User login
- The incision should be considered as a second surgical procedure, which temporarily interferes with normal abdominal wall function.
- The midline incision provides excellent exposure to all areas of the abdomen and retroperitoneum, which can be accessed with minimal risk of significant vascular or nerve injury.
- Transverse incisions create less tension on the opposing skin edges because the incision follows Langer’s lines. The incidence of incisional hernias and wound dehiscence has been reported to be lower, but these studies are not randomized.
An abdominal incision often is given little thought other than as an access site through which a surgical procedure is performed. In reality, the incision is a second surgical procedure, which interferes—at least temporarily—with normal abdominal wall function.
While most physicians concur that the essential elements of a well-planned incision include adequate access to anticipated pathology, extensibility, and security of closure, many may not consider preservation of abdominal wall function as a key factor in their decision-making. Additional considerations include certainty of diagnosis, speed of entry, body habitus, presence of previous scars, potential for problems with hemostasis, and cosmetic outcome. These factors are the key determinants of whether the incision will be longitudinal (midline or paramedian) or transverse (Pfannenstiel’s, Cherney’s, or Maylard’s). For most gynecologic procedures confined to the pelvis, either option may be considered. The exceptions are patients with uncertain diagnoses or when access to the upper abdomen is indicated.
Regardless of the type of incision selected, the skin should be incised with a single, clean stroke of a sharp scalpel. However, when it comes to dissecting the underlying subcutaneous tissues, the debate continues over whether a scalpel or electrosurgery is best. While I recently have switched to the latter, here is a look at what the data say: Johnson and Serpell demonstrated that electrosurgery is associated with faster hemostasis, with no difference in the incidence of wound infection.1 Similarly, a recent randomized trial by Kearns et al found electro-surgery causes less blood loss and does not increase the risk of wound infections or fascial dehiscence.2 In contrast, a large prospective study by Cruse et al suggested that the use of diathermy is associated with twice the wound infection rate.3
This controversy also involves patients with gynecologic malignancies. Kolb et al found that electrosurgery was an independent risk factor for wound complications following surgery for ovarian cancer.4 However, Franchi and colleagues reported no difference in the rate of wound complications between scalpel and diathermy in patients who underwent mid-line abdominal incisions for the treatment of uterine cancer.5
Use the midline when the diagnosis and the extent of surgery are uncertain.
The inconsistencies in the data may reflect differences in electrosurgical technique. Non-modulated (cutting) current concentrates energy, vaporizing the tissue with little heat injury to surrounding areas. Conversely, modulated (coagulating) current coagulates the tissue with heat-producing char over a large area, and tissue injury often extends beyond the char. This effect is magnified if the electrode comes in direct contact with the tissue. Use the arc, rather than direct contact, to prevent excessive devitalization of tissue.
This article will review the techniques for, as well as the rationale and disadvantages of, common incisions—both longitudinal and transverse—to help the gynecologic surgeon minimize morbidity and maximize outcomes.
Longitudinal incisions
The longitudinal incisions that will be reviewed here are the midline (median) and paramedian. Classically, it was thought that longitudinal incisions were at greater risk of dehiscence than transverse incisions.6 However, it is difficult to make legitimate comparisons since longitudinal incisions are more likely to be performed in cases of hemorrhage, trauma, sepsis, multiorgan disease, previous surgery, previous radiation therapy, and malignancy—all of which increase the likelihood of postoperative complications. Furthermore, prospective and randomized studies have shown little, if any, difference in the incidence of dehiscence and hernias between longitudinal and transverse incisions.6-8
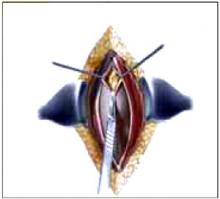
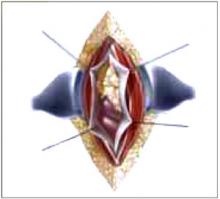
MidlineTechnique. Initiate the midline as a low abdominal incision (approximately 2 cm above the pubic symphysis), cutting along the linea alba. To extend the incision, if necessary, continue the dissection to the left of the umbilicus to avoid the ligamentum teres. Open the peritoneum at the cephalad pole of the incision (Figure 1). Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity (Figure 2).
Rationale. While this incision can be used for any surgical procedure, it is especially appropriate when the diagnosis is uncertain and the exact procedure or extent of surgery is unclear. It is an excellent choice when access to the upper abdomen may be necessary, e.g., patients with gynecologic malignancies who may need assessment of the diaphragm, liver biopsy, para-aortic node biopsy, omentectomy, or debulking procedures. Patients with benign gynecologic conditions also may benefit from a midline incision. For example, when pelvic anatomy is distorted, as with severe endometriosis or sepsis, recognizable anatomy may be found only above the pelvic brim.
A midline incision allows the quickest entry, which is especially important for an unstable or seriously ill patient. Exposure is excellent, as all areas of the abdomen and retroperitoneum can be accessed with minimal risk of significant vascular or nerve injury. This is because only terminal branches of the abdominal wall blood vessels and nerves are located at the linea alba. In addition, because deep tissue planes are not opened, this incision may be ideal for patients who are anticoagulated, have enlarged epigastric vessels that are more susceptible to injury, or have an intraabdominal infection.
Transverse incisions help reduce the rate of wound dehiscence.
Disadvantages. Two potential problems are the higher rate of hernia formation and wound dehiscence, which may be due to constant lateral tension, compared with transverse incisions. In addition, coughing, retching, and straining may exacerbate the lateral tension. Proper suture selection can reduce the incidence of complications. As previously mentioned, the reality of these disadvantages is subject to debate; further studies are needed to determine the true risk.
From a cosmetic standpoint, the midline scar often is prominent because the incision transects Langer’s lines. Hence, it cannot be concealed by lingerie or swimwear.
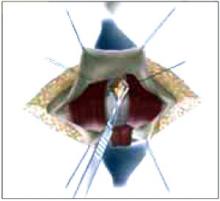
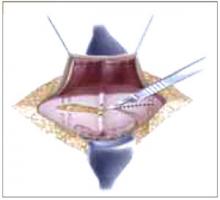
FIGURE 1 Midline incision
After incising the linea alba and separating the muscles in the midline, open the peritoneum at the cephalad pole of the incision.
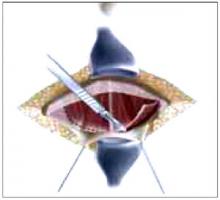
FIGURE 2 Midline incision
Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity.
