User login
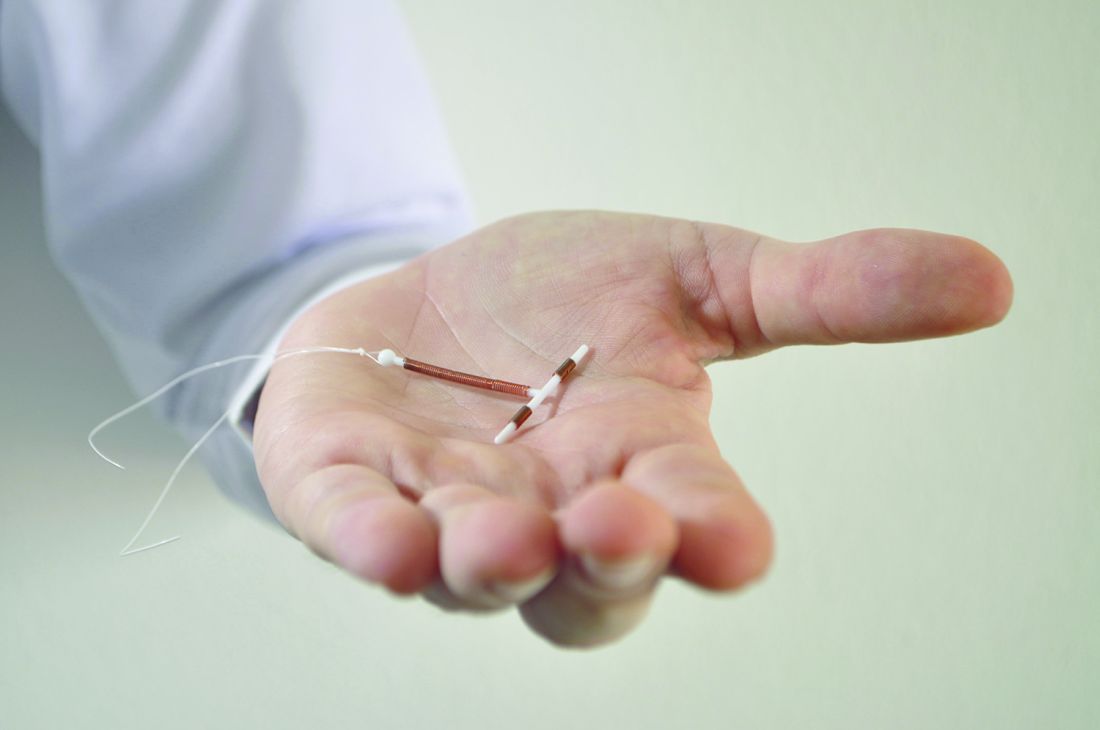
Hormonal intrauterine devices inserted immediately postpartum had a nearly six times greater likelihood of expulsion compared with copper IUDs, but most women who requested any type of long-acting reversible contraception (LARC) postpartum were still using it half a year later, a recent study found.
“With more than eight out of ten women continuing use at 6 months, in-hospital placement of postpartum LARC devices is a worthwhile intervention,” reported Jennifer L. Eggebroten, MD, and her associates at the University of Utah. “More than half of women who experienced IUD expulsion without commencement of another highly effective contraceptive went on to become pregnant within 2 years, highlighting the need for appropriate counseling prior to device placement and backup contraception planning.”
Ninety percent of the patients were Hispanic, 87% had prior children, and 87% had an income below $24,000. Most (77%) had a vaginal delivery. Those who requested the copper IUD tended to be older and have more children compared with those who asked for the hormonal IUD or implant.
Among the 289 patients who completed the 6 months of follow-up, 17% of those with a hormonal IUD had an expulsion, compared with 4% of women with copper IUDs. That translated to a 5.8 times greater risk of expulsion for hormonal IUDs than for copper ones after the researchers accounted for age, mode of delivery, parity, and any breastfeeding. Expulsion rates were statistically similar between those who had vaginal deliveries and those who had cesarean deliveries.
Just 8% of the women requested removal of their device during the 6 months of follow-up. Most (67%) of the 21 women who had expulsions asked for a replacement. Cost of the device delayed or prevented replacement in some cases. Over the next 2 years, 6 of the 11 women who did not get replacement devices became pregnant.
Meanwhile, 81% of women with a hormonal IUD (88% including replacements), 83% with a copper IUD (86% including replacements), and 90% with an implant were still using that device 6 months later. A quarter of the women who completed the study follow-up reported that they did not return to their providers for their postpartum exams.
“For patients at high risk of rapid repeat pregnancy or who may not return for a postpartum visit, the benefit of placement of a highly effective method of contraception in the hospital prior to discharge may outweigh the increased risk of expulsion,” the researchers wrote. “In some states, by 8 weeks, public insurance coverage may expire and women face much more challenging obstacles to affordable, highly effective birth control options.”
The University of Utah and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded the research. The University of Utah receives research funding from LARC manufacturers and one of the coauthors reported financial relationships with LARC manufacturers.
