User login
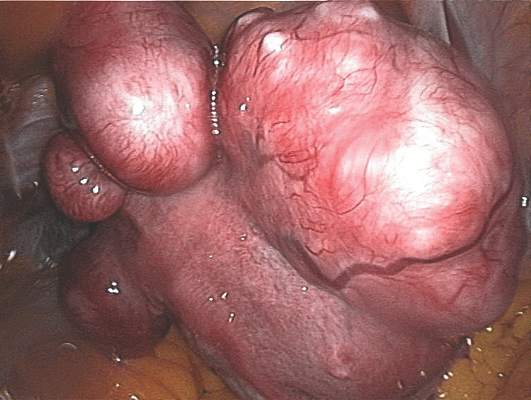
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Key clinical point: Between 20% and 39% of uterine fibroids and endometriosis cases in Europe are linked to two chemical exposures, and the associated costs exceed $1.5 billion annually.
Major finding: DDE-attributable fibroids and phthalate-attributable endometriosis cases were about 56,700 and 145,000, respectively, in 2010, with total combined economic and health care costs of about $1.5 billion.
Data source: Cohort biomarker data were used to assess European women’s exposures, and disease burden estimated from national health care databases.
Disclosures: The Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation sponsored the study, whose authors disclosed no conflicts.