User login
BERLIN – A vision perceived during America’s Great Depression has come to fruition across the globe, putting mental illness at the center of a devastating web of personal and economic costs.
In the 1930s, the Rockefeller Foundation’s director of medical science, Alan Gregg, MD, distilled an important notion from his decades of travel providing health care and advice to developing nations. As poor countries became richer, infectious diseases that had long ravaged their populations came under control. As people lived longer, however, they became subject to other disorders: chronic age-related illnesses for the old and, for the young, mental illnesses.
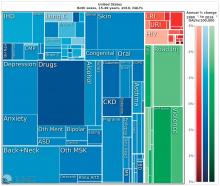
“We have a very, very low rate of infectious disease now, much as the Rockefeller Foundation predicted,” said Dr. Summergrad, the Dr. Frances S. Arkin Professor and chair of psychiatry at Tufts University, Boston. “But, in 2010, the biggest causes of morbidity and disability for U.S. residents aged 15-49 years old were major depressive disorder, dysthymia, drug and alcohol use, schizophrenia, and anxiety. These dwarf the impact of every other illness during that age period. …. They are the burdens of disease of the modern world.”
This shift from infectious disease to mental illness as a primary cause of disability has profound downstream health implications as well, Dr. Summergrad said. Mental disorders that emerge in adolescent and young adulthood are inextricably linked to the chronic diseases that develop in older people.
“Mental and behavioral disturbances are important risk factors for medical conditions that also exact a heavy burden,” he said, referring to a study in JAMA (2013 Aug 14;310[6]:591-608). The report, “The state of U.S. health, 1990-2010: Burden of diseases, injuries, and risk factors,” found that more than half of the of the Top 17 risk factors for morbidity and mortality were directly or indirectly related to mental or behavioral disorders. These included direct causes like alcohol and drug use, and indirect causes that are highly correlated with mental illnesses: physical inactivity, tobacco use, glycemic abnormalities, hypertension, and obesity.
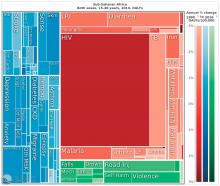
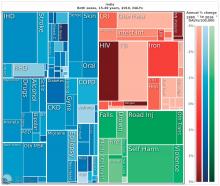
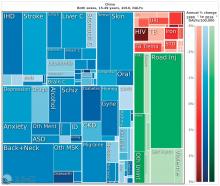
The Institute for Health Metrics and Evaluation at the University of Washington, Seattle, illustrated these global trends in September, with a report published in the Lancet (2017;390:1423-59). Produced in collaboration with the Bill and Melinda Gates Foundation, the report focused on the U.N. Sustainable Development Goals, measured 37 of the 50 health-related SDG indicators from 1990-2016 in 188 countries, and projected the indicators to 2030.
China, on the other hand, looked very much like North America. The proportion of infectious diseases was much smaller than in sub-Saharan Africa or India, a finding Dr. Summergrad attributed to the Chinese government’s post–World War II determination to eradicate communicable diseases.
Unfortunately, Dr. Summergrad said, most countries are ill equipped to handle this shift in the burden of illness. Even in the United States, there are limited mental health hospital beds and a dearth of psychiatrists to handle the burgeoning patient load. And the shift toward higher rates of mental illness will likely continue, at a shocking financial cost.
A Harvard School of Public Health policy report, issued in 2011, paints a stark picture. In 2010, mental illness cost high-income countries about $5.5 trillion in lost income and productivity, narrowly beating out the burden imposed by cardivoascular disease ($5.4 trillion). By 2030, lost wages and productivity tied to mental illiness is expected to cost the United States $7.3 trillion.
“Globally, by 2030, we can expect the direct economic impact of mental illnesses to reach $16 trillion,” Dr. Summergrad said. “We have a limited workforce, limited outpatient facilities, limited hospital beds, and limited money, even here in the U.S. All of this is almost nonexistent in much of the world. The integration of care and workforce and facilities will be a huge challenge as we move forward. We need to think about long-term investment here, much in the same way that the Rockefeller Foundation thought about this in the 1930s.”
Dr. Summergrad had no relevant financial disclosures.
BERLIN – A vision perceived during America’s Great Depression has come to fruition across the globe, putting mental illness at the center of a devastating web of personal and economic costs.
In the 1930s, the Rockefeller Foundation’s director of medical science, Alan Gregg, MD, distilled an important notion from his decades of travel providing health care and advice to developing nations. As poor countries became richer, infectious diseases that had long ravaged their populations came under control. As people lived longer, however, they became subject to other disorders: chronic age-related illnesses for the old and, for the young, mental illnesses.
“We have a very, very low rate of infectious disease now, much as the Rockefeller Foundation predicted,” said Dr. Summergrad, the Dr. Frances S. Arkin Professor and chair of psychiatry at Tufts University, Boston. “But, in 2010, the biggest causes of morbidity and disability for U.S. residents aged 15-49 years old were major depressive disorder, dysthymia, drug and alcohol use, schizophrenia, and anxiety. These dwarf the impact of every other illness during that age period. …. They are the burdens of disease of the modern world.”
This shift from infectious disease to mental illness as a primary cause of disability has profound downstream health implications as well, Dr. Summergrad said. Mental disorders that emerge in adolescent and young adulthood are inextricably linked to the chronic diseases that develop in older people.
