User login
Self‐reported penicillin allergy is common and frequently limits the available antimicrobial agents to choose from. This often results in the use of more expensive, potentially more toxic, and possibly less efficacious agents.[1, 2]
For over 30 years, penicilloyl‐polylysine (PPL) penicillin skin testing (PST) was widely used to diagnose penicillin allergy with a negative predictive value (NPV) of about 97% to 99%.[3] After being off the market for 5 years, PPL PST was reapproved in 2009 as PRE‐PEN.[4] However, many clinicians still fail to utilize PST despite its simplicity and substantial clinical impact. The main purpose of this study was to describe the predictive value of PST and impact on antibiotic selection in a sample of hospitalized patients with a reported history of penicillin allergy.
METHODS
In 2010, PST was introduced as a quality‐improvement measure after approval and support from the chief of professional services and the medical staff executive committee at Vidant Medical Center, an 861‐bed tertiary care and teaching hospital. Our antimicrobial stewardship program is regularly contacted for approval of alternative therapies in penicillin allergic patients. The PST quality‐improvement intervention was implemented to avoid resorting to less appropriate therapies in these situations. Following approval by the University and Medical Center Institutional Review Board, we designed a 4‐month study to assess the impact of this ongoing quality improvement measure from March 2012 to July 2012.
Hospitalized patients of all ages with reported penicillin allergies were obtained from our antimicrobial stewardship database. Their charts were reviewed for demographics, antibiotic use, clinical infection, and allergic description. Deciding whether to alter antibiotic therapy to a ‐lactam regimen was based on microbiologic results, laboratory values, clinical infection, and history of immunoglobulin E (IgE)‐mediated reactions, as defined by the updated drug allergy practice parameters.[5] IgE‐mediated reactions included: (1) immediate urticaria, laryngeal edema, or hypotension; (2) anemia; and (3) fever, arthralgias, lymphadenopathy, and an urticarial rash after 7 to 21 days.[5, 6, 7] We defined anaphylaxis as the development of angioedema or hemodynamic instability within 1 hour of penicillin administration. A true negative reaction was a lack of an IgE‐mediated reaction to all the drug challenges.
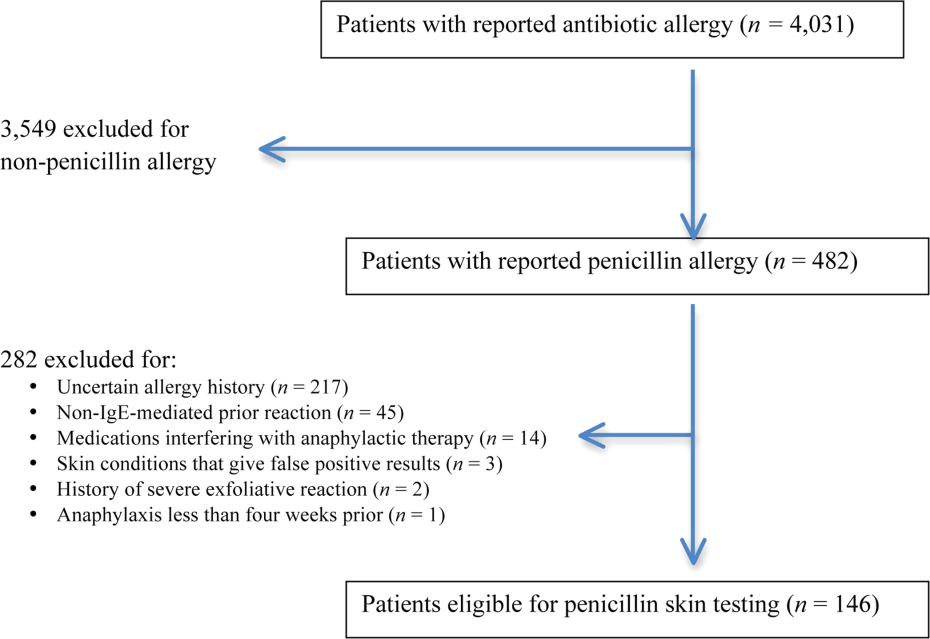
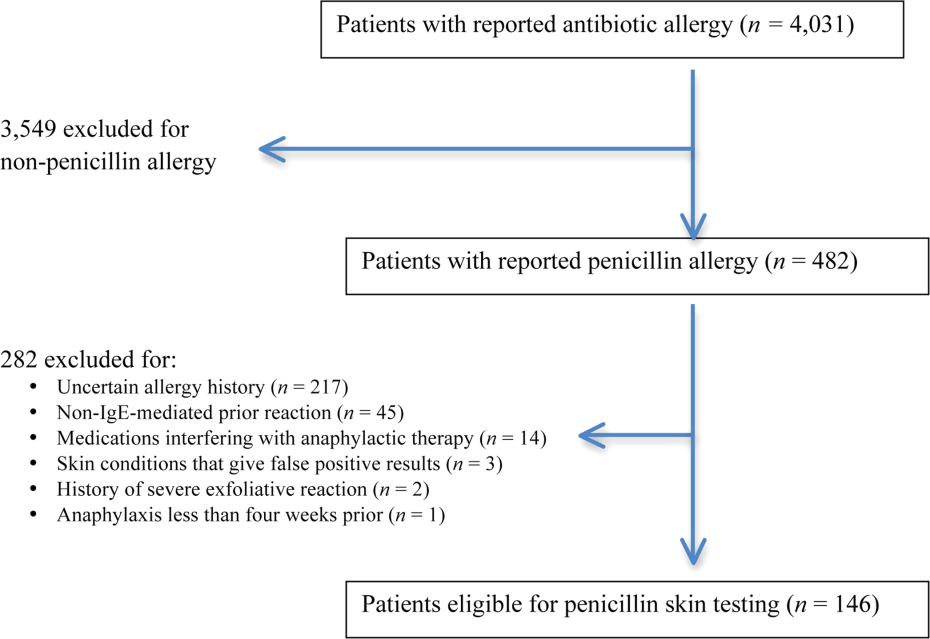
Patients in the medical, surgical, labor, and delivery wards; intensive care units; and emergency department underwent testing. The ‐lactam agent used after a negative PST was recorded, and the patients were followed for 24 hours after transitioning their therapy to a ‐lactam regimen. Excluded subjects included those with (1) nonIgE‐mediated reactions, (2) skin conditions that can give false positive results, (3) medications that may interfere with anaphylactic therapy, (4) history of severe exfoliative reactions to ‐lactams, (5) anaphylaxis less than 4 weeks prior, (6) allergies to antibiotics other than penicillin, and (7) uncertain allergy history.
PST Reagents/Procedure
Our benzylpenicilloyl major determinant molecule, commercially produced as PPL, was purchased as a PRE‐PEN from ALK‐Abello, Round Rock, Texas. Penicillin G potassium, purchased from Pfizer, New York, New York, is the only commercially available minor determinant and can improve identification of penicillin allergy by up to 97%.[2] The PST panel also included histamine (positive control) and normal saline (negative control).
