User login
CASE: Unusual suicide attempt
After a friend calls 911, Ms. M, age 20, is brought to an emergency room (ER) complaining of severe leg and abdominal pain. The ER physician finds she is bleeding from her vagina and nose and has severe ecchymosis anemia. After Ms. M is admitted, clinicians discover these conditions are secondary to a suicide attempt—she ingested 15 to 16 pellets of rat poison daily for approximately 2 months.
While hospitalized, Ms. M is treated with several transfusions of fresh frozen plasma, packed red blood cells, and phytonadione (vitamin K). A consultation-liaison psychiatrist diagnoses bipolar disorder and starts Ms. M on lamotrigine, 25 mg once daily. (The justification for this diagnosis was not documented.) After physicians judge her to be medically stable, Ms. M is involuntarily committed to a short-term psychiatric care facility. Her vital signs and coagulation values are stable.
At the psychiatric facility, our team determines that her symptoms and history are consistent with major depressive disorder, recurrent. For 5 months, Ms. M had depressed mood for most of the day, diminished interest in activities, and feelings of worthlessness. She also experienced weight loss—10 lbs in 2 months—with decreased appetite and low energy for most of the day. She denies past symptoms of mania or psychosis. She says she does not know why she was diagnosed with bipolar disorder. She admits to multiple previous suicide attempts via hanging and ingesting cleaning fluid or rat poison.
We place Ms. M on suicide precautions and prescribe escitalopram, 10 mg/d, in addition to lamotrigine, 50 mg once daily. We continue lamotrigine despite a lack of documentation for Ms. M’s bipolar diagnosis because evidence suggests the drug may be an effective augmentation to antidepressants in patients with treatment-resistant depression.1
The author’s observations
Any patient transferred from a medical floor to a psychiatric inpatient unit should have documentation that clarifies any need for further medical treatment. Ms. M’s physicians told us that she was medically stable and should require little if any further treatment for her ingestion of rat poison.
TREATMENT: Coagulation concerns
We request a medical consult to monitor possible complications from the rat poison. The physician advises that rat poison essentially is the same as the anticoagulant warfarin and its effects should steadily decrease over time because its half-life is 20 to 60 hours. However, for safety reasons, we closely follow Ms. M’s coagulation values and order daily vitamin K injections, 5 mg SC.
Further medical investigation shows no evidence of complications, but Ms. M continues to request medication for pain in her left leg. The physician prescribes acetaminophen, 650 mg every 6 hours as needed for pain, which the patient takes at almost every opportunity, often 4 times a day. The physician does not choose a nonsteroidal anti-inflammatory drug (NSAID) for pain to avoid the possibility of gastrointestinal (GI) irritation that could lead to bleeding.
In the psychiatric facility, the patient’s international normalized ratio (INR) is found to be rising, indicating a lack of clotting and a risk of uncontrolled bleeding. The physician states that given the half-life of warfarin, Ms. M’s INR should be decreasing. Liver function testing does not show that liver dysfunction is contributing to the increasing INR.
Because we assume the vitamin K the patient received has been absorbed, we hypothesize that Ms. M has continued to surreptitiously ingest rat poison or another anticoagulant, which she denies. We search Ms. M and her room. She is placed on 1-to-1 observation 24 hours a day. Ms. M’s visitors also are searched, and visits are observed. We find no evidence of an anticoagulant agent.
Ms. M’s INR continues to rise. We search the facility to rule out the possibility that the patient had hidden a supply of anticoagulant outside her room. The search finds nothing. At this point we consider performing an abdominal x-ray to rule out the possibility that Ms. M may have a supply of medication hidden in her gastrointestinal tract.
The author’s observations
Patients hiding and using contraband is a common problem in involuntary inpatient units. It seemed that Ms. M was secretly ingesting rat poison. Her history showed she was determined to end her life, and she ingested rat poison daily for months. However, because an exhaustive search for contraband and 1-to-1 observation yielded no positive results, the evidence did not support this theory. Some team members thought we were not searching hard enough. I decided we needed to pursue other theories.
