User login
A 55-year-old woman has come to the clinic because of clear rhinorrhea and nasal congestion, which occur year-round but are worse in the winter. She reports that at times her nose runs continuously. Nasal symptoms have been present for 4 to 5 years but are worsening. The clear discharge is not associated with sneezing or itching. Though she lives with a cat, her symptoms are not exacerbated by close contact with it.
One year ago, an allergist performed skin testing but found no evidence of allergies as a cause of her rhinitis. A short course of intranasal steroids did not seem to improve her nasal symptoms.
The patient also has hypertension, hypothyroidism, and hot flashes due to menopause; these conditions are well controlled with lisinopril (Zestril), levothyroxine (Synthroid), and estrogen replacement. She has no history of asthma and has had no allergies to drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs.)
How should this patient be evaluated and treated?
COMMON, OFTEN OVERLOOKED
Many patients suffer from rhinitis, but this problem can be overshadowed by other chronic diseases seen in a medical clinic, especially during a brief office visit. When a patient presents with rhinitis, a key question is whether it is allergic or nonallergic.
This review will discuss the different forms of nonallergic rhinitis and their causes, and give recommendations about therapy.
RHINITIS: ALLERGIC OR NONALLERGIC?
While allergic rhinitis affects 30 and 60 million Americans annually, or between 10% to 30% of US adults,1 how many have nonallergic rhinitis has been difficult to determine.
In a study in allergy clinics, 23% of patients with rhinitis had the nonallergic form, 43% had the allergic form, and 34% had both forms (mixed rhinitis).2 Other studies have suggested that up to 52% of patients presenting to allergy clinics with rhinitis have nonallergic rhinitis.3
Over time, patients may not stay in the same category. One study found that 24% of patients originally diagnosed with nonallergic rhinitis developed positive allergy tests when retested 3 or more years after their initial evaluation.4
Regardless of the type, untreated or uncontrolled symptoms of rhinitis can significantly affect the quality of life.
All forms of rhinitis are characterized by one or more of the following symptoms: nasal congestion, clear rhinorrhea, sneezing, and itching. These symptoms can be episodic or chronic and can range from mild to debilitating. In addition, rhinitis can lead to systemic symptoms of fatigue, headache, sleep disturbance, and cognitive impairment and can be associated with respiratory symptoms such as sinusitis and asthma.1
Mechanisms are mostly unknown
While allergic rhinitis leads to symptoms when airborne allergens bind with specific immunoglobulin E (IgE) in the nose, the etiology of most forms of nonallergic rhinitis is unknown. However, several mechanisms have been proposed. These include entopy (local nasal IgE synthesis with negative skin tests),5 nocioceptive dysfunction (hyperactive sensory receptors),6 and autonomic nervous system abnormalities (hypoactive or hyperactive dysfunction of sympathetic or parasympathetic nerves in the nose).7
Does this patient have an allergic cause of rhinitis?
When considering a patient with rhinitis, the most important question is, “Does this patient have an allergic cause of rhinitis?” Allergic and nonallergic rhinitis have similar symptoms, making them difficult to distinguish. However, their mechanisms and treatment differ. By categorizing a patient’s type of rhinitis, the physician can make specific recommendations for avoidance and can initiate treatment with the most appropriate therapy. Misclassification can lead to treatment failure, multiple visits, poor adherence, and frustration for patients with uncontrolled symptoms.
Patients for whom an allergic cause cannot be found by allergy skin testing or serum specific IgE immunoassay (Immunocap/RAST) for environmental aeroallergens are classified as having nonallergic rhinitis.
CLUES POINTING TO NONALLERGIC VS ALLERGIC RHINITIS
Nonallergic rhinitis encompasses a range of syndromes with overlapping symptoms. While tools such as the Rhinitis Diagnostic Worksheet are available to help differentiate allergic from nonallergic rhinitis, debate continues about whether it is necessary to characterize different forms of rhinitis before initiating treatment.8
The diagnosis of nonallergic rhinitis depends on a thorough history and physical examination. Key questions relate to the triggers that bring on the rhinitis, which will assist the clinician in determining which subtype of rhinitis a patient may be experiencing and therefore how to manage it. Clues:
- Patients with nonallergic rhinitis more often report nasal congestion and rhinorrhea, rather than sneezing and itching, which are predominant symptoms of allergic rhinitis.
- Patients with nonallergic rhinitis tend to develop symptoms at a later age.
- Common triggers of nonallergic rhinitis are changes in weather and temperature, food, perfumes, odors, smoke, and fumes. Animal exposure does not lead to symptoms.
- Patients with nonallergic rhinitis have few complaints of concomitant symptoms of allergic conjunctivitis (itching, watering, redness, and swelling).
- Many patients with nonallergic rhinitis find that antihistamines have no benefit. Also, they do not have other atopic diseases such as eczema or food allergies and have no family history of atopy.
PHYSICAL FINDINGS
Some findings on physical examination may help distinguish allergic from nonallergic rhinitis.
- Patients with long-standing allergic rhinitis may have an “allergic crease,” ie, a horizontal wrinkle near the tip of the nose caused by frequent upward wiping. Another sign may be a gothic arch, which is a narrowing of the hard palate occurring as a child.
- In allergic rhinitis, the turbinates are often pale, moist, and boggy with a bluish tinge.
CASE CONTINUED
Our patient’s symptoms can be caused by many different factors. Allergic triggers for rhinitis include both indoor and outdoor sources. The most common allergens include cat, dog, dust mite, cockroach, mold, and pollen allergens. The absence of acute sneezing and itching when around her cat and her recent negative skin-prick tests confirm that the rhinitis symptoms are not allergic.
In this patient, who has symptoms throughout the year but no allergic triggers, consideration of the different subtypes of nonallergic rhinitis may help guide further therapy.
SUBTYPES OF NONALLERGIC RHINITIS
Vasomotor rhinitis
Vasomotor rhinitis is thought to be caused by a variety of neural and vascular triggers, often without an inflammatory cause. These triggers lead to symptoms involving nasal congestion and clear rhinorrhea more than sneezing and itching. The symptoms can be sporadic, with acute onset in relation to identifiable nonallergic triggers, or chronic, with no clear trigger.
Gustatory rhinitis, for example, is a form of vasomotor rhinitis in which clear rhinorrhea occurs suddenly while eating or while drinking alcohol. It may be prevented by using nasal ipratropium (Atrovent) before meals.
Irritant-sensitive vasomotor rhinitis. In some patients, acute vasomotor rhinitis symptoms are brought on by strong odors, cigarette smoke, air pollution, or perfume. When asked, most patients easily identify which of these irritant triggers cause symptoms.
Weather- or temperature-sensitive vasomotor rhinitis. In other patients, a change in temperature, humidity, or barometric pressure or exposure to cold or dry air can cause nasal symptoms.9 These triggers are often hard to identify. Weather- or temperature-sensitive vasomotor rhinitis is often mistaken for seasonal allergic rhinitis because weather changes occur in close relation to the peak allergy seasons in the spring and fall. However, this subtype does not respond as well to intranasal steroids.9
Other nonallergic triggers of vasomotor rhinitis may include exercise, emotion, and sexual arousal (honeymoon rhinitis).10
Some triggers, such as tobacco smoke and perfume, are easy to avoid. Other triggers, such as weather changes, are unavoidable. If avoidance measures fail or are inadequate, medications (described below) can be used for prophylaxis and symptomatic treatment.
Drug-induced rhinitis
Drugs of various classes are known to cause either acute or chronic rhinitis. Drug-induced rhinitis has been divided into different types based on the mechanism involved.11
The local inflammatory type occurs in aspirin-exacerbated respiratory disease, which is characterized by nasal polyposis with chronic rhinosinusitis, hyposmia, and moderate to severe persistent asthma. Aspirin and other NSAIDs induce an acute local inflammation, leading to severe rhinitis and asthma symptoms. Avoiding all NSAID products is recommended; aspirin desensitization may lead to improvement in rhinosinusitis and asthma control.
The neurogenic type of drug-induced rhinitis can occur with sympatholytic drugs such as alpha receptor agonists (eg, clonidine [Cat-apres]) and antagonists (eg, prazosin [Minipress]).11 Vasodilators, including phosphodiesterase-5 inhibitors such as sildenafil (Viagra), can lead to acute rhinitis symptoms (“anniversary rhinitis”).
Unknown mechanisms. Many other medications can lead to rhinitis by unknown mechanisms, usually with normal findings on physical examination. These include beta-blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, exogenous estrogens, oral contraceptives, antipsychotics, and gabapentin (Neurontin).
Correlating the initiation of a drug with the onset of rhinitis can help identify offending medications. Stopping the suspected medication, if feasible, is the first-line treatment.
Rhinitis medicamentosa, typically caused by overuse of over-the-counter topical nasal decongestants, is also classified under drug-induced rhinitis. Patients may not think of nasal decongestants as medications, and the physician may need to ask specifically about their use.
On examination, the nasal mucosa appears beefy red without mucous. Once a diagnosis is made, the physician should identify and treat the original etiology of the nasal congestion that led the patient to self-treat.
Patients with rhinitis medicamentosa often have difficulty discontinuing use of topical decongestants. They should be educated that the withdrawal symptoms can be severe and that more than one attempt at quitting may be needed. To break the cycle of rebound congestion, topical intranasal steroids should be used, though 5 to 7 days of oral steroids may be necessary.1
Cocaine is a potent vasoconstrictor. Its illicit use should be suspected, especially if the patient presents with symptoms of chronic irritation such as frequent nosebleeds, crusting, and scabbing.12
Infectious rhinitis
One of the most common causes of acute rhinitis is upper respiratory infection.
