User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
CMS inpatient payment rule for 2024: Key takeaways
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
Bone-bashing effects of air pollution becoming clearer
We have long recognized that our environment has a significant impact on our general health. Air pollution is known to contribute to respiratory conditions, poor cardiovascular outcomes, and certain kinds of cancer.
It’s increasingly important to identify factors that might contribute to suboptimal bone density and associated fracture risk in the population as a whole, and particularly in older adults. Aging is associated with a higher risk for osteoporosis and fractures, with their attendant morbidity, but individuals differ in their extent of bone loss and risk for fractures.
Known factors affecting bone health include genetics, age, sex, nutrition, physical activity, and hormonal factors. Certain medications, diseases, and lifestyle choices – such as smoking and alcohol intake – can also have deleterious effects on bone.
More recently, researchers have started examining the impact of air pollution on bone health.
As we know, the degree of pollution varies greatly from one region to another and can potentially significantly affect life in many parts of the world. In fact, the World Health Organization indicates that 99% of the world’s population breathes air exceeding the WHO guideline limits for pollutants.
Air pollutants include particulate matter (PM) as well as gases, such as nitric oxide, nitrogen dioxide, ammonia, carbon monoxide, sulfur dioxide, ozone, and certain volatile organic compounds. Particulate pollutants include a variety of substances produced from mostly human activities (such as vehicle emissions, biofuel combustion, mining, agriculture, and manufacturing, and also forest fires). They are classified not by their composition, but by their size (for example, PM1.0, PM2.5, and PM10 indicate PM with a diameter < 1.0, 2.5, and 10 microns, respectively). The finer the particle, the more likely it is to cross into the systemic circulation from the respiratory tract, with the potential to induce oxidative, inflammatory, and other changes in the body.
Many studies report that air pollution is a risk factor for osteoporosis. Some have found associations of lower bone density, osteoporosis, and fracture risk with higher concentrations of PM1.0, PM2.5, or PM10, even after controlling for other factors that could affect bone health. Some researchers have reported that although they didn’t find a significant association between PM and bone health, they did find an association between distance from the freeway and bone health – thus, exposure to polycyclic aromatic hydrocarbons and black carbon from vehicle emissions needs to be studied as a contributor to fracture risk.
Importantly, a prospective, observational study from the Women’s Health Initiative (which included more than 9,000 ethnically diverse women from three sites in the United States) reported a significant negative impact of PM10, nitric oxide, nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years on bone density at multiple sites, and particularly at the lumbar spine, in both cross-sectional and longitudinal analyses after controlling for demographic and socioeconomic factors. This study reported that nitrogen dioxide exposure may be a key determinant of bone density at the lumbar spine and in the whole body. Similarly, other studies have reported associations between atmospheric nitrogen dioxide or sulfur dioxide and risk for osteoporotic fractures.
Why the impact on bones?
The potential negative impact of pollution on bone has been attributed to many factors. PM induces systemic inflammation and an increase in cytokines that stimulate bone cells (osteoclasts) that cause bone loss. Other pollutants (gases and metal compounds) can cause oxidative damage to bone cells, whereas others act as endocrine disrupters and affect the functioning of these cells.
Pollution might also affect the synthesis and metabolism of vitamin D, which is necessary for absorption of calcium from the gut. High rates of pollution can reduce the amount of ultraviolet radiation reaching the earth which is important because certain wavelengths of ultraviolet radiation are necessary for vitamin D synthesis in our skin. Reduced vitamin D synthesis in skin can lead to poorly mineralized bone unless there is sufficient intake of vitamin D in diet or as supplements. Also, the conversion of vitamin D to its active form happens in the kidneys, and PM can be harmful to renal function. PM is also believed to cause increased breakdown of vitamin D into its inactive form.
Conversely, some studies have reported no association between pollution and bone density or osteoporosis risk, and two meta-analyses indicated that the association between the two is inconsistent. Some factors explaining variances in results include the number of individuals included in the study (larger studies are generally considered to be more reproducible), the fact that most studies are cross-sectional and not prospective, many do not control for other factors that might be deleterious to bone, and prediction models for the extent of PM or other exposure may not be completely accurate.
However, another recent meta-analysis reported an increased risk for lower total-body bone density and hip fracture after exposure to air pollution, particularly PM2.5 and nitrogen dioxide, but not to PM10, nitric oxide, or ozone. More studies are needed to confirm, or refute, the association between air pollution and impaired bone health. But accumulating evidence suggests that air pollution very likely has a deleterious effect on bone.
When feasible, it’s important to avoid living or working in areas with poor air quality and high pollution rates. However, this isn’t always possible based on one’s occupation, geography, circumstances, or economic status. Therefore, attention to a cleaner environment is critical at both the individual and the macro level.
As an example of the latter, the city of London extended its ultralow emission zone (ULEZ) farther out of the city in October 2021, and a further expansion is planned to include all of the city’s boroughs in August 2023.
We can do our bit by driving less and walking, biking, or using public transportation more often. We can also turn off the car engine when it’s not running, maintain our vehicles, switch to electric or hand-powered yard equipment, and not burn household garbage and limit backyard fires. We can also switch from gas to solar energy or wind, use efficient appliances and heating, and avoid unnecessary energy use. And we can choose sustainable products when possible.
For optimal bone health, we should remind patients to eat a healthy diet with the requisite amount of protein, calcium, and vitamin D. Vitamin D and calcium supplementation may be necessary for people whose intake of dairy and dairy products is low. Other important strategies to optimize bone health include engaging in healthy physical activity; avoiding smoking or excessive alcohol intake; and treating underlying gastrointestinal, endocrine, or other conditions that can reduce bone density.
Madhusmita Misra, MD, MPH, is the chief of the division of pediatric endocrinology, Mass General for Children; the associate director of the Harvard Catalyst Translation and Clinical Research Center; and the director of the Pediatric Endocrine-Sports Endocrine-Neuroendocrine Lab, Mass General Hospital, Boston.
A version of this article first appeared on Medscape.com.
We have long recognized that our environment has a significant impact on our general health. Air pollution is known to contribute to respiratory conditions, poor cardiovascular outcomes, and certain kinds of cancer.
It’s increasingly important to identify factors that might contribute to suboptimal bone density and associated fracture risk in the population as a whole, and particularly in older adults. Aging is associated with a higher risk for osteoporosis and fractures, with their attendant morbidity, but individuals differ in their extent of bone loss and risk for fractures.
Known factors affecting bone health include genetics, age, sex, nutrition, physical activity, and hormonal factors. Certain medications, diseases, and lifestyle choices – such as smoking and alcohol intake – can also have deleterious effects on bone.
