User login
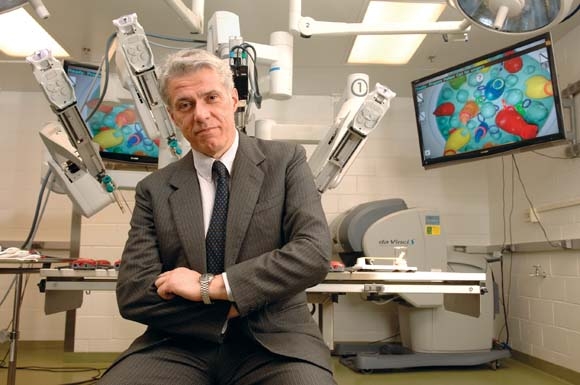
The way Dr. Pier Cristoforo Giulianotti sees it, robots will play an increasingly prominent role in the future of surgery. He should know. Dr. Giulianotti, the Lloyd Nyhus Professor of Surgery and chief, division of minimally invasive, general, and robotic surgery at the University of Illinois at Chicago, pioneered robotic lung resection in 2002 and was the first surgeon to perform a robotic Whipple procedure in 2001.
"In my opinion there is no way back from robotic surgery," he said in an interview. "It’s in the destiny of humanity, for the simple reason: to perform more precisely and to overcome our limitations – not only manual limitations, the ability to control movements at a microscopic level, for example – but also diagnostic limitations. The computer and the artificial intelligence of the future will integrate our senses and our mechanical abilities, so we will be able to perform more precisely on selected targets."
Currently, most abdominal procedures performed at the University of Illinois Medical Center are done robotically, including the Whipple procedure, splenectomy, total gastrectomy, lung lobectomy, colorectal surgery, thyroidectomy, adrenalectomy, esophagectomy, major hepatectomies, and common bile duct procedures. The robot "has enormous benefits for the patients," Dr. Giulianotti said. "Open procedures involve a longer postoperative stay and more complications, and it takes more time to enter adjuvant oncological treatment after surgery, and there is less blood loss."
In Dr. Giulianotti’s published experience of 134 robotic-assisted laparoscopic pancreatic surgery procedures, morbidity was 26%, mortality was 2.2%, the conversion rate was 10.4%, and the fistula rate was 20.9%. The majority were grade A fistulas not requiring any treatment (Surg. Endosc. 2010; 24:1646-57). He said that robotic surgery "enables difficult technical maneuvers to be performed that facilitate the success of pancreatic minimally invasive surgery. The results in this series demonstrate feasibility and safety with clinical outcomes."
In a separate study, investigators who compared 32 open vs. 28 laparoscopic vs. 17 robotic distal pancreatectomies found that all three procedures resulted in a similar cost, while the robotic group had a shorter hospital stay, a higher rate of spleen-preserving cases, and an increased operative time, compared with patients in the other two groups (Surgery 2010;148:814-23).
Pelvic indications that are becoming the gold standard for robotic surgery include robotic prostatectomy and resection for rectal cancer. "When you have a very deep and complex surgical field like the pelvis, and you need to do a radical resection for cancer while at the same time sparing nerves that can be important for urinary function, the robot combines three-dimensional vision plus improved functionality of the instruments, allowing for a more precise dissection," Dr. Giulianotti said.
Dr. Leela M. Prasad, chief of the division of colon and rectal surgery at the University of Illinois at Chicago, described robotic-assisted surgery for rectal cancer as "far superior to anything we know right now," especially in overweight males. According to combined results from three published studies, circumferential margin positivity ranged from 0 to 7%, which, Dr. Prasad said, is significantly lower than the average number of positive margins reported following open and laparoscopic rectal surgery procedures (14% and 16%, respectively) (Ann. Surg. Oncol. 2007;14:3168-73; Surg. Oncol. 2009;16:1480-7; Dis. Colon Rectum 2009;52:1824-30).
At the present time, however, in his clinical experience there are no significant differences in outcomes between robotic-assisted and laparoscopically assisted open surgery for colon cancer. "We looked at our data, and it did not make any difference robotically or laparoscopically in terms of length of stay, lymph node harvest, or survival," he said. A recent study from Korean investigators supports those findings (Surg. Endosc. 2012 Dec. 13).