Acute viral upper respiratory infection often presents with thick nasal discharge, sneezing, and nasal obstruction that usually clears in 7 to 10 days but can last up to 3 weeks. Acute bacterial sinusitis can follow, typically in fewer than 2% of patients, with symptoms of persistent nasal congestion, discolored mucus, facial pain, cough, and sometimes fever.
Chronic rhinosinusitis is a syndrome with sinus mucosal inflammation with multiple causes. It is clinically defined as persistent nasal and sinus symptoms lasting longer than 12 weeks and confirmed with computed tomography (CT).13 The CT findings of chronic rhinosinusitis include thickening of the lining of the sinus cavities or complete opacification of the pneumatized sinuses.
Major symptoms to consider for diagnosis include facial pain, congestion, obstruction, purulent discharge on examination, and changes in olfaction. Minor symptoms are cough, fatigue, headache, halitosis, fever, ear symptoms, and dental pain.
Treatment may involve 3 or more weeks of an oral antibiotic and a short course of an oral steroid, a daily nasal steroid spray, or both oral and nasal steroids. Most patients can be managed in the primary care setting, but they can be referred to an ear, nose, and throat specialist, an allergist, or an immunologist if their symptoms do not respond to initial therapy.
Nonallergic rhinitis eosinophilic syndrome
Patients with nonallergic rhinitis eosinophilic syndrome (NARES) are typically middle-aged and have perennial symptoms of sneezing, itching, and rhinorrhea with intermittent exacerbations. They occasionally have associated hyposmia (impaired sense of smell).1 The diagnosis is made when eosinophils account for more than 5% of cells on a nasal smear and allergy testing is negative.
Patients may develop nasal polyposis and aspirin sensitivity.1 Entopy has been described in some.14
Because of the eosinophilic inflammation, this form of nonallergic rhinitis responds well to intranasal steroids.
Immunologic causes
Systemic diseases can affect the nose and cause variable nasal symptoms that can be mistaken for rhinitis. Wegener granulomatosis, sarcoidosis, relapsing polychondritis, midline granulomas, Churg-Strauss syndrome, and amyloidosis can all affect the structures in the nose even before manifesting systemic symptoms. Granulomatous infections in the nose may lead to crusting, bleeding, and nasal obstruction.1
A lack of a response to intranasal steroids or oral antibiotics should lead to consideration of these conditions, and treatment should be tailored to the specific disease.
Occupational rhinitis
Occupational exposure to chemicals, biologic aerosols, flour, and latex can lead to rhinitis, typically through an inflammatory mechanism. Many patients present with associated occupational asthma. The symptoms improve when the patient is away from work and worsen throughout the work week.
Avoiding the triggering agent is necessary to treat these symptoms.
Hormonal rhinitis
Hormonal rhinitis, ie, rhinitis related to metabolic and endocrine conditions, is most commonly associated with high estrogen states. Nasal congestion has been reported with pregnancy, menses, menarche, and the use of oral contraceptives.15 The mechanism for congestion in these conditions still needs clarification.
When considering drug therapy, only intranasal budesonide (Rhinocort) has a pregnancy category B rating.
While hypothyroidism and acromegaly have been mentioned in reviews of nonallergic rhinitis, evidence that these disorders cause nonallergic rhinitis is not strong.16,17
Structurally related rhinitis
Anatomic abnormalities that can cause persistent nasal congestion include nasal septal deviation, turbinate hypertrophy, enlarged adenoids, tumors, and foreign bodies. These can be visualized by simple anterior nasal examination, nasal endoscopy, or radiologic studies. If structural causes lead to impaired quality of life or chronic rhinosinusitis, then consider referral to a specialist for possible surgical treatment.
Clear spontaneous rhinorrhea, with or without trauma, can be caused by cerebrospinal fluid leaking into the nasal cavity.18 A salty, metallic taste in the mouth can be a clue that the fluid is cerebrospinal fluid. A definitive diagnosis of cerebrospinal fluid leak is made by finding beta-2-transferrin in nasal secretions.
Atrophic rhinitis
Atrophic rhinitis is categorized as primary or secondary.
Primary (idiopathic) atrophic rhinitis is characterized by atrophy of the nasal mucosa and mucosal colonization with Klebsiella ozaenae associated with a foul-smelling nasal discharge.19,20 This disorder has been primarily reported in young people who present with nasal obstruction, dryness, crusting, and epistaxis. They are from areas with warm climates, such as the Middle East, Southeast Asia, India, Africa, and the Mediterranean.
Secondary atrophic rhinitis can be a complication of nasal or sinus surgery, trauma, granulomatous disease, or exposure to radiation.21 This disorder is typically diagnosed with nasal endoscopy and treated with daily saline rinses with or without topical antibiotics.21
CASE CONTINUED
Questioned further, our patient says her symptoms are worse when her husband smokes, but that she continues to have congestion and rhinorrhea when he is away on business trips. She notes that her symptoms are often worse on airplanes (dry air with an acute change in barometric pressure), with weather changes, and in cold, dry environments. Symptoms are not induced by eating.
We note that she started taking lisinopril 2 years ago and conjugated equine estrogens 8 years ago. Review of systems reveals no history of facial or head trauma, polyps, or hyposmia.
The rhinitis and congestion are bilateral, and she denies headaches, acid reflux, and conjunctivitis. She has a mild throat-clearing cough that she attributes to postnasal drip.
On physical examination, her blood pressure is 118/76 mm Hg and her pulse is 64. Her turbinates are congested with clear rhinorrhea. The rest of the examination is normal.
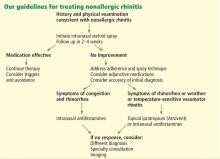
AVOID TRIGGERS, PRETREAT BEFORE EXPOSURE
People with known environmental, non-immunologic, and irritant triggers should be reminded to avoid these exposures if possible.
If triggers are unavoidable, patients can pretreat themselves with topical nasal sprays before exposure. For example, if symptoms occur while on airplanes, then intranasal steroids or antihistamine sprays should be used before getting on the plane.
Many drugs available
Fortunately, many effective drugs are available to treat nonallergic rhinitis. These have few adverse effects or drug interactions.
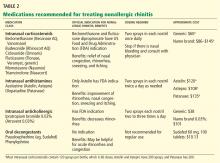
Intranasal steroid sprays are considered first-line therapy, as there are studies demonstrating effectiveness in nonallergic rhinitis.22 Intranasal fluticasone propionate (Flonase) and beclomethasone dipropionate (Beconase AQ) are approved by the US Food and Drug Administration (FDA) for treating nonallergic rhinitis. Intranasal mometasone (Nasonex) is approved for treating nasal polyps.
Nasal steroid sprays are most effective if the dominant nasal symptom is congestion, but they have also shown benefit for rhinorrhea, sneezing, and itching.
Side effects of nasal steroid sprays include nasal irritation (dryness, burning, and stinging) and epistaxis, the latter occurring in 5% to 10% of patients.23
Intranasal antihistamines include azelastine (Astelin, Astepro) and olopatadine (Patanase). They are particularly useful for treating sneezing, congestion, and rhinorrhea.24 Astelin is the only intranasal antihistamine with FDA approval for nonallergic rhinitis.
Side effects of this drug class include bitter taste (with Astelin), sweet taste (with Astepro), headache, and somnolence.
Oral antihistamines such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are now available over the counter, and many patients try them before seeking medical care. These drugs may be helpful for those bothered by sneezing. However, no study has demonstrated their effectiveness for nonallergic rhinitis.25 First-generation antihistamines may help with rhinorrhea via their anticholinergic effects.
Ipratropium, an antimuscarinic agent, decreases secretions by inhibiting the nasal parasympathetic mucous glands. Intranasal ipratropium 0.03% (Atrovent 0.03%) should be considered first-line if the dominant symptom is rhinorrhea. Higher-dose ipratropium 0.06% is approved for rhinorrhea related to the common cold or allergic rhinitis. Because it is used topically, little is absorbed. Its major side effect is nasal dryness.
Decongestants, either oral or topical, can relieve the symptoms of congestion and rhinorrhea in nonallergic rhinitis. They should only be used short-term, as there is little evidence to support their chronic use.
Phenylpropanolamine, a decongestant previously found in over-the-counter cough medicines, was withdrawn from the market in 2000 owing to concern that the drug, especially when used for weight suppression, was linked to hemorrhagic stroke in young women.26,27 Other oral decongestants, ie, pseudoephedrine and phenylephrine, are still available, but there are no definitive guidelines for their use. Their side effects include tachycardia, increase in blood pressure, and insomnia.
Nasal saline irrigation has been used for centuries to treat rhinitis and sinusitis, despite limited evidence of benefit. A Cochrane review concluded that saline irrigation was well tolerated, had minor side effects, and could provide some relief of rhinosinusitis symptoms either as the sole therapeutic measure or as adjunctive treatment.28 Hypertonic saline solutions, while possibly more effective than isotonic saline in improving mucociliary clearance, are not as well tolerated since they can cause nasal burning and irritation. Presumed benefits of saline irrigation are clearance of nasal secretions, improvement of nasociliary function, and removal of irritants and pollen from the nose.
