User login
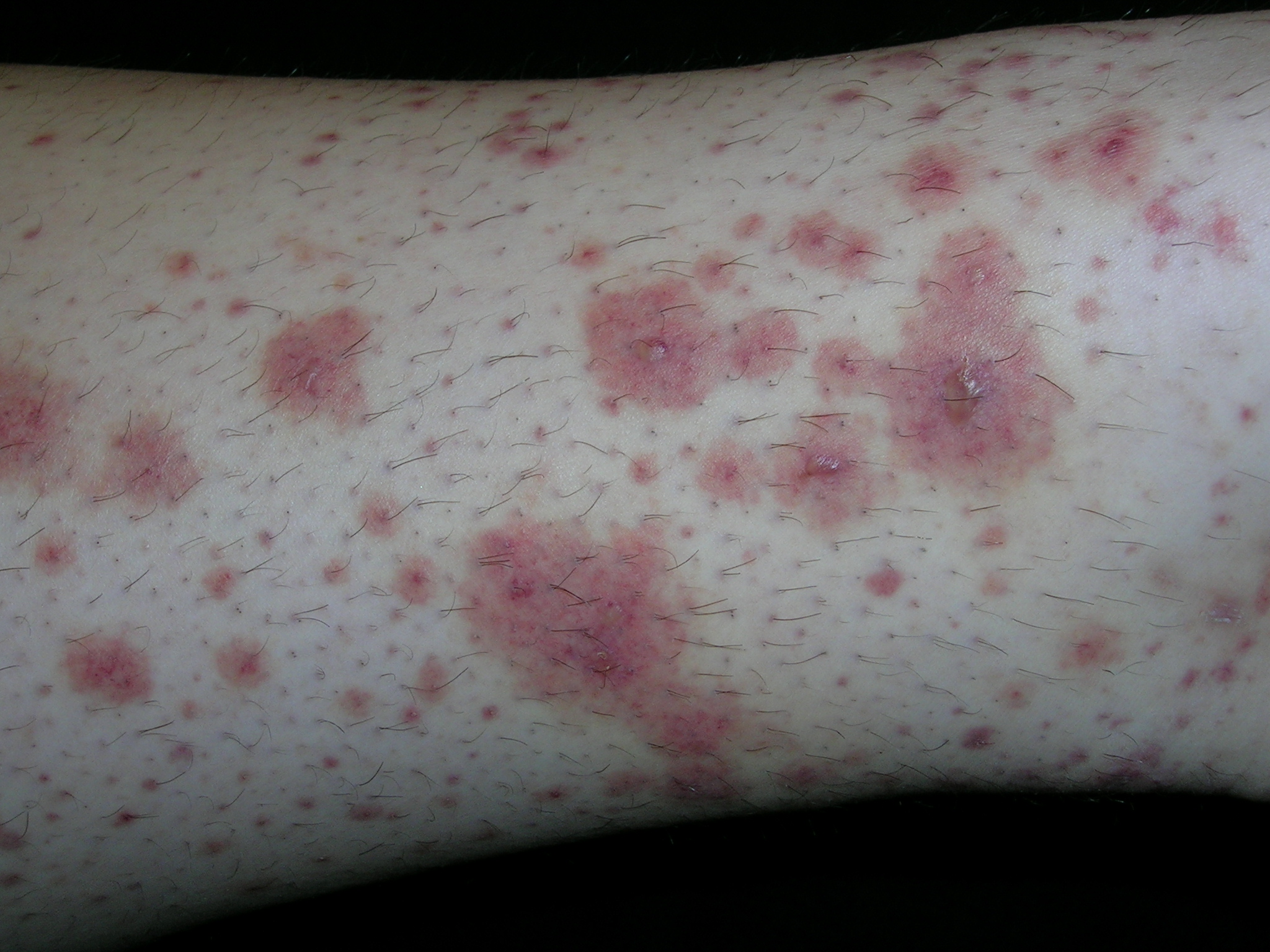
The typical palpable purpura on the legs is consistent with Henoch–Schönlein purpura. HSP occurs mainly in children and results from IgA-containing immune complexes in blood vessel walls in the skin, kidney, and gastrointestinal tract. HSP is usually benign and self-limiting. A streptococcal or viral upper respiratory infection often precedes the disease by 1 to 3 weeks. Prodromal symptoms include anorexia and fever. In half of the cases, there are recurrences, typically in the first 3 months. Recurrences are more common in patients with nephritis and are milder than the original episode.
