User login
according to the results of a systematic review of nearly 3,000 patients.
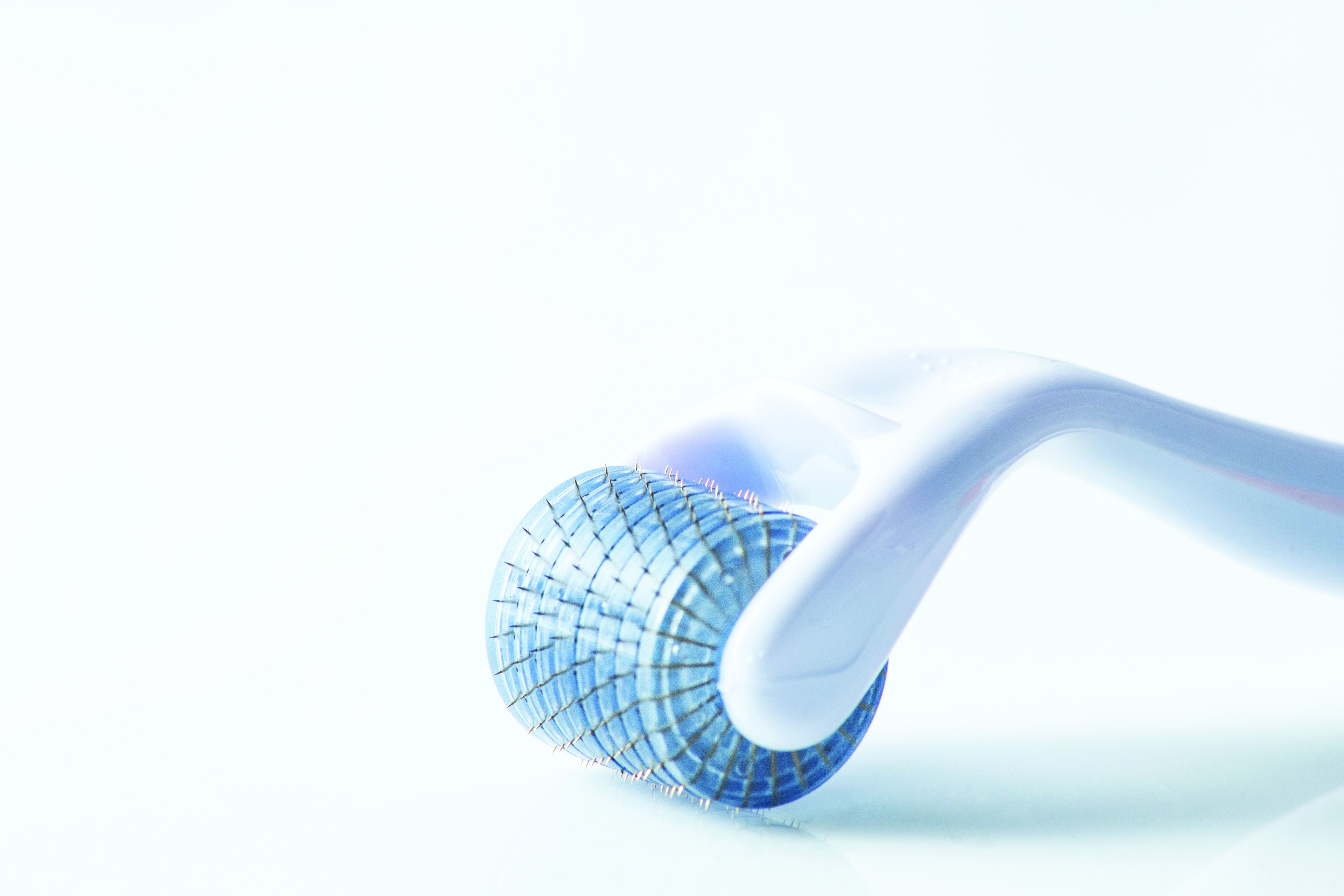
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
according to the results of a systematic review of nearly 3,000 patients.
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
according to the results of a systematic review of nearly 3,000 patients.
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
FROM DERMATOLOGIC SURGERY