User login
A 22-year-old man came into the office concerned he may have warts on his penis. He believed the warts appeared about 3 months ago. He was single and did not have a sexual partner. He had been dating a woman for 1 year until he graduated from college 4 months ago. His sexual history was serial monogamy with 5 lifetime female sexual partners.
After some hesitation, he noted he slept with a woman one night following a graduation party. He admitted that they were both drunk and that he did not use a condom. He asked if this was how the condition could have developed.
He denied any history of sexually transmitted diseases (STDs) and the result of an HIV test was negative when he donated blood last year. He did not have urethral discharge or burning on urination. The patient had no other symptoms and no chronic illnesses. He generally had a healthy lifestyle, without drug and tobacco use. He said he used to drink at college parties, but rarely had a drink since starting work full-time.
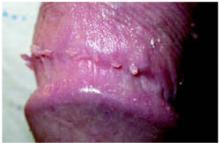
On physical exam, the patient had no fever or lymphadenopathy. A genital exam (Figure 1) with the foreskin retracted revealed skin-colored papules on the shaft of the penis that were somewhat verrucous. The papules seemed to make a ring around the shaft just proximal to the corona of the glans. Closer inspection showed smaller pearly papules surrounding the glans on the corona (Figure 2).
FIGURE 1
Large verrucuous papules
FIGURE 2
Detail of the smaller papules
Are The Larger Verrucous Papules Really Warts?
What Are The Smaller Papules And do they need treatment?
Diagnosis: Condyloma Acuminata
The larger verrucous papules are genital warts, also known as condyloma acuminata. These are caused by the human papillomavirus (HPV) and are sexually transmitted. The patient most likely acquired these from his last unprotected sexual encounter, but he may have been infected earlier and the warts just became visible in the last 3 months. The differential diagnosis includes condyloma lata, the flat warts of secondary syphilis, but these are much less common.
The small pearly papules on the corona are not warts but a variation of the normal male anatomy, called pearly penile papules. The reason to recognize these papules is to reassure worried men that they are normal and to avoid performing any invasive treatments to remove them.
Laboratory Examination
All patients with any sexually transmitted disease should be tested for syphilis and HIV regardless of other risk factors.1 In this case, testing for syphilis with either a rapid plasma reagin (RPR) or VDRL will also be helpful to rule out condyloma lata.
These genital warts do not need to be biopsied to make the diagnosis. No data support the use of type-specific HPV nucleic acid tests in the routine diagnosis or management of visible genital warts.1
Treatment: Removal With Medication Or Surgery
The primary goal of treating visible genital warts is the removal of symptomatic warts.1 Treatment can induce wart-free periods. Available therapies for genital warts may reduce, but probably do not eradicate, infectivity.1 No evidence suggests any available treatment is superior to another, and no single treatment is ideal for all patients or all warts. The natural history of genital warts is benign, and the types of HPV that usually cause external genital warts (HPV 6 and 11) are not associated with cancer.
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines1 for STDs recommend the following options. Cost data are given in the Table.
TABLE
Self-administered medications for HPV
| Medication | Method | Cost |
|---|---|---|
| Podofilox 0.5% solution or gel (podophyllotoxin) | Apply twice daily for 3 days, then off 4 days. May repeat cycle total of 4 times | Gel 0.5%, one 3.5-g tube:$164 Solution 0.5% one 3.5-g tube:$121* |
| Imiquimod 5% cream | Apply nightly 3 times per week. | 12 packets:$159* (enough for 4 weeks of therapy if 1 packet is used per application;using a packet for more than 1 day is possible) |
| Wash off after 6 to 10 hours. | ||
| May use up to 16 weeks. | ||
| * Prices from ePocrates,accessed on October 3,2004. | ||
Patient-applied treatments
- Podofilox 0.5% solution or gel. Patients should apply podofilox solution with a cotton swab, or podofilox gel with a finger, to visible genital warts twice a day for 3 days, followed by 4 days of no therapy. This cycle may be repeated, as necessary, for up to 4 cycles. The health care provider may apply the initial treatment to demonstrate the proper application technique and identify which warts should be treated.