A strategy
Imaging the sinuses with CT, which has replaced standard nasal radiography, may help if one is concerned about chronic rhinosinusitis, nasal polyps, or other anatomic condition that could contribute to persistent symptoms. Cost and radiation exposure should enter into the decision to obtain this study because a diagnosis based on the patient’s report of symptoms may be equally accurate.29,30
CASE CONTINUED
Our patient has a number of potential causes of her symptoms. Exposure to second-hand tobacco smoke at home and to the air in airplanes could be acute triggers. Weather and temperature changes could explain her chronic symptoms in the spring and fall. Use of an angiotensin-converting enzyme inhibitor (in her case, lisinopril) and estrogen replacement therapy may contribute to perennial symptoms, but the onset of her nonallergic rhinitis does not correlate with the use of these drugs. There are no symptoms to suggest chronic rhinosinusitis or anatomic causes of her symptoms.
This case is typical of vasomotor rhinitis of the weather- or temperature-sensitive type. This diagnosis may explain her lack of improvement with intranasal steroids, though adherence and spray technique should be assessed. At this point, we would recommend trying topical antihistamines daily when chronic symptoms are present or as needed for acute symptoms.
- Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122( suppl 2):S1–S84.
- Settipane RA, Charnock DR. Epidemiology of rhinitis: allergic and nonallergic. Clin Allergy Immunol 2007; 19:23–34.
- Settipane RA, Lieberman P. Update on nonallergic rhinitis. Ann Allergy Asthma Immunol 2001; 86:494–507.
- Rondón C, Doña I, Torres MJ, Campo P, Blanca M. Evolution of patients with nonallergic rhinitis supports conversion to allergic rhinitis. J Allergy Clin Immunol 2009; 123:1098–1102.
- Forester JP, Calabria CW. Local production of IgE in the respiratory mucosa and the concept of entopy: does allergy exist in nonallergic rhinitis? Ann Allergy Asthma Immunol 2010; 105:249–255.
- Silvers WS. The skier’s nose: a model of cold-induced rhinorrhea. Ann Allergy 1991; 67:32–36.
- Jaradeh SS, Smith TL, Torrico L, et al. Autonomic nervous system evaluation of patients with vasomotor rhinitis. Laryngoscope 2000; 110:1828–1831.
- Quan M, Casale TB, Blaiss MS. Should clinicians routinely determine rhinitis subtype on initial diagnosis and evaluation? A debate among experts. Clin Cornerstone 2009; 9:54–60.
- Jacobs R, Lieberman P, Kent E, Silvey M, Locantore N, Philpot EE. Weather/temperature-sensitive vasomotor rhinitis may be refractory to intranasal corticosteroid treatment. Allergy Asthma Proc 2009; 30:120–127.
- Monteseirin J, Camacho MJ, Bonilla I, Sanchez-Hernandez C, Hernandez M, Conde J. Honeymoon rhinitis. Allergy 2001; 56:353–354.
- Varghese M, Glaum MC, Lockey RF. Drug-induced rhinitis. Clin Exp Allergy 2010; 40:381–384.
- Schwartz RH, Estroff T, Fairbanks DN, Hoffmann NG. Nasal symptoms associated with cocaine abuse during adolescence. Arch Otolaryngol Head Neck Surg 1989; 115:63–64.
- Meltzer EO, Hamilos DL, Hadley JA, et al; American Academy of Allergy, Asthma and Immunology (AAAAI); American Academy of Otolaryngic Allergy (AAOA); American Academy of Otolaryngology--Head and Neck Surgery (AAO-HNS); American College of Allergy, Asthma and Immunology (ACAAI); American Rhinologic Society (ARS). Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol 2004; 114( suppl 6):155–212.
- Powe DG, Huskisson RS, Carney AS, Jenkins D, Jones NS. Evidence for an inflammatory pathophysiology in idiopathic rhinitis. Clin Exp Allergy 2001; 31:864–872.
- Philpott CM, Robinson AM, Murty GE. Nasal pathophysiology and its relationship to the female ovarian hormones. J Otolaryngol Head Neck Surg 2008; 37:540–546.
- Dykewicz MS, Fineman S, Skoner DP, et al. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma, and Immunology. Ann Allergy Asthma Immunol 1998; 81:478–518.
- Ellegård EK, Karlsson NG, Ellegård LH. Rhinitis in the menstrual cycle, pregnancy, and some endocrine disorders. Clin Allergy Immunol 2007; 19:305–321.
- Dunn CJ, Alaani A, Johnson AP. Study on spontaneous cerebrospinal fluid rhinorrhoea: its aetiology and management. J Laryngol Otol 2005; 119:12–15.
- Bunnag C, Jareoncharsri P, Tansuriyawong P, Bhothisuwan W, Chantarakul N. Characteristics of atrophic rhinitis in Thai patients at the Siriraj Hospital. Rhinology 1999; 37:125–130.
- Dutt SN, Kameswaran M. The aetiology and management of atrophic rhinitis. J Laryngol Otol 2005; 119:843–852.
- deShazo RD, Stringer SP. Atrophic rhinosinusitis: progress toward explanation of an unsolved medical mystery. Curr Opin Allergy Clin Immunol 2011; 11:1–7.
- Greiner AN, Meltzer EO. Overview of the treatment of allergic rhinitis and nonallergic rhinopathy. Proc Am Thorac Soc 2011; 8:121–131.
- Corren J. Intranasal corticosteroids for allergic rhinitis: how do different agents compare? J Allergy Clin Immunol 1999; 104:S144–S149.
- Lieberman P, Meltzer EO, LaForce CF, Darter AL, Tort MJ. Two-week comparison study of olopatadine hydrochloride nasal spray 0.6% versus azelastine hydrochloride nasal spray 0.1% in patients with vasomotor rhinitis. Allergy Asthma Proc 2011; 32:151–158.
- Bousquet J, Khaltaev N, Cruz AA, et al; World Health Organization; GA(2)LEN. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008; 63( suppl 86):8–160.
- SoRelle R. FDA warns of stroke risk associated with phenylpropanolamine; cold remedies and drugs removed from store shelves. Circulation 2000; 102:E9041–E9043.
- Kernan WN, Viscoli CM, Brass LM, et al. Phenylpropanolamine and the risk of hemorrhagic stroke. N Engl J Med 2000; 343:1826–1832.
- Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 2007;CD006394.
- Bhattacharyya N. The role of CT and MRI in the diagnosis of chronic rhinosinusitis. Curr Allergy Asthma Rep 2010; 10:171–174.
- Kenny TJ, Duncavage J, Bracikowski J, Yildirim A, Murray JJ, Tanner SB. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg 2001; 125:40–43.
A 55-year-old woman has come to the clinic because of clear rhinorrhea and nasal congestion, which occur year-round but are worse in the winter. She reports that at times her nose runs continuously. Nasal symptoms have been present for 4 to 5 years but are worsening. The clear discharge is not associated with sneezing or itching. Though she lives with a cat, her symptoms are not exacerbated by close contact with it.
One year ago, an allergist performed skin testing but found no evidence of allergies as a cause of her rhinitis. A short course of intranasal steroids did not seem to improve her nasal symptoms.
The patient also has hypertension, hypothyroidism, and hot flashes due to menopause; these conditions are well controlled with lisinopril (Zestril), levothyroxine (Synthroid), and estrogen replacement. She has no history of asthma and has had no allergies to drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs.)
How should this patient be evaluated and treated?
COMMON, OFTEN OVERLOOKED
Many patients suffer from rhinitis, but this problem can be overshadowed by other chronic diseases seen in a medical clinic, especially during a brief office visit. When a patient presents with rhinitis, a key question is whether it is allergic or nonallergic.
This review will discuss the different forms of nonallergic rhinitis and their causes, and give recommendations about therapy.
RHINITIS: ALLERGIC OR NONALLERGIC?
While allergic rhinitis affects 30 and 60 million Americans annually, or between 10% to 30% of US adults,1 how many have nonallergic rhinitis has been difficult to determine.
In a study in allergy clinics, 23% of patients with rhinitis had the nonallergic form, 43% had the allergic form, and 34% had both forms (mixed rhinitis).2 Other studies have suggested that up to 52% of patients presenting to allergy clinics with rhinitis have nonallergic rhinitis.3
Over time, patients may not stay in the same category. One study found that 24% of patients originally diagnosed with nonallergic rhinitis developed positive allergy tests when retested 3 or more years after their initial evaluation.4
Regardless of the type, untreated or uncontrolled symptoms of rhinitis can significantly affect the quality of life.
All forms of rhinitis are characterized by one or more of the following symptoms: nasal congestion, clear rhinorrhea, sneezing, and itching. These symptoms can be episodic or chronic and can range from mild to debilitating. In addition, rhinitis can lead to systemic symptoms of fatigue, headache, sleep disturbance, and cognitive impairment and can be associated with respiratory symptoms such as sinusitis and asthma.1
Mechanisms are mostly unknown
While allergic rhinitis leads to symptoms when airborne allergens bind with specific immunoglobulin E (IgE) in the nose, the etiology of most forms of nonallergic rhinitis is unknown. However, several mechanisms have been proposed. These include entopy (local nasal IgE synthesis with negative skin tests),5 nocioceptive dysfunction (hyperactive sensory receptors),6 and autonomic nervous system abnormalities (hypoactive or hyperactive dysfunction of sympathetic or parasympathetic nerves in the nose).7
Does this patient have an allergic cause of rhinitis?
When considering a patient with rhinitis, the most important question is, “Does this patient have an allergic cause of rhinitis?” Allergic and nonallergic rhinitis have similar symptoms, making them difficult to distinguish. However, their mechanisms and treatment differ. By categorizing a patient’s type of rhinitis, the physician can make specific recommendations for avoidance and can initiate treatment with the most appropriate therapy. Misclassification can lead to treatment failure, multiple visits, poor adherence, and frustration for patients with uncontrolled symptoms.