More recently, researchers have started examining the impact of air pollution on bone health.
As we know, the degree of pollution varies greatly from one region to another and can potentially significantly affect life in many parts of the world. In fact, the World Health Organization indicates that 99% of the world’s population breathes air exceeding the WHO guideline limits for pollutants.
Air pollutants include particulate matter (PM) as well as gases, such as nitric oxide, nitrogen dioxide, ammonia, carbon monoxide, sulfur dioxide, ozone, and certain volatile organic compounds. Particulate pollutants include a variety of substances produced from mostly human activities (such as vehicle emissions, biofuel combustion, mining, agriculture, and manufacturing, and also forest fires). They are classified not by their composition, but by their size (for example, PM1.0, PM2.5, and PM10 indicate PM with a diameter < 1.0, 2.5, and 10 microns, respectively). The finer the particle, the more likely it is to cross into the systemic circulation from the respiratory tract, with the potential to induce oxidative, inflammatory, and other changes in the body.
Many studies report that air pollution is a risk factor for osteoporosis. Some have found associations of lower bone density, osteoporosis, and fracture risk with higher concentrations of PM1.0, PM2.5, or PM10, even after controlling for other factors that could affect bone health. Some researchers have reported that although they didn’t find a significant association between PM and bone health, they did find an association between distance from the freeway and bone health – thus, exposure to polycyclic aromatic hydrocarbons and black carbon from vehicle emissions needs to be studied as a contributor to fracture risk.
Importantly, a prospective, observational study from the Women’s Health Initiative (which included more than 9,000 ethnically diverse women from three sites in the United States) reported a significant negative impact of PM10, nitric oxide, nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years on bone density at multiple sites, and particularly at the lumbar spine, in both cross-sectional and longitudinal analyses after controlling for demographic and socioeconomic factors. This study reported that nitrogen dioxide exposure may be a key determinant of bone density at the lumbar spine and in the whole body. Similarly, other studies have reported associations between atmospheric nitrogen dioxide or sulfur dioxide and risk for osteoporotic fractures.
Why the impact on bones?
The potential negative impact of pollution on bone has been attributed to many factors. PM induces systemic inflammation and an increase in cytokines that stimulate bone cells (osteoclasts) that cause bone loss. Other pollutants (gases and metal compounds) can cause oxidative damage to bone cells, whereas others act as endocrine disrupters and affect the functioning of these cells.
Pollution might also affect the synthesis and metabolism of vitamin D, which is necessary for absorption of calcium from the gut. High rates of pollution can reduce the amount of ultraviolet radiation reaching the earth which is important because certain wavelengths of ultraviolet radiation are necessary for vitamin D synthesis in our skin. Reduced vitamin D synthesis in skin can lead to poorly mineralized bone unless there is sufficient intake of vitamin D in diet or as supplements. Also, the conversion of vitamin D to its active form happens in the kidneys, and PM can be harmful to renal function. PM is also believed to cause increased breakdown of vitamin D into its inactive form.
Conversely, some studies have reported no association between pollution and bone density or osteoporosis risk, and two meta-analyses indicated that the association between the two is inconsistent. Some factors explaining variances in results include the number of individuals included in the study (larger studies are generally considered to be more reproducible), the fact that most studies are cross-sectional and not prospective, many do not control for other factors that might be deleterious to bone, and prediction models for the extent of PM or other exposure may not be completely accurate.
However, another recent meta-analysis reported an increased risk for lower total-body bone density and hip fracture after exposure to air pollution, particularly PM2.5 and nitrogen dioxide, but not to PM10, nitric oxide, or ozone. More studies are needed to confirm, or refute, the association between air pollution and impaired bone health. But accumulating evidence suggests that air pollution very likely has a deleterious effect on bone.
When feasible, it’s important to avoid living or working in areas with poor air quality and high pollution rates. However, this isn’t always possible based on one’s occupation, geography, circumstances, or economic status. Therefore, attention to a cleaner environment is critical at both the individual and the macro level.
As an example of the latter, the city of London extended its ultralow emission zone (ULEZ) farther out of the city in October 2021, and a further expansion is planned to include all of the city’s boroughs in August 2023.
We can do our bit by driving less and walking, biking, or using public transportation more often. We can also turn off the car engine when it’s not running, maintain our vehicles, switch to electric or hand-powered yard equipment, and not burn household garbage and limit backyard fires. We can also switch from gas to solar energy or wind, use efficient appliances and heating, and avoid unnecessary energy use. And we can choose sustainable products when possible.
For optimal bone health, we should remind patients to eat a healthy diet with the requisite amount of protein, calcium, and vitamin D. Vitamin D and calcium supplementation may be necessary for people whose intake of dairy and dairy products is low. Other important strategies to optimize bone health include engaging in healthy physical activity; avoiding smoking or excessive alcohol intake; and treating underlying gastrointestinal, endocrine, or other conditions that can reduce bone density.
Madhusmita Misra, MD, MPH, is the chief of the division of pediatric endocrinology, Mass General for Children; the associate director of the Harvard Catalyst Translation and Clinical Research Center; and the director of the Pediatric Endocrine-Sports Endocrine-Neuroendocrine Lab, Mass General Hospital, Boston.
A version of this article first appeared on Medscape.com.
We have long recognized that our environment has a significant impact on our general health. Air pollution is known to contribute to respiratory conditions, poor cardiovascular outcomes, and certain kinds of cancer.
It’s increasingly important to identify factors that might contribute to suboptimal bone density and associated fracture risk in the population as a whole, and particularly in older adults. Aging is associated with a higher risk for osteoporosis and fractures, with their attendant morbidity, but individuals differ in their extent of bone loss and risk for fractures.
Known factors affecting bone health include genetics, age, sex, nutrition, physical activity, and hormonal factors. Certain medications, diseases, and lifestyle choices – such as smoking and alcohol intake – can also have deleterious effects on bone.
More recently, researchers have started examining the impact of air pollution on bone health.
As we know, the degree of pollution varies greatly from one region to another and can potentially significantly affect life in many parts of the world. In fact, the World Health Organization indicates that 99% of the world’s population breathes air exceeding the WHO guideline limits for pollutants.