Skin Testing Procedure
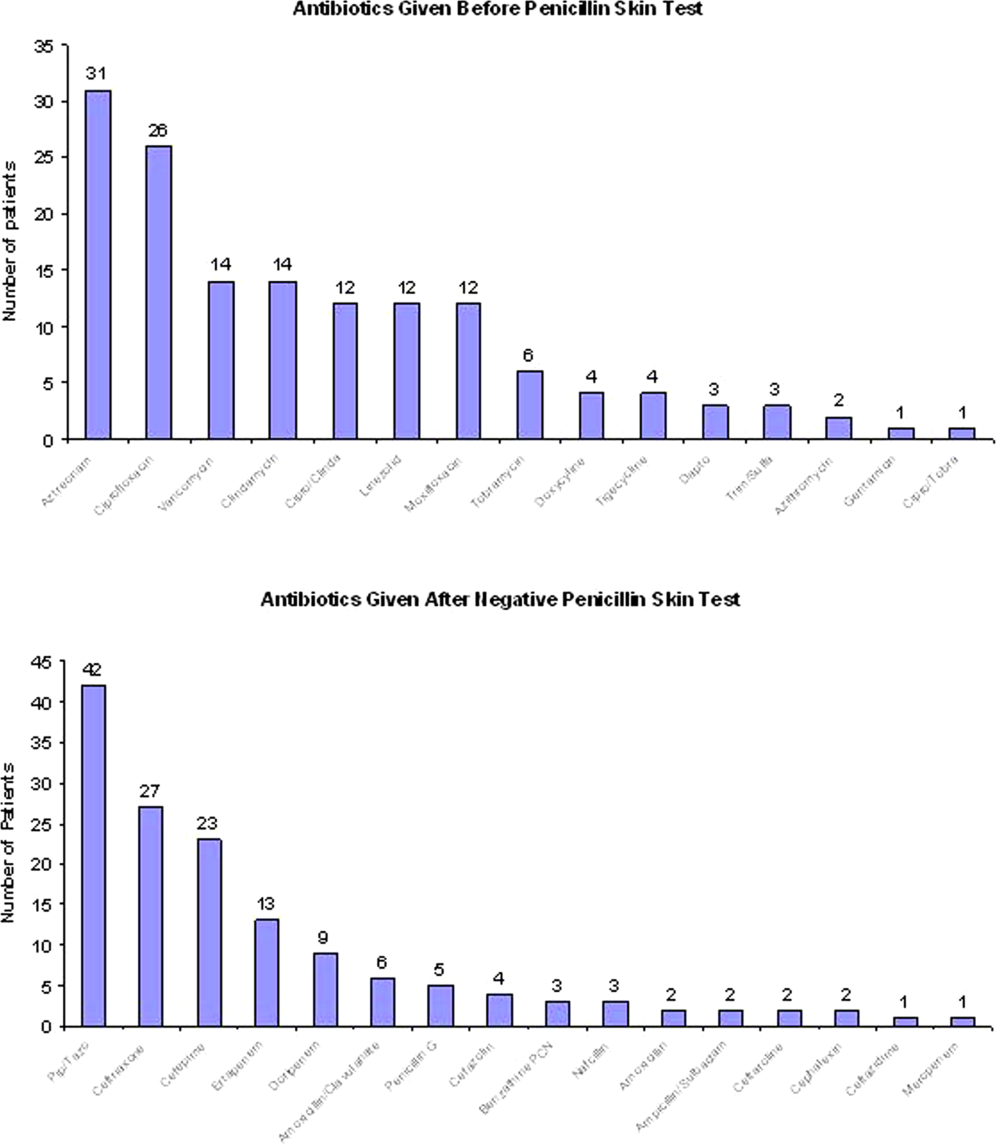
An infectious diseases fellow (R.H.R. or B.K.) was supervised in preparing for potential anaphylaxis, applying the reagents and interpreting the results based on drug allergy practice parameters.[5] The preliminary epicutaneous prick/puncture test was performed with a lancet in subjects without prior anaphylaxis using full‐strength PPL and penicillin G potassium reagents. If there was no response within 15 minutes, which we defined as a lack of wheal formation 3 mm or greater than that of the negative control, 0.02 to 0.03 mL of each reagent was injected intradermally using a tuberculin syringe and examined for 15 minutes.[5] If there was no response, patients were then challenged with either a single oral dose of penicillin V potassium 250 mg or whichever oral penicillin agent they previously reported an allergy to. If no reaction was appreciated within 2 hours, their therapy was changed to a ‐lactam agent including penicillins, cephalosporins, and carbapenems for the remaining duration of therapy (Figure 1) An estimate of NPV was obtained after 24 hours follow‐up.
Statistical Analysis
We designed a study to estimate whether the reapproved PST achieves an NPV of at least 95%.[3] We hypothesized that clinicians will be willing to utilize PST even if it has an NPV of slightly less than 98% compared to the current standard of treating patients without PST.[7] Assuming an equivalence margin of 3%, we estimated a sample size of 146 to achieve at least 82% power to test a hypothesis of NPV 95% using a 1‐sided Z test with a type‐I error rate of 5%.[8] Once the sample size of 146 subjects was reached, we stopped recruiting patients.
Sample characteristics of the subjects who underwent testing were summarized using descriptive statistics. Sample proportions were calculated to summarize categorical variables. Mean and standard deviation were calculated to summarize continuous variables. Cost analysis of antibiotic therapy was estimated from the Vidant Medical Center antibiotic pharmaceutical acquisition costs. Estimated cost of peripherally inserted central catheter (PICC) placement and removal as well as laboratory testing costs were obtained from our institution's medical billing department. Marketing costs of pharmacist drug calibration and nursing assessments with dressing changes were obtained from hospital‐affiliated outpatient antibiotic infusion companies.
