User login
Hemophilia treatment falling short, study suggests

Results of a real-world, retrospective study suggest there may be a need to improve the standard of care for hemophilia A and B in some European countries.
Hemophilia treatment practices varied widely among the 7 countries studied, as did annual bleeding rates (ABRs).
Some countries had low median ABRs in hemophilia A and B patients receiving prophylaxis—in the range of 1.0 to 2.0.
However, the median ABR was as high as 8.0 for some patients, despite receiving prophylaxis. And these were patients with moderate disease.
The study, which was sponsored by Sobi, was published in Haemophilia.
“The overall results indicate that there is a significant need to advance standard of care within hemophilia,” said Stefan Lethagen, vice president medical & clinical sciences, haemophilia at Sobi.
“Even when prophylaxis is the norm, it appears that prophylactic treatment is driven to the minimal acceptable level or even lower, which increases the risk of joint injury and limits the ability to live a full and active life.”
The study was designed to provide insight into current hemophilia treatment practice and outcomes in 7 European countries—Belgium, France, Germany, Italy, Spain, Sweden, and the UK.
The researchers analyzed data on 1346 patients with hemophilia A and 312 with hemophilia B treated in these countries.
Treatment type, dosing
Prophylaxis was, overall, the most dominating treatment for patients with severe hemophilia A. It was the most common treatment regimen among children and decreased with increasing age.
On-demand treatment was reported to be most common in moderate hemophilia A, and there was no trend across age groups.
For patients with hemophilia B, prophylaxis was the most common treatment in 4 out of the 7 countries (France, Germany, Sweden, and UK).
Overall, a majority of patients received a recombinant antihemophilic factor product as opposed to a plasma-derived product. The one exception was patients with hemophilia B in Germany. A majority of these patients (66%) received a plasma-derived product.
The mean prescribed prophylactic treatment ranged from 67.9 IU kg-1 per week (Belgium) to 108.4 IU kg-1 per week (Germany) for hemophilia A and 32.3 IU kg-1 per week (Belgium) to 97.7 IU kg-1 per week (France) for hemophilia B.
Most patients on prophylaxis were treated 3 or more times a week if they had hemophilia A and 2 times a week if they had hemophilia B.
ABRs across countries
For hemophilia A patients on prophylaxis, the median ABR ranged from 1.0 (Belgium, Italy, Sweden) to 4.0 (France, UK) for patients with severe disease and from 2.0 (Sweden) to 8.0 (Belgium) for patients with moderate disease.
The researchers pointed out that ABRs were higher for patients with moderate hemophilia A, but low patient numbers should be taken into account when interpreting these data.
The median ABRs for hemophilia A patients who received on-demand treatment ranged from 4.5 (Sweden) to 18.0 (UK, Belgium) for patients with severe disease and from 1.0 (Spain, Sweden) to 12.0 (UK) for patients with moderate disease.
For hemophilia B patients on prophylaxis, the median ABRs ranged from 1.0 (Germany, Sweden) to 6.0 (Belgium) for patients with severe disease and from 1.5 (Sweden) to 8.0 (Belgium) for patients with moderate disease. Again, ABRs were higher for patients with moderate disease.
The median ABRs for hemophilia B patients who received on-demand treatment ranged from 1.5 (Germany) to 14.0 (UK) for patients with severe disease and from 1.0 (Belgium, France, Germany, Italy) to 6.5 (UK) for patients with moderate disease.
The researchers said the high number of bleeds observed in some patients likely reflects insufficient therapy, inappropriate dose-interval, presence of target joints, poor adherence, or patient difficulty in correctly assessing bleeds.
The team said the overall results of the study suggest there is room for improvement of hemophilia therapy, even for patients currently on prophylactic treatment. ![]()

Results of a real-world, retrospective study suggest there may be a need to improve the standard of care for hemophilia A and B in some European countries.
Hemophilia treatment practices varied widely among the 7 countries studied, as did annual bleeding rates (ABRs).
Some countries had low median ABRs in hemophilia A and B patients receiving prophylaxis—in the range of 1.0 to 2.0.
However, the median ABR was as high as 8.0 for some patients, despite receiving prophylaxis. And these were patients with moderate disease.
The study, which was sponsored by Sobi, was published in Haemophilia.
“The overall results indicate that there is a significant need to advance standard of care within hemophilia,” said Stefan Lethagen, vice president medical & clinical sciences, haemophilia at Sobi.
“Even when prophylaxis is the norm, it appears that prophylactic treatment is driven to the minimal acceptable level or even lower, which increases the risk of joint injury and limits the ability to live a full and active life.”
The study was designed to provide insight into current hemophilia treatment practice and outcomes in 7 European countries—Belgium, France, Germany, Italy, Spain, Sweden, and the UK.
The researchers analyzed data on 1346 patients with hemophilia A and 312 with hemophilia B treated in these countries.
Treatment type, dosing
Prophylaxis was, overall, the most dominating treatment for patients with severe hemophilia A. It was the most common treatment regimen among children and decreased with increasing age.
On-demand treatment was reported to be most common in moderate hemophilia A, and there was no trend across age groups.
For patients with hemophilia B, prophylaxis was the most common treatment in 4 out of the 7 countries (France, Germany, Sweden, and UK).
Overall, a majority of patients received a recombinant antihemophilic factor product as opposed to a plasma-derived product. The one exception was patients with hemophilia B in Germany. A majority of these patients (66%) received a plasma-derived product.
The mean prescribed prophylactic treatment ranged from 67.9 IU kg-1 per week (Belgium) to 108.4 IU kg-1 per week (Germany) for hemophilia A and 32.3 IU kg-1 per week (Belgium) to 97.7 IU kg-1 per week (France) for hemophilia B.
Most patients on prophylaxis were treated 3 or more times a week if they had hemophilia A and 2 times a week if they had hemophilia B.
ABRs across countries
For hemophilia A patients on prophylaxis, the median ABR ranged from 1.0 (Belgium, Italy, Sweden) to 4.0 (France, UK) for patients with severe disease and from 2.0 (Sweden) to 8.0 (Belgium) for patients with moderate disease.
The researchers pointed out that ABRs were higher for patients with moderate hemophilia A, but low patient numbers should be taken into account when interpreting these data.
The median ABRs for hemophilia A patients who received on-demand treatment ranged from 4.5 (Sweden) to 18.0 (UK, Belgium) for patients with severe disease and from 1.0 (Spain, Sweden) to 12.0 (UK) for patients with moderate disease.
For hemophilia B patients on prophylaxis, the median ABRs ranged from 1.0 (Germany, Sweden) to 6.0 (Belgium) for patients with severe disease and from 1.5 (Sweden) to 8.0 (Belgium) for patients with moderate disease. Again, ABRs were higher for patients with moderate disease.
The median ABRs for hemophilia B patients who received on-demand treatment ranged from 1.5 (Germany) to 14.0 (UK) for patients with severe disease and from 1.0 (Belgium, France, Germany, Italy) to 6.5 (UK) for patients with moderate disease.
The researchers said the high number of bleeds observed in some patients likely reflects insufficient therapy, inappropriate dose-interval, presence of target joints, poor adherence, or patient difficulty in correctly assessing bleeds.
The team said the overall results of the study suggest there is room for improvement of hemophilia therapy, even for patients currently on prophylactic treatment. ![]()