Air pollutants include particulate matter (PM) as well as gases, such as nitric oxide, nitrogen dioxide, ammonia, carbon monoxide, sulfur dioxide, ozone, and certain volatile organic compounds. Particulate pollutants include a variety of substances produced from mostly human activities (such as vehicle emissions, biofuel combustion, mining, agriculture, and manufacturing, and also forest fires). They are classified not by their composition, but by their size (for example, PM1.0, PM2.5, and PM10 indicate PM with a diameter < 1.0, 2.5, and 10 microns, respectively). The finer the particle, the more likely it is to cross into the systemic circulation from the respiratory tract, with the potential to induce oxidative, inflammatory, and other changes in the body.
Many studies report that air pollution is a risk factor for osteoporosis. Some have found associations of lower bone density, osteoporosis, and fracture risk with higher concentrations of PM1.0, PM2.5, or PM10, even after controlling for other factors that could affect bone health. Some researchers have reported that although they didn’t find a significant association between PM and bone health, they did find an association between distance from the freeway and bone health – thus, exposure to polycyclic aromatic hydrocarbons and black carbon from vehicle emissions needs to be studied as a contributor to fracture risk.
Importantly, a prospective, observational study from the Women’s Health Initiative (which included more than 9,000 ethnically diverse women from three sites in the United States) reported a significant negative impact of PM10, nitric oxide, nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years on bone density at multiple sites, and particularly at the lumbar spine, in both cross-sectional and longitudinal analyses after controlling for demographic and socioeconomic factors. This study reported that nitrogen dioxide exposure may be a key determinant of bone density at the lumbar spine and in the whole body. Similarly, other studies have reported associations between atmospheric nitrogen dioxide or sulfur dioxide and risk for osteoporotic fractures.
Why the impact on bones?
The potential negative impact of pollution on bone has been attributed to many factors. PM induces systemic inflammation and an increase in cytokines that stimulate bone cells (osteoclasts) that cause bone loss. Other pollutants (gases and metal compounds) can cause oxidative damage to bone cells, whereas others act as endocrine disrupters and affect the functioning of these cells.
Pollution might also affect the synthesis and metabolism of vitamin D, which is necessary for absorption of calcium from the gut. High rates of pollution can reduce the amount of ultraviolet radiation reaching the earth which is important because certain wavelengths of ultraviolet radiation are necessary for vitamin D synthesis in our skin. Reduced vitamin D synthesis in skin can lead to poorly mineralized bone unless there is sufficient intake of vitamin D in diet or as supplements. Also, the conversion of vitamin D to its active form happens in the kidneys, and PM can be harmful to renal function. PM is also believed to cause increased breakdown of vitamin D into its inactive form.
Conversely, some studies have reported no association between pollution and bone density or osteoporosis risk, and two meta-analyses indicated that the association between the two is inconsistent. Some factors explaining variances in results include the number of individuals included in the study (larger studies are generally considered to be more reproducible), the fact that most studies are cross-sectional and not prospective, many do not control for other factors that might be deleterious to bone, and prediction models for the extent of PM or other exposure may not be completely accurate.
However, another recent meta-analysis reported an increased risk for lower total-body bone density and hip fracture after exposure to air pollution, particularly PM2.5 and nitrogen dioxide, but not to PM10, nitric oxide, or ozone. More studies are needed to confirm, or refute, the association between air pollution and impaired bone health. But accumulating evidence suggests that air pollution very likely has a deleterious effect on bone.
When feasible, it’s important to avoid living or working in areas with poor air quality and high pollution rates. However, this isn’t always possible based on one’s occupation, geography, circumstances, or economic status. Therefore, attention to a cleaner environment is critical at both the individual and the macro level.
As an example of the latter, the city of London extended its ultralow emission zone (ULEZ) farther out of the city in October 2021, and a further expansion is planned to include all of the city’s boroughs in August 2023.
We can do our bit by driving less and walking, biking, or using public transportation more often. We can also turn off the car engine when it’s not running, maintain our vehicles, switch to electric or hand-powered yard equipment, and not burn household garbage and limit backyard fires. We can also switch from gas to solar energy or wind, use efficient appliances and heating, and avoid unnecessary energy use. And we can choose sustainable products when possible.
For optimal bone health, we should remind patients to eat a healthy diet with the requisite amount of protein, calcium, and vitamin D. Vitamin D and calcium supplementation may be necessary for people whose intake of dairy and dairy products is low. Other important strategies to optimize bone health include engaging in healthy physical activity; avoiding smoking or excessive alcohol intake; and treating underlying gastrointestinal, endocrine, or other conditions that can reduce bone density.
Madhusmita Misra, MD, MPH, is the chief of the division of pediatric endocrinology, Mass General for Children; the associate director of the Harvard Catalyst Translation and Clinical Research Center; and the director of the Pediatric Endocrine-Sports Endocrine-Neuroendocrine Lab, Mass General Hospital, Boston.
A version of this article first appeared on Medscape.com.
What are the healthiest drinks for patients with type 2 diabetes?
The researchers examined data on almost 15,500 participants with type 2 diabetes from two major studies, finding that the highest level of consumption of SSBs was associated with a 20% increased risk of all-cause mortality and a 25% raised risk of cardiovascular disease, compared with consumption of the least amounts of these products.
The research, published in BMJ, also showed that drinking coffee, tea, plain water, and low-fat milk reduced the risk of all-cause death and that switching from SSBs to the other beverages was linked to lower mortality.
“Overall, these results provide additional evidence that emphasizes the importance of beverage choices in maintaining overall health among adults with diabetes,” say senior author Le Ma, PhD, department of nutrition, Harvard School of Public Health, Boston, and colleagues.
“Collectively, these findings all point in the same direction. Lower consumption of SSBs and higher consumption of coffee, tea, plain water, or low-fat milk are optimal for better health outcomes in adults with type 2 diabetes,” Nita G. Forouhi, MD, PhD, emphasizes in an accompanying editorial.
Choice of drink matters
Dr. Forouhi, from the University of Cambridge (England), warned, however, that the findings “cannot be considered cause and effect,” despite the large-scale analysis.
Moreover, “questions remain,” such as the impact of beverage consumption on coronary heart disease and stroke risk, and cancer mortality, with the current study providing “inconclusive” data on the latter.
There was also no data on the addition of sugar to tea or coffee, “so the comparative health effects of unsweetened and sweetened hot beverages remain unclear,” Dr. Forouhi points out. Also unknown is whether the type of tea consumed has a differential effect.
Despite these and other reservations, she says that overall, “Choice of beverage clearly matters.”
“The case for avoiding sugar-sweetened beverages is compelling, and it is supported by various fiscal measures in more than 45 countries. It is reasonable to shift the focus to drinks that are most likely to have positive health impacts: coffee, tea, plain water, and low-fat milk,” she notes.
