User login
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
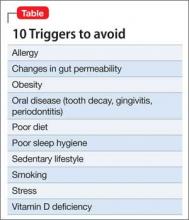
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.