User login
- Global ablation methods involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope.
- The endometrium should be destroyed or resected to the level of the basalis, which is approximately 4 to 6 mm deep.
- In cryoablation, freezing the tissue causes less pain than the heat energy associated with other ablation devices. The procedure typically takes 10 to 20 minutes.
- Not only is bipolar desiccation quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
- The advantage of hydrothermal ablation is that the circulating hot saline solution contacts the entire endometrial surface regardless of the shape or size of the cavity.
Traditionally, physicians have preferred hysterectomy for the treatment of abnormal uterine bleeding not related to endometrial cancer, representing about 20% of the 590,000 hysterectomie performed annually in the United States.1 The advent of standard endometrial ablation, e.g., surgical resection and rollerball desiccation, offered women less radical alternatives to hysterectomy. However, these “classic” methods are considered by some physicians to be technically difficult because they require the use of an operative hysteroscope—and all of its attendant risks. As a result, many Ob/Gyns continued to opt for hysterectomy when given a choice.
Now there are simpler alternatives: global ablation methods, including the newest—cryoablation, bipolar desiccation, and hydrothermal ablation. These procedures involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope. The advantage of these methods is that they are simple, rapid procedures that are easier to perform than standard endometrial ablation. Many surgeons who were uncomfortable utilizing the standard resectoscope can offer this treatment option to women with menorrhagia. In fact, it generally takes clinicians only 5 to 10 procedures to become proficient in endometrial ablation.
While global ablation is not intended to replace hysterectomy—the definitive treatment for most uterine pathology2—it gives patients a choice. Women who want permanent cessation of menses can choose hys-terectomy. Those who want to preserve the uterus or desire an outpatient procedure with minimal morbidity may opt for endometrial ablation. Regardless of the method they choose, patients who participate in the deci-sion-making process are more likely to be satisfied with their outcome.
The thinner the endometrial lining, the more likely ablation will be successful.
Part of this process includes an informed-consent discussion with the patient, including a review of each technique, its risks and complications, and outcomes. The long-term consequences of endometrial ablation remain unknown. The reason: Follow-up data beyond 24 months are minimal. And another question remains unanswered: How many women who have undergone endometrial ablation will develop endometrial carcinoma without symptomatic bleeding? There has been at least 1 report of this phenomenon occurring in a woman who ultimately underwent a hysterectomy for other reasons.3 Other case reports have noted uterine bleeding as the presenting symptom of endometrial carcinoma in women who had undergone ablation.4-6 The bottom line: The risk of asymptomatic endometrial cancer appears to be small in properly selected patients, i.e.,women without a history of endometrial hyperplasia or carcinoma (Table 1).
TABLE 1
Patient selection
INDICATIONS
|
CONTRAINDICATIONS
|
Preparation
Prior to performing any endometrial ablation, obtain an endometrial sample to rule out premalignant or malignant disease. Also, assess the endometrial cavity using either office hysteroscopy or sonohysterography to exclude the possibility of submucous myomata or polyps, which can be treated with simple resection. These imaging techniques also can reveal abnormally shaped uterine cavities, thus eliminating certain women as candidates for global techniques such as balloon ablation.
For all methods, destroy or resect the endometrium to the level of the basalis, which is approximately 4 to 6 mm deep, depending upon the stage of the menstrual cycle or cycle suppression. It is reasonable to assume that the thinner the endometrial lining, the more likely ablation will be successful. Several methods of producing endometrial atrophy have been used, including dilatation and curettage (D&C) and hormonal suppression with medroxyprogesterone acetate, oral contraceptives (OCs), danocrine, or gonadotropin releasing hormone ago-nists (GnRH-a). I prefer to use leuprolide acetate (7.5 mg for 1 dose) 4 to 5 weeks prior to performing cryoablation or hydrothermal ablation. (Pretreatment of the endometrial lining is not necessary with bipolar desiccation.)
Many patients who undergo endometrial ablation via either standard or global techniques can tolerate the procedure well with local anesthesia and intravenous sedation. This is especially true for global procedures because they are of short duration, i.e., about 5 to 20 minutes, depending on the method. Much of the pain results from cervical dilation and manipulation, as well as trauma to the endometrium. Therefore, the global ablation techniques that utilize the smallest probe (5.5 mm or smaller) and freeze the uterus, i.e., cryoablation, require the least anesthesia.
After the patient has been properly selected and prepared, proceed with one the global techniques—cryoablation, bipolar desiccation, or hydrothermal ablation—outlined in this article.
Cryoablation
Technique. Dilate the cervix and insert a 5.5-mm cryoprobe into the uterine cavity. Cool the probe to less than-80 degrees Celsius by liquid differential gas exchange, described by Joule-Thompson, utilizing the cooling unit (Her Option; CryoGen, San Diego, Calif). An elliptical ice ball approximately 3.5 by 5 cm will then form around the probe.
Using abdominal ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. (While the edge of the ice ball reaches 0 degrees Celsius, which is nondestructive to surrounding tissue, the endometrium is permanently destroyed approximately 1.5 cm from the edge of the ice ball, where a temperature of-20 degrees Celsius is reached.) Before the outer edge of the ice ball approaches the serosa of the uterus, stop the procedure (Figure 1). Heat the probe to body temperature and remove it from the cornu. Repeat the process in the contralateral cornu (Figure 2) and, in large uteri (greater than 10 cm sound), in the lower uterine segment (Figure 3). Each freeze cycle takes about 5 to 6 minutes.
