User login
Mrs. W, age 53, is referred by her primary provider for consultation on depressive symptoms, including worsening depressed mood, anhedonia, anxiety, and suicidal thoughts for 2 months. She reports at least 2 similar episodes in the past 15 years. Mrs. W has a remote history of IV drug use and history of alcohol abuse, but she attends Alcoholics Anonymous and has 10 years of sobriety. She has no history of hospitalizations for medical illness and denies any medical problems.
Mrs. W is taking amitriptyline, 50 mg, for insomnia. She has no history of manic or psychotic symptoms, and the mental status examination is consistent with major depression. Her past depressive episodes were treated successfully with a medication that she does not recall.
The psychiatrist diagnoses recurrent and severe major depression and prescribes cognitive-behavioral therapy and sertraline, 25 mg/d, titrated to 50 mg/d over the next 2 weeks. Amitriptyline is discontinued.
When the psychiatrist receives Mrs. W’s medical records, electrolytes, complete blood count, thyroid stimulating hormone level, and fasting glucose are within normal limits, but alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are greatly elevated at 250 U/L and 150 U/L, respectively. Progress notes contain no references to liver disease.
Interpreting psychiatric patients’ liver function tests (LFTs) can be challenging, especially in those with polypharmacy, co-occurring substance abuse, or risk factors for viral hepatitis. You can improve collaboration with primary care providers by understanding:
- what an LFT measures
- how to interpret abnormal results
- which conditions to suspect, based on the results.
A standard LFT usually measures several enzymes and proteins, typically ALT, AST, alkaline phosphatase (ALP), total bilirubin (TBIL), albumin (ALB), and total protein (TP). Measures of gamma-glutamyl transpeptidase (GGT) and prothrombin time (PT) are often requested with an LFT. Table 1 provides normal ranges and ranges that indicate liver damage for several of these parameters.1,2
“Liver function test” is a misnomer because LFTs do not directly measure liver function. Rather, they reflect hepatocyte injury or cholestasis (blockage or damage in the biliary system). ALB and PT measure liver synthetic function, but are nonspecific. ALB levels can be altered by nutritional status, protein-losing enteropathies, or nephropathies, whereas PT may be modified by warfarin, vitamin K deficiency, or consumptive coagulopathy.
Table 1
Test results: what’s normal, what suggests liver damage
| Parameter | Description | Normal range | Range indicating liver damage |
|---|---|---|---|
| Alanine aminotransferase (ALT) | Enzyme highly concentrated in the liver | 3 to 30 U/L | >3 times upper limit of normal |
| Alkaline phosphatase (ALP) | Enzyme highly concentrated in the liver, bile ducts, placenta, and bone | 35 to 150 U/L | >2 times upper limit of normal |
| Aspartate aminotransferase (AST) | Enzyme highly concentrated in heart muscle, liver cells, skeletal muscle cells, and (to a lesser degree) other tissues | 11 to 32 U/L | Used to evaluate elevations in other serum enzyme level |
| Gamma-glutamyl transpeptidase (GGT) | Enzyme highly concentrated in the liver, bile ducts, and kidneys | 5 to 40 U/L | Used to evaluate elevations in other serum enzyme levels |
| Total bilirubin (TBIL) | Yellow bile pigment produced when liver processes waste products | 0.3 to 1.1 mg/dL | >2 times upper limit of normal if associated with elevation in ALT or ALP |
| Sources: References 1,2 | |||
CASE CONTINUED: Spotting a pattern of injury
Mrs. W’s elevated ALT and AST levels are of unknown duration. Her AST:ALT ratio is approximately 2:1, suggesting hepatocellular injury.
Interpreting abnormal LFT results
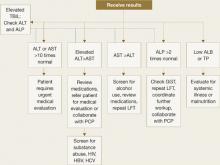
To properly interpret LFTs, consider the patient’s symptoms, physical exam findings, medical history, medical illnesses, potential substance use, risk factors for HIV and viral hepatitis, and medication list. Collaborate with the patient’s primary care provider or facilitate primary care (Figure 1).
ALT and AST are highly concentrated in the liver, but ALT is a more specific indicator of liver injury. For both, levels may vary according to age, sex, and ethnicity but in general, levels <30 U/L are considered normal.1,2
ALP originates predominately from the liver and from bone. Persistently elevated ALP levels in the liver may indicate chronic cholestasis or infiltrative liver disease.
GGT is best used to evaluate the meaning of elevations in other serum enzymes.3 Elevated GGT can help confirm hepatic origin of elevated ALP or support a suspicion of alcohol use in patients with an AST: ALT ratio >2:1.
If an asymptomatic patient has elevated LFT results, first repeat the test. If repeat results are normal, perform the test again in 3-6 months. Keep in mind, however, that normal LFT results do not always indicate the absence of disease. For example, up to 16% of patients with hepatitis C and 13% of patients with nonalcoholic steatohepatitis (NASH) have normal LFT results despite histologic abnormalities.4
If repeat results are abnormal, obtain the patient’s consent to inform the primary care provider. Then take a thorough history and perform a focused physical exam. In the history, focus on use of prescription and nonprescription medications, including over-the-counter and herbal therapies, alcohol, and drugs of abuse, such as MDMA (“ecstasy”), phencyclidine (“angel dust”), and glues or solvents. Also assess for risk factors for infectious hepatitis, such as IV drug use, work-related blood exposure, and tattoos. Ask about a family history of liver disease. Focus your physical exam on visible stigmata of chronic liver disease, such as jaundice, temporal wasting, ascites, and palmar erythema.
Next, analyze the severity and pattern of the LFT abnormality. Liver injury is defined as:
- ALT >3 times the upper limit of normal
- ALP >2 times the upper limit of normal
- or total bilirubin >2 times the upper limit of normal if associated with any elevation of ALT or ALP.5
If ALT elevations predominate, consider hepatocellular injury. If ALP elevations predominate, suspect cholestatic injury. Elevations of both ALT and ALP suggest a mixed pattern of hepatocellular and cholestatic injury.