RESULTS
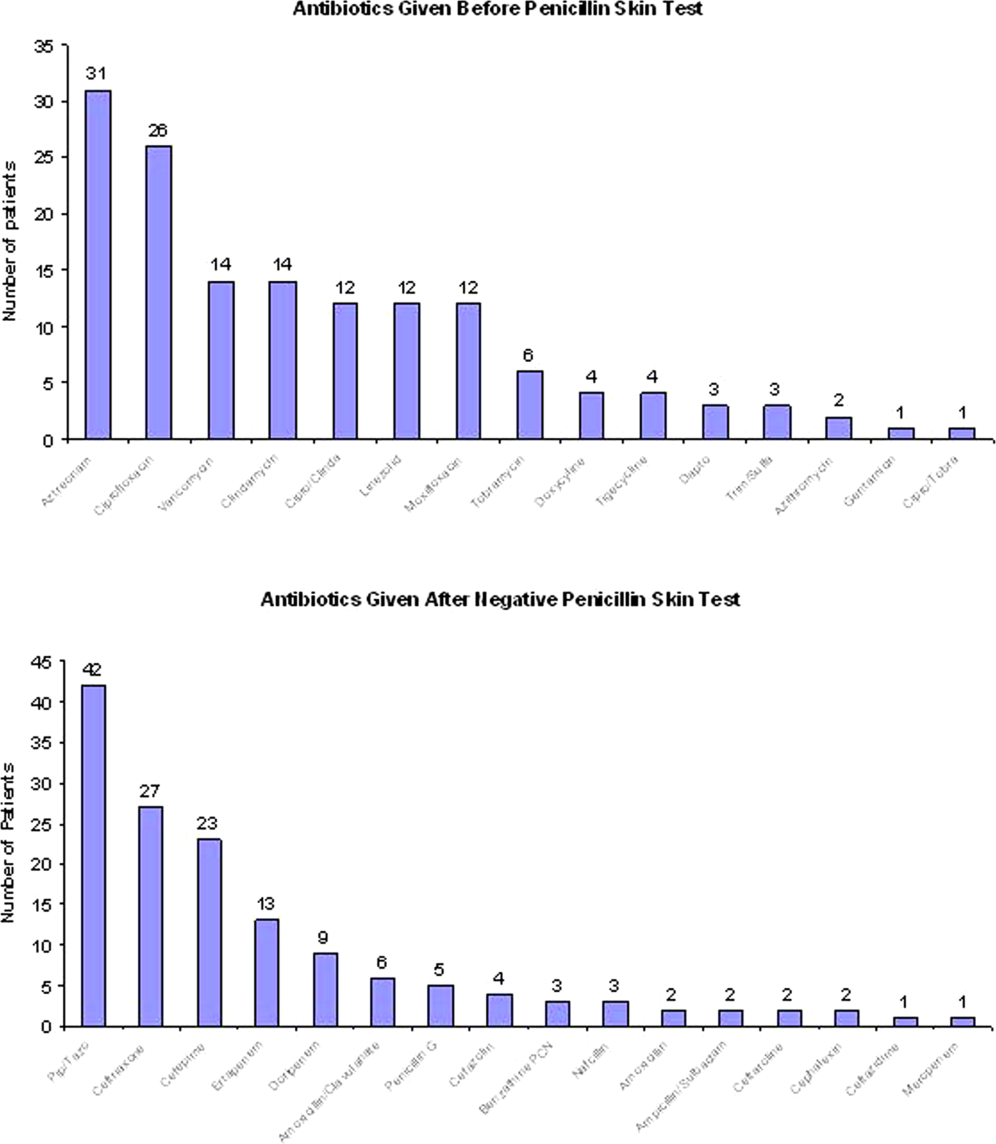
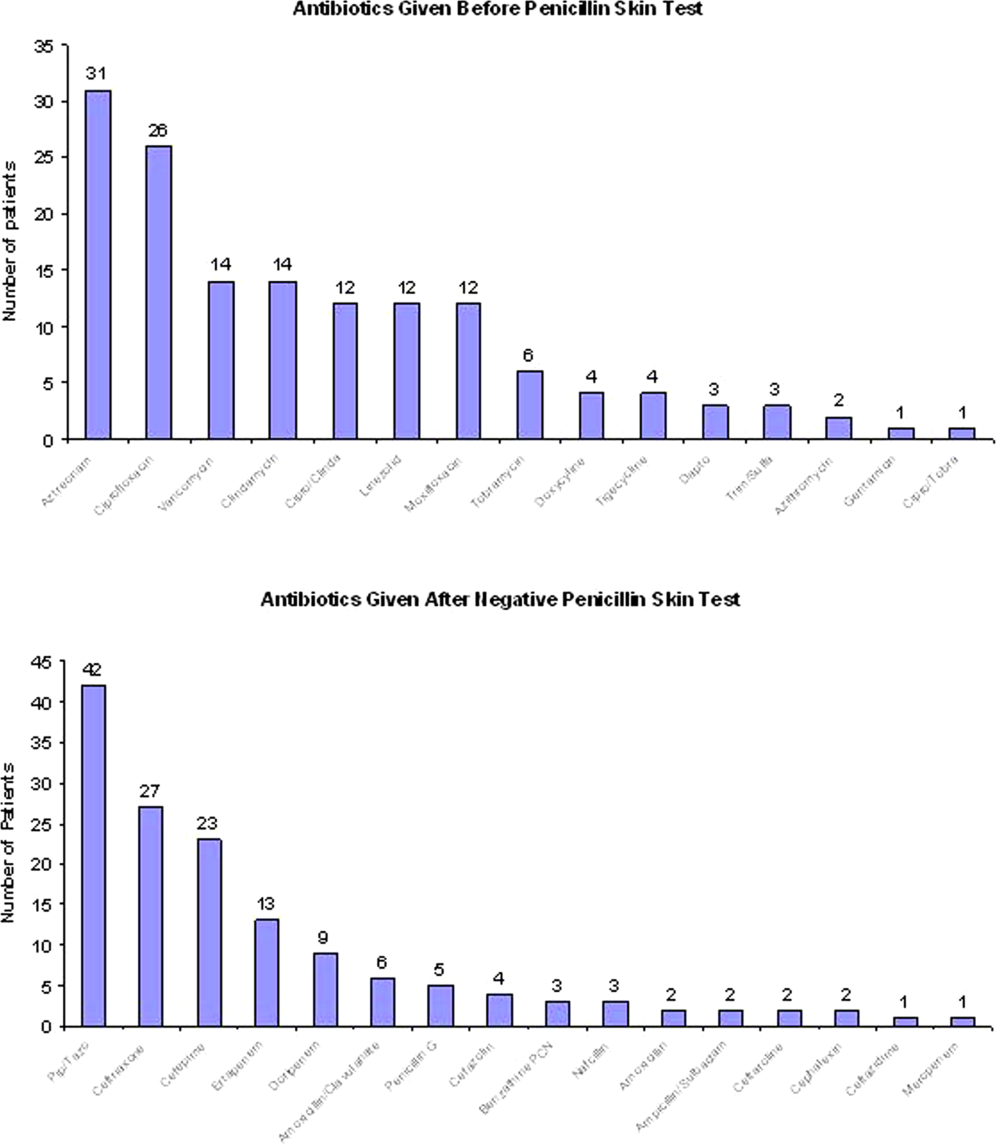
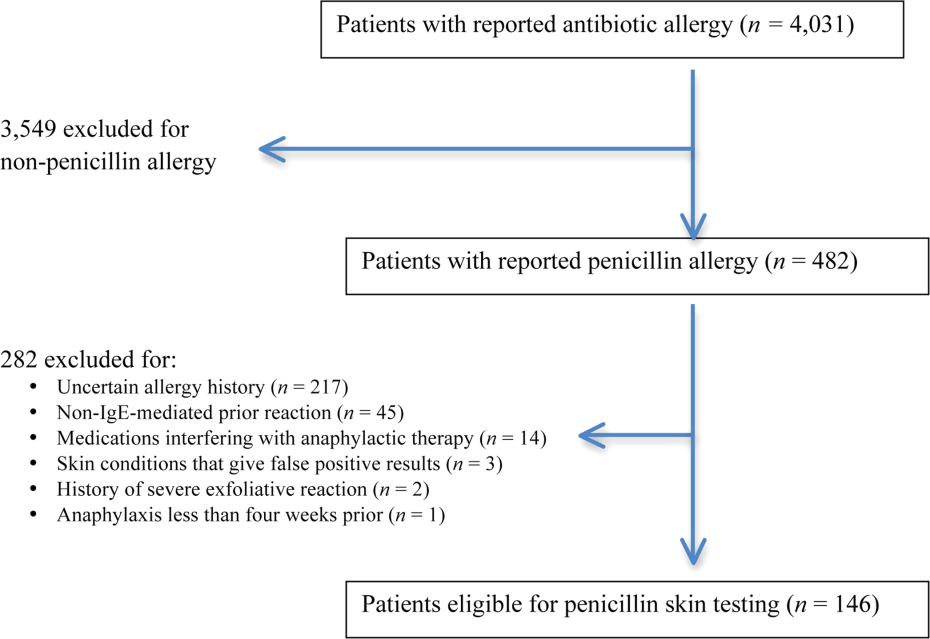
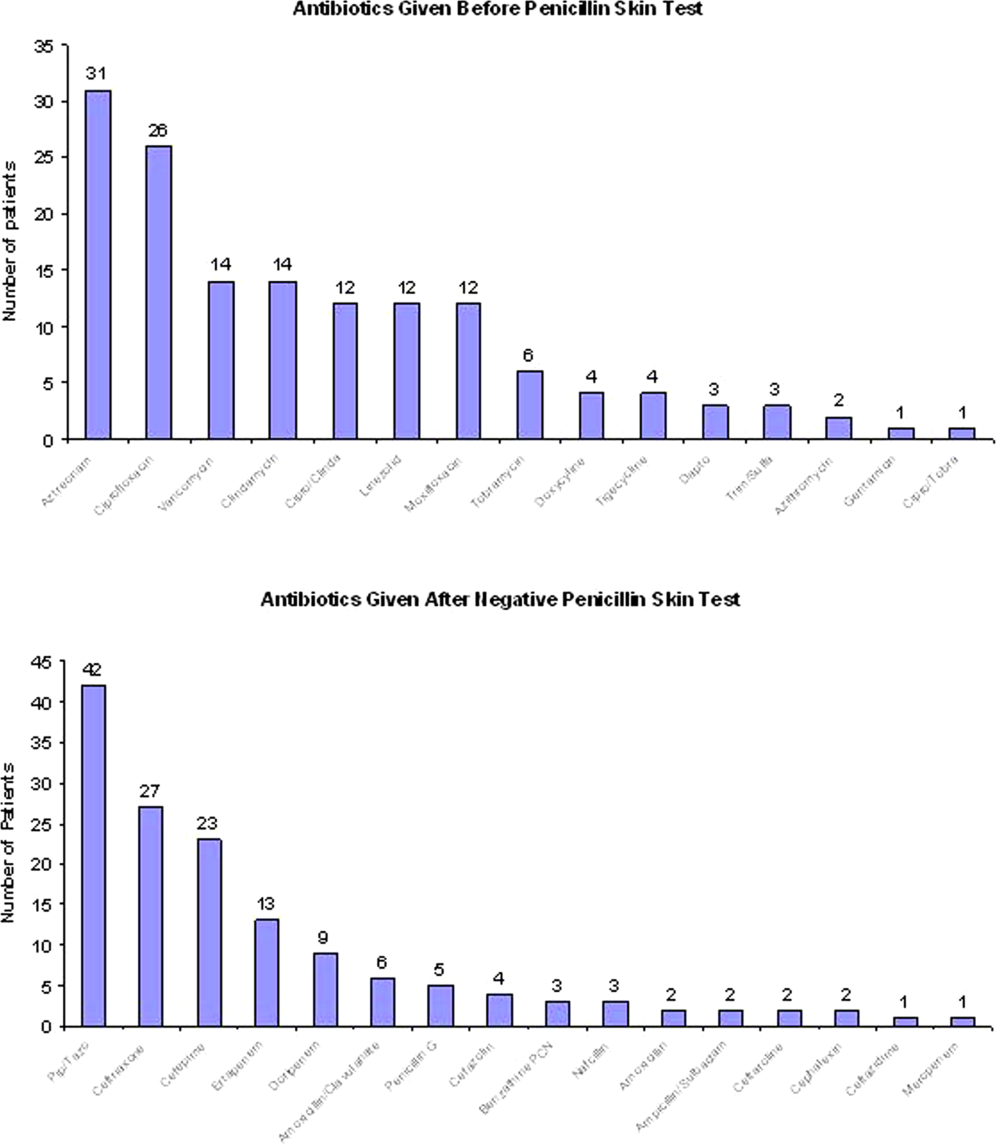
A total of 4031 allergy histories were reviewed during the 5‐month study period to achieve the sample size of 146 patients (Table 1). Of those, 3885 were excluded (Figure 2). Common infections included pneumonias (26%) and urinary tract infections (20%) (Table 2) Only 1 subject had a positive reaction with hives, edema, and itching approximately 6 minutes after the agents were injected intradermally. The remaining 145 (99%) had negative reactions to the PST and oral challenge and were then successfully transitioned to a ‐lactam agent without any reaction at 24 hours, giving an NPV of 100%. Ten subjects were switched from intravenous to oral ‐lactam agents (Figure 1). Avoidance of PICC placement ($1,200) and removal ($65), dressing changes, weekly drug‐level testing, laboratory technician, and pharmaceutical drug calibration costs allowed for a healthcare reduction of $5,233 ($520/patient) based on the 146 patients studied. The total cost of therapy would have been $113,991 if the PST had not been performed. However, the cost of altered therapy following a negative PST was $81,180, a difference of $32,811 ($225/per patient) in a 5‐month period. The total estimated annual difference, including antibiotic alteration and associated drug‐costs, would be $82,000.
| Antibiotic | No. of Patients Reporting An Allergy | % Per Total Charts Reviewed |
|---|---|---|
| Penicillin | 428 | 10.6 |
| Sulfonamide | 271 | 6.7 |
| Quinolone | 108 | 2.7 |
| Cephalosporin | 81 | 2.0 |
| Macrolide | 65 | 1.6 |
| Vancomycin | 39 | 0.9 |
| Tetracycline | 20 | 0.5 |
| Clindamycin | 18 | 0.4 |
| Metronidazole | 9 | 0.2 |
| Linezolid | 2 | 0.05 |
| Categories | No. of Patients (%) |
|---|---|
| |
| Time since last reported penicillin use | |
| 1 month1 year | 6 (4) |