I was skeptical that escitalopram could be contributing to Ms. M’s rising anticoagulation values. Selective serotonin reuptake inhibitors have antiplatelet effects, but platelet function does not affect INR to the degree we were observing.
‘Superwarfarins’
Physicians had advised us that Ms. M’s INR should decrease under the assumption that rat poison is for all practical purposes the same as warfarin, but we had not investigated distinctions between the 2 compounds. A literature search revealed that several rat poisons are not simply warfarin repackaged as a pesticide. Most are “superwarfarins”—chemicals similar to warfarin but more potent and with a much longer half-life.2 Case report data suggest the plasma half-life of these chemicals is 20 to 62 days.3
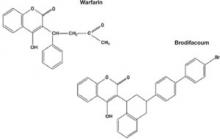
Most commercial rat poisons are made of brodifacoum, which has a chemical structure similar to warfarin but with an additional long polycyclic hydrocarbon side chain (Figure 1). The potency of brodifacoum compared with warfarin is approximately 100 to 1.4-6 The chemical is highly lipophilic and can stay in the body for an extended period.4-6 Lab tests can measure serum brodifacoum levels.3
After Ms. M identifies the brand name of the rat poison she ingested, we contact the American Association of Poison Control Centers and verify the agent she used was brodifacoum. This explains why her INR was not decreasing—but does not explain the increase.
A drug interaction? Because Ms. M’s liver function is within normal limits, the next theory to investigate is if brodifacoum is interacting with any medications she is taking. I could not find any medical journal articles, programs, or Web sites describing brodifacoum’s interactions with medications. After all, brodifacoum is a pesticide, not a medication.
I considered that because brodifacoum and warfarin have a similar structure and function, they may interact with medications in a similar manner. After another literature search, only acetaminophen had evidence of interaction with warfarin that could explain her rising INR.
Documentation of interactions between warfarin and acetaminophen are sparse. In one case, a 74-year-old man receiving warfarin for atrial fibrillation experienced an abrupt increase in INR after taking acetaminophen.7 In a double-blind, placebo controlled, randomized trial of patients taking warfarin, INR rose rapidly after the start of acetaminophen and was significantly increased within 1 week compared with patients receiving placebo.8
Figure 1 Chemical structures of warfarin and rat poison
Most commercial rat poisons are made of brodifacoum, which is chemically similar to warfarin but has an additional long polycyclic hydrocarbon side chain.
FOLLOW-UP: Analgesic substitution
We suggest to the physician that Ms. M’s INR may be increasing because of an interaction between brodifacoum and acetaminophen, which she took several times a day. On day 8 of Ms. M’s hospitalization, the physician discontinues acetaminophen and prescribes ibuprofen, 400 mg tid as needed for pain, and pantoprazole, 40 mg/d, to prevent GI bleeding from possible irritation caused by ibuprofen. The team continues to monitor Ms. M’s coagulation values.
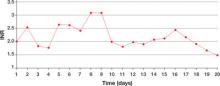
Within a day of discontinuing acetaminophen, Ms. M’s INR decreased as expected (Figure 2). The rest of her medication regimen is continued, and her INR levels continued to decrease.
One-to-one observation is discontinued. However, because of the patient’s continued determination to end her life and no significant improvement in her depression, Ms. M is considered a danger to herself and involuntary inpatient hospitalization is continued.
Figure 2 Ms. M’s INR values during hospitalization
The patient’s INR values began to rise mysteriously after she was transferred to the inpatient psychiatric unit. Acetaminophen was discontinued on day 8, and within a day her INR values began to drop.
INR: International normalized ratio
The author’s observations
Poisoning is a common method of attempting suicide, patients may use substances that clinicians rarely encounter. For most toxic, nonmedication substances, data on interactions with medications are sparse. if you suspect your patient has ingested a toxic substance with which the treatment team has little experience, contact the American Association of Poison Control Centers at 800-222-1222.
Suspect superwarfarin poisoning in suicidal patients with coagulopathy, prolonged prothrombin time, and elevated INR that does not respond to large amounts of vitamin K.9,10 These patients are at high risk of successfully completing suicide because of superwarfarins’ long half-life and daily maintenance required to keep coagulation levels within a safe range for at least several weeks.