Figure 1 Interpreting liver function test results
ALB: albumin; ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; GGT: gamma-glutamyl transpeptidase; HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus; LFT: liver function test; PCP: primary care provider; TBIL: total bilirubin; TP: total protein
CASE CONTINUED: Pinpointing a diagnosis
Mrs. W undergoes repeat LFTs with GGT testing, screening tests for hepatitis B and C, and a comprehensive physical exam. The psychiatrist screens for alcohol use, asks the patient about her use of herbal therapies and substance abuse relapse, and evaluates cognitive mental status for symptoms of encephalopathy. Results reveal that Mrs. W’s ALT and AST are elevated because of chronic active hepatitis C.
Causes of hepatocellular injury
Further evaluation of your patient’s test results can help narrow down potential causes of liver damage. If your patient’s ALT is disproportionately elevated, estimate the:
- severity of aminotransferase elevation
- ratio of AST:ALT
- rate of change over multiple LFTs.
If AST or ALT is >10 times normal, consider toxin-induced or ischemic injury.6 An AST:ALT ratio of 2:1 or 3:1, especially when associated with elevated GGT, strongly suggests alcohol-induced injury. With acute mild transaminase elevations—ALT>AST, 2 to 3 times normal—suspect medication-related injury.
A variety of factors and conditions can result in hepatocellular damage:
Common causes
Medications. Many drugs, including common psychotropics, can cause elevated liver enzymes (Table 2).5 As little as 4 grams per day of acetaminophen can cause mild transaminitis.4 Antidepressants, second-generation antipsychotics (SGAs), and anticonvulsants can cause increases in AST and ALT.7 If liver enzymes rise after a patient starts a new medication, drug-related liver toxicity is likely. Remember to consider a patient’s use of drugs of abuse and herbal therapies.
Discontinuing the suspect agent usually produces steady (although sometimes slow) improvement in LFTs. Use serial LFT testing and focused history and physical examinations to confirm improvement.
Alcohol. Screen for alcohol abuse using the CAGE questionnaire, the Alcohol Use Disorders Identification Test, or a similar tool. More than 90% of patients with an AST:ALT ratio of 2:1 have alcoholic liver disease; this percentage increases to >96% when the ratio is 3:1.1 A 2-fold increase in GGT in a patient with an AST:ALT ratio >2:1 further supports the diagnosis. In patients with alcohol abuse, AST rarely exceeds 10 times normal.5
Hepatitis C. The prevalence of hepatitis C is increasing among patients with severe mental illness, especially a dual diagnosis.8 Hepatitis C rarely causes acute symptoms.
Offer a hepatitis C antibody screening to test patients with even a remote history of IV drug use or comorbid substance abuse. Patients with a positive hepatitis C antibody test or a negative hepatitis C antibody test but a high risk for the disease should receive further testing.9
Hepatitis B. Risk factors include exposure to blood, sexual transmission, and emigration from endemic areas in Southeast Asia and sub-Saharan Africa. Initial screening panels include tests for hepatitis B surface antigen, hepatitis B surface antibody, and hepatitis B core antibody. Positive B surface antigen and core antibody tests indicate infection.
NASH. Nonalcoholic steatohepatitis (NASH) is the most common cause of mild transaminitis in the Western world (Box).4,10,11
Nonalcoholic steatohepatitis (NASH) is inflammatory liver disease of uncertain pathogenesis that commonly occurs with metabolic syndrome. It affects up to 5% of Americans, most often those who are middle-aged and overweight or obese, hyperlipidemic, or diabetic. NASH resembles alcoholic liver disease but occurs in people who drink little or no alcohol. In addition to inflammation, it is characterized by accumulation of fat and fibrous tissue in the liver. Typically patients are asymptomatic, but NASH can lead to cirrhosis.
NASH is a common cause of mild transaminitis. Aminotransferase levels are usually <4 times the normal value.10 Thirteen percent of patients with NASH have normal LFT results despite histologic abnormalities.4 NASH is a diagnosis of exclusion that is confirmed by liver biopsy.
NASH has no specific therapies or cure. Treatment focuses on controlling associated conditions such as diabetes, obesity, and hyperlipidemia. In obese patients, weight loss is the cornerstone of treatment. If you prescribe a second-generation antipsychotic (SGA) for a patient who has NASH, be aware that SGAs increase the risk of hyperglycemia and dyslipidemia, which can exacerbate NASH.11
Table 2
Medications that affect liver function test (LFT) results
| Medication class | Hepatocellular injury (↑ALT) | Cholestatic injury (↑ALP and ↑ALT) | Mixed injury (↑ALP and ↑TBIL) |
|---|---|---|---|
| Psychotropic | Bupropion, fluoxetine, paroxetine, risperidone, sertraline, trazodone, valproic acid | Chlorpromazine, mirtazapine, tricyclic antidepressants | Amitriptyline, Amitriptyline, phenobarbital, phenytoin, trazodone |
| Cardiovascular | Amiodarone, lisinopril, losartan, statins | Clopidogrel, irbesartan | Captopril, enalapril, verapamil |
| Endocrine | Acarbose, allopurinol | – | – |
| Gastrointestinal | Omeprazole | – | – |
| Herbal remedies | Germander, kava | – | – |
| Anti-infectives | HAART drugs, isoniazid, ketoconazole, pyrazinamide, rifampin, tetracycline, trovafloxacin | Amoxicillin/clavulanic acid, erythromycins, terbinafine | Clindamycin, nitrofurantoin, trimethoprim-sulfamethoxazole |
| Rheumatologic | Acetaminophen, baclofen, methotrexate, NSAIDs | Anabolic steroids | Azathioprine, sulfonamides |
| Others | – | Oral contraceptives, estrogens, phenothiazines | Cyproheptadine, flutamide |
| ALP: alkaline phosphatase; ALT: alanine aminotransferase; HAART: highly active antiretroviral therapy; NSAID: nonsteroidal anti-inflammatory drug; TBIL: total bilirubin | |||
| Source: Reference 5 | |||
Less common causes
Hemochromatosis is an autosomal recessive disease that causes pathologic deposition of iron in the liver, pancreas, and heart and leads to cirrhosis, diabetes, and heart disease. Suspect it in patients with a clinical syndrome and transferrin saturation index >45%.12 A hemochromatosis gene mutation analysis confirms the diagnosis.
