User login
IN THIS ARTICLE
- Prostate cancer screening tools
- Ethic disparities
- Screening guidance
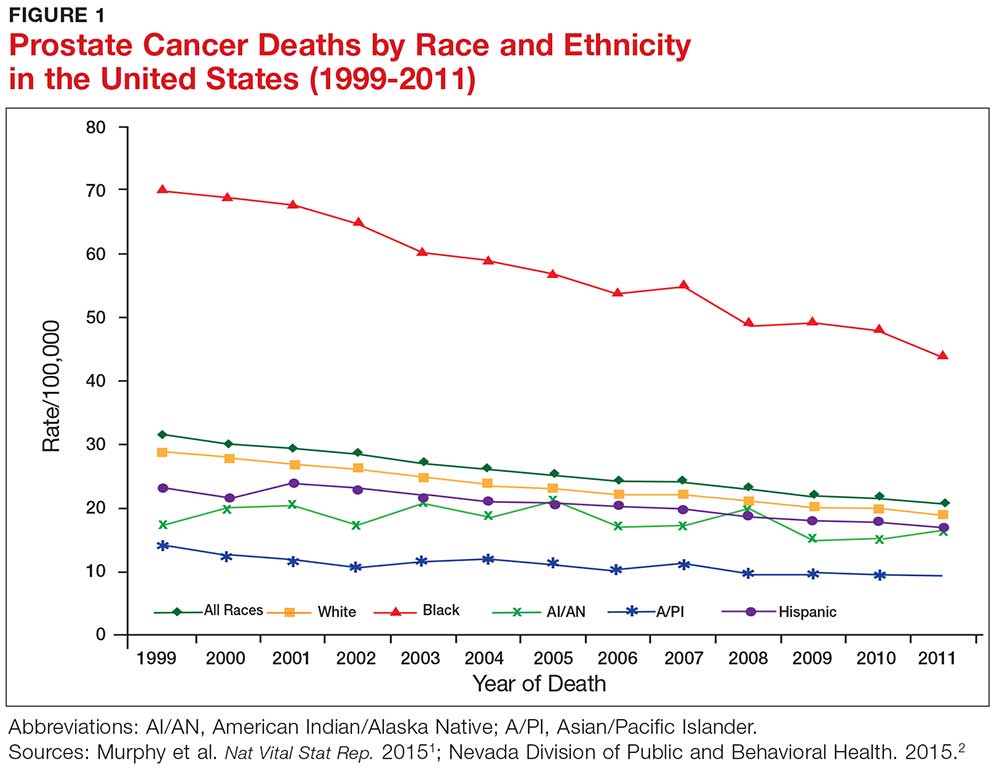
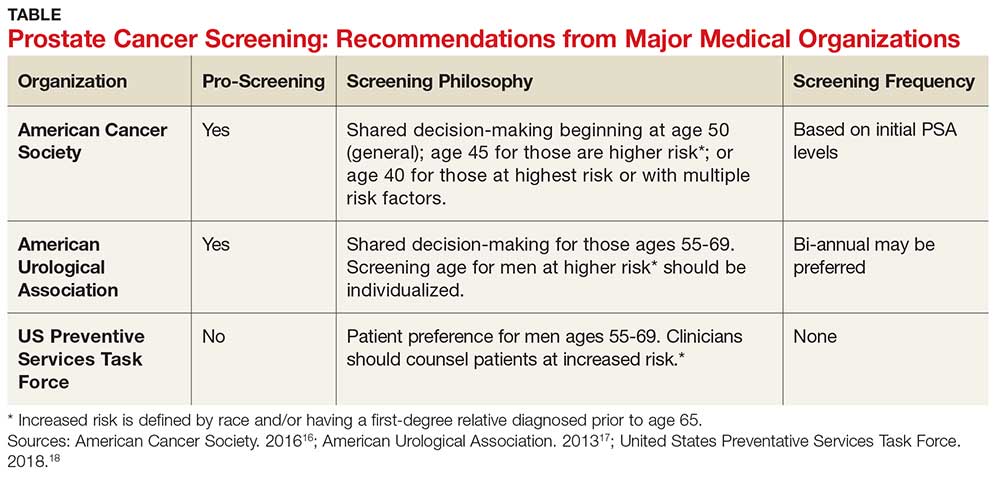
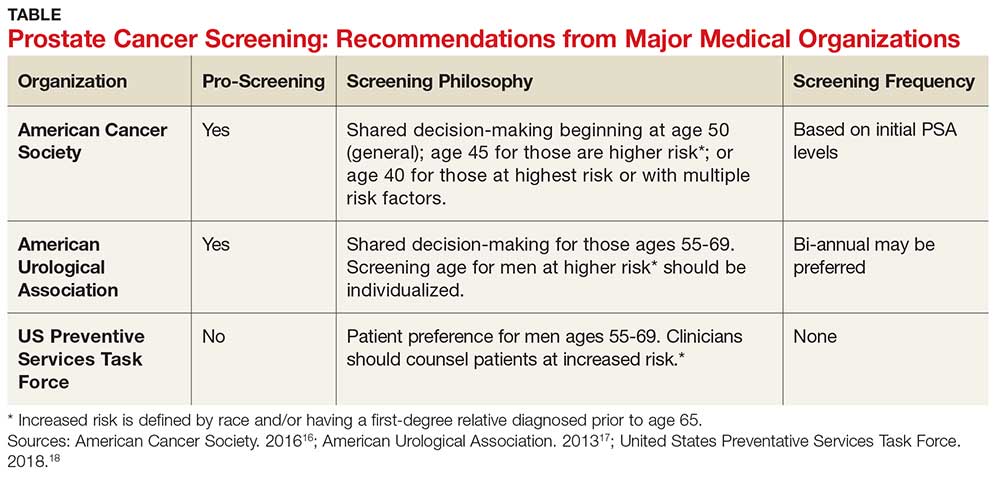
Prostate cancer, the second most common cancer to affect American men, is a slow-growing cancer that is curable when detected early. While the overall incidence has declined in the past 20 years (see Figure 1), prostate cancer remains a major concern among black men due to disproportionate incidence and mortality rates.1-3 A general understanding of the prostate and of prostate cancer lays the groundwork to acknowledge and address this divide.
