User login
Can serum inflammatory markers predict concussion recovery?
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
FROM NEUROLOGY
Key clinical point: Serum biomarkers of inflammation may help identify which athletes will take longer to recover after a sport-related concussion.
Major finding: IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration.
Study details: A prospective cohort study of high school and college football players. The analyses included 41 concussed athletes and 43 matched control athletes with an average age of about 18 years.
Disclosures: The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
Source: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
Patients with focal epilepsy have progressive cortical thinning
, according to research published online July 1 in JAMA Neurology. Methods for preventing this thinning are unknown. “Our findings appear to highlight the need for longitudinal studies to develop disease-modifying treatments for epilepsy,” said Marian Galovic, MD, a doctoral student at University College London, and colleagues.
To date, neurologists have not found a definitive answer to the question of whether epilepsy is a static or progressive disease. Few longitudinal studies have examined patients with structural neuroimaging to determine whether the brain changes over time. The studies that have taken this approach have had small populations or have lacked control populations.
Comparing brain changes in patients and controls
Dr. Galovic and colleagues analyzed data for consecutive patients with focal epilepsy who underwent follow-up at the National Hospital for Neurology and Neurosurgery in London. The data were collected from Aug. 3, 2004, to Jan. 26, 2016. The researchers chose individuals who had at least 2 high-resolution T1-weighted MRI scans performed on the same scanner more than 6 months apart. They excluded patients with brain lesions other than hippocampal sclerosis, those with inadequate MRI scan quality, and those for whom clinical data were missing. To match these patients with controls, Dr. Galovic and colleagues chose three longitudinal data sets with data for healthy volunteers between ages 20 and 70 years. Each control participant had two high-resolution T1-weighted scans taken more than 6 months apart. The investigators matched patients and controls on age and sex. The automated and validated Computational Anatomy Toolbox (CAT12) estimated cortical thickness.
Dr. Galovic’s group included 190 patients with focal epilepsy, who had had 396 MRI scans, and 141 healthy controls, who had had 282 MRI scans, in their analysis. Age, sex, and image quality did not differ significantly between the two groups. Mean age was 36 years for patients and 35 years for controls. The proportion of women was 52.1% among patients and 53.9% among controls.
The rate of atrophy was doubled in patients
Approximately 77% of people with epilepsy had progressive cortical thinning that was distinct from that associated with normal aging. The mean overall annual rate of global cortical thinning was higher among patients with epilepsy (0.024) than among controls (0.011). The mean annual rate of cortical thinning increased among people with epilepsy who were older than 55 years. This rate was 0.021 in patients aged 18 to less than 35 years, compared with 0.023 in patients aged 35 to less than 55 years. Seizure frequency, number of antiepileptic drugs (AEDs) taken, and history of secondarily generalized seizures did not differ between age groups.
Compared with healthy controls, patients with focal epilepsy had widespread areas of greater progressive atrophy. Bilaterally affected areas included the lateral and posterior temporal lobes, posterior cingulate gyri, occipital lobes, pericentral gyri, and opercula. The distribution of progressive thinning in all patients with epilepsy was similar to regions connected to both hippocampi. Healthy controls had no areas of greater cortical thinning, compared with patients with epilepsy.
Progressive thinning in the left postcentral gyrus was greater in patients with left temporal lobe epilepsy (TLE) than in those with right TLE. Cortical thinning was more progressive in patients with right frontal lobe epilepsy (FLE) than in those with left FLE, particularly in right parietotemporal and right frontal areas.
Dr. Galovic and colleagues found no association between the rate of cortical thinning and seizure frequency, history of secondarily generalized seizures, or number of AEDs taken between MRIs. They found no difference in the rate of atrophy between patients with epilepsy with ongoing seizures and those without. The annual mean rate of cortical thinning was higher in people with a short duration of epilepsy (i.e., less than 5 years), compared with patients with a longer duration of epilepsy (i.e., 5 years or more).
A surrogate marker for neurodegeneration?
“The most likely cause of cortical thinning is neuronal loss, suggesting that these measurements are a surrogate marker for neurodegeneration,” said Dr. Galovic and colleagues. The finding that progressive morphologic changes were most pronounced in the first 5 years after epilepsy onset “supports the need for early diagnosis, rapid treatment, and reduction of delays of surgical referral in people with epilepsy,” they added.
One limitation of the current study is the fact that data from patients and controls were acquired using different MRI scanners. In addition, the patients included in the study had been referred to the center because their cases were more complicated, thus introducing the possibility of referral bias. The findings thus cannot be generalized readily to the overall population, said Dr. Galovic and colleagues.
Future studies should examine whether particular AEDs have differential influences on the progressive morphologic changes observed in epilepsy, said the investigators. “Future research should also address whether progressive changes in cortical morphologic characteristics correlate with deficits on serial cognitive testing or spreading of the irritative zone on EEG recordings,” they concluded.
The study and the authors received support from the Medical Research Council, the Wellcome Trust, and the University College London Hospital.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Jul 1. doi: 10.1001/jamaneurol.2019.1708.
, according to research published online July 1 in JAMA Neurology. Methods for preventing this thinning are unknown. “Our findings appear to highlight the need for longitudinal studies to develop disease-modifying treatments for epilepsy,” said Marian Galovic, MD, a doctoral student at University College London, and colleagues.
To date, neurologists have not found a definitive answer to the question of whether epilepsy is a static or progressive disease. Few longitudinal studies have examined patients with structural neuroimaging to determine whether the brain changes over time. The studies that have taken this approach have had small populations or have lacked control populations.
Comparing brain changes in patients and controls
Dr. Galovic and colleagues analyzed data for consecutive patients with focal epilepsy who underwent follow-up at the National Hospital for Neurology and Neurosurgery in London. The data were collected from Aug. 3, 2004, to Jan. 26, 2016. The researchers chose individuals who had at least 2 high-resolution T1-weighted MRI scans performed on the same scanner more than 6 months apart. They excluded patients with brain lesions other than hippocampal sclerosis, those with inadequate MRI scan quality, and those for whom clinical data were missing. To match these patients with controls, Dr. Galovic and colleagues chose three longitudinal data sets with data for healthy volunteers between ages 20 and 70 years. Each control participant had two high-resolution T1-weighted scans taken more than 6 months apart. The investigators matched patients and controls on age and sex. The automated and validated Computational Anatomy Toolbox (CAT12) estimated cortical thickness.
Dr. Galovic’s group included 190 patients with focal epilepsy, who had had 396 MRI scans, and 141 healthy controls, who had had 282 MRI scans, in their analysis. Age, sex, and image quality did not differ significantly between the two groups. Mean age was 36 years for patients and 35 years for controls. The proportion of women was 52.1% among patients and 53.9% among controls.
The rate of atrophy was doubled in patients
Approximately 77% of people with epilepsy had progressive cortical thinning that was distinct from that associated with normal aging. The mean overall annual rate of global cortical thinning was higher among patients with epilepsy (0.024) than among controls (0.011). The mean annual rate of cortical thinning increased among people with epilepsy who were older than 55 years. This rate was 0.021 in patients aged 18 to less than 35 years, compared with 0.023 in patients aged 35 to less than 55 years. Seizure frequency, number of antiepileptic drugs (AEDs) taken, and history of secondarily generalized seizures did not differ between age groups.
Compared with healthy controls, patients with focal epilepsy had widespread areas of greater progressive atrophy. Bilaterally affected areas included the lateral and posterior temporal lobes, posterior cingulate gyri, occipital lobes, pericentral gyri, and opercula. The distribution of progressive thinning in all patients with epilepsy was similar to regions connected to both hippocampi. Healthy controls had no areas of greater cortical thinning, compared with patients with epilepsy.
Progressive thinning in the left postcentral gyrus was greater in patients with left temporal lobe epilepsy (TLE) than in those with right TLE. Cortical thinning was more progressive in patients with right frontal lobe epilepsy (FLE) than in those with left FLE, particularly in right parietotemporal and right frontal areas.
Dr. Galovic and colleagues found no association between the rate of cortical thinning and seizure frequency, history of secondarily generalized seizures, or number of AEDs taken between MRIs. They found no difference in the rate of atrophy between patients with epilepsy with ongoing seizures and those without. The annual mean rate of cortical thinning was higher in people with a short duration of epilepsy (i.e., less than 5 years), compared with patients with a longer duration of epilepsy (i.e., 5 years or more).
A surrogate marker for neurodegeneration?
“The most likely cause of cortical thinning is neuronal loss, suggesting that these measurements are a surrogate marker for neurodegeneration,” said Dr. Galovic and colleagues. The finding that progressive morphologic changes were most pronounced in the first 5 years after epilepsy onset “supports the need for early diagnosis, rapid treatment, and reduction of delays of surgical referral in people with epilepsy,” they added.
One limitation of the current study is the fact that data from patients and controls were acquired using different MRI scanners. In addition, the patients included in the study had been referred to the center because their cases were more complicated, thus introducing the possibility of referral bias. The findings thus cannot be generalized readily to the overall population, said Dr. Galovic and colleagues.
Future studies should examine whether particular AEDs have differential influences on the progressive morphologic changes observed in epilepsy, said the investigators. “Future research should also address whether progressive changes in cortical morphologic characteristics correlate with deficits on serial cognitive testing or spreading of the irritative zone on EEG recordings,” they concluded.
The study and the authors received support from the Medical Research Council, the Wellcome Trust, and the University College London Hospital.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Jul 1. doi: 10.1001/jamaneurol.2019.1708.
, according to research published online July 1 in JAMA Neurology. Methods for preventing this thinning are unknown. “Our findings appear to highlight the need for longitudinal studies to develop disease-modifying treatments for epilepsy,” said Marian Galovic, MD, a doctoral student at University College London, and colleagues.
To date, neurologists have not found a definitive answer to the question of whether epilepsy is a static or progressive disease. Few longitudinal studies have examined patients with structural neuroimaging to determine whether the brain changes over time. The studies that have taken this approach have had small populations or have lacked control populations.
Comparing brain changes in patients and controls
Dr. Galovic and colleagues analyzed data for consecutive patients with focal epilepsy who underwent follow-up at the National Hospital for Neurology and Neurosurgery in London. The data were collected from Aug. 3, 2004, to Jan. 26, 2016. The researchers chose individuals who had at least 2 high-resolution T1-weighted MRI scans performed on the same scanner more than 6 months apart. They excluded patients with brain lesions other than hippocampal sclerosis, those with inadequate MRI scan quality, and those for whom clinical data were missing. To match these patients with controls, Dr. Galovic and colleagues chose three longitudinal data sets with data for healthy volunteers between ages 20 and 70 years. Each control participant had two high-resolution T1-weighted scans taken more than 6 months apart. The investigators matched patients and controls on age and sex. The automated and validated Computational Anatomy Toolbox (CAT12) estimated cortical thickness.
Dr. Galovic’s group included 190 patients with focal epilepsy, who had had 396 MRI scans, and 141 healthy controls, who had had 282 MRI scans, in their analysis. Age, sex, and image quality did not differ significantly between the two groups. Mean age was 36 years for patients and 35 years for controls. The proportion of women was 52.1% among patients and 53.9% among controls.
The rate of atrophy was doubled in patients
Approximately 77% of people with epilepsy had progressive cortical thinning that was distinct from that associated with normal aging. The mean overall annual rate of global cortical thinning was higher among patients with epilepsy (0.024) than among controls (0.011). The mean annual rate of cortical thinning increased among people with epilepsy who were older than 55 years. This rate was 0.021 in patients aged 18 to less than 35 years, compared with 0.023 in patients aged 35 to less than 55 years. Seizure frequency, number of antiepileptic drugs (AEDs) taken, and history of secondarily generalized seizures did not differ between age groups.
Compared with healthy controls, patients with focal epilepsy had widespread areas of greater progressive atrophy. Bilaterally affected areas included the lateral and posterior temporal lobes, posterior cingulate gyri, occipital lobes, pericentral gyri, and opercula. The distribution of progressive thinning in all patients with epilepsy was similar to regions connected to both hippocampi. Healthy controls had no areas of greater cortical thinning, compared with patients with epilepsy.
Progressive thinning in the left postcentral gyrus was greater in patients with left temporal lobe epilepsy (TLE) than in those with right TLE. Cortical thinning was more progressive in patients with right frontal lobe epilepsy (FLE) than in those with left FLE, particularly in right parietotemporal and right frontal areas.
Dr. Galovic and colleagues found no association between the rate of cortical thinning and seizure frequency, history of secondarily generalized seizures, or number of AEDs taken between MRIs. They found no difference in the rate of atrophy between patients with epilepsy with ongoing seizures and those without. The annual mean rate of cortical thinning was higher in people with a short duration of epilepsy (i.e., less than 5 years), compared with patients with a longer duration of epilepsy (i.e., 5 years or more).
A surrogate marker for neurodegeneration?
“The most likely cause of cortical thinning is neuronal loss, suggesting that these measurements are a surrogate marker for neurodegeneration,” said Dr. Galovic and colleagues. The finding that progressive morphologic changes were most pronounced in the first 5 years after epilepsy onset “supports the need for early diagnosis, rapid treatment, and reduction of delays of surgical referral in people with epilepsy,” they added.
One limitation of the current study is the fact that data from patients and controls were acquired using different MRI scanners. In addition, the patients included in the study had been referred to the center because their cases were more complicated, thus introducing the possibility of referral bias. The findings thus cannot be generalized readily to the overall population, said Dr. Galovic and colleagues.
Future studies should examine whether particular AEDs have differential influences on the progressive morphologic changes observed in epilepsy, said the investigators. “Future research should also address whether progressive changes in cortical morphologic characteristics correlate with deficits on serial cognitive testing or spreading of the irritative zone on EEG recordings,” they concluded.
The study and the authors received support from the Medical Research Council, the Wellcome Trust, and the University College London Hospital.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Jul 1. doi: 10.1001/jamaneurol.2019.1708.
FROM JAMA NEUROLOGY
Automated measurements of plasma predict amyloid status
, according to research published online ahead of print June 24 in JAMA Neurology. Analyzing APOE genotype in addition to these biomarkers increases the accuracy of the prediction. This blood test thus could allow neurologists to identify patients at risk of amyloid-beta positivity who should undergo further assessment, said the authors. It also could be used to enroll amyloid-beta–positive participants in clinical trials.
In vivo PET imaging and analysis of cerebrospinal fluid (CSF) can detect amyloid-beta, but these procedures are expensive, and their availability is limited. Clinicians need readily available methods for detecting amyloid-beta, and research has indicated that blood-based biomarkers correlate with those in CSF. Fully automated immunoassays, such as the Elecsys test developed by Roche Diagnostics, have recently demonstrated high reliability and precision for CSF amyloid-beta. Using the Elecsys assay, Sebastian Palmqvist, MD, PhD, a neurologist at Skåne University Hospital in Malmö, Sweden, and colleagues sought to examine the accuracy of plasma amyloid-beta and tau, together with other blood-based biomarkers, at detecting cerebral amyloid-beta.