The most serious complication these patients face is intracranial hemorrhage, which occurs in 2% of patients with excessive warfarin-based coagulation and is associated with a 77% mortality rate.11 GI bleeding occurs in 67% of these patients.2
Also take into account medical conditions—such as hypertension or hepatic disease—and medication side effects that can increase bleeding risk. When treating pain in these patients, consider avoiding acetaminophen but be aware of the risks of NSAIDs, such as gastritis or GI bleeding.
Related resource
- The American Association of Poison Control Centers. 800-222-1222; www.aapcc.org.
Drug brand names
- Escitalopram • Lexapro
- Lamotrigine • Lamictal
- Pantoprazole • Protonix
- Warfarin • Coumadin
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sharma V, Khan M, Corpse C. Role of lamotrigine in the management of treatment-resistant bipolar II depression: a chart review. J Affect Disord Epub 2008 Mar 1.
2. Su M, Hoffman R. Anticoagulants. In: Flomenbaum NE, Goldfrank LR, Hoffman RS, et al, eds. Goldfrank’s toxicologic emergencies. 8th ed. New York, NY: McGraw-Hill Medical Publishing; 2006:891-4.
3. Chua JD, Friedenberg WR. Superwarfarin poisoning. Anaesth Intensive Care 1997;25:707-9.
4. Leck JB, Park BK. A comparative study of the effect of warfarin and brodifacoum on the relationship between vitamin K1 metabolism and clotting factor activity in warfarin susceptible and warfarin resistant rats. Biochem Pharmacol 1981;30:123-9.
5. Lund M. Comparative effect of the three rodenticides warfarin, difenacoum and brodifacoum on eight rodent species in short feeding periods. J Hyg 1981;87:101-7.
6. Park BK, Scott AK, Wilson AC, et al. Plasma disposition of vitamin K antagonism by warfarin, difenacoum and brodifacoum in the rabbit. Biochem Pharmacol 1982;31:3535-639.
7. Gebauer MG, Nyfort-Hansen K, Henschke PJ, Gallus AS. Warfarin and acetaminophen interaction. Pharmacotherapy 2003;23(1):109-12.
8. Mahe I, Bertrand N, Drouet L, et al. Interaction between paracetamol and warfarin in patients: a double-blind, placebo-controlled, randomized study. Haematologica 2006;91(12):1621-7.
9. Sharma P, Bentley P. Of rats and men: superwarfarin toxicity. Lancet 2005;365:552-3.
10. Scully M. Warfarin therapy: rat poison and the prevention of thrombosis. Biochemist 2002;24:15-7.
11. Mathiesen T, Benediktsdottir K, Johnsson H, Lindqvist M. Intracranial traumatic and nontraumatic haemorrhagic complications of warfarin treatment. Acta Neurol Scan 1995;91:208-14.
CASE: Unusual suicide attempt
After a friend calls 911, Ms. M, age 20, is brought to an emergency room (ER) complaining of severe leg and abdominal pain. The ER physician finds she is bleeding from her vagina and nose and has severe ecchymosis anemia. After Ms. M is admitted, clinicians discover these conditions are secondary to a suicide attempt—she ingested 15 to 16 pellets of rat poison daily for approximately 2 months.
While hospitalized, Ms. M is treated with several transfusions of fresh frozen plasma, packed red blood cells, and phytonadione (vitamin K). A consultation-liaison psychiatrist diagnoses bipolar disorder and starts Ms. M on lamotrigine, 25 mg once daily. (The justification for this diagnosis was not documented.) After physicians judge her to be medically stable, Ms. M is involuntarily committed to a short-term psychiatric care facility. Her vital signs and coagulation values are stable.
At the psychiatric facility, our team determines that her symptoms and history are consistent with major depressive disorder, recurrent. For 5 months, Ms. M had depressed mood for most of the day, diminished interest in activities, and feelings of worthlessness. She also experienced weight loss—10 lbs in 2 months—with decreased appetite and low energy for most of the day. She denies past symptoms of mania or psychosis. She says she does not know why she was diagnosed with bipolar disorder. She admits to multiple previous suicide attempts via hanging and ingesting cleaning fluid or rat poison.