FIGURE 1
Using ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. Stop before the edge of the ice ball approaches the serosa.
FIGURE 2
Heat the probe to body temperature, remove it from the first cornu, and repeat the process in the contralateral cornu.
FIGURE 3
For large uteri (greater than 10 cm sound), perform another freeze cycle in the lower uterine segment. Each cycle takes about 5 to 6 minutes.The number of ice balls needed to destroy the entire uterine cavity and the length of time required to perform the procedure depend on the size of the cavity. In general, 2 to 3 ice balls are sufficient, and the entire procedure takes 10 to 20 minutes.
In a recent randomized multicenter study, researchers investigated whether a freeze cycle longer than recommended would result in better outcomes. At 12-month follow-up, 7 (64%) of the 12 patients who underwent treatments of 5 to 7 minutes rather than 4 minutes were amenorrheic/spotting, with a 91% success rate.7 Larger studies are underway to confirm these data. Further, repeat treatment can contribute to better outcomes, especially when the patient receives leuprolide acetate prior to the procedure.8
Advantages. The primary advantage of cryoab-lation is that it is not a totally blind procedure. The visual feedback provided by the ultrasound facilitates complete ablation of the entire uterine cavity, regardless of size. Further, while the hysteroscope used in standard ablation allows the physician to see only the destruction of the surface epithelium, ultrasound enables the surgeon to visualize the depth of treatment during cryoablation.
Another advantage: Freezing tissue causes less pain (cryoanesthesia) than the heat energy associated with other ablation devices.
Disadvantages. While ultrasound visualization has its benefits, it also can complicate matters because accurate imaging and interpretation require a certain level of skill. For Ob/Gyns not experienced in ultrasound, there is a potential for poor positioning of the probe, which could lead to bowel and bladder injuries. Further, physicians can mistakenly place the cryoprobe back into the treated cornu instead of the contralateral side, leading to ablation of the uterine serosa. Lastly, the technology involved in this procedure increases the cost of the equipment and disposable instruments.
What the evidence shows. According to an unpublished study conducted by Cryogen, 54% of 222 patients experienced amenorrhea or staining only at 6-month follow-up. Ninety-three percent of the patients had a Patient Bleeding Assessment Card (PBAC) score of less than 75, and 75% of the patients had a greater than 90% reduction in their PBAC scores. (A score of greater than 150 was needed to enter the study; the score is reached by assigning a value to the amount of staining on a validated pad and adding these points based on the number of pads used per cycle.)
Cost. The disposable cryoprobes are $1,250 per case, and the unit costs $29,995. Since most ablation procedures currently are performed in the operating room, ancillary costs of the techniques are similar.
Bipolar desiccation
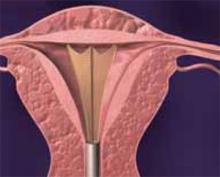
Technique. After dilating the cervix, insert the 8-mm NovaSure System (Novacept, Palo Alto, Calif) catheter into the uterus. To rule out auterine perforation prior to beginning the procedure, insert carbon dioxide (CO2) into the cavity (Figure 4).The machine will not turn on if a seal of CO2 has not been created, unless the surgeon overrides the system.
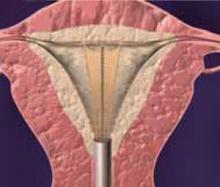
Then expand the 3-dimensional gold-plated bipolar mesh electrode, which imitates the shape of the uterine cavity, out of the catheter. Gently push the probe toward the fundus so that the mesh electrode is accurately positioned within the uterine cavity (Figure 5). Once the electrode is activated with up to 180 W of bipolar power, gentle suction brings the endometrium into close contact with the mesh (Figure 6). This suction also removes debris and allows for more complete desiccation.
The entire bipolar desiccation procedure takes less than 5 minutes to perform.
The system shuts down automatically when complete desiccation (calculated at 50 ohms of resistance) has occurred. The average treatment time is just over 1 minute, and the average depth of ablation is 4 to 5 mm.9 Once ablation is complete, retract the mesh electrode and remove the catheter (Figure 7). The entire procedure takes less than 5 minutes.
Advantages. Not only is the technique quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
Disadvantages. There are limited data on the 1-year success rates for this completely blind procedure. In addition, the uterus needs to be of normal shape to successfully ablate the endometrium.
What the evidence shows. Unpublished data from randomized, controlled clinical trials comparing bipolar desiccation with balloon ablation have demonstrated that the former achieves higher amenorrhea and success (a return to normal menstrual bleeding) rates than the latter. Further, patients treated with bipolar desiccation experienced less pain, both intra-operatively and postoperatively, than women who underwent balloon ablation.
Cost. Each disposable probe costs $850, and the bipolar controller lists for $15,000.
FIGURE 4
Dilate the cervix and insert the 8-mm catheter. To rule out a uterine perforation prior to beginning the procedure, place carbon dioxide in the cavity.
FIGURE 5
Expand the bipolar mesh electrode. Gently push the probe toward the fundus to accurately position the electrode within the uterine cavity.
FIGURE 6
Activate the electrode with up to 180 W of bipolar power. A gentle suction brings the endometrium into close contact with the mesh.