Testing the immunoassay in two cohorts
Dr. Palmqvist and colleagues examined participants in the prospective Swedish BioFINDER Study, which enrolled patients between July 6, 2009, and February 11, 2015. This cohort included 513 cognitively unimpaired (CU) participants, 265 participants with mild cognitive impairment (MCI), and 64 participants with Alzheimer’s disease dementia. Investigators collected blood and CSF samples at the same time from all participants. Participants’ amyloid-beta status was ascertained using the Elecsys CSF amyloid-beta 42/amyloid-beta 40 ratio. The researchers defined amyloid-beta positivity with an unbiased cutoff of less than 0.059.
Dr. Palmqvist and colleagues also examined a validation cohort that included 237 participants who had been enrolled between January 29, 2000, and October 11, 2006, in Ulm and Hannover, Germany. This group included 34 CU participants, 109 participants with MCI, and 94 participants with mild Alzheimer’s disease dementia. The investigators applied the same cutoff of CSF amyloid-beta 42/amyloid-beta 40 to define amyloid-beta positivity in this cohort as they applied to the BioFINDER cohort.
Automated immunoassay had high predictive accuracy
The mean age of the BioFINDER cohort was 72 years, and 52.5% of participants were female. Overall, 44% of this cohort was amyloid-beta positive, including 29% of CU participants, 60% of participants with MCI, and 100% of participants with Alzheimer’s dementia. The investigators found statistically significant positive correlations between all plasma and corresponding CSF biomarkers in this cohort.
Plasma amyloid-beta 42 and amyloid-beta 40 levels predicted amyloid-beta status with an area under the receiver operating characteristic curve (AUC) of 0.80. When the researchers added APOE to the model, the AUC increased significantly to 0.85. Accuracy improved slightly when the researchers added plasma tau (AUC, 0.86) or tau and neurofilament light (AUC, 0.87) to amyloid-beta 42, amyloid-beta 40, and APOE. The results were similar in CU and cognitively impaired participants, and in younger and older participants.
In the validation cohort, the mean age was 66 years, and 50.6% of participants were female. When Dr. Palmqvist and colleagues applied the plasma amyloid-beta 42 and amyloid-beta 40 model from the BioFINDER cohort to this population, they obtained a slightly higher AUC (0.86), but plasma tau did not increase predictive accuracy.
The investigators performed a cost-benefit analysis using a scenario in which 1,000 amyloid-positive participants are included in a trial and given a cost of $4,000 per participant for amyloid PET. Using plasma amyloid-beta 42, amyloid-beta 40, and APOE in this scenario reduced PET costs by as much as 30%-50%, depending on the cutoff.
Validation cohort was small
Dr. Palmqvist and colleagues acknowledged that a lack of data about APOE was a limitation of their validation analysis. Other limitations that they acknowledged were the small population size, which precluded subpopulation analysis, and the lack of improvement in predictive ability when they replicated the model that included plasma tau.
“Overall, the accuracies of the amyloid-beta 42 and amyloid-beta 40 assays are not sufficient to be used on their own as a clinical test of amyloid-beta positivity,” said Dr. Palmqvist and colleagues. “Additional assay development is needed before this can be recommended, possibly together with other blood biomarkers and screening tools in diagnostic algorithms.”
Even though additional validation studies are necessary, the present findings indicate “the potential usefulness blood assays might have, especially considering the ongoing great need to recruit large cohorts for Alzheimer’s disease drug trials in preclinical and prodromal stages,” the authors concluded.
This investigation was funded by foundations including the European Research Council, the Swedish Research Council, and the Knut and Alice Wallenberg foundation. Several authors are employees of the Roche Group. One author served on a scientific advisory board for Roche Diagnostics, and another received institutional research support from that company.
SOURCE: Palmqvist S et al. JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1632.
The investigation by Palmqvist et al. “makes several significant advancements in the field,” said Sid E. O’Bryant, PhD, professor of pharmacology and neuroscience at the University of North Texas Health Science Center in Fort Worth, in an accompanying editorial. The study’s protocol design clears the ground for a context of use of a blood screen for amyloid positivity. Also, the fully automated immunoassay “yields performance measurements that are superior to [those of] many earlier nonautomated procedures,” said Dr. O’Bryant. When Dr. Palmqvist and colleagues applied their discovery findings from a training cohort directly to a test cohort, it produced strong results. “This study suggests that the field is one step closer to the actual application of blood-based biomarkers with specific contexts of use in Alzheimer’s disease.”
The main concern about the plasma biomarkers, however, is the scalability of the methods used to measure them. “If primary care physicians are to use such a technology, the technology must have the capacity to conduct hundreds of millions of assays annually around the globe,” said Dr. O’Bryant. “A blood test for primary care must fit into the existing protocols and parameters in clinical laboratory settings. The blood collection and processing procedures are not applicable to standard clinical lab practice and will cause substantial barriers to clinical application.”
In addition, the study authors emphasize the utility of the immunoassay for primary care, but the study was designed to test for amyloid positivity, which is more appropriate for clinical trials. “No currently available drugs for patient use target amyloid,” said Dr. O’Bryant. “Therefore, this specific context of use is geared more toward clinical trial application than primary care physicians who currently need a test for the presence or absence of Alzheimer’s disease so currently available treatments and support can be put in place for patients and family members.”
Nevertheless, Dr. Palmqvist and associates have presented promising data, Dr. O’Bryant continued. The question in the field is ceasing to be whether blood biomarkers can be used in Alzheimer’s disease, and becoming how they can be used.
The investigation by Palmqvist et al. “makes several significant advancements in the field,” said Sid E. O’Bryant, PhD, professor of pharmacology and neuroscience at the University of North Texas Health Science Center in Fort Worth, in an accompanying editorial. The study’s protocol design clears the ground for a context of use of a blood screen for amyloid positivity. Also, the fully automated immunoassay “yields performance measurements that are superior to [those of] many earlier nonautomated procedures,” said Dr. O’Bryant. When Dr. Palmqvist and colleagues applied their discovery findings from a training cohort directly to a test cohort, it produced strong results. “This study suggests that the field is one step closer to the actual application of blood-based biomarkers with specific contexts of use in Alzheimer’s disease.”
The main concern about the plasma biomarkers, however, is the scalability of the methods used to measure them. “If primary care physicians are to use such a technology, the technology must have the capacity to conduct hundreds of millions of assays annually around the globe,” said Dr. O’Bryant. “A blood test for primary care must fit into the existing protocols and parameters in clinical laboratory settings. The blood collection and processing procedures are not applicable to standard clinical lab practice and will cause substantial barriers to clinical application.”
In addition, the study authors emphasize the utility of the immunoassay for primary care, but the study was designed to test for amyloid positivity, which is more appropriate for clinical trials. “No currently available drugs for patient use target amyloid,” said Dr. O’Bryant. “Therefore, this specific context of use is geared more toward clinical trial application than primary care physicians who currently need a test for the presence or absence of Alzheimer’s disease so currently available treatments and support can be put in place for patients and family members.”
Nevertheless, Dr. Palmqvist and associates have presented promising data, Dr. O’Bryant continued. The question in the field is ceasing to be whether blood biomarkers can be used in Alzheimer’s disease, and becoming how they can be used.
The investigation by Palmqvist et al. “makes several significant advancements in the field,” said Sid E. O’Bryant, PhD, professor of pharmacology and neuroscience at the University of North Texas Health Science Center in Fort Worth, in an accompanying editorial. The study’s protocol design clears the ground for a context of use of a blood screen for amyloid positivity. Also, the fully automated immunoassay “yields performance measurements that are superior to [those of] many earlier nonautomated procedures,” said Dr. O’Bryant. When Dr. Palmqvist and colleagues applied their discovery findings from a training cohort directly to a test cohort, it produced strong results. “This study suggests that the field is one step closer to the actual application of blood-based biomarkers with specific contexts of use in Alzheimer’s disease.”
The main concern about the plasma biomarkers, however, is the scalability of the methods used to measure them. “If primary care physicians are to use such a technology, the technology must have the capacity to conduct hundreds of millions of assays annually around the globe,” said Dr. O’Bryant. “A blood test for primary care must fit into the existing protocols and parameters in clinical laboratory settings. The blood collection and processing procedures are not applicable to standard clinical lab practice and will cause substantial barriers to clinical application.”
In addition, the study authors emphasize the utility of the immunoassay for primary care, but the study was designed to test for amyloid positivity, which is more appropriate for clinical trials. “No currently available drugs for patient use target amyloid,” said Dr. O’Bryant. “Therefore, this specific context of use is geared more toward clinical trial application than primary care physicians who currently need a test for the presence or absence of Alzheimer’s disease so currently available treatments and support can be put in place for patients and family members.”
Nevertheless, Dr. Palmqvist and associates have presented promising data, Dr. O’Bryant continued. The question in the field is ceasing to be whether blood biomarkers can be used in Alzheimer’s disease, and becoming how they can be used.
, according to research published online ahead of print June 24 in JAMA Neurology. Analyzing APOE genotype in addition to these biomarkers increases the accuracy of the prediction. This blood test thus could allow neurologists to identify patients at risk of amyloid-beta positivity who should undergo further assessment, said the authors. It also could be used to enroll amyloid-beta–positive participants in clinical trials.
In vivo PET imaging and analysis of cerebrospinal fluid (CSF) can detect amyloid-beta, but these procedures are expensive, and their availability is limited. Clinicians need readily available methods for detecting amyloid-beta, and research has indicated that blood-based biomarkers correlate with those in CSF. Fully automated immunoassays, such as the Elecsys test developed by Roche Diagnostics, have recently demonstrated high reliability and precision for CSF amyloid-beta. Using the Elecsys assay, Sebastian Palmqvist, MD, PhD, a neurologist at Skåne University Hospital in Malmö, Sweden, and colleagues sought to examine the accuracy of plasma amyloid-beta and tau, together with other blood-based biomarkers, at detecting cerebral amyloid-beta.
Testing the immunoassay in two cohorts
Dr. Palmqvist and colleagues examined participants in the prospective Swedish BioFINDER Study, which enrolled patients between July 6, 2009, and February 11, 2015. This cohort included 513 cognitively unimpaired (CU) participants, 265 participants with mild cognitive impairment (MCI), and 64 participants with Alzheimer’s disease dementia. Investigators collected blood and CSF samples at the same time from all participants. Participants’ amyloid-beta status was ascertained using the Elecsys CSF amyloid-beta 42/amyloid-beta 40 ratio. The researchers defined amyloid-beta positivity with an unbiased cutoff of less than 0.059.
Dr. Palmqvist and colleagues also examined a validation cohort that included 237 participants who had been enrolled between January 29, 2000, and October 11, 2006, in Ulm and Hannover, Germany. This group included 34 CU participants, 109 participants with MCI, and 94 participants with mild Alzheimer’s disease dementia. The investigators applied the same cutoff of CSF amyloid-beta 42/amyloid-beta 40 to define amyloid-beta positivity in this cohort as they applied to the BioFINDER cohort.
Automated immunoassay had high predictive accuracy
The mean age of the BioFINDER cohort was 72 years, and 52.5% of participants were female. Overall, 44% of this cohort was amyloid-beta positive, including 29% of CU participants, 60% of participants with MCI, and 100% of participants with Alzheimer’s dementia. The investigators found statistically significant positive correlations between all plasma and corresponding CSF biomarkers in this cohort.
Plasma amyloid-beta 42 and amyloid-beta 40 levels predicted amyloid-beta status with an area under the receiver operating characteristic curve (AUC) of 0.80. When the researchers added APOE to the model, the AUC increased significantly to 0.85. Accuracy improved slightly when the researchers added plasma tau (AUC, 0.86) or tau and neurofilament light (AUC, 0.87) to amyloid-beta 42, amyloid-beta 40, and APOE. The results were similar in CU and cognitively impaired participants, and in younger and older participants.
In the validation cohort, the mean age was 66 years, and 50.6% of participants were female. When Dr. Palmqvist and colleagues applied the plasma amyloid-beta 42 and amyloid-beta 40 model from the BioFINDER cohort to this population, they obtained a slightly higher AUC (0.86), but plasma tau did not increase predictive accuracy.
The investigators performed a cost-benefit analysis using a scenario in which 1,000 amyloid-positive participants are included in a trial and given a cost of $4,000 per participant for amyloid PET. Using plasma amyloid-beta 42, amyloid-beta 40, and APOE in this scenario reduced PET costs by as much as 30%-50%, depending on the cutoff.
Validation cohort was small
Dr. Palmqvist and colleagues acknowledged that a lack of data about APOE was a limitation of their validation analysis. Other limitations that they acknowledged were the small population size, which precluded subpopulation analysis, and the lack of improvement in predictive ability when they replicated the model that included plasma tau.
“Overall, the accuracies of the amyloid-beta 42 and amyloid-beta 40 assays are not sufficient to be used on their own as a clinical test of amyloid-beta positivity,” said Dr. Palmqvist and colleagues. “Additional assay development is needed before this can be recommended, possibly together with other blood biomarkers and screening tools in diagnostic algorithms.”
Even though additional validation studies are necessary, the present findings indicate “the potential usefulness blood assays might have, especially considering the ongoing great need to recruit large cohorts for Alzheimer’s disease drug trials in preclinical and prodromal stages,” the authors concluded.
This investigation was funded by foundations including the European Research Council, the Swedish Research Council, and the Knut and Alice Wallenberg foundation. Several authors are employees of the Roche Group. One author served on a scientific advisory board for Roche Diagnostics, and another received institutional research support from that company.
SOURCE: Palmqvist S et al. JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1632.
, according to research published online ahead of print June 24 in JAMA Neurology. Analyzing APOE genotype in addition to these biomarkers increases the accuracy of the prediction. This blood test thus could allow neurologists to identify patients at risk of amyloid-beta positivity who should undergo further assessment, said the authors. It also could be used to enroll amyloid-beta–positive participants in clinical trials.
In vivo PET imaging and analysis of cerebrospinal fluid (CSF) can detect amyloid-beta, but these procedures are expensive, and their availability is limited. Clinicians need readily available methods for detecting amyloid-beta, and research has indicated that blood-based biomarkers correlate with those in CSF. Fully automated immunoassays, such as the Elecsys test developed by Roche Diagnostics, have recently demonstrated high reliability and precision for CSF amyloid-beta. Using the Elecsys assay, Sebastian Palmqvist, MD, PhD, a neurologist at Skåne University Hospital in Malmö, Sweden, and colleagues sought to examine the accuracy of plasma amyloid-beta and tau, together with other blood-based biomarkers, at detecting cerebral amyloid-beta.