Patients for whom an allergic cause cannot be found by allergy skin testing or serum specific IgE immunoassay (Immunocap/RAST) for environmental aeroallergens are classified as having nonallergic rhinitis.
CLUES POINTING TO NONALLERGIC VS ALLERGIC RHINITIS
Nonallergic rhinitis encompasses a range of syndromes with overlapping symptoms. While tools such as the Rhinitis Diagnostic Worksheet are available to help differentiate allergic from nonallergic rhinitis, debate continues about whether it is necessary to characterize different forms of rhinitis before initiating treatment.8
The diagnosis of nonallergic rhinitis depends on a thorough history and physical examination. Key questions relate to the triggers that bring on the rhinitis, which will assist the clinician in determining which subtype of rhinitis a patient may be experiencing and therefore how to manage it. Clues:
- Patients with nonallergic rhinitis more often report nasal congestion and rhinorrhea, rather than sneezing and itching, which are predominant symptoms of allergic rhinitis.
- Patients with nonallergic rhinitis tend to develop symptoms at a later age.
- Common triggers of nonallergic rhinitis are changes in weather and temperature, food, perfumes, odors, smoke, and fumes. Animal exposure does not lead to symptoms.
- Patients with nonallergic rhinitis have few complaints of concomitant symptoms of allergic conjunctivitis (itching, watering, redness, and swelling).
- Many patients with nonallergic rhinitis find that antihistamines have no benefit. Also, they do not have other atopic diseases such as eczema or food allergies and have no family history of atopy.
PHYSICAL FINDINGS
Some findings on physical examination may help distinguish allergic from nonallergic rhinitis.
- Patients with long-standing allergic rhinitis may have an “allergic crease,” ie, a horizontal wrinkle near the tip of the nose caused by frequent upward wiping. Another sign may be a gothic arch, which is a narrowing of the hard palate occurring as a child.
- In allergic rhinitis, the turbinates are often pale, moist, and boggy with a bluish tinge.
CASE CONTINUED
Our patient’s symptoms can be caused by many different factors. Allergic triggers for rhinitis include both indoor and outdoor sources. The most common allergens include cat, dog, dust mite, cockroach, mold, and pollen allergens. The absence of acute sneezing and itching when around her cat and her recent negative skin-prick tests confirm that the rhinitis symptoms are not allergic.
In this patient, who has symptoms throughout the year but no allergic triggers, consideration of the different subtypes of nonallergic rhinitis may help guide further therapy.
SUBTYPES OF NONALLERGIC RHINITIS
Vasomotor rhinitis
Vasomotor rhinitis is thought to be caused by a variety of neural and vascular triggers, often without an inflammatory cause. These triggers lead to symptoms involving nasal congestion and clear rhinorrhea more than sneezing and itching. The symptoms can be sporadic, with acute onset in relation to identifiable nonallergic triggers, or chronic, with no clear trigger.
Gustatory rhinitis, for example, is a form of vasomotor rhinitis in which clear rhinorrhea occurs suddenly while eating or while drinking alcohol. It may be prevented by using nasal ipratropium (Atrovent) before meals.
Irritant-sensitive vasomotor rhinitis. In some patients, acute vasomotor rhinitis symptoms are brought on by strong odors, cigarette smoke, air pollution, or perfume. When asked, most patients easily identify which of these irritant triggers cause symptoms.
Weather- or temperature-sensitive vasomotor rhinitis. In other patients, a change in temperature, humidity, or barometric pressure or exposure to cold or dry air can cause nasal symptoms.9 These triggers are often hard to identify. Weather- or temperature-sensitive vasomotor rhinitis is often mistaken for seasonal allergic rhinitis because weather changes occur in close relation to the peak allergy seasons in the spring and fall. However, this subtype does not respond as well to intranasal steroids.9
Other nonallergic triggers of vasomotor rhinitis may include exercise, emotion, and sexual arousal (honeymoon rhinitis).10
Some triggers, such as tobacco smoke and perfume, are easy to avoid. Other triggers, such as weather changes, are unavoidable. If avoidance measures fail or are inadequate, medications (described below) can be used for prophylaxis and symptomatic treatment.
Drug-induced rhinitis
Drugs of various classes are known to cause either acute or chronic rhinitis. Drug-induced rhinitis has been divided into different types based on the mechanism involved.11
The local inflammatory type occurs in aspirin-exacerbated respiratory disease, which is characterized by nasal polyposis with chronic rhinosinusitis, hyposmia, and moderate to severe persistent asthma. Aspirin and other NSAIDs induce an acute local inflammation, leading to severe rhinitis and asthma symptoms. Avoiding all NSAID products is recommended; aspirin desensitization may lead to improvement in rhinosinusitis and asthma control.
The neurogenic type of drug-induced rhinitis can occur with sympatholytic drugs such as alpha receptor agonists (eg, clonidine [Cat-apres]) and antagonists (eg, prazosin [Minipress]).11 Vasodilators, including phosphodiesterase-5 inhibitors such as sildenafil (Viagra), can lead to acute rhinitis symptoms (“anniversary rhinitis”).
Unknown mechanisms. Many other medications can lead to rhinitis by unknown mechanisms, usually with normal findings on physical examination. These include beta-blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, exogenous estrogens, oral contraceptives, antipsychotics, and gabapentin (Neurontin).
Correlating the initiation of a drug with the onset of rhinitis can help identify offending medications. Stopping the suspected medication, if feasible, is the first-line treatment.
Rhinitis medicamentosa, typically caused by overuse of over-the-counter topical nasal decongestants, is also classified under drug-induced rhinitis. Patients may not think of nasal decongestants as medications, and the physician may need to ask specifically about their use.
On examination, the nasal mucosa appears beefy red without mucous. Once a diagnosis is made, the physician should identify and treat the original etiology of the nasal congestion that led the patient to self-treat.
Patients with rhinitis medicamentosa often have difficulty discontinuing use of topical decongestants. They should be educated that the withdrawal symptoms can be severe and that more than one attempt at quitting may be needed. To break the cycle of rebound congestion, topical intranasal steroids should be used, though 5 to 7 days of oral steroids may be necessary.1
Cocaine is a potent vasoconstrictor. Its illicit use should be suspected, especially if the patient presents with symptoms of chronic irritation such as frequent nosebleeds, crusting, and scabbing.12
Infectious rhinitis
One of the most common causes of acute rhinitis is upper respiratory infection.
Acute viral upper respiratory infection often presents with thick nasal discharge, sneezing, and nasal obstruction that usually clears in 7 to 10 days but can last up to 3 weeks. Acute bacterial sinusitis can follow, typically in fewer than 2% of patients, with symptoms of persistent nasal congestion, discolored mucus, facial pain, cough, and sometimes fever.
Chronic rhinosinusitis is a syndrome with sinus mucosal inflammation with multiple causes. It is clinically defined as persistent nasal and sinus symptoms lasting longer than 12 weeks and confirmed with computed tomography (CT).13 The CT findings of chronic rhinosinusitis include thickening of the lining of the sinus cavities or complete opacification of the pneumatized sinuses.
Major symptoms to consider for diagnosis include facial pain, congestion, obstruction, purulent discharge on examination, and changes in olfaction. Minor symptoms are cough, fatigue, headache, halitosis, fever, ear symptoms, and dental pain.
Treatment may involve 3 or more weeks of an oral antibiotic and a short course of an oral steroid, a daily nasal steroid spray, or both oral and nasal steroids. Most patients can be managed in the primary care setting, but they can be referred to an ear, nose, and throat specialist, an allergist, or an immunologist if their symptoms do not respond to initial therapy.
Nonallergic rhinitis eosinophilic syndrome
Patients with nonallergic rhinitis eosinophilic syndrome (NARES) are typically middle-aged and have perennial symptoms of sneezing, itching, and rhinorrhea with intermittent exacerbations. They occasionally have associated hyposmia (impaired sense of smell).1 The diagnosis is made when eosinophils account for more than 5% of cells on a nasal smear and allergy testing is negative.
Patients may develop nasal polyposis and aspirin sensitivity.1 Entopy has been described in some.14
Because of the eosinophilic inflammation, this form of nonallergic rhinitis responds well to intranasal steroids.
Immunologic causes
Systemic diseases can affect the nose and cause variable nasal symptoms that can be mistaken for rhinitis. Wegener granulomatosis, sarcoidosis, relapsing polychondritis, midline granulomas, Churg-Strauss syndrome, and amyloidosis can all affect the structures in the nose even before manifesting systemic symptoms. Granulomatous infections in the nose may lead to crusting, bleeding, and nasal obstruction.1
A lack of a response to intranasal steroids or oral antibiotics should lead to consideration of these conditions, and treatment should be tailored to the specific disease.
Occupational rhinitis
Occupational exposure to chemicals, biologic aerosols, flour, and latex can lead to rhinitis, typically through an inflammatory mechanism. Many patients present with associated occupational asthma. The symptoms improve when the patient is away from work and worsen throughout the work week.
Avoiding the triggering agent is necessary to treat these symptoms.
Hormonal rhinitis
Hormonal rhinitis, ie, rhinitis related to metabolic and endocrine conditions, is most commonly associated with high estrogen states. Nasal congestion has been reported with pregnancy, menses, menarche, and the use of oral contraceptives.15 The mechanism for congestion in these conditions still needs clarification.