FIGURE 7
The system shuts down automatically when complete desiccation has occurred. Retract the bipolar mesh electrode and remove the catheter.
Hydrothermal ablation/circulating heated saline
Technique. Begin by dilating the cervix and inserting the sheath, which includes an 8-mm hysteroscope (Hydro ThermAblator; BEI Medical Systems, Teterboro, NJ), into the uter-ine cavity. Using gravity rather than a pump, introduce saline solution through the sheath into the uterus. As the saline circulates, gradually heat it until the solution reaches and maintains 90 degrees Celsius for 10 minutes, completely destroying the endometrium. (The total time from insertion of the sheath to completion of the procedure is 17 minutes.)
A safety feature detects whether any fluid has escaped from the closed system; a shutoff mechanism activates if more than 10 cc of fluid are lost. The system is controlled by software, so even physicians who are inexperienced with hysteroscopy can easily perform this technique.
Advantages. The primary advantage of hydrothermal ablation (HTA) is that the circulating hot saline solution contacts the entire endometrial surface regardless of the size or shape of the uterine cavity. In addition, since the procedure is performed under direct visualization, the surgeon can ensure that the entire cavity has been thoroughly ablated.
Disadvantages. One drawback is that it can be a painful procedure because the hysteroscope is large, necessitating wide dilation of the cervix, and hot water stimulates pain. Further, there have been unpublished reports of vaginal burns when the cervix created a poor seal around the sheath.
What the evidence shows. Based on their research of 276 women (187 women in the HTA group and 89 patients in the rollerball group), investigators have found that HTA has a treatment success rate of 77% compared to 82% for rollerball ablation. (The treatment success rate is defined as a PBAC score of 75 or lower; eumenorrhea is a score of less than 100.) Amenorrhea rates at 12-month follow-up were 40% and 51%, respectively. The researchers concluded that HTA offers an advantage over rollerball ablation in that it reduces anesthesia requirements and eliminates the problem of hypotonic fluid absorption.10
Cost. Disposable hysteroscopic tubing is $625 per case. The machine costs $10,900 plus $395 for the heater canister.
The author reports no financial relationship with any companies whose products are mentioned in this article.
1. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Engl J Med. 1993;Mar 25 328(12):856-860.
2. Carlson KJ, Miller BA, Fowler FJ, Jr. The Maine Women’s Health Study: I. Outcomes of hysterectomy. Obstet Gynecol. 1994;83-556.
3. Margolis MT, et al. Asymptomatic endometrial carcinoma after endometrial ablation. Int J Gynaecol Obstet. 1995;51-255.
4. Gimpelson RJ. Not so benign endometrial hyperplasia: endometrial cancer after endometrial ablation. J Am Assoc Gynecol Laparosc. 1997;4-507.
5. Horowitz IR, Copas PR, Aaronoff, et al. Endometrial adenocarcinoma following endometrial ablation for postmenopausal bleeding. Gynecol Oncol. 1995;56:460.-
6. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;179:569.-
7. Heppard M, et al. Data on 222 patients from a multicenter study using Cryogen First Option uterine cryoablation therapy in women with abnormal uterine bleeding. Obstet Gynecol. 2001;97(4 Suppl 1):S21.-
8. Sanders B. Preliminary outcomes of longer freeze cycles in the treatment of women with abnormal uterine bleeding using Cryogen First Option uterine cryoablation therapy. Obstet Gynecol. 2001;97(4 Suppl 1):S14.-
9. Cooper JM, Erickson ML. Global endometrial ablation technologies. Obstet Gynecol Clin North Am. 2000;27-385.
10. Corson SL. A multicenter evaluation of endometrial ablation by Hydro ThermAblator and rollerball for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2001;8(3):359-367.
- Global ablation methods involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope.
- The endometrium should be destroyed or resected to the level of the basalis, which is approximately 4 to 6 mm deep.
- In cryoablation, freezing the tissue causes less pain than the heat energy associated with other ablation devices. The procedure typically takes 10 to 20 minutes.
- Not only is bipolar desiccation quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
- The advantage of hydrothermal ablation is that the circulating hot saline solution contacts the entire endometrial surface regardless of the shape or size of the cavity.
Traditionally, physicians have preferred hysterectomy for the treatment of abnormal uterine bleeding not related to endometrial cancer, representing about 20% of the 590,000 hysterectomie performed annually in the United States.1 The advent of standard endometrial ablation, e.g., surgical resection and rollerball desiccation, offered women less radical alternatives to hysterectomy. However, these “classic” methods are considered by some physicians to be technically difficult because they require the use of an operative hysteroscope—and all of its attendant risks. As a result, many Ob/Gyns continued to opt for hysterectomy when given a choice.
Now there are simpler alternatives: global ablation methods, including the newest—cryoablation, bipolar desiccation, and hydrothermal ablation. These procedures involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope. The advantage of these methods is that they are simple, rapid procedures that are easier to perform than standard endometrial ablation. Many surgeons who were uncomfortable utilizing the standard resectoscope can offer this treatment option to women with menorrhagia. In fact, it generally takes clinicians only 5 to 10 procedures to become proficient in endometrial ablation.