The clinical features of HSP include nonthrombocytopenic palpable purpura mainly on the lower extremities and buttocks, gastrointestinal symptoms, arthralgia, and nephritis. Visceral involvement (with, say, the kidneys and lungs) most commonly occurs in vasculitis associated with HSP, cryoglobulinemia, or systemic lupus erythematosus.
In HSP, treatment with nonsteroidal anti-inflammatory drugs is usually preferred. Treatment with corticosteroids may be of more benefit in patients with more severe disease such as more pronounced abdominal pain and renal involvement. Oral prednisone is used to treat visceral involvement and more severe cases of vasculitis of the skin. Short courses of prednisone (60–80 mg/d) are effective and should be tapered slowly.
This patient had some hematuria but her creatinine was normal. She was started on ibuprofen with some relief of her skin pain. By the following week, her hematuria was resolved but her skin was not improving. The risks and benefits of prednisone were discussed and the patient decided to take the prednisone. Even on the steroids, the painful rash took 3 to 4 weeks to resolve. Ultimately, it did resolve with no scarring and no sequelae.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ, Usatine R. Cutaneous vasculitis. In: Usatine R, Smith M, Mayeaux EJ, et al., eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:760-765.
To learn more about The Color Atlas of Family Medicine, see:
* http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
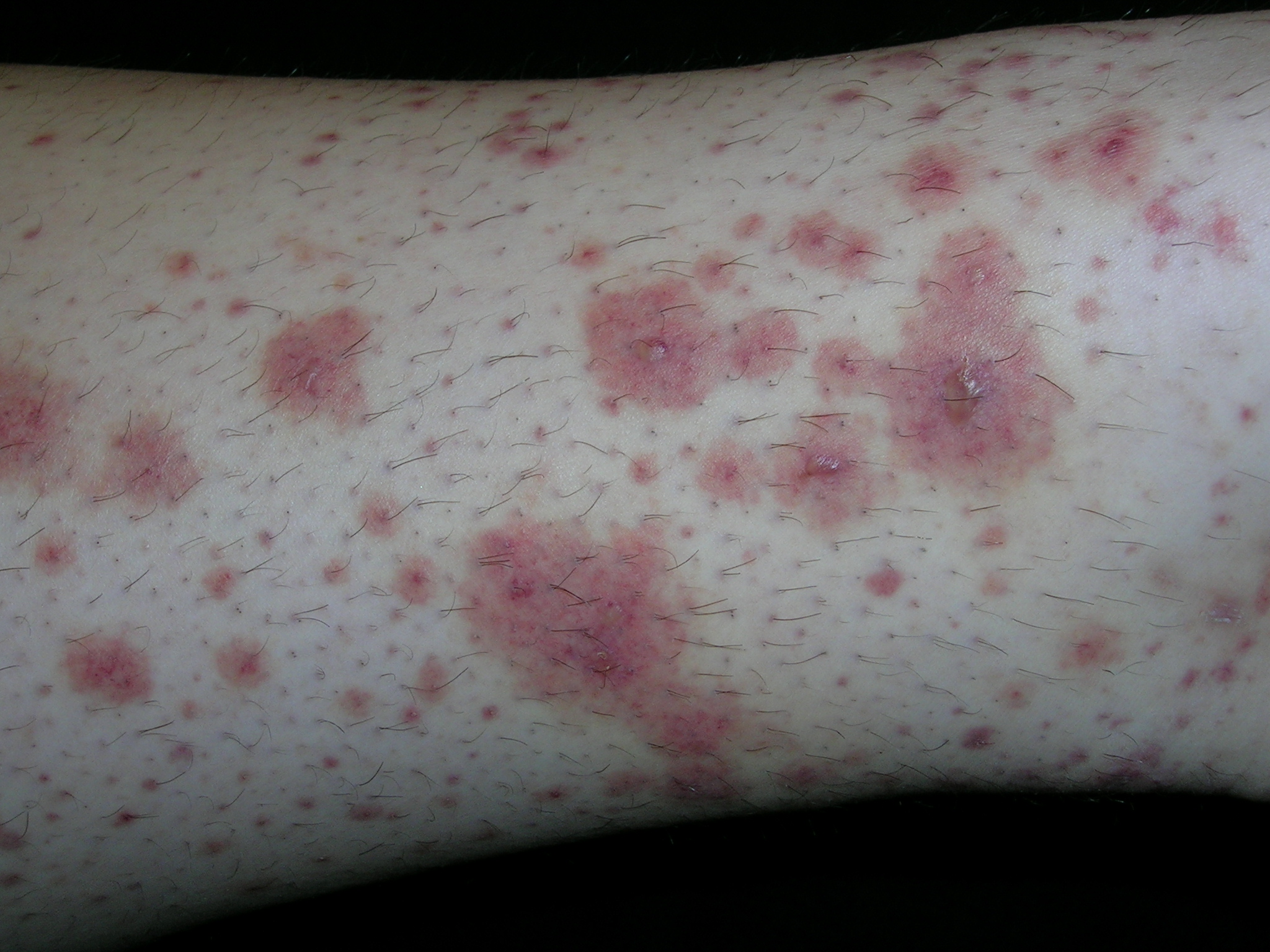
The typical palpable purpura on the legs is consistent with Henoch–Schönlein purpura. HSP occurs mainly in children and results from IgA-containing immune complexes in blood vessel walls in the skin, kidney, and gastrointestinal tract. HSP is usually benign and self-limiting. A streptococcal or viral upper respiratory infection often precedes the disease by 1 to 3 weeks. Prodromal symptoms include anorexia and fever. In half of the cases, there are recurrences, typically in the first 3 months. Recurrences are more common in patients with nephritis and are milder than the original episode.