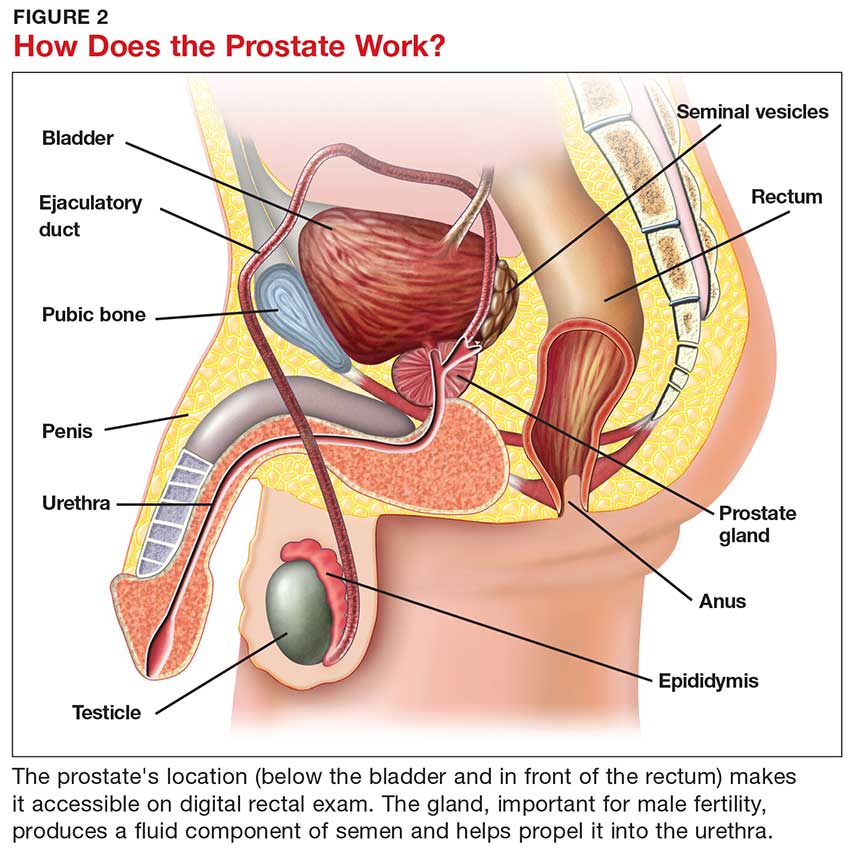
Although most men know where the prostate gland is located, many do not understand how it functions.4 The largest accessory gland of the male reproductive system, the prostate is located below the bladder and in front of the rectum (see Figure 2).5 The urethra passes through this gland; therefore, enlargement of the prostate can cause constriction of the urethra, which can affect the ability to eliminate urine from the body.5
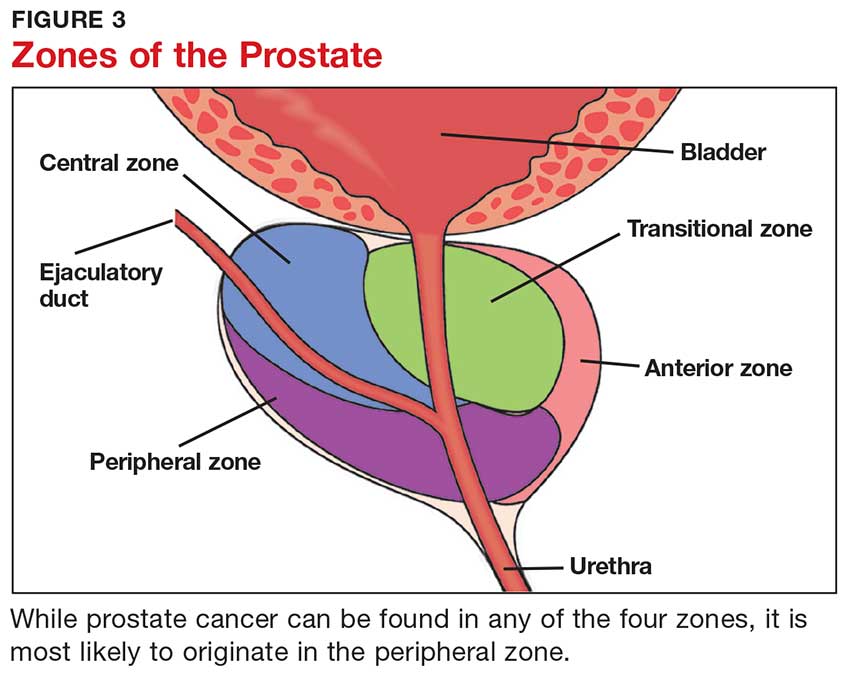
The prostate is broken down into four distinct regions (see Figure 3). Certain types of inflammation may occur more often in some regions of the prostate than others; as such, 75% of prostate cancer occurs in the peripheral zone (the region located closest to the rectal wall).5,6
DIAGNOSING PROSTATE CANCER
Signs and symptoms
According to the CDC, the signs and symptoms of prostate cancer include
- Difficulty starting urination
- Weak or interrupted flow of urine
- Frequent urination (especially at night)
- Difficulty emptying the bladder
- Pain or burning during urination
- Blood in the urine or semen
- Pain in the back, hips, or pelvis
- Painful ejaculation.
However, none of these signs and symptoms are unique to prostate cancer.7 For instance, difficulty starting urination, weak or interrupted flow of urine, and frequent urination can also be attributed to benign prostatic hyperplasia. Further, in its early stages, prostate cancer may not exhibit any signs or symptoms, making accurate screening essential for detection and treatment.7
Screening tools
There are two primary tools for detection of prostate cancer: the prostate-specific antigen (PSA) test and the digital rectal exam (DRE).8 The blood test for PSA is routinely used as a screening tool and is therefore considered a standard test for prostate cancer.9 A PSA level above 4.0 ng/mL is considered abnormal.10 Although measuring the PSA level can improve the odds of early prostate cancer detection, there is considerable debate over its dependability in this regard, as PSA can be elevated for benign reasons.
Sociocultural and genetic risk factors
While both black and white men are at an increased risk for prostate cancer if a first-degree relative (ie, father, brother, son) had the disease, one in five black men will develop prostate cancer in their lifetimes, compared with one in seven white men.3 And despite a five-year survival rate of nearly 100% for regional prostate cancer, black men are more than two times as likely as white men to die of the disease (1 in 23 and 1 in 38, respectively).8,11 From 2011 to 2015, the age-adjusted mortality rate of prostate cancer among black men was 40.8, versus 18.2 for non-Hispanic white men (per 100,000 population).12
Continue to: The disparity in prostate cancer mortality...