- Imiquimod 5% cream. Patients should apply imiquimod cream once daily at bedtime, 3 times a week for up to 16 weeks. The treatment area should be washed with soap and water 6 to 10 hours after the application.
Provider-administered treatments
- Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1 to 2 weeks.
- Podophyllin resin 10% to 25% in a compound tincture of benzoin. A small amount should be applied to each wart and allowed to air-dry. The treatment can be repeated weekly, if necessary. To avoid the possibility of complications associated with systemic absorption and toxicity, some specialists recommend that application be limited to ≤0.5 mL of podophyllin or an area of <10 cm2 of warts per session. Some specialists suggest the preparation should be thoroughly washed off 1 to 4 hours after application to reduce local irritation. The safety of podophyllin during pregnancy has not been established.
- Trichloroacetic acid (TCA): a small amount should be applied only to warts and allowed to dry, at which time a white “frosting” develops (Figure 3). This treatment can be repeated weekly, if necessary.
- Surgical removal either by tangential scissor excision, tangential shave excision, curettage, or electrosurgery.
FIGURE 3
Treatment of genital warts
Keratinized vs nonkeratinized warts
In choosing the type of therapy for a patient, it is helpful to note that the soft, nonkeratinized warts respond well to the various forms of podophyllin and trichloroacetic acid. The more keratinized lesions, however, respond better to physical ablative methods such as cryotherapy, excision, or electrocautery. Imiquimod appears to work well for both types of lesions but is more effective for the nonkeratinized warts.
The softer, nonkeratinized warts are found more often on softer mucosa around the anus, under the foreskin, and around the female introitus. The firmer, more keratinized warts are found more often on more keratinized skin such as on the shaft of the penis.
Most options yield inadequate results
The reason for so many treatment options is in part due to the therapeutic inadequacy of any one of them. Cure rates are far less than optimal, and relapse rates are disappointing. While we have reasonable treatment guidelines from the CDC, studies on many of the treatment options are limited. There are few head-to-head studies of one method vs another.
One double-blind, randomized, multicenter, vehicle-controlled study2 demonstrated that 0.5% podofilox gel was significantly better than vehicle gel for successfully eliminating and reducing the number and size of anogenital warts. In the intention-to-treat population, 37% treated with podofilox gel had complete clearing of the treated areas, compared with 2% who had clearing of warts with the vehicle gel after 4 weeks (P<.001; number needed to treat=3) (level of evidence [LOE]: 1b).
The best systematic review of genital wart treatment was published in 2004 in the International Journal of STD & AIDS.3 Imiquimod has proven effective in many studies, including 3 randomized controlled trials in which clearance rates were 37% to 52% after 8 to 16 weeks of treatment (LOE=1a).3 One study using imiquimod found that clearance rates were twofold higher for women than for men (72% and 33%, respectively).4 This is probably because genital warts in females are less keratinized than warts on the usual site in males, the penile shaft. Similarly, clearance rates with imiquimod seem to be higher in uncircumcised men (62%) than circumcised men (33%), probably related to the degree of keratinization.3
Recurrence rates for sole therapy with imiquimod (9%–19%) are substantially lower than for most other genital wart treatments, including podophyllotoxin.3 Imiquimod may even be effective in reducing wart recurrence rates when used as an adjunct to surgical treatment.3
The Patient’s Treatment: Cryotherapy, Imiquimod Cream
The treatment options were discussed with the patient. The patient decided to have cryotherapy performed in the office and was given a prescription for imiquimod cream to be used on any remaining warts. The normal pearly penile papules on the corona were left alone and the patient tolerated the cryotherapy to the real warts with an acceptable level of temporary discomfort.
- Imiquimod • Aldara
- Podofilox • Condylox
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6):1-78.Available online at: http://www.cdc.gov/std/treatment/. (Note: The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at the following website: www.cdcnpin.org/scripts/std/pda.asp.)
2. Tyring S, Edwards L, Cherry LK, et al. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenital warts. Arch Dermatol 1998;134:33-38.
3. Maw R. Critical appraisal of commonly used treatment for genital warts. Int J STD AIDS 2004;15:357-364.
4. Sauder DN, Skinner RB, Fox TL, Owens ML. Topical imiquimod 5% cream as an effective treatment for external genital and perianal warts in different patient populations. Sex Transm Dis 2003;Feb;30(2):124-8.
