, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania, and his colleagues reported this discovery in Science.
Dr Blobel noted that hydroxyurea remains the only approved drug that can increase fetal Hb in adults.
“Our goal was to identify new potential drug targets that regulate fetal Hb levels,” he said.
To that end, the researchers conducted a CRISPR-Cas9 screen targeting protein kinases. They designed a library of single-guide RNAs targeting 482 kinase domains, which covered almost all known kinases in the human genome.
The team attempted to determine if interference with any of the kinases in an immortalized human red blood cell line would increase HbF levels.
Results suggested that HRI, an erythroid-specific kinase that controls protein translation, is a repressor of HbF.
To confirm that HRI plays a key role in regulating HbF levels, the researchers depleted HRI in primary cultured human red blood cell precursors.
Reduced activity of HRI resulted in decreased phosphorylation of eIF2a and increased levels of HbF, but interfering with HRI levels did not impair cell viability or maturation.
The researchers next showed that HRI was a repressor of HbF in cultured primary cells from patients with SCD.
When HRI levels were artificially reduced, HbF levels were significantly increased, and cells were less prone to sickling. This suggested to the researchers that “HRI depletion may achieve therapeutically relevant levels of HbF.”
Mechanistically, the effects of HRI on HbF were shown to occur, in large measure, through modulating the activity of BCL11A, a direct repressor of HbF transcription.
The observation that HRI inhibition elevated HbF levels and reduced cell sickling in culture suggested that future pharmacologic HRI inhibitors might provide clinical benefit in patients with SCD.
To that end, an important aspect of this work was to determine if the effect of HRI inhibition could be increased with another drug added to the mix, Dr Blobel said.
He and his colleagues therefore tested whether pomalidomide, which was previously shown to increase HbF in an experimental setting, could be such a drug.
HRI depletion in combination with pomalidomide treatment raised HbF levels more than either treatment alone, suggesting that HRI inhibition might be combined with another HbF-inducing drug to increase the therapeutic index.
A kinase called heme-regulated inhibitor (HRI) could be a therapeutic target for sickle cell disease (SCD) and some forms of β-thalassemia, according to researchers.
The team found that reducing the activity of HRI (also known as EIF2AK1) can boost the production of fetal hemoglobin (HbF).
Gerd Blobel MD, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania, and his colleagues reported this discovery in Science.
Dr Blobel noted that hydroxyurea remains the only approved drug that can increase fetal Hb in adults.
“Our goal was to identify new potential drug targets that regulate fetal Hb levels,” he said.
To that end, the researchers conducted a CRISPR-Cas9 screen targeting protein kinases. They designed a library of single-guide RNAs targeting 482 kinase domains, which covered almost all known kinases in the human genome.
The team attempted to determine if interference with any of the kinases in an immortalized human red blood cell line would increase HbF levels.
Results suggested that HRI, an erythroid-specific kinase that controls protein translation, is a repressor of HbF.
To confirm that HRI plays a key role in regulating HbF levels, the researchers depleted HRI in primary cultured human red blood cell precursors.
Reduced activity of HRI resulted in decreased phosphorylation of eIF2a and increased levels of HbF, but interfering with HRI levels did not impair cell viability or maturation.
The researchers next showed that HRI was a repressor of HbF in cultured primary cells from patients with SCD.
When HRI levels were artificially reduced, HbF levels were significantly increased, and cells were less prone to sickling. This suggested to the researchers that “HRI depletion may achieve therapeutically relevant levels of HbF.”
Mechanistically, the effects of HRI on HbF were shown to occur, in large measure, through modulating the activity of BCL11A, a direct repressor of HbF transcription.
The observation that HRI inhibition elevated HbF levels and reduced cell sickling in culture suggested that future pharmacologic HRI inhibitors might provide clinical benefit in patients with SCD.
To that end, an important aspect of this work was to determine if the effect of HRI inhibition could be increased with another drug added to the mix, Dr Blobel said.
He and his colleagues therefore tested whether pomalidomide, which was previously shown to increase HbF in an experimental setting, could be such a drug.
HRI depletion in combination with pomalidomide treatment raised HbF levels more than either treatment alone, suggesting that HRI inhibition might be combined with another HbF-inducing drug to increase the therapeutic index.
A kinase called heme-regulated inhibitor (HRI) could be a therapeutic target for sickle cell disease (SCD) and some forms of β-thalassemia, according to researchers.
The team found that reducing the activity of HRI (also known as EIF2AK1) can boost the production of fetal hemoglobin (HbF).
Gerd Blobel MD, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania, and his colleagues reported this discovery in Science.
Dr Blobel noted that hydroxyurea remains the only approved drug that can increase fetal Hb in adults.
“Our goal was to identify new potential drug targets that regulate fetal Hb levels,” he said.
To that end, the researchers conducted a CRISPR-Cas9 screen targeting protein kinases. They designed a library of single-guide RNAs targeting 482 kinase domains, which covered almost all known kinases in the human genome.
The team attempted to determine if interference with any of the kinases in an immortalized human red blood cell line would increase HbF levels.
Results suggested that HRI, an erythroid-specific kinase that controls protein translation, is a repressor of HbF.
To confirm that HRI plays a key role in regulating HbF levels, the researchers depleted HRI in primary cultured human red blood cell precursors.
Reduced activity of HRI resulted in decreased phosphorylation of eIF2a and increased levels of HbF, but interfering with HRI levels did not impair cell viability or maturation.
The researchers next showed that HRI was a repressor of HbF in cultured primary cells from patients with SCD.
When HRI levels were artificially reduced, HbF levels were significantly increased, and cells were less prone to sickling. This suggested to the researchers that “HRI depletion may achieve therapeutically relevant levels of HbF.”
Mechanistically, the effects of HRI on HbF were shown to occur, in large measure, through modulating the activity of BCL11A, a direct repressor of HbF transcription.
The observation that HRI inhibition elevated HbF levels and reduced cell sickling in culture suggested that future pharmacologic HRI inhibitors might provide clinical benefit in patients with SCD.
To that end, an important aspect of this work was to determine if the effect of HRI inhibition could be increased with another drug added to the mix, Dr Blobel said.
He and his colleagues therefore tested whether pomalidomide, which was previously shown to increase HbF in an experimental setting, could be such a drug.
HRI depletion in combination with pomalidomide treatment raised HbF levels more than either treatment alone, suggesting that HRI inhibition might be combined with another HbF-inducing drug to increase the therapeutic index.