Results of a real-world, retrospective study suggest there may be a need to improve the standard of care for hemophilia A and B in some European countries.
Hemophilia treatment practices varied widely among the 7 countries studied, as did annual bleeding rates (ABRs).
Some countries had low median ABRs in hemophilia A and B patients receiving prophylaxis—in the range of 1.0 to 2.0.
However, the median ABR was as high as 8.0 for some patients, despite receiving prophylaxis. And these were patients with moderate disease.
The study, which was sponsored by Sobi, was published in Haemophilia.
“The overall results indicate that there is a significant need to advance standard of care within hemophilia,” said Stefan Lethagen, vice president medical & clinical sciences, haemophilia at Sobi.
“Even when prophylaxis is the norm, it appears that prophylactic treatment is driven to the minimal acceptable level or even lower, which increases the risk of joint injury and limits the ability to live a full and active life.”
The study was designed to provide insight into current hemophilia treatment practice and outcomes in 7 European countries—Belgium, France, Germany, Italy, Spain, Sweden, and the UK.
The researchers analyzed data on 1346 patients with hemophilia A and 312 with hemophilia B treated in these countries.
Treatment type, dosing
Prophylaxis was, overall, the most dominating treatment for patients with severe hemophilia A. It was the most common treatment regimen among children and decreased with increasing age.
On-demand treatment was reported to be most common in moderate hemophilia A, and there was no trend across age groups.
For patients with hemophilia B, prophylaxis was the most common treatment in 4 out of the 7 countries (France, Germany, Sweden, and UK).
Overall, a majority of patients received a recombinant antihemophilic factor product as opposed to a plasma-derived product. The one exception was patients with hemophilia B in Germany. A majority of these patients (66%) received a plasma-derived product.
The mean prescribed prophylactic treatment ranged from 67.9 IU kg-1 per week (Belgium) to 108.4 IU kg-1 per week (Germany) for hemophilia A and 32.3 IU kg-1 per week (Belgium) to 97.7 IU kg-1 per week (France) for hemophilia B.
Most patients on prophylaxis were treated 3 or more times a week if they had hemophilia A and 2 times a week if they had hemophilia B.
ABRs across countries
For hemophilia A patients on prophylaxis, the median ABR ranged from 1.0 (Belgium, Italy, Sweden) to 4.0 (France, UK) for patients with severe disease and from 2.0 (Sweden) to 8.0 (Belgium) for patients with moderate disease.
The researchers pointed out that ABRs were higher for patients with moderate hemophilia A, but low patient numbers should be taken into account when interpreting these data.
The median ABRs for hemophilia A patients who received on-demand treatment ranged from 4.5 (Sweden) to 18.0 (UK, Belgium) for patients with severe disease and from 1.0 (Spain, Sweden) to 12.0 (UK) for patients with moderate disease.
For hemophilia B patients on prophylaxis, the median ABRs ranged from 1.0 (Germany, Sweden) to 6.0 (Belgium) for patients with severe disease and from 1.5 (Sweden) to 8.0 (Belgium) for patients with moderate disease. Again, ABRs were higher for patients with moderate disease.
The median ABRs for hemophilia B patients who received on-demand treatment ranged from 1.5 (Germany) to 14.0 (UK) for patients with severe disease and from 1.0 (Belgium, France, Germany, Italy) to 6.5 (UK) for patients with moderate disease.
The researchers said the high number of bleeds observed in some patients likely reflects insufficient therapy, inappropriate dose-interval, presence of target joints, poor adherence, or patient difficulty in correctly assessing bleeds.
The team said the overall results of the study suggest there is room for improvement of hemophilia therapy, even for patients currently on prophylactic treatment. ![]()
Company withdraws application for eryaspase in ALL
ERYTECH Pharma has announced its decision to withdraw the European marketing authorization application (MAA) for eryaspase (GRASPA®) as a treatment for acute lymphoblastic leukemia (ALL).
The European Medicines Agency’s (EMA’s) Committee for Medicinal Products for Human Use (CHMP) asked for additional data on eryaspase, but ERYTECH said the time allowed by the EMA’s approval process is not sufficient to provide the data requested.
Therefore, the company decided to withdraw the MAA and resubmit it next year.
About eryaspase
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Research has suggested this delivery system provides improved pharmacodynamics, protecting L-asparaginase from circulating proteolytic enzymes and preventing early liver or renal clearance.
The system also appears to reduce the risk of adverse events compared to native L-asparaginase.
The EMA and the US Food and Drug Administration have granted orphan drug designations for eryaspase for the treatment of ALL, acute myeloid
leukemia, and pancreatic cancer.
About the MAA
ERYTECH submitted an MAA for eryaspase in September 2015, based on positive results from a phase 2/3 study in which researchers compared eryaspase and native L-asparaginase in patients with relapsed and refractory ALL.
One year later (September 2016), the company received the CHMP’s Day 180 List of Outstanding Issues, which highlighted the need for additional data.
Specifically, the CHMP asked for data regarding the comparability between the old and new form of asparaginase encapsulated in eryaspase and the development of a new immunogenicity assay, as well as the pharmacodynamic effects of eryaspase.
Given the fact that the generation of these data will require more time than allowed in the EMA’s approval procedures, ERYTECH has notified the CHMP of the withdrawal of the MAA.
The company intends to resubmit the MAA in mid-2017, as soon as the newly generated data are available.
ERYTECH stressed that there have been no safety issues with eryaspase, and the withdrawal of this MAA will not affect any ongoing trials.
“We are committed to pursuing regulatory approval for GRASPA and intend to work closely with our investigators and advisors to generate the additional information requested and to resubmit an MAA next year,” said Iman El-Hariry, chief medical officer of ERYTECH.
“We believe we have generated strong clinical data in our different programs of eryaspase, and we continue to execute our plans towards making the product available to patients with aggressive forms of cancer, such as acute lymphoblastic leukemia, acute myeloid leukemia, and pancreatic cancer,” added Gil Beyen, ERYTECH’s chairman and chief executive officer. ![]()
ERYTECH Pharma has announced its decision to withdraw the European marketing authorization application (MAA) for eryaspase (GRASPA®) as a treatment for acute lymphoblastic leukemia (ALL).
The European Medicines Agency’s (EMA’s) Committee for Medicinal Products for Human Use (CHMP) asked for additional data on eryaspase, but ERYTECH said the time allowed by the EMA’s approval process is not sufficient to provide the data requested.
Therefore, the company decided to withdraw the MAA and resubmit it next year.
About eryaspase
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Research has suggested this delivery system provides improved pharmacodynamics, protecting L-asparaginase from circulating proteolytic enzymes and preventing early liver or renal clearance.
The system also appears to reduce the risk of adverse events compared to native L-asparaginase.
The EMA and the US Food and Drug Administration have granted orphan drug designations for eryaspase for the treatment of ALL, acute myeloid
leukemia, and pancreatic cancer.
About the MAA
ERYTECH submitted an MAA for eryaspase in September 2015, based on positive results from a phase 2/3 study in which researchers compared eryaspase and native L-asparaginase in patients with relapsed and refractory ALL.
One year later (September 2016), the company received the CHMP’s Day 180 List of Outstanding Issues, which highlighted the need for additional data.
Specifically, the CHMP asked for data regarding the comparability between the old and new form of asparaginase encapsulated in eryaspase and the development of a new immunogenicity assay, as well as the pharmacodynamic effects of eryaspase.
Given the fact that the generation of these data will require more time than allowed in the EMA’s approval procedures, ERYTECH has notified the CHMP of the withdrawal of the MAA.
The company intends to resubmit the MAA in mid-2017, as soon as the newly generated data are available.
ERYTECH stressed that there have been no safety issues with eryaspase, and the withdrawal of this MAA will not affect any ongoing trials.
“We are committed to pursuing regulatory approval for GRASPA and intend to work closely with our investigators and advisors to generate the additional information requested and to resubmit an MAA next year,” said Iman El-Hariry, chief medical officer of ERYTECH.
“We believe we have generated strong clinical data in our different programs of eryaspase, and we continue to execute our plans towards making the product available to patients with aggressive forms of cancer, such as acute lymphoblastic leukemia, acute myeloid leukemia, and pancreatic cancer,” added Gil Beyen, ERYTECH’s chairman and chief executive officer. ![]()
ERYTECH Pharma has announced its decision to withdraw the European marketing authorization application (MAA) for eryaspase (GRASPA®) as a treatment for acute lymphoblastic leukemia (ALL).
The European Medicines Agency’s (EMA’s) Committee for Medicinal Products for Human Use (CHMP) asked for additional data on eryaspase, but ERYTECH said the time allowed by the EMA’s approval process is not sufficient to provide the data requested.
Therefore, the company decided to withdraw the MAA and resubmit it next year.
About eryaspase
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Research has suggested this delivery system provides improved pharmacodynamics, protecting L-asparaginase from circulating proteolytic enzymes and preventing early liver or renal clearance.
The system also appears to reduce the risk of adverse events compared to native L-asparaginase.
The EMA and the US Food and Drug Administration have granted orphan drug designations for eryaspase for the treatment of ALL, acute myeloid
leukemia, and pancreatic cancer.
About the MAA
ERYTECH submitted an MAA for eryaspase in September 2015, based on positive results from a phase 2/3 study in which researchers compared eryaspase and native L-asparaginase in patients with relapsed and refractory ALL.
One year later (September 2016), the company received the CHMP’s Day 180 List of Outstanding Issues, which highlighted the need for additional data.
Specifically, the CHMP asked for data regarding the comparability between the old and new form of asparaginase encapsulated in eryaspase and the development of a new immunogenicity assay, as well as the pharmacodynamic effects of eryaspase.
Given the fact that the generation of these data will require more time than allowed in the EMA’s approval procedures, ERYTECH has notified the CHMP of the withdrawal of the MAA.
The company intends to resubmit the MAA in mid-2017, as soon as the newly generated data are available.
ERYTECH stressed that there have been no safety issues with eryaspase, and the withdrawal of this MAA will not affect any ongoing trials.
“We are committed to pursuing regulatory approval for GRASPA and intend to work closely with our investigators and advisors to generate the additional information requested and to resubmit an MAA next year,” said Iman El-Hariry, chief medical officer of ERYTECH.
“We believe we have generated strong clinical data in our different programs of eryaspase, and we continue to execute our plans towards making the product available to patients with aggressive forms of cancer, such as acute lymphoblastic leukemia, acute myeloid leukemia, and pancreatic cancer,” added Gil Beyen, ERYTECH’s chairman and chief executive officer. ![]()
MRI detects early stages of MF in mice

