User login
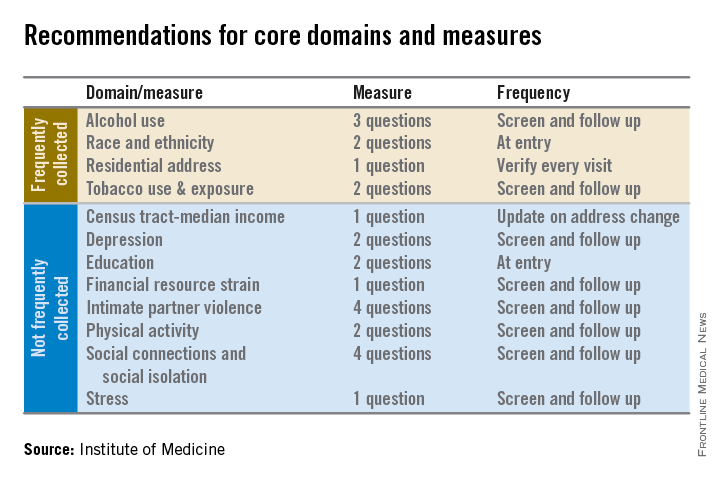
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
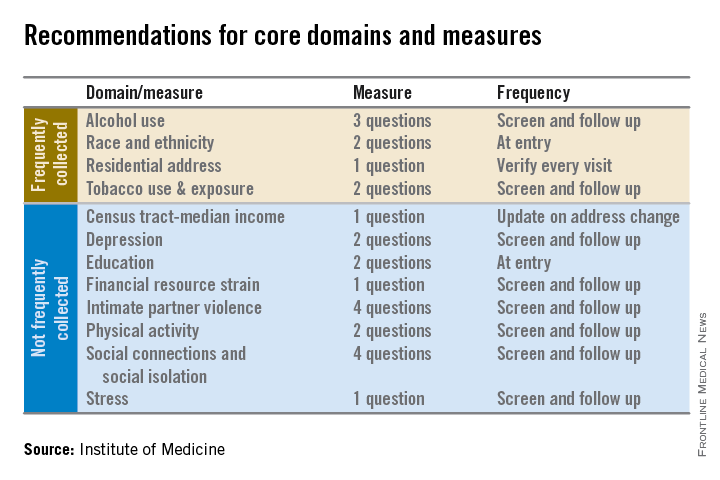
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.
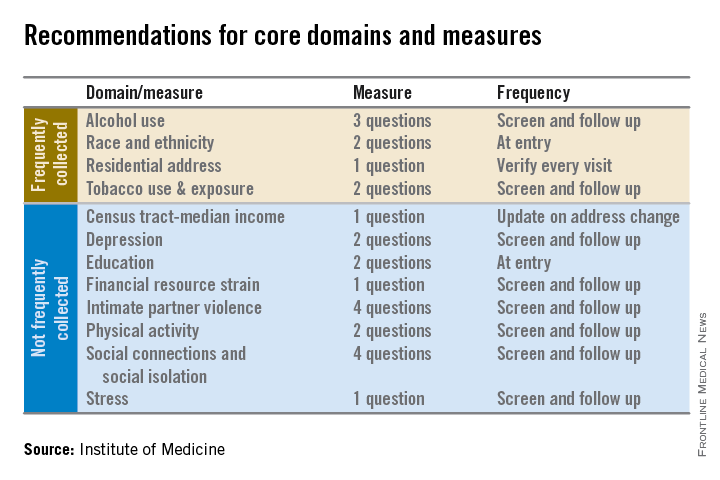
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
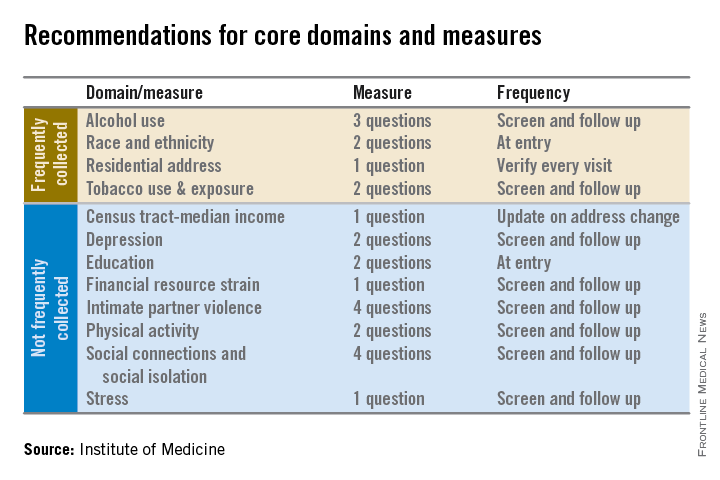
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.