When considering drug therapy, only intranasal budesonide (Rhinocort) has a pregnancy category B rating.
While hypothyroidism and acromegaly have been mentioned in reviews of nonallergic rhinitis, evidence that these disorders cause nonallergic rhinitis is not strong.16,17
Structurally related rhinitis
Anatomic abnormalities that can cause persistent nasal congestion include nasal septal deviation, turbinate hypertrophy, enlarged adenoids, tumors, and foreign bodies. These can be visualized by simple anterior nasal examination, nasal endoscopy, or radiologic studies. If structural causes lead to impaired quality of life or chronic rhinosinusitis, then consider referral to a specialist for possible surgical treatment.
Clear spontaneous rhinorrhea, with or without trauma, can be caused by cerebrospinal fluid leaking into the nasal cavity.18 A salty, metallic taste in the mouth can be a clue that the fluid is cerebrospinal fluid. A definitive diagnosis of cerebrospinal fluid leak is made by finding beta-2-transferrin in nasal secretions.
Atrophic rhinitis
Atrophic rhinitis is categorized as primary or secondary.
Primary (idiopathic) atrophic rhinitis is characterized by atrophy of the nasal mucosa and mucosal colonization with Klebsiella ozaenae associated with a foul-smelling nasal discharge.19,20 This disorder has been primarily reported in young people who present with nasal obstruction, dryness, crusting, and epistaxis. They are from areas with warm climates, such as the Middle East, Southeast Asia, India, Africa, and the Mediterranean.
Secondary atrophic rhinitis can be a complication of nasal or sinus surgery, trauma, granulomatous disease, or exposure to radiation.21 This disorder is typically diagnosed with nasal endoscopy and treated with daily saline rinses with or without topical antibiotics.21
CASE CONTINUED
Questioned further, our patient says her symptoms are worse when her husband smokes, but that she continues to have congestion and rhinorrhea when he is away on business trips. She notes that her symptoms are often worse on airplanes (dry air with an acute change in barometric pressure), with weather changes, and in cold, dry environments. Symptoms are not induced by eating.
We note that she started taking lisinopril 2 years ago and conjugated equine estrogens 8 years ago. Review of systems reveals no history of facial or head trauma, polyps, or hyposmia.
The rhinitis and congestion are bilateral, and she denies headaches, acid reflux, and conjunctivitis. She has a mild throat-clearing cough that she attributes to postnasal drip.
On physical examination, her blood pressure is 118/76 mm Hg and her pulse is 64. Her turbinates are congested with clear rhinorrhea. The rest of the examination is normal.
AVOID TRIGGERS, PRETREAT BEFORE EXPOSURE
People with known environmental, non-immunologic, and irritant triggers should be reminded to avoid these exposures if possible.
If triggers are unavoidable, patients can pretreat themselves with topical nasal sprays before exposure. For example, if symptoms occur while on airplanes, then intranasal steroids or antihistamine sprays should be used before getting on the plane.
Many drugs available
Fortunately, many effective drugs are available to treat nonallergic rhinitis. These have few adverse effects or drug interactions.
Intranasal steroid sprays are considered first-line therapy, as there are studies demonstrating effectiveness in nonallergic rhinitis.22 Intranasal fluticasone propionate (Flonase) and beclomethasone dipropionate (Beconase AQ) are approved by the US Food and Drug Administration (FDA) for treating nonallergic rhinitis. Intranasal mometasone (Nasonex) is approved for treating nasal polyps.
Nasal steroid sprays are most effective if the dominant nasal symptom is congestion, but they have also shown benefit for rhinorrhea, sneezing, and itching.
Side effects of nasal steroid sprays include nasal irritation (dryness, burning, and stinging) and epistaxis, the latter occurring in 5% to 10% of patients.23
Intranasal antihistamines include azelastine (Astelin, Astepro) and olopatadine (Patanase). They are particularly useful for treating sneezing, congestion, and rhinorrhea.24 Astelin is the only intranasal antihistamine with FDA approval for nonallergic rhinitis.
Side effects of this drug class include bitter taste (with Astelin), sweet taste (with Astepro), headache, and somnolence.
Oral antihistamines such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are now available over the counter, and many patients try them before seeking medical care. These drugs may be helpful for those bothered by sneezing. However, no study has demonstrated their effectiveness for nonallergic rhinitis.25 First-generation antihistamines may help with rhinorrhea via their anticholinergic effects.
Ipratropium, an antimuscarinic agent, decreases secretions by inhibiting the nasal parasympathetic mucous glands. Intranasal ipratropium 0.03% (Atrovent 0.03%) should be considered first-line if the dominant symptom is rhinorrhea. Higher-dose ipratropium 0.06% is approved for rhinorrhea related to the common cold or allergic rhinitis. Because it is used topically, little is absorbed. Its major side effect is nasal dryness.
Decongestants, either oral or topical, can relieve the symptoms of congestion and rhinorrhea in nonallergic rhinitis. They should only be used short-term, as there is little evidence to support their chronic use.
Phenylpropanolamine, a decongestant previously found in over-the-counter cough medicines, was withdrawn from the market in 2000 owing to concern that the drug, especially when used for weight suppression, was linked to hemorrhagic stroke in young women.26,27 Other oral decongestants, ie, pseudoephedrine and phenylephrine, are still available, but there are no definitive guidelines for their use. Their side effects include tachycardia, increase in blood pressure, and insomnia.
Nasal saline irrigation has been used for centuries to treat rhinitis and sinusitis, despite limited evidence of benefit. A Cochrane review concluded that saline irrigation was well tolerated, had minor side effects, and could provide some relief of rhinosinusitis symptoms either as the sole therapeutic measure or as adjunctive treatment.28 Hypertonic saline solutions, while possibly more effective than isotonic saline in improving mucociliary clearance, are not as well tolerated since they can cause nasal burning and irritation. Presumed benefits of saline irrigation are clearance of nasal secretions, improvement of nasociliary function, and removal of irritants and pollen from the nose.
A strategy
Imaging the sinuses with CT, which has replaced standard nasal radiography, may help if one is concerned about chronic rhinosinusitis, nasal polyps, or other anatomic condition that could contribute to persistent symptoms. Cost and radiation exposure should enter into the decision to obtain this study because a diagnosis based on the patient’s report of symptoms may be equally accurate.29,30
CASE CONTINUED
Our patient has a number of potential causes of her symptoms. Exposure to second-hand tobacco smoke at home and to the air in airplanes could be acute triggers. Weather and temperature changes could explain her chronic symptoms in the spring and fall. Use of an angiotensin-converting enzyme inhibitor (in her case, lisinopril) and estrogen replacement therapy may contribute to perennial symptoms, but the onset of her nonallergic rhinitis does not correlate with the use of these drugs. There are no symptoms to suggest chronic rhinosinusitis or anatomic causes of her symptoms.
This case is typical of vasomotor rhinitis of the weather- or temperature-sensitive type. This diagnosis may explain her lack of improvement with intranasal steroids, though adherence and spray technique should be assessed. At this point, we would recommend trying topical antihistamines daily when chronic symptoms are present or as needed for acute symptoms.
A 55-year-old woman has come to the clinic because of clear rhinorrhea and nasal congestion, which occur year-round but are worse in the winter. She reports that at times her nose runs continuously. Nasal symptoms have been present for 4 to 5 years but are worsening. The clear discharge is not associated with sneezing or itching. Though she lives with a cat, her symptoms are not exacerbated by close contact with it.
One year ago, an allergist performed skin testing but found no evidence of allergies as a cause of her rhinitis. A short course of intranasal steroids did not seem to improve her nasal symptoms.
The patient also has hypertension, hypothyroidism, and hot flashes due to menopause; these conditions are well controlled with lisinopril (Zestril), levothyroxine (Synthroid), and estrogen replacement. She has no history of asthma and has had no allergies to drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs.)
How should this patient be evaluated and treated?
COMMON, OFTEN OVERLOOKED
Many patients suffer from rhinitis, but this problem can be overshadowed by other chronic diseases seen in a medical clinic, especially during a brief office visit. When a patient presents with rhinitis, a key question is whether it is allergic or nonallergic.
This review will discuss the different forms of nonallergic rhinitis and their causes, and give recommendations about therapy.
RHINITIS: ALLERGIC OR NONALLERGIC?
While allergic rhinitis affects 30 and 60 million Americans annually, or between 10% to 30% of US adults,1 how many have nonallergic rhinitis has been difficult to determine.
In a study in allergy clinics, 23% of patients with rhinitis had the nonallergic form, 43% had the allergic form, and 34% had both forms (mixed rhinitis).2 Other studies have suggested that up to 52% of patients presenting to allergy clinics with rhinitis have nonallergic rhinitis.3
Over time, patients may not stay in the same category. One study found that 24% of patients originally diagnosed with nonallergic rhinitis developed positive allergy tests when retested 3 or more years after their initial evaluation.4
Regardless of the type, untreated or uncontrolled symptoms of rhinitis can significantly affect the quality of life.
All forms of rhinitis are characterized by one or more of the following symptoms: nasal congestion, clear rhinorrhea, sneezing, and itching. These symptoms can be episodic or chronic and can range from mild to debilitating. In addition, rhinitis can lead to systemic symptoms of fatigue, headache, sleep disturbance, and cognitive impairment and can be associated with respiratory symptoms such as sinusitis and asthma.1
Mechanisms are mostly unknown
While allergic rhinitis leads to symptoms when airborne allergens bind with specific immunoglobulin E (IgE) in the nose, the etiology of most forms of nonallergic rhinitis is unknown. However, several mechanisms have been proposed. These include entopy (local nasal IgE synthesis with negative skin tests),5 nocioceptive dysfunction (hyperactive sensory receptors),6 and autonomic nervous system abnormalities (hypoactive or hyperactive dysfunction of sympathetic or parasympathetic nerves in the nose).7
Does this patient have an allergic cause of rhinitis?