Magnetic resonance imaging (MRI) can effectively detect myelofibrosis (MF) in a mouse model, according to research published in the journal Blood Cancer.
In fact, researchers found that MRI could detect early and late stages of primary MF.
The researchers believe this discovery could potentially change the way MF is diagnosed, as MRI might be used to help physicians decide if or where to biopsy.
Katya Ravid, PhD, of Boston University School of Medicine in Massachusetts, and her colleagues conducted this research, aiming to determine whether T2-weighted MRI could detect bone marrow fibrosis in a mouse model of primary MF.
The team looked specifically at how effectively MRI could detect MF during the pre-fibrotic stage (when mice were less than 16 weeks old), when the mice had early MF (16 to 36 weeks old), and once the mice had overt MF (older than 36 weeks).
The researchers found that MRI could detect MF at the pre-fibrotic stage as well as detecting progressive MF.
The team said they observed a clear, bright signal that allowed them to differentiate mice with MF from healthy control mice.
The researchers proposed that the abundance of large megakaryocytes contributed to the bright signal they observed, since, in T2-weighted MR images, increased water/proton content, as in increased cellularity, yields high MR-signal intensity.
The team said this study provides proof of concept that T2-weighted MRI can detect primary MF in the early and late stages. ![]()

Magnetic resonance imaging (MRI) can effectively detect myelofibrosis (MF) in a mouse model, according to research published in the journal Blood Cancer.
In fact, researchers found that MRI could detect early and late stages of primary MF.
The researchers believe this discovery could potentially change the way MF is diagnosed, as MRI might be used to help physicians decide if or where to biopsy.
Katya Ravid, PhD, of Boston University School of Medicine in Massachusetts, and her colleagues conducted this research, aiming to determine whether T2-weighted MRI could detect bone marrow fibrosis in a mouse model of primary MF.
The team looked specifically at how effectively MRI could detect MF during the pre-fibrotic stage (when mice were less than 16 weeks old), when the mice had early MF (16 to 36 weeks old), and once the mice had overt MF (older than 36 weeks).
The researchers found that MRI could detect MF at the pre-fibrotic stage as well as detecting progressive MF.
The team said they observed a clear, bright signal that allowed them to differentiate mice with MF from healthy control mice.
The researchers proposed that the abundance of large megakaryocytes contributed to the bright signal they observed, since, in T2-weighted MR images, increased water/proton content, as in increased cellularity, yields high MR-signal intensity.
The team said this study provides proof of concept that T2-weighted MRI can detect primary MF in the early and late stages. ![]()

Magnetic resonance imaging (MRI) can effectively detect myelofibrosis (MF) in a mouse model, according to research published in the journal Blood Cancer.
In fact, researchers found that MRI could detect early and late stages of primary MF.
The researchers believe this discovery could potentially change the way MF is diagnosed, as MRI might be used to help physicians decide if or where to biopsy.
Katya Ravid, PhD, of Boston University School of Medicine in Massachusetts, and her colleagues conducted this research, aiming to determine whether T2-weighted MRI could detect bone marrow fibrosis in a mouse model of primary MF.
The team looked specifically at how effectively MRI could detect MF during the pre-fibrotic stage (when mice were less than 16 weeks old), when the mice had early MF (16 to 36 weeks old), and once the mice had overt MF (older than 36 weeks).
The researchers found that MRI could detect MF at the pre-fibrotic stage as well as detecting progressive MF.
The team said they observed a clear, bright signal that allowed them to differentiate mice with MF from healthy control mice.
The researchers proposed that the abundance of large megakaryocytes contributed to the bright signal they observed, since, in T2-weighted MR images, increased water/proton content, as in increased cellularity, yields high MR-signal intensity.
The team said this study provides proof of concept that T2-weighted MRI can detect primary MF in the early and late stages. ![]()
Antiplatelet drugs produce similar results in PAD

Photo from AstraZeneca
NEW ORLEANS—Results of the EUCLID trial suggest ticagrelor does not a provide a benefit over clopidogrel in patients with symptomatic peripheral artery disease (PAD).
The incidence of atherothrombotic events was similar in patients who received ticagrelor and those who received clopidogrel.
Likewise, there was no significant difference between the treatment arms with regard to major bleeding.
Manesh R. Patel, MD, of Duke University Medical Center in Durham, North Carolina, presented results from the EUCLID trial at the American Heart Association Scientific Sessions.
Results were also published in NEJM. The trial was supported by AstraZeneca.
EUCLID included 13,885 patients with symptomatic PAD. They had median age of 66, and 72% were male.
The patients were randomized to receive ticagrelor at 90 mg twice daily or clopidogrel at 75 mg once daily.
The study’s primary efficacy endpoint was a composite of adjudicated cardiovascular death, myocardial infarction, and ischemic stroke.
At a median follow-up of 30 months, the primary efficacy endpoint had occurred in 10.8% (751/6930) of patients in the ticagrelor arm and 10.6% (740/6955) in the clopidogrel arm (P=0.65).
When the researchers assessed each of the components of the primary endpoint alone, they found a significant difference between the treatment groups in the incidence of ischemic stroke but not cardiovascular death or myocardial infarction.
Cardiovascular death occurred in 5.2% of patients in the ticagrelor arm and 4.9% of those in the clopidogrel arm (P=0.40). Myocardial infarction occurred in 5% and 4.8%, respectively (P=0.48). And ischemic stroke occurred in 1.9% and 2.4%, respectively (P=0.03).
The study’s primary safety endpoint was major bleeding, which occurred in 1.6% of patients in both treatment arms (P=0.49).
Fatal bleeding occurred in 0.1% of patients in the ticagrelor arm and 0.3% of patients in the clopidogrel arm (P=0.10). And intracranial bleeding occurred in 0.5% of patients in both arms (P=0.82).
However, significantly more patients discontinued ticagrelor due to bleeding—2.4%, compared to 1.6% of patients who discontinued clopidogrel due to bleeding (P<0.001).
Significantly more patients discontinued ticagrelor due to dyspnea as well—4.8% vs 0.8% (P<0.001).
In all, 30.1% of patients in the ticagrelor arm and 25.9% of those in the clopidogrel arm prematurely discontinued treatment. This includes patients who discontinued due to adverse events, meeting the primary efficacy endpoint, and death. ![]()

