User login
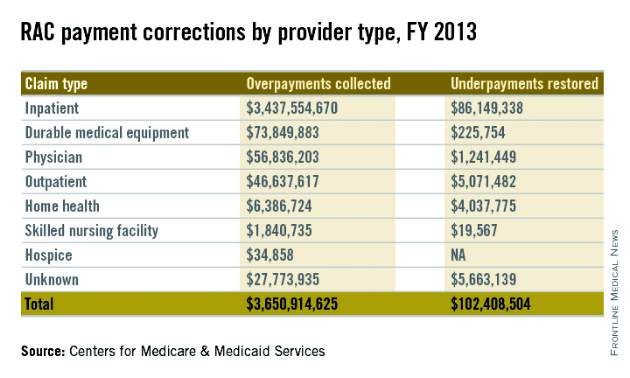
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med