Dr. Forouhi ends by underlining that the current findings tally with those seen in the general population, so “one important message is that having diabetes does not have to be especially restrictive.”
Expanding the evidence
It was estimated that 537 million adults worldwide had type 2 diabetes in 2021, a figure set to increase to 783 million by 2045, say the authors.
Individuals with type 2 diabetes have an increased risk of cardiovascular disease, among many other comorbidities, as well as premature death. Dietary interventions can play an important role in managing these risks.
Recommendations on the healthiest beverages to drink are largely based on evidence from the general population, and data are limited on the best options for adults with type 2 diabetes, who have altered metabolism, the researchers note.
To expand on this, they examined data from the Nurses’ Health Study, which enrolled female registered nurses aged 30-55 years and was initiated in 1976, and the Health Professionals Follow-Up Study, which included male health professionals aged 40-75 years and was initiated in 1996.
For the current analysis, 11,399 women and 4,087 men with type 2 diabetes were included from the two studies, of whom 2,715 were diagnosed before study entry.
Participants’ average daily beverage intake was assessed using a validated food frequency questionnaire administered every 2-4 years. SSBs included caffeinated and caffeine-free colas, other carbonated SSBs, and noncarbonated SSBs, such as fruit punches, lemonades, or other fruit drinks.
During 285,967 person-years of follow-up, there were 7,638 (49.3%) deaths, and 3,447 (22.3%) cases of incident cardiovascular disease were documented during 248,447 person-years of follow-up.
Fully adjusted multivariate analysis comparing the lowest and highest beverage intake indicated that SSBs were associated with a significant increase in all-cause mortality, at a pooled hazard ratio of 1.20, or 1.08 for each additional serving per day (P = .01).
In contrast, the associations between all-cause mortality and consumption of artificially sweetened beverages, fruit juice, and full-fat milk were not significant, whereas coffee (HR, 0.74), tea (HR, 0.79), plain water (HR, 0.77), and low-fat milk (HR, 0.88) were linked to a reduced risk.
The team reported that there were similar associations between beverage intake and cardiovascular disease incidence, at an HR of 1.25 for SSBs, as well as for cardiovascular disease mortality, at an HR of 1.29.
Participants who increased their tea, coffee, and low-fat milk consumption during the course of the study had lower all-cause mortality than those who did not. Switching from SSBs to other beverages was also associated with lower mortality.
The researchers note, however, that there are “several potential limitations” to their study, including that “individual beverage consumption may be correlated with other dietary and lifestyle risk factors for cardiovascular disease incidence and mortality among adults with [type 2] diabetes.”
The study was sponsored by the National Institutes of Health. Dr. Ma has reported no relevant financial relationships. Disclosures for the other authors are listed with the article. Dr. Forouhi has declared receiving support from the U.K. Medical Research Council Epidemiology Unit and U.K. National Institute for Health and Care Research Biomedical Research Centre Cambridge.
A version of this article first appeared on Medscape.com.
The researchers examined data on almost 15,500 participants with type 2 diabetes from two major studies, finding that the highest level of consumption of SSBs was associated with a 20% increased risk of all-cause mortality and a 25% raised risk of cardiovascular disease, compared with consumption of the least amounts of these products.
The research, published in BMJ, also showed that drinking coffee, tea, plain water, and low-fat milk reduced the risk of all-cause death and that switching from SSBs to the other beverages was linked to lower mortality.
“Overall, these results provide additional evidence that emphasizes the importance of beverage choices in maintaining overall health among adults with diabetes,” say senior author Le Ma, PhD, department of nutrition, Harvard School of Public Health, Boston, and colleagues.
“Collectively, these findings all point in the same direction. Lower consumption of SSBs and higher consumption of coffee, tea, plain water, or low-fat milk are optimal for better health outcomes in adults with type 2 diabetes,” Nita G. Forouhi, MD, PhD, emphasizes in an accompanying editorial.
Choice of drink matters
Dr. Forouhi, from the University of Cambridge (England), warned, however, that the findings “cannot be considered cause and effect,” despite the large-scale analysis.
Moreover, “questions remain,” such as the impact of beverage consumption on coronary heart disease and stroke risk, and cancer mortality, with the current study providing “inconclusive” data on the latter.
There was also no data on the addition of sugar to tea or coffee, “so the comparative health effects of unsweetened and sweetened hot beverages remain unclear,” Dr. Forouhi points out. Also unknown is whether the type of tea consumed has a differential effect.
Despite these and other reservations, she says that overall, “Choice of beverage clearly matters.”
“The case for avoiding sugar-sweetened beverages is compelling, and it is supported by various fiscal measures in more than 45 countries. It is reasonable to shift the focus to drinks that are most likely to have positive health impacts: coffee, tea, plain water, and low-fat milk,” she notes.
Dr. Forouhi ends by underlining that the current findings tally with those seen in the general population, so “one important message is that having diabetes does not have to be especially restrictive.”
Expanding the evidence
It was estimated that 537 million adults worldwide had type 2 diabetes in 2021, a figure set to increase to 783 million by 2045, say the authors.
Individuals with type 2 diabetes have an increased risk of cardiovascular disease, among many other comorbidities, as well as premature death. Dietary interventions can play an important role in managing these risks.
Recommendations on the healthiest beverages to drink are largely based on evidence from the general population, and data are limited on the best options for adults with type 2 diabetes, who have altered metabolism, the researchers note.
To expand on this, they examined data from the Nurses’ Health Study, which enrolled female registered nurses aged 30-55 years and was initiated in 1976, and the Health Professionals Follow-Up Study, which included male health professionals aged 40-75 years and was initiated in 1996.
For the current analysis, 11,399 women and 4,087 men with type 2 diabetes were included from the two studies, of whom 2,715 were diagnosed before study entry.
Participants’ average daily beverage intake was assessed using a validated food frequency questionnaire administered every 2-4 years. SSBs included caffeinated and caffeine-free colas, other carbonated SSBs, and noncarbonated SSBs, such as fruit punches, lemonades, or other fruit drinks.
During 285,967 person-years of follow-up, there were 7,638 (49.3%) deaths, and 3,447 (22.3%) cases of incident cardiovascular disease were documented during 248,447 person-years of follow-up.
Fully adjusted multivariate analysis comparing the lowest and highest beverage intake indicated that SSBs were associated with a significant increase in all-cause mortality, at a pooled hazard ratio of 1.20, or 1.08 for each additional serving per day (P = .01).
In contrast, the associations between all-cause mortality and consumption of artificially sweetened beverages, fruit juice, and full-fat milk were not significant, whereas coffee (HR, 0.74), tea (HR, 0.79), plain water (HR, 0.77), and low-fat milk (HR, 0.88) were linked to a reduced risk.