We place Ms. M on suicide precautions and prescribe escitalopram, 10 mg/d, in addition to lamotrigine, 50 mg once daily. We continue lamotrigine despite a lack of documentation for Ms. M’s bipolar diagnosis because evidence suggests the drug may be an effective augmentation to antidepressants in patients with treatment-resistant depression.1
The author’s observations
Any patient transferred from a medical floor to a psychiatric inpatient unit should have documentation that clarifies any need for further medical treatment. Ms. M’s physicians told us that she was medically stable and should require little if any further treatment for her ingestion of rat poison.
TREATMENT: Coagulation concerns
We request a medical consult to monitor possible complications from the rat poison. The physician advises that rat poison essentially is the same as the anticoagulant warfarin and its effects should steadily decrease over time because its half-life is 20 to 60 hours. However, for safety reasons, we closely follow Ms. M’s coagulation values and order daily vitamin K injections, 5 mg SC.
Further medical investigation shows no evidence of complications, but Ms. M continues to request medication for pain in her left leg. The physician prescribes acetaminophen, 650 mg every 6 hours as needed for pain, which the patient takes at almost every opportunity, often 4 times a day. The physician does not choose a nonsteroidal anti-inflammatory drug (NSAID) for pain to avoid the possibility of gastrointestinal (GI) irritation that could lead to bleeding.
In the psychiatric facility, the patient’s international normalized ratio (INR) is found to be rising, indicating a lack of clotting and a risk of uncontrolled bleeding. The physician states that given the half-life of warfarin, Ms. M’s INR should be decreasing. Liver function testing does not show that liver dysfunction is contributing to the increasing INR.
Because we assume the vitamin K the patient received has been absorbed, we hypothesize that Ms. M has continued to surreptitiously ingest rat poison or another anticoagulant, which she denies. We search Ms. M and her room. She is placed on 1-to-1 observation 24 hours a day. Ms. M’s visitors also are searched, and visits are observed. We find no evidence of an anticoagulant agent.
Ms. M’s INR continues to rise. We search the facility to rule out the possibility that the patient had hidden a supply of anticoagulant outside her room. The search finds nothing. At this point we consider performing an abdominal x-ray to rule out the possibility that Ms. M may have a supply of medication hidden in her gastrointestinal tract.
The author’s observations
Patients hiding and using contraband is a common problem in involuntary inpatient units. It seemed that Ms. M was secretly ingesting rat poison. Her history showed she was determined to end her life, and she ingested rat poison daily for months. However, because an exhaustive search for contraband and 1-to-1 observation yielded no positive results, the evidence did not support this theory. Some team members thought we were not searching hard enough. I decided we needed to pursue other theories.
I was skeptical that escitalopram could be contributing to Ms. M’s rising anticoagulation values. Selective serotonin reuptake inhibitors have antiplatelet effects, but platelet function does not affect INR to the degree we were observing.
‘Superwarfarins’
Physicians had advised us that Ms. M’s INR should decrease under the assumption that rat poison is for all practical purposes the same as warfarin, but we had not investigated distinctions between the 2 compounds. A literature search revealed that several rat poisons are not simply warfarin repackaged as a pesticide. Most are “superwarfarins”—chemicals similar to warfarin but more potent and with a much longer half-life.2 Case report data suggest the plasma half-life of these chemicals is 20 to 62 days.3
Most commercial rat poisons are made of brodifacoum, which has a chemical structure similar to warfarin but with an additional long polycyclic hydrocarbon side chain (Figure 1). The potency of brodifacoum compared with warfarin is approximately 100 to 1.4-6 The chemical is highly lipophilic and can stay in the body for an extended period.4-6 Lab tests can measure serum brodifacoum levels.3
After Ms. M identifies the brand name of the rat poison she ingested, we contact the American Association of Poison Control Centers and verify the agent she used was brodifacoum. This explains why her INR was not decreasing—but does not explain the increase.