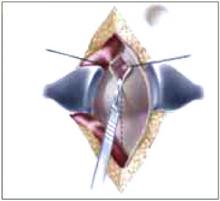
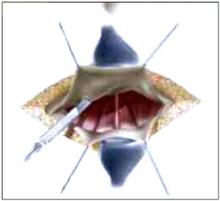
ParamedianTechnique. Place this incision 2 to 5 cm to the left or right of the midline, depending on the indication for surgery. After dissecting the skin and subcutaneous layers, incise the anterior rectus sheath vertically over the rectus abdominis muscle (Figure 3) and dissect it from the medial muscle edge. Retract the muscle laterally to expose the posterior rectus sheath and then incise the sheath and the peritoneum vertically to expose the peritoneal cavity (Figure 4). Alternatively, a more lateral paramedian incision can be placed over the rectus abdominis muscle. In this case, however, the rectus muscle should be separated vertically, instead of retracted laterally, to expose the posterior rectus sheath.
Rationale. Paramedian incisions provide excellent exposure of the pelvis, excluding the upper abdomen. Therefore, consider this technique when the procedure will be confined to the ipsilateral pelvis, e.g., rightor left-side lymph node biopsies and exposure of the sigmoid colon on the left. Also, a paramedian incision at the level of the umbilicus can be used for a cesarean delivery or a hysterectomy.
This incision is the best choice when performing pelvic surgery on morbidly obese patients. By placing the incision low on the abdomen, the large panniculus can be retracted over the mons pubis and thighs, providing excellent exposure of the pelvis.
Disadvantages. Some researchers have reported that muscle-splitting lateral paramedian incisions have a lower incidence of incisional hernias compared with midline incisions.7,9 However, they take longer to perform and restrict access to the contralateral pelvis. In addition, the risk of vascular injury and hematomas is increased, especially in the lower pole where branches of the epigastric arteries penetrate the muscle.
With regard to nerve injury, terminal nerves are cut, resulting in paralysis of the inner portion of the rectus abdominis muscle. This paralysis can be permanent, as the muscle medial to the vertical separation is involved. However, if only the medial third of the muscle is denervated, the paralysis rarely limits function.
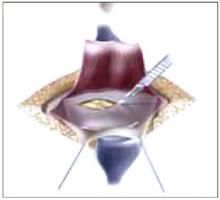
FIGURE 3 Paramedian incision
Place the incision 2 to 5 cm to the left or right of the midline. Incise the anterior rectus sheath vertically over the rectus abdominis muscle.
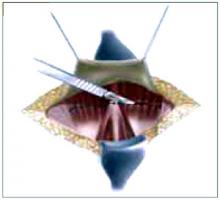
FIGURE 4 Paramedian incision
Retract the muscle laterally to expose the posterior sheath; then incise the sheath and the peritoneum vertically to expose the pelvic cavity.
Transverse incisions
Transverse incisions such as Pfannenstiel’s (muscle separating), Cherney’s (tendon detaching), and Maylard’s (muscle cutting) were developed to reduce the incidence of incisional hernias and wound dehiscence. Their success lies in the fact that they cause less tension on the opposing wound edges because the incisions follow Langer’s lines, unlike longitudinal incisions. Their placement also allows for a better cosmetic outcome. Because they can be placed in the pubic hairline or in a natural skin crease, they are easily concealed by lingerie or swimwear. However, the incision should not be placed in a deep skin fold of a large panniculus where maceration of the skin can increase the risk of infection.
The main disadvantages of transverse incisions are limited exposure of the upper abdomen and limited extensibility. Further, because more tissue planes are opened and more vessels are encountered, these incisions increase the risk of hematomas and infection.
Pfannenstiel’sTechnique. Incise the skin and subcutaneous tissues 2 to 5 cm above the pubic symphysis.10 Then dissect the rectus sheath transversely, separating it sharply from the rectus muscle at the linea alba and retracting it superiorly toward the umbilicus and inferiorly toward the pubic symphysis (Figure 5). Divide the rectus abdominis muscle along the midline raphe and retract it laterally, exposing the transversalis fascia and the posterior rectus sheath. Incise these layers and the peritoneum vertically to expose the peritoneal cavity (Figure 6).
To minimize retraction of the rectus abdominus muscle during Maylard’s, do not separate it from the anterior rectus sheath.
Rationale. Since exposure is limited and the incision can be only minimally extended, this incision is appropriate for procedures that are limited to the pelvis, e.g., abdominal hysterectomy, cesarean delivery, retropubic urethropexy, and paravaginal defect repairs. (Extension of the incision can be achieved by modifying it to Cherney’s incision.)
Disadvantages. The fact that the incision severs multiple tissue planes is an advantage as well as a disadvantage. Postoperative dehiscence and incisional hernias are rare because the closed wound has a high tensile strength. However, the incidence of inguinal hernias may increase when the incision is placed close to the external inguinal ring,11 and very low incisions may increase the risk of femoral nerve injury.12 The ilioinguinal and iliohypogastric nerves may be damaged, especially if the rectus incision is extended far laterally. Most commonly, they are trapped in the suture during closure, producing postoperative pain. Incising multiple layers also slows entry and increases the risk of seromas, hematomas, and wound infections.
This approach is contraindicated when time is of the essence, e.g., hemorrhage, or in the face of an abdominal infection, e.g., sepsis.
FIGURE 5 Pfannenstiel’s incision
After incising the skin and subcutaneous tissues, dissect the rectus sheath transversely, separating it sharply from the rectus muscle.
FIGURE 6 Pfannenstiel’s incision
Divide and retract the rectus abdominus muscle and then incise the tranversalis fascia and posterior rectus sheath vertically.
Cherney’sTechnique. Dissect the skin and subcutaneous tissue 2 to 3 cm above the pubic symphysis, which is lower than most Pfannenstiel’s incisions. Then incise the anterior rectus sheath transversely and dissect it from the rectus abdominis muscle superiorly and inferiorly. Using blunt dissection, separate the rectus and pyramidalis muscles from the underlying bladder and adventitial tissue. Then incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis (Figure 7). (This segment of tendon facilitates the reattachment of the muscles at closure.) Retract the muscles and tendons cephalad to expose the retropubic space. Incise the peritoneum transversely to expose the peritoneal cavity (Figure 8).
Rationale. Cherney’s incision provides excellent access to the retropubic space of Retzius, making it a good choice for retropubic urethropexy and paravaginal repair. Exposure is the main advantage to Cherney’s incision. The reason: It is a modification of Pfannenstiel’s incision and, as such, provides excellent lateral exposure because it is placed much lower on the abdominal wall.
Disadvantages. The benefits and risks of this incision are similar to those of Pfannenstiel’s incision since the same tissue planes are opened. However, it is more time consuming due to the dissection required to separate the muscles and tendons from the underlying tissues.
In addition, the deep inferior epigastric arteries could be injured as a result of the lateral dissection. Lastly, reattachment of the tendons is tedious.
FIGURE 7 Cherney’s incision
Incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis.