The clinical features of HSP include nonthrombocytopenic palpable purpura mainly on the lower extremities and buttocks, gastrointestinal symptoms, arthralgia, and nephritis. Visceral involvement (with, say, the kidneys and lungs) most commonly occurs in vasculitis associated with HSP, cryoglobulinemia, or systemic lupus erythematosus.
In HSP, treatment with nonsteroidal anti-inflammatory drugs is usually preferred. Treatment with corticosteroids may be of more benefit in patients with more severe disease such as more pronounced abdominal pain and renal involvement. Oral prednisone is used to treat visceral involvement and more severe cases of vasculitis of the skin. Short courses of prednisone (60–80 mg/d) are effective and should be tapered slowly.
This patient had some hematuria but her creatinine was normal. She was started on ibuprofen with some relief of her skin pain. By the following week, her hematuria was resolved but her skin was not improving. The risks and benefits of prednisone were discussed and the patient decided to take the prednisone. Even on the steroids, the painful rash took 3 to 4 weeks to resolve. Ultimately, it did resolve with no scarring and no sequelae.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ, Usatine R. Cutaneous vasculitis. In: Usatine R, Smith M, Mayeaux EJ, et al., eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:760-765.
To learn more about The Color Atlas of Family Medicine, see:
* http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
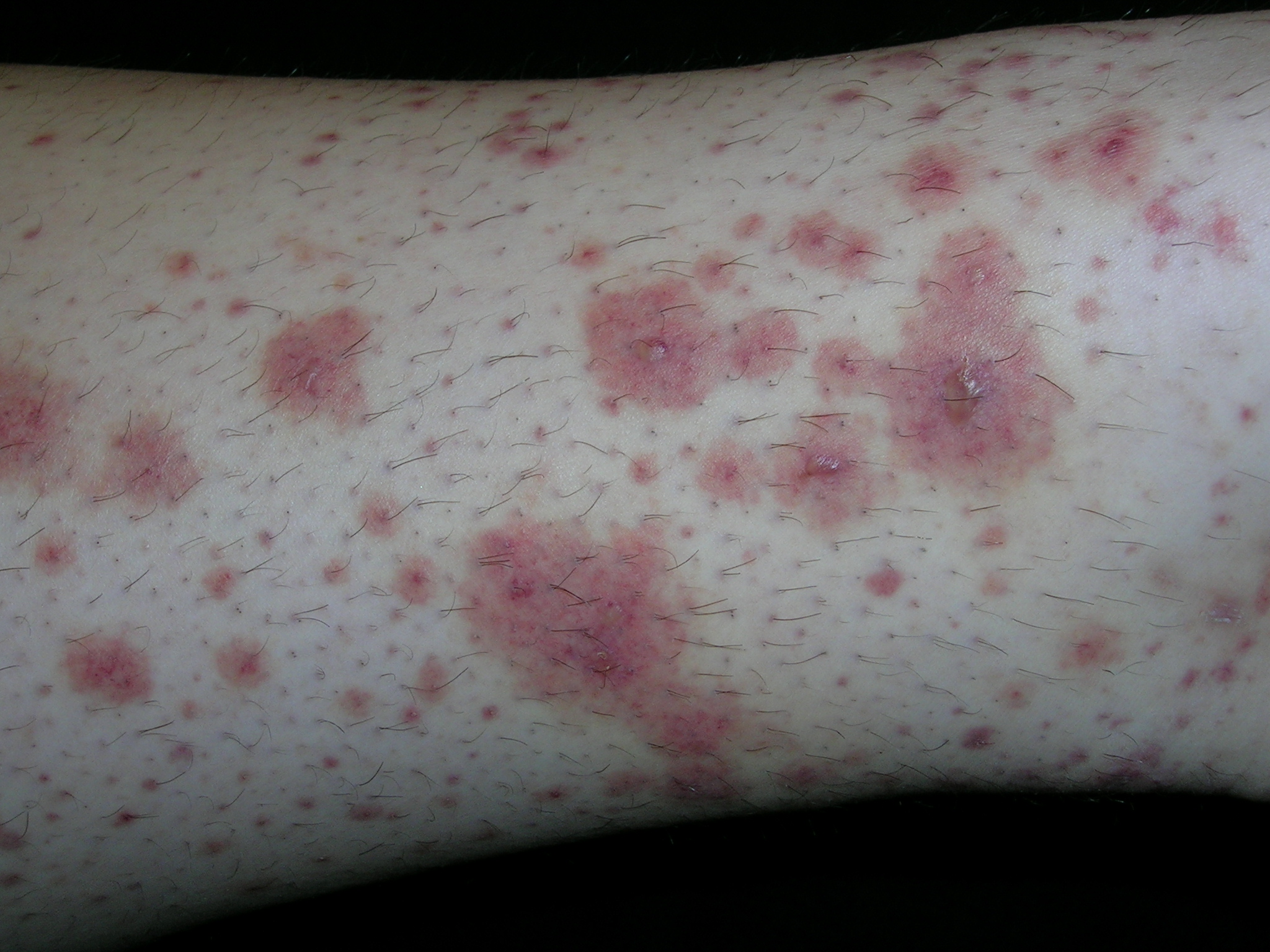