While global ablation is not intended to replace hysterectomy—the definitive treatment for most uterine pathology2—it gives patients a choice. Women who want permanent cessation of menses can choose hys-terectomy. Those who want to preserve the uterus or desire an outpatient procedure with minimal morbidity may opt for endometrial ablation. Regardless of the method they choose, patients who participate in the deci-sion-making process are more likely to be satisfied with their outcome.
The thinner the endometrial lining, the more likely ablation will be successful.
Part of this process includes an informed-consent discussion with the patient, including a review of each technique, its risks and complications, and outcomes. The long-term consequences of endometrial ablation remain unknown. The reason: Follow-up data beyond 24 months are minimal. And another question remains unanswered: How many women who have undergone endometrial ablation will develop endometrial carcinoma without symptomatic bleeding? There has been at least 1 report of this phenomenon occurring in a woman who ultimately underwent a hysterectomy for other reasons.3 Other case reports have noted uterine bleeding as the presenting symptom of endometrial carcinoma in women who had undergone ablation.4-6 The bottom line: The risk of asymptomatic endometrial cancer appears to be small in properly selected patients, i.e.,women without a history of endometrial hyperplasia or carcinoma (Table 1).
TABLE 1
Patient selection
INDICATIONS
|
CONTRAINDICATIONS
|
Preparation
Prior to performing any endometrial ablation, obtain an endometrial sample to rule out premalignant or malignant disease. Also, assess the endometrial cavity using either office hysteroscopy or sonohysterography to exclude the possibility of submucous myomata or polyps, which can be treated with simple resection. These imaging techniques also can reveal abnormally shaped uterine cavities, thus eliminating certain women as candidates for global techniques such as balloon ablation.
For all methods, destroy or resect the endometrium to the level of the basalis, which is approximately 4 to 6 mm deep, depending upon the stage of the menstrual cycle or cycle suppression. It is reasonable to assume that the thinner the endometrial lining, the more likely ablation will be successful. Several methods of producing endometrial atrophy have been used, including dilatation and curettage (D&C) and hormonal suppression with medroxyprogesterone acetate, oral contraceptives (OCs), danocrine, or gonadotropin releasing hormone ago-nists (GnRH-a). I prefer to use leuprolide acetate (7.5 mg for 1 dose) 4 to 5 weeks prior to performing cryoablation or hydrothermal ablation. (Pretreatment of the endometrial lining is not necessary with bipolar desiccation.)
Many patients who undergo endometrial ablation via either standard or global techniques can tolerate the procedure well with local anesthesia and intravenous sedation. This is especially true for global procedures because they are of short duration, i.e., about 5 to 20 minutes, depending on the method. Much of the pain results from cervical dilation and manipulation, as well as trauma to the endometrium. Therefore, the global ablation techniques that utilize the smallest probe (5.5 mm or smaller) and freeze the uterus, i.e., cryoablation, require the least anesthesia.
After the patient has been properly selected and prepared, proceed with one the global techniques—cryoablation, bipolar desiccation, or hydrothermal ablation—outlined in this article.
Cryoablation
Technique. Dilate the cervix and insert a 5.5-mm cryoprobe into the uterine cavity. Cool the probe to less than-80 degrees Celsius by liquid differential gas exchange, described by Joule-Thompson, utilizing the cooling unit (Her Option; CryoGen, San Diego, Calif). An elliptical ice ball approximately 3.5 by 5 cm will then form around the probe.
Using abdominal ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. (While the edge of the ice ball reaches 0 degrees Celsius, which is nondestructive to surrounding tissue, the endometrium is permanently destroyed approximately 1.5 cm from the edge of the ice ball, where a temperature of-20 degrees Celsius is reached.) Before the outer edge of the ice ball approaches the serosa of the uterus, stop the procedure (Figure 1). Heat the probe to body temperature and remove it from the cornu. Repeat the process in the contralateral cornu (Figure 2) and, in large uteri (greater than 10 cm sound), in the lower uterine segment (Figure 3). Each freeze cycle takes about 5 to 6 minutes.
FIGURE 1
Using ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. Stop before the edge of the ice ball approaches the serosa.
FIGURE 2
Heat the probe to body temperature, remove it from the first cornu, and repeat the process in the contralateral cornu.
FIGURE 3
For large uteri (greater than 10 cm sound), perform another freeze cycle in the lower uterine segment. Each cycle takes about 5 to 6 minutes.The number of ice balls needed to destroy the entire uterine cavity and the length of time required to perform the procedure depend on the size of the cavity. In general, 2 to 3 ice balls are sufficient, and the entire procedure takes 10 to 20 minutes.
In a recent randomized multicenter study, researchers investigated whether a freeze cycle longer than recommended would result in better outcomes. At 12-month follow-up, 7 (64%) of the 12 patients who underwent treatments of 5 to 7 minutes rather than 4 minutes were amenorrheic/spotting, with a 91% success rate.7 Larger studies are underway to confirm these data. Further, repeat treatment can contribute to better outcomes, especially when the patient receives leuprolide acetate prior to the procedure.8
Advantages. The primary advantage of cryoab-lation is that it is not a totally blind procedure. The visual feedback provided by the ultrasound facilitates complete ablation of the entire uterine cavity, regardless of size. Further, while the hysteroscope used in standard ablation allows the physician to see only the destruction of the surface epithelium, ultrasound enables the surgeon to visualize the depth of treatment during cryoablation.