Dr. Giulianotti estimated that there are more than 1,600 robotic surgery systems in the United States. Some of them are devoted to urologic or gynecologic applications, "but in the majority of hospitals there is a growing tendency to use the robot as part of a multidisciplinary program," he said. "That means at the same institution different surgical teams on different days are using the robot for different indications. Of the 1,600 systems out there, I would estimate that about half are used for general surgery."
While hospital administrators have warmed up to the idea of initiating robotic surgery programs at their institutions in recent years, Dr. Giulianotti and Dr. Prasad both called for a culture change in terms of how surgeons and medical educators think about the robot’s place in clinical medicine. "There is a cultural resistance in accepting big changes in surgery," Dr. Giulianotti said. "Academic medical institutions can play a key role here. They need to start teaching robotics in a mandatory way by offering training opportunities in a lab. We also believe that simulation has a big future in this kind of training."
The economic investment required to launch a robotic surgery program is another challenge. "Some hospitals are only concerned about the cost," he said. "When you are doing the same procedure laparoscopically, the cost is probably about 30% less. In the future I hope we can better impact the overall economic aspect of surgical procedures. That means speeding up the postoperative and outpatient treatment of some pathologies. We are already doing Nissen fundoplication and gallbladder removal with robotic surgery, and patients are being discharged a few hours after the surgery."
Dr. Prasad said the field will be poised to further advance when makers of robotic surgery devices and instruments improve on existing technology. "I am using the same robot and instruments as I was using 3 years ago," he said. "I think we need new technologies – including a smaller robot to cut down the costs and speed up the operations. This will make it easier for patients."
To launch a successful robotic surgery program in this day and age, "you need a good team of nurses and surgeons who are dedicated to doing robotic surgery," Dr. Prasad concluded. "It is dangerous in the hands of a surgeon who is not qualified."
Dr. Giulianotti said that he had no relevant financial conflicts to disclose. Dr. Prasad disclosed that he has received honoraria from Intuitive Surgical, Ethicon Endo-Surgery, and Covidien.
I would like to congratulate Dr. Pier Cristoforo Giulianotti for his work to date demonstrating the effectiveness of robotic pancreatic surgery. Clearly the “robot,” as it is affectionately termed, is here to stay.
It has clear applications in all surgical subspecialties and is being embraced by surgeons, administrators, and patients as an important tool. It is a platform that will facilitate future developments that are certain to change the way we practice our craft.
Dr. John Sweeney |
Given the focus being placed on the value of health care deliveredin the United States, it is incumbent upon surgeons to continuously evaluate the quality and costs of each intervention that we offer to our patients. To many, this type of evaluative process might seem to come up short when it comes to robotic applications for many minimally invasive procedures. Quality in most studies has been equivalent, while the costs associated with this expensive technology can be very significant. Because this new piece of technology is the first step in a new direction, we must continue to place the time, effort and cost into refining, enhancing and improving it’s applications as the technology stands today. However unless we are able to accomplish this goal, I fear we fall into the trap of “using a Cadillac for a golf cart” which is something that the U.S. health care system cannot afford nor sustain.
Dr. John Sweeney, is an ACS Fellow and the W. Dean Warren Distinguished Chair in Surgery at Emory University, Atlanta.
I would like to congratulate Dr. Pier Cristoforo Giulianotti for his work to date demonstrating the effectiveness of robotic pancreatic surgery. Clearly the “robot,” as it is affectionately termed, is here to stay.
It has clear applications in all surgical subspecialties and is being embraced by surgeons, administrators, and patients as an important tool. It is a platform that will facilitate future developments that are certain to change the way we practice our craft.
Dr. John Sweeney |
Given the focus being placed on the value of health care deliveredin the United States, it is incumbent upon surgeons to continuously evaluate the quality and costs of each intervention that we offer to our patients. To many, this type of evaluative process might seem to come up short when it comes to robotic applications for many minimally invasive procedures. Quality in most studies has been equivalent, while the costs associated with this expensive technology can be very significant. Because this new piece of technology is the first step in a new direction, we must continue to place the time, effort and cost into refining, enhancing and improving it’s applications as the technology stands today. However unless we are able to accomplish this goal, I fear we fall into the trap of “using a Cadillac for a golf cart” which is something that the U.S. health care system cannot afford nor sustain.