Autoimmune hepatitis occurs primarily in women ages 20 to 50 years.13 Because >80% of patients with autoimmune hepatitis have hypergammaglobulinemia, serum protein electrophores is a useful screening test.5
Wilson’s disease is a genetic disorder of biliary copper excretion classically diagnosed in young people with concomitant neurologic or psychiatric conditions. Those affected have low serum ceruloplasmin. Neuropsychiatric symptoms include parkinsonian-like tremor, rigidity, clumsiness of gait, slurred speech, drooling, and inappropriate and uncontrollable grinning (risus sardonicus).8 Psychosis and suicidality also are common in patients with Wilson’s disease.
Alpha-1 antitrypsin deficiency. Alpha-1 antitrypsin is a protein produced primarily in the liver that protects the lungs from neutrophil elastase. Suspect alpha-1 antitrypsin deficiency in patients with abnormal LFTs and emphysema. Low serum alpha-1 antitrypsin confirms the diagnosis.
Celiac disease. Consider celiac disease in patients with chronic diarrhea or abdominal distension and abnormal LFTs. Small bowel biopsy and elevated tissue transglutaminase antibodies and anti-endomysial antibodies confirm the diagnosis.
Causes of cholestatic injury
If your patient has a disproportionate ALP elevation, identify the source of the ALP by testing GGT. GGT levels are elevated in liver disease but not in bone disease. Partial bile duct obstruction is a common cause of ALP elevation. For initial testing, include ultrasonography of the right upper quadrant.
Medications. Many medications can cause biliary stasis and cholestatic LFTs, including mirtazapine, tricyclic antidepressants, anabolic steroids, phenytoin, and estrogens.
Primary sclerosing cholangitis is inflammatory disease of the bile ducts that can lead to cholestasis (blockage of bile transport blockage). Consider it in patients with inflammatory bowel disease. Endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography aid diagnosis.
Primary biliary cirrhosis generally presents in middle-aged women with other autoimmune processes, cholestasis, and pruritus. Consider testing serum antimitochondrial antibodies.
Infiltrative liver diseases such as sarcoidosis, metastatic disease, or lymphoma can also present with cholestasis. Liver imaging is required for these diagnoses.
Causes of mixed injury
If LFT results suggest a mixed injury pattern, focus on the predominant pattern and evaluate the causes listed above. Certain medications typically result in a mixed injury pattern.
Related resources
- American Gastroenterological Association medical position statement: evaluation of liver chemistry tests. www.guideline.gov/summary/summary.aspx?ss=15&doc_id=3492&nbr=002718.
- Johnston DE. Special considerations in interpreting liver function tests. Am Fam Physician 1999;59(8):2223-30.
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Equetro, Tegretol
- Chlorpromazine • Thorazine
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Phenobarbital • Luminal
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Sertraline • Zoloft
- Trazodone • Desyrel
- Valproic acid • Depakene
- Warfarin • Coumadin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med 2002;137(1):1-10.
2. Gopal DV, Rosen HR. Abnormal findings on liver function tests. Interpreting results to narrow the diagnosis and establish a prognosis. Postgrad Med 2000;107(2):100-14.
3. Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med 2000;342(17):1266-71.
4. Ioannou GN, Boyko EJ, Lee SP. The prevalence and predictors of elevated serum aminotransferase activity in the United States in 1999-2002. Am J Gastroenterol 2006;101(1):76-82.
5. Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med 2006;354(7):731-9.
6. Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005;172(3):367-79.
7. Bezchilibny-Butler KZ, Jeffries JJ, eds. Clinical handbook of psychotropic drugs, 15th ed. Cambridge Hogrefe & Huber; 2005.
8. Crone CC, Gabriel GM, Dimartini A. An overview of psychiatric issues in liver disease for the consultation-liaison psychiatrist. Psychosomatics 2006;47(3):188-205.
9. Kaplan MA. Approach to the patient with abnormal liver function tests. Available at: http://www.uptodate.com. Accessed December 12, 2006.
10. Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 1994;107(4):1103-9.
11. Lieberman JA, Stroup SS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353(12):1209-23.
12. Yen AW, Fancher TL, Bowlus CL. Revisiting hereditary hemochromatosis: current concepts and progress. Am J Med 2006;119(5):391-9.
13. Krawitt EL. Autoimmune hepatitis. N Engl J Med 1996;334(14):897-903.
Mrs. W, age 53, is referred by her primary provider for consultation on depressive symptoms, including worsening depressed mood, anhedonia, anxiety, and suicidal thoughts for 2 months. She reports at least 2 similar episodes in the past 15 years. Mrs. W has a remote history of IV drug use and history of alcohol abuse, but she attends Alcoholics Anonymous and has 10 years of sobriety. She has no history of hospitalizations for medical illness and denies any medical problems.
Mrs. W is taking amitriptyline, 50 mg, for insomnia. She has no history of manic or psychotic symptoms, and the mental status examination is consistent with major depression. Her past depressive episodes were treated successfully with a medication that she does not recall.
The psychiatrist diagnoses recurrent and severe major depression and prescribes cognitive-behavioral therapy and sertraline, 25 mg/d, titrated to 50 mg/d over the next 2 weeks. Amitriptyline is discontinued.
When the psychiatrist receives Mrs. W’s medical records, electrolytes, complete blood count, thyroid stimulating hormone level, and fasting glucose are within normal limits, but alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are greatly elevated at 250 U/L and 150 U/L, respectively. Progress notes contain no references to liver disease.
Interpreting psychiatric patients’ liver function tests (LFTs) can be challenging, especially in those with polypharmacy, co-occurring substance abuse, or risk factors for viral hepatitis. You can improve collaboration with primary care providers by understanding:
- what an LFT measures
- how to interpret abnormal results
- which conditions to suspect, based on the results.
A standard LFT usually measures several enzymes and proteins, typically ALT, AST, alkaline phosphatase (ALP), total bilirubin (TBIL), albumin (ALB), and total protein (TP). Measures of gamma-glutamyl transpeptidase (GGT) and prothrombin time (PT) are often requested with an LFT. Table 1 provides normal ranges and ranges that indicate liver damage for several of these parameters.1,2
“Liver function test” is a misnomer because LFTs do not directly measure liver function. Rather, they reflect hepatocyte injury or cholestasis (blockage or damage in the biliary system). ALB and PT measure liver synthetic function, but are nonspecific. ALB levels can be altered by nutritional status, protein-losing enteropathies, or nephropathies, whereas PT may be modified by warfarin, vitamin K deficiency, or consumptive coagulopathy.