A 22-year-old man came into the office concerned he may have warts on his penis. He believed the warts appeared about 3 months ago. He was single and did not have a sexual partner. He had been dating a woman for 1 year until he graduated from college 4 months ago. His sexual history was serial monogamy with 5 lifetime female sexual partners.
After some hesitation, he noted he slept with a woman one night following a graduation party. He admitted that they were both drunk and that he did not use a condom. He asked if this was how the condition could have developed.
He denied any history of sexually transmitted diseases (STDs) and the result of an HIV test was negative when he donated blood last year. He did not have urethral discharge or burning on urination. The patient had no other symptoms and no chronic illnesses. He generally had a healthy lifestyle, without drug and tobacco use. He said he used to drink at college parties, but rarely had a drink since starting work full-time.
On physical exam, the patient had no fever or lymphadenopathy. A genital exam (Figure 1) with the foreskin retracted revealed skin-colored papules on the shaft of the penis that were somewhat verrucous. The papules seemed to make a ring around the shaft just proximal to the corona of the glans. Closer inspection showed smaller pearly papules surrounding the glans on the corona (Figure 2).
FIGURE 1
Large verrucuous papules
FIGURE 2
Detail of the smaller papules
Are The Larger Verrucous Papules Really Warts?
What Are The Smaller Papules And do they need treatment?
Diagnosis: Condyloma Acuminata
The larger verrucous papules are genital warts, also known as condyloma acuminata. These are caused by the human papillomavirus (HPV) and are sexually transmitted. The patient most likely acquired these from his last unprotected sexual encounter, but he may have been infected earlier and the warts just became visible in the last 3 months. The differential diagnosis includes condyloma lata, the flat warts of secondary syphilis, but these are much less common.
The small pearly papules on the corona are not warts but a variation of the normal male anatomy, called pearly penile papules. The reason to recognize these papules is to reassure worried men that they are normal and to avoid performing any invasive treatments to remove them.
Laboratory Examination
All patients with any sexually transmitted disease should be tested for syphilis and HIV regardless of other risk factors.1 In this case, testing for syphilis with either a rapid plasma reagin (RPR) or VDRL will also be helpful to rule out condyloma lata.
These genital warts do not need to be biopsied to make the diagnosis. No data support the use of type-specific HPV nucleic acid tests in the routine diagnosis or management of visible genital warts.1
Treatment: Removal With Medication Or Surgery
The primary goal of treating visible genital warts is the removal of symptomatic warts.1 Treatment can induce wart-free periods. Available therapies for genital warts may reduce, but probably do not eradicate, infectivity.1 No evidence suggests any available treatment is superior to another, and no single treatment is ideal for all patients or all warts. The natural history of genital warts is benign, and the types of HPV that usually cause external genital warts (HPV 6 and 11) are not associated with cancer.
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines1 for STDs recommend the following options. Cost data are given in the Table.
TABLE
Self-administered medications for HPV
| Medication | Method | Cost |
|---|---|---|
| Podofilox 0.5% solution or gel (podophyllotoxin) | Apply twice daily for 3 days, then off 4 days. May repeat cycle total of 4 times | Gel 0.5%, one 3.5-g tube:$164 Solution 0.5% one 3.5-g tube:$121* |
| Imiquimod 5% cream | Apply nightly 3 times per week. | 12 packets:$159* (enough for 4 weeks of therapy if 1 packet is used per application;using a packet for more than 1 day is possible) |
| Wash off after 6 to 10 hours. | ||
| May use up to 16 weeks. | ||
| * Prices from ePocrates,accessed on October 3,2004. | ||
Patient-applied treatments
- Podofilox 0.5% solution or gel. Patients should apply podofilox solution with a cotton swab, or podofilox gel with a finger, to visible genital warts twice a day for 3 days, followed by 4 days of no therapy. This cycle may be repeated, as necessary, for up to 4 cycles. The health care provider may apply the initial treatment to demonstrate the proper application technique and identify which warts should be treated.
- Imiquimod 5% cream. Patients should apply imiquimod cream once daily at bedtime, 3 times a week for up to 16 weeks. The treatment area should be washed with soap and water 6 to 10 hours after the application.