Photo from AstraZeneca
NEW ORLEANS—Results of the EUCLID trial suggest ticagrelor does not a provide a benefit over clopidogrel in patients with symptomatic peripheral artery disease (PAD).
The incidence of atherothrombotic events was similar in patients who received ticagrelor and those who received clopidogrel.
Likewise, there was no significant difference between the treatment arms with regard to major bleeding.
Manesh R. Patel, MD, of Duke University Medical Center in Durham, North Carolina, presented results from the EUCLID trial at the American Heart Association Scientific Sessions.
Results were also published in NEJM. The trial was supported by AstraZeneca.
EUCLID included 13,885 patients with symptomatic PAD. They had median age of 66, and 72% were male.
The patients were randomized to receive ticagrelor at 90 mg twice daily or clopidogrel at 75 mg once daily.
The study’s primary efficacy endpoint was a composite of adjudicated cardiovascular death, myocardial infarction, and ischemic stroke.
At a median follow-up of 30 months, the primary efficacy endpoint had occurred in 10.8% (751/6930) of patients in the ticagrelor arm and 10.6% (740/6955) in the clopidogrel arm (P=0.65).
When the researchers assessed each of the components of the primary endpoint alone, they found a significant difference between the treatment groups in the incidence of ischemic stroke but not cardiovascular death or myocardial infarction.
Cardiovascular death occurred in 5.2% of patients in the ticagrelor arm and 4.9% of those in the clopidogrel arm (P=0.40). Myocardial infarction occurred in 5% and 4.8%, respectively (P=0.48). And ischemic stroke occurred in 1.9% and 2.4%, respectively (P=0.03).
The study’s primary safety endpoint was major bleeding, which occurred in 1.6% of patients in both treatment arms (P=0.49).
Fatal bleeding occurred in 0.1% of patients in the ticagrelor arm and 0.3% of patients in the clopidogrel arm (P=0.10). And intracranial bleeding occurred in 0.5% of patients in both arms (P=0.82).
However, significantly more patients discontinued ticagrelor due to bleeding—2.4%, compared to 1.6% of patients who discontinued clopidogrel due to bleeding (P<0.001).
Significantly more patients discontinued ticagrelor due to dyspnea as well—4.8% vs 0.8% (P<0.001).
In all, 30.1% of patients in the ticagrelor arm and 25.9% of those in the clopidogrel arm prematurely discontinued treatment. This includes patients who discontinued due to adverse events, meeting the primary efficacy endpoint, and death. ![]()