Testing the immunoassay in two cohorts
Dr. Palmqvist and colleagues examined participants in the prospective Swedish BioFINDER Study, which enrolled patients between July 6, 2009, and February 11, 2015. This cohort included 513 cognitively unimpaired (CU) participants, 265 participants with mild cognitive impairment (MCI), and 64 participants with Alzheimer’s disease dementia. Investigators collected blood and CSF samples at the same time from all participants. Participants’ amyloid-beta status was ascertained using the Elecsys CSF amyloid-beta 42/amyloid-beta 40 ratio. The researchers defined amyloid-beta positivity with an unbiased cutoff of less than 0.059.
Dr. Palmqvist and colleagues also examined a validation cohort that included 237 participants who had been enrolled between January 29, 2000, and October 11, 2006, in Ulm and Hannover, Germany. This group included 34 CU participants, 109 participants with MCI, and 94 participants with mild Alzheimer’s disease dementia. The investigators applied the same cutoff of CSF amyloid-beta 42/amyloid-beta 40 to define amyloid-beta positivity in this cohort as they applied to the BioFINDER cohort.
Automated immunoassay had high predictive accuracy
The mean age of the BioFINDER cohort was 72 years, and 52.5% of participants were female. Overall, 44% of this cohort was amyloid-beta positive, including 29% of CU participants, 60% of participants with MCI, and 100% of participants with Alzheimer’s dementia. The investigators found statistically significant positive correlations between all plasma and corresponding CSF biomarkers in this cohort.
Plasma amyloid-beta 42 and amyloid-beta 40 levels predicted amyloid-beta status with an area under the receiver operating characteristic curve (AUC) of 0.80. When the researchers added APOE to the model, the AUC increased significantly to 0.85. Accuracy improved slightly when the researchers added plasma tau (AUC, 0.86) or tau and neurofilament light (AUC, 0.87) to amyloid-beta 42, amyloid-beta 40, and APOE. The results were similar in CU and cognitively impaired participants, and in younger and older participants.
In the validation cohort, the mean age was 66 years, and 50.6% of participants were female. When Dr. Palmqvist and colleagues applied the plasma amyloid-beta 42 and amyloid-beta 40 model from the BioFINDER cohort to this population, they obtained a slightly higher AUC (0.86), but plasma tau did not increase predictive accuracy.
The investigators performed a cost-benefit analysis using a scenario in which 1,000 amyloid-positive participants are included in a trial and given a cost of $4,000 per participant for amyloid PET. Using plasma amyloid-beta 42, amyloid-beta 40, and APOE in this scenario reduced PET costs by as much as 30%-50%, depending on the cutoff.
Validation cohort was small
Dr. Palmqvist and colleagues acknowledged that a lack of data about APOE was a limitation of their validation analysis. Other limitations that they acknowledged were the small population size, which precluded subpopulation analysis, and the lack of improvement in predictive ability when they replicated the model that included plasma tau.
“Overall, the accuracies of the amyloid-beta 42 and amyloid-beta 40 assays are not sufficient to be used on their own as a clinical test of amyloid-beta positivity,” said Dr. Palmqvist and colleagues. “Additional assay development is needed before this can be recommended, possibly together with other blood biomarkers and screening tools in diagnostic algorithms.”
Even though additional validation studies are necessary, the present findings indicate “the potential usefulness blood assays might have, especially considering the ongoing great need to recruit large cohorts for Alzheimer’s disease drug trials in preclinical and prodromal stages,” the authors concluded.
This investigation was funded by foundations including the European Research Council, the Swedish Research Council, and the Knut and Alice Wallenberg foundation. Several authors are employees of the Roche Group. One author served on a scientific advisory board for Roche Diagnostics, and another received institutional research support from that company.
SOURCE: Palmqvist S et al. JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1632.
FROM JAMA NEUROLOGY
Rituximab and vemurafenib could challenge frontline chemotherapy for HCL
AMSTERDAM – A combination of rituximab and the BRAF inhibitor vemurafenib could be the one-two punch needed for relapsed or refractory hairy cell leukemia (HCL), according to investigators.
Among evaluable patients treated with this combination, 96% achieved complete remission, reported lead author, Enrico Tiacci, MD, of the University and Hospital of Perugia, Italy.
This level of efficacy is “clearly superior to historical results with either agent alone,” Dr. Tiacci said during a presentation at the annual congress of the European Hematology Association, citing previous complete response rates with vemurafenib alone of 35%-40%. “[This combination] has potential for challenging chemotherapy in the frontline setting,” he said.
The phase 2 trial involved 31 patients with relapsed or refractory HCL who had received a median of three previous therapies. Eight of the patients (26%) had primary refractory disease. Patients received vemurafenib 960 mg, twice daily for 8 weeks and rituximab 375 mg/m2, every 2 weeks. After finishing vemurafenib, patients received rituximab four more times, keeping the interval of 2 weeks. Complete remission was defined as a normal blood count, no leukemic cells in bone marrow biopsies and blood smears, and no palpable splenomegaly.
Out of 31 patients, 27 were evaluable at data cutoff. Of these, 26 (96%) achieved complete remission. The investigators noted that two complete responders had incomplete platelet recovery at the end of treatment that resolved soon after, and two patients had persistent splenomegaly, but were considered to be in complete remission at 22.5 and 25 months after finishing therapy.
All of the complete responders had previously received purine analogs, while a few had been refractory to a prior BRAF inhibitor (n = 7) and/or rituximab (n = 5).
The investigators also pointed out that 15 out of 24 evaluable patients (63%) achieved complete remission just 4 weeks after starting the trial regimen. Almost two-thirds of patients (65%) were negative for minimal residual disease (MRD). The rate of progression-free survival at a median follow-up of 29.5 months was 83%. Disease progression occurred exclusively in patients who were MRD positive.
The combination was well tolerated; most adverse events were of grade 1 or 2, overlapping with the safety profile of each agent alone.
Reflecting on the study findings, Dr. Tiacci suggested that the combination could be most effective if delivered immediately, instead of after BRAF failure.
“Interestingly,” he said, “the relapse-free survival in patients naive to a BRAF inhibitor remained significantly longer than the relapse-free interval that patients previously exposed to a BRAF inhibitor enjoyed, both following monotherapy with a BRAF inhibitor and following subsequent combination with rituximab, potentially suggesting that vemurafenib should be used directly in combination with rituximab rather than being delivered first as a monotherapy and then added to rituximab at relapse.”
Randomized testing of the combination against the chemotherapy-based standard of care in the frontline setting is warranted, the investigators concluded.
Dr. Tiacci reported financial relationships with Roche, AbbVie, and Shire.
SOURCE: Tiacci E et al. EHA Congress, Abstract S104.
AMSTERDAM – A combination of rituximab and the BRAF inhibitor vemurafenib could be the one-two punch needed for relapsed or refractory hairy cell leukemia (HCL), according to investigators.
Among evaluable patients treated with this combination, 96% achieved complete remission, reported lead author, Enrico Tiacci, MD, of the University and Hospital of Perugia, Italy.
This level of efficacy is “clearly superior to historical results with either agent alone,” Dr. Tiacci said during a presentation at the annual congress of the European Hematology Association, citing previous complete response rates with vemurafenib alone of 35%-40%. “[This combination] has potential for challenging chemotherapy in the frontline setting,” he said.
The phase 2 trial involved 31 patients with relapsed or refractory HCL who had received a median of three previous therapies. Eight of the patients (26%) had primary refractory disease. Patients received vemurafenib 960 mg, twice daily for 8 weeks and rituximab 375 mg/m2, every 2 weeks. After finishing vemurafenib, patients received rituximab four more times, keeping the interval of 2 weeks. Complete remission was defined as a normal blood count, no leukemic cells in bone marrow biopsies and blood smears, and no palpable splenomegaly.
Out of 31 patients, 27 were evaluable at data cutoff. Of these, 26 (96%) achieved complete remission. The investigators noted that two complete responders had incomplete platelet recovery at the end of treatment that resolved soon after, and two patients had persistent splenomegaly, but were considered to be in complete remission at 22.5 and 25 months after finishing therapy.
All of the complete responders had previously received purine analogs, while a few had been refractory to a prior BRAF inhibitor (n = 7) and/or rituximab (n = 5).
The investigators also pointed out that 15 out of 24 evaluable patients (63%) achieved complete remission just 4 weeks after starting the trial regimen. Almost two-thirds of patients (65%) were negative for minimal residual disease (MRD). The rate of progression-free survival at a median follow-up of 29.5 months was 83%. Disease progression occurred exclusively in patients who were MRD positive.
The combination was well tolerated; most adverse events were of grade 1 or 2, overlapping with the safety profile of each agent alone.
Reflecting on the study findings, Dr. Tiacci suggested that the combination could be most effective if delivered immediately, instead of after BRAF failure.
“Interestingly,” he said, “the relapse-free survival in patients naive to a BRAF inhibitor remained significantly longer than the relapse-free interval that patients previously exposed to a BRAF inhibitor enjoyed, both following monotherapy with a BRAF inhibitor and following subsequent combination with rituximab, potentially suggesting that vemurafenib should be used directly in combination with rituximab rather than being delivered first as a monotherapy and then added to rituximab at relapse.”
Randomized testing of the combination against the chemotherapy-based standard of care in the frontline setting is warranted, the investigators concluded.
Dr. Tiacci reported financial relationships with Roche, AbbVie, and Shire.
SOURCE: Tiacci E et al. EHA Congress, Abstract S104.
AMSTERDAM – A combination of rituximab and the BRAF inhibitor vemurafenib could be the one-two punch needed for relapsed or refractory hairy cell leukemia (HCL), according to investigators.
Among evaluable patients treated with this combination, 96% achieved complete remission, reported lead author, Enrico Tiacci, MD, of the University and Hospital of Perugia, Italy.
This level of efficacy is “clearly superior to historical results with either agent alone,” Dr. Tiacci said during a presentation at the annual congress of the European Hematology Association, citing previous complete response rates with vemurafenib alone of 35%-40%. “[This combination] has potential for challenging chemotherapy in the frontline setting,” he said.
The phase 2 trial involved 31 patients with relapsed or refractory HCL who had received a median of three previous therapies. Eight of the patients (26%) had primary refractory disease. Patients received vemurafenib 960 mg, twice daily for 8 weeks and rituximab 375 mg/m2, every 2 weeks. After finishing vemurafenib, patients received rituximab four more times, keeping the interval of 2 weeks. Complete remission was defined as a normal blood count, no leukemic cells in bone marrow biopsies and blood smears, and no palpable splenomegaly.
Out of 31 patients, 27 were evaluable at data cutoff. Of these, 26 (96%) achieved complete remission. The investigators noted that two complete responders had incomplete platelet recovery at the end of treatment that resolved soon after, and two patients had persistent splenomegaly, but were considered to be in complete remission at 22.5 and 25 months after finishing therapy.
All of the complete responders had previously received purine analogs, while a few had been refractory to a prior BRAF inhibitor (n = 7) and/or rituximab (n = 5).
The investigators also pointed out that 15 out of 24 evaluable patients (63%) achieved complete remission just 4 weeks after starting the trial regimen. Almost two-thirds of patients (65%) were negative for minimal residual disease (MRD). The rate of progression-free survival at a median follow-up of 29.5 months was 83%. Disease progression occurred exclusively in patients who were MRD positive.
The combination was well tolerated; most adverse events were of grade 1 or 2, overlapping with the safety profile of each agent alone.
Reflecting on the study findings, Dr. Tiacci suggested that the combination could be most effective if delivered immediately, instead of after BRAF failure.
“Interestingly,” he said, “the relapse-free survival in patients naive to a BRAF inhibitor remained significantly longer than the relapse-free interval that patients previously exposed to a BRAF inhibitor enjoyed, both following monotherapy with a BRAF inhibitor and following subsequent combination with rituximab, potentially suggesting that vemurafenib should be used directly in combination with rituximab rather than being delivered first as a monotherapy and then added to rituximab at relapse.”
Randomized testing of the combination against the chemotherapy-based standard of care in the frontline setting is warranted, the investigators concluded.
Dr. Tiacci reported financial relationships with Roche, AbbVie, and Shire.
SOURCE: Tiacci E et al. EHA Congress, Abstract S104.
REPORTING FROM EHA CONGRESS
Cell count ratios appear to predict thromboembolism in lymphoma
AMSTERDAM – When predicting the risk of thromboembolism in lymphoma patients receiving chemotherapy, clinicians can rely on a routine diagnostic tool: complete blood count, investigators reported.
A recent study found that high neutrophil to lymphocyte (NLR) and platelet to lymphocyte (PLR) ratios were prognostic for thromboembolism in this setting, reported lead author Vladimir Otasevic, MD, of the Clinical Centre of Serbia in Belgrade.
“Because of the presence of a broad spectrum of risk factors [in patients with lymphoma undergoing chemotherapy], some authors have published risk-assessment models for prediction of thromboembolism,” Dr. Otasevic said during a presentation at the annual congress of the European Hematology Association. While the underlying pathophysiology that precedes thromboembolism is complex, Dr. Otasevic suggested that risk prediction may not have to be, noting that NLR and PLR were recently proposed as risk biomarkers.
To test the utility of these potential biomarkers, Dr. Otasevic and his colleagues retrospectively analyzed data from 484 patients with non-Hodgkin and Hodgkin lymphoma who had undergone at least one cycle of chemotherapy at the Clinic for Hematology, Clinical Centre of Serbia. Patients were followed for venous and arterial thromboembolic events from the time of diagnosis to 3 months beyond their final cycle of chemotherapy. NLR and PLR ratios were calculated from complete blood count. Thromboembolism was diagnosed by radiography, clinical exam, and laboratory evaluation, with probable diagnoses reviewed by an internist and radiologist.
The median patient age was 53 years with a range from 18 to 89 years. Most patients were recently diagnosed with advanced disease (21.1% stage III and 42.5% stage IV). Half of the population had high-grade non-Hodgkin lymphoma (50.0%) and slightly more than a quarter had low-grade non-Hodgkin lymphoma (28.3%). Low-grade Hodgkin lymphoma was less common (17.4%) and followed distantly by other forms (4.3%).
Thirty-five patients (7.2%) developed thromboembolic events; of these, 30 had venous thromboembolism (6.2%), 6 had arterial thromboembolism (1.2%), and 1 had both. Patients who experienced thromboembolic events had significantly higher NLR and PLR than patients without thromboembolism, and both ratios were significantly associated with one another.
A positive NLR, defined as a ratio of 3.1 or more, was associated with a relative risk of 4.1 for thromboembolism (P less than .001), while a positive PLR, defined as a ratio of 10 or more, was associated with a relative risk of 2.9 (P = .008). Using a multivariate model, a positive NLR was associated with an even higher relative risk (RR = 4.5; P less than .001).