The disparity in prostate cancer mortality among black men has been attributed to multiple variables. Cultural differences can play a role in whether patients choose to undergo prostate cancer screening. Black men are, for example, less likely than other men to participate in preventive health care practices.13 Although an in-depth discussion is outside the scope of this article, researchers have identified some plausible factors for this, including economic limitations, lack of access to health care, distrust of the health care system, and an indifference to pain or discomfort.13,14 Decisions surrounding prostate screening can also be affected by a patient’s perceived risk for prostate cancer, the impact of a cancer diagnosis, and the availability of treatment.
Other factors that contribute to the higher incidence and mortality rate among black men include genetic predisposition, health beliefs, and knowledge about the prostate and cancer screenings.15 While most researchers have focused on men ages 40 and older, Ogunsanya et al suggested that educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.15
PRACTICE POINTS
- Prostate cancer remains a major concern among black men due to disproportionate incidence and mortality.
- Developing prostate cancer screening recommendations for black men would help reduce mortality and morbidity in this population.
- Educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.
IMPLICATIONS FOR PRACTICE
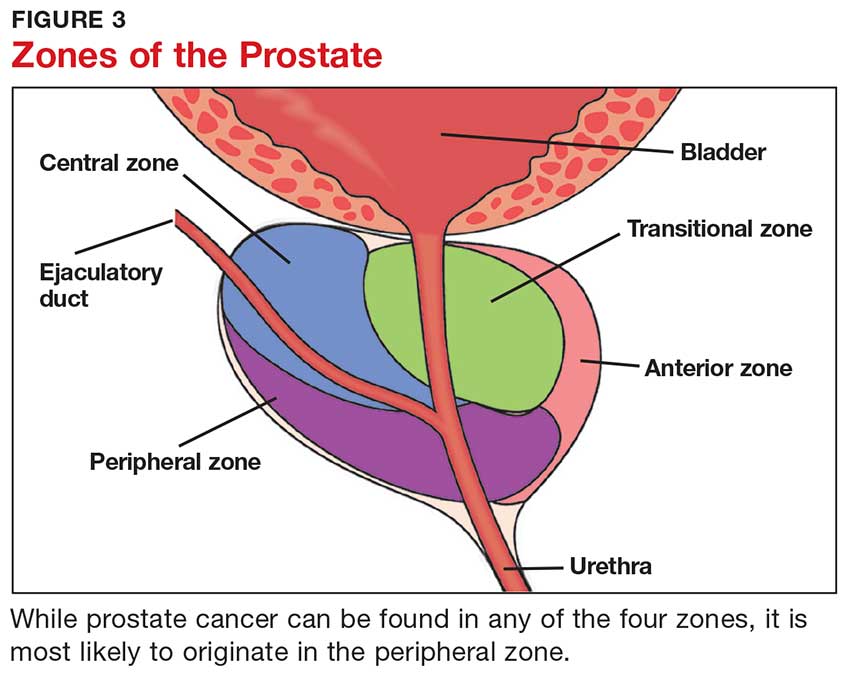
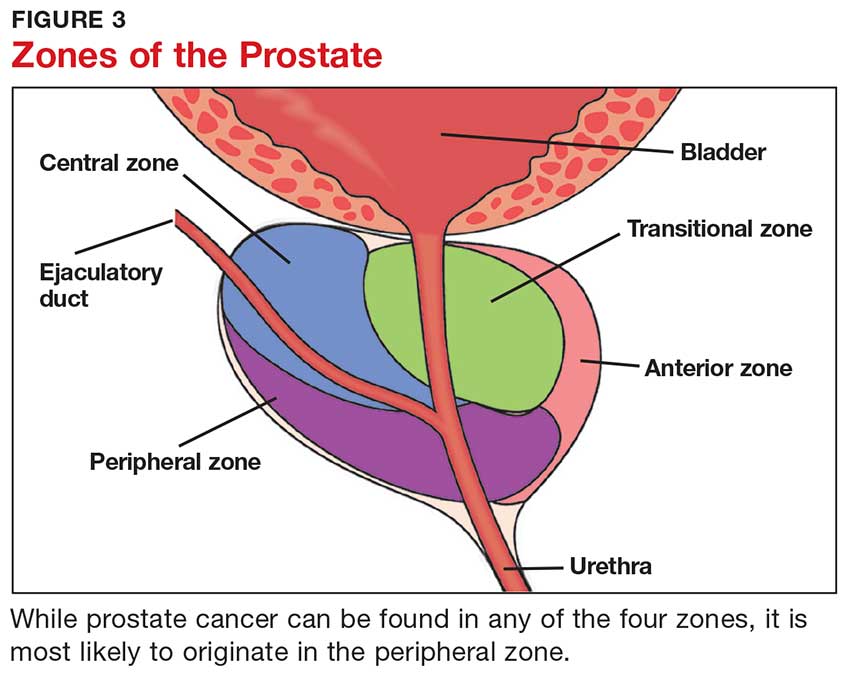
The age at which men should begin screening for prostate cancer has been a source of controversy due to the lack of consensus between the American Cancer Society, the American Urological Association, and the United States Preventive Services Task Force (USPSTF) guidelines (see Table).16-18 The current USPSTF recommendations for prostate cancer screening do not take into account ethnic differences, despite the identified racial disparity.19 Ambiguity in public health policy creates a quandary in the decision-making process regarding testing and treatment.9,19,20
In addition, these guidelines recommend the use of both the DRE and PSA screening tests. Screening should be performed every two years for men who have a PSA level < 2.5 ng/mL, and every year for men who have a level > 2.5 ng/mL.
Continue to: TREATMENT
TREATMENT
Fortunately, there are several treatment options for men who are diagnosed with prostate cancer.22 These include watchful waiting, surgery, radiation, cryotherapy, hormone therapy, and chemotherapy. The type of treatment chosen depends on many factors, such as the tumor grade or cancer stage, the implications for quality of life, and the shared provider/patient decision-making process. Indeed, choosing the right treatment is a specialized approach that varies according to case and circumstance.22
CONCLUSION
There has been an increase in prostate cancer screening in recent years. However, black men still lag behind when it comes to having DRE and PSA tests. Many factors, including cultural perceptions of medical care among black men, often cause delays in seeking evaluation and treatment. Developing consistent and uniform prostate cancer screening recommendations for black men would be an important step in reducing mortality and morbidity in this population.