Another advantage: Freezing tissue causes less pain (cryoanesthesia) than the heat energy associated with other ablation devices.
Disadvantages. While ultrasound visualization has its benefits, it also can complicate matters because accurate imaging and interpretation require a certain level of skill. For Ob/Gyns not experienced in ultrasound, there is a potential for poor positioning of the probe, which could lead to bowel and bladder injuries. Further, physicians can mistakenly place the cryoprobe back into the treated cornu instead of the contralateral side, leading to ablation of the uterine serosa. Lastly, the technology involved in this procedure increases the cost of the equipment and disposable instruments.
What the evidence shows. According to an unpublished study conducted by Cryogen, 54% of 222 patients experienced amenorrhea or staining only at 6-month follow-up. Ninety-three percent of the patients had a Patient Bleeding Assessment Card (PBAC) score of less than 75, and 75% of the patients had a greater than 90% reduction in their PBAC scores. (A score of greater than 150 was needed to enter the study; the score is reached by assigning a value to the amount of staining on a validated pad and adding these points based on the number of pads used per cycle.)
Cost. The disposable cryoprobes are $1,250 per case, and the unit costs $29,995. Since most ablation procedures currently are performed in the operating room, ancillary costs of the techniques are similar.
Bipolar desiccation
Technique. After dilating the cervix, insert the 8-mm NovaSure System (Novacept, Palo Alto, Calif) catheter into the uterus. To rule out auterine perforation prior to beginning the procedure, insert carbon dioxide (CO2) into the cavity (Figure 4).The machine will not turn on if a seal of CO2 has not been created, unless the surgeon overrides the system.
Then expand the 3-dimensional gold-plated bipolar mesh electrode, which imitates the shape of the uterine cavity, out of the catheter. Gently push the probe toward the fundus so that the mesh electrode is accurately positioned within the uterine cavity (Figure 5). Once the electrode is activated with up to 180 W of bipolar power, gentle suction brings the endometrium into close contact with the mesh (Figure 6). This suction also removes debris and allows for more complete desiccation.
The entire bipolar desiccation procedure takes less than 5 minutes to perform.
The system shuts down automatically when complete desiccation (calculated at 50 ohms of resistance) has occurred. The average treatment time is just over 1 minute, and the average depth of ablation is 4 to 5 mm.9 Once ablation is complete, retract the mesh electrode and remove the catheter (Figure 7). The entire procedure takes less than 5 minutes.
Advantages. Not only is the technique quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
Disadvantages. There are limited data on the 1-year success rates for this completely blind procedure. In addition, the uterus needs to be of normal shape to successfully ablate the endometrium.
What the evidence shows. Unpublished data from randomized, controlled clinical trials comparing bipolar desiccation with balloon ablation have demonstrated that the former achieves higher amenorrhea and success (a return to normal menstrual bleeding) rates than the latter. Further, patients treated with bipolar desiccation experienced less pain, both intra-operatively and postoperatively, than women who underwent balloon ablation.
Cost. Each disposable probe costs $850, and the bipolar controller lists for $15,000.
FIGURE 4
Dilate the cervix and insert the 8-mm catheter. To rule out a uterine perforation prior to beginning the procedure, place carbon dioxide in the cavity.
FIGURE 5
Expand the bipolar mesh electrode. Gently push the probe toward the fundus to accurately position the electrode within the uterine cavity.
FIGURE 6
Activate the electrode with up to 180 W of bipolar power. A gentle suction brings the endometrium into close contact with the mesh.
FIGURE 7
The system shuts down automatically when complete desiccation has occurred. Retract the bipolar mesh electrode and remove the catheter.
Hydrothermal ablation/circulating heated saline
Technique. Begin by dilating the cervix and inserting the sheath, which includes an 8-mm hysteroscope (Hydro ThermAblator; BEI Medical Systems, Teterboro, NJ), into the uter-ine cavity. Using gravity rather than a pump, introduce saline solution through the sheath into the uterus. As the saline circulates, gradually heat it until the solution reaches and maintains 90 degrees Celsius for 10 minutes, completely destroying the endometrium. (The total time from insertion of the sheath to completion of the procedure is 17 minutes.)
A safety feature detects whether any fluid has escaped from the closed system; a shutoff mechanism activates if more than 10 cc of fluid are lost. The system is controlled by software, so even physicians who are inexperienced with hysteroscopy can easily perform this technique.
Advantages. The primary advantage of hydrothermal ablation (HTA) is that the circulating hot saline solution contacts the entire endometrial surface regardless of the size or shape of the uterine cavity. In addition, since the procedure is performed under direct visualization, the surgeon can ensure that the entire cavity has been thoroughly ablated.
Disadvantages. One drawback is that it can be a painful procedure because the hysteroscope is large, necessitating wide dilation of the cervix, and hot water stimulates pain. Further, there have been unpublished reports of vaginal burns when the cervix created a poor seal around the sheath.
What the evidence shows. Based on their research of 276 women (187 women in the HTA group and 89 patients in the rollerball group), investigators have found that HTA has a treatment success rate of 77% compared to 82% for rollerball ablation. (The treatment success rate is defined as a PBAC score of 75 or lower; eumenorrhea is a score of less than 100.) Amenorrhea rates at 12-month follow-up were 40% and 51%, respectively. The researchers concluded that HTA offers an advantage over rollerball ablation in that it reduces anesthesia requirements and eliminates the problem of hypotonic fluid absorption.10
Cost. Disposable hysteroscopic tubing is $625 per case. The machine costs $10,900 plus $395 for the heater canister.