“NLR and PLR demonstrated significant powerfulness in prediction of future risk of [thromboembolism] in lymphoma patients,” the investigators concluded. “Simplicity, effectiveness, modesty, and practicability qualify these new tools for routine [thromboembolism] prognostic assessment.”
Dr. Otasevic said that he and his colleagues have plans to build on these findings with further analysis involving progression-free and overall survival.
The investigators reported no disclosures.
SOURCE: Otasevic V et al. EHA Congress, Abstract S1645.
AMSTERDAM – When predicting the risk of thromboembolism in lymphoma patients receiving chemotherapy, clinicians can rely on a routine diagnostic tool: complete blood count, investigators reported.
A recent study found that high neutrophil to lymphocyte (NLR) and platelet to lymphocyte (PLR) ratios were prognostic for thromboembolism in this setting, reported lead author Vladimir Otasevic, MD, of the Clinical Centre of Serbia in Belgrade.
“Because of the presence of a broad spectrum of risk factors [in patients with lymphoma undergoing chemotherapy], some authors have published risk-assessment models for prediction of thromboembolism,” Dr. Otasevic said during a presentation at the annual congress of the European Hematology Association. While the underlying pathophysiology that precedes thromboembolism is complex, Dr. Otasevic suggested that risk prediction may not have to be, noting that NLR and PLR were recently proposed as risk biomarkers.
To test the utility of these potential biomarkers, Dr. Otasevic and his colleagues retrospectively analyzed data from 484 patients with non-Hodgkin and Hodgkin lymphoma who had undergone at least one cycle of chemotherapy at the Clinic for Hematology, Clinical Centre of Serbia. Patients were followed for venous and arterial thromboembolic events from the time of diagnosis to 3 months beyond their final cycle of chemotherapy. NLR and PLR ratios were calculated from complete blood count. Thromboembolism was diagnosed by radiography, clinical exam, and laboratory evaluation, with probable diagnoses reviewed by an internist and radiologist.
The median patient age was 53 years with a range from 18 to 89 years. Most patients were recently diagnosed with advanced disease (21.1% stage III and 42.5% stage IV). Half of the population had high-grade non-Hodgkin lymphoma (50.0%) and slightly more than a quarter had low-grade non-Hodgkin lymphoma (28.3%). Low-grade Hodgkin lymphoma was less common (17.4%) and followed distantly by other forms (4.3%).
Thirty-five patients (7.2%) developed thromboembolic events; of these, 30 had venous thromboembolism (6.2%), 6 had arterial thromboembolism (1.2%), and 1 had both. Patients who experienced thromboembolic events had significantly higher NLR and PLR than patients without thromboembolism, and both ratios were significantly associated with one another.
A positive NLR, defined as a ratio of 3.1 or more, was associated with a relative risk of 4.1 for thromboembolism (P less than .001), while a positive PLR, defined as a ratio of 10 or more, was associated with a relative risk of 2.9 (P = .008). Using a multivariate model, a positive NLR was associated with an even higher relative risk (RR = 4.5; P less than .001).
“NLR and PLR demonstrated significant powerfulness in prediction of future risk of [thromboembolism] in lymphoma patients,” the investigators concluded. “Simplicity, effectiveness, modesty, and practicability qualify these new tools for routine [thromboembolism] prognostic assessment.”
Dr. Otasevic said that he and his colleagues have plans to build on these findings with further analysis involving progression-free and overall survival.
The investigators reported no disclosures.
SOURCE: Otasevic V et al. EHA Congress, Abstract S1645.
AMSTERDAM – When predicting the risk of thromboembolism in lymphoma patients receiving chemotherapy, clinicians can rely on a routine diagnostic tool: complete blood count, investigators reported.
A recent study found that high neutrophil to lymphocyte (NLR) and platelet to lymphocyte (PLR) ratios were prognostic for thromboembolism in this setting, reported lead author Vladimir Otasevic, MD, of the Clinical Centre of Serbia in Belgrade.
“Because of the presence of a broad spectrum of risk factors [in patients with lymphoma undergoing chemotherapy], some authors have published risk-assessment models for prediction of thromboembolism,” Dr. Otasevic said during a presentation at the annual congress of the European Hematology Association. While the underlying pathophysiology that precedes thromboembolism is complex, Dr. Otasevic suggested that risk prediction may not have to be, noting that NLR and PLR were recently proposed as risk biomarkers.
To test the utility of these potential biomarkers, Dr. Otasevic and his colleagues retrospectively analyzed data from 484 patients with non-Hodgkin and Hodgkin lymphoma who had undergone at least one cycle of chemotherapy at the Clinic for Hematology, Clinical Centre of Serbia. Patients were followed for venous and arterial thromboembolic events from the time of diagnosis to 3 months beyond their final cycle of chemotherapy. NLR and PLR ratios were calculated from complete blood count. Thromboembolism was diagnosed by radiography, clinical exam, and laboratory evaluation, with probable diagnoses reviewed by an internist and radiologist.
The median patient age was 53 years with a range from 18 to 89 years. Most patients were recently diagnosed with advanced disease (21.1% stage III and 42.5% stage IV). Half of the population had high-grade non-Hodgkin lymphoma (50.0%) and slightly more than a quarter had low-grade non-Hodgkin lymphoma (28.3%). Low-grade Hodgkin lymphoma was less common (17.4%) and followed distantly by other forms (4.3%).
Thirty-five patients (7.2%) developed thromboembolic events; of these, 30 had venous thromboembolism (6.2%), 6 had arterial thromboembolism (1.2%), and 1 had both. Patients who experienced thromboembolic events had significantly higher NLR and PLR than patients without thromboembolism, and both ratios were significantly associated with one another.
A positive NLR, defined as a ratio of 3.1 or more, was associated with a relative risk of 4.1 for thromboembolism (P less than .001), while a positive PLR, defined as a ratio of 10 or more, was associated with a relative risk of 2.9 (P = .008). Using a multivariate model, a positive NLR was associated with an even higher relative risk (RR = 4.5; P less than .001).
“NLR and PLR demonstrated significant powerfulness in prediction of future risk of [thromboembolism] in lymphoma patients,” the investigators concluded. “Simplicity, effectiveness, modesty, and practicability qualify these new tools for routine [thromboembolism] prognostic assessment.”
Dr. Otasevic said that he and his colleagues have plans to build on these findings with further analysis involving progression-free and overall survival.
The investigators reported no disclosures.
SOURCE: Otasevic V et al. EHA Congress, Abstract S1645.
REPORTING FROM EHA CONGRESS
Partners in Oncology Care: Coordinated Follicular Lymphoma Management (FULL)
Four case examples illustrate the important role of multidisciplinary medical care for the optimal long-term care of patients with follicular lymphoma.
Patients benefit from multidisciplinary care that coordinates management of complex medical problems. Traditionally, multidisciplinary cancer care involves oncology specialty providers in fields that include medical oncology, radiation oncology, and surgical oncology. Multidisciplinary cancer care intends to improve patient outcomes by bringing together different health care providers (HCPs) who are involved in the treatment of patients with cancer. Because new therapies are more effective and allow patients with cancer to live longer, adverse effects (AEs) are more likely to impact patients’ well-being, both while receiving treatment and long after it has completed. Thus, this population may benefit from an expanded approach to multidisciplinary care that includes input from specialty and primary care providers (PCPs), clinical pharmacy specialists (CPS), physical and occupational therapists, and patient navigators and educators.
We present 4 hypothetical cases, based on actual patients, that illustrate opportunities where multidisciplinary care coordination may improve patient experiences. These cases draw on current quality initiatives from the National Cancer Institute Community Cancer Centers Program, which has focused on improving the quality of multidisciplinary cancer care at selected community centers, and the Veterans Health Administration (VHA) patient-aligned care team (PACT) model, which brings together different health professionals to optimize primary care coordination.1,2 In addition, the National Committee for Quality Assurance has introduced an educational initiative to facilitate implementation of an oncologic medical home.3 This initiative stresses increased multidisciplinary communication, patient-centered care delivery, and reduced fragmentation of care for this population. Despite these guidelines and experiences from other medical specialties, models for integrated cancer care have not been implemented in a prospective fashion within the VHA.
In this article, we focus on opportunities to take collaborative care approaches for the treatment of patients with follicular lymphoma (FL): a common, incurable, and often indolent B-cell non-Hodgkin lymphoma.4 FL was selected because these patients may be treated numerous times and long-term sequalae can accumulate throughout their cancer continuum (a series of health events encompassing cancer screening, diagnosis, treatment, survivorship, relapse, and death).5 HCPs in distinct roles can assist patients with cancer in optimizing their health outcomes and overall wellbeing.6
Case Example 1
A 70-year-old male was diagnosed with stage IV FL. Because of his advanced disease, he began therapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone). Prednisone was administered at 100 mg daily on the first 5 days of each 21-day cycle. On day 4 of the first treatment cycle, the patient notified his oncologist that he had been very thirsty and his random blood sugar values on 2 different days were 283 mg/dL and 312 mg/dL. A laboratory review revealed his hemoglobin A1c (HbA1c) 7 months prior was 5.6%.
Discussion
The high-dose prednisone component of this and other lymphoma therapy regimens can worsen diabetes mellitus (DM) control and/or worsen prediabetes. Patient characteristics that increase the risk of developing glucocorticoid-induced DM after CHOP chemotherapy include age ≥ 60 years, HbA1c > 6.1%, and body mass index > 30.7 This patient did not have DM prior to the FL therapy initiation, but afterwards he met diagnostic criteria for DM. For completeness, other causes for elevated blood glucose should be ruled out (ie, infection, laboratory error, etc.). An oncologist often will triage acute hyperglycemia, treating immediately with IV fluids and/or insulin. Thereafter, ongoing chronic disease management for DM may be best managed by PCPs, certified DM educators, and registered dieticians.
Several programs involving multidisciplinary DM care, comprised of physicians, advanced practice providers, nurses, certified DM educators, and/or pharmacists have been shown to improve HbA1c, cardiovascular outcomes, and all-cause mortality, while reducing health care costs.8 In addition, patient navigators can assist patients with coordinating visits to disease-state specialists and identifying further educational needs. For example, in 1 program, nonclinical peer navigators were shown to improve the number of appointments attended and reduce HbA1c in a population of patients with DM who were primarily minority, urban, and of low socioeconomic status.9 Thus, integrating DM care shows potential to improve outcomes for patients with lymphoma who develop glucocorticoid
Case Example 2
A 75-year-old male was diagnosed with FL. He was treated initially with bendamustine and rituximab. He required reinitiation of therapy 20 months later when he developed lymphadenopathy, fatigue, and night sweats and began treatment with oral idelalisib, a second-line therapy. Later, the patient presented to his PCP for a routine visit, and on medication reconciliation review, the patient reported regular use of trimethoprim-sulfamethoxazole.
Discussion
Upon consultation with the CPS and the patient’s oncologist, the PCP confirmed trimethoprim-sulfamethoxazole should be continued during therapy and for about 6 months following completion of therapy. Trimethoprim-sulfamethoxazole is used for prophylaxis against Pneumocystis jirovecii (formerly Pneumocystis carinii). While use of prophylactic therapy is not necessary for all patients with FL, idelalisib impairs the function of circulating lymphoid B-cells and thus has been associated with an increased risk of serious infection.10 A CPS can provide insight that maximizes medication adherence and efficacy while minimizing food-drug, drug-drug interactions, and AEs. CPS have been shown to: improve adherence to oral therapies, increase prospective monitoring required for safe therapy dose selection, and document assessment of chemotherapy-related AEs.11,12 Thus, multidisciplinary, integrated care is an important component of providing quality oncology care.
Case Example 3
A 60-year-old female presented to her PCP with a 2-week history of shortness of breath and leg swelling. She was treated for FL 4 years previously with 6 cycles of R-CHOP. She reported no chest pain and did not have a prior history of hypertension, DM, or heart disease. On physical exam, she had elevated jugular venous pressure to jaw at 45°, bilateral pulmonary rales, and 2+ pitting pretibial edema. Laboratory tests that included complete blood count, basic chemistries, and thyroid stimulating hormone were unremarkable, though brain natriuretic peptide (BNP) was elevated at 425 pg/mL.
As this patient’s laboratory results and physical examination suggested new-onset congestive heart failure, the PCP obtained an echocardiogram, which demonstrated an ejection fraction of 35% and global hypokinesis. Because the patient was symptomatic, she was admitted to the hospital to begin guideline-directed medical therapy (GDMT) including IV diuresis.
Discussion
Given the absence of significant risk factors and prior history of coronary artery disease, the most probable cause for this patient’s cardiomyopathy is doxorubicin. Doxorubicin is an anthracycline chemotherapy that can cause nonischemic, dilated cardiomyopathy, particularly when cumulative doses > 400 mg/m2 are administered, or when combined with chest radiation.13 This patient benefited from GDMT for reduced ejection-fraction heart failure (HFrEF). Studies have demonstrated positive outcomes when HFrEF patients are cared for by a multidisciplinary team who focus of volume management as well as uptitration of therapies to target doses.14
Case Example 4
An 80-year-old female was diagnosed with stage III FL but did not require immediate therapy. After developing discomfort due to enlarging lymphadenopathy, she initiated therapy with rituximab, cyclophosphamide, vincristine, and prednisone (R-CVP). She presented to her oncologist for consideration of her fifth cycle of R-CVP and reported a burning sensation on the soles of her feet and numbness in her fingertips and toes. On examination, her pulses were intact and there were no signs of infection, reduced blood flow, or edema. The patient demonstrated decreased sensation on monofilament testing. She had no history of DM and a recent HbA1c test was 4.9% An evaluation for other causes of neuropathy, such as hypothyroidism and vitamin B12 deficiency was negative. Thus, vincristine therapy was identified as the most likely etiology for her peripheral neuropathy. The oncologist decided to proceed with cycle 5 of chemotherapy but reduced the dose of vincristine by 50%.
Discussion
Vincristine is a microtubule inhibitor used in many chemotherapy regimens and may cause reversible or permanent neuropathy, including autonomic (constipation), sensory (stocking-glove distribution), or motor (foot-drop).15 A nerve conduction study may be indicated as part of the diagnostic evaluation. Treatment for painful sensory neuropathy may include pharmacologic therapy (such as gabapentin, pregabalin, capsaicin cream).16 Podiatrists can provide foot care and may provide shoes and inserts if appropriate. Physical therapists may assist with safety and mobility evaluations and can provide therapeutic exercises and assistive devices that improve function and quality of life.17
Conclusion
As cancer becomes more curable and more manageable, patients with cancer and survivors no longer rely exclusively on their oncologists for medical care. This is increasingly prevalent for patients with incurable but indolent cancers that may be present for years to decades, as acute and cumulative toxicities may complicate existing comorbidities. Thus, in this era of increasingly complex cancer therapies, multidisciplinary medical care that involves PCPs, specialists, and allied medical professionals, is essential for providing care that optimizes health and fully addresses patients’ needs.