1. Murphy SL, Kochanek KD, Xu J, Heron M. Deaths: final data for 2012. Nat Vital Stat Rep. 2015;63(9):37-80.
2. Nevada Division of Public and Behavioral Health. Comprehensive report: prostate cancer. September 2015. http://dpbh.nv.gov/Programs/Office_of_Public_Healh_Informatics_and_Epidemiology_(OPHIE)/. Accessed September 19, 2018.
3. Odedina FT, Dagne G, Pressey S, et al. Prostate cancer health and cultural beliefs of black men: the Florida prostate cancer disparity project. Infect Agent Cancer. 2011;6(2):1-7.
4. Winterich JA, Grzywacz JG, Quandt SA, et al. Men’s knowledge and beliefs about prostate cancer: education, race, and screening status. Ethn Dis. 2009;19(2):199-203.
5. Bhavsar A, Verma S. Anatomic imaging of the prostate. Biomed Res Int. 2014,1-9.
6. National Institutes of Health. Zones of the prostate. www.training.seer.cancer.gov/prostate/anatomy/zones.html. Accessed September 7, 2018.
7. CDC. Prostate cancer statistics. June 12, 2017. www.cdc.gov/cancer/prostate/statistics/. Accessed September 7, 2018.
8. American Cancer Society. Prostate cancer risk factors. www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/what-causes.html.
9. Mkanta W, Ndjakani Y, Bandiera F, et al. Prostate cancer screening and mortality in blacks and whites: a hospital-based case-control study. J Nat Med Assoc. 2015;107(2):32-38.
10. Hoffman R. Screening for prostate cancer. N Engl J Med. 2011;365(21):2013-2019.
11. CDC. Who is at risk for prostate cancer? June 7, 2018. www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm. Accessed September 7, 2018.
12. American Cancer Society. Cancer facts and figures 2017. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Accessed September 7, 2018.
13. Woods VD, Montgomery SB, Belliard JC, et al. Culture, black men, and prostate cancer: what is reality? Cancer Control. 2004;11(6):388-396.
14. Braithwaite RL. Health Issues in the Black Community. 2nd ed. San Francisco, Calif: Jossey-Bass Publishers; 2001.
15. Ogunsanya ME, Brown CM, Odedina FT, et al. Beliefs regarding prostate cancer screening among black males aged 18 to 40 years. Am J Mens Health. 2017;11(1):41-53.
16. American Cancer Society. American Cancer Society Recommendations for Prostate Cancer Early Detection. April 14, 2016. www.cancer.org/cancer/prostate-cancer/early-detection/acs-recommendations.html. Accessed September 7, 2018.
17. American Urological Association. Early detection of prostate cancer. 2013. www.auanet.org/guidelines/prostate-cancer-early-detection-(2013-reviewed-for-currency-2018). Accessed September 7, 2018.
18. United States Preventative Services Task Force. Final recommendation statement. Prostate cancer: screening. 2018. www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1. Accessed September 7, 2018.
19. Shenoy D, Packianathan S, Chen AM, Vijayakumar S. Do African-American men need separate prostate cancer screening guidelines? BMC Urol. 2016;16(19):1-6.
20. Odedina FT, Campbell E, LaRose-Pierre M, et al. Personal factors affecting African-American men’s prostate cancer screening behavior. J Natl Med Assoc. 2008;100(6):724-733.
IN THIS ARTICLE
- Prostate cancer screening tools
- Ethic disparities
- Screening guidance
Prostate cancer, the second most common cancer to affect American men, is a slow-growing cancer that is curable when detected early. While the overall incidence has declined in the past 20 years (see Figure 1), prostate cancer remains a major concern among black men due to disproportionate incidence and mortality rates.1-3 A general understanding of the prostate and of prostate cancer lays the groundwork to acknowledge and address this divide.
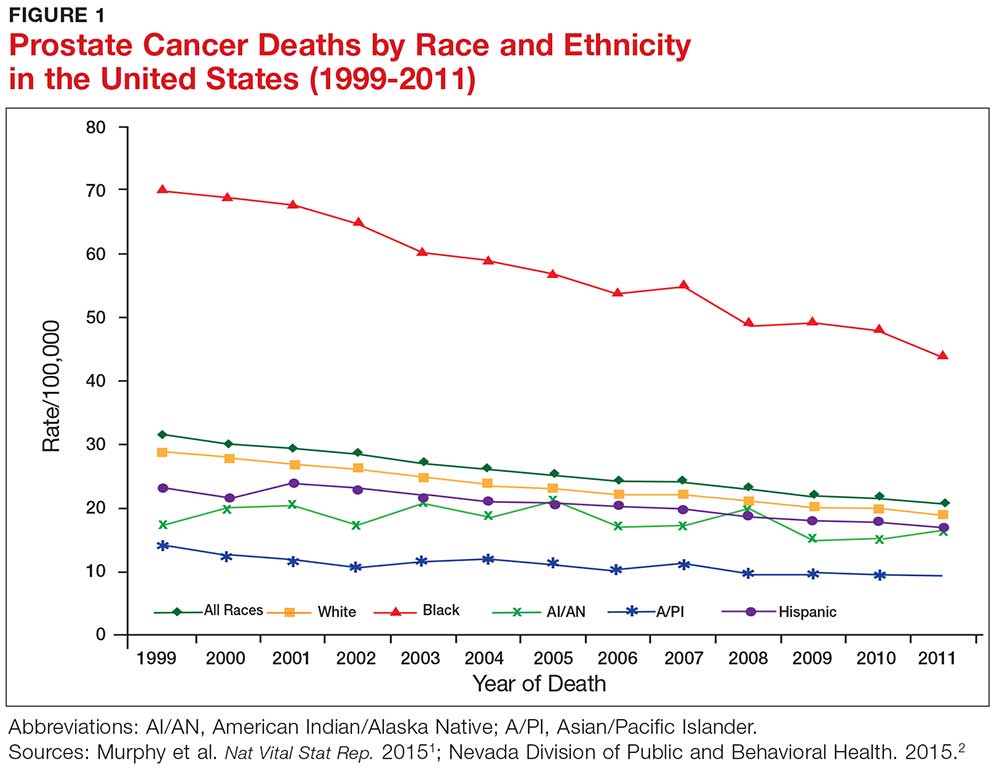
Although most men know where the prostate gland is located, many do not understand how it functions.4 The largest accessory gland of the male reproductive system, the prostate is located below the bladder and in front of the rectum (see Figure 2).5 The urethra passes through this gland; therefore, enlargement of the prostate can cause constriction of the urethra, which can affect the ability to eliminate urine from the body.5
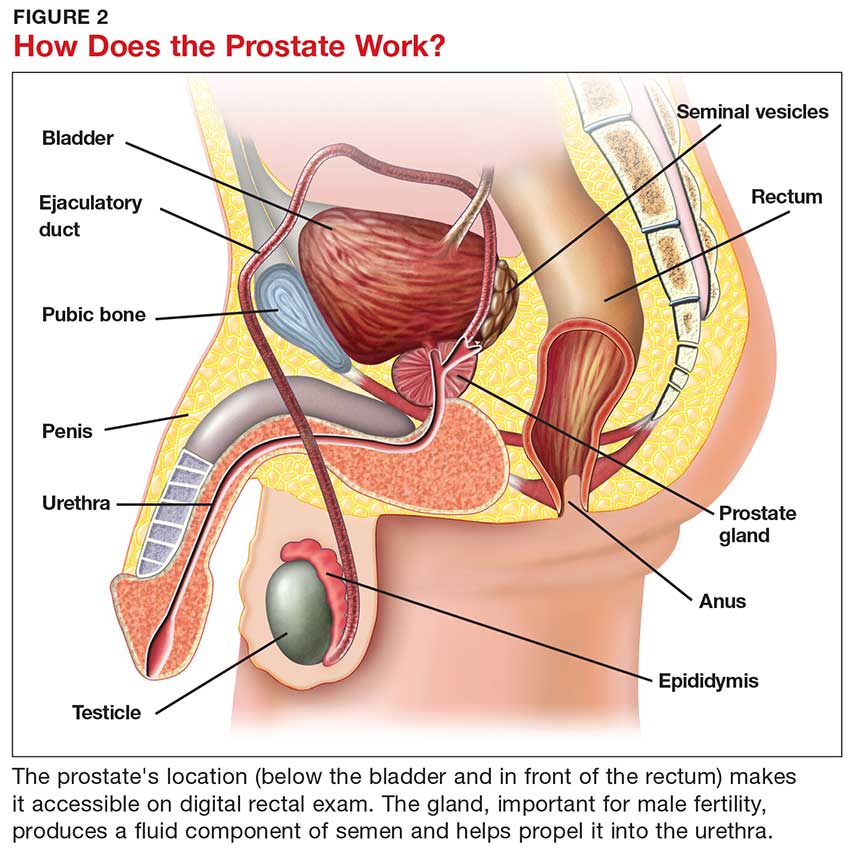
The prostate is broken down into four distinct regions (see Figure 3). Certain types of inflammation may occur more often in some regions of the prostate than others; as such, 75% of prostate cancer occurs in the peripheral zone (the region located closest to the rectal wall).5,6