Dr. John Sweeney, is an ACS Fellow and the W. Dean Warren Distinguished Chair in Surgery at Emory University, Atlanta.
I would like to congratulate Dr. Pier Cristoforo Giulianotti for his work to date demonstrating the effectiveness of robotic pancreatic surgery. Clearly the “robot,” as it is affectionately termed, is here to stay.
It has clear applications in all surgical subspecialties and is being embraced by surgeons, administrators, and patients as an important tool. It is a platform that will facilitate future developments that are certain to change the way we practice our craft.
Dr. John Sweeney |
Given the focus being placed on the value of health care deliveredin the United States, it is incumbent upon surgeons to continuously evaluate the quality and costs of each intervention that we offer to our patients. To many, this type of evaluative process might seem to come up short when it comes to robotic applications for many minimally invasive procedures. Quality in most studies has been equivalent, while the costs associated with this expensive technology can be very significant. Because this new piece of technology is the first step in a new direction, we must continue to place the time, effort and cost into refining, enhancing and improving it’s applications as the technology stands today. However unless we are able to accomplish this goal, I fear we fall into the trap of “using a Cadillac for a golf cart” which is something that the U.S. health care system cannot afford nor sustain.
Dr. John Sweeney, is an ACS Fellow and the W. Dean Warren Distinguished Chair in Surgery at Emory University, Atlanta.
The way Dr. Pier Cristoforo Giulianotti sees it, robots will play an increasingly prominent role in the future of surgery. He should know. Dr. Giulianotti, the Lloyd Nyhus Professor of Surgery and chief, division of minimally invasive, general, and robotic surgery at the University of Illinois at Chicago, pioneered robotic lung resection in 2002 and was the first surgeon to perform a robotic Whipple procedure in 2001.
"In my opinion there is no way back from robotic surgery," he said in an interview. "It’s in the destiny of humanity, for the simple reason: to perform more precisely and to overcome our limitations – not only manual limitations, the ability to control movements at a microscopic level, for example – but also diagnostic limitations. The computer and the artificial intelligence of the future will integrate our senses and our mechanical abilities, so we will be able to perform more precisely on selected targets."
Currently, most abdominal procedures performed at the University of Illinois Medical Center are done robotically, including the Whipple procedure, splenectomy, total gastrectomy, lung lobectomy, colorectal surgery, thyroidectomy, adrenalectomy, esophagectomy, major hepatectomies, and common bile duct procedures. The robot "has enormous benefits for the patients," Dr. Giulianotti said. "Open procedures involve a longer postoperative stay and more complications, and it takes more time to enter adjuvant oncological treatment after surgery, and there is less blood loss."
In Dr. Giulianotti’s published experience of 134 robotic-assisted laparoscopic pancreatic surgery procedures, morbidity was 26%, mortality was 2.2%, the conversion rate was 10.4%, and the fistula rate was 20.9%. The majority were grade A fistulas not requiring any treatment (Surg. Endosc. 2010; 24:1646-57). He said that robotic surgery "enables difficult technical maneuvers to be performed that facilitate the success of pancreatic minimally invasive surgery. The results in this series demonstrate feasibility and safety with clinical outcomes."
In a separate study, investigators who compared 32 open vs. 28 laparoscopic vs. 17 robotic distal pancreatectomies found that all three procedures resulted in a similar cost, while the robotic group had a shorter hospital stay, a higher rate of spleen-preserving cases, and an increased operative time, compared with patients in the other two groups (Surgery 2010;148:814-23).
Pelvic indications that are becoming the gold standard for robotic surgery include robotic prostatectomy and resection for rectal cancer. "When you have a very deep and complex surgical field like the pelvis, and you need to do a radical resection for cancer while at the same time sparing nerves that can be important for urinary function, the robot combines three-dimensional vision plus improved functionality of the instruments, allowing for a more precise dissection," Dr. Giulianotti said.
