User login
In their article in this issue of the Cleveland Clinic Journal of Medicine, Kabach et al answer no to the question of whether stenting of severe renal artery stenosis improves outcomes compared with medical therapy alone.1 They review the findings of four key studies2–5 published between 2003 and 2014 and conclude that, in patients with severe atherosclerotic renal artery stenosis and hypertension or chronic kidney disease, renal artery stenting with medical therapy can improve blood pressure control but has no significant impact on cardiovascular or mortality outcomes.1
Furthermore, the authors state that in view of the risk of complications associated with stenting, medical management should continue to be the first-line therapy.1 Indeed, the ASTRAL study (Angioplasty and Stenting for Renal Artery Lesions) investigators found substantial risks without evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.3
Nevertheless, I believe that this procedure may benefit certain patients.
MAYO CLINIC COHORT STUDY
In 2008, our group at Mayo Clinic Health system in Eau Claire, Wisconsin, published the results of a prospective cohort study in 26 patients with renal artery stenosis and chronic kidney disease who presented with rapidly worsening renal failure (defined as an increase in serum creatinine of ≥ 25%) while receiving an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB).6,7
These drugs—inhibitors of the renin-angiotensin-aldosterone system—slow the progression of chronic kidney disease but can acutely worsen renal function, especially in patients with renal artery stenosis, and withdrawing them in this situation was the focus of our study.
The patients (10 men and 16 women) ranged in age from 63 to 87 (mean age 75.3).
At enrollment, the ACE inhibitors and ARBs were discontinued, standard nephrologic care was applied, and the glomerular filtration rate (estimated by the Modification of Diet in Renal Disease Study equation) was monitored. After at least 2 weeks, percutaneous renal angioplasty with stent placement was considered if the patient met any of the following criteria:
- Persistence of renal failure
- Flash pulmonary edema
- Uncontrolled hypertension despite the use of at least three antihypertensive medications.
Nine patients underwent percutaneous angioplasty and stenting and 17 did not. The procedure was done on one renal artery in 8 patients and both renal arteries in 1. Indications for the procedure were recent worsening of renal failure in 8 patients and recent worsening renal failure together with symptomatic flash pulmonary edema in 1 patient. (Flash pulmonary edema is the only class I recommendation for percutaneous renal angioplasty in the 2006 joint guidelines of the American College of Cardiology and the American Heart Association.8) As noted above, all the patients were experiencing acute exacerbation of chronic kidney disease at the time.
We found clear evidence of additional improved and sustained renal function in the patients who underwent percutaneous renal angioplasty and stenting compared with the patients who did not (Figures 1 and 2).6,7
In an editorial9 following publication of the ASTRAL study, our group reported a subsequent 82-month analysis of our 26-patient cohort completed in June 2009. In the 7 surviving patients who had undergone percutaneous renal angioplasty and stenting, the estimated glomerular filtration rate had increased from 27.4 mL/min/1.73 m2 (± 12.7, range 11–47) at baseline to 50.3 (± 21.7, range 23–68) (P = .018) after 46.9 months.
PATIENT NUMBER 13
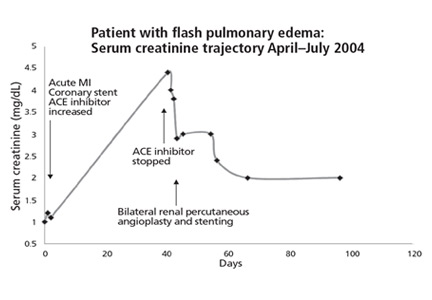
To illustrate how percutaneous renal angioplasty and stenting can reverse recently worsening renal failure in renal artery stenosis, I would like to discuss in greater detail a patient from our two previous reports.6,7
Patient 13, a 67-year-old woman with hypertension, was referred to our nephrology service in September 2004 to consider starting hemodialysis for symptomatic renal failure. Her serum creatinine had increased to 3.4 mg/dL from a previous baseline level of 2.0 mg/dL, and she also had worsening anemia and hyperkalemia. She had been taking lisinopril 10 mg/day for the last 12 months. Magnetic resonance angiography revealed high-grade (> 95%) bilateral renal artery stenosis with an atrophic left kidney.