DIAGNOSING PROSTATE CANCER
Signs and symptoms
According to the CDC, the signs and symptoms of prostate cancer include
- Difficulty starting urination
- Weak or interrupted flow of urine
- Frequent urination (especially at night)
- Difficulty emptying the bladder
- Pain or burning during urination
- Blood in the urine or semen
- Pain in the back, hips, or pelvis
- Painful ejaculation.
However, none of these signs and symptoms are unique to prostate cancer.7 For instance, difficulty starting urination, weak or interrupted flow of urine, and frequent urination can also be attributed to benign prostatic hyperplasia. Further, in its early stages, prostate cancer may not exhibit any signs or symptoms, making accurate screening essential for detection and treatment.7
Screening tools
There are two primary tools for detection of prostate cancer: the prostate-specific antigen (PSA) test and the digital rectal exam (DRE).8 The blood test for PSA is routinely used as a screening tool and is therefore considered a standard test for prostate cancer.9 A PSA level above 4.0 ng/mL is considered abnormal.10 Although measuring the PSA level can improve the odds of early prostate cancer detection, there is considerable debate over its dependability in this regard, as PSA can be elevated for benign reasons.
Sociocultural and genetic risk factors
While both black and white men are at an increased risk for prostate cancer if a first-degree relative (ie, father, brother, son) had the disease, one in five black men will develop prostate cancer in their lifetimes, compared with one in seven white men.3 And despite a five-year survival rate of nearly 100% for regional prostate cancer, black men are more than two times as likely as white men to die of the disease (1 in 23 and 1 in 38, respectively).8,11 From 2011 to 2015, the age-adjusted mortality rate of prostate cancer among black men was 40.8, versus 18.2 for non-Hispanic white men (per 100,000 population).12
Continue to: The disparity in prostate cancer mortality...
The disparity in prostate cancer mortality among black men has been attributed to multiple variables. Cultural differences can play a role in whether patients choose to undergo prostate cancer screening. Black men are, for example, less likely than other men to participate in preventive health care practices.13 Although an in-depth discussion is outside the scope of this article, researchers have identified some plausible factors for this, including economic limitations, lack of access to health care, distrust of the health care system, and an indifference to pain or discomfort.13,14 Decisions surrounding prostate screening can also be affected by a patient’s perceived risk for prostate cancer, the impact of a cancer diagnosis, and the availability of treatment.
Other factors that contribute to the higher incidence and mortality rate among black men include genetic predisposition, health beliefs, and knowledge about the prostate and cancer screenings.15 While most researchers have focused on men ages 40 and older, Ogunsanya et al suggested that educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.15
PRACTICE POINTS
- Prostate cancer remains a major concern among black men due to disproportionate incidence and mortality.
- Developing prostate cancer screening recommendations for black men would help reduce mortality and morbidity in this population.
- Educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.
IMPLICATIONS FOR PRACTICE
The age at which men should begin screening for prostate cancer has been a source of controversy due to the lack of consensus between the American Cancer Society, the American Urological Association, and the United States Preventive Services Task Force (USPSTF) guidelines (see Table).16-18 The current USPSTF recommendations for prostate cancer screening do not take into account ethnic differences, despite the identified racial disparity.19 Ambiguity in public health policy creates a quandary in the decision-making process regarding testing and treatment.9,19,20
In addition, these guidelines recommend the use of both the DRE and PSA screening tests. Screening should be performed every two years for men who have a PSA level < 2.5 ng/mL, and every year for men who have a level > 2.5 ng/mL.