Dr. Leela M. Prasad, chief of the division of colon and rectal surgery at the University of Illinois at Chicago, described robotic-assisted surgery for rectal cancer as "far superior to anything we know right now," especially in overweight males. According to combined results from three published studies, circumferential margin positivity ranged from 0 to 7%, which, Dr. Prasad said, is significantly lower than the average number of positive margins reported following open and laparoscopic rectal surgery procedures (14% and 16%, respectively) (Ann. Surg. Oncol. 2007;14:3168-73; Surg. Oncol. 2009;16:1480-7; Dis. Colon Rectum 2009;52:1824-30).
At the present time, however, in his clinical experience there are no significant differences in outcomes between robotic-assisted and laparoscopically assisted open surgery for colon cancer. "We looked at our data, and it did not make any difference robotically or laparoscopically in terms of length of stay, lymph node harvest, or survival," he said. A recent study from Korean investigators supports those findings (Surg. Endosc. 2012 Dec. 13).
Dr. Giulianotti estimated that there are more than 1,600 robotic surgery systems in the United States. Some of them are devoted to urologic or gynecologic applications, "but in the majority of hospitals there is a growing tendency to use the robot as part of a multidisciplinary program," he said. "That means at the same institution different surgical teams on different days are using the robot for different indications. Of the 1,600 systems out there, I would estimate that about half are used for general surgery."
While hospital administrators have warmed up to the idea of initiating robotic surgery programs at their institutions in recent years, Dr. Giulianotti and Dr. Prasad both called for a culture change in terms of how surgeons and medical educators think about the robot’s place in clinical medicine. "There is a cultural resistance in accepting big changes in surgery," Dr. Giulianotti said. "Academic medical institutions can play a key role here. They need to start teaching robotics in a mandatory way by offering training opportunities in a lab. We also believe that simulation has a big future in this kind of training."
The economic investment required to launch a robotic surgery program is another challenge. "Some hospitals are only concerned about the cost," he said. "When you are doing the same procedure laparoscopically, the cost is probably about 30% less. In the future I hope we can better impact the overall economic aspect of surgical procedures. That means speeding up the postoperative and outpatient treatment of some pathologies. We are already doing Nissen fundoplication and gallbladder removal with robotic surgery, and patients are being discharged a few hours after the surgery."
Dr. Prasad said the field will be poised to further advance when makers of robotic surgery devices and instruments improve on existing technology. "I am using the same robot and instruments as I was using 3 years ago," he said. "I think we need new technologies – including a smaller robot to cut down the costs and speed up the operations. This will make it easier for patients."
To launch a successful robotic surgery program in this day and age, "you need a good team of nurses and surgeons who are dedicated to doing robotic surgery," Dr. Prasad concluded. "It is dangerous in the hands of a surgeon who is not qualified."
Dr. Giulianotti said that he had no relevant financial conflicts to disclose. Dr. Prasad disclosed that he has received honoraria from Intuitive Surgical, Ethicon Endo-Surgery, and Covidien.
The way Dr. Pier Cristoforo Giulianotti sees it, robots will play an increasingly prominent role in the future of surgery. He should know. Dr. Giulianotti, the Lloyd Nyhus Professor of Surgery and chief, division of minimally invasive, general, and robotic surgery at the University of Illinois at Chicago, pioneered robotic lung resection in 2002 and was the first surgeon to perform a robotic Whipple procedure in 2001.
"In my opinion there is no way back from robotic surgery," he said in an interview. "It’s in the destiny of humanity, for the simple reason: to perform more precisely and to overcome our limitations – not only manual limitations, the ability to control movements at a microscopic level, for example – but also diagnostic limitations. The computer and the artificial intelligence of the future will integrate our senses and our mechanical abilities, so we will be able to perform more precisely on selected targets."
Currently, most abdominal procedures performed at the University of Illinois Medical Center are done robotically, including the Whipple procedure, splenectomy, total gastrectomy, lung lobectomy, colorectal surgery, thyroidectomy, adrenalectomy, esophagectomy, major hepatectomies, and common bile duct procedures. The robot "has enormous benefits for the patients," Dr. Giulianotti said. "Open procedures involve a longer postoperative stay and more complications, and it takes more time to enter adjuvant oncological treatment after surgery, and there is less blood loss."