Lisinopril was promptly discontinued, and within 2 weeks her serum creatinine level had decreased by more than 0.5 mg/dL. In mid-November 2004, she underwent right renal artery angioplasty with stent placement. After that, her serum creatinine decreased further, and 3 months later it had dropped to 1.6 mg/dL. The value continued to improve, with the lowest measurement of 1.1 mg/dL, equivalent to an estimated glomerular filtration rate of 51 mL/min/1.73 m2. This was in May 2006, 19 months after stopping lisinopril and 17 months after angioplasty and stenting. The last available serum creatinine level (August 2006) was 1.2 mg/dL, equivalent to an estimated glomerular filtration rate of 45 mL/min/1.73 m2 (Figure 1). Unfortunately, the patient died of metastatic lung cancer in December of that year.
Also of note, the patient who underwent angioplasty because of recurrent flash pulmonary edema had no recurrences of it afterward.
We concluded that, in patients with hemodynamically significant renal artery stenosis presenting with acutely worsening renal failure, renal angioplasty with stenting has the potential to reverse renal failure, improve blood pressure control, and stop flash pulmonary edema.6–8
Notably, all patients in our study who underwent renal angioplasty with stenting had new-onset acute renal injury as defined by an increase in the baseline serum creatinine of more than 25% during the 3 months before stent placement.6–8 Patients in the STAR,2 HERCULES,4 and CORAL5 studies had renal artery stenosis but otherwise stable chronic kidney disease at the time of enrollment. In the ASTRAL study,3 12% of the patients had acute kidney injury on study enrollment, defined as an increase in the serum creatinine level of more than 20% or of more than 1.13 mg/dL.3
While we strongly agree with aggressive yet monitored medical therapy for patients with hemodynamically significant renal artery stenosis, I posit that selected patients do indeed derive significant clinical benefits from renal angioplasty and stenting. Our group’s prospective individual-patient-level data support the paradigm that angioplasty with stenting is useful in patients with renal artery stenosis who experience “acute-on-chronic” kidney disease.
The pathophysiology of renal artery stenosis and the progression of chronic kidney disease are complex, and many factors affect patient outcomes and response to treatment. Thus, the message is that treatment of severe renal artery stenosis must be individualized.9–11 No one treatment fits all.10,11
- Kabach A, Agha OQ, Baibars M, Alraiyes AH, Alraies MC. Does stenting of severe renal artery stenosis improve outcomes compared with medical therapy alone? Cleve Clin J Med 2015; 82:491–494.
- Bax L, Mali WP, Buskens E, et al; STAR Study Group. The benefit of STent placement and blood pressure and lipid-lowering for the prevention of progression of renal dysfunction caused by Atherosclerotic ostial stenosis of the Renal artery. The STAR-study: rationale and study design. J Nephrol 2003; 16:807–812.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Jaff MR, Bates M, Sullivan T, et al; HERCULES Investigators. Significant reduction in systolic blood pressure following renal artery stenting in patients with uncontrolled hypertension: results from the HERCULES trial. Catheter Cardiovasc Interv 2012; 80:343–350.
- Cooper CJ, Murphy TP, Cutlip DE, et al; CORAL Investigators. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med 2014; 370:13–22.
- Onuigbo MAC, Onuigbo NTC. Worsening renal failure in older chronic kidney disease patients with renal artery stenosis concurrently on renin angiotensin aldosterone system blockade: a prospective 50-month Mayo Health System clinic analysis. QJM 2008; 101:519–527.
- Onuigbo MA, Onuigbo NT. Renal failure and concurrent RAAS blockade in older CKD patients with renal artery stenosis: an extended Mayo Clinic prospective 63-month experience. Ren Fail 2008; 30:363–371.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary. J Am Coll Cardiol 2006; 47:1239–1312.
- Onuigbo M, Frenandes R, Nijhawan V. The ASTRAL trial results revisited—to stent or not to stent in renal artery stenosis? QJM 2010; 103:357.
- Singh M, Kovacs DF, Singh A, Dhaliwal P, Khosla S. ACE inhibition and renal artery stenosis: what lessons have we learnt? A 21st century perspective. In: Onuigbo MAC, ed. ACE inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 2. New York, NY: NOVA Publishers; 2013:203–218.