A drug interaction? Because Ms. M’s liver function is within normal limits, the next theory to investigate is if brodifacoum is interacting with any medications she is taking. I could not find any medical journal articles, programs, or Web sites describing brodifacoum’s interactions with medications. After all, brodifacoum is a pesticide, not a medication.
I considered that because brodifacoum and warfarin have a similar structure and function, they may interact with medications in a similar manner. After another literature search, only acetaminophen had evidence of interaction with warfarin that could explain her rising INR.
Documentation of interactions between warfarin and acetaminophen are sparse. In one case, a 74-year-old man receiving warfarin for atrial fibrillation experienced an abrupt increase in INR after taking acetaminophen.7 In a double-blind, placebo controlled, randomized trial of patients taking warfarin, INR rose rapidly after the start of acetaminophen and was significantly increased within 1 week compared with patients receiving placebo.8
Figure 1 Chemical structures of warfarin and rat poison
Most commercial rat poisons are made of brodifacoum, which is chemically similar to warfarin but has an additional long polycyclic hydrocarbon side chain.
FOLLOW-UP: Analgesic substitution
We suggest to the physician that Ms. M’s INR may be increasing because of an interaction between brodifacoum and acetaminophen, which she took several times a day. On day 8 of Ms. M’s hospitalization, the physician discontinues acetaminophen and prescribes ibuprofen, 400 mg tid as needed for pain, and pantoprazole, 40 mg/d, to prevent GI bleeding from possible irritation caused by ibuprofen. The team continues to monitor Ms. M’s coagulation values.
Within a day of discontinuing acetaminophen, Ms. M’s INR decreased as expected (Figure 2). The rest of her medication regimen is continued, and her INR levels continued to decrease.
One-to-one observation is discontinued. However, because of the patient’s continued determination to end her life and no significant improvement in her depression, Ms. M is considered a danger to herself and involuntary inpatient hospitalization is continued.
Figure 2 Ms. M’s INR values during hospitalization
The patient’s INR values began to rise mysteriously after she was transferred to the inpatient psychiatric unit. Acetaminophen was discontinued on day 8, and within a day her INR values began to drop.
INR: International normalized ratio
The author’s observations
Poisoning is a common method of attempting suicide, patients may use substances that clinicians rarely encounter. For most toxic, nonmedication substances, data on interactions with medications are sparse. if you suspect your patient has ingested a toxic substance with which the treatment team has little experience, contact the American Association of Poison Control Centers at 800-222-1222.
Suspect superwarfarin poisoning in suicidal patients with coagulopathy, prolonged prothrombin time, and elevated INR that does not respond to large amounts of vitamin K.9,10 These patients are at high risk of successfully completing suicide because of superwarfarins’ long half-life and daily maintenance required to keep coagulation levels within a safe range for at least several weeks.
The most serious complication these patients face is intracranial hemorrhage, which occurs in 2% of patients with excessive warfarin-based coagulation and is associated with a 77% mortality rate.11 GI bleeding occurs in 67% of these patients.2
Also take into account medical conditions—such as hypertension or hepatic disease—and medication side effects that can increase bleeding risk. When treating pain in these patients, consider avoiding acetaminophen but be aware of the risks of NSAIDs, such as gastritis or GI bleeding.
Related resource
- The American Association of Poison Control Centers. 800-222-1222; www.aapcc.org.
Drug brand names
- Escitalopram • Lexapro
- Lamotrigine • Lamictal
- Pantoprazole • Protonix
- Warfarin • Coumadin
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Unusual suicide attempt
After a friend calls 911, Ms. M, age 20, is brought to an emergency room (ER) complaining of severe leg and abdominal pain. The ER physician finds she is bleeding from her vagina and nose and has severe ecchymosis anemia. After Ms. M is admitted, clinicians discover these conditions are secondary to a suicide attempt—she ingested 15 to 16 pellets of rat poison daily for approximately 2 months.
While hospitalized, Ms. M is treated with several transfusions of fresh frozen plasma, packed red blood cells, and phytonadione (vitamin K). A consultation-liaison psychiatrist diagnoses bipolar disorder and starts Ms. M on lamotrigine, 25 mg once daily. (The justification for this diagnosis was not documented.) After physicians judge her to be medically stable, Ms. M is involuntarily committed to a short-term psychiatric care facility. Her vital signs and coagulation values are stable.