In Dr. Giulianotti’s published experience of 134 robotic-assisted laparoscopic pancreatic surgery procedures, morbidity was 26%, mortality was 2.2%, the conversion rate was 10.4%, and the fistula rate was 20.9%. The majority were grade A fistulas not requiring any treatment (Surg. Endosc. 2010; 24:1646-57). He said that robotic surgery "enables difficult technical maneuvers to be performed that facilitate the success of pancreatic minimally invasive surgery. The results in this series demonstrate feasibility and safety with clinical outcomes."
In a separate study, investigators who compared 32 open vs. 28 laparoscopic vs. 17 robotic distal pancreatectomies found that all three procedures resulted in a similar cost, while the robotic group had a shorter hospital stay, a higher rate of spleen-preserving cases, and an increased operative time, compared with patients in the other two groups (Surgery 2010;148:814-23).
Pelvic indications that are becoming the gold standard for robotic surgery include robotic prostatectomy and resection for rectal cancer. "When you have a very deep and complex surgical field like the pelvis, and you need to do a radical resection for cancer while at the same time sparing nerves that can be important for urinary function, the robot combines three-dimensional vision plus improved functionality of the instruments, allowing for a more precise dissection," Dr. Giulianotti said.
Dr. Leela M. Prasad, chief of the division of colon and rectal surgery at the University of Illinois at Chicago, described robotic-assisted surgery for rectal cancer as "far superior to anything we know right now," especially in overweight males. According to combined results from three published studies, circumferential margin positivity ranged from 0 to 7%, which, Dr. Prasad said, is significantly lower than the average number of positive margins reported following open and laparoscopic rectal surgery procedures (14% and 16%, respectively) (Ann. Surg. Oncol. 2007;14:3168-73; Surg. Oncol. 2009;16:1480-7; Dis. Colon Rectum 2009;52:1824-30).
At the present time, however, in his clinical experience there are no significant differences in outcomes between robotic-assisted and laparoscopically assisted open surgery for colon cancer. "We looked at our data, and it did not make any difference robotically or laparoscopically in terms of length of stay, lymph node harvest, or survival," he said. A recent study from Korean investigators supports those findings (Surg. Endosc. 2012 Dec. 13).
Dr. Giulianotti estimated that there are more than 1,600 robotic surgery systems in the United States. Some of them are devoted to urologic or gynecologic applications, "but in the majority of hospitals there is a growing tendency to use the robot as part of a multidisciplinary program," he said. "That means at the same institution different surgical teams on different days are using the robot for different indications. Of the 1,600 systems out there, I would estimate that about half are used for general surgery."
While hospital administrators have warmed up to the idea of initiating robotic surgery programs at their institutions in recent years, Dr. Giulianotti and Dr. Prasad both called for a culture change in terms of how surgeons and medical educators think about the robot’s place in clinical medicine. "There is a cultural resistance in accepting big changes in surgery," Dr. Giulianotti said. "Academic medical institutions can play a key role here. They need to start teaching robotics in a mandatory way by offering training opportunities in a lab. We also believe that simulation has a big future in this kind of training."
The economic investment required to launch a robotic surgery program is another challenge. "Some hospitals are only concerned about the cost," he said. "When you are doing the same procedure laparoscopically, the cost is probably about 30% less. In the future I hope we can better impact the overall economic aspect of surgical procedures. That means speeding up the postoperative and outpatient treatment of some pathologies. We are already doing Nissen fundoplication and gallbladder removal with robotic surgery, and patients are being discharged a few hours after the surgery."
Dr. Prasad said the field will be poised to further advance when makers of robotic surgery devices and instruments improve on existing technology. "I am using the same robot and instruments as I was using 3 years ago," he said. "I think we need new technologies – including a smaller robot to cut down the costs and speed up the operations. This will make it easier for patients."
To launch a successful robotic surgery program in this day and age, "you need a good team of nurses and surgeons who are dedicated to doing robotic surgery," Dr. Prasad concluded. "It is dangerous in the hands of a surgeon who is not qualified."
Dr. Giulianotti said that he had no relevant financial conflicts to disclose. Dr. Prasad disclosed that he has received honoraria from Intuitive Surgical, Ethicon Endo-Surgery, and Covidien.