- Onuigbo MA, Onuigbo C, Onuigbo V, et al. The CKD enigma, reengineering CKD care, narrowing asymmetric information and confronting ethicomedicinomics in CKD care: the introduction of the new 'CKD express©' IT software program. In: Onuigbo MAC, ed. ACE Inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 1. New York, NY: NOVA Publishers; 2013: 41–56.
In their article in this issue of the Cleveland Clinic Journal of Medicine, Kabach et al answer no to the question of whether stenting of severe renal artery stenosis improves outcomes compared with medical therapy alone.1 They review the findings of four key studies2–5 published between 2003 and 2014 and conclude that, in patients with severe atherosclerotic renal artery stenosis and hypertension or chronic kidney disease, renal artery stenting with medical therapy can improve blood pressure control but has no significant impact on cardiovascular or mortality outcomes.1
Furthermore, the authors state that in view of the risk of complications associated with stenting, medical management should continue to be the first-line therapy.1 Indeed, the ASTRAL study (Angioplasty and Stenting for Renal Artery Lesions) investigators found substantial risks without evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.3
Nevertheless, I believe that this procedure may benefit certain patients.
MAYO CLINIC COHORT STUDY
In 2008, our group at Mayo Clinic Health system in Eau Claire, Wisconsin, published the results of a prospective cohort study in 26 patients with renal artery stenosis and chronic kidney disease who presented with rapidly worsening renal failure (defined as an increase in serum creatinine of ≥ 25%) while receiving an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB).6,7
These drugs—inhibitors of the renin-angiotensin-aldosterone system—slow the progression of chronic kidney disease but can acutely worsen renal function, especially in patients with renal artery stenosis, and withdrawing them in this situation was the focus of our study.
The patients (10 men and 16 women) ranged in age from 63 to 87 (mean age 75.3).
At enrollment, the ACE inhibitors and ARBs were discontinued, standard nephrologic care was applied, and the glomerular filtration rate (estimated by the Modification of Diet in Renal Disease Study equation) was monitored. After at least 2 weeks, percutaneous renal angioplasty with stent placement was considered if the patient met any of the following criteria:
- Persistence of renal failure
- Flash pulmonary edema
- Uncontrolled hypertension despite the use of at least three antihypertensive medications.
Nine patients underwent percutaneous angioplasty and stenting and 17 did not. The procedure was done on one renal artery in 8 patients and both renal arteries in 1. Indications for the procedure were recent worsening of renal failure in 8 patients and recent worsening renal failure together with symptomatic flash pulmonary edema in 1 patient. (Flash pulmonary edema is the only class I recommendation for percutaneous renal angioplasty in the 2006 joint guidelines of the American College of Cardiology and the American Heart Association.8) As noted above, all the patients were experiencing acute exacerbation of chronic kidney disease at the time.
We found clear evidence of additional improved and sustained renal function in the patients who underwent percutaneous renal angioplasty and stenting compared with the patients who did not (Figures 1 and 2).6,7
In an editorial9 following publication of the ASTRAL study, our group reported a subsequent 82-month analysis of our 26-patient cohort completed in June 2009. In the 7 surviving patients who had undergone percutaneous renal angioplasty and stenting, the estimated glomerular filtration rate had increased from 27.4 mL/min/1.73 m2 (± 12.7, range 11–47) at baseline to 50.3 (± 21.7, range 23–68) (P = .018) after 46.9 months.
PATIENT NUMBER 13
To illustrate how percutaneous renal angioplasty and stenting can reverse recently worsening renal failure in renal artery stenosis, I would like to discuss in greater detail a patient from our two previous reports.6,7
Patient 13, a 67-year-old woman with hypertension, was referred to our nephrology service in September 2004 to consider starting hemodialysis for symptomatic renal failure. Her serum creatinine had increased to 3.4 mg/dL from a previous baseline level of 2.0 mg/dL, and she also had worsening anemia and hyperkalemia. She had been taking lisinopril 10 mg/day for the last 12 months. Magnetic resonance angiography revealed high-grade (> 95%) bilateral renal artery stenosis with an atrophic left kidney.