The team reported that there were similar associations between beverage intake and cardiovascular disease incidence, at an HR of 1.25 for SSBs, as well as for cardiovascular disease mortality, at an HR of 1.29.
Participants who increased their tea, coffee, and low-fat milk consumption during the course of the study had lower all-cause mortality than those who did not. Switching from SSBs to other beverages was also associated with lower mortality.
The researchers note, however, that there are “several potential limitations” to their study, including that “individual beverage consumption may be correlated with other dietary and lifestyle risk factors for cardiovascular disease incidence and mortality among adults with [type 2] diabetes.”
The study was sponsored by the National Institutes of Health. Dr. Ma has reported no relevant financial relationships. Disclosures for the other authors are listed with the article. Dr. Forouhi has declared receiving support from the U.K. Medical Research Council Epidemiology Unit and U.K. National Institute for Health and Care Research Biomedical Research Centre Cambridge.
A version of this article first appeared on Medscape.com.
The researchers examined data on almost 15,500 participants with type 2 diabetes from two major studies, finding that the highest level of consumption of SSBs was associated with a 20% increased risk of all-cause mortality and a 25% raised risk of cardiovascular disease, compared with consumption of the least amounts of these products.
The research, published in BMJ, also showed that drinking coffee, tea, plain water, and low-fat milk reduced the risk of all-cause death and that switching from SSBs to the other beverages was linked to lower mortality.
“Overall, these results provide additional evidence that emphasizes the importance of beverage choices in maintaining overall health among adults with diabetes,” say senior author Le Ma, PhD, department of nutrition, Harvard School of Public Health, Boston, and colleagues.
“Collectively, these findings all point in the same direction. Lower consumption of SSBs and higher consumption of coffee, tea, plain water, or low-fat milk are optimal for better health outcomes in adults with type 2 diabetes,” Nita G. Forouhi, MD, PhD, emphasizes in an accompanying editorial.
Choice of drink matters
Dr. Forouhi, from the University of Cambridge (England), warned, however, that the findings “cannot be considered cause and effect,” despite the large-scale analysis.
Moreover, “questions remain,” such as the impact of beverage consumption on coronary heart disease and stroke risk, and cancer mortality, with the current study providing “inconclusive” data on the latter.
There was also no data on the addition of sugar to tea or coffee, “so the comparative health effects of unsweetened and sweetened hot beverages remain unclear,” Dr. Forouhi points out. Also unknown is whether the type of tea consumed has a differential effect.
Despite these and other reservations, she says that overall, “Choice of beverage clearly matters.”
“The case for avoiding sugar-sweetened beverages is compelling, and it is supported by various fiscal measures in more than 45 countries. It is reasonable to shift the focus to drinks that are most likely to have positive health impacts: coffee, tea, plain water, and low-fat milk,” she notes.
Dr. Forouhi ends by underlining that the current findings tally with those seen in the general population, so “one important message is that having diabetes does not have to be especially restrictive.”
Expanding the evidence
It was estimated that 537 million adults worldwide had type 2 diabetes in 2021, a figure set to increase to 783 million by 2045, say the authors.
Individuals with type 2 diabetes have an increased risk of cardiovascular disease, among many other comorbidities, as well as premature death. Dietary interventions can play an important role in managing these risks.
Recommendations on the healthiest beverages to drink are largely based on evidence from the general population, and data are limited on the best options for adults with type 2 diabetes, who have altered metabolism, the researchers note.
To expand on this, they examined data from the Nurses’ Health Study, which enrolled female registered nurses aged 30-55 years and was initiated in 1976, and the Health Professionals Follow-Up Study, which included male health professionals aged 40-75 years and was initiated in 1996.
For the current analysis, 11,399 women and 4,087 men with type 2 diabetes were included from the two studies, of whom 2,715 were diagnosed before study entry.
Participants’ average daily beverage intake was assessed using a validated food frequency questionnaire administered every 2-4 years. SSBs included caffeinated and caffeine-free colas, other carbonated SSBs, and noncarbonated SSBs, such as fruit punches, lemonades, or other fruit drinks.
During 285,967 person-years of follow-up, there were 7,638 (49.3%) deaths, and 3,447 (22.3%) cases of incident cardiovascular disease were documented during 248,447 person-years of follow-up.
Fully adjusted multivariate analysis comparing the lowest and highest beverage intake indicated that SSBs were associated with a significant increase in all-cause mortality, at a pooled hazard ratio of 1.20, or 1.08 for each additional serving per day (P = .01).
In contrast, the associations between all-cause mortality and consumption of artificially sweetened beverages, fruit juice, and full-fat milk were not significant, whereas coffee (HR, 0.74), tea (HR, 0.79), plain water (HR, 0.77), and low-fat milk (HR, 0.88) were linked to a reduced risk.
The team reported that there were similar associations between beverage intake and cardiovascular disease incidence, at an HR of 1.25 for SSBs, as well as for cardiovascular disease mortality, at an HR of 1.29.
Participants who increased their tea, coffee, and low-fat milk consumption during the course of the study had lower all-cause mortality than those who did not. Switching from SSBs to other beverages was also associated with lower mortality.
The researchers note, however, that there are “several potential limitations” to their study, including that “individual beverage consumption may be correlated with other dietary and lifestyle risk factors for cardiovascular disease incidence and mortality among adults with [type 2] diabetes.”
The study was sponsored by the National Institutes of Health. Dr. Ma has reported no relevant financial relationships. Disclosures for the other authors are listed with the article. Dr. Forouhi has declared receiving support from the U.K. Medical Research Council Epidemiology Unit and U.K. National Institute for Health and Care Research Biomedical Research Centre Cambridge.
A version of this article first appeared on Medscape.com.
FROM THE BMJ
Infographic: Is your compensation rising as fast as your peers?