FIGURE 8 Cherney’s incision
Retract the muscles and tendons cephalad and incise the peritoneum transversely to expose the peritoneal cavity.
Maylard’sTechnique. After transecting the skin and subcutaneous layers in a plane at the level of the anterior superior iliac spine, incise the rectus sheath transversely and extend the incision through the aponeuroses of the abdominal muscles to about 2 to 3 cm medial to the anterior iliac crest. Then dissect the rectus abdominis muscle transversely with a scalpel, electrocautery, or surgical stapler (Figure 9). To minimize retraction of this muscle, do not separate it from the anterior rectus sheath. (Alternatively, many surgeons recommend that the cut edge of the muscle be secured to the anterior sheath with mattress sutures to prevent retraction and reduce blood loss.)
Prior to transecting the peritoneum, isolate, ligate, and divide the deep inferior epigastric vessels. (Patients with significant aortoiliac atherosclerosis or aortic coarctation develop considerable collateral circulation through the epigastric vessels for perfusion of the lower extremities. Ligating these vessels may cause claudication and even lifethreatening ischemia. Therefore, assess iliac flow before ligating and transecting the arteries.) Then transect the transversalis fascia and peritoneum transversely, allowing access to the peritoneal cavity (Figure 10).
Rationale. Many oncologists use this approach for pelvic lymphadenectomy and staging procedures because the exposure to the lateral pelvis is excellent. The reason: This transverse incision cuts through all layers of the abdominal wall at the level of the anterior iliac spine. It also may be appropriate when pelvic pathology extends to the sidewall, e.g., endometriosis.
It is advisable to place a drain prior to closing Maylard’s.
Physicians should consider using this approach more than they currently are, especially when Pfannenstiel’s incision cannot provide satisfactory exposure or a longitudinal incision is thought to be the only alternative. The decision to use Maylard’s incision should be planned during the preoperative assessment, as Pfannenstiel’s incision should not be modified to Maylard’s intraoperatively.
Disadvantages. Although Maylard’s incision improves access to the upper abdomen compared to other transverse incisions, exposure is still limited. In addition, trauma to the deep epigastric arteries may result in considerable hemorrhage. And since hematomas commonly infiltrate the retroperitoneal space, large quantities of blood already may be lost before the hemorrhage is clinically apparent. Finally, oozing from the cut edge of the muscles may result in significant fluid collection, increasing the risk of infection. Therefore, it is advisable to place a drain prior to closure.
Like other transverse incisions, the wound parallels the nerves, providing a measure of protection. However, the rectus incision approaches the anterior iliac spine, where both the ilioinguinal and iliohypogastric nerves lie. Both may be damaged during the incision and can become entrapped during closure. Additionally, the femoral nerve, the lateral femoral cutaneous nerve, and the genitofemoral nerve are easily compressed by the lateral blades of the retractors because of the extreme lateral positions of the incision’s poles. Injury to these nerves can result in paresthesia, pain, and paralysis of the leg muscles.
FIGURE 9 Maylard’s incision
After incising the aponeuroses of the abdominal muscles medial to the anterior iliac crest, dissect the rectus abdominus muscle transversely.
FIGURE 10 Maylard’s incision
Isolate, ligate, and divide the epigastric vessels. Then incise the transversalis fascia and peritoneum transversely to access the peritoneal cavity.
In summary
While the midline and Pfannenstiel’s incisions are an integral part of the gynecologic surgeon’s armamentarium, the paramedian and Maylard’s incisions should be added to the repertoire because these incisions can greatly enhance exposure. The paramedian shares the advantages of the midline incision but also allows better access to the ipsilateral pelvis. Furthermore, although Maylard’s incision takes longer to perform than other techniques, the excellent exposure—both laterally and superiorly—makes it worthwhile.
The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Johnson CD, Serpell JW. Wound infection after abdominal incision with scalpel or diathermy. Br J Surg. 1990;77:626-627.
2. Cruse PJE, Ford R. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27.-
3. Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg. 2001;88(1):41-44.
4. Kolb BA, Buller RE, Connoer JP, et al. Effects of early postoperative chemotherapy on wound healing. Obstet Gynecol. 1992;79:988-992.
5. Franchi M, Ghezzi F, Bendetti-Panici PL, et al. A multicenter collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg. 2001;181(2):128-132.
6. Hendrix SL, Schimp V, Martin J. The legendary superior strength of the Pfannenstiel incision: a myth? Am J Obstet Gynecol. 2000;182(6):1446-1451.
7. Ellis H, Coleridge-Smith PD, Joyce AD. Abdominal incisions—vertical or transverse? Postgrad Med J. 1984;60:407-410.
8. Sanders RJ, DiClementi D. Principles of abdominal wound closure. II. Prevention of wound dehiscence. Arch Surg. 1977;112:1188.-
9. Donaldson DR, Hegarty JH, Brennan TG, et al. The lateral paramedian incision-experience with 850 cases. Br J Surg. 1982;69:630.-
10. Greenall MJ, et al. Midline or transverse laparotomy? A random controlled clinical trial. Part I: Influence on healing. Br J Surg. 1980;7:188.-
11. Pfannenstiel J. Ueber die Vortheile des suprasymphysaren Fascienquerschnitts für die gynakologischen Koliotomien zugleich ein Beitrag zu der Indikationsstellung der Operationswege. Samml Klin Vortr (Leipzig). 1900;268:1735.-
12. Griffiths DA. A reappraisal of the Pfannenstiel incision. Br J Urol. 1976;48:469.-
- The incision should be considered as a second surgical procedure, which temporarily interferes with normal abdominal wall function.
- The midline incision provides excellent exposure to all areas of the abdomen and retroperitoneum, which can be accessed with minimal risk of significant vascular or nerve injury.
- Transverse incisions create less tension on the opposing skin edges because the incision follows Langer’s lines. The incidence of incisional hernias and wound dehiscence has been reported to be lower, but these studies are not randomized.
An abdominal incision often is given little thought other than as an access site through which a surgical procedure is performed. In reality, the incision is a second surgical procedure, which interferes—at least temporarily—with normal abdominal wall function.
While most physicians concur that the essential elements of a well-planned incision include adequate access to anticipated pathology, extensibility, and security of closure, many may not consider preservation of abdominal wall function as a key factor in their decision-making. Additional considerations include certainty of diagnosis, speed of entry, body habitus, presence of previous scars, potential for problems with hemostasis, and cosmetic outcome. These factors are the key determinants of whether the incision will be longitudinal (midline or paramedian) or transverse (Pfannenstiel’s, Cherney’s, or Maylard’s). For most gynecologic procedures confined to the pelvis, either option may be considered. The exceptions are patients with uncertain diagnoses or when access to the upper abdomen is indicated.