Lisinopril was promptly discontinued, and within 2 weeks her serum creatinine level had decreased by more than 0.5 mg/dL. In mid-November 2004, she underwent right renal artery angioplasty with stent placement. After that, her serum creatinine decreased further, and 3 months later it had dropped to 1.6 mg/dL. The value continued to improve, with the lowest measurement of 1.1 mg/dL, equivalent to an estimated glomerular filtration rate of 51 mL/min/1.73 m2. This was in May 2006, 19 months after stopping lisinopril and 17 months after angioplasty and stenting. The last available serum creatinine level (August 2006) was 1.2 mg/dL, equivalent to an estimated glomerular filtration rate of 45 mL/min/1.73 m2 (Figure 1). Unfortunately, the patient died of metastatic lung cancer in December of that year.
Also of note, the patient who underwent angioplasty because of recurrent flash pulmonary edema had no recurrences of it afterward.
We concluded that, in patients with hemodynamically significant renal artery stenosis presenting with acutely worsening renal failure, renal angioplasty with stenting has the potential to reverse renal failure, improve blood pressure control, and stop flash pulmonary edema.6–8
Notably, all patients in our study who underwent renal angioplasty with stenting had new-onset acute renal injury as defined by an increase in the baseline serum creatinine of more than 25% during the 3 months before stent placement.6–8 Patients in the STAR,2 HERCULES,4 and CORAL5 studies had renal artery stenosis but otherwise stable chronic kidney disease at the time of enrollment. In the ASTRAL study,3 12% of the patients had acute kidney injury on study enrollment, defined as an increase in the serum creatinine level of more than 20% or of more than 1.13 mg/dL.3
While we strongly agree with aggressive yet monitored medical therapy for patients with hemodynamically significant renal artery stenosis, I posit that selected patients do indeed derive significant clinical benefits from renal angioplasty and stenting. Our group’s prospective individual-patient-level data support the paradigm that angioplasty with stenting is useful in patients with renal artery stenosis who experience “acute-on-chronic” kidney disease.
The pathophysiology of renal artery stenosis and the progression of chronic kidney disease are complex, and many factors affect patient outcomes and response to treatment. Thus, the message is that treatment of severe renal artery stenosis must be individualized.9–11 No one treatment fits all.10,11
In their article in this issue of the Cleveland Clinic Journal of Medicine, Kabach et al answer no to the question of whether stenting of severe renal artery stenosis improves outcomes compared with medical therapy alone.1 They review the findings of four key studies2–5 published between 2003 and 2014 and conclude that, in patients with severe atherosclerotic renal artery stenosis and hypertension or chronic kidney disease, renal artery stenting with medical therapy can improve blood pressure control but has no significant impact on cardiovascular or mortality outcomes.1
Furthermore, the authors state that in view of the risk of complications associated with stenting, medical management should continue to be the first-line therapy.1 Indeed, the ASTRAL study (Angioplasty and Stenting for Renal Artery Lesions) investigators found substantial risks without evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.3
Nevertheless, I believe that this procedure may benefit certain patients.
MAYO CLINIC COHORT STUDY
In 2008, our group at Mayo Clinic Health system in Eau Claire, Wisconsin, published the results of a prospective cohort study in 26 patients with renal artery stenosis and chronic kidney disease who presented with rapidly worsening renal failure (defined as an increase in serum creatinine of ≥ 25%) while receiving an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB).6,7
These drugs—inhibitors of the renin-angiotensin-aldosterone system—slow the progression of chronic kidney disease but can acutely worsen renal function, especially in patients with renal artery stenosis, and withdrawing them in this situation was the focus of our study.
The patients (10 men and 16 women) ranged in age from 63 to 87 (mean age 75.3).
At enrollment, the ACE inhibitors and ARBs were discontinued, standard nephrologic care was applied, and the glomerular filtration rate (estimated by the Modification of Diet in Renal Disease Study equation) was monitored. After at least 2 weeks, percutaneous renal angioplasty with stent placement was considered if the patient met any of the following criteria:
- Persistence of renal failure
- Flash pulmonary edema
- Uncontrolled hypertension despite the use of at least three antihypertensive medications.
Nine patients underwent percutaneous angioplasty and stenting and 17 did not. The procedure was done on one renal artery in 8 patients and both renal arteries in 1. Indications for the procedure were recent worsening of renal failure in 8 patients and recent worsening renal failure together with symptomatic flash pulmonary edema in 1 patient. (Flash pulmonary edema is the only class I recommendation for percutaneous renal angioplasty in the 2006 joint guidelines of the American College of Cardiology and the American Heart Association.8) As noted above, all the patients were experiencing acute exacerbation of chronic kidney disease at the time.