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.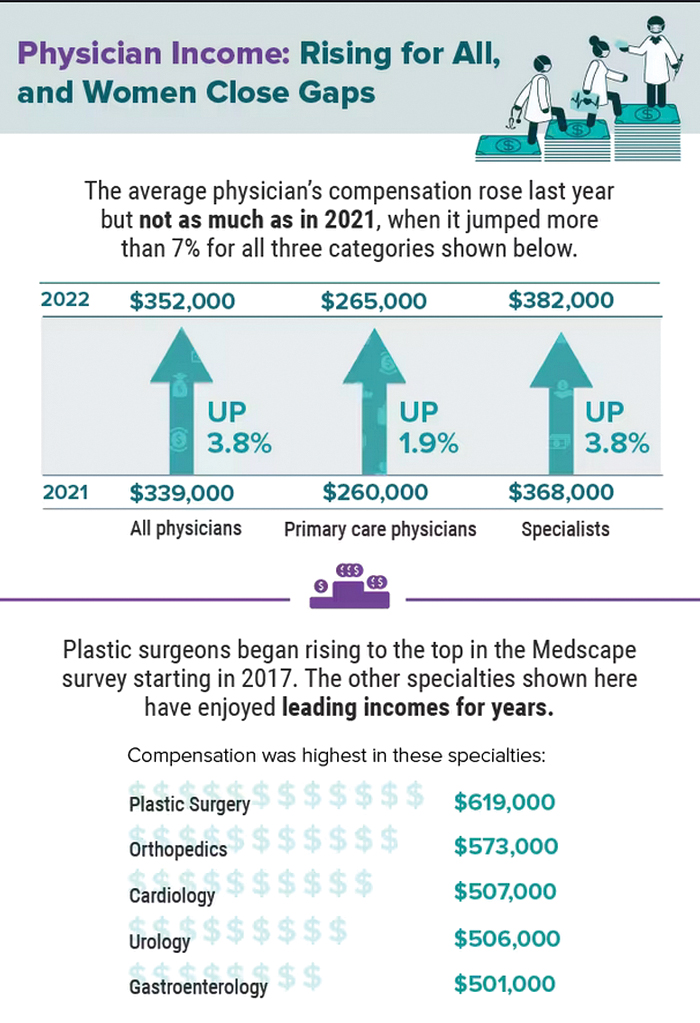
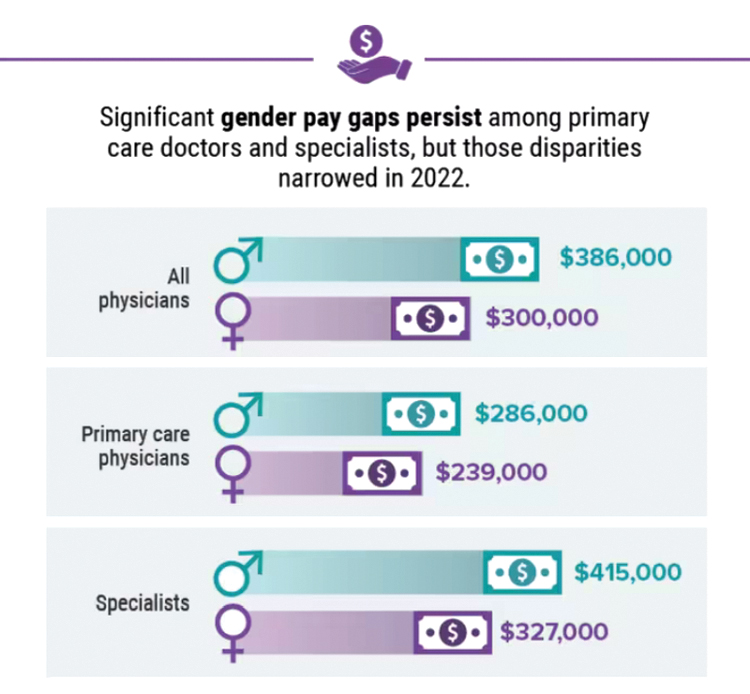
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.
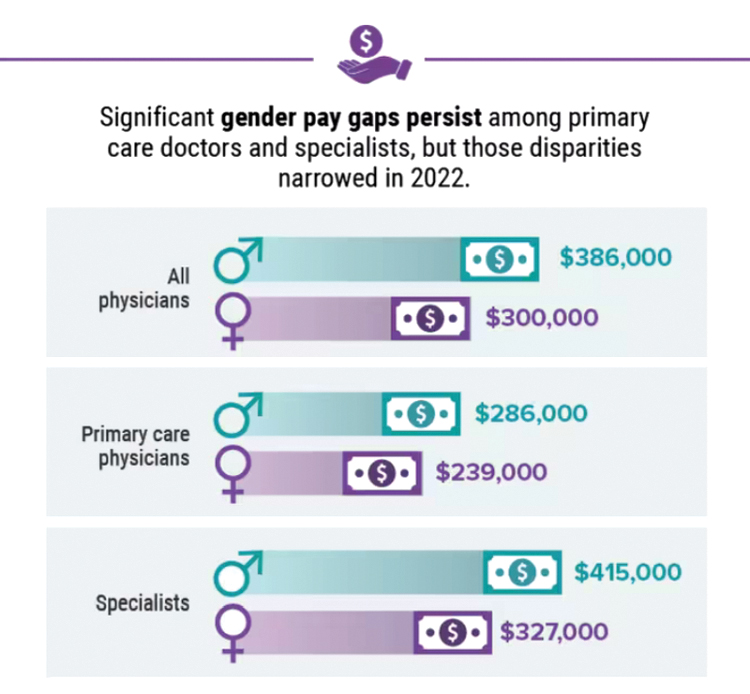
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.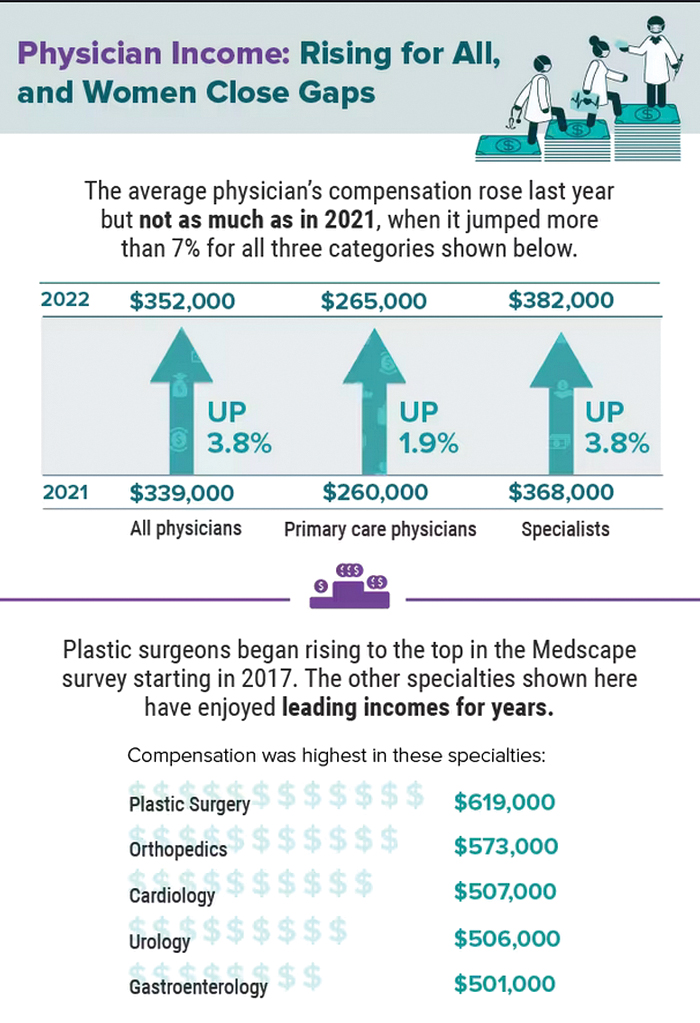
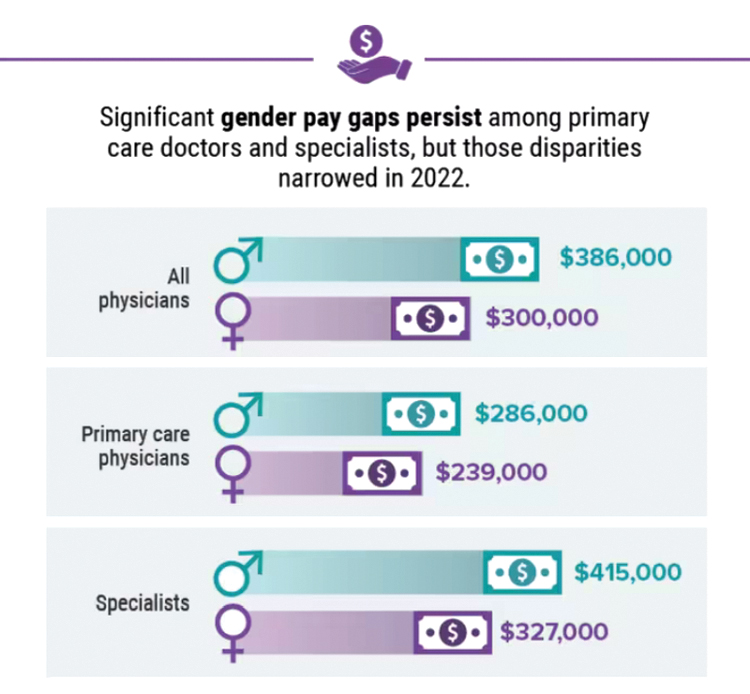
A version of this article first appeared on Medscape.com.
Five chronic mistakes that can sabotage your medical practice
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
Living the introvert’s dream: Alone for 500 days, but never lonely
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Green Mediterranean diet may relieve aortic stiffness
A green adaptation to the traditional Mediterranean diet improves proximal aortic stiffness (PAS), a distinct marker of vascular aging and increased cardiovascular risk, according to an exploratory post hoc analysis of the DIRECT-PLUS randomized clinical trial.
The green Mediterranean diet is distinct from the traditional Mediterranean diet because of its more abundant dietary polyphenols, from green tea and a Wolffia globosa (Mankai) plant green shake, and lower intake of red or processed meat.
Independent of weight loss, the modified green Mediterranean diet regressed PAS by 15%, the traditional Mediterranean diet by 7.3%, and the healthy dietary guideline–based diet by 4.8%, the study team observed.
“The DIRECT-PLUS trial research team was the first to introduce the concept of the green-Mediterranean/high polyphenols diet,” lead researcher Iris Shai, RD, PhD, with Ben-Gurion University of the Negev, Be’er-Sheva, Israel, told this news organization.
This diet promoted “dramatic proximal aortic de-stiffening” as assessed by MRI over 18 months in roughly 300 participants with abdominal obesity/dyslipidemia. “To date, no dietary strategies have been shown to impact vascular aging physiology,” Dr. Shai said.
The analysis was published online in the Journal of the American College of Cardiology.
Not all healthy diets are equal
Of the 294 participants, 281 had valid PAS measurements at baseline. The baseline PAS (6.1 m/s) was similar across intervention groups (P = .20). Increased PAS was associated with aging, hypertension, dyslipidemia, diabetes, and visceral adiposity (P < .05).
After 18 months’ intervention (retention rate 89.8%), all diet groups showed significant PAS reductions: –0.05 m/s with the standard healthy diet (4.8%), –0.08 m/s with the traditional Mediterranean diet (7.3%) and –0.15 the green Mediterranean diet (15%).