| 25 years | 39 (27) |
| 610 years | 23 (16) |
| >10 years | 78 (53) |
| Reported IgE‐mediated reactions | |
| Bronchospasm | 23 (16) |
| Urticarial rash | 100 (68) |
| Edema | 32 (22) |
| Anaphylaxis | 21 (14) |
| Age on admission, y | |
| 2050 | 28 (19) |
| 5160 | 29 (20) |
| 6170 | 41 (28) |
| 7180 | 24 (16) |
| >80 | 24 (16) |
| Gender | |
| Male | 55 (40) |
| Female | 88 (60) |
| Race | |
| White | 82 (56) |
| Black | 61 (42) |
| Hispanic | 3 (2) |
| Infections being treated | |
| Bacteremia | 7 (4.8) |
| Catheter‐related bloodstream infection | 2 (1.4) |
| Empyema | 1 (0.7) |
| Epidural abscess | 2 (1.4) |
| Infective endocarditis | 4 (2.7) |
| Intra‐abdominal infection | 24 (16.4) |
| Meningitis | 1 (0.7) |
| Neutropenic fever | 1 (0.7) |
| Osteomyelitis | 6 (4.1) |
| Pericardial effusion | 1 (0.7) |
| Prosthetic joint infection | 5 (3.4) |
| Pneumonia | 40 (27.4) |
| Skin and soft‐tissue infection | 20 (13.7) |
| Syphilis | 3 (2.1) |
| Urinary tract infection | 29 (19.7) |
DISCUSSION
PST is the most rapid, sensitive, and cost‐effective modality for evaluating patients with immediate allergic reactions to penicillin. Over 90% of individuals with a true history of penicillin allergy have confirmed sensitivity with a PST, implying most patients who are skin tested negative are truly not allergic.[7, 9, 10, 11, 12] Our study shows that the reapproved PST with the PPL and penicillin G determinants continues to have a high NPV. A patient with a negative PST result is generally at a low risk of developing an immediate‐type hypersensitivity reaction to penicillin.[2, 11] PST frequently allowed for less expensive agents that would have been avoided due to a reported allergy. The estimated annual savings of $82,000 dollars from antibiotic alteration with successful transition to a ‐lactam agent after a negative PST illustrates its value, supports its validity, and makes this study novel.