When considering a patient with rhinitis, the most important question is, “Does this patient have an allergic cause of rhinitis?” Allergic and nonallergic rhinitis have similar symptoms, making them difficult to distinguish. However, their mechanisms and treatment differ. By categorizing a patient’s type of rhinitis, the physician can make specific recommendations for avoidance and can initiate treatment with the most appropriate therapy. Misclassification can lead to treatment failure, multiple visits, poor adherence, and frustration for patients with uncontrolled symptoms.
Patients for whom an allergic cause cannot be found by allergy skin testing or serum specific IgE immunoassay (Immunocap/RAST) for environmental aeroallergens are classified as having nonallergic rhinitis.
CLUES POINTING TO NONALLERGIC VS ALLERGIC RHINITIS
Nonallergic rhinitis encompasses a range of syndromes with overlapping symptoms. While tools such as the Rhinitis Diagnostic Worksheet are available to help differentiate allergic from nonallergic rhinitis, debate continues about whether it is necessary to characterize different forms of rhinitis before initiating treatment.8
The diagnosis of nonallergic rhinitis depends on a thorough history and physical examination. Key questions relate to the triggers that bring on the rhinitis, which will assist the clinician in determining which subtype of rhinitis a patient may be experiencing and therefore how to manage it. Clues:
- Patients with nonallergic rhinitis more often report nasal congestion and rhinorrhea, rather than sneezing and itching, which are predominant symptoms of allergic rhinitis.
- Patients with nonallergic rhinitis tend to develop symptoms at a later age.
- Common triggers of nonallergic rhinitis are changes in weather and temperature, food, perfumes, odors, smoke, and fumes. Animal exposure does not lead to symptoms.
- Patients with nonallergic rhinitis have few complaints of concomitant symptoms of allergic conjunctivitis (itching, watering, redness, and swelling).
- Many patients with nonallergic rhinitis find that antihistamines have no benefit. Also, they do not have other atopic diseases such as eczema or food allergies and have no family history of atopy.
PHYSICAL FINDINGS
Some findings on physical examination may help distinguish allergic from nonallergic rhinitis.
- Patients with long-standing allergic rhinitis may have an “allergic crease,” ie, a horizontal wrinkle near the tip of the nose caused by frequent upward wiping. Another sign may be a gothic arch, which is a narrowing of the hard palate occurring as a child.
- In allergic rhinitis, the turbinates are often pale, moist, and boggy with a bluish tinge.
CASE CONTINUED
Our patient’s symptoms can be caused by many different factors. Allergic triggers for rhinitis include both indoor and outdoor sources. The most common allergens include cat, dog, dust mite, cockroach, mold, and pollen allergens. The absence of acute sneezing and itching when around her cat and her recent negative skin-prick tests confirm that the rhinitis symptoms are not allergic.
In this patient, who has symptoms throughout the year but no allergic triggers, consideration of the different subtypes of nonallergic rhinitis may help guide further therapy.
SUBTYPES OF NONALLERGIC RHINITIS
Vasomotor rhinitis
Vasomotor rhinitis is thought to be caused by a variety of neural and vascular triggers, often without an inflammatory cause. These triggers lead to symptoms involving nasal congestion and clear rhinorrhea more than sneezing and itching. The symptoms can be sporadic, with acute onset in relation to identifiable nonallergic triggers, or chronic, with no clear trigger.
Gustatory rhinitis, for example, is a form of vasomotor rhinitis in which clear rhinorrhea occurs suddenly while eating or while drinking alcohol. It may be prevented by using nasal ipratropium (Atrovent) before meals.
Irritant-sensitive vasomotor rhinitis. In some patients, acute vasomotor rhinitis symptoms are brought on by strong odors, cigarette smoke, air pollution, or perfume. When asked, most patients easily identify which of these irritant triggers cause symptoms.
Weather- or temperature-sensitive vasomotor rhinitis. In other patients, a change in temperature, humidity, or barometric pressure or exposure to cold or dry air can cause nasal symptoms.9 These triggers are often hard to identify. Weather- or temperature-sensitive vasomotor rhinitis is often mistaken for seasonal allergic rhinitis because weather changes occur in close relation to the peak allergy seasons in the spring and fall. However, this subtype does not respond as well to intranasal steroids.9
Other nonallergic triggers of vasomotor rhinitis may include exercise, emotion, and sexual arousal (honeymoon rhinitis).10
Some triggers, such as tobacco smoke and perfume, are easy to avoid. Other triggers, such as weather changes, are unavoidable. If avoidance measures fail or are inadequate, medications (described below) can be used for prophylaxis and symptomatic treatment.
Drug-induced rhinitis
Drugs of various classes are known to cause either acute or chronic rhinitis. Drug-induced rhinitis has been divided into different types based on the mechanism involved.11
The local inflammatory type occurs in aspirin-exacerbated respiratory disease, which is characterized by nasal polyposis with chronic rhinosinusitis, hyposmia, and moderate to severe persistent asthma. Aspirin and other NSAIDs induce an acute local inflammation, leading to severe rhinitis and asthma symptoms. Avoiding all NSAID products is recommended; aspirin desensitization may lead to improvement in rhinosinusitis and asthma control.
The neurogenic type of drug-induced rhinitis can occur with sympatholytic drugs such as alpha receptor agonists (eg, clonidine [Cat-apres]) and antagonists (eg, prazosin [Minipress]).11 Vasodilators, including phosphodiesterase-5 inhibitors such as sildenafil (Viagra), can lead to acute rhinitis symptoms (“anniversary rhinitis”).
Unknown mechanisms. Many other medications can lead to rhinitis by unknown mechanisms, usually with normal findings on physical examination. These include beta-blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, exogenous estrogens, oral contraceptives, antipsychotics, and gabapentin (Neurontin).
Correlating the initiation of a drug with the onset of rhinitis can help identify offending medications. Stopping the suspected medication, if feasible, is the first-line treatment.
Rhinitis medicamentosa, typically caused by overuse of over-the-counter topical nasal decongestants, is also classified under drug-induced rhinitis. Patients may not think of nasal decongestants as medications, and the physician may need to ask specifically about their use.
On examination, the nasal mucosa appears beefy red without mucous. Once a diagnosis is made, the physician should identify and treat the original etiology of the nasal congestion that led the patient to self-treat.
Patients with rhinitis medicamentosa often have difficulty discontinuing use of topical decongestants. They should be educated that the withdrawal symptoms can be severe and that more than one attempt at quitting may be needed. To break the cycle of rebound congestion, topical intranasal steroids should be used, though 5 to 7 days of oral steroids may be necessary.1
Cocaine is a potent vasoconstrictor. Its illicit use should be suspected, especially if the patient presents with symptoms of chronic irritation such as frequent nosebleeds, crusting, and scabbing.12
Infectious rhinitis
One of the most common causes of acute rhinitis is upper respiratory infection.
Acute viral upper respiratory infection often presents with thick nasal discharge, sneezing, and nasal obstruction that usually clears in 7 to 10 days but can last up to 3 weeks. Acute bacterial sinusitis can follow, typically in fewer than 2% of patients, with symptoms of persistent nasal congestion, discolored mucus, facial pain, cough, and sometimes fever.
Chronic rhinosinusitis is a syndrome with sinus mucosal inflammation with multiple causes. It is clinically defined as persistent nasal and sinus symptoms lasting longer than 12 weeks and confirmed with computed tomography (CT).13 The CT findings of chronic rhinosinusitis include thickening of the lining of the sinus cavities or complete opacification of the pneumatized sinuses.
Major symptoms to consider for diagnosis include facial pain, congestion, obstruction, purulent discharge on examination, and changes in olfaction. Minor symptoms are cough, fatigue, headache, halitosis, fever, ear symptoms, and dental pain.
Treatment may involve 3 or more weeks of an oral antibiotic and a short course of an oral steroid, a daily nasal steroid spray, or both oral and nasal steroids. Most patients can be managed in the primary care setting, but they can be referred to an ear, nose, and throat specialist, an allergist, or an immunologist if their symptoms do not respond to initial therapy.
Nonallergic rhinitis eosinophilic syndrome
Patients with nonallergic rhinitis eosinophilic syndrome (NARES) are typically middle-aged and have perennial symptoms of sneezing, itching, and rhinorrhea with intermittent exacerbations. They occasionally have associated hyposmia (impaired sense of smell).1 The diagnosis is made when eosinophils account for more than 5% of cells on a nasal smear and allergy testing is negative.
Patients may develop nasal polyposis and aspirin sensitivity.1 Entopy has been described in some.14
Because of the eosinophilic inflammation, this form of nonallergic rhinitis responds well to intranasal steroids.
Immunologic causes
Systemic diseases can affect the nose and cause variable nasal symptoms that can be mistaken for rhinitis. Wegener granulomatosis, sarcoidosis, relapsing polychondritis, midline granulomas, Churg-Strauss syndrome, and amyloidosis can all affect the structures in the nose even before manifesting systemic symptoms. Granulomatous infections in the nose may lead to crusting, bleeding, and nasal obstruction.1
A lack of a response to intranasal steroids or oral antibiotics should lead to consideration of these conditions, and treatment should be tailored to the specific disease.
