User login
THE CASE
A 63-year-old multiparous woman visited her general practitioner because of nausea, vomiting, and general malaise. A proton pump inhibitor was prescribed, which temporarily relieved her symptoms. Two weeks later, however, her symptoms worsened and she was admitted to the hospital.
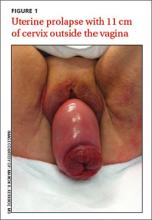
The patient’s physical examination on admission was normal, but laboratory findings revealed severe renal failure with a creatinine level of 7.4 mg/dL (normal, 0.6-1.1 mg/dL), potassium level of 7.4 mmol/L (3.5-5 mmol/L), and a sodium level of 123 mmol/L (135-145 mmol/L). A renal ultrasound revealed severe bilateral hydronephrosis with hydroureteronephrosis caused by obstructive uropathy. A radiologist examined the patient and determined that she had a total uterine prolapse; the cervix was 11 cm outside of the vagina (FIGURE 1). Our patient’s untreated pelvic organ prolapse (POP) had caused chronic renal failure. The patient was referred to a urogynecologist.
Previous attempts at treatment. It appeared that our patient had POP for years and there had been a previous attempt to treat it with a pessary. However, because of an unpleasant experience at her initial appointment and because her biggest complaint (until recently) had been the need to urinate frequently, she had not returned for follow-up appointments.
DISCUSSION
POP is not life-threatening, but the condition lowers the quality of life for 50% of parous women age >50 years.1 It can present as stress urinary incontinence, fecal incontinence, sexual dysfunction, and mechanical problems due to vaginal bulging or pelvic pressure.2 With the exception of vaginal bulging, symptoms are not specific for POP and there is no linear relationship between the severity of the prolapse and the symptoms.3,4
The condition is staged using the POP-Quantification (POP-Q) system5:
1. Stage 0: no prolapse
2. Stage I: the most distal portion of the prolapse is >1 cm above the hymen
3. Stage II: the prolapse is ≤1 cm proximal or distal to the plane of the hymen
4. Stage III: the prolapse is >1 cm below the plane of the hymen, but protrudes no farther
than 2 cm less than the total vaginal length
5. Stage IV: complete eversion of the lower genital tract.
As was the case with our patient, it is possible for a woman with severe total uterine prolapse (Stage IV) to have no major problems with urination or defecation.
The link between POP and hydronephrosis
Hydronephrosis appears to be a frequent finding in women with POP.4 A recent prospective observational study reported an overall prevalence of 10.3% (95% confidence interval, 6%-14%) in women with POP.4 Patients with advanced stages of POP (POP-Q Stage III or IV)4 who also had diabetes mellitus and hypertension were at particularly high risk, with a prevalence of about 20%. An analysis of factors, including age, parity, diabetes, hypertension, and type of prolapse, found that severity of POP was the strongest predictor of hydronephrosis: Patients with a Stage III to IV prolapse are 3.4 times more likely to have hydronephrosis than those with a Stage I or II prolapse.4,6
Possible causes of hydronephrosis in POP patients. Some researchers have proposed that hydronephrosis in patients with uterine prolapse may be due to a kinking of the ureters by the extrinsic compression of the prolapsed uterus. In patients with vaginal vault prolapse, the cause of the hydronephrosis could be a weakening or disintegration of the cardinal ligaments after hysterectomy.4,7
Patients may not complain. When hydronephrosis caused by POP occurs, it may develop slowly, causing little or no discomfort. As time passes, patients may complain of dull pain in the flank, suffer from urinary tract infections, or develop kidney stones before progressive renal dysfunction or renal failure occurs.4
There are 2 other cases in the literature of women who, like our patient, had uterine prolapse that went untreated until they were in renal failure.8,9 The patients noticed only mechanical problems due to the POP; bilateral hydroureteronephrosis and renal failure had developed undetected. In the end, both women needed lifelong hemodialysis.
Treatment options
Treatment options for POP include supervised pelvic floor exercise programs, pessary insertion, or reconstructive pelvic surgery. If POP is treated adequately, an estimated 95% of the hydronephrosis can resolve, regardless of its severity at presentation.4
Our patient was treated with a 95 mm Falk pessary. After 24 hours, renal ultrasonography showed a decrease in both the hydroureteronephrosis and the hydronephrosis (FIGURE 2A and 2B). Four weeks later, her serum creatinine level had decreased to 3.3 mg/dL. Four years later, our patient continues to wear the pessary but has chronic renal failure.
THE TAKEAWAY
POP often is viewed as a minor problem, but it can cause obstructive uropathy with unilateral or bilateral hydronephrosis or renal dysfunction and/or failure. The delay often seen with reporting genital prolapse may be due to the mild symptoms or feelings of shame or fear. Combining screening for cervical pathology in general practice with a screening for genital prolapse could identify these problems.