1. Friedman EL, Chawla N, Morris PT, et al. Assessing the development of multidisciplinary care: experience of the National Cancer Institute community cancer centers program. J Oncol Pract. 2015;11(1):e36-e43.
2. Peterson K, Helfand M, Humphrey L, Christensen V, Carson S. Evidence brief: effectiveness of intensive primary care programs. https://www.hsrd.research.va.gov/publications/esp/Intensive-Primary-Care-Supplement.pdf. Published February 2013. Accessed April 5, 2019.
3. National Committee for Quality Assurance. Oncology medical home recognition. https://www.ncqa.org/programs/health-care-providers-practices/oncology-medical-home. Accessed April 5, 2019.
4. Kahl BS, Yang DT. Follicular lymphoma: evolving therapeutic strategies. Blood. 2016;127(17):2055-2063.
5. Dulaney C, Wallace AS, Everett AS, Dover L, McDonald A, Kropp L. Defining health across the cancer continuum. Cureus. 2017;9(2):e1029.
6. Hopkins J, Mumber MP. Patient navigation through the cancer care continuum: an overview. J Oncol Pract. 2009;5(4):150-152.
7. Lee SY, Kurita N, Yokoyama Y, et al. Glucocorticoid-induced diabetes mellitus in patients with lymphoma treated with CHOP chemotherapy. Support Care Cancer. 2014;22(5):1385-1390.
8. McGill M, Blonde L, Juliana CN, et al; Global Partnership for Effective Diabetes Management. The interdisciplinary team in type 2 diabetes management: challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. 2017;7:21-27.
9. Horný M, Glover W, Gupte G, Saraswat A, Vimalananda V, Rosenzweig J. Patient navigation to improve diabetes outpatient care at a safety-net hospital: a retrospective cohort study. BMC Health Serv Res. 2017;17(1):759.
10. Reinwald M, Silva JT, Mueller NJ, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Intracellular signaling pathways: tyrosine kinase and mTOR inhibitors). Clin Microbiol Infect. 2018;24(suppl 2):S53-S70.
11. Holle LM, Boehnke Michaud L. Oncology pharmacists in health care delivery: vital members of the cancer care team. J. Oncol. Pract. 2014;10(3):e142-e145.
12. Morgan KP, Muluneh B, Dean AM, Amerine LB. Impact of an integrated oral chemotherapy program on patient adherence. J Oncol Pharm Pract. 2018;24(5):332-336.
13. Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869-2879.
14. Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774-784.
15. Mora E, Smith EM, Donohoe C, Hertz DL. Vincristine-induced peripheral neuropathy in pediatric cancer patients. Am J Cancer Res. 2016;6(11):2416-2430.
16. Hershman DL, Lacchetti C, Dworkin RH, et al; American Society of Clinical Oncology. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(18):1941–1967
17. Duregon F, Vendramin B, Bullo V, et al. Effects of exercise on cancer patients suffering chemotherapy-induced peripheral neuropathy undergoing treatment: a systematic review. Crit Rev Oncol Hematol. 2018;121:90-100.
Four case examples illustrate the important role of multidisciplinary medical care for the optimal long-term care of patients with follicular lymphoma.
Four case examples illustrate the important role of multidisciplinary medical care for the optimal long-term care of patients with follicular lymphoma.
Patients benefit from multidisciplinary care that coordinates management of complex medical problems. Traditionally, multidisciplinary cancer care involves oncology specialty providers in fields that include medical oncology, radiation oncology, and surgical oncology. Multidisciplinary cancer care intends to improve patient outcomes by bringing together different health care providers (HCPs) who are involved in the treatment of patients with cancer. Because new therapies are more effective and allow patients with cancer to live longer, adverse effects (AEs) are more likely to impact patients’ well-being, both while receiving treatment and long after it has completed. Thus, this population may benefit from an expanded approach to multidisciplinary care that includes input from specialty and primary care providers (PCPs), clinical pharmacy specialists (CPS), physical and occupational therapists, and patient navigators and educators.
We present 4 hypothetical cases, based on actual patients, that illustrate opportunities where multidisciplinary care coordination may improve patient experiences. These cases draw on current quality initiatives from the National Cancer Institute Community Cancer Centers Program, which has focused on improving the quality of multidisciplinary cancer care at selected community centers, and the Veterans Health Administration (VHA) patient-aligned care team (PACT) model, which brings together different health professionals to optimize primary care coordination.1,2 In addition, the National Committee for Quality Assurance has introduced an educational initiative to facilitate implementation of an oncologic medical home.3 This initiative stresses increased multidisciplinary communication, patient-centered care delivery, and reduced fragmentation of care for this population. Despite these guidelines and experiences from other medical specialties, models for integrated cancer care have not been implemented in a prospective fashion within the VHA.
In this article, we focus on opportunities to take collaborative care approaches for the treatment of patients with follicular lymphoma (FL): a common, incurable, and often indolent B-cell non-Hodgkin lymphoma.4 FL was selected because these patients may be treated numerous times and long-term sequalae can accumulate throughout their cancer continuum (a series of health events encompassing cancer screening, diagnosis, treatment, survivorship, relapse, and death).5 HCPs in distinct roles can assist patients with cancer in optimizing their health outcomes and overall wellbeing.6
Case Example 1
A 70-year-old male was diagnosed with stage IV FL. Because of his advanced disease, he began therapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone). Prednisone was administered at 100 mg daily on the first 5 days of each 21-day cycle. On day 4 of the first treatment cycle, the patient notified his oncologist that he had been very thirsty and his random blood sugar values on 2 different days were 283 mg/dL and 312 mg/dL. A laboratory review revealed his hemoglobin A1c (HbA1c) 7 months prior was 5.6%.
Discussion
The high-dose prednisone component of this and other lymphoma therapy regimens can worsen diabetes mellitus (DM) control and/or worsen prediabetes. Patient characteristics that increase the risk of developing glucocorticoid-induced DM after CHOP chemotherapy include age ≥ 60 years, HbA1c > 6.1%, and body mass index > 30.7 This patient did not have DM prior to the FL therapy initiation, but afterwards he met diagnostic criteria for DM. For completeness, other causes for elevated blood glucose should be ruled out (ie, infection, laboratory error, etc.). An oncologist often will triage acute hyperglycemia, treating immediately with IV fluids and/or insulin. Thereafter, ongoing chronic disease management for DM may be best managed by PCPs, certified DM educators, and registered dieticians.
Several programs involving multidisciplinary DM care, comprised of physicians, advanced practice providers, nurses, certified DM educators, and/or pharmacists have been shown to improve HbA1c, cardiovascular outcomes, and all-cause mortality, while reducing health care costs.8 In addition, patient navigators can assist patients with coordinating visits to disease-state specialists and identifying further educational needs. For example, in 1 program, nonclinical peer navigators were shown to improve the number of appointments attended and reduce HbA1c in a population of patients with DM who were primarily minority, urban, and of low socioeconomic status.9 Thus, integrating DM care shows potential to improve outcomes for patients with lymphoma who develop glucocorticoid
Case Example 2
A 75-year-old male was diagnosed with FL. He was treated initially with bendamustine and rituximab. He required reinitiation of therapy 20 months later when he developed lymphadenopathy, fatigue, and night sweats and began treatment with oral idelalisib, a second-line therapy. Later, the patient presented to his PCP for a routine visit, and on medication reconciliation review, the patient reported regular use of trimethoprim-sulfamethoxazole.
Discussion
Upon consultation with the CPS and the patient’s oncologist, the PCP confirmed trimethoprim-sulfamethoxazole should be continued during therapy and for about 6 months following completion of therapy. Trimethoprim-sulfamethoxazole is used for prophylaxis against Pneumocystis jirovecii (formerly Pneumocystis carinii). While use of prophylactic therapy is not necessary for all patients with FL, idelalisib impairs the function of circulating lymphoid B-cells and thus has been associated with an increased risk of serious infection.10 A CPS can provide insight that maximizes medication adherence and efficacy while minimizing food-drug, drug-drug interactions, and AEs. CPS have been shown to: improve adherence to oral therapies, increase prospective monitoring required for safe therapy dose selection, and document assessment of chemotherapy-related AEs.11,12 Thus, multidisciplinary, integrated care is an important component of providing quality oncology care.
Case Example 3
A 60-year-old female presented to her PCP with a 2-week history of shortness of breath and leg swelling. She was treated for FL 4 years previously with 6 cycles of R-CHOP. She reported no chest pain and did not have a prior history of hypertension, DM, or heart disease. On physical exam, she had elevated jugular venous pressure to jaw at 45°, bilateral pulmonary rales, and 2+ pitting pretibial edema. Laboratory tests that included complete blood count, basic chemistries, and thyroid stimulating hormone were unremarkable, though brain natriuretic peptide (BNP) was elevated at 425 pg/mL.
As this patient’s laboratory results and physical examination suggested new-onset congestive heart failure, the PCP obtained an echocardiogram, which demonstrated an ejection fraction of 35% and global hypokinesis. Because the patient was symptomatic, she was admitted to the hospital to begin guideline-directed medical therapy (GDMT) including IV diuresis.
Discussion
Given the absence of significant risk factors and prior history of coronary artery disease, the most probable cause for this patient’s cardiomyopathy is doxorubicin. Doxorubicin is an anthracycline chemotherapy that can cause nonischemic, dilated cardiomyopathy, particularly when cumulative doses > 400 mg/m2 are administered, or when combined with chest radiation.13 This patient benefited from GDMT for reduced ejection-fraction heart failure (HFrEF). Studies have demonstrated positive outcomes when HFrEF patients are cared for by a multidisciplinary team who focus of volume management as well as uptitration of therapies to target doses.14
Case Example 4
An 80-year-old female was diagnosed with stage III FL but did not require immediate therapy. After developing discomfort due to enlarging lymphadenopathy, she initiated therapy with rituximab, cyclophosphamide, vincristine, and prednisone (R-CVP). She presented to her oncologist for consideration of her fifth cycle of R-CVP and reported a burning sensation on the soles of her feet and numbness in her fingertips and toes. On examination, her pulses were intact and there were no signs of infection, reduced blood flow, or edema. The patient demonstrated decreased sensation on monofilament testing. She had no history of DM and a recent HbA1c test was 4.9% An evaluation for other causes of neuropathy, such as hypothyroidism and vitamin B12 deficiency was negative. Thus, vincristine therapy was identified as the most likely etiology for her peripheral neuropathy. The oncologist decided to proceed with cycle 5 of chemotherapy but reduced the dose of vincristine by 50%.
Discussion
Vincristine is a microtubule inhibitor used in many chemotherapy regimens and may cause reversible or permanent neuropathy, including autonomic (constipation), sensory (stocking-glove distribution), or motor (foot-drop).15 A nerve conduction study may be indicated as part of the diagnostic evaluation. Treatment for painful sensory neuropathy may include pharmacologic therapy (such as gabapentin, pregabalin, capsaicin cream).16 Podiatrists can provide foot care and may provide shoes and inserts if appropriate. Physical therapists may assist with safety and mobility evaluations and can provide therapeutic exercises and assistive devices that improve function and quality of life.17
Conclusion
As cancer becomes more curable and more manageable, patients with cancer and survivors no longer rely exclusively on their oncologists for medical care. This is increasingly prevalent for patients with incurable but indolent cancers that may be present for years to decades, as acute and cumulative toxicities may complicate existing comorbidities. Thus, in this era of increasingly complex cancer therapies, multidisciplinary medical care that involves PCPs, specialists, and allied medical professionals, is essential for providing care that optimizes health and fully addresses patients’ needs.
Patients benefit from multidisciplinary care that coordinates management of complex medical problems. Traditionally, multidisciplinary cancer care involves oncology specialty providers in fields that include medical oncology, radiation oncology, and surgical oncology. Multidisciplinary cancer care intends to improve patient outcomes by bringing together different health care providers (HCPs) who are involved in the treatment of patients with cancer. Because new therapies are more effective and allow patients with cancer to live longer, adverse effects (AEs) are more likely to impact patients’ well-being, both while receiving treatment and long after it has completed. Thus, this population may benefit from an expanded approach to multidisciplinary care that includes input from specialty and primary care providers (PCPs), clinical pharmacy specialists (CPS), physical and occupational therapists, and patient navigators and educators.
We present 4 hypothetical cases, based on actual patients, that illustrate opportunities where multidisciplinary care coordination may improve patient experiences. These cases draw on current quality initiatives from the National Cancer Institute Community Cancer Centers Program, which has focused on improving the quality of multidisciplinary cancer care at selected community centers, and the Veterans Health Administration (VHA) patient-aligned care team (PACT) model, which brings together different health professionals to optimize primary care coordination.1,2 In addition, the National Committee for Quality Assurance has introduced an educational initiative to facilitate implementation of an oncologic medical home.3 This initiative stresses increased multidisciplinary communication, patient-centered care delivery, and reduced fragmentation of care for this population. Despite these guidelines and experiences from other medical specialties, models for integrated cancer care have not been implemented in a prospective fashion within the VHA.
In this article, we focus on opportunities to take collaborative care approaches for the treatment of patients with follicular lymphoma (FL): a common, incurable, and often indolent B-cell non-Hodgkin lymphoma.4 FL was selected because these patients may be treated numerous times and long-term sequalae can accumulate throughout their cancer continuum (a series of health events encompassing cancer screening, diagnosis, treatment, survivorship, relapse, and death).5 HCPs in distinct roles can assist patients with cancer in optimizing their health outcomes and overall wellbeing.6
Case Example 1
A 70-year-old male was diagnosed with stage IV FL. Because of his advanced disease, he began therapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone). Prednisone was administered at 100 mg daily on the first 5 days of each 21-day cycle. On day 4 of the first treatment cycle, the patient notified his oncologist that he had been very thirsty and his random blood sugar values on 2 different days were 283 mg/dL and 312 mg/dL. A laboratory review revealed his hemoglobin A1c (HbA1c) 7 months prior was 5.6%.
Discussion
The high-dose prednisone component of this and other lymphoma therapy regimens can worsen diabetes mellitus (DM) control and/or worsen prediabetes. Patient characteristics that increase the risk of developing glucocorticoid-induced DM after CHOP chemotherapy include age ≥ 60 years, HbA1c > 6.1%, and body mass index > 30.7 This patient did not have DM prior to the FL therapy initiation, but afterwards he met diagnostic criteria for DM. For completeness, other causes for elevated blood glucose should be ruled out (ie, infection, laboratory error, etc.). An oncologist often will triage acute hyperglycemia, treating immediately with IV fluids and/or insulin. Thereafter, ongoing chronic disease management for DM may be best managed by PCPs, certified DM educators, and registered dieticians.