Many ‐lactamase inhibitors (ie, piperacillin‐tazobactam), fourth generation cephalosporins (ie, cefepime), and carbapenems still remain costly. Despite this, we were still able to achieve a significant reduction in overall cost. In addition to financial benefits, PST allowed for the use of more appropriate agents with less potential adverse effects. Narrow‐spectrum, non‐lactam agents were sometimes altered to a broader‐spectrum ‐lactam agent. We also frequently tailored 2 agents to just 1 broad‐spectrum ‐lactam. This led to more patients being given broad‐spectrum agents after the PST (72 vs 89 patients). However, we were able to avoid using second‐line agents, such as aztreonam, vancomycin, linezolid, daptomycin, and tobramycin, in many patients with infections that are often best treated with penicillin‐based antibiotics (ie, syphilis, group B Streptococcus infections). With increasing incidence and recovery of multidrug‐resistant bacteria, PST may also allow use of potentially more effective antimicrobial agents.
A possible limitation is that our prevalence of a true penicillin allergy was 1%, whereas Bousquet et al. illustrate a higher prevalence of about 20%.[7] Although our prevalence may not be generalizable, Bousquet's study only assessed patients with allergies 5 years prior.
The introduction of PST into clinical practice will allow trained healthcare providers to prescribe cheaper, more appropriate, less toxic antimicrobial agents. The overall benefit of reintroducing penicillin agents when needed in the future is far more cost‐effective than what is described here. PST should become a standard of care when prescribing antibiotics to patients with a history of penicillin allergy. Medical providers should be aware of its utility, acquire training, and incorporate it into their practice.
Acknowledgment
Disclosures: Paul P. Cook, MD, has potential conflicts of interest with Gilead (investigator), Pfizer (investigator), Merck (investigator and speakers' bureau), and Forest (speakers' bureau). Neither he nor any of the other authors has received any sources of funding for this article. For the remaining authors, no conflicts were declared. The corresponding author, Ramzy Rimawi, MD, had full access to all of the data in the study and had final responsibility for the decision to submit for publication.
- , , . Elective penicillin skin testing in a pediatric outpatient setting. Ann Allergy Asthma Immunol. 2006;97(6):807–812.
- US Department of Veterans Affairs Web site. Benzypenicilloyl polylisine (PRE‐PEN) national drug monograph. May 2012. Available at: http://www.pbm.va.gov/DrugMonograph.aspx. Accessed September 1, 2012.
- , . Diagnosis and management of penicillin allergy. Mayo Clin Proc. 2005;80(3):405–410.
- PRE‐PEN penicillin skin test antigen. Available at: http://www.alk‐abello.com/us/products/pre‐pen/Pages/PREPEN.aspx. Accessed September 1, 2012.
- , , , et al.; Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010;105:259–273.
- . Immunochemical mechanisms in penicillin allergy. Fed Proc. 1965;24:51–54.
- , , , et al. Oral challenges are needed in the diagnosis of beta‐lactam hypersensitivity. Clin Exp Allergy. 2008;38(1):185–190.
- , , . Sample Size Calculations in Clinical Research. New York, NY: Chapman 2003.
- , , , et al. Retrospective case series analysis of penicillin allergy testing in a UK specialist regional allergy clinic. J Clin Pathol. 2011;64:1014–1018.
- . Prevalence of skin test reactivity in patients with convincing, vague and unnacceptible histories of penicillin allergy. Allergy Asthma Proc. 2005;26(1):59–64.
- , . Frequency of systemic reactions to penicillin skin tests. Ann Allergy Asthma Immunol. 2000;85:363–365.
- , , , et al. The incidence of antimicrobial allergies in hospitalized patients. Arch Intern Med. 2000;160;2819–2822.
Self‐reported penicillin allergy is common and frequently limits the available antimicrobial agents to choose from. This often results in the use of more expensive, potentially more toxic, and possibly less efficacious agents.[1, 2]
For over 30 years, penicilloyl‐polylysine (PPL) penicillin skin testing (PST) was widely used to diagnose penicillin allergy with a negative predictive value (NPV) of about 97% to 99%.[3] After being off the market for 5 years, PPL PST was reapproved in 2009 as PRE‐PEN.[4] However, many clinicians still fail to utilize PST despite its simplicity and substantial clinical impact. The main purpose of this study was to describe the predictive value of PST and impact on antibiotic selection in a sample of hospitalized patients with a reported history of penicillin allergy.
METHODS
In 2010, PST was introduced as a quality‐improvement measure after approval and support from the chief of professional services and the medical staff executive committee at Vidant Medical Center, an 861‐bed tertiary care and teaching hospital. Our antimicrobial stewardship program is regularly contacted for approval of alternative therapies in penicillin allergic patients. The PST quality‐improvement intervention was implemented to avoid resorting to less appropriate therapies in these situations. Following approval by the University and Medical Center Institutional Review Board, we designed a 4‐month study to assess the impact of this ongoing quality improvement measure from March 2012 to July 2012.
Hospitalized patients of all ages with reported penicillin allergies were obtained from our antimicrobial stewardship database. Their charts were reviewed for demographics, antibiotic use, clinical infection, and allergic description. Deciding whether to alter antibiotic therapy to a ‐lactam regimen was based on microbiologic results, laboratory values, clinical infection, and history of immunoglobulin E (IgE)‐mediated reactions, as defined by the updated drug allergy practice parameters.[5] IgE‐mediated reactions included: (1) immediate urticaria, laryngeal edema, or hypotension; (2) anemia; and (3) fever, arthralgias, lymphadenopathy, and an urticarial rash after 7 to 21 days.[5, 6, 7] We defined anaphylaxis as the development of angioedema or hemodynamic instability within 1 hour of penicillin administration. A true negative reaction was a lack of an IgE‐mediated reaction to all the drug challenges.
Patients in the medical, surgical, labor, and delivery wards; intensive care units; and emergency department underwent testing. The ‐lactam agent used after a negative PST was recorded, and the patients were followed for 24 hours after transitioning their therapy to a ‐lactam regimen. Excluded subjects included those with (1) nonIgE‐mediated reactions, (2) skin conditions that can give false positive results, (3) medications that may interfere with anaphylactic therapy, (4) history of severe exfoliative reactions to ‐lactams, (5) anaphylaxis less than 4 weeks prior, (6) allergies to antibiotics other than penicillin, and (7) uncertain allergy history.
PST Reagents/Procedure
Our benzylpenicilloyl major determinant molecule, commercially produced as PPL, was purchased as a PRE‐PEN from ALK‐Abello, Round Rock, Texas. Penicillin G potassium, purchased from Pfizer, New York, New York, is the only commercially available minor determinant and can improve identification of penicillin allergy by up to 97%.[2] The PST panel also included histamine (positive control) and normal saline (negative control).
Skin Testing Procedure
An infectious diseases fellow (R.H.R. or B.K.) was supervised in preparing for potential anaphylaxis, applying the reagents and interpreting the results based on drug allergy practice parameters.[5] The preliminary epicutaneous prick/puncture test was performed with a lancet in subjects without prior anaphylaxis using full‐strength PPL and penicillin G potassium reagents. If there was no response within 15 minutes, which we defined as a lack of wheal formation 3 mm or greater than that of the negative control, 0.02 to 0.03 mL of each reagent was injected intradermally using a tuberculin syringe and examined for 15 minutes.[5] If there was no response, patients were then challenged with either a single oral dose of penicillin V potassium 250 mg or whichever oral penicillin agent they previously reported an allergy to. If no reaction was appreciated within 2 hours, their therapy was changed to a ‐lactam agent including penicillins, cephalosporins, and carbapenems for the remaining duration of therapy (Figure 1) An estimate of NPV was obtained after 24 hours follow‐up.