Provider-administered treatments
- Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1 to 2 weeks.
- Podophyllin resin 10% to 25% in a compound tincture of benzoin. A small amount should be applied to each wart and allowed to air-dry. The treatment can be repeated weekly, if necessary. To avoid the possibility of complications associated with systemic absorption and toxicity, some specialists recommend that application be limited to ≤0.5 mL of podophyllin or an area of <10 cm2 of warts per session. Some specialists suggest the preparation should be thoroughly washed off 1 to 4 hours after application to reduce local irritation. The safety of podophyllin during pregnancy has not been established.
- Trichloroacetic acid (TCA): a small amount should be applied only to warts and allowed to dry, at which time a white “frosting” develops (Figure 3). This treatment can be repeated weekly, if necessary.
- Surgical removal either by tangential scissor excision, tangential shave excision, curettage, or electrosurgery.
FIGURE 3
Treatment of genital warts
Keratinized vs nonkeratinized warts
In choosing the type of therapy for a patient, it is helpful to note that the soft, nonkeratinized warts respond well to the various forms of podophyllin and trichloroacetic acid. The more keratinized lesions, however, respond better to physical ablative methods such as cryotherapy, excision, or electrocautery. Imiquimod appears to work well for both types of lesions but is more effective for the nonkeratinized warts.
The softer, nonkeratinized warts are found more often on softer mucosa around the anus, under the foreskin, and around the female introitus. The firmer, more keratinized warts are found more often on more keratinized skin such as on the shaft of the penis.
Most options yield inadequate results
The reason for so many treatment options is in part due to the therapeutic inadequacy of any one of them. Cure rates are far less than optimal, and relapse rates are disappointing. While we have reasonable treatment guidelines from the CDC, studies on many of the treatment options are limited. There are few head-to-head studies of one method vs another.
One double-blind, randomized, multicenter, vehicle-controlled study2 demonstrated that 0.5% podofilox gel was significantly better than vehicle gel for successfully eliminating and reducing the number and size of anogenital warts. In the intention-to-treat population, 37% treated with podofilox gel had complete clearing of the treated areas, compared with 2% who had clearing of warts with the vehicle gel after 4 weeks (P<.001; number needed to treat=3) (level of evidence [LOE]: 1b).
The best systematic review of genital wart treatment was published in 2004 in the International Journal of STD & AIDS.3 Imiquimod has proven effective in many studies, including 3 randomized controlled trials in which clearance rates were 37% to 52% after 8 to 16 weeks of treatment (LOE=1a).3 One study using imiquimod found that clearance rates were twofold higher for women than for men (72% and 33%, respectively).4 This is probably because genital warts in females are less keratinized than warts on the usual site in males, the penile shaft. Similarly, clearance rates with imiquimod seem to be higher in uncircumcised men (62%) than circumcised men (33%), probably related to the degree of keratinization.3
Recurrence rates for sole therapy with imiquimod (9%–19%) are substantially lower than for most other genital wart treatments, including podophyllotoxin.3 Imiquimod may even be effective in reducing wart recurrence rates when used as an adjunct to surgical treatment.3
The Patient’s Treatment: Cryotherapy, Imiquimod Cream
The treatment options were discussed with the patient. The patient decided to have cryotherapy performed in the office and was given a prescription for imiquimod cream to be used on any remaining warts. The normal pearly penile papules on the corona were left alone and the patient tolerated the cryotherapy to the real warts with an acceptable level of temporary discomfort.
- Imiquimod • Aldara
- Podofilox • Condylox
A 22-year-old man came into the office concerned he may have warts on his penis. He believed the warts appeared about 3 months ago. He was single and did not have a sexual partner. He had been dating a woman for 1 year until he graduated from college 4 months ago. His sexual history was serial monogamy with 5 lifetime female sexual partners.
After some hesitation, he noted he slept with a woman one night following a graduation party. He admitted that they were both drunk and that he did not use a condom. He asked if this was how the condition could have developed.