Table 1
Test results: what’s normal, what suggests liver damage
| Parameter | Description | Normal range | Range indicating liver damage |
|---|---|---|---|
| Alanine aminotransferase (ALT) | Enzyme highly concentrated in the liver | 3 to 30 U/L | >3 times upper limit of normal |
| Alkaline phosphatase (ALP) | Enzyme highly concentrated in the liver, bile ducts, placenta, and bone | 35 to 150 U/L | >2 times upper limit of normal |
| Aspartate aminotransferase (AST) | Enzyme highly concentrated in heart muscle, liver cells, skeletal muscle cells, and (to a lesser degree) other tissues | 11 to 32 U/L | Used to evaluate elevations in other serum enzyme level |
| Gamma-glutamyl transpeptidase (GGT) | Enzyme highly concentrated in the liver, bile ducts, and kidneys | 5 to 40 U/L | Used to evaluate elevations in other serum enzyme levels |
| Total bilirubin (TBIL) | Yellow bile pigment produced when liver processes waste products | 0.3 to 1.1 mg/dL | >2 times upper limit of normal if associated with elevation in ALT or ALP |
| Sources: References 1,2 | |||
CASE CONTINUED: Spotting a pattern of injury
Mrs. W’s elevated ALT and AST levels are of unknown duration. Her AST:ALT ratio is approximately 2:1, suggesting hepatocellular injury.
Interpreting abnormal LFT results
To properly interpret LFTs, consider the patient’s symptoms, physical exam findings, medical history, medical illnesses, potential substance use, risk factors for HIV and viral hepatitis, and medication list. Collaborate with the patient’s primary care provider or facilitate primary care (Figure 1).
ALT and AST are highly concentrated in the liver, but ALT is a more specific indicator of liver injury. For both, levels may vary according to age, sex, and ethnicity but in general, levels <30 U/L are considered normal.1,2
ALP originates predominately from the liver and from bone. Persistently elevated ALP levels in the liver may indicate chronic cholestasis or infiltrative liver disease.
GGT is best used to evaluate the meaning of elevations in other serum enzymes.3 Elevated GGT can help confirm hepatic origin of elevated ALP or support a suspicion of alcohol use in patients with an AST: ALT ratio >2:1.
If an asymptomatic patient has elevated LFT results, first repeat the test. If repeat results are normal, perform the test again in 3-6 months. Keep in mind, however, that normal LFT results do not always indicate the absence of disease. For example, up to 16% of patients with hepatitis C and 13% of patients with nonalcoholic steatohepatitis (NASH) have normal LFT results despite histologic abnormalities.4
If repeat results are abnormal, obtain the patient’s consent to inform the primary care provider. Then take a thorough history and perform a focused physical exam. In the history, focus on use of prescription and nonprescription medications, including over-the-counter and herbal therapies, alcohol, and drugs of abuse, such as MDMA (“ecstasy”), phencyclidine (“angel dust”), and glues or solvents. Also assess for risk factors for infectious hepatitis, such as IV drug use, work-related blood exposure, and tattoos. Ask about a family history of liver disease. Focus your physical exam on visible stigmata of chronic liver disease, such as jaundice, temporal wasting, ascites, and palmar erythema.
Next, analyze the severity and pattern of the LFT abnormality. Liver injury is defined as:
- ALT >3 times the upper limit of normal
- ALP >2 times the upper limit of normal
- or total bilirubin >2 times the upper limit of normal if associated with any elevation of ALT or ALP.5
If ALT elevations predominate, consider hepatocellular injury. If ALP elevations predominate, suspect cholestatic injury. Elevations of both ALT and ALP suggest a mixed pattern of hepatocellular and cholestatic injury.
Figure 1 Interpreting liver function test results
ALB: albumin; ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; GGT: gamma-glutamyl transpeptidase; HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus; LFT: liver function test; PCP: primary care provider; TBIL: total bilirubin; TP: total protein
CASE CONTINUED: Pinpointing a diagnosis
Mrs. W undergoes repeat LFTs with GGT testing, screening tests for hepatitis B and C, and a comprehensive physical exam. The psychiatrist screens for alcohol use, asks the patient about her use of herbal therapies and substance abuse relapse, and evaluates cognitive mental status for symptoms of encephalopathy. Results reveal that Mrs. W’s ALT and AST are elevated because of chronic active hepatitis C.
Causes of hepatocellular injury
Further evaluation of your patient’s test results can help narrow down potential causes of liver damage. If your patient’s ALT is disproportionately elevated, estimate the:
- severity of aminotransferase elevation
- ratio of AST:ALT
- rate of change over multiple LFTs.
If AST or ALT is >10 times normal, consider toxin-induced or ischemic injury.6 An AST:ALT ratio of 2:1 or 3:1, especially when associated with elevated GGT, strongly suggests alcohol-induced injury. With acute mild transaminase elevations—ALT>AST, 2 to 3 times normal—suspect medication-related injury.
A variety of factors and conditions can result in hepatocellular damage:
Common causes
Medications. Many drugs, including common psychotropics, can cause elevated liver enzymes (Table 2).5 As little as 4 grams per day of acetaminophen can cause mild transaminitis.4 Antidepressants, second-generation antipsychotics (SGAs), and anticonvulsants can cause increases in AST and ALT.7 If liver enzymes rise after a patient starts a new medication, drug-related liver toxicity is likely. Remember to consider a patient’s use of drugs of abuse and herbal therapies.
Discontinuing the suspect agent usually produces steady (although sometimes slow) improvement in LFTs. Use serial LFT testing and focused history and physical examinations to confirm improvement.
Alcohol. Screen for alcohol abuse using the CAGE questionnaire, the Alcohol Use Disorders Identification Test, or a similar tool. More than 90% of patients with an AST:ALT ratio of 2:1 have alcoholic liver disease; this percentage increases to >96% when the ratio is 3:1.1 A 2-fold increase in GGT in a patient with an AST:ALT ratio >2:1 further supports the diagnosis. In patients with alcohol abuse, AST rarely exceeds 10 times normal.5
Hepatitis C. The prevalence of hepatitis C is increasing among patients with severe mental illness, especially a dual diagnosis.8 Hepatitis C rarely causes acute symptoms.