Statistical Analysis
We designed a study to estimate whether the reapproved PST achieves an NPV of at least 95%.[3] We hypothesized that clinicians will be willing to utilize PST even if it has an NPV of slightly less than 98% compared to the current standard of treating patients without PST.[7] Assuming an equivalence margin of 3%, we estimated a sample size of 146 to achieve at least 82% power to test a hypothesis of NPV 95% using a 1‐sided Z test with a type‐I error rate of 5%.[8] Once the sample size of 146 subjects was reached, we stopped recruiting patients.
Sample characteristics of the subjects who underwent testing were summarized using descriptive statistics. Sample proportions were calculated to summarize categorical variables. Mean and standard deviation were calculated to summarize continuous variables. Cost analysis of antibiotic therapy was estimated from the Vidant Medical Center antibiotic pharmaceutical acquisition costs. Estimated cost of peripherally inserted central catheter (PICC) placement and removal as well as laboratory testing costs were obtained from our institution's medical billing department. Marketing costs of pharmacist drug calibration and nursing assessments with dressing changes were obtained from hospital‐affiliated outpatient antibiotic infusion companies.
RESULTS
A total of 4031 allergy histories were reviewed during the 5‐month study period to achieve the sample size of 146 patients (Table 1). Of those, 3885 were excluded (Figure 2). Common infections included pneumonias (26%) and urinary tract infections (20%) (Table 2) Only 1 subject had a positive reaction with hives, edema, and itching approximately 6 minutes after the agents were injected intradermally. The remaining 145 (99%) had negative reactions to the PST and oral challenge and were then successfully transitioned to a ‐lactam agent without any reaction at 24 hours, giving an NPV of 100%. Ten subjects were switched from intravenous to oral ‐lactam agents (Figure 1). Avoidance of PICC placement ($1,200) and removal ($65), dressing changes, weekly drug‐level testing, laboratory technician, and pharmaceutical drug calibration costs allowed for a healthcare reduction of $5,233 ($520/patient) based on the 146 patients studied. The total cost of therapy would have been $113,991 if the PST had not been performed. However, the cost of altered therapy following a negative PST was $81,180, a difference of $32,811 ($225/per patient) in a 5‐month period. The total estimated annual difference, including antibiotic alteration and associated drug‐costs, would be $82,000.
| Antibiotic | No. of Patients Reporting An Allergy | % Per Total Charts Reviewed |
|---|---|---|
| Penicillin | 428 | 10.6 |
| Sulfonamide | 271 | 6.7 |
| Quinolone | 108 | 2.7 |
| Cephalosporin | 81 | 2.0 |
| Macrolide | 65 | 1.6 |
| Vancomycin | 39 | 0.9 |
| Tetracycline | 20 | 0.5 |
| Clindamycin | 18 | 0.4 |
| Metronidazole | 9 | 0.2 |
| Linezolid | 2 | 0.05 |
| Categories | No. of Patients (%) |
|---|---|
| |
| Time since last reported penicillin use | |
| 1 month1 year | 6 (4) |
| 25 years | 39 (27) |
| 610 years | 23 (16) |
| >10 years | 78 (53) |
| Reported IgE‐mediated reactions | |
| Bronchospasm | 23 (16) |
| Urticarial rash | 100 (68) |
| Edema | 32 (22) |
| Anaphylaxis | 21 (14) |
| Age on admission, y | |
| 2050 | 28 (19) |
| 5160 | 29 (20) |
| 6170 | 41 (28) |
| 7180 | 24 (16) |
| >80 | 24 (16) |
| Gender | |
| Male | 55 (40) |
| Female | 88 (60) |
| Race | |
| White | 82 (56) |
| Black | 61 (42) |
| Hispanic | 3 (2) |
| Infections being treated | |
| Bacteremia | 7 (4.8) |
| Catheter‐related bloodstream infection | 2 (1.4) |
| Empyema | 1 (0.7) |
| Epidural abscess | 2 (1.4) |
| Infective endocarditis | 4 (2.7) |
| Intra‐abdominal infection | 24 (16.4) |
| Meningitis | 1 (0.7) |
| Neutropenic fever | 1 (0.7) |
| Osteomyelitis | 6 (4.1) |
| Pericardial effusion | 1 (0.7) |
| Prosthetic joint infection | 5 (3.4) |
| Pneumonia | 40 (27.4) |
| Skin and soft‐tissue infection | 20 (13.7) |
| Syphilis | 3 (2.1) |
| Urinary tract infection | 29 (19.7) |
DISCUSSION
PST is the most rapid, sensitive, and cost‐effective modality for evaluating patients with immediate allergic reactions to penicillin. Over 90% of individuals with a true history of penicillin allergy have confirmed sensitivity with a PST, implying most patients who are skin tested negative are truly not allergic.[7, 9, 10, 11, 12] Our study shows that the reapproved PST with the PPL and penicillin G determinants continues to have a high NPV. A patient with a negative PST result is generally at a low risk of developing an immediate‐type hypersensitivity reaction to penicillin.[2, 11] PST frequently allowed for less expensive agents that would have been avoided due to a reported allergy. The estimated annual savings of $82,000 dollars from antibiotic alteration with successful transition to a ‐lactam agent after a negative PST illustrates its value, supports its validity, and makes this study novel.
Many ‐lactamase inhibitors (ie, piperacillin‐tazobactam), fourth generation cephalosporins (ie, cefepime), and carbapenems still remain costly. Despite this, we were still able to achieve a significant reduction in overall cost. In addition to financial benefits, PST allowed for the use of more appropriate agents with less potential adverse effects. Narrow‐spectrum, non‐lactam agents were sometimes altered to a broader‐spectrum ‐lactam agent. We also frequently tailored 2 agents to just 1 broad‐spectrum ‐lactam. This led to more patients being given broad‐spectrum agents after the PST (72 vs 89 patients). However, we were able to avoid using second‐line agents, such as aztreonam, vancomycin, linezolid, daptomycin, and tobramycin, in many patients with infections that are often best treated with penicillin‐based antibiotics (ie, syphilis, group B Streptococcus infections). With increasing incidence and recovery of multidrug‐resistant bacteria, PST may also allow use of potentially more effective antimicrobial agents.
A possible limitation is that our prevalence of a true penicillin allergy was 1%, whereas Bousquet et al. illustrate a higher prevalence of about 20%.[7] Although our prevalence may not be generalizable, Bousquet's study only assessed patients with allergies 5 years prior.
The introduction of PST into clinical practice will allow trained healthcare providers to prescribe cheaper, more appropriate, less toxic antimicrobial agents. The overall benefit of reintroducing penicillin agents when needed in the future is far more cost‐effective than what is described here. PST should become a standard of care when prescribing antibiotics to patients with a history of penicillin allergy. Medical providers should be aware of its utility, acquire training, and incorporate it into their practice.