In the multivariable model, the green Mediterranean dieters had greater PAS reduction than did the healthy-diet and Mediterranean dieters (P = .003 and P = .032, respectively).
The researchers caution that DIRECT-PLUS had multiple endpoints and this exploratory post hoc analysis might be sensitive to type I statistical error and should be considered “hypothesis-generating.”
High-quality study, believable results
Reached for comment on the study, Deepak L. Bhatt, MD, MPH, director of Mount Sinai Heart in New York, said, “There is not a lot of high-quality research on diet, and I would call this high-quality research in as much as they used randomization which most dietary studies don’t do.
“The greener Mediterranean diet seemed to be the best one on the surrogate marker of MRI-defined aortic stiffness,” Dr. Bhatt, professor of cardiovascular medicine, Icahn School of Medicine at Mount Sinai, who wasn’t involved in the study, told this news organization.
“It makes sense that a diet that has more green in it, more polyphenols, would be healthier. This has been shown in some other studies, that these plant-based polyphenols might have various cardiovascular protective aspects to them,” Dr. Bhatt said.
Overall, he said the results are “quite believable, with the caveat that it would be nice to see the results reproduced in a more diverse and larger sample.”
“There is emerging evidence that diets that are higher in fresh fruits and vegetables and whole grains and lower in overall caloric intake, in general, seem to be good diets to reduce cardiovascular risk factors and maybe even reduce actual cardiovascular risk,” Dr. Bhatt added.
The study was funded by grants from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation), the Rosetrees Trust, Israel Ministry of Health, Israel Ministry of Science and Technology, and the California Walnuts Commission. Dr. Shai and Dr. Bhatt have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A green adaptation to the traditional Mediterranean diet improves proximal aortic stiffness (PAS), a distinct marker of vascular aging and increased cardiovascular risk, according to an exploratory post hoc analysis of the DIRECT-PLUS randomized clinical trial.
The green Mediterranean diet is distinct from the traditional Mediterranean diet because of its more abundant dietary polyphenols, from green tea and a Wolffia globosa (Mankai) plant green shake, and lower intake of red or processed meat.