Monitoring renal function is advised in patients with a Stage III or IV POP and any patients with POP who also have hypertension or diabetes mellitus. Because only minor changes in laboratory findings may be observed in patients with unilateral hydronephrosis, consider renal ultrasonography.
Treatment options for POP includes pelvic floor exercises, pessary insertion, and reconstructive surgery. Early treatment can resolve hydronephrosis and possibly prevent irreversible renal damage.
ACKNOWLEDGEMENTS
The authors thank Wilhelm Van Dorp, MD, Rob A. van de Beek, MD, and Alan Brind for their help with this manuscript.
1. Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;(4):CD004014.
2. Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027-1038.
3. Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, et al. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009;200:184. e1-184.e7.
4. Hui SY, Chan SC, Lam SY, et al. A prospective study on the prevalence of hydronephrosis in women with pelvic organ prolapse and their outcomes after treatment. Int Urogynecol J. 2011;22:1529-1534.
5. Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10-17.
6. Gemer O, Bergman M, Segal S. Prevalence of hydronephrosis in patients with genital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;86:11-13.
7. Lieberthal F, Frankenthal L Jr. The mechanism of urethral obstruction in prolapse of the uterus. Surg Gynaecol Obstet. 1941;73:838-842.
8. Sanai T, Yamashiro Y, Nakayama M, et al. End-stage renal failure due to total uterine prolapse. Urology. 2006;67:622. e5-622.e7.
9. Nässberger L, Larsson R. End-stage chronic renal failure due to total uterine prolapse. Acta Obstet Gynecol Scand. 1982;61: 495-497.
THE CASE
A 63-year-old multiparous woman visited her general practitioner because of nausea, vomiting, and general malaise. A proton pump inhibitor was prescribed, which temporarily relieved her symptoms. Two weeks later, however, her symptoms worsened and she was admitted to the hospital.
The patient’s physical examination on admission was normal, but laboratory findings revealed severe renal failure with a creatinine level of 7.4 mg/dL (normal, 0.6-1.1 mg/dL), potassium level of 7.4 mmol/L (3.5-5 mmol/L), and a sodium level of 123 mmol/L (135-145 mmol/L). A renal ultrasound revealed severe bilateral hydronephrosis with hydroureteronephrosis caused by obstructive uropathy. A radiologist examined the patient and determined that she had a total uterine prolapse; the cervix was 11 cm outside of the vagina (FIGURE 1). Our patient’s untreated pelvic organ prolapse (POP) had caused chronic renal failure. The patient was referred to a urogynecologist.
Previous attempts at treatment. It appeared that our patient had POP for years and there had been a previous attempt to treat it with a pessary. However, because of an unpleasant experience at her initial appointment and because her biggest complaint (until recently) had been the need to urinate frequently, she had not returned for follow-up appointments.
DISCUSSION
POP is not life-threatening, but the condition lowers the quality of life for 50% of parous women age >50 years.1 It can present as stress urinary incontinence, fecal incontinence, sexual dysfunction, and mechanical problems due to vaginal bulging or pelvic pressure.2 With the exception of vaginal bulging, symptoms are not specific for POP and there is no linear relationship between the severity of the prolapse and the symptoms.3,4
The condition is staged using the POP-Quantification (POP-Q) system5:
1. Stage 0: no prolapse
2. Stage I: the most distal portion of the prolapse is >1 cm above the hymen
3. Stage II: the prolapse is ≤1 cm proximal or distal to the plane of the hymen
4. Stage III: the prolapse is >1 cm below the plane of the hymen, but protrudes no farther
than 2 cm less than the total vaginal length
5. Stage IV: complete eversion of the lower genital tract.
As was the case with our patient, it is possible for a woman with severe total uterine prolapse (Stage IV) to have no major problems with urination or defecation.
The link between POP and hydronephrosis
Hydronephrosis appears to be a frequent finding in women with POP.4 A recent prospective observational study reported an overall prevalence of 10.3% (95% confidence interval, 6%-14%) in women with POP.4 Patients with advanced stages of POP (POP-Q Stage III or IV)4 who also had diabetes mellitus and hypertension were at particularly high risk, with a prevalence of about 20%. An analysis of factors, including age, parity, diabetes, hypertension, and type of prolapse, found that severity of POP was the strongest predictor of hydronephrosis: Patients with a Stage III to IV prolapse are 3.4 times more likely to have hydronephrosis than those with a Stage I or II prolapse.4,6
Possible causes of hydronephrosis in POP patients. Some researchers have proposed that hydronephrosis in patients with uterine prolapse may be due to a kinking of the ureters by the extrinsic compression of the prolapsed uterus. In patients with vaginal vault prolapse, the cause of the hydronephrosis could be a weakening or disintegration of the cardinal ligaments after hysterectomy.4,7
Patients may not complain. When hydronephrosis caused by POP occurs, it may develop slowly, causing little or no discomfort. As time passes, patients may complain of dull pain in the flank, suffer from urinary tract infections, or develop kidney stones before progressive renal dysfunction or renal failure occurs.4
There are 2 other cases in the literature of women who, like our patient, had uterine prolapse that went untreated until they were in renal failure.8,9 The patients noticed only mechanical problems due to the POP; bilateral hydroureteronephrosis and renal failure had developed undetected. In the end, both women needed lifelong hemodialysis.