Acknowledgment
Disclosures: Paul P. Cook, MD, has potential conflicts of interest with Gilead (investigator), Pfizer (investigator), Merck (investigator and speakers' bureau), and Forest (speakers' bureau). Neither he nor any of the other authors has received any sources of funding for this article. For the remaining authors, no conflicts were declared. The corresponding author, Ramzy Rimawi, MD, had full access to all of the data in the study and had final responsibility for the decision to submit for publication.
Self‐reported penicillin allergy is common and frequently limits the available antimicrobial agents to choose from. This often results in the use of more expensive, potentially more toxic, and possibly less efficacious agents.[1, 2]
For over 30 years, penicilloyl‐polylysine (PPL) penicillin skin testing (PST) was widely used to diagnose penicillin allergy with a negative predictive value (NPV) of about 97% to 99%.[3] After being off the market for 5 years, PPL PST was reapproved in 2009 as PRE‐PEN.[4] However, many clinicians still fail to utilize PST despite its simplicity and substantial clinical impact. The main purpose of this study was to describe the predictive value of PST and impact on antibiotic selection in a sample of hospitalized patients with a reported history of penicillin allergy.
METHODS
In 2010, PST was introduced as a quality‐improvement measure after approval and support from the chief of professional services and the medical staff executive committee at Vidant Medical Center, an 861‐bed tertiary care and teaching hospital. Our antimicrobial stewardship program is regularly contacted for approval of alternative therapies in penicillin allergic patients. The PST quality‐improvement intervention was implemented to avoid resorting to less appropriate therapies in these situations. Following approval by the University and Medical Center Institutional Review Board, we designed a 4‐month study to assess the impact of this ongoing quality improvement measure from March 2012 to July 2012.
Hospitalized patients of all ages with reported penicillin allergies were obtained from our antimicrobial stewardship database. Their charts were reviewed for demographics, antibiotic use, clinical infection, and allergic description. Deciding whether to alter antibiotic therapy to a ‐lactam regimen was based on microbiologic results, laboratory values, clinical infection, and history of immunoglobulin E (IgE)‐mediated reactions, as defined by the updated drug allergy practice parameters.[5] IgE‐mediated reactions included: (1) immediate urticaria, laryngeal edema, or hypotension; (2) anemia; and (3) fever, arthralgias, lymphadenopathy, and an urticarial rash after 7 to 21 days.[5, 6, 7] We defined anaphylaxis as the development of angioedema or hemodynamic instability within 1 hour of penicillin administration. A true negative reaction was a lack of an IgE‐mediated reaction to all the drug challenges.
Patients in the medical, surgical, labor, and delivery wards; intensive care units; and emergency department underwent testing. The ‐lactam agent used after a negative PST was recorded, and the patients were followed for 24 hours after transitioning their therapy to a ‐lactam regimen. Excluded subjects included those with (1) nonIgE‐mediated reactions, (2) skin conditions that can give false positive results, (3) medications that may interfere with anaphylactic therapy, (4) history of severe exfoliative reactions to ‐lactams, (5) anaphylaxis less than 4 weeks prior, (6) allergies to antibiotics other than penicillin, and (7) uncertain allergy history.
PST Reagents/Procedure
Our benzylpenicilloyl major determinant molecule, commercially produced as PPL, was purchased as a PRE‐PEN from ALK‐Abello, Round Rock, Texas. Penicillin G potassium, purchased from Pfizer, New York, New York, is the only commercially available minor determinant and can improve identification of penicillin allergy by up to 97%.[2] The PST panel also included histamine (positive control) and normal saline (negative control).
Skin Testing Procedure
An infectious diseases fellow (R.H.R. or B.K.) was supervised in preparing for potential anaphylaxis, applying the reagents and interpreting the results based on drug allergy practice parameters.[5] The preliminary epicutaneous prick/puncture test was performed with a lancet in subjects without prior anaphylaxis using full‐strength PPL and penicillin G potassium reagents. If there was no response within 15 minutes, which we defined as a lack of wheal formation 3 mm or greater than that of the negative control, 0.02 to 0.03 mL of each reagent was injected intradermally using a tuberculin syringe and examined for 15 minutes.[5] If there was no response, patients were then challenged with either a single oral dose of penicillin V potassium 250 mg or whichever oral penicillin agent they previously reported an allergy to. If no reaction was appreciated within 2 hours, their therapy was changed to a ‐lactam agent including penicillins, cephalosporins, and carbapenems for the remaining duration of therapy (Figure 1) An estimate of NPV was obtained after 24 hours follow‐up.
Statistical Analysis
We designed a study to estimate whether the reapproved PST achieves an NPV of at least 95%.[3] We hypothesized that clinicians will be willing to utilize PST even if it has an NPV of slightly less than 98% compared to the current standard of treating patients without PST.[7] Assuming an equivalence margin of 3%, we estimated a sample size of 146 to achieve at least 82% power to test a hypothesis of NPV 95% using a 1‐sided Z test with a type‐I error rate of 5%.[8] Once the sample size of 146 subjects was reached, we stopped recruiting patients.
Sample characteristics of the subjects who underwent testing were summarized using descriptive statistics. Sample proportions were calculated to summarize categorical variables. Mean and standard deviation were calculated to summarize continuous variables. Cost analysis of antibiotic therapy was estimated from the Vidant Medical Center antibiotic pharmaceutical acquisition costs. Estimated cost of peripherally inserted central catheter (PICC) placement and removal as well as laboratory testing costs were obtained from our institution's medical billing department. Marketing costs of pharmacist drug calibration and nursing assessments with dressing changes were obtained from hospital‐affiliated outpatient antibiotic infusion companies.
RESULTS
A total of 4031 allergy histories were reviewed during the 5‐month study period to achieve the sample size of 146 patients (Table 1). Of those, 3885 were excluded (Figure 2). Common infections included pneumonias (26%) and urinary tract infections (20%) (Table 2) Only 1 subject had a positive reaction with hives, edema, and itching approximately 6 minutes after the agents were injected intradermally. The remaining 145 (99%) had negative reactions to the PST and oral challenge and were then successfully transitioned to a ‐lactam agent without any reaction at 24 hours, giving an NPV of 100%. Ten subjects were switched from intravenous to oral ‐lactam agents (Figure 1). Avoidance of PICC placement ($1,200) and removal ($65), dressing changes, weekly drug‐level testing, laboratory technician, and pharmaceutical drug calibration costs allowed for a healthcare reduction of $5,233 ($520/patient) based on the 146 patients studied. The total cost of therapy would have been $113,991 if the PST had not been performed. However, the cost of altered therapy following a negative PST was $81,180, a difference of $32,811 ($225/per patient) in a 5‐month period. The total estimated annual difference, including antibiotic alteration and associated drug‐costs, would be $82,000.