Continue to: TREATMENT
TREATMENT
Fortunately, there are several treatment options for men who are diagnosed with prostate cancer.22 These include watchful waiting, surgery, radiation, cryotherapy, hormone therapy, and chemotherapy. The type of treatment chosen depends on many factors, such as the tumor grade or cancer stage, the implications for quality of life, and the shared provider/patient decision-making process. Indeed, choosing the right treatment is a specialized approach that varies according to case and circumstance.22
CONCLUSION
There has been an increase in prostate cancer screening in recent years. However, black men still lag behind when it comes to having DRE and PSA tests. Many factors, including cultural perceptions of medical care among black men, often cause delays in seeking evaluation and treatment. Developing consistent and uniform prostate cancer screening recommendations for black men would be an important step in reducing mortality and morbidity in this population.
IN THIS ARTICLE
- Prostate cancer screening tools
- Ethic disparities
- Screening guidance
Prostate cancer, the second most common cancer to affect American men, is a slow-growing cancer that is curable when detected early. While the overall incidence has declined in the past 20 years (see Figure 1), prostate cancer remains a major concern among black men due to disproportionate incidence and mortality rates.1-3 A general understanding of the prostate and of prostate cancer lays the groundwork to acknowledge and address this divide.
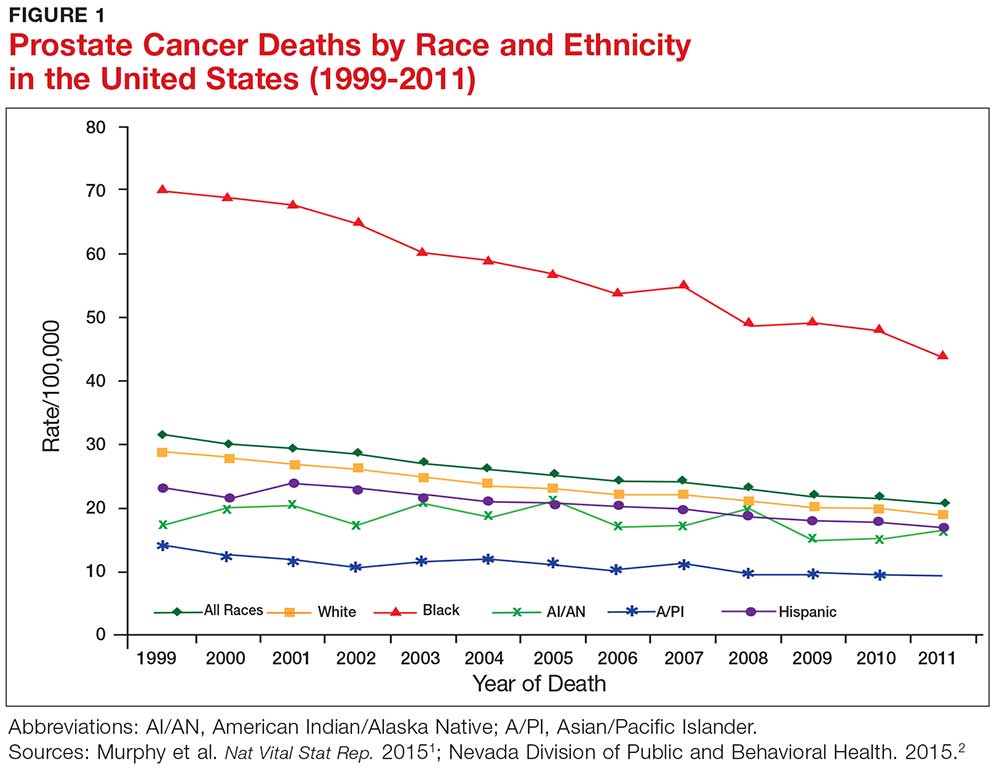
Although most men know where the prostate gland is located, many do not understand how it functions.4 The largest accessory gland of the male reproductive system, the prostate is located below the bladder and in front of the rectum (see Figure 2).5 The urethra passes through this gland; therefore, enlargement of the prostate can cause constriction of the urethra, which can affect the ability to eliminate urine from the body.5
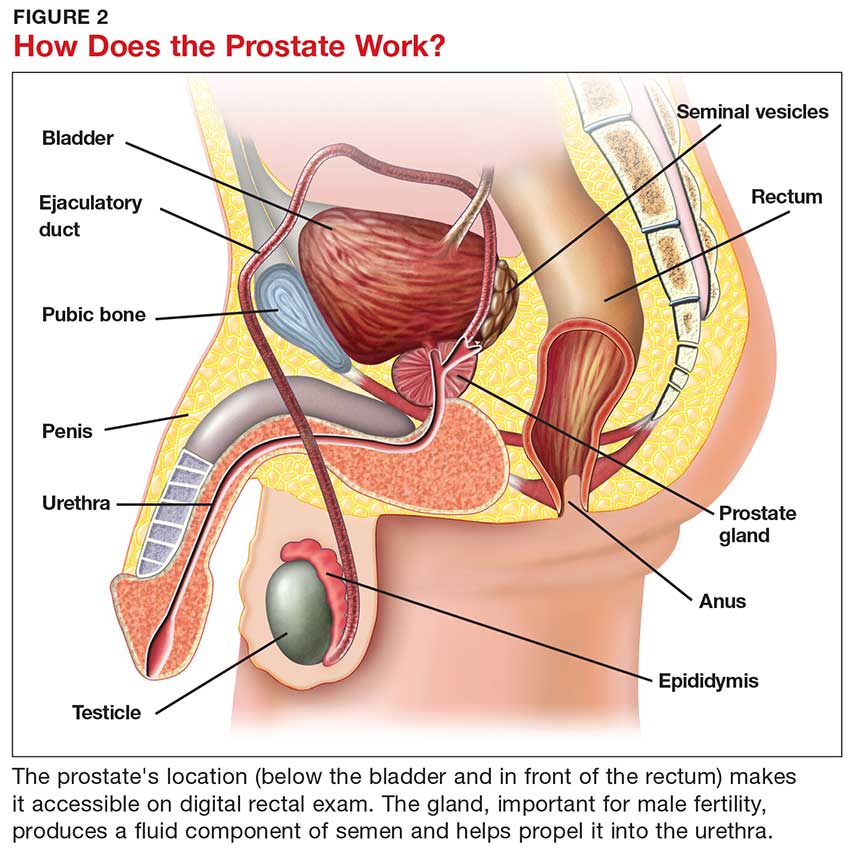
The prostate is broken down into four distinct regions (see Figure 3). Certain types of inflammation may occur more often in some regions of the prostate than others; as such, 75% of prostate cancer occurs in the peripheral zone (the region located closest to the rectal wall).5,6
DIAGNOSING PROSTATE CANCER
Signs and symptoms
According to the CDC, the signs and symptoms of prostate cancer include
- Difficulty starting urination
- Weak or interrupted flow of urine
- Frequent urination (especially at night)
- Difficulty emptying the bladder
- Pain or burning during urination
- Blood in the urine or semen
- Pain in the back, hips, or pelvis
- Painful ejaculation.