Occupational rhinitis
Occupational exposure to chemicals, biologic aerosols, flour, and latex can lead to rhinitis, typically through an inflammatory mechanism. Many patients present with associated occupational asthma. The symptoms improve when the patient is away from work and worsen throughout the work week.
Avoiding the triggering agent is necessary to treat these symptoms.
Hormonal rhinitis
Hormonal rhinitis, ie, rhinitis related to metabolic and endocrine conditions, is most commonly associated with high estrogen states. Nasal congestion has been reported with pregnancy, menses, menarche, and the use of oral contraceptives.15 The mechanism for congestion in these conditions still needs clarification.
When considering drug therapy, only intranasal budesonide (Rhinocort) has a pregnancy category B rating.
While hypothyroidism and acromegaly have been mentioned in reviews of nonallergic rhinitis, evidence that these disorders cause nonallergic rhinitis is not strong.16,17
Structurally related rhinitis
Anatomic abnormalities that can cause persistent nasal congestion include nasal septal deviation, turbinate hypertrophy, enlarged adenoids, tumors, and foreign bodies. These can be visualized by simple anterior nasal examination, nasal endoscopy, or radiologic studies. If structural causes lead to impaired quality of life or chronic rhinosinusitis, then consider referral to a specialist for possible surgical treatment.
Clear spontaneous rhinorrhea, with or without trauma, can be caused by cerebrospinal fluid leaking into the nasal cavity.18 A salty, metallic taste in the mouth can be a clue that the fluid is cerebrospinal fluid. A definitive diagnosis of cerebrospinal fluid leak is made by finding beta-2-transferrin in nasal secretions.
Atrophic rhinitis
Atrophic rhinitis is categorized as primary or secondary.
Primary (idiopathic) atrophic rhinitis is characterized by atrophy of the nasal mucosa and mucosal colonization with Klebsiella ozaenae associated with a foul-smelling nasal discharge.19,20 This disorder has been primarily reported in young people who present with nasal obstruction, dryness, crusting, and epistaxis. They are from areas with warm climates, such as the Middle East, Southeast Asia, India, Africa, and the Mediterranean.
Secondary atrophic rhinitis can be a complication of nasal or sinus surgery, trauma, granulomatous disease, or exposure to radiation.21 This disorder is typically diagnosed with nasal endoscopy and treated with daily saline rinses with or without topical antibiotics.21
CASE CONTINUED
Questioned further, our patient says her symptoms are worse when her husband smokes, but that she continues to have congestion and rhinorrhea when he is away on business trips. She notes that her symptoms are often worse on airplanes (dry air with an acute change in barometric pressure), with weather changes, and in cold, dry environments. Symptoms are not induced by eating.
We note that she started taking lisinopril 2 years ago and conjugated equine estrogens 8 years ago. Review of systems reveals no history of facial or head trauma, polyps, or hyposmia.
The rhinitis and congestion are bilateral, and she denies headaches, acid reflux, and conjunctivitis. She has a mild throat-clearing cough that she attributes to postnasal drip.
On physical examination, her blood pressure is 118/76 mm Hg and her pulse is 64. Her turbinates are congested with clear rhinorrhea. The rest of the examination is normal.
AVOID TRIGGERS, PRETREAT BEFORE EXPOSURE
People with known environmental, non-immunologic, and irritant triggers should be reminded to avoid these exposures if possible.
If triggers are unavoidable, patients can pretreat themselves with topical nasal sprays before exposure. For example, if symptoms occur while on airplanes, then intranasal steroids or antihistamine sprays should be used before getting on the plane.
Many drugs available
Fortunately, many effective drugs are available to treat nonallergic rhinitis. These have few adverse effects or drug interactions.
Intranasal steroid sprays are considered first-line therapy, as there are studies demonstrating effectiveness in nonallergic rhinitis.22 Intranasal fluticasone propionate (Flonase) and beclomethasone dipropionate (Beconase AQ) are approved by the US Food and Drug Administration (FDA) for treating nonallergic rhinitis. Intranasal mometasone (Nasonex) is approved for treating nasal polyps.
Nasal steroid sprays are most effective if the dominant nasal symptom is congestion, but they have also shown benefit for rhinorrhea, sneezing, and itching.
Side effects of nasal steroid sprays include nasal irritation (dryness, burning, and stinging) and epistaxis, the latter occurring in 5% to 10% of patients.23
Intranasal antihistamines include azelastine (Astelin, Astepro) and olopatadine (Patanase). They are particularly useful for treating sneezing, congestion, and rhinorrhea.24 Astelin is the only intranasal antihistamine with FDA approval for nonallergic rhinitis.
Side effects of this drug class include bitter taste (with Astelin), sweet taste (with Astepro), headache, and somnolence.
Oral antihistamines such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are now available over the counter, and many patients try them before seeking medical care. These drugs may be helpful for those bothered by sneezing. However, no study has demonstrated their effectiveness for nonallergic rhinitis.25 First-generation antihistamines may help with rhinorrhea via their anticholinergic effects.
Ipratropium, an antimuscarinic agent, decreases secretions by inhibiting the nasal parasympathetic mucous glands. Intranasal ipratropium 0.03% (Atrovent 0.03%) should be considered first-line if the dominant symptom is rhinorrhea. Higher-dose ipratropium 0.06% is approved for rhinorrhea related to the common cold or allergic rhinitis. Because it is used topically, little is absorbed. Its major side effect is nasal dryness.
Decongestants, either oral or topical, can relieve the symptoms of congestion and rhinorrhea in nonallergic rhinitis. They should only be used short-term, as there is little evidence to support their chronic use.
Phenylpropanolamine, a decongestant previously found in over-the-counter cough medicines, was withdrawn from the market in 2000 owing to concern that the drug, especially when used for weight suppression, was linked to hemorrhagic stroke in young women.26,27 Other oral decongestants, ie, pseudoephedrine and phenylephrine, are still available, but there are no definitive guidelines for their use. Their side effects include tachycardia, increase in blood pressure, and insomnia.
Nasal saline irrigation has been used for centuries to treat rhinitis and sinusitis, despite limited evidence of benefit. A Cochrane review concluded that saline irrigation was well tolerated, had minor side effects, and could provide some relief of rhinosinusitis symptoms either as the sole therapeutic measure or as adjunctive treatment.28 Hypertonic saline solutions, while possibly more effective than isotonic saline in improving mucociliary clearance, are not as well tolerated since they can cause nasal burning and irritation. Presumed benefits of saline irrigation are clearance of nasal secretions, improvement of nasociliary function, and removal of irritants and pollen from the nose.
A strategy
Imaging the sinuses with CT, which has replaced standard nasal radiography, may help if one is concerned about chronic rhinosinusitis, nasal polyps, or other anatomic condition that could contribute to persistent symptoms. Cost and radiation exposure should enter into the decision to obtain this study because a diagnosis based on the patient’s report of symptoms may be equally accurate.29,30
CASE CONTINUED
Our patient has a number of potential causes of her symptoms. Exposure to second-hand tobacco smoke at home and to the air in airplanes could be acute triggers. Weather and temperature changes could explain her chronic symptoms in the spring and fall. Use of an angiotensin-converting enzyme inhibitor (in her case, lisinopril) and estrogen replacement therapy may contribute to perennial symptoms, but the onset of her nonallergic rhinitis does not correlate with the use of these drugs. There are no symptoms to suggest chronic rhinosinusitis or anatomic causes of her symptoms.
This case is typical of vasomotor rhinitis of the weather- or temperature-sensitive type. This diagnosis may explain her lack of improvement with intranasal steroids, though adherence and spray technique should be assessed. At this point, we would recommend trying topical antihistamines daily when chronic symptoms are present or as needed for acute symptoms.
- Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122( suppl 2):S1–S84.
- Settipane RA, Charnock DR. Epidemiology of rhinitis: allergic and nonallergic. Clin Allergy Immunol 2007; 19:23–34.
- Settipane RA, Lieberman P. Update on nonallergic rhinitis. Ann Allergy Asthma Immunol 2001; 86:494–507.
- Rondón C, Doña I, Torres MJ, Campo P, Blanca M. Evolution of patients with nonallergic rhinitis supports conversion to allergic rhinitis. J Allergy Clin Immunol 2009; 123:1098–1102.
- Forester JP, Calabria CW. Local production of IgE in the respiratory mucosa and the concept of entopy: does allergy exist in nonallergic rhinitis? Ann Allergy Asthma Immunol 2010; 105:249–255.
- Silvers WS. The skier’s nose: a model of cold-induced rhinorrhea. Ann Allergy 1991; 67:32–36.
- Jaradeh SS, Smith TL, Torrico L, et al. Autonomic nervous system evaluation of patients with vasomotor rhinitis. Laryngoscope 2000; 110:1828–1831.
- Quan M, Casale TB, Blaiss MS. Should clinicians routinely determine rhinitis subtype on initial diagnosis and evaluation? A debate among experts. Clin Cornerstone 2009; 9:54–60.
- Jacobs R, Lieberman P, Kent E, Silvey M, Locantore N, Philpot EE. Weather/temperature-sensitive vasomotor rhinitis may be refractory to intranasal corticosteroid treatment. Allergy Asthma Proc 2009; 30:120–127.
- Monteseirin J, Camacho MJ, Bonilla I, Sanchez-Hernandez C, Hernandez M, Conde J. Honeymoon rhinitis. Allergy 2001; 56:353–354.
- Varghese M, Glaum MC, Lockey RF. Drug-induced rhinitis. Clin Exp Allergy 2010; 40:381–384.
