User login
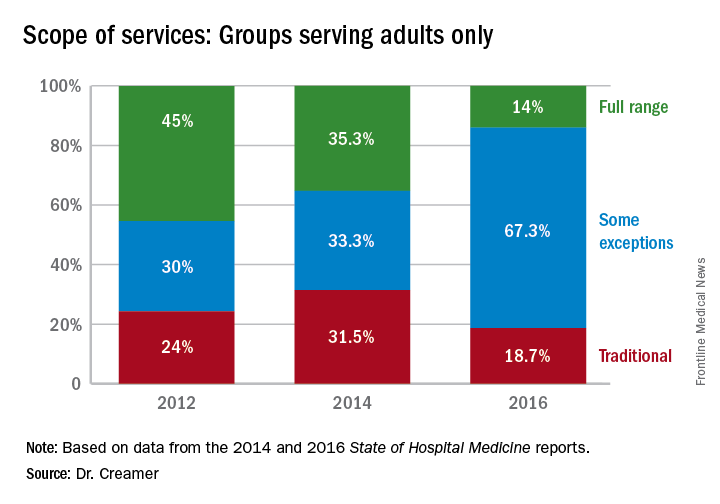
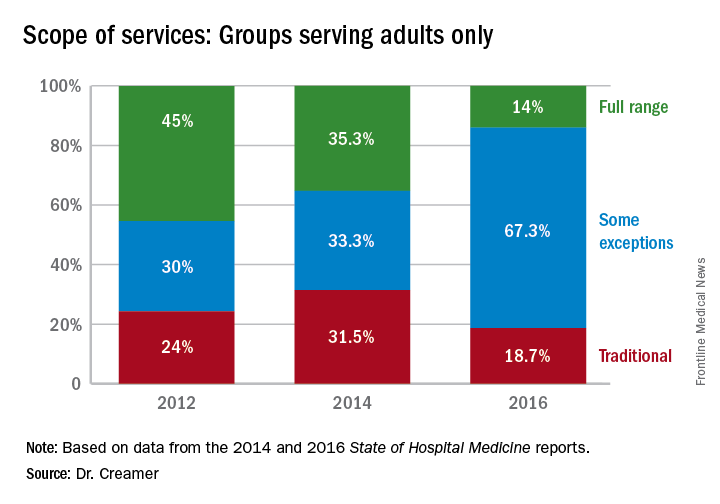
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
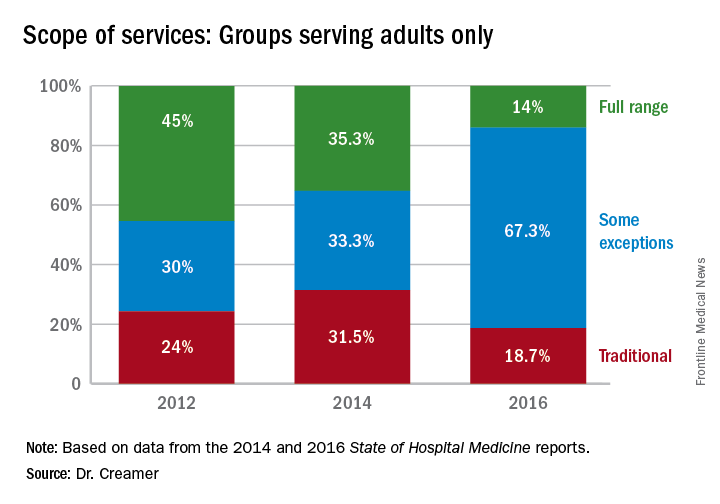
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
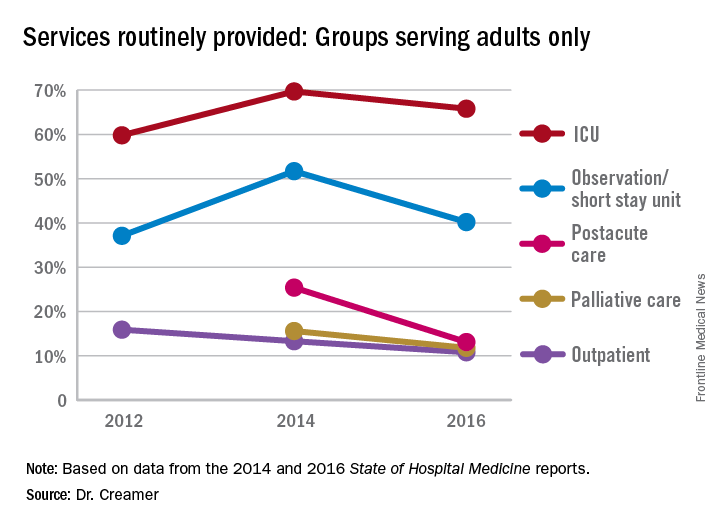
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
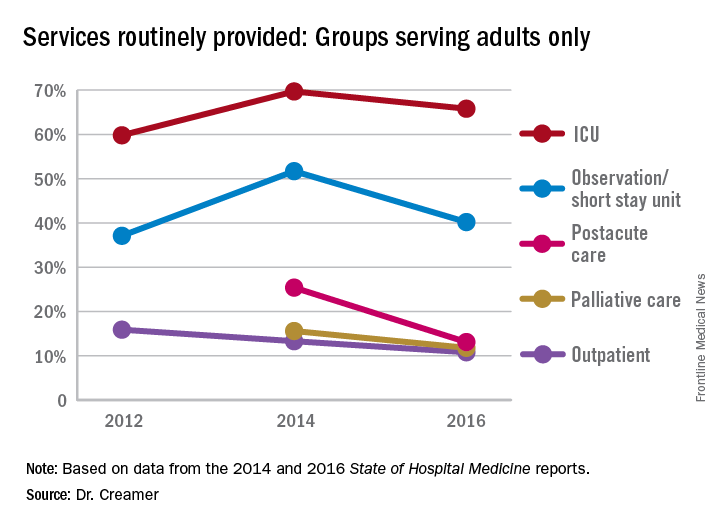
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
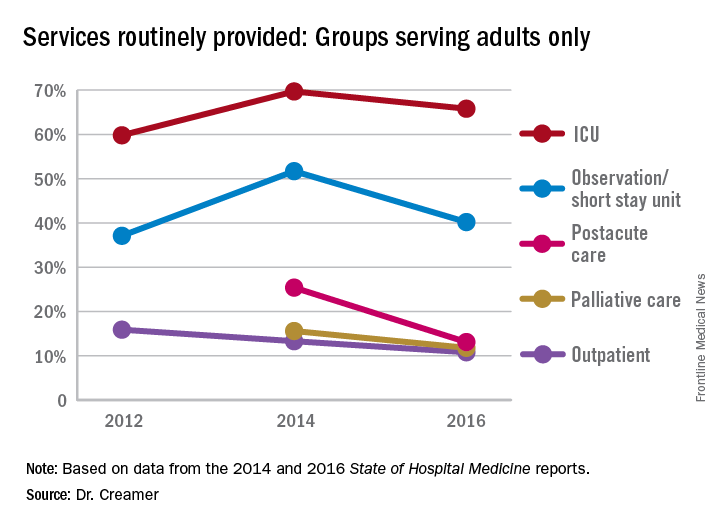
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).