The typical palpable purpura on the legs is consistent with Henoch–Schönlein purpura. HSP occurs mainly in children and results from IgA-containing immune complexes in blood vessel walls in the skin, kidney, and gastrointestinal tract. HSP is usually benign and self-limiting. A streptococcal or viral upper respiratory infection often precedes the disease by 1 to 3 weeks. Prodromal symptoms include anorexia and fever. In half of the cases, there are recurrences, typically in the first 3 months. Recurrences are more common in patients with nephritis and are milder than the original episode.
The clinical features of HSP include nonthrombocytopenic palpable purpura mainly on the lower extremities and buttocks, gastrointestinal symptoms, arthralgia, and nephritis. Visceral involvement (with, say, the kidneys and lungs) most commonly occurs in vasculitis associated with HSP, cryoglobulinemia, or systemic lupus erythematosus.
In HSP, treatment with nonsteroidal anti-inflammatory drugs is usually preferred. Treatment with corticosteroids may be of more benefit in patients with more severe disease such as more pronounced abdominal pain and renal involvement. Oral prednisone is used to treat visceral involvement and more severe cases of vasculitis of the skin. Short courses of prednisone (60–80 mg/d) are effective and should be tapered slowly.
This patient had some hematuria but her creatinine was normal. She was started on ibuprofen with some relief of her skin pain. By the following week, her hematuria was resolved but her skin was not improving. The risks and benefits of prednisone were discussed and the patient decided to take the prednisone. Even on the steroids, the painful rash took 3 to 4 weeks to resolve. Ultimately, it did resolve with no scarring and no sequelae.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ, Usatine R. Cutaneous vasculitis. In: Usatine R, Smith M, Mayeaux EJ, et al., eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:760-765.
To learn more about The Color Atlas of Family Medicine, see:
* http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641