Offer a hepatitis C antibody screening to test patients with even a remote history of IV drug use or comorbid substance abuse. Patients with a positive hepatitis C antibody test or a negative hepatitis C antibody test but a high risk for the disease should receive further testing.9
Hepatitis B. Risk factors include exposure to blood, sexual transmission, and emigration from endemic areas in Southeast Asia and sub-Saharan Africa. Initial screening panels include tests for hepatitis B surface antigen, hepatitis B surface antibody, and hepatitis B core antibody. Positive B surface antigen and core antibody tests indicate infection.
NASH. Nonalcoholic steatohepatitis (NASH) is the most common cause of mild transaminitis in the Western world (Box).4,10,11
Nonalcoholic steatohepatitis (NASH) is inflammatory liver disease of uncertain pathogenesis that commonly occurs with metabolic syndrome. It affects up to 5% of Americans, most often those who are middle-aged and overweight or obese, hyperlipidemic, or diabetic. NASH resembles alcoholic liver disease but occurs in people who drink little or no alcohol. In addition to inflammation, it is characterized by accumulation of fat and fibrous tissue in the liver. Typically patients are asymptomatic, but NASH can lead to cirrhosis.
NASH is a common cause of mild transaminitis. Aminotransferase levels are usually <4 times the normal value.10 Thirteen percent of patients with NASH have normal LFT results despite histologic abnormalities.4 NASH is a diagnosis of exclusion that is confirmed by liver biopsy.
NASH has no specific therapies or cure. Treatment focuses on controlling associated conditions such as diabetes, obesity, and hyperlipidemia. In obese patients, weight loss is the cornerstone of treatment. If you prescribe a second-generation antipsychotic (SGA) for a patient who has NASH, be aware that SGAs increase the risk of hyperglycemia and dyslipidemia, which can exacerbate NASH.11
Table 2
Medications that affect liver function test (LFT) results
| Medication class | Hepatocellular injury (↑ALT) | Cholestatic injury (↑ALP and ↑ALT) | Mixed injury (↑ALP and ↑TBIL) |
|---|---|---|---|
| Psychotropic | Bupropion, fluoxetine, paroxetine, risperidone, sertraline, trazodone, valproic acid | Chlorpromazine, mirtazapine, tricyclic antidepressants | Amitriptyline, Amitriptyline, phenobarbital, phenytoin, trazodone |
| Cardiovascular | Amiodarone, lisinopril, losartan, statins | Clopidogrel, irbesartan | Captopril, enalapril, verapamil |
| Endocrine | Acarbose, allopurinol | – | – |
| Gastrointestinal | Omeprazole | – | – |
| Herbal remedies | Germander, kava | – | – |
| Anti-infectives | HAART drugs, isoniazid, ketoconazole, pyrazinamide, rifampin, tetracycline, trovafloxacin | Amoxicillin/clavulanic acid, erythromycins, terbinafine | Clindamycin, nitrofurantoin, trimethoprim-sulfamethoxazole |
| Rheumatologic | Acetaminophen, baclofen, methotrexate, NSAIDs | Anabolic steroids | Azathioprine, sulfonamides |
| Others | – | Oral contraceptives, estrogens, phenothiazines | Cyproheptadine, flutamide |
| ALP: alkaline phosphatase; ALT: alanine aminotransferase; HAART: highly active antiretroviral therapy; NSAID: nonsteroidal anti-inflammatory drug; TBIL: total bilirubin | |||
| Source: Reference 5 | |||
Less common causes
Hemochromatosis is an autosomal recessive disease that causes pathologic deposition of iron in the liver, pancreas, and heart and leads to cirrhosis, diabetes, and heart disease. Suspect it in patients with a clinical syndrome and transferrin saturation index >45%.12 A hemochromatosis gene mutation analysis confirms the diagnosis.
Autoimmune hepatitis occurs primarily in women ages 20 to 50 years.13 Because >80% of patients with autoimmune hepatitis have hypergammaglobulinemia, serum protein electrophores is a useful screening test.5
Wilson’s disease is a genetic disorder of biliary copper excretion classically diagnosed in young people with concomitant neurologic or psychiatric conditions. Those affected have low serum ceruloplasmin. Neuropsychiatric symptoms include parkinsonian-like tremor, rigidity, clumsiness of gait, slurred speech, drooling, and inappropriate and uncontrollable grinning (risus sardonicus).8 Psychosis and suicidality also are common in patients with Wilson’s disease.
Alpha-1 antitrypsin deficiency. Alpha-1 antitrypsin is a protein produced primarily in the liver that protects the lungs from neutrophil elastase. Suspect alpha-1 antitrypsin deficiency in patients with abnormal LFTs and emphysema. Low serum alpha-1 antitrypsin confirms the diagnosis.
Celiac disease. Consider celiac disease in patients with chronic diarrhea or abdominal distension and abnormal LFTs. Small bowel biopsy and elevated tissue transglutaminase antibodies and anti-endomysial antibodies confirm the diagnosis.
Causes of cholestatic injury
If your patient has a disproportionate ALP elevation, identify the source of the ALP by testing GGT. GGT levels are elevated in liver disease but not in bone disease. Partial bile duct obstruction is a common cause of ALP elevation. For initial testing, include ultrasonography of the right upper quadrant.
Medications. Many medications can cause biliary stasis and cholestatic LFTs, including mirtazapine, tricyclic antidepressants, anabolic steroids, phenytoin, and estrogens.
Primary sclerosing cholangitis is inflammatory disease of the bile ducts that can lead to cholestasis (blockage of bile transport blockage). Consider it in patients with inflammatory bowel disease. Endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography aid diagnosis.
Primary biliary cirrhosis generally presents in middle-aged women with other autoimmune processes, cholestasis, and pruritus. Consider testing serum antimitochondrial antibodies.
Infiltrative liver diseases such as sarcoidosis, metastatic disease, or lymphoma can also present with cholestasis. Liver imaging is required for these diagnoses.