However, none of these signs and symptoms are unique to prostate cancer.7 For instance, difficulty starting urination, weak or interrupted flow of urine, and frequent urination can also be attributed to benign prostatic hyperplasia. Further, in its early stages, prostate cancer may not exhibit any signs or symptoms, making accurate screening essential for detection and treatment.7
Screening tools
There are two primary tools for detection of prostate cancer: the prostate-specific antigen (PSA) test and the digital rectal exam (DRE).8 The blood test for PSA is routinely used as a screening tool and is therefore considered a standard test for prostate cancer.9 A PSA level above 4.0 ng/mL is considered abnormal.10 Although measuring the PSA level can improve the odds of early prostate cancer detection, there is considerable debate over its dependability in this regard, as PSA can be elevated for benign reasons.
Sociocultural and genetic risk factors
While both black and white men are at an increased risk for prostate cancer if a first-degree relative (ie, father, brother, son) had the disease, one in five black men will develop prostate cancer in their lifetimes, compared with one in seven white men.3 And despite a five-year survival rate of nearly 100% for regional prostate cancer, black men are more than two times as likely as white men to die of the disease (1 in 23 and 1 in 38, respectively).8,11 From 2011 to 2015, the age-adjusted mortality rate of prostate cancer among black men was 40.8, versus 18.2 for non-Hispanic white men (per 100,000 population).12
Continue to: The disparity in prostate cancer mortality...
The disparity in prostate cancer mortality among black men has been attributed to multiple variables. Cultural differences can play a role in whether patients choose to undergo prostate cancer screening. Black men are, for example, less likely than other men to participate in preventive health care practices.13 Although an in-depth discussion is outside the scope of this article, researchers have identified some plausible factors for this, including economic limitations, lack of access to health care, distrust of the health care system, and an indifference to pain or discomfort.13,14 Decisions surrounding prostate screening can also be affected by a patient’s perceived risk for prostate cancer, the impact of a cancer diagnosis, and the availability of treatment.
Other factors that contribute to the higher incidence and mortality rate among black men include genetic predisposition, health beliefs, and knowledge about the prostate and cancer screenings.15 While most researchers have focused on men ages 40 and older, Ogunsanya et al suggested that educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.15
PRACTICE POINTS
- Prostate cancer remains a major concern among black men due to disproportionate incidence and mortality.
- Developing prostate cancer screening recommendations for black men would help reduce mortality and morbidity in this population.
- Educating black men about screening for prostate cancer at an earlier age may help them to make informed decisions later in life.
IMPLICATIONS FOR PRACTICE
The age at which men should begin screening for prostate cancer has been a source of controversy due to the lack of consensus between the American Cancer Society, the American Urological Association, and the United States Preventive Services Task Force (USPSTF) guidelines (see Table).16-18 The current USPSTF recommendations for prostate cancer screening do not take into account ethnic differences, despite the identified racial disparity.19 Ambiguity in public health policy creates a quandary in the decision-making process regarding testing and treatment.9,19,20
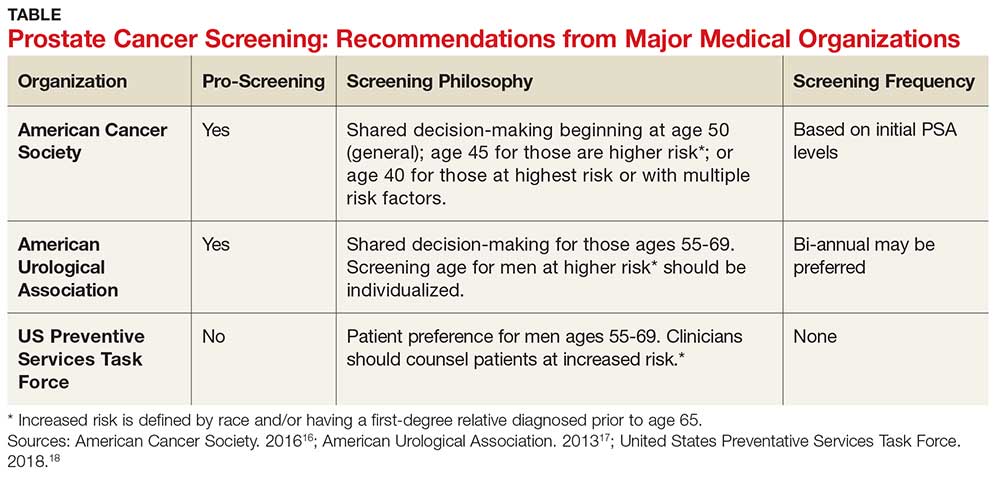
In addition, these guidelines recommend the use of both the DRE and PSA screening tests. Screening should be performed every two years for men who have a PSA level < 2.5 ng/mL, and every year for men who have a level > 2.5 ng/mL.
Continue to: TREATMENT
TREATMENT
Fortunately, there are several treatment options for men who are diagnosed with prostate cancer.22 These include watchful waiting, surgery, radiation, cryotherapy, hormone therapy, and chemotherapy. The type of treatment chosen depends on many factors, such as the tumor grade or cancer stage, the implications for quality of life, and the shared provider/patient decision-making process. Indeed, choosing the right treatment is a specialized approach that varies according to case and circumstance.22
CONCLUSION
There has been an increase in prostate cancer screening in recent years. However, black men still lag behind when it comes to having DRE and PSA tests. Many factors, including cultural perceptions of medical care among black men, often cause delays in seeking evaluation and treatment. Developing consistent and uniform prostate cancer screening recommendations for black men would be an important step in reducing mortality and morbidity in this population.