The author reports no financial relationship with any companies whose products are mentioned in this article.
- Global ablation methods involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope.
- The endometrium should be destroyed or resected to the level of the basalis, which is approximately 4 to 6 mm deep.
- In cryoablation, freezing the tissue causes less pain than the heat energy associated with other ablation devices. The procedure typically takes 10 to 20 minutes.
- Not only is bipolar desiccation quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
- The advantage of hydrothermal ablation is that the circulating hot saline solution contacts the entire endometrial surface regardless of the shape or size of the cavity.
Traditionally, physicians have preferred hysterectomy for the treatment of abnormal uterine bleeding not related to endometrial cancer, representing about 20% of the 590,000 hysterectomie performed annually in the United States.1 The advent of standard endometrial ablation, e.g., surgical resection and rollerball desiccation, offered women less radical alternatives to hysterectomy. However, these “classic” methods are considered by some physicians to be technically difficult because they require the use of an operative hysteroscope—and all of its attendant risks. As a result, many Ob/Gyns continued to opt for hysterectomy when given a choice.
Now there are simpler alternatives: global ablation methods, including the newest—cryoablation, bipolar desiccation, and hydrothermal ablation. These procedures involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope. The advantage of these methods is that they are simple, rapid procedures that are easier to perform than standard endometrial ablation. Many surgeons who were uncomfortable utilizing the standard resectoscope can offer this treatment option to women with menorrhagia. In fact, it generally takes clinicians only 5 to 10 procedures to become proficient in endometrial ablation.
While global ablation is not intended to replace hysterectomy—the definitive treatment for most uterine pathology2—it gives patients a choice. Women who want permanent cessation of menses can choose hys-terectomy. Those who want to preserve the uterus or desire an outpatient procedure with minimal morbidity may opt for endometrial ablation. Regardless of the method they choose, patients who participate in the deci-sion-making process are more likely to be satisfied with their outcome.
The thinner the endometrial lining, the more likely ablation will be successful.
Part of this process includes an informed-consent discussion with the patient, including a review of each technique, its risks and complications, and outcomes. The long-term consequences of endometrial ablation remain unknown. The reason: Follow-up data beyond 24 months are minimal. And another question remains unanswered: How many women who have undergone endometrial ablation will develop endometrial carcinoma without symptomatic bleeding? There has been at least 1 report of this phenomenon occurring in a woman who ultimately underwent a hysterectomy for other reasons.3 Other case reports have noted uterine bleeding as the presenting symptom of endometrial carcinoma in women who had undergone ablation.4-6 The bottom line: The risk of asymptomatic endometrial cancer appears to be small in properly selected patients, i.e.,women without a history of endometrial hyperplasia or carcinoma (Table 1).
TABLE 1
Patient selection
INDICATIONS
|
CONTRAINDICATIONS
|
Preparation
Prior to performing any endometrial ablation, obtain an endometrial sample to rule out premalignant or malignant disease. Also, assess the endometrial cavity using either office hysteroscopy or sonohysterography to exclude the possibility of submucous myomata or polyps, which can be treated with simple resection. These imaging techniques also can reveal abnormally shaped uterine cavities, thus eliminating certain women as candidates for global techniques such as balloon ablation.
For all methods, destroy or resect the endometrium to the level of the basalis, which is approximately 4 to 6 mm deep, depending upon the stage of the menstrual cycle or cycle suppression. It is reasonable to assume that the thinner the endometrial lining, the more likely ablation will be successful. Several methods of producing endometrial atrophy have been used, including dilatation and curettage (D&C) and hormonal suppression with medroxyprogesterone acetate, oral contraceptives (OCs), danocrine, or gonadotropin releasing hormone ago-nists (GnRH-a). I prefer to use leuprolide acetate (7.5 mg for 1 dose) 4 to 5 weeks prior to performing cryoablation or hydrothermal ablation. (Pretreatment of the endometrial lining is not necessary with bipolar desiccation.)
Many patients who undergo endometrial ablation via either standard or global techniques can tolerate the procedure well with local anesthesia and intravenous sedation. This is especially true for global procedures because they are of short duration, i.e., about 5 to 20 minutes, depending on the method. Much of the pain results from cervical dilation and manipulation, as well as trauma to the endometrium. Therefore, the global ablation techniques that utilize the smallest probe (5.5 mm or smaller) and freeze the uterus, i.e., cryoablation, require the least anesthesia.
After the patient has been properly selected and prepared, proceed with one the global techniques—cryoablation, bipolar desiccation, or hydrothermal ablation—outlined in this article.
Cryoablation
Technique. Dilate the cervix and insert a 5.5-mm cryoprobe into the uterine cavity. Cool the probe to less than-80 degrees Celsius by liquid differential gas exchange, described by Joule-Thompson, utilizing the cooling unit (Her Option; CryoGen, San Diego, Calif). An elliptical ice ball approximately 3.5 by 5 cm will then form around the probe.