Regardless of the type of incision selected, the skin should be incised with a single, clean stroke of a sharp scalpel. However, when it comes to dissecting the underlying subcutaneous tissues, the debate continues over whether a scalpel or electrosurgery is best. While I recently have switched to the latter, here is a look at what the data say: Johnson and Serpell demonstrated that electrosurgery is associated with faster hemostasis, with no difference in the incidence of wound infection.1 Similarly, a recent randomized trial by Kearns et al found electro-surgery causes less blood loss and does not increase the risk of wound infections or fascial dehiscence.2 In contrast, a large prospective study by Cruse et al suggested that the use of diathermy is associated with twice the wound infection rate.3
This controversy also involves patients with gynecologic malignancies. Kolb et al found that electrosurgery was an independent risk factor for wound complications following surgery for ovarian cancer.4 However, Franchi and colleagues reported no difference in the rate of wound complications between scalpel and diathermy in patients who underwent mid-line abdominal incisions for the treatment of uterine cancer.5
Use the midline when the diagnosis and the extent of surgery are uncertain.
The inconsistencies in the data may reflect differences in electrosurgical technique. Non-modulated (cutting) current concentrates energy, vaporizing the tissue with little heat injury to surrounding areas. Conversely, modulated (coagulating) current coagulates the tissue with heat-producing char over a large area, and tissue injury often extends beyond the char. This effect is magnified if the electrode comes in direct contact with the tissue. Use the arc, rather than direct contact, to prevent excessive devitalization of tissue.
This article will review the techniques for, as well as the rationale and disadvantages of, common incisions—both longitudinal and transverse—to help the gynecologic surgeon minimize morbidity and maximize outcomes.
Longitudinal incisions
The longitudinal incisions that will be reviewed here are the midline (median) and paramedian. Classically, it was thought that longitudinal incisions were at greater risk of dehiscence than transverse incisions.6 However, it is difficult to make legitimate comparisons since longitudinal incisions are more likely to be performed in cases of hemorrhage, trauma, sepsis, multiorgan disease, previous surgery, previous radiation therapy, and malignancy—all of which increase the likelihood of postoperative complications. Furthermore, prospective and randomized studies have shown little, if any, difference in the incidence of dehiscence and hernias between longitudinal and transverse incisions.6-8
MidlineTechnique. Initiate the midline as a low abdominal incision (approximately 2 cm above the pubic symphysis), cutting along the linea alba. To extend the incision, if necessary, continue the dissection to the left of the umbilicus to avoid the ligamentum teres. Open the peritoneum at the cephalad pole of the incision (Figure 1). Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity (Figure 2).
Rationale. While this incision can be used for any surgical procedure, it is especially appropriate when the diagnosis is uncertain and the exact procedure or extent of surgery is unclear. It is an excellent choice when access to the upper abdomen may be necessary, e.g., patients with gynecologic malignancies who may need assessment of the diaphragm, liver biopsy, para-aortic node biopsy, omentectomy, or debulking procedures. Patients with benign gynecologic conditions also may benefit from a midline incision. For example, when pelvic anatomy is distorted, as with severe endometriosis or sepsis, recognizable anatomy may be found only above the pelvic brim.
A midline incision allows the quickest entry, which is especially important for an unstable or seriously ill patient. Exposure is excellent, as all areas of the abdomen and retroperitoneum can be accessed with minimal risk of significant vascular or nerve injury. This is because only terminal branches of the abdominal wall blood vessels and nerves are located at the linea alba. In addition, because deep tissue planes are not opened, this incision may be ideal for patients who are anticoagulated, have enlarged epigastric vessels that are more susceptible to injury, or have an intraabdominal infection.
Transverse incisions help reduce the rate of wound dehiscence.
Disadvantages. Two potential problems are the higher rate of hernia formation and wound dehiscence, which may be due to constant lateral tension, compared with transverse incisions. In addition, coughing, retching, and straining may exacerbate the lateral tension. Proper suture selection can reduce the incidence of complications. As previously mentioned, the reality of these disadvantages is subject to debate; further studies are needed to determine the true risk.
From a cosmetic standpoint, the midline scar often is prominent because the incision transects Langer’s lines. Hence, it cannot be concealed by lingerie or swimwear.
FIGURE 1 Midline incision
After incising the linea alba and separating the muscles in the midline, open the peritoneum at the cephalad pole of the incision.
FIGURE 2 Midline incision
Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity.
ParamedianTechnique. Place this incision 2 to 5 cm to the left or right of the midline, depending on the indication for surgery. After dissecting the skin and subcutaneous layers, incise the anterior rectus sheath vertically over the rectus abdominis muscle (Figure 3) and dissect it from the medial muscle edge. Retract the muscle laterally to expose the posterior rectus sheath and then incise the sheath and the peritoneum vertically to expose the peritoneal cavity (Figure 4). Alternatively, a more lateral paramedian incision can be placed over the rectus abdominis muscle. In this case, however, the rectus muscle should be separated vertically, instead of retracted laterally, to expose the posterior rectus sheath.
Rationale. Paramedian incisions provide excellent exposure of the pelvis, excluding the upper abdomen. Therefore, consider this technique when the procedure will be confined to the ipsilateral pelvis, e.g., rightor left-side lymph node biopsies and exposure of the sigmoid colon on the left. Also, a paramedian incision at the level of the umbilicus can be used for a cesarean delivery or a hysterectomy.
This incision is the best choice when performing pelvic surgery on morbidly obese patients. By placing the incision low on the abdomen, the large panniculus can be retracted over the mons pubis and thighs, providing excellent exposure of the pelvis.
Disadvantages. Some researchers have reported that muscle-splitting lateral paramedian incisions have a lower incidence of incisional hernias compared with midline incisions.7,9 However, they take longer to perform and restrict access to the contralateral pelvis. In addition, the risk of vascular injury and hematomas is increased, especially in the lower pole where branches of the epigastric arteries penetrate the muscle.
With regard to nerve injury, terminal nerves are cut, resulting in paralysis of the inner portion of the rectus abdominis muscle. This paralysis can be permanent, as the muscle medial to the vertical separation is involved. However, if only the medial third of the muscle is denervated, the paralysis rarely limits function.
FIGURE 3 Paramedian incision
Place the incision 2 to 5 cm to the left or right of the midline. Incise the anterior rectus sheath vertically over the rectus abdominis muscle.
FIGURE 4 Paramedian incision
Retract the muscle laterally to expose the posterior sheath; then incise the sheath and the peritoneum vertically to expose the pelvic cavity.
Transverse incisions
Transverse incisions such as Pfannenstiel’s (muscle separating), Cherney’s (tendon detaching), and Maylard’s (muscle cutting) were developed to reduce the incidence of incisional hernias and wound dehiscence. Their success lies in the fact that they cause less tension on the opposing wound edges because the incisions follow Langer’s lines, unlike longitudinal incisions. Their placement also allows for a better cosmetic outcome. Because they can be placed in the pubic hairline or in a natural skin crease, they are easily concealed by lingerie or swimwear. However, the incision should not be placed in a deep skin fold of a large panniculus where maceration of the skin can increase the risk of infection.