Several programs involving multidisciplinary DM care, comprised of physicians, advanced practice providers, nurses, certified DM educators, and/or pharmacists have been shown to improve HbA1c, cardiovascular outcomes, and all-cause mortality, while reducing health care costs.8 In addition, patient navigators can assist patients with coordinating visits to disease-state specialists and identifying further educational needs. For example, in 1 program, nonclinical peer navigators were shown to improve the number of appointments attended and reduce HbA1c in a population of patients with DM who were primarily minority, urban, and of low socioeconomic status.9 Thus, integrating DM care shows potential to improve outcomes for patients with lymphoma who develop glucocorticoid
Case Example 2
A 75-year-old male was diagnosed with FL. He was treated initially with bendamustine and rituximab. He required reinitiation of therapy 20 months later when he developed lymphadenopathy, fatigue, and night sweats and began treatment with oral idelalisib, a second-line therapy. Later, the patient presented to his PCP for a routine visit, and on medication reconciliation review, the patient reported regular use of trimethoprim-sulfamethoxazole.
Discussion
Upon consultation with the CPS and the patient’s oncologist, the PCP confirmed trimethoprim-sulfamethoxazole should be continued during therapy and for about 6 months following completion of therapy. Trimethoprim-sulfamethoxazole is used for prophylaxis against Pneumocystis jirovecii (formerly Pneumocystis carinii). While use of prophylactic therapy is not necessary for all patients with FL, idelalisib impairs the function of circulating lymphoid B-cells and thus has been associated with an increased risk of serious infection.10 A CPS can provide insight that maximizes medication adherence and efficacy while minimizing food-drug, drug-drug interactions, and AEs. CPS have been shown to: improve adherence to oral therapies, increase prospective monitoring required for safe therapy dose selection, and document assessment of chemotherapy-related AEs.11,12 Thus, multidisciplinary, integrated care is an important component of providing quality oncology care.
Case Example 3
A 60-year-old female presented to her PCP with a 2-week history of shortness of breath and leg swelling. She was treated for FL 4 years previously with 6 cycles of R-CHOP. She reported no chest pain and did not have a prior history of hypertension, DM, or heart disease. On physical exam, she had elevated jugular venous pressure to jaw at 45°, bilateral pulmonary rales, and 2+ pitting pretibial edema. Laboratory tests that included complete blood count, basic chemistries, and thyroid stimulating hormone were unremarkable, though brain natriuretic peptide (BNP) was elevated at 425 pg/mL.
As this patient’s laboratory results and physical examination suggested new-onset congestive heart failure, the PCP obtained an echocardiogram, which demonstrated an ejection fraction of 35% and global hypokinesis. Because the patient was symptomatic, she was admitted to the hospital to begin guideline-directed medical therapy (GDMT) including IV diuresis.
Discussion
Given the absence of significant risk factors and prior history of coronary artery disease, the most probable cause for this patient’s cardiomyopathy is doxorubicin. Doxorubicin is an anthracycline chemotherapy that can cause nonischemic, dilated cardiomyopathy, particularly when cumulative doses > 400 mg/m2 are administered, or when combined with chest radiation.13 This patient benefited from GDMT for reduced ejection-fraction heart failure (HFrEF). Studies have demonstrated positive outcomes when HFrEF patients are cared for by a multidisciplinary team who focus of volume management as well as uptitration of therapies to target doses.14
Case Example 4
An 80-year-old female was diagnosed with stage III FL but did not require immediate therapy. After developing discomfort due to enlarging lymphadenopathy, she initiated therapy with rituximab, cyclophosphamide, vincristine, and prednisone (R-CVP). She presented to her oncologist for consideration of her fifth cycle of R-CVP and reported a burning sensation on the soles of her feet and numbness in her fingertips and toes. On examination, her pulses were intact and there were no signs of infection, reduced blood flow, or edema. The patient demonstrated decreased sensation on monofilament testing. She had no history of DM and a recent HbA1c test was 4.9% An evaluation for other causes of neuropathy, such as hypothyroidism and vitamin B12 deficiency was negative. Thus, vincristine therapy was identified as the most likely etiology for her peripheral neuropathy. The oncologist decided to proceed with cycle 5 of chemotherapy but reduced the dose of vincristine by 50%.
Discussion
Vincristine is a microtubule inhibitor used in many chemotherapy regimens and may cause reversible or permanent neuropathy, including autonomic (constipation), sensory (stocking-glove distribution), or motor (foot-drop).15 A nerve conduction study may be indicated as part of the diagnostic evaluation. Treatment for painful sensory neuropathy may include pharmacologic therapy (such as gabapentin, pregabalin, capsaicin cream).16 Podiatrists can provide foot care and may provide shoes and inserts if appropriate. Physical therapists may assist with safety and mobility evaluations and can provide therapeutic exercises and assistive devices that improve function and quality of life.17
Conclusion
As cancer becomes more curable and more manageable, patients with cancer and survivors no longer rely exclusively on their oncologists for medical care. This is increasingly prevalent for patients with incurable but indolent cancers that may be present for years to decades, as acute and cumulative toxicities may complicate existing comorbidities. Thus, in this era of increasingly complex cancer therapies, multidisciplinary medical care that involves PCPs, specialists, and allied medical professionals, is essential for providing care that optimizes health and fully addresses patients’ needs.
1. Friedman EL, Chawla N, Morris PT, et al. Assessing the development of multidisciplinary care: experience of the National Cancer Institute community cancer centers program. J Oncol Pract. 2015;11(1):e36-e43.
2. Peterson K, Helfand M, Humphrey L, Christensen V, Carson S. Evidence brief: effectiveness of intensive primary care programs. https://www.hsrd.research.va.gov/publications/esp/Intensive-Primary-Care-Supplement.pdf. Published February 2013. Accessed April 5, 2019.
3. National Committee for Quality Assurance. Oncology medical home recognition. https://www.ncqa.org/programs/health-care-providers-practices/oncology-medical-home. Accessed April 5, 2019.
4. Kahl BS, Yang DT. Follicular lymphoma: evolving therapeutic strategies. Blood. 2016;127(17):2055-2063.
5. Dulaney C, Wallace AS, Everett AS, Dover L, McDonald A, Kropp L. Defining health across the cancer continuum. Cureus. 2017;9(2):e1029.
6. Hopkins J, Mumber MP. Patient navigation through the cancer care continuum: an overview. J Oncol Pract. 2009;5(4):150-152.
7. Lee SY, Kurita N, Yokoyama Y, et al. Glucocorticoid-induced diabetes mellitus in patients with lymphoma treated with CHOP chemotherapy. Support Care Cancer. 2014;22(5):1385-1390.
8. McGill M, Blonde L, Juliana CN, et al; Global Partnership for Effective Diabetes Management. The interdisciplinary team in type 2 diabetes management: challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. 2017;7:21-27.
9. Horný M, Glover W, Gupte G, Saraswat A, Vimalananda V, Rosenzweig J. Patient navigation to improve diabetes outpatient care at a safety-net hospital: a retrospective cohort study. BMC Health Serv Res. 2017;17(1):759.
10. Reinwald M, Silva JT, Mueller NJ, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Intracellular signaling pathways: tyrosine kinase and mTOR inhibitors). Clin Microbiol Infect. 2018;24(suppl 2):S53-S70.
11. Holle LM, Boehnke Michaud L. Oncology pharmacists in health care delivery: vital members of the cancer care team. J. Oncol. Pract. 2014;10(3):e142-e145.
12. Morgan KP, Muluneh B, Dean AM, Amerine LB. Impact of an integrated oral chemotherapy program on patient adherence. J Oncol Pharm Pract. 2018;24(5):332-336.
13. Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869-2879.
14. Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774-784.
15. Mora E, Smith EM, Donohoe C, Hertz DL. Vincristine-induced peripheral neuropathy in pediatric cancer patients. Am J Cancer Res. 2016;6(11):2416-2430.
16. Hershman DL, Lacchetti C, Dworkin RH, et al; American Society of Clinical Oncology. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(18):1941–1967
17. Duregon F, Vendramin B, Bullo V, et al. Effects of exercise on cancer patients suffering chemotherapy-induced peripheral neuropathy undergoing treatment: a systematic review. Crit Rev Oncol Hematol. 2018;121:90-100.
1. Friedman EL, Chawla N, Morris PT, et al. Assessing the development of multidisciplinary care: experience of the National Cancer Institute community cancer centers program. J Oncol Pract. 2015;11(1):e36-e43.
2. Peterson K, Helfand M, Humphrey L, Christensen V, Carson S. Evidence brief: effectiveness of intensive primary care programs. https://www.hsrd.research.va.gov/publications/esp/Intensive-Primary-Care-Supplement.pdf. Published February 2013. Accessed April 5, 2019.
3. National Committee for Quality Assurance. Oncology medical home recognition. https://www.ncqa.org/programs/health-care-providers-practices/oncology-medical-home. Accessed April 5, 2019.
4. Kahl BS, Yang DT. Follicular lymphoma: evolving therapeutic strategies. Blood. 2016;127(17):2055-2063.
5. Dulaney C, Wallace AS, Everett AS, Dover L, McDonald A, Kropp L. Defining health across the cancer continuum. Cureus. 2017;9(2):e1029.
6. Hopkins J, Mumber MP. Patient navigation through the cancer care continuum: an overview. J Oncol Pract. 2009;5(4):150-152.
7. Lee SY, Kurita N, Yokoyama Y, et al. Glucocorticoid-induced diabetes mellitus in patients with lymphoma treated with CHOP chemotherapy. Support Care Cancer. 2014;22(5):1385-1390.
8. McGill M, Blonde L, Juliana CN, et al; Global Partnership for Effective Diabetes Management. The interdisciplinary team in type 2 diabetes management: challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. 2017;7:21-27.
9. Horný M, Glover W, Gupte G, Saraswat A, Vimalananda V, Rosenzweig J. Patient navigation to improve diabetes outpatient care at a safety-net hospital: a retrospective cohort study. BMC Health Serv Res. 2017;17(1):759.
10. Reinwald M, Silva JT, Mueller NJ, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Intracellular signaling pathways: tyrosine kinase and mTOR inhibitors). Clin Microbiol Infect. 2018;24(suppl 2):S53-S70.
11. Holle LM, Boehnke Michaud L. Oncology pharmacists in health care delivery: vital members of the cancer care team. J. Oncol. Pract. 2014;10(3):e142-e145.
12. Morgan KP, Muluneh B, Dean AM, Amerine LB. Impact of an integrated oral chemotherapy program on patient adherence. J Oncol Pharm Pract. 2018;24(5):332-336.
13. Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869-2879.
14. Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774-784.
15. Mora E, Smith EM, Donohoe C, Hertz DL. Vincristine-induced peripheral neuropathy in pediatric cancer patients. Am J Cancer Res. 2016;6(11):2416-2430.
16. Hershman DL, Lacchetti C, Dworkin RH, et al; American Society of Clinical Oncology. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(18):1941–1967
17. Duregon F, Vendramin B, Bullo V, et al. Effects of exercise on cancer patients suffering chemotherapy-induced peripheral neuropathy undergoing treatment: a systematic review. Crit Rev Oncol Hematol. 2018;121:90-100.
Hedgehog signaling offers prognostic, therapeutic potential in CLL
Activation of hedgehog (Hh) signaling could predict early disease progression in chronic lymphocytic leukemia (CLL) and offer a new therapeutic target, according to investigators.
Approximately 11% of treatment-naive patients had mutations associated with Hh signaling, reported lead author Emanuela M. Ghia, PhD, of the University of California, San Diego, and colleagues. In addition to early progression, Hh signaling was associated with expression of GLI1, which could be a future therapeutic target. In support of this possibility, in vitro experimentation with a GLI1 inhibitor showed high cytotoxicity for GLI1-positive CLL cells.
“Targeting GLI1 could block ligand-independent and ligand-dependent Hh pathway activation and perhaps overcome the apparent resistance to SMO inhibitors,” the investigators wrote in Blood.
Using the HALT Pan-Leukemia Gene Panel, which includes 103 genes, the investigators tested for mutations in cell samples from 841 patients with treatment-naive CLL. Specifically, the investigators focused on mutations that did not map to seven well-known signaling/metabolic pathways, such as Wnt and Notch.
This strategy revealed that 89 patients (11%) had nonsynonymous mutations in genes that drive Hh signaling. These mutations were highly associated with GLI1 expression (x2 test; P less than .0001), which stands to reason, as GLI1 is the main effector of the Hh signaling pathway. Of note, 62 of the 161 patients (38%) who did not test positive for an Hh pathway mutation still tested positive for GLI1, suggesting that they had Hh pathway activation, albeit without an identifiable mutational cause.
These findings are clinically significant, as GLI1 overexpression has been linked to numerous types of cancer and is an adverse prognostic indicator for acute myeloid leukemia and several carcinomas, the investigators wrote.
Considering these associations with other cancer types, the investigators looked for a relationship between GLI1 expression and outcomes in CLL. Comparing 103 patients with GLI1-positive disease with 107 GLI-negative patients revealed that GLI1 positivity was significantly associated with shorter median treatment-free survival (4.7 vs. 6.4 years; P = .002). Additional analysis showed that this prognostic relationship was present regardless of IgVH mutational status.
Based on these findings, the investigators concluded that “[a]ctivation of the Hh pathway can strongly influence disease progression in CLL.”
Two additional tests showed that GLI1-positivity was associated with cell survival. First, silencing GLI1 with a GLI1-specific small interfering RNA led to decreased cell viability. Second, GANT61, a small molecule inhibitor of GLI1, was highly cytotoxic for GLI1-positive cells. According to the investigators, these findings suggest that GLI1 could be a future therapeutic target.
“[T]his report shows that the Hh pathway frequently is activated in CLL and associated with relatively rapid disease progression, while identifying a new avenue for therapeutic intervention for patients with this disease,” they concluded.
The study was funded by the National Institutes of Health, the Cancer Stem Cell Consortium, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other groups. The investigators reported having no competing financial interests.
SOURCE: Ghia EM et al. Blood. 2019 Jun 20;133(25):2651-63.
Activation of hedgehog (Hh) signaling could predict early disease progression in chronic lymphocytic leukemia (CLL) and offer a new therapeutic target, according to investigators.
Approximately 11% of treatment-naive patients had mutations associated with Hh signaling, reported lead author Emanuela M. Ghia, PhD, of the University of California, San Diego, and colleagues. In addition to early progression, Hh signaling was associated with expression of GLI1, which could be a future therapeutic target. In support of this possibility, in vitro experimentation with a GLI1 inhibitor showed high cytotoxicity for GLI1-positive CLL cells.
“Targeting GLI1 could block ligand-independent and ligand-dependent Hh pathway activation and perhaps overcome the apparent resistance to SMO inhibitors,” the investigators wrote in Blood.