Causes of mixed injury
If LFT results suggest a mixed injury pattern, focus on the predominant pattern and evaluate the causes listed above. Certain medications typically result in a mixed injury pattern.
Related resources
- American Gastroenterological Association medical position statement: evaluation of liver chemistry tests. www.guideline.gov/summary/summary.aspx?ss=15&doc_id=3492&nbr=002718.
- Johnston DE. Special considerations in interpreting liver function tests. Am Fam Physician 1999;59(8):2223-30.
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Equetro, Tegretol
- Chlorpromazine • Thorazine
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Phenobarbital • Luminal
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Sertraline • Zoloft
- Trazodone • Desyrel
- Valproic acid • Depakene
- Warfarin • Coumadin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Mrs. W, age 53, is referred by her primary provider for consultation on depressive symptoms, including worsening depressed mood, anhedonia, anxiety, and suicidal thoughts for 2 months. She reports at least 2 similar episodes in the past 15 years. Mrs. W has a remote history of IV drug use and history of alcohol abuse, but she attends Alcoholics Anonymous and has 10 years of sobriety. She has no history of hospitalizations for medical illness and denies any medical problems.
Mrs. W is taking amitriptyline, 50 mg, for insomnia. She has no history of manic or psychotic symptoms, and the mental status examination is consistent with major depression. Her past depressive episodes were treated successfully with a medication that she does not recall.
The psychiatrist diagnoses recurrent and severe major depression and prescribes cognitive-behavioral therapy and sertraline, 25 mg/d, titrated to 50 mg/d over the next 2 weeks. Amitriptyline is discontinued.
When the psychiatrist receives Mrs. W’s medical records, electrolytes, complete blood count, thyroid stimulating hormone level, and fasting glucose are within normal limits, but alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are greatly elevated at 250 U/L and 150 U/L, respectively. Progress notes contain no references to liver disease.
Interpreting psychiatric patients’ liver function tests (LFTs) can be challenging, especially in those with polypharmacy, co-occurring substance abuse, or risk factors for viral hepatitis. You can improve collaboration with primary care providers by understanding:
- what an LFT measures
- how to interpret abnormal results
- which conditions to suspect, based on the results.
A standard LFT usually measures several enzymes and proteins, typically ALT, AST, alkaline phosphatase (ALP), total bilirubin (TBIL), albumin (ALB), and total protein (TP). Measures of gamma-glutamyl transpeptidase (GGT) and prothrombin time (PT) are often requested with an LFT. Table 1 provides normal ranges and ranges that indicate liver damage for several of these parameters.1,2
“Liver function test” is a misnomer because LFTs do not directly measure liver function. Rather, they reflect hepatocyte injury or cholestasis (blockage or damage in the biliary system). ALB and PT measure liver synthetic function, but are nonspecific. ALB levels can be altered by nutritional status, protein-losing enteropathies, or nephropathies, whereas PT may be modified by warfarin, vitamin K deficiency, or consumptive coagulopathy.
Table 1
Test results: what’s normal, what suggests liver damage
| Parameter | Description | Normal range | Range indicating liver damage |
|---|---|---|---|
| Alanine aminotransferase (ALT) | Enzyme highly concentrated in the liver | 3 to 30 U/L | >3 times upper limit of normal |
| Alkaline phosphatase (ALP) | Enzyme highly concentrated in the liver, bile ducts, placenta, and bone | 35 to 150 U/L | >2 times upper limit of normal |
| Aspartate aminotransferase (AST) | Enzyme highly concentrated in heart muscle, liver cells, skeletal muscle cells, and (to a lesser degree) other tissues | 11 to 32 U/L | Used to evaluate elevations in other serum enzyme level |
| Gamma-glutamyl transpeptidase (GGT) | Enzyme highly concentrated in the liver, bile ducts, and kidneys | 5 to 40 U/L | Used to evaluate elevations in other serum enzyme levels |
| Total bilirubin (TBIL) | Yellow bile pigment produced when liver processes waste products | 0.3 to 1.1 mg/dL | >2 times upper limit of normal if associated with elevation in ALT or ALP |
| Sources: References 1,2 | |||
CASE CONTINUED: Spotting a pattern of injury
Mrs. W’s elevated ALT and AST levels are of unknown duration. Her AST:ALT ratio is approximately 2:1, suggesting hepatocellular injury.
Interpreting abnormal LFT results
To properly interpret LFTs, consider the patient’s symptoms, physical exam findings, medical history, medical illnesses, potential substance use, risk factors for HIV and viral hepatitis, and medication list. Collaborate with the patient’s primary care provider or facilitate primary care (Figure 1).
ALT and AST are highly concentrated in the liver, but ALT is a more specific indicator of liver injury. For both, levels may vary according to age, sex, and ethnicity but in general, levels <30 U/L are considered normal.1,2
ALP originates predominately from the liver and from bone. Persistently elevated ALP levels in the liver may indicate chronic cholestasis or infiltrative liver disease.
GGT is best used to evaluate the meaning of elevations in other serum enzymes.3 Elevated GGT can help confirm hepatic origin of elevated ALP or support a suspicion of alcohol use in patients with an AST: ALT ratio >2:1.
If an asymptomatic patient has elevated LFT results, first repeat the test. If repeat results are normal, perform the test again in 3-6 months. Keep in mind, however, that normal LFT results do not always indicate the absence of disease. For example, up to 16% of patients with hepatitis C and 13% of patients with nonalcoholic steatohepatitis (NASH) have normal LFT results despite histologic abnormalities.4
If repeat results are abnormal, obtain the patient’s consent to inform the primary care provider. Then take a thorough history and perform a focused physical exam. In the history, focus on use of prescription and nonprescription medications, including over-the-counter and herbal therapies, alcohol, and drugs of abuse, such as MDMA (“ecstasy”), phencyclidine (“angel dust”), and glues or solvents. Also assess for risk factors for infectious hepatitis, such as IV drug use, work-related blood exposure, and tattoos. Ask about a family history of liver disease. Focus your physical exam on visible stigmata of chronic liver disease, such as jaundice, temporal wasting, ascites, and palmar erythema.