The main disadvantages of transverse incisions are limited exposure of the upper abdomen and limited extensibility. Further, because more tissue planes are opened and more vessels are encountered, these incisions increase the risk of hematomas and infection.
Pfannenstiel’sTechnique. Incise the skin and subcutaneous tissues 2 to 5 cm above the pubic symphysis.10 Then dissect the rectus sheath transversely, separating it sharply from the rectus muscle at the linea alba and retracting it superiorly toward the umbilicus and inferiorly toward the pubic symphysis (Figure 5). Divide the rectus abdominis muscle along the midline raphe and retract it laterally, exposing the transversalis fascia and the posterior rectus sheath. Incise these layers and the peritoneum vertically to expose the peritoneal cavity (Figure 6).
To minimize retraction of the rectus abdominus muscle during Maylard’s, do not separate it from the anterior rectus sheath.
Rationale. Since exposure is limited and the incision can be only minimally extended, this incision is appropriate for procedures that are limited to the pelvis, e.g., abdominal hysterectomy, cesarean delivery, retropubic urethropexy, and paravaginal defect repairs. (Extension of the incision can be achieved by modifying it to Cherney’s incision.)
Disadvantages. The fact that the incision severs multiple tissue planes is an advantage as well as a disadvantage. Postoperative dehiscence and incisional hernias are rare because the closed wound has a high tensile strength. However, the incidence of inguinal hernias may increase when the incision is placed close to the external inguinal ring,11 and very low incisions may increase the risk of femoral nerve injury.12 The ilioinguinal and iliohypogastric nerves may be damaged, especially if the rectus incision is extended far laterally. Most commonly, they are trapped in the suture during closure, producing postoperative pain. Incising multiple layers also slows entry and increases the risk of seromas, hematomas, and wound infections.
This approach is contraindicated when time is of the essence, e.g., hemorrhage, or in the face of an abdominal infection, e.g., sepsis.
FIGURE 5 Pfannenstiel’s incision
After incising the skin and subcutaneous tissues, dissect the rectus sheath transversely, separating it sharply from the rectus muscle.
FIGURE 6 Pfannenstiel’s incision
Divide and retract the rectus abdominus muscle and then incise the tranversalis fascia and posterior rectus sheath vertically.
Cherney’sTechnique. Dissect the skin and subcutaneous tissue 2 to 3 cm above the pubic symphysis, which is lower than most Pfannenstiel’s incisions. Then incise the anterior rectus sheath transversely and dissect it from the rectus abdominis muscle superiorly and inferiorly. Using blunt dissection, separate the rectus and pyramidalis muscles from the underlying bladder and adventitial tissue. Then incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis (Figure 7). (This segment of tendon facilitates the reattachment of the muscles at closure.) Retract the muscles and tendons cephalad to expose the retropubic space. Incise the peritoneum transversely to expose the peritoneal cavity (Figure 8).
Rationale. Cherney’s incision provides excellent access to the retropubic space of Retzius, making it a good choice for retropubic urethropexy and paravaginal repair. Exposure is the main advantage to Cherney’s incision. The reason: It is a modification of Pfannenstiel’s incision and, as such, provides excellent lateral exposure because it is placed much lower on the abdominal wall.
Disadvantages. The benefits and risks of this incision are similar to those of Pfannenstiel’s incision since the same tissue planes are opened. However, it is more time consuming due to the dissection required to separate the muscles and tendons from the underlying tissues.
In addition, the deep inferior epigastric arteries could be injured as a result of the lateral dissection. Lastly, reattachment of the tendons is tedious.
FIGURE 7 Cherney’s incision
Incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis.
FIGURE 8 Cherney’s incision
Retract the muscles and tendons cephalad and incise the peritoneum transversely to expose the peritoneal cavity.
Maylard’sTechnique. After transecting the skin and subcutaneous layers in a plane at the level of the anterior superior iliac spine, incise the rectus sheath transversely and extend the incision through the aponeuroses of the abdominal muscles to about 2 to 3 cm medial to the anterior iliac crest. Then dissect the rectus abdominis muscle transversely with a scalpel, electrocautery, or surgical stapler (Figure 9). To minimize retraction of this muscle, do not separate it from the anterior rectus sheath. (Alternatively, many surgeons recommend that the cut edge of the muscle be secured to the anterior sheath with mattress sutures to prevent retraction and reduce blood loss.)
Prior to transecting the peritoneum, isolate, ligate, and divide the deep inferior epigastric vessels. (Patients with significant aortoiliac atherosclerosis or aortic coarctation develop considerable collateral circulation through the epigastric vessels for perfusion of the lower extremities. Ligating these vessels may cause claudication and even lifethreatening ischemia. Therefore, assess iliac flow before ligating and transecting the arteries.) Then transect the transversalis fascia and peritoneum transversely, allowing access to the peritoneal cavity (Figure 10).
Rationale. Many oncologists use this approach for pelvic lymphadenectomy and staging procedures because the exposure to the lateral pelvis is excellent. The reason: This transverse incision cuts through all layers of the abdominal wall at the level of the anterior iliac spine. It also may be appropriate when pelvic pathology extends to the sidewall, e.g., endometriosis.
It is advisable to place a drain prior to closing Maylard’s.
Physicians should consider using this approach more than they currently are, especially when Pfannenstiel’s incision cannot provide satisfactory exposure or a longitudinal incision is thought to be the only alternative. The decision to use Maylard’s incision should be planned during the preoperative assessment, as Pfannenstiel’s incision should not be modified to Maylard’s intraoperatively.
Disadvantages. Although Maylard’s incision improves access to the upper abdomen compared to other transverse incisions, exposure is still limited. In addition, trauma to the deep epigastric arteries may result in considerable hemorrhage. And since hematomas commonly infiltrate the retroperitoneal space, large quantities of blood already may be lost before the hemorrhage is clinically apparent. Finally, oozing from the cut edge of the muscles may result in significant fluid collection, increasing the risk of infection. Therefore, it is advisable to place a drain prior to closure.
Like other transverse incisions, the wound parallels the nerves, providing a measure of protection. However, the rectus incision approaches the anterior iliac spine, where both the ilioinguinal and iliohypogastric nerves lie. Both may be damaged during the incision and can become entrapped during closure. Additionally, the femoral nerve, the lateral femoral cutaneous nerve, and the genitofemoral nerve are easily compressed by the lateral blades of the retractors because of the extreme lateral positions of the incision’s poles. Injury to these nerves can result in paresthesia, pain, and paralysis of the leg muscles.