Using the HALT Pan-Leukemia Gene Panel, which includes 103 genes, the investigators tested for mutations in cell samples from 841 patients with treatment-naive CLL. Specifically, the investigators focused on mutations that did not map to seven well-known signaling/metabolic pathways, such as Wnt and Notch.
This strategy revealed that 89 patients (11%) had nonsynonymous mutations in genes that drive Hh signaling. These mutations were highly associated with GLI1 expression (x2 test; P less than .0001), which stands to reason, as GLI1 is the main effector of the Hh signaling pathway. Of note, 62 of the 161 patients (38%) who did not test positive for an Hh pathway mutation still tested positive for GLI1, suggesting that they had Hh pathway activation, albeit without an identifiable mutational cause.
These findings are clinically significant, as GLI1 overexpression has been linked to numerous types of cancer and is an adverse prognostic indicator for acute myeloid leukemia and several carcinomas, the investigators wrote.
Considering these associations with other cancer types, the investigators looked for a relationship between GLI1 expression and outcomes in CLL. Comparing 103 patients with GLI1-positive disease with 107 GLI-negative patients revealed that GLI1 positivity was significantly associated with shorter median treatment-free survival (4.7 vs. 6.4 years; P = .002). Additional analysis showed that this prognostic relationship was present regardless of IgVH mutational status.
Based on these findings, the investigators concluded that “[a]ctivation of the Hh pathway can strongly influence disease progression in CLL.”
Two additional tests showed that GLI1-positivity was associated with cell survival. First, silencing GLI1 with a GLI1-specific small interfering RNA led to decreased cell viability. Second, GANT61, a small molecule inhibitor of GLI1, was highly cytotoxic for GLI1-positive cells. According to the investigators, these findings suggest that GLI1 could be a future therapeutic target.
“[T]his report shows that the Hh pathway frequently is activated in CLL and associated with relatively rapid disease progression, while identifying a new avenue for therapeutic intervention for patients with this disease,” they concluded.
The study was funded by the National Institutes of Health, the Cancer Stem Cell Consortium, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other groups. The investigators reported having no competing financial interests.
SOURCE: Ghia EM et al. Blood. 2019 Jun 20;133(25):2651-63.
Activation of hedgehog (Hh) signaling could predict early disease progression in chronic lymphocytic leukemia (CLL) and offer a new therapeutic target, according to investigators.
Approximately 11% of treatment-naive patients had mutations associated with Hh signaling, reported lead author Emanuela M. Ghia, PhD, of the University of California, San Diego, and colleagues. In addition to early progression, Hh signaling was associated with expression of GLI1, which could be a future therapeutic target. In support of this possibility, in vitro experimentation with a GLI1 inhibitor showed high cytotoxicity for GLI1-positive CLL cells.
“Targeting GLI1 could block ligand-independent and ligand-dependent Hh pathway activation and perhaps overcome the apparent resistance to SMO inhibitors,” the investigators wrote in Blood.
Using the HALT Pan-Leukemia Gene Panel, which includes 103 genes, the investigators tested for mutations in cell samples from 841 patients with treatment-naive CLL. Specifically, the investigators focused on mutations that did not map to seven well-known signaling/metabolic pathways, such as Wnt and Notch.
This strategy revealed that 89 patients (11%) had nonsynonymous mutations in genes that drive Hh signaling. These mutations were highly associated with GLI1 expression (x2 test; P less than .0001), which stands to reason, as GLI1 is the main effector of the Hh signaling pathway. Of note, 62 of the 161 patients (38%) who did not test positive for an Hh pathway mutation still tested positive for GLI1, suggesting that they had Hh pathway activation, albeit without an identifiable mutational cause.
These findings are clinically significant, as GLI1 overexpression has been linked to numerous types of cancer and is an adverse prognostic indicator for acute myeloid leukemia and several carcinomas, the investigators wrote.
Considering these associations with other cancer types, the investigators looked for a relationship between GLI1 expression and outcomes in CLL. Comparing 103 patients with GLI1-positive disease with 107 GLI-negative patients revealed that GLI1 positivity was significantly associated with shorter median treatment-free survival (4.7 vs. 6.4 years; P = .002). Additional analysis showed that this prognostic relationship was present regardless of IgVH mutational status.
Based on these findings, the investigators concluded that “[a]ctivation of the Hh pathway can strongly influence disease progression in CLL.”
Two additional tests showed that GLI1-positivity was associated with cell survival. First, silencing GLI1 with a GLI1-specific small interfering RNA led to decreased cell viability. Second, GANT61, a small molecule inhibitor of GLI1, was highly cytotoxic for GLI1-positive cells. According to the investigators, these findings suggest that GLI1 could be a future therapeutic target.
“[T]his report shows that the Hh pathway frequently is activated in CLL and associated with relatively rapid disease progression, while identifying a new avenue for therapeutic intervention for patients with this disease,” they concluded.
The study was funded by the National Institutes of Health, the Cancer Stem Cell Consortium, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other groups. The investigators reported having no competing financial interests.
SOURCE: Ghia EM et al. Blood. 2019 Jun 20;133(25):2651-63.
FROM BLOOD
BET inhibitors may target oncogene in ABC-like DLBCL
(ABC-like DLBCL).
Researchers found the TCF4 (E2-2) transcription factor is an oncogene in ABC-like DLBCL, and TCF4 can be targeted via BET inhibition.
The BET protein degrader ARV771 reduced TCF4 expression and exhibited activity against ABC-like DLBCL in vitro and in vivo.
Neeraj Jain, PhD, of the University of Texas MD Anderson Cancer Center in Houston and colleagues reported these findings in Science Translational Medicine.
The researchers performed a genomic analysis of 1,000 DLBCL tumors and discovered that gains of 18q21.2 were the most frequent genetic alteration in ABC-like DLBCL. In analyzing another 249 tumors, the researchers found that TCF4 was the target of the 18q21.2 gains.
Additional experiments with primary DLBCL tumors and DLBCL cell lines indicated that TCF4 regulates IGHM and MYC expression. The researchers also found that the TCF4 gene was “one of the most highly BRD4-loaded genes in DLBCL,” and knocking down BRD4 in DLBCL cell lines reduced TCF4 expression.
These findings prompted the team to test small-molecule BET inhibitors – JQ1 and OTX015 – and a BET protein degrader – ARV771 – in ABC-like DLBCL cell lines with a high TCF4 copy number.
Treatment with JQ1 and OTX015 resulted in upregulation of BRD4, but ARV771 treatment did not. As a result, subsequent experiments were performed with ARV771.
The researchers found that ARV771 induced apoptosis in the cell lines and reduced the expression of TCF4, IgM, and MYC. However, enforced TCF4 expression during ARV771 treatment rescued IgM and MYC expression. This suggests that “reduction of TCF4 is one of the mechanisms by which BET inhibition reduces IgM and MYC expression and induces apoptosis,” according to the researchers.
The team also tested ARV771 in mouse models of ABC-like DLBCL with high TCF4 expression. ARV771 significantly reduced tumor growth and prolonged survival (P less than .05 for both), and there were no signs of toxicity in ARV771-treated mice.
“Our data provide a clear functional rationale for BET inhibition in ABC-like DLBCL,” the researchers wrote. They did note, however, that BCL2 overexpression is associated with resistance to BET inhibitors, and most of the 18q DNA copy number gains the researchers observed in DLBCL encompass TCF4 and BCL2. The team therefore theorized that combining a BET inhibitor with a BCL2 inhibitor could be a promising treatment approach in ABC-like DLBCL and is worthy of further investigation.
This research was supported by the Nebraska Department of Health & Human Services, the Schweitzer Family Fund, the Fred & Pamela Buffet Cancer Center Support Grant, and the MD Anderson Cancer Center NCI CORE Grant. The authors reported having no conflicts of interest related to the study.
SOURCE: Jain N et al. Sci. Transl. Med. 2019 Jun 19. doi: 10.1126/scitranslmed.aav5599.
(ABC-like DLBCL).
Researchers found the TCF4 (E2-2) transcription factor is an oncogene in ABC-like DLBCL, and TCF4 can be targeted via BET inhibition.
The BET protein degrader ARV771 reduced TCF4 expression and exhibited activity against ABC-like DLBCL in vitro and in vivo.
Neeraj Jain, PhD, of the University of Texas MD Anderson Cancer Center in Houston and colleagues reported these findings in Science Translational Medicine.
The researchers performed a genomic analysis of 1,000 DLBCL tumors and discovered that gains of 18q21.2 were the most frequent genetic alteration in ABC-like DLBCL. In analyzing another 249 tumors, the researchers found that TCF4 was the target of the 18q21.2 gains.
Additional experiments with primary DLBCL tumors and DLBCL cell lines indicated that TCF4 regulates IGHM and MYC expression. The researchers also found that the TCF4 gene was “one of the most highly BRD4-loaded genes in DLBCL,” and knocking down BRD4 in DLBCL cell lines reduced TCF4 expression.
These findings prompted the team to test small-molecule BET inhibitors – JQ1 and OTX015 – and a BET protein degrader – ARV771 – in ABC-like DLBCL cell lines with a high TCF4 copy number.
Treatment with JQ1 and OTX015 resulted in upregulation of BRD4, but ARV771 treatment did not. As a result, subsequent experiments were performed with ARV771.
The researchers found that ARV771 induced apoptosis in the cell lines and reduced the expression of TCF4, IgM, and MYC. However, enforced TCF4 expression during ARV771 treatment rescued IgM and MYC expression. This suggests that “reduction of TCF4 is one of the mechanisms by which BET inhibition reduces IgM and MYC expression and induces apoptosis,” according to the researchers.
The team also tested ARV771 in mouse models of ABC-like DLBCL with high TCF4 expression. ARV771 significantly reduced tumor growth and prolonged survival (P less than .05 for both), and there were no signs of toxicity in ARV771-treated mice.
“Our data provide a clear functional rationale for BET inhibition in ABC-like DLBCL,” the researchers wrote. They did note, however, that BCL2 overexpression is associated with resistance to BET inhibitors, and most of the 18q DNA copy number gains the researchers observed in DLBCL encompass TCF4 and BCL2. The team therefore theorized that combining a BET inhibitor with a BCL2 inhibitor could be a promising treatment approach in ABC-like DLBCL and is worthy of further investigation.
This research was supported by the Nebraska Department of Health & Human Services, the Schweitzer Family Fund, the Fred & Pamela Buffet Cancer Center Support Grant, and the MD Anderson Cancer Center NCI CORE Grant. The authors reported having no conflicts of interest related to the study.
SOURCE: Jain N et al. Sci. Transl. Med. 2019 Jun 19. doi: 10.1126/scitranslmed.aav5599.
(ABC-like DLBCL).
Researchers found the TCF4 (E2-2) transcription factor is an oncogene in ABC-like DLBCL, and TCF4 can be targeted via BET inhibition.
The BET protein degrader ARV771 reduced TCF4 expression and exhibited activity against ABC-like DLBCL in vitro and in vivo.
Neeraj Jain, PhD, of the University of Texas MD Anderson Cancer Center in Houston and colleagues reported these findings in Science Translational Medicine.
The researchers performed a genomic analysis of 1,000 DLBCL tumors and discovered that gains of 18q21.2 were the most frequent genetic alteration in ABC-like DLBCL. In analyzing another 249 tumors, the researchers found that TCF4 was the target of the 18q21.2 gains.
Additional experiments with primary DLBCL tumors and DLBCL cell lines indicated that TCF4 regulates IGHM and MYC expression. The researchers also found that the TCF4 gene was “one of the most highly BRD4-loaded genes in DLBCL,” and knocking down BRD4 in DLBCL cell lines reduced TCF4 expression.
These findings prompted the team to test small-molecule BET inhibitors – JQ1 and OTX015 – and a BET protein degrader – ARV771 – in ABC-like DLBCL cell lines with a high TCF4 copy number.
Treatment with JQ1 and OTX015 resulted in upregulation of BRD4, but ARV771 treatment did not. As a result, subsequent experiments were performed with ARV771.
The researchers found that ARV771 induced apoptosis in the cell lines and reduced the expression of TCF4, IgM, and MYC. However, enforced TCF4 expression during ARV771 treatment rescued IgM and MYC expression. This suggests that “reduction of TCF4 is one of the mechanisms by which BET inhibition reduces IgM and MYC expression and induces apoptosis,” according to the researchers.
The team also tested ARV771 in mouse models of ABC-like DLBCL with high TCF4 expression. ARV771 significantly reduced tumor growth and prolonged survival (P less than .05 for both), and there were no signs of toxicity in ARV771-treated mice.
“Our data provide a clear functional rationale for BET inhibition in ABC-like DLBCL,” the researchers wrote. They did note, however, that BCL2 overexpression is associated with resistance to BET inhibitors, and most of the 18q DNA copy number gains the researchers observed in DLBCL encompass TCF4 and BCL2. The team therefore theorized that combining a BET inhibitor with a BCL2 inhibitor could be a promising treatment approach in ABC-like DLBCL and is worthy of further investigation.
This research was supported by the Nebraska Department of Health & Human Services, the Schweitzer Family Fund, the Fred & Pamela Buffet Cancer Center Support Grant, and the MD Anderson Cancer Center NCI CORE Grant. The authors reported having no conflicts of interest related to the study.
SOURCE: Jain N et al. Sci. Transl. Med. 2019 Jun 19. doi: 10.1126/scitranslmed.aav5599.