We found clear evidence of additional improved and sustained renal function in the patients who underwent percutaneous renal angioplasty and stenting compared with the patients who did not (Figures 1 and 2).6,7
In an editorial9 following publication of the ASTRAL study, our group reported a subsequent 82-month analysis of our 26-patient cohort completed in June 2009. In the 7 surviving patients who had undergone percutaneous renal angioplasty and stenting, the estimated glomerular filtration rate had increased from 27.4 mL/min/1.73 m2 (± 12.7, range 11–47) at baseline to 50.3 (± 21.7, range 23–68) (P = .018) after 46.9 months.
PATIENT NUMBER 13
To illustrate how percutaneous renal angioplasty and stenting can reverse recently worsening renal failure in renal artery stenosis, I would like to discuss in greater detail a patient from our two previous reports.6,7
Patient 13, a 67-year-old woman with hypertension, was referred to our nephrology service in September 2004 to consider starting hemodialysis for symptomatic renal failure. Her serum creatinine had increased to 3.4 mg/dL from a previous baseline level of 2.0 mg/dL, and she also had worsening anemia and hyperkalemia. She had been taking lisinopril 10 mg/day for the last 12 months. Magnetic resonance angiography revealed high-grade (> 95%) bilateral renal artery stenosis with an atrophic left kidney.
Lisinopril was promptly discontinued, and within 2 weeks her serum creatinine level had decreased by more than 0.5 mg/dL. In mid-November 2004, she underwent right renal artery angioplasty with stent placement. After that, her serum creatinine decreased further, and 3 months later it had dropped to 1.6 mg/dL. The value continued to improve, with the lowest measurement of 1.1 mg/dL, equivalent to an estimated glomerular filtration rate of 51 mL/min/1.73 m2. This was in May 2006, 19 months after stopping lisinopril and 17 months after angioplasty and stenting. The last available serum creatinine level (August 2006) was 1.2 mg/dL, equivalent to an estimated glomerular filtration rate of 45 mL/min/1.73 m2 (Figure 1). Unfortunately, the patient died of metastatic lung cancer in December of that year.
Also of note, the patient who underwent angioplasty because of recurrent flash pulmonary edema had no recurrences of it afterward.
We concluded that, in patients with hemodynamically significant renal artery stenosis presenting with acutely worsening renal failure, renal angioplasty with stenting has the potential to reverse renal failure, improve blood pressure control, and stop flash pulmonary edema.6–8
Notably, all patients in our study who underwent renal angioplasty with stenting had new-onset acute renal injury as defined by an increase in the baseline serum creatinine of more than 25% during the 3 months before stent placement.6–8 Patients in the STAR,2 HERCULES,4 and CORAL5 studies had renal artery stenosis but otherwise stable chronic kidney disease at the time of enrollment. In the ASTRAL study,3 12% of the patients had acute kidney injury on study enrollment, defined as an increase in the serum creatinine level of more than 20% or of more than 1.13 mg/dL.3
While we strongly agree with aggressive yet monitored medical therapy for patients with hemodynamically significant renal artery stenosis, I posit that selected patients do indeed derive significant clinical benefits from renal angioplasty and stenting. Our group’s prospective individual-patient-level data support the paradigm that angioplasty with stenting is useful in patients with renal artery stenosis who experience “acute-on-chronic” kidney disease.
The pathophysiology of renal artery stenosis and the progression of chronic kidney disease are complex, and many factors affect patient outcomes and response to treatment. Thus, the message is that treatment of severe renal artery stenosis must be individualized.9–11 No one treatment fits all.10,11
- Kabach A, Agha OQ, Baibars M, Alraiyes AH, Alraies MC. Does stenting of severe renal artery stenosis improve outcomes compared with medical therapy alone? Cleve Clin J Med 2015; 82:491–494.
- Bax L, Mali WP, Buskens E, et al; STAR Study Group. The benefit of STent placement and blood pressure and lipid-lowering for the prevention of progression of renal dysfunction caused by Atherosclerotic ostial stenosis of the Renal artery. The STAR-study: rationale and study design. J Nephrol 2003; 16:807–812.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Jaff MR, Bates M, Sullivan T, et al; HERCULES Investigators. Significant reduction in systolic blood pressure following renal artery stenting in patients with uncontrolled hypertension: results from the HERCULES trial. Catheter Cardiovasc Interv 2012; 80:343–350.