Independent of weight loss, the modified green Mediterranean diet regressed PAS by 15%, the traditional Mediterranean diet by 7.3%, and the healthy dietary guideline–based diet by 4.8%, the study team observed.
“The DIRECT-PLUS trial research team was the first to introduce the concept of the green-Mediterranean/high polyphenols diet,” lead researcher Iris Shai, RD, PhD, with Ben-Gurion University of the Negev, Be’er-Sheva, Israel, told this news organization.
This diet promoted “dramatic proximal aortic de-stiffening” as assessed by MRI over 18 months in roughly 300 participants with abdominal obesity/dyslipidemia. “To date, no dietary strategies have been shown to impact vascular aging physiology,” Dr. Shai said.
The analysis was published online in the Journal of the American College of Cardiology.
Not all healthy diets are equal
Of the 294 participants, 281 had valid PAS measurements at baseline. The baseline PAS (6.1 m/s) was similar across intervention groups (P = .20). Increased PAS was associated with aging, hypertension, dyslipidemia, diabetes, and visceral adiposity (P < .05).
After 18 months’ intervention (retention rate 89.8%), all diet groups showed significant PAS reductions: –0.05 m/s with the standard healthy diet (4.8%), –0.08 m/s with the traditional Mediterranean diet (7.3%) and –0.15 the green Mediterranean diet (15%).
In the multivariable model, the green Mediterranean dieters had greater PAS reduction than did the healthy-diet and Mediterranean dieters (P = .003 and P = .032, respectively).
The researchers caution that DIRECT-PLUS had multiple endpoints and this exploratory post hoc analysis might be sensitive to type I statistical error and should be considered “hypothesis-generating.”
High-quality study, believable results
Reached for comment on the study, Deepak L. Bhatt, MD, MPH, director of Mount Sinai Heart in New York, said, “There is not a lot of high-quality research on diet, and I would call this high-quality research in as much as they used randomization which most dietary studies don’t do.
“The greener Mediterranean diet seemed to be the best one on the surrogate marker of MRI-defined aortic stiffness,” Dr. Bhatt, professor of cardiovascular medicine, Icahn School of Medicine at Mount Sinai, who wasn’t involved in the study, told this news organization.
“It makes sense that a diet that has more green in it, more polyphenols, would be healthier. This has been shown in some other studies, that these plant-based polyphenols might have various cardiovascular protective aspects to them,” Dr. Bhatt said.
Overall, he said the results are “quite believable, with the caveat that it would be nice to see the results reproduced in a more diverse and larger sample.”
“There is emerging evidence that diets that are higher in fresh fruits and vegetables and whole grains and lower in overall caloric intake, in general, seem to be good diets to reduce cardiovascular risk factors and maybe even reduce actual cardiovascular risk,” Dr. Bhatt added.
The study was funded by grants from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation), the Rosetrees Trust, Israel Ministry of Health, Israel Ministry of Science and Technology, and the California Walnuts Commission. Dr. Shai and Dr. Bhatt have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A green adaptation to the traditional Mediterranean diet improves proximal aortic stiffness (PAS), a distinct marker of vascular aging and increased cardiovascular risk, according to an exploratory post hoc analysis of the DIRECT-PLUS randomized clinical trial.
The green Mediterranean diet is distinct from the traditional Mediterranean diet because of its more abundant dietary polyphenols, from green tea and a Wolffia globosa (Mankai) plant green shake, and lower intake of red or processed meat.
Independent of weight loss, the modified green Mediterranean diet regressed PAS by 15%, the traditional Mediterranean diet by 7.3%, and the healthy dietary guideline–based diet by 4.8%, the study team observed.
“The DIRECT-PLUS trial research team was the first to introduce the concept of the green-Mediterranean/high polyphenols diet,” lead researcher Iris Shai, RD, PhD, with Ben-Gurion University of the Negev, Be’er-Sheva, Israel, told this news organization.
This diet promoted “dramatic proximal aortic de-stiffening” as assessed by MRI over 18 months in roughly 300 participants with abdominal obesity/dyslipidemia. “To date, no dietary strategies have been shown to impact vascular aging physiology,” Dr. Shai said.
The analysis was published online in the Journal of the American College of Cardiology.
Not all healthy diets are equal
Of the 294 participants, 281 had valid PAS measurements at baseline. The baseline PAS (6.1 m/s) was similar across intervention groups (P = .20). Increased PAS was associated with aging, hypertension, dyslipidemia, diabetes, and visceral adiposity (P < .05).
After 18 months’ intervention (retention rate 89.8%), all diet groups showed significant PAS reductions: –0.05 m/s with the standard healthy diet (4.8%), –0.08 m/s with the traditional Mediterranean diet (7.3%) and –0.15 the green Mediterranean diet (15%).
In the multivariable model, the green Mediterranean dieters had greater PAS reduction than did the healthy-diet and Mediterranean dieters (P = .003 and P = .032, respectively).
The researchers caution that DIRECT-PLUS had multiple endpoints and this exploratory post hoc analysis might be sensitive to type I statistical error and should be considered “hypothesis-generating.”
High-quality study, believable results
Reached for comment on the study, Deepak L. Bhatt, MD, MPH, director of Mount Sinai Heart in New York, said, “There is not a lot of high-quality research on diet, and I would call this high-quality research in as much as they used randomization which most dietary studies don’t do.
“The greener Mediterranean diet seemed to be the best one on the surrogate marker of MRI-defined aortic stiffness,” Dr. Bhatt, professor of cardiovascular medicine, Icahn School of Medicine at Mount Sinai, who wasn’t involved in the study, told this news organization.
“It makes sense that a diet that has more green in it, more polyphenols, would be healthier. This has been shown in some other studies, that these plant-based polyphenols might have various cardiovascular protective aspects to them,” Dr. Bhatt said.
Overall, he said the results are “quite believable, with the caveat that it would be nice to see the results reproduced in a more diverse and larger sample.”
“There is emerging evidence that diets that are higher in fresh fruits and vegetables and whole grains and lower in overall caloric intake, in general, seem to be good diets to reduce cardiovascular risk factors and maybe even reduce actual cardiovascular risk,” Dr. Bhatt added.
The study was funded by grants from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation), the Rosetrees Trust, Israel Ministry of Health, Israel Ministry of Science and Technology, and the California Walnuts Commission. Dr. Shai and Dr. Bhatt have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Optimal time period for weight loss drugs: Debate continues
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
Physicians may retire en masse soon. What does that mean for medicine?
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
Physician compensation continues to climb amid postpandemic change
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.