Using abdominal ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. (While the edge of the ice ball reaches 0 degrees Celsius, which is nondestructive to surrounding tissue, the endometrium is permanently destroyed approximately 1.5 cm from the edge of the ice ball, where a temperature of-20 degrees Celsius is reached.) Before the outer edge of the ice ball approaches the serosa of the uterus, stop the procedure (Figure 1). Heat the probe to body temperature and remove it from the cornu. Repeat the process in the contralateral cornu (Figure 2) and, in large uteri (greater than 10 cm sound), in the lower uterine segment (Figure 3). Each freeze cycle takes about 5 to 6 minutes.
FIGURE 1
Using ultrasound guidance, follow the edge of the ice ball into the uterine muscle at 1 cornu. Stop before the edge of the ice ball approaches the serosa.
FIGURE 2
Heat the probe to body temperature, remove it from the first cornu, and repeat the process in the contralateral cornu.
FIGURE 3
For large uteri (greater than 10 cm sound), perform another freeze cycle in the lower uterine segment. Each cycle takes about 5 to 6 minutes.The number of ice balls needed to destroy the entire uterine cavity and the length of time required to perform the procedure depend on the size of the cavity. In general, 2 to 3 ice balls are sufficient, and the entire procedure takes 10 to 20 minutes.
In a recent randomized multicenter study, researchers investigated whether a freeze cycle longer than recommended would result in better outcomes. At 12-month follow-up, 7 (64%) of the 12 patients who underwent treatments of 5 to 7 minutes rather than 4 minutes were amenorrheic/spotting, with a 91% success rate.7 Larger studies are underway to confirm these data. Further, repeat treatment can contribute to better outcomes, especially when the patient receives leuprolide acetate prior to the procedure.8
Advantages. The primary advantage of cryoab-lation is that it is not a totally blind procedure. The visual feedback provided by the ultrasound facilitates complete ablation of the entire uterine cavity, regardless of size. Further, while the hysteroscope used in standard ablation allows the physician to see only the destruction of the surface epithelium, ultrasound enables the surgeon to visualize the depth of treatment during cryoablation.
Another advantage: Freezing tissue causes less pain (cryoanesthesia) than the heat energy associated with other ablation devices.
Disadvantages. While ultrasound visualization has its benefits, it also can complicate matters because accurate imaging and interpretation require a certain level of skill. For Ob/Gyns not experienced in ultrasound, there is a potential for poor positioning of the probe, which could lead to bowel and bladder injuries. Further, physicians can mistakenly place the cryoprobe back into the treated cornu instead of the contralateral side, leading to ablation of the uterine serosa. Lastly, the technology involved in this procedure increases the cost of the equipment and disposable instruments.
What the evidence shows. According to an unpublished study conducted by Cryogen, 54% of 222 patients experienced amenorrhea or staining only at 6-month follow-up. Ninety-three percent of the patients had a Patient Bleeding Assessment Card (PBAC) score of less than 75, and 75% of the patients had a greater than 90% reduction in their PBAC scores. (A score of greater than 150 was needed to enter the study; the score is reached by assigning a value to the amount of staining on a validated pad and adding these points based on the number of pads used per cycle.)
Cost. The disposable cryoprobes are $1,250 per case, and the unit costs $29,995. Since most ablation procedures currently are performed in the operating room, ancillary costs of the techniques are similar.
Bipolar desiccation
Technique. After dilating the cervix, insert the 8-mm NovaSure System (Novacept, Palo Alto, Calif) catheter into the uterus. To rule out auterine perforation prior to beginning the procedure, insert carbon dioxide (CO2) into the cavity (Figure 4).The machine will not turn on if a seal of CO2 has not been created, unless the surgeon overrides the system.
Then expand the 3-dimensional gold-plated bipolar mesh electrode, which imitates the shape of the uterine cavity, out of the catheter. Gently push the probe toward the fundus so that the mesh electrode is accurately positioned within the uterine cavity (Figure 5). Once the electrode is activated with up to 180 W of bipolar power, gentle suction brings the endometrium into close contact with the mesh (Figure 6). This suction also removes debris and allows for more complete desiccation.
The entire bipolar desiccation procedure takes less than 5 minutes to perform.
The system shuts down automatically when complete desiccation (calculated at 50 ohms of resistance) has occurred. The average treatment time is just over 1 minute, and the average depth of ablation is 4 to 5 mm.9 Once ablation is complete, retract the mesh electrode and remove the catheter (Figure 7). The entire procedure takes less than 5 minutes.
Advantages. Not only is the technique quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness.
Disadvantages. There are limited data on the 1-year success rates for this completely blind procedure. In addition, the uterus needs to be of normal shape to successfully ablate the endometrium.
What the evidence shows. Unpublished data from randomized, controlled clinical trials comparing bipolar desiccation with balloon ablation have demonstrated that the former achieves higher amenorrhea and success (a return to normal menstrual bleeding) rates than the latter. Further, patients treated with bipolar desiccation experienced less pain, both intra-operatively and postoperatively, than women who underwent balloon ablation.
Cost. Each disposable probe costs $850, and the bipolar controller lists for $15,000.
FIGURE 4
Dilate the cervix and insert the 8-mm catheter. To rule out a uterine perforation prior to beginning the procedure, place carbon dioxide in the cavity.
FIGURE 5
Expand the bipolar mesh electrode. Gently push the probe toward the fundus to accurately position the electrode within the uterine cavity.
FIGURE 6
Activate the electrode with up to 180 W of bipolar power. A gentle suction brings the endometrium into close contact with the mesh.