Treatment options
Treatment options for POP include supervised pelvic floor exercise programs, pessary insertion, or reconstructive pelvic surgery. If POP is treated adequately, an estimated 95% of the hydronephrosis can resolve, regardless of its severity at presentation.4
Our patient was treated with a 95 mm Falk pessary. After 24 hours, renal ultrasonography showed a decrease in both the hydroureteronephrosis and the hydronephrosis (FIGURE 2A and 2B). Four weeks later, her serum creatinine level had decreased to 3.3 mg/dL. Four years later, our patient continues to wear the pessary but has chronic renal failure.
THE TAKEAWAY
POP often is viewed as a minor problem, but it can cause obstructive uropathy with unilateral or bilateral hydronephrosis or renal dysfunction and/or failure. The delay often seen with reporting genital prolapse may be due to the mild symptoms or feelings of shame or fear. Combining screening for cervical pathology in general practice with a screening for genital prolapse could identify these problems.
Monitoring renal function is advised in patients with a Stage III or IV POP and any patients with POP who also have hypertension or diabetes mellitus. Because only minor changes in laboratory findings may be observed in patients with unilateral hydronephrosis, consider renal ultrasonography.
Treatment options for POP includes pelvic floor exercises, pessary insertion, and reconstructive surgery. Early treatment can resolve hydronephrosis and possibly prevent irreversible renal damage.
ACKNOWLEDGEMENTS
The authors thank Wilhelm Van Dorp, MD, Rob A. van de Beek, MD, and Alan Brind for their help with this manuscript.
THE CASE
A 63-year-old multiparous woman visited her general practitioner because of nausea, vomiting, and general malaise. A proton pump inhibitor was prescribed, which temporarily relieved her symptoms. Two weeks later, however, her symptoms worsened and she was admitted to the hospital.
The patient’s physical examination on admission was normal, but laboratory findings revealed severe renal failure with a creatinine level of 7.4 mg/dL (normal, 0.6-1.1 mg/dL), potassium level of 7.4 mmol/L (3.5-5 mmol/L), and a sodium level of 123 mmol/L (135-145 mmol/L). A renal ultrasound revealed severe bilateral hydronephrosis with hydroureteronephrosis caused by obstructive uropathy. A radiologist examined the patient and determined that she had a total uterine prolapse; the cervix was 11 cm outside of the vagina (FIGURE 1). Our patient’s untreated pelvic organ prolapse (POP) had caused chronic renal failure. The patient was referred to a urogynecologist.
Previous attempts at treatment. It appeared that our patient had POP for years and there had been a previous attempt to treat it with a pessary. However, because of an unpleasant experience at her initial appointment and because her biggest complaint (until recently) had been the need to urinate frequently, she had not returned for follow-up appointments.
DISCUSSION
POP is not life-threatening, but the condition lowers the quality of life for 50% of parous women age >50 years.1 It can present as stress urinary incontinence, fecal incontinence, sexual dysfunction, and mechanical problems due to vaginal bulging or pelvic pressure.2 With the exception of vaginal bulging, symptoms are not specific for POP and there is no linear relationship between the severity of the prolapse and the symptoms.3,4
The condition is staged using the POP-Quantification (POP-Q) system5:
1. Stage 0: no prolapse
2. Stage I: the most distal portion of the prolapse is >1 cm above the hymen
3. Stage II: the prolapse is ≤1 cm proximal or distal to the plane of the hymen
4. Stage III: the prolapse is >1 cm below the plane of the hymen, but protrudes no farther
than 2 cm less than the total vaginal length
5. Stage IV: complete eversion of the lower genital tract.
As was the case with our patient, it is possible for a woman with severe total uterine prolapse (Stage IV) to have no major problems with urination or defecation.