FIGURE 9 Maylard’s incision
After incising the aponeuroses of the abdominal muscles medial to the anterior iliac crest, dissect the rectus abdominus muscle transversely.
FIGURE 10 Maylard’s incision
Isolate, ligate, and divide the epigastric vessels. Then incise the transversalis fascia and peritoneum transversely to access the peritoneal cavity.
In summary
While the midline and Pfannenstiel’s incisions are an integral part of the gynecologic surgeon’s armamentarium, the paramedian and Maylard’s incisions should be added to the repertoire because these incisions can greatly enhance exposure. The paramedian shares the advantages of the midline incision but also allows better access to the ipsilateral pelvis. Furthermore, although Maylard’s incision takes longer to perform than other techniques, the excellent exposure—both laterally and superiorly—makes it worthwhile.
The authors report no financial relationship with any companies whose products are mentioned in this article.
- The incision should be considered as a second surgical procedure, which temporarily interferes with normal abdominal wall function.
- The midline incision provides excellent exposure to all areas of the abdomen and retroperitoneum, which can be accessed with minimal risk of significant vascular or nerve injury.
- Transverse incisions create less tension on the opposing skin edges because the incision follows Langer’s lines. The incidence of incisional hernias and wound dehiscence has been reported to be lower, but these studies are not randomized.
An abdominal incision often is given little thought other than as an access site through which a surgical procedure is performed. In reality, the incision is a second surgical procedure, which interferes—at least temporarily—with normal abdominal wall function.
While most physicians concur that the essential elements of a well-planned incision include adequate access to anticipated pathology, extensibility, and security of closure, many may not consider preservation of abdominal wall function as a key factor in their decision-making. Additional considerations include certainty of diagnosis, speed of entry, body habitus, presence of previous scars, potential for problems with hemostasis, and cosmetic outcome. These factors are the key determinants of whether the incision will be longitudinal (midline or paramedian) or transverse (Pfannenstiel’s, Cherney’s, or Maylard’s). For most gynecologic procedures confined to the pelvis, either option may be considered. The exceptions are patients with uncertain diagnoses or when access to the upper abdomen is indicated.
Regardless of the type of incision selected, the skin should be incised with a single, clean stroke of a sharp scalpel. However, when it comes to dissecting the underlying subcutaneous tissues, the debate continues over whether a scalpel or electrosurgery is best. While I recently have switched to the latter, here is a look at what the data say: Johnson and Serpell demonstrated that electrosurgery is associated with faster hemostasis, with no difference in the incidence of wound infection.1 Similarly, a recent randomized trial by Kearns et al found electro-surgery causes less blood loss and does not increase the risk of wound infections or fascial dehiscence.2 In contrast, a large prospective study by Cruse et al suggested that the use of diathermy is associated with twice the wound infection rate.3
This controversy also involves patients with gynecologic malignancies. Kolb et al found that electrosurgery was an independent risk factor for wound complications following surgery for ovarian cancer.4 However, Franchi and colleagues reported no difference in the rate of wound complications between scalpel and diathermy in patients who underwent mid-line abdominal incisions for the treatment of uterine cancer.5
Use the midline when the diagnosis and the extent of surgery are uncertain.
The inconsistencies in the data may reflect differences in electrosurgical technique. Non-modulated (cutting) current concentrates energy, vaporizing the tissue with little heat injury to surrounding areas. Conversely, modulated (coagulating) current coagulates the tissue with heat-producing char over a large area, and tissue injury often extends beyond the char. This effect is magnified if the electrode comes in direct contact with the tissue. Use the arc, rather than direct contact, to prevent excessive devitalization of tissue.
This article will review the techniques for, as well as the rationale and disadvantages of, common incisions—both longitudinal and transverse—to help the gynecologic surgeon minimize morbidity and maximize outcomes.
Longitudinal incisions
The longitudinal incisions that will be reviewed here are the midline (median) and paramedian. Classically, it was thought that longitudinal incisions were at greater risk of dehiscence than transverse incisions.6 However, it is difficult to make legitimate comparisons since longitudinal incisions are more likely to be performed in cases of hemorrhage, trauma, sepsis, multiorgan disease, previous surgery, previous radiation therapy, and malignancy—all of which increase the likelihood of postoperative complications. Furthermore, prospective and randomized studies have shown little, if any, difference in the incidence of dehiscence and hernias between longitudinal and transverse incisions.6-8
MidlineTechnique. Initiate the midline as a low abdominal incision (approximately 2 cm above the pubic symphysis), cutting along the linea alba. To extend the incision, if necessary, continue the dissection to the left of the umbilicus to avoid the ligamentum teres. Open the peritoneum at the cephalad pole of the incision (Figure 1). Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity (Figure 2).
Rationale. While this incision can be used for any surgical procedure, it is especially appropriate when the diagnosis is uncertain and the exact procedure or extent of surgery is unclear. It is an excellent choice when access to the upper abdomen may be necessary, e.g., patients with gynecologic malignancies who may need assessment of the diaphragm, liver biopsy, para-aortic node biopsy, omentectomy, or debulking procedures. Patients with benign gynecologic conditions also may benefit from a midline incision. For example, when pelvic anatomy is distorted, as with severe endometriosis or sepsis, recognizable anatomy may be found only above the pelvic brim.
A midline incision allows the quickest entry, which is especially important for an unstable or seriously ill patient. Exposure is excellent, as all areas of the abdomen and retroperitoneum can be accessed with minimal risk of significant vascular or nerve injury. This is because only terminal branches of the abdominal wall blood vessels and nerves are located at the linea alba. In addition, because deep tissue planes are not opened, this incision may be ideal for patients who are anticoagulated, have enlarged epigastric vessels that are more susceptible to injury, or have an intraabdominal infection.
Transverse incisions help reduce the rate of wound dehiscence.
Disadvantages. Two potential problems are the higher rate of hernia formation and wound dehiscence, which may be due to constant lateral tension, compared with transverse incisions. In addition, coughing, retching, and straining may exacerbate the lateral tension. Proper suture selection can reduce the incidence of complications. As previously mentioned, the reality of these disadvantages is subject to debate; further studies are needed to determine the true risk.
From a cosmetic standpoint, the midline scar often is prominent because the incision transects Langer’s lines. Hence, it cannot be concealed by lingerie or swimwear.
FIGURE 1 Midline incision
After incising the linea alba and separating the muscles in the midline, open the peritoneum at the cephalad pole of the incision.
FIGURE 2 Midline incision
Expand this cut slightly off midline to avoid the urachus yet adequately expose the peritoneal cavity.