1. Murphy SL, Kochanek KD, Xu J, Heron M. Deaths: final data for 2012. Nat Vital Stat Rep. 2015;63(9):37-80.
2. Nevada Division of Public and Behavioral Health. Comprehensive report: prostate cancer. September 2015. http://dpbh.nv.gov/Programs/Office_of_Public_Healh_Informatics_and_Epidemiology_(OPHIE)/. Accessed September 19, 2018.
3. Odedina FT, Dagne G, Pressey S, et al. Prostate cancer health and cultural beliefs of black men: the Florida prostate cancer disparity project. Infect Agent Cancer. 2011;6(2):1-7.
4. Winterich JA, Grzywacz JG, Quandt SA, et al. Men’s knowledge and beliefs about prostate cancer: education, race, and screening status. Ethn Dis. 2009;19(2):199-203.
5. Bhavsar A, Verma S. Anatomic imaging of the prostate. Biomed Res Int. 2014,1-9.
6. National Institutes of Health. Zones of the prostate. www.training.seer.cancer.gov/prostate/anatomy/zones.html. Accessed September 7, 2018.
7. CDC. Prostate cancer statistics. June 12, 2017. www.cdc.gov/cancer/prostate/statistics/. Accessed September 7, 2018.
8. American Cancer Society. Prostate cancer risk factors. www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/what-causes.html.
9. Mkanta W, Ndjakani Y, Bandiera F, et al. Prostate cancer screening and mortality in blacks and whites: a hospital-based case-control study. J Nat Med Assoc. 2015;107(2):32-38.
10. Hoffman R. Screening for prostate cancer. N Engl J Med. 2011;365(21):2013-2019.
11. CDC. Who is at risk for prostate cancer? June 7, 2018. www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm. Accessed September 7, 2018.
12. American Cancer Society. Cancer facts and figures 2017. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Accessed September 7, 2018.
13. Woods VD, Montgomery SB, Belliard JC, et al. Culture, black men, and prostate cancer: what is reality? Cancer Control. 2004;11(6):388-396.
14. Braithwaite RL. Health Issues in the Black Community. 2nd ed. San Francisco, Calif: Jossey-Bass Publishers; 2001.
15. Ogunsanya ME, Brown CM, Odedina FT, et al. Beliefs regarding prostate cancer screening among black males aged 18 to 40 years. Am J Mens Health. 2017;11(1):41-53.
16. American Cancer Society. American Cancer Society Recommendations for Prostate Cancer Early Detection. April 14, 2016. www.cancer.org/cancer/prostate-cancer/early-detection/acs-recommendations.html. Accessed September 7, 2018.
17. American Urological Association. Early detection of prostate cancer. 2013. www.auanet.org/guidelines/prostate-cancer-early-detection-(2013-reviewed-for-currency-2018). Accessed September 7, 2018.
18. United States Preventative Services Task Force. Final recommendation statement. Prostate cancer: screening. 2018. www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1. Accessed September 7, 2018.
19. Shenoy D, Packianathan S, Chen AM, Vijayakumar S. Do African-American men need separate prostate cancer screening guidelines? BMC Urol. 2016;16(19):1-6.
20. Odedina FT, Campbell E, LaRose-Pierre M, et al. Personal factors affecting African-American men’s prostate cancer screening behavior. J Natl Med Assoc. 2008;100(6):724-733.
1. Murphy SL, Kochanek KD, Xu J, Heron M. Deaths: final data for 2012. Nat Vital Stat Rep. 2015;63(9):37-80.
2. Nevada Division of Public and Behavioral Health. Comprehensive report: prostate cancer. September 2015. http://dpbh.nv.gov/Programs/Office_of_Public_Healh_Informatics_and_Epidemiology_(OPHIE)/. Accessed September 19, 2018.
3. Odedina FT, Dagne G, Pressey S, et al. Prostate cancer health and cultural beliefs of black men: the Florida prostate cancer disparity project. Infect Agent Cancer. 2011;6(2):1-7.
4. Winterich JA, Grzywacz JG, Quandt SA, et al. Men’s knowledge and beliefs about prostate cancer: education, race, and screening status. Ethn Dis. 2009;19(2):199-203.
5. Bhavsar A, Verma S. Anatomic imaging of the prostate. Biomed Res Int. 2014,1-9.
6. National Institutes of Health. Zones of the prostate. www.training.seer.cancer.gov/prostate/anatomy/zones.html. Accessed September 7, 2018.
7. CDC. Prostate cancer statistics. June 12, 2017. www.cdc.gov/cancer/prostate/statistics/. Accessed September 7, 2018.
8. American Cancer Society. Prostate cancer risk factors. www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/what-causes.html.
9. Mkanta W, Ndjakani Y, Bandiera F, et al. Prostate cancer screening and mortality in blacks and whites: a hospital-based case-control study. J Nat Med Assoc. 2015;107(2):32-38.
10. Hoffman R. Screening for prostate cancer. N Engl J Med. 2011;365(21):2013-2019.
11. CDC. Who is at risk for prostate cancer? June 7, 2018. www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm. Accessed September 7, 2018.
12. American Cancer Society. Cancer facts and figures 2017. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Accessed September 7, 2018.
13. Woods VD, Montgomery SB, Belliard JC, et al. Culture, black men, and prostate cancer: what is reality? Cancer Control. 2004;11(6):388-396.
14. Braithwaite RL. Health Issues in the Black Community. 2nd ed. San Francisco, Calif: Jossey-Bass Publishers; 2001.
15. Ogunsanya ME, Brown CM, Odedina FT, et al. Beliefs regarding prostate cancer screening among black males aged 18 to 40 years. Am J Mens Health. 2017;11(1):41-53.
16. American Cancer Society. American Cancer Society Recommendations for Prostate Cancer Early Detection. April 14, 2016. www.cancer.org/cancer/prostate-cancer/early-detection/acs-recommendations.html. Accessed September 7, 2018.
17. American Urological Association. Early detection of prostate cancer. 2013. www.auanet.org/guidelines/prostate-cancer-early-detection-(2013-reviewed-for-currency-2018). Accessed September 7, 2018.
18. United States Preventative Services Task Force. Final recommendation statement. Prostate cancer: screening. 2018. www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1. Accessed September 7, 2018.
19. Shenoy D, Packianathan S, Chen AM, Vijayakumar S. Do African-American men need separate prostate cancer screening guidelines? BMC Urol. 2016;16(19):1-6.
20. Odedina FT, Campbell E, LaRose-Pierre M, et al. Personal factors affecting African-American men’s prostate cancer screening behavior. J Natl Med Assoc. 2008;100(6):724-733.