- Schwartz RH, Estroff T, Fairbanks DN, Hoffmann NG. Nasal symptoms associated with cocaine abuse during adolescence. Arch Otolaryngol Head Neck Surg 1989; 115:63–64.
- Meltzer EO, Hamilos DL, Hadley JA, et al; American Academy of Allergy, Asthma and Immunology (AAAAI); American Academy of Otolaryngic Allergy (AAOA); American Academy of Otolaryngology--Head and Neck Surgery (AAO-HNS); American College of Allergy, Asthma and Immunology (ACAAI); American Rhinologic Society (ARS). Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol 2004; 114( suppl 6):155–212.
- Powe DG, Huskisson RS, Carney AS, Jenkins D, Jones NS. Evidence for an inflammatory pathophysiology in idiopathic rhinitis. Clin Exp Allergy 2001; 31:864–872.
- Philpott CM, Robinson AM, Murty GE. Nasal pathophysiology and its relationship to the female ovarian hormones. J Otolaryngol Head Neck Surg 2008; 37:540–546.
- Dykewicz MS, Fineman S, Skoner DP, et al. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma, and Immunology. Ann Allergy Asthma Immunol 1998; 81:478–518.
- Ellegård EK, Karlsson NG, Ellegård LH. Rhinitis in the menstrual cycle, pregnancy, and some endocrine disorders. Clin Allergy Immunol 2007; 19:305–321.
- Dunn CJ, Alaani A, Johnson AP. Study on spontaneous cerebrospinal fluid rhinorrhoea: its aetiology and management. J Laryngol Otol 2005; 119:12–15.
- Bunnag C, Jareoncharsri P, Tansuriyawong P, Bhothisuwan W, Chantarakul N. Characteristics of atrophic rhinitis in Thai patients at the Siriraj Hospital. Rhinology 1999; 37:125–130.
- Dutt SN, Kameswaran M. The aetiology and management of atrophic rhinitis. J Laryngol Otol 2005; 119:843–852.
- deShazo RD, Stringer SP. Atrophic rhinosinusitis: progress toward explanation of an unsolved medical mystery. Curr Opin Allergy Clin Immunol 2011; 11:1–7.
- Greiner AN, Meltzer EO. Overview of the treatment of allergic rhinitis and nonallergic rhinopathy. Proc Am Thorac Soc 2011; 8:121–131.
- Corren J. Intranasal corticosteroids for allergic rhinitis: how do different agents compare? J Allergy Clin Immunol 1999; 104:S144–S149.
- Lieberman P, Meltzer EO, LaForce CF, Darter AL, Tort MJ. Two-week comparison study of olopatadine hydrochloride nasal spray 0.6% versus azelastine hydrochloride nasal spray 0.1% in patients with vasomotor rhinitis. Allergy Asthma Proc 2011; 32:151–158.
- Bousquet J, Khaltaev N, Cruz AA, et al; World Health Organization; GA(2)LEN. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008; 63( suppl 86):8–160.
- SoRelle R. FDA warns of stroke risk associated with phenylpropanolamine; cold remedies and drugs removed from store shelves. Circulation 2000; 102:E9041–E9043.
- Kernan WN, Viscoli CM, Brass LM, et al. Phenylpropanolamine and the risk of hemorrhagic stroke. N Engl J Med 2000; 343:1826–1832.
- Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 2007;CD006394.
- Bhattacharyya N. The role of CT and MRI in the diagnosis of chronic rhinosinusitis. Curr Allergy Asthma Rep 2010; 10:171–174.
- Kenny TJ, Duncavage J, Bracikowski J, Yildirim A, Murray JJ, Tanner SB. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg 2001; 125:40–43.
- Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122( suppl 2):S1–S84.
- Settipane RA, Charnock DR. Epidemiology of rhinitis: allergic and nonallergic. Clin Allergy Immunol 2007; 19:23–34.
- Settipane RA, Lieberman P. Update on nonallergic rhinitis. Ann Allergy Asthma Immunol 2001; 86:494–507.
- Rondón C, Doña I, Torres MJ, Campo P, Blanca M. Evolution of patients with nonallergic rhinitis supports conversion to allergic rhinitis. J Allergy Clin Immunol 2009; 123:1098–1102.
- Forester JP, Calabria CW. Local production of IgE in the respiratory mucosa and the concept of entopy: does allergy exist in nonallergic rhinitis? Ann Allergy Asthma Immunol 2010; 105:249–255.
- Silvers WS. The skier’s nose: a model of cold-induced rhinorrhea. Ann Allergy 1991; 67:32–36.
- Jaradeh SS, Smith TL, Torrico L, et al. Autonomic nervous system evaluation of patients with vasomotor rhinitis. Laryngoscope 2000; 110:1828–1831.
- Quan M, Casale TB, Blaiss MS. Should clinicians routinely determine rhinitis subtype on initial diagnosis and evaluation? A debate among experts. Clin Cornerstone 2009; 9:54–60.
- Jacobs R, Lieberman P, Kent E, Silvey M, Locantore N, Philpot EE. Weather/temperature-sensitive vasomotor rhinitis may be refractory to intranasal corticosteroid treatment. Allergy Asthma Proc 2009; 30:120–127.
- Monteseirin J, Camacho MJ, Bonilla I, Sanchez-Hernandez C, Hernandez M, Conde J. Honeymoon rhinitis. Allergy 2001; 56:353–354.
- Varghese M, Glaum MC, Lockey RF. Drug-induced rhinitis. Clin Exp Allergy 2010; 40:381–384.
- Schwartz RH, Estroff T, Fairbanks DN, Hoffmann NG. Nasal symptoms associated with cocaine abuse during adolescence. Arch Otolaryngol Head Neck Surg 1989; 115:63–64.
- Meltzer EO, Hamilos DL, Hadley JA, et al; American Academy of Allergy, Asthma and Immunology (AAAAI); American Academy of Otolaryngic Allergy (AAOA); American Academy of Otolaryngology--Head and Neck Surgery (AAO-HNS); American College of Allergy, Asthma and Immunology (ACAAI); American Rhinologic Society (ARS). Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol 2004; 114( suppl 6):155–212.
- Powe DG, Huskisson RS, Carney AS, Jenkins D, Jones NS. Evidence for an inflammatory pathophysiology in idiopathic rhinitis. Clin Exp Allergy 2001; 31:864–872.
- Philpott CM, Robinson AM, Murty GE. Nasal pathophysiology and its relationship to the female ovarian hormones. J Otolaryngol Head Neck Surg 2008; 37:540–546.
- Dykewicz MS, Fineman S, Skoner DP, et al. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma, and Immunology. Ann Allergy Asthma Immunol 1998; 81:478–518.
- Ellegård EK, Karlsson NG, Ellegård LH. Rhinitis in the menstrual cycle, pregnancy, and some endocrine disorders. Clin Allergy Immunol 2007; 19:305–321.
- Dunn CJ, Alaani A, Johnson AP. Study on spontaneous cerebrospinal fluid rhinorrhoea: its aetiology and management. J Laryngol Otol 2005; 119:12–15.
- Bunnag C, Jareoncharsri P, Tansuriyawong P, Bhothisuwan W, Chantarakul N. Characteristics of atrophic rhinitis in Thai patients at the Siriraj Hospital. Rhinology 1999; 37:125–130.
- Dutt SN, Kameswaran M. The aetiology and management of atrophic rhinitis. J Laryngol Otol 2005; 119:843–852.
- deShazo RD, Stringer SP. Atrophic rhinosinusitis: progress toward explanation of an unsolved medical mystery. Curr Opin Allergy Clin Immunol 2011; 11:1–7.
- Greiner AN, Meltzer EO. Overview of the treatment of allergic rhinitis and nonallergic rhinopathy. Proc Am Thorac Soc 2011; 8:121–131.
- Corren J. Intranasal corticosteroids for allergic rhinitis: how do different agents compare? J Allergy Clin Immunol 1999; 104:S144–S149.
- Lieberman P, Meltzer EO, LaForce CF, Darter AL, Tort MJ. Two-week comparison study of olopatadine hydrochloride nasal spray 0.6% versus azelastine hydrochloride nasal spray 0.1% in patients with vasomotor rhinitis. Allergy Asthma Proc 2011; 32:151–158.
- Bousquet J, Khaltaev N, Cruz AA, et al; World Health Organization; GA(2)LEN. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008; 63( suppl 86):8–160.
- SoRelle R. FDA warns of stroke risk associated with phenylpropanolamine; cold remedies and drugs removed from store shelves. Circulation 2000; 102:E9041–E9043.
- Kernan WN, Viscoli CM, Brass LM, et al. Phenylpropanolamine and the risk of hemorrhagic stroke. N Engl J Med 2000; 343:1826–1832.
- Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 2007;CD006394.
- Bhattacharyya N. The role of CT and MRI in the diagnosis of chronic rhinosinusitis. Curr Allergy Asthma Rep 2010; 10:171–174.
- Kenny TJ, Duncavage J, Bracikowski J, Yildirim A, Murray JJ, Tanner SB. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg 2001; 125:40–43.
KEY POINTS
- When evaluating a patient with rhinitis, a key question is whether it is allergic or nonallergic.
- Identifying triggers that should be avoided is important for controlling symptoms.
- If symptoms continue, then the first-line treatment for nonallergic rhinitis is intranasal steroids.
- Failure of intranasal steroids to control symptoms should prompt a consideration of the many potential causes of rhinitis, and further evaluation and treatment can be tailored accordingly.