The link between POP and hydronephrosis
Hydronephrosis appears to be a frequent finding in women with POP.4 A recent prospective observational study reported an overall prevalence of 10.3% (95% confidence interval, 6%-14%) in women with POP.4 Patients with advanced stages of POP (POP-Q Stage III or IV)4 who also had diabetes mellitus and hypertension were at particularly high risk, with a prevalence of about 20%. An analysis of factors, including age, parity, diabetes, hypertension, and type of prolapse, found that severity of POP was the strongest predictor of hydronephrosis: Patients with a Stage III to IV prolapse are 3.4 times more likely to have hydronephrosis than those with a Stage I or II prolapse.4,6
Possible causes of hydronephrosis in POP patients. Some researchers have proposed that hydronephrosis in patients with uterine prolapse may be due to a kinking of the ureters by the extrinsic compression of the prolapsed uterus. In patients with vaginal vault prolapse, the cause of the hydronephrosis could be a weakening or disintegration of the cardinal ligaments after hysterectomy.4,7
Patients may not complain. When hydronephrosis caused by POP occurs, it may develop slowly, causing little or no discomfort. As time passes, patients may complain of dull pain in the flank, suffer from urinary tract infections, or develop kidney stones before progressive renal dysfunction or renal failure occurs.4
There are 2 other cases in the literature of women who, like our patient, had uterine prolapse that went untreated until they were in renal failure.8,9 The patients noticed only mechanical problems due to the POP; bilateral hydroureteronephrosis and renal failure had developed undetected. In the end, both women needed lifelong hemodialysis.
Treatment options
Treatment options for POP include supervised pelvic floor exercise programs, pessary insertion, or reconstructive pelvic surgery. If POP is treated adequately, an estimated 95% of the hydronephrosis can resolve, regardless of its severity at presentation.4
Our patient was treated with a 95 mm Falk pessary. After 24 hours, renal ultrasonography showed a decrease in both the hydroureteronephrosis and the hydronephrosis (FIGURE 2A and 2B). Four weeks later, her serum creatinine level had decreased to 3.3 mg/dL. Four years later, our patient continues to wear the pessary but has chronic renal failure.
THE TAKEAWAY
POP often is viewed as a minor problem, but it can cause obstructive uropathy with unilateral or bilateral hydronephrosis or renal dysfunction and/or failure. The delay often seen with reporting genital prolapse may be due to the mild symptoms or feelings of shame or fear. Combining screening for cervical pathology in general practice with a screening for genital prolapse could identify these problems.
Monitoring renal function is advised in patients with a Stage III or IV POP and any patients with POP who also have hypertension or diabetes mellitus. Because only minor changes in laboratory findings may be observed in patients with unilateral hydronephrosis, consider renal ultrasonography.
Treatment options for POP includes pelvic floor exercises, pessary insertion, and reconstructive surgery. Early treatment can resolve hydronephrosis and possibly prevent irreversible renal damage.
ACKNOWLEDGEMENTS
The authors thank Wilhelm Van Dorp, MD, Rob A. van de Beek, MD, and Alan Brind for their help with this manuscript.
1. Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;(4):CD004014.
2. Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027-1038.
3. Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, et al. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009;200:184. e1-184.e7.
4. Hui SY, Chan SC, Lam SY, et al. A prospective study on the prevalence of hydronephrosis in women with pelvic organ prolapse and their outcomes after treatment. Int Urogynecol J. 2011;22:1529-1534.
5. Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10-17.
6. Gemer O, Bergman M, Segal S. Prevalence of hydronephrosis in patients with genital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;86:11-13.
7. Lieberthal F, Frankenthal L Jr. The mechanism of urethral obstruction in prolapse of the uterus. Surg Gynaecol Obstet. 1941;73:838-842.
8. Sanai T, Yamashiro Y, Nakayama M, et al. End-stage renal failure due to total uterine prolapse. Urology. 2006;67:622. e5-622.e7.
9. Nässberger L, Larsson R. End-stage chronic renal failure due to total uterine prolapse. Acta Obstet Gynecol Scand. 1982;61: 495-497.
1. Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;(4):CD004014.
2. Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027-1038.
3. Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, et al. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009;200:184. e1-184.e7.
4. Hui SY, Chan SC, Lam SY, et al. A prospective study on the prevalence of hydronephrosis in women with pelvic organ prolapse and their outcomes after treatment. Int Urogynecol J. 2011;22:1529-1534.
5. Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10-17.
6. Gemer O, Bergman M, Segal S. Prevalence of hydronephrosis in patients with genital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;86:11-13.
7. Lieberthal F, Frankenthal L Jr. The mechanism of urethral obstruction in prolapse of the uterus. Surg Gynaecol Obstet. 1941;73:838-842.
8. Sanai T, Yamashiro Y, Nakayama M, et al. End-stage renal failure due to total uterine prolapse. Urology. 2006;67:622. e5-622.e7.
9. Nässberger L, Larsson R. End-stage chronic renal failure due to total uterine prolapse. Acta Obstet Gynecol Scand. 1982;61: 495-497.