He denied any history of sexually transmitted diseases (STDs) and the result of an HIV test was negative when he donated blood last year. He did not have urethral discharge or burning on urination. The patient had no other symptoms and no chronic illnesses. He generally had a healthy lifestyle, without drug and tobacco use. He said he used to drink at college parties, but rarely had a drink since starting work full-time.
On physical exam, the patient had no fever or lymphadenopathy. A genital exam (Figure 1) with the foreskin retracted revealed skin-colored papules on the shaft of the penis that were somewhat verrucous. The papules seemed to make a ring around the shaft just proximal to the corona of the glans. Closer inspection showed smaller pearly papules surrounding the glans on the corona (Figure 2).
FIGURE 1
Large verrucuous papules
FIGURE 2
Detail of the smaller papules
Are The Larger Verrucous Papules Really Warts?
What Are The Smaller Papules And do they need treatment?
Diagnosis: Condyloma Acuminata
The larger verrucous papules are genital warts, also known as condyloma acuminata. These are caused by the human papillomavirus (HPV) and are sexually transmitted. The patient most likely acquired these from his last unprotected sexual encounter, but he may have been infected earlier and the warts just became visible in the last 3 months. The differential diagnosis includes condyloma lata, the flat warts of secondary syphilis, but these are much less common.
The small pearly papules on the corona are not warts but a variation of the normal male anatomy, called pearly penile papules. The reason to recognize these papules is to reassure worried men that they are normal and to avoid performing any invasive treatments to remove them.
Laboratory Examination
All patients with any sexually transmitted disease should be tested for syphilis and HIV regardless of other risk factors.1 In this case, testing for syphilis with either a rapid plasma reagin (RPR) or VDRL will also be helpful to rule out condyloma lata.
These genital warts do not need to be biopsied to make the diagnosis. No data support the use of type-specific HPV nucleic acid tests in the routine diagnosis or management of visible genital warts.1
Treatment: Removal With Medication Or Surgery
The primary goal of treating visible genital warts is the removal of symptomatic warts.1 Treatment can induce wart-free periods. Available therapies for genital warts may reduce, but probably do not eradicate, infectivity.1 No evidence suggests any available treatment is superior to another, and no single treatment is ideal for all patients or all warts. The natural history of genital warts is benign, and the types of HPV that usually cause external genital warts (HPV 6 and 11) are not associated with cancer.
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines1 for STDs recommend the following options. Cost data are given in the Table.
TABLE
Self-administered medications for HPV
| Medication | Method | Cost |
|---|---|---|
| Podofilox 0.5% solution or gel (podophyllotoxin) | Apply twice daily for 3 days, then off 4 days. May repeat cycle total of 4 times | Gel 0.5%, one 3.5-g tube:$164 Solution 0.5% one 3.5-g tube:$121* |
| Imiquimod 5% cream | Apply nightly 3 times per week. | 12 packets:$159* (enough for 4 weeks of therapy if 1 packet is used per application;using a packet for more than 1 day is possible) |
| Wash off after 6 to 10 hours. | ||
| May use up to 16 weeks. | ||
| * Prices from ePocrates,accessed on October 3,2004. | ||
Patient-applied treatments
- Podofilox 0.5% solution or gel. Patients should apply podofilox solution with a cotton swab, or podofilox gel with a finger, to visible genital warts twice a day for 3 days, followed by 4 days of no therapy. This cycle may be repeated, as necessary, for up to 4 cycles. The health care provider may apply the initial treatment to demonstrate the proper application technique and identify which warts should be treated.
- Imiquimod 5% cream. Patients should apply imiquimod cream once daily at bedtime, 3 times a week for up to 16 weeks. The treatment area should be washed with soap and water 6 to 10 hours after the application.
Provider-administered treatments
- Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1 to 2 weeks.
- Podophyllin resin 10% to 25% in a compound tincture of benzoin. A small amount should be applied to each wart and allowed to air-dry. The treatment can be repeated weekly, if necessary. To avoid the possibility of complications associated with systemic absorption and toxicity, some specialists recommend that application be limited to ≤0.5 mL of podophyllin or an area of <10 cm2 of warts per session. Some specialists suggest the preparation should be thoroughly washed off 1 to 4 hours after application to reduce local irritation. The safety of podophyllin during pregnancy has not been established.