At the psychiatric facility, our team determines that her symptoms and history are consistent with major depressive disorder, recurrent. For 5 months, Ms. M had depressed mood for most of the day, diminished interest in activities, and feelings of worthlessness. She also experienced weight loss—10 lbs in 2 months—with decreased appetite and low energy for most of the day. She denies past symptoms of mania or psychosis. She says she does not know why she was diagnosed with bipolar disorder. She admits to multiple previous suicide attempts via hanging and ingesting cleaning fluid or rat poison.
We place Ms. M on suicide precautions and prescribe escitalopram, 10 mg/d, in addition to lamotrigine, 50 mg once daily. We continue lamotrigine despite a lack of documentation for Ms. M’s bipolar diagnosis because evidence suggests the drug may be an effective augmentation to antidepressants in patients with treatment-resistant depression.1
The author’s observations
Any patient transferred from a medical floor to a psychiatric inpatient unit should have documentation that clarifies any need for further medical treatment. Ms. M’s physicians told us that she was medically stable and should require little if any further treatment for her ingestion of rat poison.
TREATMENT: Coagulation concerns
We request a medical consult to monitor possible complications from the rat poison. The physician advises that rat poison essentially is the same as the anticoagulant warfarin and its effects should steadily decrease over time because its half-life is 20 to 60 hours. However, for safety reasons, we closely follow Ms. M’s coagulation values and order daily vitamin K injections, 5 mg SC.
Further medical investigation shows no evidence of complications, but Ms. M continues to request medication for pain in her left leg. The physician prescribes acetaminophen, 650 mg every 6 hours as needed for pain, which the patient takes at almost every opportunity, often 4 times a day. The physician does not choose a nonsteroidal anti-inflammatory drug (NSAID) for pain to avoid the possibility of gastrointestinal (GI) irritation that could lead to bleeding.
In the psychiatric facility, the patient’s international normalized ratio (INR) is found to be rising, indicating a lack of clotting and a risk of uncontrolled bleeding. The physician states that given the half-life of warfarin, Ms. M’s INR should be decreasing. Liver function testing does not show that liver dysfunction is contributing to the increasing INR.
Because we assume the vitamin K the patient received has been absorbed, we hypothesize that Ms. M has continued to surreptitiously ingest rat poison or another anticoagulant, which she denies. We search Ms. M and her room. She is placed on 1-to-1 observation 24 hours a day. Ms. M’s visitors also are searched, and visits are observed. We find no evidence of an anticoagulant agent.
Ms. M’s INR continues to rise. We search the facility to rule out the possibility that the patient had hidden a supply of anticoagulant outside her room. The search finds nothing. At this point we consider performing an abdominal x-ray to rule out the possibility that Ms. M may have a supply of medication hidden in her gastrointestinal tract.
The author’s observations
Patients hiding and using contraband is a common problem in involuntary inpatient units. It seemed that Ms. M was secretly ingesting rat poison. Her history showed she was determined to end her life, and she ingested rat poison daily for months. However, because an exhaustive search for contraband and 1-to-1 observation yielded no positive results, the evidence did not support this theory. Some team members thought we were not searching hard enough. I decided we needed to pursue other theories.
I was skeptical that escitalopram could be contributing to Ms. M’s rising anticoagulation values. Selective serotonin reuptake inhibitors have antiplatelet effects, but platelet function does not affect INR to the degree we were observing.
‘Superwarfarins’
Physicians had advised us that Ms. M’s INR should decrease under the assumption that rat poison is for all practical purposes the same as warfarin, but we had not investigated distinctions between the 2 compounds. A literature search revealed that several rat poisons are not simply warfarin repackaged as a pesticide. Most are “superwarfarins”—chemicals similar to warfarin but more potent and with a much longer half-life.2 Case report data suggest the plasma half-life of these chemicals is 20 to 62 days.3
Most commercial rat poisons are made of brodifacoum, which has a chemical structure similar to warfarin but with an additional long polycyclic hydrocarbon side chain (Figure 1). The potency of brodifacoum compared with warfarin is approximately 100 to 1.4-6 The chemical is highly lipophilic and can stay in the body for an extended period.4-6 Lab tests can measure serum brodifacoum levels.3
After Ms. M identifies the brand name of the rat poison she ingested, we contact the American Association of Poison Control Centers and verify the agent she used was brodifacoum. This explains why her INR was not decreasing—but does not explain the increase.