FIGURE 7
The system shuts down automatically when complete desiccation has occurred. Retract the bipolar mesh electrode and remove the catheter.
Hydrothermal ablation/circulating heated saline
Technique. Begin by dilating the cervix and inserting the sheath, which includes an 8-mm hysteroscope (Hydro ThermAblator; BEI Medical Systems, Teterboro, NJ), into the uter-ine cavity. Using gravity rather than a pump, introduce saline solution through the sheath into the uterus. As the saline circulates, gradually heat it until the solution reaches and maintains 90 degrees Celsius for 10 minutes, completely destroying the endometrium. (The total time from insertion of the sheath to completion of the procedure is 17 minutes.)
A safety feature detects whether any fluid has escaped from the closed system; a shutoff mechanism activates if more than 10 cc of fluid are lost. The system is controlled by software, so even physicians who are inexperienced with hysteroscopy can easily perform this technique.
Advantages. The primary advantage of hydrothermal ablation (HTA) is that the circulating hot saline solution contacts the entire endometrial surface regardless of the size or shape of the uterine cavity. In addition, since the procedure is performed under direct visualization, the surgeon can ensure that the entire cavity has been thoroughly ablated.
Disadvantages. One drawback is that it can be a painful procedure because the hysteroscope is large, necessitating wide dilation of the cervix, and hot water stimulates pain. Further, there have been unpublished reports of vaginal burns when the cervix created a poor seal around the sheath.
What the evidence shows. Based on their research of 276 women (187 women in the HTA group and 89 patients in the rollerball group), investigators have found that HTA has a treatment success rate of 77% compared to 82% for rollerball ablation. (The treatment success rate is defined as a PBAC score of 75 or lower; eumenorrhea is a score of less than 100.) Amenorrhea rates at 12-month follow-up were 40% and 51%, respectively. The researchers concluded that HTA offers an advantage over rollerball ablation in that it reduces anesthesia requirements and eliminates the problem of hypotonic fluid absorption.10
Cost. Disposable hysteroscopic tubing is $625 per case. The machine costs $10,900 plus $395 for the heater canister.
The author reports no financial relationship with any companies whose products are mentioned in this article.
1. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Engl J Med. 1993;Mar 25 328(12):856-860.
2. Carlson KJ, Miller BA, Fowler FJ, Jr. The Maine Women’s Health Study: I. Outcomes of hysterectomy. Obstet Gynecol. 1994;83-556.
3. Margolis MT, et al. Asymptomatic endometrial carcinoma after endometrial ablation. Int J Gynaecol Obstet. 1995;51-255.
4. Gimpelson RJ. Not so benign endometrial hyperplasia: endometrial cancer after endometrial ablation. J Am Assoc Gynecol Laparosc. 1997;4-507.
5. Horowitz IR, Copas PR, Aaronoff, et al. Endometrial adenocarcinoma following endometrial ablation for postmenopausal bleeding. Gynecol Oncol. 1995;56:460.-
6. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;179:569.-
7. Heppard M, et al. Data on 222 patients from a multicenter study using Cryogen First Option uterine cryoablation therapy in women with abnormal uterine bleeding. Obstet Gynecol. 2001;97(4 Suppl 1):S21.-
8. Sanders B. Preliminary outcomes of longer freeze cycles in the treatment of women with abnormal uterine bleeding using Cryogen First Option uterine cryoablation therapy. Obstet Gynecol. 2001;97(4 Suppl 1):S14.-
9. Cooper JM, Erickson ML. Global endometrial ablation technologies. Obstet Gynecol Clin North Am. 2000;27-385.
10. Corson SL. A multicenter evaluation of endometrial ablation by Hydro ThermAblator and rollerball for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2001;8(3):359-367.
1. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Engl J Med. 1993;Mar 25 328(12):856-860.
2. Carlson KJ, Miller BA, Fowler FJ, Jr. The Maine Women’s Health Study: I. Outcomes of hysterectomy. Obstet Gynecol. 1994;83-556.
3. Margolis MT, et al. Asymptomatic endometrial carcinoma after endometrial ablation. Int J Gynaecol Obstet. 1995;51-255.
4. Gimpelson RJ. Not so benign endometrial hyperplasia: endometrial cancer after endometrial ablation. J Am Assoc Gynecol Laparosc. 1997;4-507.
5. Horowitz IR, Copas PR, Aaronoff, et al. Endometrial adenocarcinoma following endometrial ablation for postmenopausal bleeding. Gynecol Oncol. 1995;56:460.-
6. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;179:569.-
7. Heppard M, et al. Data on 222 patients from a multicenter study using Cryogen First Option uterine cryoablation therapy in women with abnormal uterine bleeding. Obstet Gynecol. 2001;97(4 Suppl 1):S21.-
8. Sanders B. Preliminary outcomes of longer freeze cycles in the treatment of women with abnormal uterine bleeding using Cryogen First Option uterine cryoablation therapy. Obstet Gynecol. 2001;97(4 Suppl 1):S14.-
9. Cooper JM, Erickson ML. Global endometrial ablation technologies. Obstet Gynecol Clin North Am. 2000;27-385.
10. Corson SL. A multicenter evaluation of endometrial ablation by Hydro ThermAblator and rollerball for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2001;8(3):359-367.