Next, analyze the severity and pattern of the LFT abnormality. Liver injury is defined as:
- ALT >3 times the upper limit of normal
- ALP >2 times the upper limit of normal
- or total bilirubin >2 times the upper limit of normal if associated with any elevation of ALT or ALP.5
If ALT elevations predominate, consider hepatocellular injury. If ALP elevations predominate, suspect cholestatic injury. Elevations of both ALT and ALP suggest a mixed pattern of hepatocellular and cholestatic injury.
Figure 1 Interpreting liver function test results
ALB: albumin; ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; GGT: gamma-glutamyl transpeptidase; HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus; LFT: liver function test; PCP: primary care provider; TBIL: total bilirubin; TP: total protein
CASE CONTINUED: Pinpointing a diagnosis
Mrs. W undergoes repeat LFTs with GGT testing, screening tests for hepatitis B and C, and a comprehensive physical exam. The psychiatrist screens for alcohol use, asks the patient about her use of herbal therapies and substance abuse relapse, and evaluates cognitive mental status for symptoms of encephalopathy. Results reveal that Mrs. W’s ALT and AST are elevated because of chronic active hepatitis C.
Causes of hepatocellular injury
Further evaluation of your patient’s test results can help narrow down potential causes of liver damage. If your patient’s ALT is disproportionately elevated, estimate the:
- severity of aminotransferase elevation
- ratio of AST:ALT
- rate of change over multiple LFTs.
If AST or ALT is >10 times normal, consider toxin-induced or ischemic injury.6 An AST:ALT ratio of 2:1 or 3:1, especially when associated with elevated GGT, strongly suggests alcohol-induced injury. With acute mild transaminase elevations—ALT>AST, 2 to 3 times normal—suspect medication-related injury.
A variety of factors and conditions can result in hepatocellular damage:
Common causes
Medications. Many drugs, including common psychotropics, can cause elevated liver enzymes (Table 2).5 As little as 4 grams per day of acetaminophen can cause mild transaminitis.4 Antidepressants, second-generation antipsychotics (SGAs), and anticonvulsants can cause increases in AST and ALT.7 If liver enzymes rise after a patient starts a new medication, drug-related liver toxicity is likely. Remember to consider a patient’s use of drugs of abuse and herbal therapies.
Discontinuing the suspect agent usually produces steady (although sometimes slow) improvement in LFTs. Use serial LFT testing and focused history and physical examinations to confirm improvement.
Alcohol. Screen for alcohol abuse using the CAGE questionnaire, the Alcohol Use Disorders Identification Test, or a similar tool. More than 90% of patients with an AST:ALT ratio of 2:1 have alcoholic liver disease; this percentage increases to >96% when the ratio is 3:1.1 A 2-fold increase in GGT in a patient with an AST:ALT ratio >2:1 further supports the diagnosis. In patients with alcohol abuse, AST rarely exceeds 10 times normal.5
Hepatitis C. The prevalence of hepatitis C is increasing among patients with severe mental illness, especially a dual diagnosis.8 Hepatitis C rarely causes acute symptoms.
Offer a hepatitis C antibody screening to test patients with even a remote history of IV drug use or comorbid substance abuse. Patients with a positive hepatitis C antibody test or a negative hepatitis C antibody test but a high risk for the disease should receive further testing.9
Hepatitis B. Risk factors include exposure to blood, sexual transmission, and emigration from endemic areas in Southeast Asia and sub-Saharan Africa. Initial screening panels include tests for hepatitis B surface antigen, hepatitis B surface antibody, and hepatitis B core antibody. Positive B surface antigen and core antibody tests indicate infection.
NASH. Nonalcoholic steatohepatitis (NASH) is the most common cause of mild transaminitis in the Western world (Box).4,10,11
Nonalcoholic steatohepatitis (NASH) is inflammatory liver disease of uncertain pathogenesis that commonly occurs with metabolic syndrome. It affects up to 5% of Americans, most often those who are middle-aged and overweight or obese, hyperlipidemic, or diabetic. NASH resembles alcoholic liver disease but occurs in people who drink little or no alcohol. In addition to inflammation, it is characterized by accumulation of fat and fibrous tissue in the liver. Typically patients are asymptomatic, but NASH can lead to cirrhosis.
NASH is a common cause of mild transaminitis. Aminotransferase levels are usually <4 times the normal value.10 Thirteen percent of patients with NASH have normal LFT results despite histologic abnormalities.4 NASH is a diagnosis of exclusion that is confirmed by liver biopsy.
NASH has no specific therapies or cure. Treatment focuses on controlling associated conditions such as diabetes, obesity, and hyperlipidemia. In obese patients, weight loss is the cornerstone of treatment. If you prescribe a second-generation antipsychotic (SGA) for a patient who has NASH, be aware that SGAs increase the risk of hyperglycemia and dyslipidemia, which can exacerbate NASH.11
Table 2
Medications that affect liver function test (LFT) results
| Medication class | Hepatocellular injury (↑ALT) | Cholestatic injury (↑ALP and ↑ALT) | Mixed injury (↑ALP and ↑TBIL) |
|---|---|---|---|
| Psychotropic | Bupropion, fluoxetine, paroxetine, risperidone, sertraline, trazodone, valproic acid | Chlorpromazine, mirtazapine, tricyclic antidepressants | Amitriptyline, Amitriptyline, phenobarbital, phenytoin, trazodone |
| Cardiovascular | Amiodarone, lisinopril, losartan, statins | Clopidogrel, irbesartan | Captopril, enalapril, verapamil |
| Endocrine | Acarbose, allopurinol | – | – |
| Gastrointestinal | Omeprazole | – | – |
| Herbal remedies | Germander, kava | – | – |
| Anti-infectives | HAART drugs, isoniazid, ketoconazole, pyrazinamide, rifampin, tetracycline, trovafloxacin | Amoxicillin/clavulanic acid, erythromycins, terbinafine | Clindamycin, nitrofurantoin, trimethoprim-sulfamethoxazole |
| Rheumatologic | Acetaminophen, baclofen, methotrexate, NSAIDs | Anabolic steroids | Azathioprine, sulfonamides |
| Others | – | Oral contraceptives, estrogens, phenothiazines | Cyproheptadine, flutamide |
| ALP: alkaline phosphatase; ALT: alanine aminotransferase; HAART: highly active antiretroviral therapy; NSAID: nonsteroidal anti-inflammatory drug; TBIL: total bilirubin | |||
| Source: Reference 5 | |||
Less common causes
Hemochromatosis is an autosomal recessive disease that causes pathologic deposition of iron in the liver, pancreas, and heart and leads to cirrhosis, diabetes, and heart disease. Suspect it in patients with a clinical syndrome and transferrin saturation index >45%.12 A hemochromatosis gene mutation analysis confirms the diagnosis.