Photo from AstraZeneca
NEW ORLEANS—Results of the EUCLID trial suggest ticagrelor does not a provide a benefit over clopidogrel in patients with symptomatic peripheral artery disease (PAD).
The incidence of atherothrombotic events was similar in patients who received ticagrelor and those who received clopidogrel.
Likewise, there was no significant difference between the treatment arms with regard to major bleeding.
Manesh R. Patel, MD, of Duke University Medical Center in Durham, North Carolina, presented results from the EUCLID trial at the American Heart Association Scientific Sessions.
Results were also published in NEJM. The trial was supported by AstraZeneca.
EUCLID included 13,885 patients with symptomatic PAD. They had median age of 66, and 72% were male.
The patients were randomized to receive ticagrelor at 90 mg twice daily or clopidogrel at 75 mg once daily.
The study’s primary efficacy endpoint was a composite of adjudicated cardiovascular death, myocardial infarction, and ischemic stroke.
At a median follow-up of 30 months, the primary efficacy endpoint had occurred in 10.8% (751/6930) of patients in the ticagrelor arm and 10.6% (740/6955) in the clopidogrel arm (P=0.65).
When the researchers assessed each of the components of the primary endpoint alone, they found a significant difference between the treatment groups in the incidence of ischemic stroke but not cardiovascular death or myocardial infarction.
Cardiovascular death occurred in 5.2% of patients in the ticagrelor arm and 4.9% of those in the clopidogrel arm (P=0.40). Myocardial infarction occurred in 5% and 4.8%, respectively (P=0.48). And ischemic stroke occurred in 1.9% and 2.4%, respectively (P=0.03).
The study’s primary safety endpoint was major bleeding, which occurred in 1.6% of patients in both treatment arms (P=0.49).
Fatal bleeding occurred in 0.1% of patients in the ticagrelor arm and 0.3% of patients in the clopidogrel arm (P=0.10). And intracranial bleeding occurred in 0.5% of patients in both arms (P=0.82).
However, significantly more patients discontinued ticagrelor due to bleeding—2.4%, compared to 1.6% of patients who discontinued clopidogrel due to bleeding (P<0.001).
Significantly more patients discontinued ticagrelor due to dyspnea as well—4.8% vs 0.8% (P<0.001).
In all, 30.1% of patients in the ticagrelor arm and 25.9% of those in the clopidogrel arm prematurely discontinued treatment. This includes patients who discontinued due to adverse events, meeting the primary efficacy endpoint, and death. ![]()
FDA grants priority review for midostaurin
The US Food and Drug Administration (FDA) has granted priority review for the new drug application for midostaurin (PKC412) as a treatment for advanced systemic mastocytosis (SM) and newly diagnosed, FLT3-mutated acute myeloid leukemia (AML).
The FDA has also accepted for review the premarket approval application for the midostaurin FLT3 companion diagnostic, which is designed to help identify patients who may have a FLT3 mutation and could potentially benefit from treatment with midostaurin.
Midostaurin is being developed by Novartis. The companion diagnostic is being developed by Novartis and Invivoscribe Technologies, Inc.
About priority review
The FDA grants priority review to applications for therapies that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it. The goal in the standard review process is to take action within 10 months.
About midostaurin
Midostaurin is an oral, multi-targeted kinase inhibitor. The drug was granted breakthrough therapy designation by the FDA earlier this year for newly diagnosed, FLT3-mutated AML.
According to Novartis, the new drug application submission for midostaurin includes data from the largest clinical trials conducted to date in advanced SM and newly diagnosed, FLT3-mutated AML.
Midostaurin in AML
In the phase 3 RATIFY trial, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in adults younger than 60 with FLT3-mutated AML. Results from this trial were presented at the 2015 ASH Annual Meeting.
Patients in the midostaurin arm experienced a statistically significant improvement in overall survival, with a 23% reduction in risk of death compared to the placebo arm (hazard ratio=0.77, P=0.0074).
There was no significant difference in the overall rate of grade 3 or higher hematologic and non-hematologic adverse events in midostaurin arm and the placebo arm. Similarly, there was no significant difference in treatment-related deaths between the arms.
Midostaurin in SM
Data from the phase 2 study of midostaurin in patients with advanced SM were published in NEJM in June.
The drug produced a 60% overall response rate, and the median duration of response was 24.1 months.
Fifty-six percent of patients required dose reductions due to toxic effects, but 32% of these patients were able to return to the starting dose of midostaurin.
Access to midostaurin
Since midostaurin remains investigational, both within the US and globally, Novartis opened a Global Individual Patient Program (compassionate use program) and, in the US, an Expanded Treatment Protocol, to provide access to midostaurin for eligible patients with newly diagnosed AML and advanced SM.
Physicians who want to request midostaurin for eligible patients can contact a Novartis medical representative in their respective countries. In the US, physicians can call 1-888-NOW-NOVA (1-888-669-6682) for more information. ![]()
The US Food and Drug Administration (FDA) has granted priority review for the new drug application for midostaurin (PKC412) as a treatment for advanced systemic mastocytosis (SM) and newly diagnosed, FLT3-mutated acute myeloid leukemia (AML).
The FDA has also accepted for review the premarket approval application for the midostaurin FLT3 companion diagnostic, which is designed to help identify patients who may have a FLT3 mutation and could potentially benefit from treatment with midostaurin.
Midostaurin is being developed by Novartis. The companion diagnostic is being developed by Novartis and Invivoscribe Technologies, Inc.
About priority review
The FDA grants priority review to applications for therapies that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it. The goal in the standard review process is to take action within 10 months.
About midostaurin
Midostaurin is an oral, multi-targeted kinase inhibitor. The drug was granted breakthrough therapy designation by the FDA earlier this year for newly diagnosed, FLT3-mutated AML.
According to Novartis, the new drug application submission for midostaurin includes data from the largest clinical trials conducted to date in advanced SM and newly diagnosed, FLT3-mutated AML.
Midostaurin in AML
In the phase 3 RATIFY trial, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in adults younger than 60 with FLT3-mutated AML. Results from this trial were presented at the 2015 ASH Annual Meeting.
Patients in the midostaurin arm experienced a statistically significant improvement in overall survival, with a 23% reduction in risk of death compared to the placebo arm (hazard ratio=0.77, P=0.0074).
There was no significant difference in the overall rate of grade 3 or higher hematologic and non-hematologic adverse events in midostaurin arm and the placebo arm. Similarly, there was no significant difference in treatment-related deaths between the arms.
Midostaurin in SM
Data from the phase 2 study of midostaurin in patients with advanced SM were published in NEJM in June.
The drug produced a 60% overall response rate, and the median duration of response was 24.1 months.
Fifty-six percent of patients required dose reductions due to toxic effects, but 32% of these patients were able to return to the starting dose of midostaurin.
Access to midostaurin
Since midostaurin remains investigational, both within the US and globally, Novartis opened a Global Individual Patient Program (compassionate use program) and, in the US, an Expanded Treatment Protocol, to provide access to midostaurin for eligible patients with newly diagnosed AML and advanced SM.
Physicians who want to request midostaurin for eligible patients can contact a Novartis medical representative in their respective countries. In the US, physicians can call 1-888-NOW-NOVA (1-888-669-6682) for more information. ![]()
The US Food and Drug Administration (FDA) has granted priority review for the new drug application for midostaurin (PKC412) as a treatment for advanced systemic mastocytosis (SM) and newly diagnosed, FLT3-mutated acute myeloid leukemia (AML).
The FDA has also accepted for review the premarket approval application for the midostaurin FLT3 companion diagnostic, which is designed to help identify patients who may have a FLT3 mutation and could potentially benefit from treatment with midostaurin.
Midostaurin is being developed by Novartis. The companion diagnostic is being developed by Novartis and Invivoscribe Technologies, Inc.
About priority review
The FDA grants priority review to applications for therapies that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it. The goal in the standard review process is to take action within 10 months.
About midostaurin
Midostaurin is an oral, multi-targeted kinase inhibitor. The drug was granted breakthrough therapy designation by the FDA earlier this year for newly diagnosed, FLT3-mutated AML.
According to Novartis, the new drug application submission for midostaurin includes data from the largest clinical trials conducted to date in advanced SM and newly diagnosed, FLT3-mutated AML.
Midostaurin in AML
In the phase 3 RATIFY trial, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in adults younger than 60 with FLT3-mutated AML. Results from this trial were presented at the 2015 ASH Annual Meeting.
Patients in the midostaurin arm experienced a statistically significant improvement in overall survival, with a 23% reduction in risk of death compared to the placebo arm (hazard ratio=0.77, P=0.0074).
There was no significant difference in the overall rate of grade 3 or higher hematologic and non-hematologic adverse events in midostaurin arm and the placebo arm. Similarly, there was no significant difference in treatment-related deaths between the arms.
Midostaurin in SM
Data from the phase 2 study of midostaurin in patients with advanced SM were published in NEJM in June.
The drug produced a 60% overall response rate, and the median duration of response was 24.1 months.
Fifty-six percent of patients required dose reductions due to toxic effects, but 32% of these patients were able to return to the starting dose of midostaurin.
Access to midostaurin
Since midostaurin remains investigational, both within the US and globally, Novartis opened a Global Individual Patient Program (compassionate use program) and, in the US, an Expanded Treatment Protocol, to provide access to midostaurin for eligible patients with newly diagnosed AML and advanced SM.
Physicians who want to request midostaurin for eligible patients can contact a Novartis medical representative in their respective countries. In the US, physicians can call 1-888-NOW-NOVA (1-888-669-6682) for more information. ![]()
EMA recommends orphan status for drug in AML

The European Medicines Agency’s (EMA) Committee for Orphan Medicinal Products (COMP) has recommended that BP1001 receive orphan designation as a treatment for acute myeloid leukemia (AML).
BP1001 (liposomal Grb2 antisense) is a neutral-charge, liposome-incorporated, antisense drug designed to inhibit protein synthesis of growth factor receptor bound protein 2 (Grb2).
BP1001 is being developed by Bio-Path Holdings, Inc.
According to Bio-Path, inhibition of Grb2 by BP1001 represents a significant advance in treating cancers with activated tyrosine kinases using a target not druggable with small molecule inhibitors.
Research has suggested that Grb2 plays an essential role in cancer cell activation via the RAS pathway. Grb2 bridges signals between activated and mutated tyrosine kinases, such as Flt3, c-Kit, and Bcr-Abl, and the Ras pathway, leading to activation of the ERK and AKT proteins.
About orphan designation
The EMA’s COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
Trials of BP1001
Bio-Path has completed a phase 1 trial of BP1001 in patients with relapsed/refractory AML, chronic myeloid leukemia, and myelodysplastic syndromes.
The company has also completed the safety segment of a phase 2 trial in which BP1001 is being investigated in combination with low-dose ara-C to treat AML.
Bio-Path recently released data from these studies.
The phase 1 study included patients who had received an average of 6 prior therapies.
The patients received 8 doses of BP1001 over 4 weeks, escalating to a maximum dose of 90 mg/m2. There were no dose-limiting toxicities, and Bio-Path said the drug was well tolerated.
Of the 18 evaluable patients with circulating blasts, 83% responded to BP1001. The average reduction in circulating blasts was 67%.
The phase 2 trial included patients with relapsed/refractory AML. There were 3 evaluable patients in each of 2 dosing cohorts—60 mg/m2 and 90 mg/m2. Patients received BP1001 twice a week for 4 weeks.
Five of the patients responded—3 with a complete response and 2 with a partial response. There were no adverse events attributed to BP1001, and the maximum-tolerated dose was not reached. ![]()