- Cooper CJ, Murphy TP, Cutlip DE, et al; CORAL Investigators. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med 2014; 370:13–22.
- Onuigbo MAC, Onuigbo NTC. Worsening renal failure in older chronic kidney disease patients with renal artery stenosis concurrently on renin angiotensin aldosterone system blockade: a prospective 50-month Mayo Health System clinic analysis. QJM 2008; 101:519–527.
- Onuigbo MA, Onuigbo NT. Renal failure and concurrent RAAS blockade in older CKD patients with renal artery stenosis: an extended Mayo Clinic prospective 63-month experience. Ren Fail 2008; 30:363–371.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary. J Am Coll Cardiol 2006; 47:1239–1312.
- Onuigbo M, Frenandes R, Nijhawan V. The ASTRAL trial results revisited—to stent or not to stent in renal artery stenosis? QJM 2010; 103:357.
- Singh M, Kovacs DF, Singh A, Dhaliwal P, Khosla S. ACE inhibition and renal artery stenosis: what lessons have we learnt? A 21st century perspective. In: Onuigbo MAC, ed. ACE inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 2. New York, NY: NOVA Publishers; 2013:203–218.
- Onuigbo MA, Onuigbo C, Onuigbo V, et al. The CKD enigma, reengineering CKD care, narrowing asymmetric information and confronting ethicomedicinomics in CKD care: the introduction of the new 'CKD express©' IT software program. In: Onuigbo MAC, ed. ACE Inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 1. New York, NY: NOVA Publishers; 2013: 41–56.
- Kabach A, Agha OQ, Baibars M, Alraiyes AH, Alraies MC. Does stenting of severe renal artery stenosis improve outcomes compared with medical therapy alone? Cleve Clin J Med 2015; 82:491–494.
- Bax L, Mali WP, Buskens E, et al; STAR Study Group. The benefit of STent placement and blood pressure and lipid-lowering for the prevention of progression of renal dysfunction caused by Atherosclerotic ostial stenosis of the Renal artery. The STAR-study: rationale and study design. J Nephrol 2003; 16:807–812.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Jaff MR, Bates M, Sullivan T, et al; HERCULES Investigators. Significant reduction in systolic blood pressure following renal artery stenting in patients with uncontrolled hypertension: results from the HERCULES trial. Catheter Cardiovasc Interv 2012; 80:343–350.
- Cooper CJ, Murphy TP, Cutlip DE, et al; CORAL Investigators. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med 2014; 370:13–22.
- Onuigbo MAC, Onuigbo NTC. Worsening renal failure in older chronic kidney disease patients with renal artery stenosis concurrently on renin angiotensin aldosterone system blockade: a prospective 50-month Mayo Health System clinic analysis. QJM 2008; 101:519–527.
- Onuigbo MA, Onuigbo NT. Renal failure and concurrent RAAS blockade in older CKD patients with renal artery stenosis: an extended Mayo Clinic prospective 63-month experience. Ren Fail 2008; 30:363–371.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary. J Am Coll Cardiol 2006; 47:1239–1312.
- Onuigbo M, Frenandes R, Nijhawan V. The ASTRAL trial results revisited—to stent or not to stent in renal artery stenosis? QJM 2010; 103:357.
- Singh M, Kovacs DF, Singh A, Dhaliwal P, Khosla S. ACE inhibition and renal artery stenosis: what lessons have we learnt? A 21st century perspective. In: Onuigbo MAC, ed. ACE inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 2. New York, NY: NOVA Publishers; 2013:203–218.
- Onuigbo MA, Onuigbo C, Onuigbo V, et al. The CKD enigma, reengineering CKD care, narrowing asymmetric information and confronting ethicomedicinomics in CKD care: the introduction of the new 'CKD express©' IT software program. In: Onuigbo MAC, ed. ACE Inhibitors: Medical Uses, Mechanisms of Action, Potential Adverse Effects and Related Topics. Volume 1. New York, NY: NOVA Publishers; 2013: 41–56.