A drug interaction? Because Ms. M’s liver function is within normal limits, the next theory to investigate is if brodifacoum is interacting with any medications she is taking. I could not find any medical journal articles, programs, or Web sites describing brodifacoum’s interactions with medications. After all, brodifacoum is a pesticide, not a medication.
I considered that because brodifacoum and warfarin have a similar structure and function, they may interact with medications in a similar manner. After another literature search, only acetaminophen had evidence of interaction with warfarin that could explain her rising INR.
Documentation of interactions between warfarin and acetaminophen are sparse. In one case, a 74-year-old man receiving warfarin for atrial fibrillation experienced an abrupt increase in INR after taking acetaminophen.7 In a double-blind, placebo controlled, randomized trial of patients taking warfarin, INR rose rapidly after the start of acetaminophen and was significantly increased within 1 week compared with patients receiving placebo.8
Figure 1 Chemical structures of warfarin and rat poison
Most commercial rat poisons are made of brodifacoum, which is chemically similar to warfarin but has an additional long polycyclic hydrocarbon side chain.
FOLLOW-UP: Analgesic substitution
We suggest to the physician that Ms. M’s INR may be increasing because of an interaction between brodifacoum and acetaminophen, which she took several times a day. On day 8 of Ms. M’s hospitalization, the physician discontinues acetaminophen and prescribes ibuprofen, 400 mg tid as needed for pain, and pantoprazole, 40 mg/d, to prevent GI bleeding from possible irritation caused by ibuprofen. The team continues to monitor Ms. M’s coagulation values.
Within a day of discontinuing acetaminophen, Ms. M’s INR decreased as expected (Figure 2). The rest of her medication regimen is continued, and her INR levels continued to decrease.
One-to-one observation is discontinued. However, because of the patient’s continued determination to end her life and no significant improvement in her depression, Ms. M is considered a danger to herself and involuntary inpatient hospitalization is continued.
Figure 2 Ms. M’s INR values during hospitalization
The patient’s INR values began to rise mysteriously after she was transferred to the inpatient psychiatric unit. Acetaminophen was discontinued on day 8, and within a day her INR values began to drop.
INR: International normalized ratio
The author’s observations
Poisoning is a common method of attempting suicide, patients may use substances that clinicians rarely encounter. For most toxic, nonmedication substances, data on interactions with medications are sparse. if you suspect your patient has ingested a toxic substance with which the treatment team has little experience, contact the American Association of Poison Control Centers at 800-222-1222.
Suspect superwarfarin poisoning in suicidal patients with coagulopathy, prolonged prothrombin time, and elevated INR that does not respond to large amounts of vitamin K.9,10 These patients are at high risk of successfully completing suicide because of superwarfarins’ long half-life and daily maintenance required to keep coagulation levels within a safe range for at least several weeks.
The most serious complication these patients face is intracranial hemorrhage, which occurs in 2% of patients with excessive warfarin-based coagulation and is associated with a 77% mortality rate.11 GI bleeding occurs in 67% of these patients.2
Also take into account medical conditions—such as hypertension or hepatic disease—and medication side effects that can increase bleeding risk. When treating pain in these patients, consider avoiding acetaminophen but be aware of the risks of NSAIDs, such as gastritis or GI bleeding.
Related resource
- The American Association of Poison Control Centers. 800-222-1222; www.aapcc.org.
Drug brand names
- Escitalopram • Lexapro
- Lamotrigine • Lamictal
- Pantoprazole • Protonix
- Warfarin • Coumadin
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sharma V, Khan M, Corpse C. Role of lamotrigine in the management of treatment-resistant bipolar II depression: a chart review. J Affect Disord Epub 2008 Mar 1.