The European Medicines Agency’s (EMA) Committee for Orphan Medicinal Products (COMP) has recommended that BP1001 receive orphan designation as a treatment for acute myeloid leukemia (AML).
BP1001 (liposomal Grb2 antisense) is a neutral-charge, liposome-incorporated, antisense drug designed to inhibit protein synthesis of growth factor receptor bound protein 2 (Grb2).
BP1001 is being developed by Bio-Path Holdings, Inc.
According to Bio-Path, inhibition of Grb2 by BP1001 represents a significant advance in treating cancers with activated tyrosine kinases using a target not druggable with small molecule inhibitors.
Research has suggested that Grb2 plays an essential role in cancer cell activation via the RAS pathway. Grb2 bridges signals between activated and mutated tyrosine kinases, such as Flt3, c-Kit, and Bcr-Abl, and the Ras pathway, leading to activation of the ERK and AKT proteins.
About orphan designation
The EMA’s COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
Trials of BP1001
Bio-Path has completed a phase 1 trial of BP1001 in patients with relapsed/refractory AML, chronic myeloid leukemia, and myelodysplastic syndromes.
The company has also completed the safety segment of a phase 2 trial in which BP1001 is being investigated in combination with low-dose ara-C to treat AML.
Bio-Path recently released data from these studies.
The phase 1 study included patients who had received an average of 6 prior therapies.
The patients received 8 doses of BP1001 over 4 weeks, escalating to a maximum dose of 90 mg/m2. There were no dose-limiting toxicities, and Bio-Path said the drug was well tolerated.
Of the 18 evaluable patients with circulating blasts, 83% responded to BP1001. The average reduction in circulating blasts was 67%.
The phase 2 trial included patients with relapsed/refractory AML. There were 3 evaluable patients in each of 2 dosing cohorts—60 mg/m2 and 90 mg/m2. Patients received BP1001 twice a week for 4 weeks.
Five of the patients responded—3 with a complete response and 2 with a partial response. There were no adverse events attributed to BP1001, and the maximum-tolerated dose was not reached. ![]()

The European Medicines Agency’s (EMA) Committee for Orphan Medicinal Products (COMP) has recommended that BP1001 receive orphan designation as a treatment for acute myeloid leukemia (AML).
BP1001 (liposomal Grb2 antisense) is a neutral-charge, liposome-incorporated, antisense drug designed to inhibit protein synthesis of growth factor receptor bound protein 2 (Grb2).
BP1001 is being developed by Bio-Path Holdings, Inc.
According to Bio-Path, inhibition of Grb2 by BP1001 represents a significant advance in treating cancers with activated tyrosine kinases using a target not druggable with small molecule inhibitors.
Research has suggested that Grb2 plays an essential role in cancer cell activation via the RAS pathway. Grb2 bridges signals between activated and mutated tyrosine kinases, such as Flt3, c-Kit, and Bcr-Abl, and the Ras pathway, leading to activation of the ERK and AKT proteins.
About orphan designation
The EMA’s COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
Trials of BP1001
Bio-Path has completed a phase 1 trial of BP1001 in patients with relapsed/refractory AML, chronic myeloid leukemia, and myelodysplastic syndromes.
The company has also completed the safety segment of a phase 2 trial in which BP1001 is being investigated in combination with low-dose ara-C to treat AML.
Bio-Path recently released data from these studies.
The phase 1 study included patients who had received an average of 6 prior therapies.
The patients received 8 doses of BP1001 over 4 weeks, escalating to a maximum dose of 90 mg/m2. There were no dose-limiting toxicities, and Bio-Path said the drug was well tolerated.
Of the 18 evaluable patients with circulating blasts, 83% responded to BP1001. The average reduction in circulating blasts was 67%.
The phase 2 trial included patients with relapsed/refractory AML. There were 3 evaluable patients in each of 2 dosing cohorts—60 mg/m2 and 90 mg/m2. Patients received BP1001 twice a week for 4 weeks.
Five of the patients responded—3 with a complete response and 2 with a partial response. There were no adverse events attributed to BP1001, and the maximum-tolerated dose was not reached. ![]()
Mutations aid resistance, growth of malaria parasite

Plasmodium falciparum
Image from CDC/Mae Melvin
Some mutations that enable drug resistance in the malaria parasite Plasmodium falciparum may also help it grow, according to a study published in PLOS Pathogens.
Some strains of P falciparum have evolved to become resistant to antimalarial drugs, including chloroquine.
Often, chloroquine resistance mutations hinder P falciparum’s ability to infect the bloodstream and grow.
However, in a previous study, researchers discovered that a uniquely mutated version of the P falciparum gene pfcrt provides drug resistance while avoiding the detrimental impact of growth seen with other mutated pfcrt variants.
In the new study, the same group of researchers—Stanislaw Gabryszewski, of Columbia University Medical Center in New York, and his colleagues—investigated this version of the pfcrt gene, which is called Cam734 and has been found in certain regions in Southeast Asia.
Using zinc-finger nucleases, the team characterized the individual mutations unique to Cam734 in terms of their effects on drug resistance, metabolism, and growth rates in living parasites.
The researchers found that a mutation called A144F is required for the chloroquine resistance enabled by Cam734, and this mutation also contributes to resistance to the drugs amodiaquine and quinine.
The team identified additional mutations that contribute to resistance to chloroquine and impact the potency of other antimalarials as well.
When the researchers reversed these mutations in living parasites that had the Cam734 allele, growth slowed, indicating that these mutations also enhance infection.
Additional experiments revealed specific effects of Cam734 mutations on several metabolic pathways in P falciparum, including the digestion of human hemoglobin that parasites use to obtain amino acids for protein synthesis.
The researchers also found evidence suggesting that Cam734 helps to maintain an electrochemical gradient that allows the protein encoded by the pfcrt gene to thwart the cellular effects of chloroquine.
The team said these findings broaden our understanding of Cam734, the second most common variant of the pfcrt gene in Southeast Asia. The findings identify multiple intracellular processes and multidrug resistance phenotypes impacted by changes in pfcrt and can help inform future malaria treatment efforts. ![]()

Plasmodium falciparum
Image from CDC/Mae Melvin
Some mutations that enable drug resistance in the malaria parasite Plasmodium falciparum may also help it grow, according to a study published in PLOS Pathogens.
Some strains of P falciparum have evolved to become resistant to antimalarial drugs, including chloroquine.
Often, chloroquine resistance mutations hinder P falciparum’s ability to infect the bloodstream and grow.
However, in a previous study, researchers discovered that a uniquely mutated version of the P falciparum gene pfcrt provides drug resistance while avoiding the detrimental impact of growth seen with other mutated pfcrt variants.
In the new study, the same group of researchers—Stanislaw Gabryszewski, of Columbia University Medical Center in New York, and his colleagues—investigated this version of the pfcrt gene, which is called Cam734 and has been found in certain regions in Southeast Asia.
Using zinc-finger nucleases, the team characterized the individual mutations unique to Cam734 in terms of their effects on drug resistance, metabolism, and growth rates in living parasites.
The researchers found that a mutation called A144F is required for the chloroquine resistance enabled by Cam734, and this mutation also contributes to resistance to the drugs amodiaquine and quinine.
The team identified additional mutations that contribute to resistance to chloroquine and impact the potency of other antimalarials as well.
When the researchers reversed these mutations in living parasites that had the Cam734 allele, growth slowed, indicating that these mutations also enhance infection.
Additional experiments revealed specific effects of Cam734 mutations on several metabolic pathways in P falciparum, including the digestion of human hemoglobin that parasites use to obtain amino acids for protein synthesis.
The researchers also found evidence suggesting that Cam734 helps to maintain an electrochemical gradient that allows the protein encoded by the pfcrt gene to thwart the cellular effects of chloroquine.
The team said these findings broaden our understanding of Cam734, the second most common variant of the pfcrt gene in Southeast Asia. The findings identify multiple intracellular processes and multidrug resistance phenotypes impacted by changes in pfcrt and can help inform future malaria treatment efforts. ![]()