“Mental and behavioral disturbances are important risk factors for medical conditions that also exact a heavy burden,” he said, referring to a study in JAMA (2013 Aug 14;310[6]:591-608). The report, “The state of U.S. health, 1990-2010: Burden of diseases, injuries, and risk factors,” found that more than half of the of the Top 17 risk factors for morbidity and mortality were directly or indirectly related to mental or behavioral disorders. These included direct causes like alcohol and drug use, and indirect causes that are highly correlated with mental illnesses: physical inactivity, tobacco use, glycemic abnormalities, hypertension, and obesity.
The Institute for Health Metrics and Evaluation at the University of Washington, Seattle, illustrated these global trends in September, with a report published in the Lancet (2017;390:1423-59). Produced in collaboration with the Bill and Melinda Gates Foundation, the report focused on the U.N. Sustainable Development Goals, measured 37 of the 50 health-related SDG indicators from 1990-2016 in 188 countries, and projected the indicators to 2030.
China, on the other hand, looked very much like North America. The proportion of infectious diseases was much smaller than in sub-Saharan Africa or India, a finding Dr. Summergrad attributed to the Chinese government’s post–World War II determination to eradicate communicable diseases.
Unfortunately, Dr. Summergrad said, most countries are ill equipped to handle this shift in the burden of illness. Even in the United States, there are limited mental health hospital beds and a dearth of psychiatrists to handle the burgeoning patient load. And the shift toward higher rates of mental illness will likely continue, at a shocking financial cost.
A Harvard School of Public Health policy report, issued in 2011, paints a stark picture. In 2010, mental illness cost high-income countries about $5.5 trillion in lost income and productivity, narrowly beating out the burden imposed by cardivoascular disease ($5.4 trillion). By 2030, lost wages and productivity tied to mental illiness is expected to cost the United States $7.3 trillion.
“Globally, by 2030, we can expect the direct economic impact of mental illnesses to reach $16 trillion,” Dr. Summergrad said. “We have a limited workforce, limited outpatient facilities, limited hospital beds, and limited money, even here in the U.S. All of this is almost nonexistent in much of the world. The integration of care and workforce and facilities will be a huge challenge as we move forward. We need to think about long-term investment here, much in the same way that the Rockefeller Foundation thought about this in the 1930s.”
Dr. Summergrad had no relevant financial disclosures.
BERLIN – A vision perceived during America’s Great Depression has come to fruition across the globe, putting mental illness at the center of a devastating web of personal and economic costs.
In the 1930s, the Rockefeller Foundation’s director of medical science, Alan Gregg, MD, distilled an important notion from his decades of travel providing health care and advice to developing nations. As poor countries became richer, infectious diseases that had long ravaged their populations came under control. As people lived longer, however, they became subject to other disorders: chronic age-related illnesses for the old and, for the young, mental illnesses.
“We have a very, very low rate of infectious disease now, much as the Rockefeller Foundation predicted,” said Dr. Summergrad, the Dr. Frances S. Arkin Professor and chair of psychiatry at Tufts University, Boston. “But, in 2010, the biggest causes of morbidity and disability for U.S. residents aged 15-49 years old were major depressive disorder, dysthymia, drug and alcohol use, schizophrenia, and anxiety. These dwarf the impact of every other illness during that age period. …. They are the burdens of disease of the modern world.”
This shift from infectious disease to mental illness as a primary cause of disability has profound downstream health implications as well, Dr. Summergrad said. Mental disorders that emerge in adolescent and young adulthood are inextricably linked to the chronic diseases that develop in older people.
“Mental and behavioral disturbances are important risk factors for medical conditions that also exact a heavy burden,” he said, referring to a study in JAMA (2013 Aug 14;310[6]:591-608). The report, “The state of U.S. health, 1990-2010: Burden of diseases, injuries, and risk factors,” found that more than half of the of the Top 17 risk factors for morbidity and mortality were directly or indirectly related to mental or behavioral disorders. These included direct causes like alcohol and drug use, and indirect causes that are highly correlated with mental illnesses: physical inactivity, tobacco use, glycemic abnormalities, hypertension, and obesity.
The Institute for Health Metrics and Evaluation at the University of Washington, Seattle, illustrated these global trends in September, with a report published in the Lancet (2017;390:1423-59). Produced in collaboration with the Bill and Melinda Gates Foundation, the report focused on the U.N. Sustainable Development Goals, measured 37 of the 50 health-related SDG indicators from 1990-2016 in 188 countries, and projected the indicators to 2030.
China, on the other hand, looked very much like North America. The proportion of infectious diseases was much smaller than in sub-Saharan Africa or India, a finding Dr. Summergrad attributed to the Chinese government’s post–World War II determination to eradicate communicable diseases.
Unfortunately, Dr. Summergrad said, most countries are ill equipped to handle this shift in the burden of illness. Even in the United States, there are limited mental health hospital beds and a dearth of psychiatrists to handle the burgeoning patient load. And the shift toward higher rates of mental illness will likely continue, at a shocking financial cost.
A Harvard School of Public Health policy report, issued in 2011, paints a stark picture. In 2010, mental illness cost high-income countries about $5.5 trillion in lost income and productivity, narrowly beating out the burden imposed by cardivoascular disease ($5.4 trillion). By 2030, lost wages and productivity tied to mental illiness is expected to cost the United States $7.3 trillion.
“Globally, by 2030, we can expect the direct economic impact of mental illnesses to reach $16 trillion,” Dr. Summergrad said. “We have a limited workforce, limited outpatient facilities, limited hospital beds, and limited money, even here in the U.S. All of this is almost nonexistent in much of the world. The integration of care and workforce and facilities will be a huge challenge as we move forward. We need to think about long-term investment here, much in the same way that the Rockefeller Foundation thought about this in the 1930s.”
Dr. Summergrad had no relevant financial disclosures.
EXPERT ANALYSIS FROM WPA 2017