ParamedianTechnique. Place this incision 2 to 5 cm to the left or right of the midline, depending on the indication for surgery. After dissecting the skin and subcutaneous layers, incise the anterior rectus sheath vertically over the rectus abdominis muscle (Figure 3) and dissect it from the medial muscle edge. Retract the muscle laterally to expose the posterior rectus sheath and then incise the sheath and the peritoneum vertically to expose the peritoneal cavity (Figure 4). Alternatively, a more lateral paramedian incision can be placed over the rectus abdominis muscle. In this case, however, the rectus muscle should be separated vertically, instead of retracted laterally, to expose the posterior rectus sheath.
Rationale. Paramedian incisions provide excellent exposure of the pelvis, excluding the upper abdomen. Therefore, consider this technique when the procedure will be confined to the ipsilateral pelvis, e.g., rightor left-side lymph node biopsies and exposure of the sigmoid colon on the left. Also, a paramedian incision at the level of the umbilicus can be used for a cesarean delivery or a hysterectomy.
This incision is the best choice when performing pelvic surgery on morbidly obese patients. By placing the incision low on the abdomen, the large panniculus can be retracted over the mons pubis and thighs, providing excellent exposure of the pelvis.
Disadvantages. Some researchers have reported that muscle-splitting lateral paramedian incisions have a lower incidence of incisional hernias compared with midline incisions.7,9 However, they take longer to perform and restrict access to the contralateral pelvis. In addition, the risk of vascular injury and hematomas is increased, especially in the lower pole where branches of the epigastric arteries penetrate the muscle.
With regard to nerve injury, terminal nerves are cut, resulting in paralysis of the inner portion of the rectus abdominis muscle. This paralysis can be permanent, as the muscle medial to the vertical separation is involved. However, if only the medial third of the muscle is denervated, the paralysis rarely limits function.
FIGURE 3 Paramedian incision
Place the incision 2 to 5 cm to the left or right of the midline. Incise the anterior rectus sheath vertically over the rectus abdominis muscle.
FIGURE 4 Paramedian incision
Retract the muscle laterally to expose the posterior sheath; then incise the sheath and the peritoneum vertically to expose the pelvic cavity.
Transverse incisions
Transverse incisions such as Pfannenstiel’s (muscle separating), Cherney’s (tendon detaching), and Maylard’s (muscle cutting) were developed to reduce the incidence of incisional hernias and wound dehiscence. Their success lies in the fact that they cause less tension on the opposing wound edges because the incisions follow Langer’s lines, unlike longitudinal incisions. Their placement also allows for a better cosmetic outcome. Because they can be placed in the pubic hairline or in a natural skin crease, they are easily concealed by lingerie or swimwear. However, the incision should not be placed in a deep skin fold of a large panniculus where maceration of the skin can increase the risk of infection.
The main disadvantages of transverse incisions are limited exposure of the upper abdomen and limited extensibility. Further, because more tissue planes are opened and more vessels are encountered, these incisions increase the risk of hematomas and infection.
Pfannenstiel’sTechnique. Incise the skin and subcutaneous tissues 2 to 5 cm above the pubic symphysis.10 Then dissect the rectus sheath transversely, separating it sharply from the rectus muscle at the linea alba and retracting it superiorly toward the umbilicus and inferiorly toward the pubic symphysis (Figure 5). Divide the rectus abdominis muscle along the midline raphe and retract it laterally, exposing the transversalis fascia and the posterior rectus sheath. Incise these layers and the peritoneum vertically to expose the peritoneal cavity (Figure 6).
To minimize retraction of the rectus abdominus muscle during Maylard’s, do not separate it from the anterior rectus sheath.
Rationale. Since exposure is limited and the incision can be only minimally extended, this incision is appropriate for procedures that are limited to the pelvis, e.g., abdominal hysterectomy, cesarean delivery, retropubic urethropexy, and paravaginal defect repairs. (Extension of the incision can be achieved by modifying it to Cherney’s incision.)
Disadvantages. The fact that the incision severs multiple tissue planes is an advantage as well as a disadvantage. Postoperative dehiscence and incisional hernias are rare because the closed wound has a high tensile strength. However, the incidence of inguinal hernias may increase when the incision is placed close to the external inguinal ring,11 and very low incisions may increase the risk of femoral nerve injury.12 The ilioinguinal and iliohypogastric nerves may be damaged, especially if the rectus incision is extended far laterally. Most commonly, they are trapped in the suture during closure, producing postoperative pain. Incising multiple layers also slows entry and increases the risk of seromas, hematomas, and wound infections.
This approach is contraindicated when time is of the essence, e.g., hemorrhage, or in the face of an abdominal infection, e.g., sepsis.
FIGURE 5 Pfannenstiel’s incision
After incising the skin and subcutaneous tissues, dissect the rectus sheath transversely, separating it sharply from the rectus muscle.
FIGURE 6 Pfannenstiel’s incision
Divide and retract the rectus abdominus muscle and then incise the tranversalis fascia and posterior rectus sheath vertically.
Cherney’sTechnique. Dissect the skin and subcutaneous tissue 2 to 3 cm above the pubic symphysis, which is lower than most Pfannenstiel’s incisions. Then incise the anterior rectus sheath transversely and dissect it from the rectus abdominis muscle superiorly and inferiorly. Using blunt dissection, separate the rectus and pyramidalis muscles from the underlying bladder and adventitial tissue. Then incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis (Figure 7). (This segment of tendon facilitates the reattachment of the muscles at closure.) Retract the muscles and tendons cephalad to expose the retropubic space. Incise the peritoneum transversely to expose the peritoneal cavity (Figure 8).
Rationale. Cherney’s incision provides excellent access to the retropubic space of Retzius, making it a good choice for retropubic urethropexy and paravaginal repair. Exposure is the main advantage to Cherney’s incision. The reason: It is a modification of Pfannenstiel’s incision and, as such, provides excellent lateral exposure because it is placed much lower on the abdominal wall.
Disadvantages. The benefits and risks of this incision are similar to those of Pfannenstiel’s incision since the same tissue planes are opened. However, it is more time consuming due to the dissection required to separate the muscles and tendons from the underlying tissues.
In addition, the deep inferior epigastric arteries could be injured as a result of the lateral dissection. Lastly, reattachment of the tendons is tedious.
FIGURE 7 Cherney’s incision
Incise transversely the tendons of the rectus and pyramidalis muscles 0.5 cm above the pubic symphysis.
FIGURE 8 Cherney’s incision
Retract the muscles and tendons cephalad and incise the peritoneum transversely to expose the peritoneal cavity.
Maylard’sTechnique. After transecting the skin and subcutaneous layers in a plane at the level of the anterior superior iliac spine, incise the rectus sheath transversely and extend the incision through the aponeuroses of the abdominal muscles to about 2 to 3 cm medial to the anterior iliac crest. Then dissect the rectus abdominis muscle transversely with a scalpel, electrocautery, or surgical stapler (Figure 9). To minimize retraction of this muscle, do not separate it from the anterior rectus sheath. (Alternatively, many surgeons recommend that the cut edge of the muscle be secured to the anterior sheath with mattress sutures to prevent retraction and reduce blood loss.)