Plasmodium falciparum
Image from CDC/Mae Melvin
Some mutations that enable drug resistance in the malaria parasite Plasmodium falciparum may also help it grow, according to a study published in PLOS Pathogens.
Some strains of P falciparum have evolved to become resistant to antimalarial drugs, including chloroquine.
Often, chloroquine resistance mutations hinder P falciparum’s ability to infect the bloodstream and grow.
However, in a previous study, researchers discovered that a uniquely mutated version of the P falciparum gene pfcrt provides drug resistance while avoiding the detrimental impact of growth seen with other mutated pfcrt variants.
In the new study, the same group of researchers—Stanislaw Gabryszewski, of Columbia University Medical Center in New York, and his colleagues—investigated this version of the pfcrt gene, which is called Cam734 and has been found in certain regions in Southeast Asia.
Using zinc-finger nucleases, the team characterized the individual mutations unique to Cam734 in terms of their effects on drug resistance, metabolism, and growth rates in living parasites.
The researchers found that a mutation called A144F is required for the chloroquine resistance enabled by Cam734, and this mutation also contributes to resistance to the drugs amodiaquine and quinine.
The team identified additional mutations that contribute to resistance to chloroquine and impact the potency of other antimalarials as well.
When the researchers reversed these mutations in living parasites that had the Cam734 allele, growth slowed, indicating that these mutations also enhance infection.
Additional experiments revealed specific effects of Cam734 mutations on several metabolic pathways in P falciparum, including the digestion of human hemoglobin that parasites use to obtain amino acids for protein synthesis.
The researchers also found evidence suggesting that Cam734 helps to maintain an electrochemical gradient that allows the protein encoded by the pfcrt gene to thwart the cellular effects of chloroquine.
The team said these findings broaden our understanding of Cam734, the second most common variant of the pfcrt gene in Southeast Asia. The findings identify multiple intracellular processes and multidrug resistance phenotypes impacted by changes in pfcrt and can help inform future malaria treatment efforts.
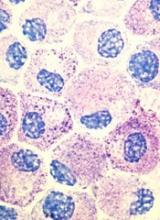
How EBV drives lymphomagenesis

Image by Ed Uthman
Results of research published in eLIFE appear to explain how Epstein-Barr virus (EBV) controls a pair of genes to drive lymphomagenesis.
Researchers set out to determine how EBV controls MYC, which is known to drive lymphoma development when activated, and BCL2L11, a gene that normally triggers apoptosis to prevent lymphoma but can be silenced by EBV.
The team discovered that EBV controls MYC and BCL2L11 by hijacking enhancer regions of DNA, which are situated far away from the genes.
These enhancers act as “control centers” and are able to contact and control genes from long distances by the looping out of the intervening stretches of DNA.
The researchers found that EBV activates MYC by increasing contacts between a specific set of enhancers and the gene.
The team said an Epstein-Barr nuclear antigen, EBNA2, activates multiple MYC enhancers and reconfigures the MYC locus to increase upstream enhancer-promoter interactions and decrease downstream interactions.
They noted that EBNA2 recruits the BRG1 ATPase of the SWI/SNF remodeller to MYC enhancers, and BRG1 is required for enhancer-promoter interactions in EBV-infected cells.
The researchers also discovered new enhancers that control BCL2L11. In this case, though, EBV stops these control centers from contacting the gene.
Specifically, the team found a hematopoietic enhancer hub that is inactivated by the Epstein-Barr nuclear antigens EBNA3A and EBNA3C through recruitment of the H3K27 methyltransferase EZH2.
Therefore, the researchers set out to determine if an EZH1/2 inhibitor, UNC1999, could reverse this effect. They found that UNC1999 did reverse enhancer inactivation, upregulated BCL2L11, and induced apoptosis in EBV-positive Burkitt lymphoma cells.
“This is a key step towards uncovering how this common virus, which affects thousands of people every year, causes blood cancer,” said study author Michelle West, PhD, of the University of Sussex in Brighton, UK.
“It is now important to carry out further studies to determine how the Epstein-Barr virus controls other genes that are associated with lymphoma. This will tell us more about how the virus drives lymphoma development and will help to identify new ways of targeting Epstein-Barr virus-infected cancer cells with specific drugs.”

Image by Ed Uthman
Results of research published in eLIFE appear to explain how Epstein-Barr virus (EBV) controls a pair of genes to drive lymphomagenesis.
Researchers set out to determine how EBV controls MYC, which is known to drive lymphoma development when activated, and BCL2L11, a gene that normally triggers apoptosis to prevent lymphoma but can be silenced by EBV.
The team discovered that EBV controls MYC and BCL2L11 by hijacking enhancer regions of DNA, which are situated far away from the genes.
These enhancers act as “control centers” and are able to contact and control genes from long distances by the looping out of the intervening stretches of DNA.
The researchers found that EBV activates MYC by increasing contacts between a specific set of enhancers and the gene.
The team said an Epstein-Barr nuclear antigen, EBNA2, activates multiple MYC enhancers and reconfigures the MYC locus to increase upstream enhancer-promoter interactions and decrease downstream interactions.
They noted that EBNA2 recruits the BRG1 ATPase of the SWI/SNF remodeller to MYC enhancers, and BRG1 is required for enhancer-promoter interactions in EBV-infected cells.
The researchers also discovered new enhancers that control BCL2L11. In this case, though, EBV stops these control centers from contacting the gene.
Specifically, the team found a hematopoietic enhancer hub that is inactivated by the Epstein-Barr nuclear antigens EBNA3A and EBNA3C through recruitment of the H3K27 methyltransferase EZH2.
Therefore, the researchers set out to determine if an EZH1/2 inhibitor, UNC1999, could reverse this effect. They found that UNC1999 did reverse enhancer inactivation, upregulated BCL2L11, and induced apoptosis in EBV-positive Burkitt lymphoma cells.
“This is a key step towards uncovering how this common virus, which affects thousands of people every year, causes blood cancer,” said study author Michelle West, PhD, of the University of Sussex in Brighton, UK.
“It is now important to carry out further studies to determine how the Epstein-Barr virus controls other genes that are associated with lymphoma. This will tell us more about how the virus drives lymphoma development and will help to identify new ways of targeting Epstein-Barr virus-infected cancer cells with specific drugs.”

Image by Ed Uthman
Results of research published in eLIFE appear to explain how Epstein-Barr virus (EBV) controls a pair of genes to drive lymphomagenesis.
Researchers set out to determine how EBV controls MYC, which is known to drive lymphoma development when activated, and BCL2L11, a gene that normally triggers apoptosis to prevent lymphoma but can be silenced by EBV.
The team discovered that EBV controls MYC and BCL2L11 by hijacking enhancer regions of DNA, which are situated far away from the genes.
These enhancers act as “control centers” and are able to contact and control genes from long distances by the looping out of the intervening stretches of DNA.
The researchers found that EBV activates MYC by increasing contacts between a specific set of enhancers and the gene.
The team said an Epstein-Barr nuclear antigen, EBNA2, activates multiple MYC enhancers and reconfigures the MYC locus to increase upstream enhancer-promoter interactions and decrease downstream interactions.
They noted that EBNA2 recruits the BRG1 ATPase of the SWI/SNF remodeller to MYC enhancers, and BRG1 is required for enhancer-promoter interactions in EBV-infected cells.
The researchers also discovered new enhancers that control BCL2L11. In this case, though, EBV stops these control centers from contacting the gene.
Specifically, the team found a hematopoietic enhancer hub that is inactivated by the Epstein-Barr nuclear antigens EBNA3A and EBNA3C through recruitment of the H3K27 methyltransferase EZH2.
Therefore, the researchers set out to determine if an EZH1/2 inhibitor, UNC1999, could reverse this effect. They found that UNC1999 did reverse enhancer inactivation, upregulated BCL2L11, and induced apoptosis in EBV-positive Burkitt lymphoma cells.
“This is a key step towards uncovering how this common virus, which affects thousands of people every year, causes blood cancer,” said study author Michelle West, PhD, of the University of Sussex in Brighton, UK.
“It is now important to carry out further studies to determine how the Epstein-Barr virus controls other genes that are associated with lymphoma. This will tell us more about how the virus drives lymphoma development and will help to identify new ways of targeting Epstein-Barr virus-infected cancer cells with specific drugs.”
CHMP recommends drug for hemophilia A