| Antibiotic | No. of Patients Reporting An Allergy | % Per Total Charts Reviewed |
|---|---|---|
| Penicillin | 428 | 10.6 |
| Sulfonamide | 271 | 6.7 |
| Quinolone | 108 | 2.7 |
| Cephalosporin | 81 | 2.0 |
| Macrolide | 65 | 1.6 |
| Vancomycin | 39 | 0.9 |
| Tetracycline | 20 | 0.5 |
| Clindamycin | 18 | 0.4 |
| Metronidazole | 9 | 0.2 |
| Linezolid | 2 | 0.05 |
| Categories | No. of Patients (%) |
|---|---|
| |
| Time since last reported penicillin use | |
| 1 month1 year | 6 (4) |
| 25 years | 39 (27) |
| 610 years | 23 (16) |
| >10 years | 78 (53) |
| Reported IgE‐mediated reactions | |
| Bronchospasm | 23 (16) |
| Urticarial rash | 100 (68) |
| Edema | 32 (22) |
| Anaphylaxis | 21 (14) |
| Age on admission, y | |
| 2050 | 28 (19) |
| 5160 | 29 (20) |
| 6170 | 41 (28) |
| 7180 | 24 (16) |
| >80 | 24 (16) |
| Gender | |
| Male | 55 (40) |
| Female | 88 (60) |
| Race | |
| White | 82 (56) |
| Black | 61 (42) |
| Hispanic | 3 (2) |
| Infections being treated | |
| Bacteremia | 7 (4.8) |
| Catheter‐related bloodstream infection | 2 (1.4) |
| Empyema | 1 (0.7) |
| Epidural abscess | 2 (1.4) |
| Infective endocarditis | 4 (2.7) |
| Intra‐abdominal infection | 24 (16.4) |
| Meningitis | 1 (0.7) |
| Neutropenic fever | 1 (0.7) |
| Osteomyelitis | 6 (4.1) |
| Pericardial effusion | 1 (0.7) |
| Prosthetic joint infection | 5 (3.4) |
| Pneumonia | 40 (27.4) |
| Skin and soft‐tissue infection | 20 (13.7) |
| Syphilis | 3 (2.1) |
| Urinary tract infection | 29 (19.7) |
DISCUSSION
PST is the most rapid, sensitive, and cost‐effective modality for evaluating patients with immediate allergic reactions to penicillin. Over 90% of individuals with a true history of penicillin allergy have confirmed sensitivity with a PST, implying most patients who are skin tested negative are truly not allergic.[7, 9, 10, 11, 12] Our study shows that the reapproved PST with the PPL and penicillin G determinants continues to have a high NPV. A patient with a negative PST result is generally at a low risk of developing an immediate‐type hypersensitivity reaction to penicillin.[2, 11] PST frequently allowed for less expensive agents that would have been avoided due to a reported allergy. The estimated annual savings of $82,000 dollars from antibiotic alteration with successful transition to a ‐lactam agent after a negative PST illustrates its value, supports its validity, and makes this study novel.
Many ‐lactamase inhibitors (ie, piperacillin‐tazobactam), fourth generation cephalosporins (ie, cefepime), and carbapenems still remain costly. Despite this, we were still able to achieve a significant reduction in overall cost. In addition to financial benefits, PST allowed for the use of more appropriate agents with less potential adverse effects. Narrow‐spectrum, non‐lactam agents were sometimes altered to a broader‐spectrum ‐lactam agent. We also frequently tailored 2 agents to just 1 broad‐spectrum ‐lactam. This led to more patients being given broad‐spectrum agents after the PST (72 vs 89 patients). However, we were able to avoid using second‐line agents, such as aztreonam, vancomycin, linezolid, daptomycin, and tobramycin, in many patients with infections that are often best treated with penicillin‐based antibiotics (ie, syphilis, group B Streptococcus infections). With increasing incidence and recovery of multidrug‐resistant bacteria, PST may also allow use of potentially more effective antimicrobial agents.
A possible limitation is that our prevalence of a true penicillin allergy was 1%, whereas Bousquet et al. illustrate a higher prevalence of about 20%.[7] Although our prevalence may not be generalizable, Bousquet's study only assessed patients with allergies 5 years prior.
The introduction of PST into clinical practice will allow trained healthcare providers to prescribe cheaper, more appropriate, less toxic antimicrobial agents. The overall benefit of reintroducing penicillin agents when needed in the future is far more cost‐effective than what is described here. PST should become a standard of care when prescribing antibiotics to patients with a history of penicillin allergy. Medical providers should be aware of its utility, acquire training, and incorporate it into their practice.
Acknowledgment
Disclosures: Paul P. Cook, MD, has potential conflicts of interest with Gilead (investigator), Pfizer (investigator), Merck (investigator and speakers' bureau), and Forest (speakers' bureau). Neither he nor any of the other authors has received any sources of funding for this article. For the remaining authors, no conflicts were declared. The corresponding author, Ramzy Rimawi, MD, had full access to all of the data in the study and had final responsibility for the decision to submit for publication.
- , , . Elective penicillin skin testing in a pediatric outpatient setting. Ann Allergy Asthma Immunol. 2006;97(6):807–812.
- US Department of Veterans Affairs Web site. Benzypenicilloyl polylisine (PRE‐PEN) national drug monograph. May 2012. Available at: http://www.pbm.va.gov/DrugMonograph.aspx. Accessed September 1, 2012.
- , . Diagnosis and management of penicillin allergy. Mayo Clin Proc. 2005;80(3):405–410.
- PRE‐PEN penicillin skin test antigen. Available at: http://www.alk‐abello.com/us/products/pre‐pen/Pages/PREPEN.aspx. Accessed September 1, 2012.
- , , , et al.; Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010;105:259–273.
- . Immunochemical mechanisms in penicillin allergy. Fed Proc. 1965;24:51–54.
- , , , et al. Oral challenges are needed in the diagnosis of beta‐lactam hypersensitivity. Clin Exp Allergy. 2008;38(1):185–190.
- , , . Sample Size Calculations in Clinical Research. New York, NY: Chapman 2003.
- , , , et al. Retrospective case series analysis of penicillin allergy testing in a UK specialist regional allergy clinic. J Clin Pathol. 2011;64:1014–1018.
- . Prevalence of skin test reactivity in patients with convincing, vague and unnacceptible histories of penicillin allergy. Allergy Asthma Proc. 2005;26(1):59–64.
- , . Frequency of systemic reactions to penicillin skin tests. Ann Allergy Asthma Immunol. 2000;85:363–365.
- , , , et al. The incidence of antimicrobial allergies in hospitalized patients. Arch Intern Med. 2000;160;2819–2822.
- , , . Elective penicillin skin testing in a pediatric outpatient setting. Ann Allergy Asthma Immunol. 2006;97(6):807–812.
- US Department of Veterans Affairs Web site. Benzypenicilloyl polylisine (PRE‐PEN) national drug monograph. May 2012. Available at: http://www.pbm.va.gov/DrugMonograph.aspx. Accessed September 1, 2012.
- , . Diagnosis and management of penicillin allergy. Mayo Clin Proc. 2005;80(3):405–410.
- PRE‐PEN penicillin skin test antigen. Available at: http://www.alk‐abello.com/us/products/pre‐pen/Pages/PREPEN.aspx. Accessed September 1, 2012.
- , , , et al.; Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010;105:259–273.
- . Immunochemical mechanisms in penicillin allergy. Fed Proc. 1965;24:51–54.
- , , , et al. Oral challenges are needed in the diagnosis of beta‐lactam hypersensitivity. Clin Exp Allergy. 2008;38(1):185–190.
- , , . Sample Size Calculations in Clinical Research. New York, NY: Chapman 2003.
- , , , et al. Retrospective case series analysis of penicillin allergy testing in a UK specialist regional allergy clinic. J Clin Pathol. 2011;64:1014–1018.
- . Prevalence of skin test reactivity in patients with convincing, vague and unnacceptible histories of penicillin allergy. Allergy Asthma Proc. 2005;26(1):59–64.
- , . Frequency of systemic reactions to penicillin skin tests. Ann Allergy Asthma Immunol. 2000;85:363–365.
- , , , et al. The incidence of antimicrobial allergies in hospitalized patients. Arch Intern Med. 2000;160;2819–2822.