Autoimmune hepatitis occurs primarily in women ages 20 to 50 years.13 Because >80% of patients with autoimmune hepatitis have hypergammaglobulinemia, serum protein electrophores is a useful screening test.5
Wilson’s disease is a genetic disorder of biliary copper excretion classically diagnosed in young people with concomitant neurologic or psychiatric conditions. Those affected have low serum ceruloplasmin. Neuropsychiatric symptoms include parkinsonian-like tremor, rigidity, clumsiness of gait, slurred speech, drooling, and inappropriate and uncontrollable grinning (risus sardonicus).8 Psychosis and suicidality also are common in patients with Wilson’s disease.
Alpha-1 antitrypsin deficiency. Alpha-1 antitrypsin is a protein produced primarily in the liver that protects the lungs from neutrophil elastase. Suspect alpha-1 antitrypsin deficiency in patients with abnormal LFTs and emphysema. Low serum alpha-1 antitrypsin confirms the diagnosis.
Celiac disease. Consider celiac disease in patients with chronic diarrhea or abdominal distension and abnormal LFTs. Small bowel biopsy and elevated tissue transglutaminase antibodies and anti-endomysial antibodies confirm the diagnosis.
Causes of cholestatic injury
If your patient has a disproportionate ALP elevation, identify the source of the ALP by testing GGT. GGT levels are elevated in liver disease but not in bone disease. Partial bile duct obstruction is a common cause of ALP elevation. For initial testing, include ultrasonography of the right upper quadrant.
Medications. Many medications can cause biliary stasis and cholestatic LFTs, including mirtazapine, tricyclic antidepressants, anabolic steroids, phenytoin, and estrogens.
Primary sclerosing cholangitis is inflammatory disease of the bile ducts that can lead to cholestasis (blockage of bile transport blockage). Consider it in patients with inflammatory bowel disease. Endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography aid diagnosis.
Primary biliary cirrhosis generally presents in middle-aged women with other autoimmune processes, cholestasis, and pruritus. Consider testing serum antimitochondrial antibodies.
Infiltrative liver diseases such as sarcoidosis, metastatic disease, or lymphoma can also present with cholestasis. Liver imaging is required for these diagnoses.
Causes of mixed injury
If LFT results suggest a mixed injury pattern, focus on the predominant pattern and evaluate the causes listed above. Certain medications typically result in a mixed injury pattern.
Related resources
- American Gastroenterological Association medical position statement: evaluation of liver chemistry tests. www.guideline.gov/summary/summary.aspx?ss=15&doc_id=3492&nbr=002718.
- Johnston DE. Special considerations in interpreting liver function tests. Am Fam Physician 1999;59(8):2223-30.
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Equetro, Tegretol
- Chlorpromazine • Thorazine
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Phenobarbital • Luminal
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Sertraline • Zoloft
- Trazodone • Desyrel
- Valproic acid • Depakene
- Warfarin • Coumadin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med 2002;137(1):1-10.
2. Gopal DV, Rosen HR. Abnormal findings on liver function tests. Interpreting results to narrow the diagnosis and establish a prognosis. Postgrad Med 2000;107(2):100-14.
3. Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med 2000;342(17):1266-71.
4. Ioannou GN, Boyko EJ, Lee SP. The prevalence and predictors of elevated serum aminotransferase activity in the United States in 1999-2002. Am J Gastroenterol 2006;101(1):76-82.
5. Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med 2006;354(7):731-9.
6. Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005;172(3):367-79.
7. Bezchilibny-Butler KZ, Jeffries JJ, eds. Clinical handbook of psychotropic drugs, 15th ed. Cambridge Hogrefe & Huber; 2005.
8. Crone CC, Gabriel GM, Dimartini A. An overview of psychiatric issues in liver disease for the consultation-liaison psychiatrist. Psychosomatics 2006;47(3):188-205.
9. Kaplan MA. Approach to the patient with abnormal liver function tests. Available at: http://www.uptodate.com. Accessed December 12, 2006.
10. Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 1994;107(4):1103-9.
11. Lieberman JA, Stroup SS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353(12):1209-23.
12. Yen AW, Fancher TL, Bowlus CL. Revisiting hereditary hemochromatosis: current concepts and progress. Am J Med 2006;119(5):391-9.
13. Krawitt EL. Autoimmune hepatitis. N Engl J Med 1996;334(14):897-903.
1. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med 2002;137(1):1-10.
2. Gopal DV, Rosen HR. Abnormal findings on liver function tests. Interpreting results to narrow the diagnosis and establish a prognosis. Postgrad Med 2000;107(2):100-14.
3. Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med 2000;342(17):1266-71.
4. Ioannou GN, Boyko EJ, Lee SP. The prevalence and predictors of elevated serum aminotransferase activity in the United States in 1999-2002. Am J Gastroenterol 2006;101(1):76-82.
5. Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med 2006;354(7):731-9.
6. Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005;172(3):367-79.
7. Bezchilibny-Butler KZ, Jeffries JJ, eds. Clinical handbook of psychotropic drugs, 15th ed. Cambridge Hogrefe & Huber; 2005.
8. Crone CC, Gabriel GM, Dimartini A. An overview of psychiatric issues in liver disease for the consultation-liaison psychiatrist. Psychosomatics 2006;47(3):188-205.
9. Kaplan MA. Approach to the patient with abnormal liver function tests. Available at: http://www.uptodate.com. Accessed December 12, 2006.
10. Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 1994;107(4):1103-9.
11. Lieberman JA, Stroup SS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353(12):1209-23.
12. Yen AW, Fancher TL, Bowlus CL. Revisiting hereditary hemochromatosis: current concepts and progress. Am J Med 2006;119(5):391-9.
13. Krawitt EL. Autoimmune hepatitis. N Engl J Med 1996;334(14):897-903.