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is intended for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
The CHMP’s recommendation will be reviewed by the European Commission, which is expected to make a decision in the next few months.
Lonoctocog alfa is designed to provide lasting protection from bleeds with 2- to 3-times weekly dosing. The product uses a covalent bond that forms one structural entity, a single polypeptide-chain, to improve the stability of FVIII and provide longer-lasting FVIII activity.
Lonoctocog alfa is being developed by CSL Behring GmbH.
Clinical trials
The CHMP’s positive opinion of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults and adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is intended for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
The CHMP’s recommendation will be reviewed by the European Commission, which is expected to make a decision in the next few months.
Lonoctocog alfa is designed to provide lasting protection from bleeds with 2- to 3-times weekly dosing. The product uses a covalent bond that forms one structural entity, a single polypeptide-chain, to improve the stability of FVIII and provide longer-lasting FVIII activity.
Lonoctocog alfa is being developed by CSL Behring GmbH.
Clinical trials
The CHMP’s positive opinion of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults and adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is intended for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
The CHMP’s recommendation will be reviewed by the European Commission, which is expected to make a decision in the next few months.
Lonoctocog alfa is designed to provide lasting protection from bleeds with 2- to 3-times weekly dosing. The product uses a covalent bond that forms one structural entity, a single polypeptide-chain, to improve the stability of FVIII and provide longer-lasting FVIII activity.
Lonoctocog alfa is being developed by CSL Behring GmbH.
Clinical trials
The CHMP’s positive opinion of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults and adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Drug dubbed ‘breakthrough’ for CTCL subtypes

Photo from Business Wire
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to brentuximab vedotin (Adcetris) as a treatment for 2 subtypes of cutaneous T-cell lymphoma (CTCL).
The drug now has this designation for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous anaplastic large-cell lymphoma (pcALCL) who require systemic therapy and have received 1 prior systemic therapy.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Brentuximab vedotin in CTCL
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin has orphan drug designation from the FDA for the treatment of MF. The drug also received orphan drug designation from the European Commission for CTCL, including subtypes pcALCL and MF.
Brentuximab vedotin has been evaluated in CD30-expressing CTCL in investigator- and corporate-sponsored clinical trials, including the phase 3 ALCANZA trial.
This trial was designed to compare single-agent brentuximab vedotin to investigator’s choice of standard therapies—methotrexate or bexarotene—in patients with CD30-expressing CTCL, including those with pcALCL or MF.
The trial has enrolled 131 patients at 50 sites globally. Patients with pcALCL must have received at least 1 prior systemic or radiation therapy, and patients with MF must have received at least 1 prior systemic therapy.
The study’s primary endpoint is objective response lasting at least 4 months (ORR4), as assessed by Global Response Score, in the brentuximab vedotin arm compared to the control arm. Key secondary endpoints are complete response rate, progression-free survival, and reduction in the burden of symptoms during treatment.
Topline results of the trial were announced in August. The data showed a significant improvement in the ORR4 for the brentuximab vedotin arm compared to the control arm. The ORR4 was 56.3% and 12.5%, respectively (P<0.0001).
The key secondary endpoints were all statistically significant in favor of the brentuximab vedotin arm. And investigators said the safety profile of brentuximab vedotin was generally consistent with the existing prescribing information.
An abstract detailing results of the ALCANZA trial was accepted for oral presentation at the upcoming ASH Annual Meeting (abstract 182).

Photo from Business Wire
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to brentuximab vedotin (Adcetris) as a treatment for 2 subtypes of cutaneous T-cell lymphoma (CTCL).
The drug now has this designation for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous anaplastic large-cell lymphoma (pcALCL) who require systemic therapy and have received 1 prior systemic therapy.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Brentuximab vedotin in CTCL
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin has orphan drug designation from the FDA for the treatment of MF. The drug also received orphan drug designation from the European Commission for CTCL, including subtypes pcALCL and MF.
Brentuximab vedotin has been evaluated in CD30-expressing CTCL in investigator- and corporate-sponsored clinical trials, including the phase 3 ALCANZA trial.
This trial was designed to compare single-agent brentuximab vedotin to investigator’s choice of standard therapies—methotrexate or bexarotene—in patients with CD30-expressing CTCL, including those with pcALCL or MF.
The trial has enrolled 131 patients at 50 sites globally. Patients with pcALCL must have received at least 1 prior systemic or radiation therapy, and patients with MF must have received at least 1 prior systemic therapy.
The study’s primary endpoint is objective response lasting at least 4 months (ORR4), as assessed by Global Response Score, in the brentuximab vedotin arm compared to the control arm. Key secondary endpoints are complete response rate, progression-free survival, and reduction in the burden of symptoms during treatment.
Topline results of the trial were announced in August. The data showed a significant improvement in the ORR4 for the brentuximab vedotin arm compared to the control arm. The ORR4 was 56.3% and 12.5%, respectively (P<0.0001).
The key secondary endpoints were all statistically significant in favor of the brentuximab vedotin arm. And investigators said the safety profile of brentuximab vedotin was generally consistent with the existing prescribing information.
An abstract detailing results of the ALCANZA trial was accepted for oral presentation at the upcoming ASH Annual Meeting (abstract 182).

Photo from Business Wire
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to brentuximab vedotin (Adcetris) as a treatment for 2 subtypes of cutaneous T-cell lymphoma (CTCL).
The drug now has this designation for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous anaplastic large-cell lymphoma (pcALCL) who require systemic therapy and have received 1 prior systemic therapy.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Brentuximab vedotin in CTCL
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin has orphan drug designation from the FDA for the treatment of MF. The drug also received orphan drug designation from the European Commission for CTCL, including subtypes pcALCL and MF.
Brentuximab vedotin has been evaluated in CD30-expressing CTCL in investigator- and corporate-sponsored clinical trials, including the phase 3 ALCANZA trial.
This trial was designed to compare single-agent brentuximab vedotin to investigator’s choice of standard therapies—methotrexate or bexarotene—in patients with CD30-expressing CTCL, including those with pcALCL or MF.
The trial has enrolled 131 patients at 50 sites globally. Patients with pcALCL must have received at least 1 prior systemic or radiation therapy, and patients with MF must have received at least 1 prior systemic therapy.
The study’s primary endpoint is objective response lasting at least 4 months (ORR4), as assessed by Global Response Score, in the brentuximab vedotin arm compared to the control arm. Key secondary endpoints are complete response rate, progression-free survival, and reduction in the burden of symptoms during treatment.
Topline results of the trial were announced in August. The data showed a significant improvement in the ORR4 for the brentuximab vedotin arm compared to the control arm. The ORR4 was 56.3% and 12.5%, respectively (P<0.0001).
The key secondary endpoints were all statistically significant in favor of the brentuximab vedotin arm. And investigators said the safety profile of brentuximab vedotin was generally consistent with the existing prescribing information.
An abstract detailing results of the ALCANZA trial was accepted for oral presentation at the upcoming ASH Annual Meeting (abstract 182).