User login
Drug allows for treatment-free periods in PV
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
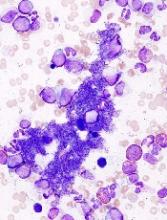
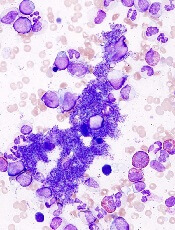
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
Risk stratification may be possible with JCAR017
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
FDA expands approved use of bosutinib in CML
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
Allo-HSCT leads to long-term survival in MF
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
FDA issues requirements, recommendations for GBCA use
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
Edoxaban noninferior to dalteparin for VTE in cancer
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
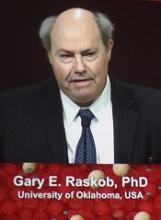
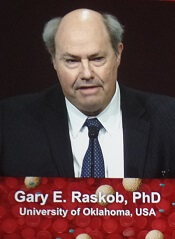
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
FDA lifts clinical hold on fitusiran trials
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period. ![]()
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period. ![]()
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period.
NK cell product receives orphan designation
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Ruxolitinib improves survival for MF patients in CP-e
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures.
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures.
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures.
CHMP recommends generic drug for ET
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.