2. Su M, Hoffman R. Anticoagulants. In: Flomenbaum NE, Goldfrank LR, Hoffman RS, et al, eds. Goldfrank’s toxicologic emergencies. 8th ed. New York, NY: McGraw-Hill Medical Publishing; 2006:891-4.
3. Chua JD, Friedenberg WR. Superwarfarin poisoning. Anaesth Intensive Care 1997;25:707-9.
4. Leck JB, Park BK. A comparative study of the effect of warfarin and brodifacoum on the relationship between vitamin K1 metabolism and clotting factor activity in warfarin susceptible and warfarin resistant rats. Biochem Pharmacol 1981;30:123-9.
5. Lund M. Comparative effect of the three rodenticides warfarin, difenacoum and brodifacoum on eight rodent species in short feeding periods. J Hyg 1981;87:101-7.
6. Park BK, Scott AK, Wilson AC, et al. Plasma disposition of vitamin K antagonism by warfarin, difenacoum and brodifacoum in the rabbit. Biochem Pharmacol 1982;31:3535-639.
7. Gebauer MG, Nyfort-Hansen K, Henschke PJ, Gallus AS. Warfarin and acetaminophen interaction. Pharmacotherapy 2003;23(1):109-12.
8. Mahe I, Bertrand N, Drouet L, et al. Interaction between paracetamol and warfarin in patients: a double-blind, placebo-controlled, randomized study. Haematologica 2006;91(12):1621-7.
9. Sharma P, Bentley P. Of rats and men: superwarfarin toxicity. Lancet 2005;365:552-3.
10. Scully M. Warfarin therapy: rat poison and the prevention of thrombosis. Biochemist 2002;24:15-7.
11. Mathiesen T, Benediktsdottir K, Johnsson H, Lindqvist M. Intracranial traumatic and nontraumatic haemorrhagic complications of warfarin treatment. Acta Neurol Scan 1995;91:208-14.
1. Sharma V, Khan M, Corpse C. Role of lamotrigine in the management of treatment-resistant bipolar II depression: a chart review. J Affect Disord Epub 2008 Mar 1.
2. Su M, Hoffman R. Anticoagulants. In: Flomenbaum NE, Goldfrank LR, Hoffman RS, et al, eds. Goldfrank’s toxicologic emergencies. 8th ed. New York, NY: McGraw-Hill Medical Publishing; 2006:891-4.
3. Chua JD, Friedenberg WR. Superwarfarin poisoning. Anaesth Intensive Care 1997;25:707-9.
4. Leck JB, Park BK. A comparative study of the effect of warfarin and brodifacoum on the relationship between vitamin K1 metabolism and clotting factor activity in warfarin susceptible and warfarin resistant rats. Biochem Pharmacol 1981;30:123-9.
5. Lund M. Comparative effect of the three rodenticides warfarin, difenacoum and brodifacoum on eight rodent species in short feeding periods. J Hyg 1981;87:101-7.
6. Park BK, Scott AK, Wilson AC, et al. Plasma disposition of vitamin K antagonism by warfarin, difenacoum and brodifacoum in the rabbit. Biochem Pharmacol 1982;31:3535-639.
7. Gebauer MG, Nyfort-Hansen K, Henschke PJ, Gallus AS. Warfarin and acetaminophen interaction. Pharmacotherapy 2003;23(1):109-12.
8. Mahe I, Bertrand N, Drouet L, et al. Interaction between paracetamol and warfarin in patients: a double-blind, placebo-controlled, randomized study. Haematologica 2006;91(12):1621-7.
9. Sharma P, Bentley P. Of rats and men: superwarfarin toxicity. Lancet 2005;365:552-3.
10. Scully M. Warfarin therapy: rat poison and the prevention of thrombosis. Biochemist 2002;24:15-7.
11. Mathiesen T, Benediktsdottir K, Johnsson H, Lindqvist M. Intracranial traumatic and nontraumatic haemorrhagic complications of warfarin treatment. Acta Neurol Scan 1995;91:208-14.