Prior to transecting the peritoneum, isolate, ligate, and divide the deep inferior epigastric vessels. (Patients with significant aortoiliac atherosclerosis or aortic coarctation develop considerable collateral circulation through the epigastric vessels for perfusion of the lower extremities. Ligating these vessels may cause claudication and even lifethreatening ischemia. Therefore, assess iliac flow before ligating and transecting the arteries.) Then transect the transversalis fascia and peritoneum transversely, allowing access to the peritoneal cavity (Figure 10).
Rationale. Many oncologists use this approach for pelvic lymphadenectomy and staging procedures because the exposure to the lateral pelvis is excellent. The reason: This transverse incision cuts through all layers of the abdominal wall at the level of the anterior iliac spine. It also may be appropriate when pelvic pathology extends to the sidewall, e.g., endometriosis.
It is advisable to place a drain prior to closing Maylard’s.
Physicians should consider using this approach more than they currently are, especially when Pfannenstiel’s incision cannot provide satisfactory exposure or a longitudinal incision is thought to be the only alternative. The decision to use Maylard’s incision should be planned during the preoperative assessment, as Pfannenstiel’s incision should not be modified to Maylard’s intraoperatively.
Disadvantages. Although Maylard’s incision improves access to the upper abdomen compared to other transverse incisions, exposure is still limited. In addition, trauma to the deep epigastric arteries may result in considerable hemorrhage. And since hematomas commonly infiltrate the retroperitoneal space, large quantities of blood already may be lost before the hemorrhage is clinically apparent. Finally, oozing from the cut edge of the muscles may result in significant fluid collection, increasing the risk of infection. Therefore, it is advisable to place a drain prior to closure.
Like other transverse incisions, the wound parallels the nerves, providing a measure of protection. However, the rectus incision approaches the anterior iliac spine, where both the ilioinguinal and iliohypogastric nerves lie. Both may be damaged during the incision and can become entrapped during closure. Additionally, the femoral nerve, the lateral femoral cutaneous nerve, and the genitofemoral nerve are easily compressed by the lateral blades of the retractors because of the extreme lateral positions of the incision’s poles. Injury to these nerves can result in paresthesia, pain, and paralysis of the leg muscles.
FIGURE 9 Maylard’s incision
After incising the aponeuroses of the abdominal muscles medial to the anterior iliac crest, dissect the rectus abdominus muscle transversely.
FIGURE 10 Maylard’s incision
Isolate, ligate, and divide the epigastric vessels. Then incise the transversalis fascia and peritoneum transversely to access the peritoneal cavity.
In summary
While the midline and Pfannenstiel’s incisions are an integral part of the gynecologic surgeon’s armamentarium, the paramedian and Maylard’s incisions should be added to the repertoire because these incisions can greatly enhance exposure. The paramedian shares the advantages of the midline incision but also allows better access to the ipsilateral pelvis. Furthermore, although Maylard’s incision takes longer to perform than other techniques, the excellent exposure—both laterally and superiorly—makes it worthwhile.
The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Johnson CD, Serpell JW. Wound infection after abdominal incision with scalpel or diathermy. Br J Surg. 1990;77:626-627.
2. Cruse PJE, Ford R. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27.-
3. Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg. 2001;88(1):41-44.
4. Kolb BA, Buller RE, Connoer JP, et al. Effects of early postoperative chemotherapy on wound healing. Obstet Gynecol. 1992;79:988-992.
5. Franchi M, Ghezzi F, Bendetti-Panici PL, et al. A multicenter collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg. 2001;181(2):128-132.
6. Hendrix SL, Schimp V, Martin J. The legendary superior strength of the Pfannenstiel incision: a myth? Am J Obstet Gynecol. 2000;182(6):1446-1451.
7. Ellis H, Coleridge-Smith PD, Joyce AD. Abdominal incisions—vertical or transverse? Postgrad Med J. 1984;60:407-410.
8. Sanders RJ, DiClementi D. Principles of abdominal wound closure. II. Prevention of wound dehiscence. Arch Surg. 1977;112:1188.-
9. Donaldson DR, Hegarty JH, Brennan TG, et al. The lateral paramedian incision-experience with 850 cases. Br J Surg. 1982;69:630.-
10. Greenall MJ, et al. Midline or transverse laparotomy? A random controlled clinical trial. Part I: Influence on healing. Br J Surg. 1980;7:188.-
11. Pfannenstiel J. Ueber die Vortheile des suprasymphysaren Fascienquerschnitts für die gynakologischen Koliotomien zugleich ein Beitrag zu der Indikationsstellung der Operationswege. Samml Klin Vortr (Leipzig). 1900;268:1735.-
12. Griffiths DA. A reappraisal of the Pfannenstiel incision. Br J Urol. 1976;48:469.-
1. Johnson CD, Serpell JW. Wound infection after abdominal incision with scalpel or diathermy. Br J Surg. 1990;77:626-627.
2. Cruse PJE, Ford R. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27.-
3. Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg. 2001;88(1):41-44.
4. Kolb BA, Buller RE, Connoer JP, et al. Effects of early postoperative chemotherapy on wound healing. Obstet Gynecol. 1992;79:988-992.
5. Franchi M, Ghezzi F, Bendetti-Panici PL, et al. A multicenter collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg. 2001;181(2):128-132.
6. Hendrix SL, Schimp V, Martin J. The legendary superior strength of the Pfannenstiel incision: a myth? Am J Obstet Gynecol. 2000;182(6):1446-1451.
7. Ellis H, Coleridge-Smith PD, Joyce AD. Abdominal incisions—vertical or transverse? Postgrad Med J. 1984;60:407-410.
8. Sanders RJ, DiClementi D. Principles of abdominal wound closure. II. Prevention of wound dehiscence. Arch Surg. 1977;112:1188.-
9. Donaldson DR, Hegarty JH, Brennan TG, et al. The lateral paramedian incision-experience with 850 cases. Br J Surg. 1982;69:630.-
10. Greenall MJ, et al. Midline or transverse laparotomy? A random controlled clinical trial. Part I: Influence on healing. Br J Surg. 1980;7:188.-
11. Pfannenstiel J. Ueber die Vortheile des suprasymphysaren Fascienquerschnitts für die gynakologischen Koliotomien zugleich ein Beitrag zu der Indikationsstellung der Operationswege. Samml Klin Vortr (Leipzig). 1900;268:1735.-
12. Griffiths DA. A reappraisal of the Pfannenstiel incision. Br J Urol. 1976;48:469.-