Hormonal intrauterine devices inserted immediately postpartum had a nearly six times greater likelihood of expulsion compared with copper IUDs, but most women who requested any type of long-acting reversible contraception (LARC) postpartum were still using it half a year later, a recent study found.
“With more than eight out of ten women continuing use at 6 months, in-hospital placement of postpartum LARC devices is a worthwhile intervention,” reported Jennifer L. Eggebroten, MD, and her associates at the University of Utah. “More than half of women who experienced IUD expulsion without commencement of another highly effective contraceptive went on to become pregnant within 2 years, highlighting the need for appropriate counseling prior to device placement and backup contraception planning.”
Ninety percent of the patients were Hispanic, 87% had prior children, and 87% had an income below $24,000. Most (77%) had a vaginal delivery. Those who requested the copper IUD tended to be older and have more children compared with those who asked for the hormonal IUD or implant.
Among the 289 patients who completed the 6 months of follow-up, 17% of those with a hormonal IUD had an expulsion, compared with 4% of women with copper IUDs. That translated to a 5.8 times greater risk of expulsion for hormonal IUDs than for copper ones after the researchers accounted for age, mode of delivery, parity, and any breastfeeding. Expulsion rates were statistically similar between those who had vaginal deliveries and those who had cesarean deliveries.
Just 8% of the women requested removal of their device during the 6 months of follow-up. Most (67%) of the 21 women who had expulsions asked for a replacement. Cost of the device delayed or prevented replacement in some cases. Over the next 2 years, 6 of the 11 women who did not get replacement devices became pregnant.
Meanwhile, 81% of women with a hormonal IUD (88% including replacements), 83% with a copper IUD (86% including replacements), and 90% with an implant were still using that device 6 months later. A quarter of the women who completed the study follow-up reported that they did not return to their providers for their postpartum exams.
“For patients at high risk of rapid repeat pregnancy or who may not return for a postpartum visit, the benefit of placement of a highly effective method of contraception in the hospital prior to discharge may outweigh the increased risk of expulsion,” the researchers wrote. “In some states, by 8 weeks, public insurance coverage may expire and women face much more challenging obstacles to affordable, highly effective birth control options.”
The University of Utah and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded the research. The University of Utah receives research funding from LARC manufacturers and one of the coauthors reported financial relationships with LARC manufacturers.
Hormonal intrauterine devices inserted immediately postpartum had a nearly six times greater likelihood of expulsion compared with copper IUDs, but most women who requested any type of long-acting reversible contraception (LARC) postpartum were still using it half a year later, a recent study found.
“With more than eight out of ten women continuing use at 6 months, in-hospital placement of postpartum LARC devices is a worthwhile intervention,” reported Jennifer L. Eggebroten, MD, and her associates at the University of Utah. “More than half of women who experienced IUD expulsion without commencement of another highly effective contraceptive went on to become pregnant within 2 years, highlighting the need for appropriate counseling prior to device placement and backup contraception planning.”
Ninety percent of the patients were Hispanic, 87% had prior children, and 87% had an income below $24,000. Most (77%) had a vaginal delivery. Those who requested the copper IUD tended to be older and have more children compared with those who asked for the hormonal IUD or implant.
Among the 289 patients who completed the 6 months of follow-up, 17% of those with a hormonal IUD had an expulsion, compared with 4% of women with copper IUDs. That translated to a 5.8 times greater risk of expulsion for hormonal IUDs than for copper ones after the researchers accounted for age, mode of delivery, parity, and any breastfeeding. Expulsion rates were statistically similar between those who had vaginal deliveries and those who had cesarean deliveries.
Just 8% of the women requested removal of their device during the 6 months of follow-up. Most (67%) of the 21 women who had expulsions asked for a replacement. Cost of the device delayed or prevented replacement in some cases. Over the next 2 years, 6 of the 11 women who did not get replacement devices became pregnant.
Meanwhile, 81% of women with a hormonal IUD (88% including replacements), 83% with a copper IUD (86% including replacements), and 90% with an implant were still using that device 6 months later. A quarter of the women who completed the study follow-up reported that they did not return to their providers for their postpartum exams.
“For patients at high risk of rapid repeat pregnancy or who may not return for a postpartum visit, the benefit of placement of a highly effective method of contraception in the hospital prior to discharge may outweigh the increased risk of expulsion,” the researchers wrote. “In some states, by 8 weeks, public insurance coverage may expire and women face much more challenging obstacles to affordable, highly effective birth control options.”
The University of Utah and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded the research. The University of Utah receives research funding from LARC manufacturers and one of the coauthors reported financial relationships with LARC manufacturers.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: Hormonal IUDs were 5.8 times more likely to be expelled than were copper ones, but at least 80% of women who received a LARC still had it 6 months later.
Data source: A prospective cohort of 325 women who received a hormonal or copper IUD or a contraceptive implant immediately postpartum between October 2013 and February 2016.
Disclosures: The University of Utah and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded the research. The University of Utah receives research funding from LARC manufacturers and one of the coauthors reported financial relationships with LARC manufacturers.