- Trichloroacetic acid (TCA): a small amount should be applied only to warts and allowed to dry, at which time a white “frosting” develops (Figure 3). This treatment can be repeated weekly, if necessary.
- Surgical removal either by tangential scissor excision, tangential shave excision, curettage, or electrosurgery.
FIGURE 3
Treatment of genital warts
Keratinized vs nonkeratinized warts
In choosing the type of therapy for a patient, it is helpful to note that the soft, nonkeratinized warts respond well to the various forms of podophyllin and trichloroacetic acid. The more keratinized lesions, however, respond better to physical ablative methods such as cryotherapy, excision, or electrocautery. Imiquimod appears to work well for both types of lesions but is more effective for the nonkeratinized warts.
The softer, nonkeratinized warts are found more often on softer mucosa around the anus, under the foreskin, and around the female introitus. The firmer, more keratinized warts are found more often on more keratinized skin such as on the shaft of the penis.
Most options yield inadequate results
The reason for so many treatment options is in part due to the therapeutic inadequacy of any one of them. Cure rates are far less than optimal, and relapse rates are disappointing. While we have reasonable treatment guidelines from the CDC, studies on many of the treatment options are limited. There are few head-to-head studies of one method vs another.
One double-blind, randomized, multicenter, vehicle-controlled study2 demonstrated that 0.5% podofilox gel was significantly better than vehicle gel for successfully eliminating and reducing the number and size of anogenital warts. In the intention-to-treat population, 37% treated with podofilox gel had complete clearing of the treated areas, compared with 2% who had clearing of warts with the vehicle gel after 4 weeks (P<.001; number needed to treat=3) (level of evidence [LOE]: 1b).
The best systematic review of genital wart treatment was published in 2004 in the International Journal of STD & AIDS.3 Imiquimod has proven effective in many studies, including 3 randomized controlled trials in which clearance rates were 37% to 52% after 8 to 16 weeks of treatment (LOE=1a).3 One study using imiquimod found that clearance rates were twofold higher for women than for men (72% and 33%, respectively).4 This is probably because genital warts in females are less keratinized than warts on the usual site in males, the penile shaft. Similarly, clearance rates with imiquimod seem to be higher in uncircumcised men (62%) than circumcised men (33%), probably related to the degree of keratinization.3
Recurrence rates for sole therapy with imiquimod (9%–19%) are substantially lower than for most other genital wart treatments, including podophyllotoxin.3 Imiquimod may even be effective in reducing wart recurrence rates when used as an adjunct to surgical treatment.3
The Patient’s Treatment: Cryotherapy, Imiquimod Cream
The treatment options were discussed with the patient. The patient decided to have cryotherapy performed in the office and was given a prescription for imiquimod cream to be used on any remaining warts. The normal pearly penile papules on the corona were left alone and the patient tolerated the cryotherapy to the real warts with an acceptable level of temporary discomfort.
- Imiquimod • Aldara
- Podofilox • Condylox
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6):1-78.Available online at: http://www.cdc.gov/std/treatment/. (Note: The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at the following website: www.cdcnpin.org/scripts/std/pda.asp.)
2. Tyring S, Edwards L, Cherry LK, et al. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenital warts. Arch Dermatol 1998;134:33-38.
3. Maw R. Critical appraisal of commonly used treatment for genital warts. Int J STD AIDS 2004;15:357-364.
4. Sauder DN, Skinner RB, Fox TL, Owens ML. Topical imiquimod 5% cream as an effective treatment for external genital and perianal warts in different patient populations. Sex Transm Dis 2003;Feb;30(2):124-8.
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6):1-78.Available online at: http://www.cdc.gov/std/treatment/. (Note: The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at the following website: www.cdcnpin.org/scripts/std/pda.asp.)
2. Tyring S, Edwards L, Cherry LK, et al. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenital warts. Arch Dermatol 1998;134:33-38.
3. Maw R. Critical appraisal of commonly used treatment for genital warts. Int J STD AIDS 2004;15:357-364.
4. Sauder DN, Skinner RB, Fox TL, Owens ML. Topical imiquimod 5% cream as an effective treatment for external genital and perianal warts in different patient populations. Sex Transm Dis 2003;Feb;30(2):124-8.