FROM SCIENCE TRANSLATIONAL MEDICINE
Bispecific CAR T-cell therapy yields complete responses in relapsed/refractory non-Hodgkin lymphomas
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
REPORTING FROM ASCO 2019
Psoriasis Treatment in Patients With Human Immunodeficiency Virus
The treatment of psoriasis in patients with HIV infection represents a clinical challenge.1,2 Up to 3% of patients with HIV infection are estimated to have psoriasis. Although this prevalence is similar to the general population, psoriatic disease in patients with HIV tends to be more severe, refractory, and more difficult to treat.3-5 Additionally, up to half of patients with comorbid HIV and psoriasis also have substantial psoriatic arthritis (PsA).1,6
Drug treatments for psoriasis and PsA often are immunosuppressive; as such, the treatment of psoriasis in this patient population requires careful consideration of the potential risks and benefits of treatment as well as fastidious monitoring for the emergence of potentially adverse treatment effects.1 A careful diagnostic process to determine the severity of HIV-associated psoriasis and to select the appropriate treatment relative to the patient’s immunologic status is of critical importance.3
Presentation of Psoriasis in Patients With HIV Infection
The presentation and severity of psoriasis in patients with HIV infection is highly variable and is often related to the degree of immune suppression experienced by the patient.3,7 In some individuals, psoriasis may be the first outward manifestation of HIV, whereas in others, it only manifests after HIV has progressed to AIDS.7
Recognition of the atypical presentations of psoriasis that are frequently seen in patients with HIV infection can help to facilitate early diagnosis and treatment to improve patient outcomes.3,8 Psoriasis vulgaris, for example, typically presents as erythematous plaques with silvery-white scales on extensor surfaces of the body such as the knees and elbows. However, in patients with HIV, psoriasis vulgaris may present with scales that appear thick and oyster shell–like instead of silvery-white; these lesions also may occur on flexural areas rather than extensor surfaces.8 Similarly, the sudden onset of widespread psoriasis in otherwise healthy persons should trigger suspicion for HIV infection and recommendations for appropriate testing, even when no risk factors are present.8

Guttate, inverse, and erythrodermic psoriasis are the most common subtypes in patients with HIV infection, though all clinical subtypes may occur. Overlapping of psoriasis subtypes often occurs in individuals with HIV infection and should serve as a red flag to recommend screening for HIV.5,8 Acral involvement, frequently with pustules and occasionally with severe destructive nail changes, is commonly seen in patients with HIV-associated psoriasis.7,9 In cases involving severe psoriatic exacerbations among individuals with AIDS, there is a heightened risk of developing systemic infections, including superinfection of Staphylococcus aureus, which is a rare occurrence in immunocompetent patients with psoriasis.7,10,11
Therapeutic Options
Because the clinical course of psoriasis in patients with HIV infection is frequently progressive and refractory to treatment, traditional first- and second-line therapies (Table) including topical agents, phototherapy, and oral retinoids may be unable to achieve lasting control of both skin and joint manifestations.1
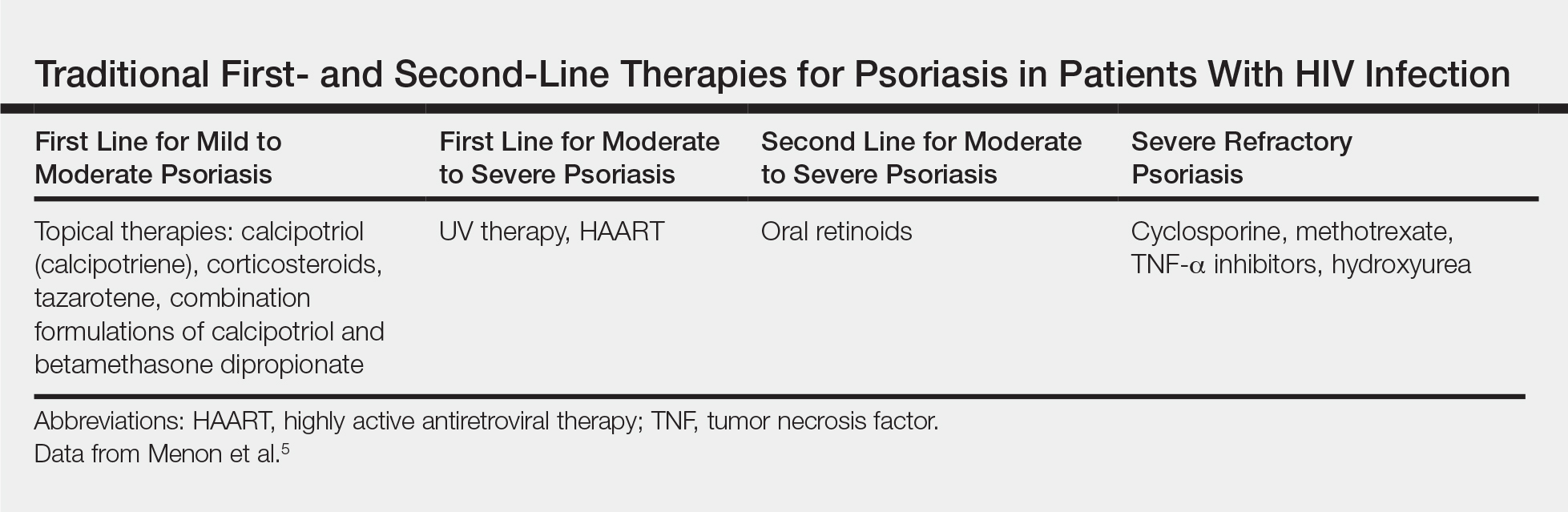
Topical Therapy
As in the general population, targeted therapies such as topical agents are recommended as first-line treatment of mild HIV-associated psoriasis.12 Topical corticosteroids, calcipotriol, tazarotene, and formulations combining 2 of these medications form the cornerstone of topical therapies for mild psoriasis in patients with HIV infection. These agents have the advantage of possessing limited and localized effects, making it unlikely for them to increase immunosuppression in patients with HIV infection. They generally can be safely used in patients with HIV infection, and their side-effect profile in patients with HIV infection is similar to the general population.12 However, calcipotriol is the least desirable for use in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4
UV Phototherapy
Topical therapy is limited by its lack of potency; limited field coverage; and the inconvenience of application, particularly in patients with more widespread disease.12 Therefore, UV phototherapy is preferred as first-line treatment of moderate to severe psoriasis. UV phototherapy has been shown to inhibit cell proliferation and inflammation and result in clinical improvement of HIV-associated psoriasis; moreover, most of the reports in the literature support it as an option that will not increase immunocompromise in patients with HIV infection.12
Caution is warranted, however, regarding the immunomodulatory effects of UV therapies, which may result in an increased risk for skin cancer and diminished resistance to infection, which can be of particular concern in immunocompromised patients who are already at risk.7,13,14 In patients who are candidates for phototherapy, HIV serology and close monitoring of viral load and CD4 lymphocyte count before treatment, at monthly interludes throughout treatment, and 3 months following the cessation of treatment have been recommended.7,15 Careful consideration of the risk-benefit ratio of phototherapy for individual patients, including the patient’s stage of HIV disease, the degree of discomfort, disfigurement, and disability caused by the psoriasis (or other dermatologic condition), as well as the availability of alternative treatment options is essential.7,16
Systemic Agents
In patients who are intolerant of or unresponsive to antiretroviral therapy, topical therapies, and phototherapy, traditional systemic agents may be considered,12 including acitretin, methotrexate, and cyclosporine. However, updated guidelines indicate that methotrexate and cyclosporine should be avoided in this population given the risk for increased immunosuppression with these agents.4,17
Oral retinoids, such as acitretin, continue to be important options for second-line psoriasis treatment in patients with comorbid HIV infection, either as monotherapy or in association with phototherapy.3 Acitretin has the notable benefit of not causing or worsening immune compromise; however, its use is less than desirable in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4,12 Providers also must be aware of the possible association between acitretin (and other antiretrovirals) and pancreatitis, remaining vigilant in monitoring patients for this adverse effect.3
Biologics
The relatively recent addition of cytokine-suppressive biologic agents to the treatment armamentarium has transformed the management of psoriasis in otherwise healthy individuals. These agents have been shown to possess an excellent safety and efficacy profile.12 However, their use in patients with HIV infection has been mired in concerns regarding a potential increase in the risk for opportunistic infections, sepsis, and HIV disease progression in this patient population.7,12
Case reports have detailed the safe treatment of recalcitrant HIV-associated psoriasis with tumor necrosis factor (TNF) blockers, such as etanercept.7,12 In most of these case reports, no harm to CD4 lymphocyte counts, serum viral loads, overall immune status, and susceptibility to infection have been noted; on the contrary, CD4 count increased in most patients following treatment with biologic agents.12 Because patients with HIV infection tend to be excluded from clinical trials, anecdotal evidence derived from case reports and case series often provides clinically relevant information and often forms the basis for treatment recommendations in this patient population.12 Indeed, in the wake of positive case reports, TNF-α inhibitors are now recommended for highly selected patients with refractory chronic psoriatic disease, including those with incapacitating joint pain.7,18
When TNF-α inhibitors are used in patients with HIV infection and psoriasis, optimal antiretroviral therapy and exceedingly close monitoring of clinical and laboratory parameters are of the utmost importance; Pneumocystis jiroveci prophylaxis also is recommended in patients with low CD4 counts.7,18
In 2014, the oral phosphodiesterase 4 inhibitor apremilast was approved for the treatment of moderate to severe plaque psoriasis and PsA. Recent case reports have described its successful use in patients with HIV infection and psoriasis, including the case reported herein, with no reports of opportunistic infections.4,19 Furthermore, HIV infection is not listed as a contraindication on its label.20
Apremilast is thought to increase intracellular cyclic adenosine monophosphate, thereby helping to attain improved homeostasis between proinflammatory and anti-inflammatory mediators.4,19 Several of the proinflammatory mediators that are indirectly targeted by apremilast, including TNF-α and IL-23, are explicitly inhibited by other biologics. It is this equilibrium between proinflammatory and anti-inflammatory mediators that most markedly differentiates apremilast from most other available biologic therapies for psoriasis, which typically have a specific proinflammatory target.4,21 As with other systemic therapies, close monitoring of CD4 levels and viral loads, as well as use of relevant prophylactic agents, is essential when apremilast is used in the setting of HIV infection, making coordination with infectious disease specialists essential.19
Bottom Line
Management of psoriasis in patients with HIV infection represents a clinical challenge. Case reports suggest a role for apremilast as an adjuvant to first-line therapy such as UV phototherapy in the setting of HIV infection in a patient with moderate to severe psoriasis, but close monitoring of CD4 count and viral load in these patients is needed in collaboration with infectious disease specialists. Updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population are needed.
- Nakamura M, Abrouk M, Farahnik B, et al. Psoriasis treatment in HIV-positive patients: a systematic review of systemic immunosuppressive therapies. Cutis. 2018;101:38, 42, 56.
- Patel RV, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 2: review of treatment. Cutis. 2008;82:202-210.
- Ceccarelli M, Venanzi Rullo E, Vaccaro M, et al. HIV‐associated psoriasis: epidemiology, pathogenesis, and management [published online January 6, 2019]. Dermatol Ther. 2019;32:e12806. doi:10.1111/dth.12806.
- Zarbafian M, Richer V. Treatment of moderate to severe psoriasis with apremilast over 2 years in the context of long-term treated HIV infection: a case report. SAGE Open Med Case Rep. 2019;7:2050313X19845193. doi:10.1177/2050313X19845193.
- Menon K, Van Vorhees AS, Bebo, BF, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Mallon E, Bunker CB. HIV-associated psoriasis. AIDS Patient Care STDS. 2000;14:239-246.
- Patel VA, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 1: review of pathogenesis. Cutis. 2008;82:117-122.
- Castillo RL, Racaza GZ, Dela Cruz Roa F. Ostraceous and inverse psoriasis with psoriatic arthritis as the presenting features of advanced HIV infection. Singapore Med J. 2014;55:e60-e63.
- Duvic M, Crane MM, Conant M, et al. Zidovudine improves psoriasis in human immunodeficiency virus- positive males. Arch Dermatol. 1994;130:447.
- Jaffee D, May LP, Sanchez M, et al. Staphylococcal sepsis in HIV antibody seropositive psoriasis patients. J Am Acad Dermatol. 1991;24:970-972.
- King LE, Dufresne RG, Lovette GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
- Kaminetsky J, Aziz M, Kaushik S. A review of biologics and other treatment modalities in HIV-associated psoriasis. Skin. 2018;2:389-401.
- Wolff K. Side effects of psoralen photochemotherapy (PUVA). Br J Dermatol. 1990;122:117-125.
- Stern RS, Mills DK, Krell K, et al. HIV-positive patients differ from HIV-negative patients in indications for and type of UV therapy used. J Am Acad Dermatol. 1998;39:48-55.
- Oracion RM, Skiest DJ, Keiser PH, et al. HIV-related skin diseases. Prog Dermatol. 1999;33:1-6.
- Finkelstein M, Berman B. HIV and AIDS in inpatient dermatology: approach to the consultation. Dermatol Clin. 2000;18:509-520.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections. J Am Acad Dermatol. 2019;80:43-53.
- Sellam J, Bouvard B, Masson C, et al. Use of infliximab to treat psoriatic arthritis in HIV-positive patients. Joint Bone Spine. 2007;74:197-200.
- Reddy SP, Lee E, Wu JJ. Apremilast and phototherapy for treatment of psoriasis in a patient with human immunodeficiency virus. Cutis. 2019;103:E1-E7.
- Otezla (apremilast). Summit, NJ: Celgene Corporation; 2017.
- Schafer P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem Pharmacol. 2012;83:1583-1590.
The treatment of psoriasis in patients with HIV infection represents a clinical challenge.1,2 Up to 3% of patients with HIV infection are estimated to have psoriasis. Although this prevalence is similar to the general population, psoriatic disease in patients with HIV tends to be more severe, refractory, and more difficult to treat.3-5 Additionally, up to half of patients with comorbid HIV and psoriasis also have substantial psoriatic arthritis (PsA).1,6
Drug treatments for psoriasis and PsA often are immunosuppressive; as such, the treatment of psoriasis in this patient population requires careful consideration of the potential risks and benefits of treatment as well as fastidious monitoring for the emergence of potentially adverse treatment effects.1 A careful diagnostic process to determine the severity of HIV-associated psoriasis and to select the appropriate treatment relative to the patient’s immunologic status is of critical importance.3
Presentation of Psoriasis in Patients With HIV Infection
The presentation and severity of psoriasis in patients with HIV infection is highly variable and is often related to the degree of immune suppression experienced by the patient.3,7 In some individuals, psoriasis may be the first outward manifestation of HIV, whereas in others, it only manifests after HIV has progressed to AIDS.7
Recognition of the atypical presentations of psoriasis that are frequently seen in patients with HIV infection can help to facilitate early diagnosis and treatment to improve patient outcomes.3,8 Psoriasis vulgaris, for example, typically presents as erythematous plaques with silvery-white scales on extensor surfaces of the body such as the knees and elbows. However, in patients with HIV, psoriasis vulgaris may present with scales that appear thick and oyster shell–like instead of silvery-white; these lesions also may occur on flexural areas rather than extensor surfaces.8 Similarly, the sudden onset of widespread psoriasis in otherwise healthy persons should trigger suspicion for HIV infection and recommendations for appropriate testing, even when no risk factors are present.8

Guttate, inverse, and erythrodermic psoriasis are the most common subtypes in patients with HIV infection, though all clinical subtypes may occur. Overlapping of psoriasis subtypes often occurs in individuals with HIV infection and should serve as a red flag to recommend screening for HIV.5,8 Acral involvement, frequently with pustules and occasionally with severe destructive nail changes, is commonly seen in patients with HIV-associated psoriasis.7,9 In cases involving severe psoriatic exacerbations among individuals with AIDS, there is a heightened risk of developing systemic infections, including superinfection of Staphylococcus aureus, which is a rare occurrence in immunocompetent patients with psoriasis.7,10,11
Therapeutic Options
Because the clinical course of psoriasis in patients with HIV infection is frequently progressive and refractory to treatment, traditional first- and second-line therapies (Table) including topical agents, phototherapy, and oral retinoids may be unable to achieve lasting control of both skin and joint manifestations.1
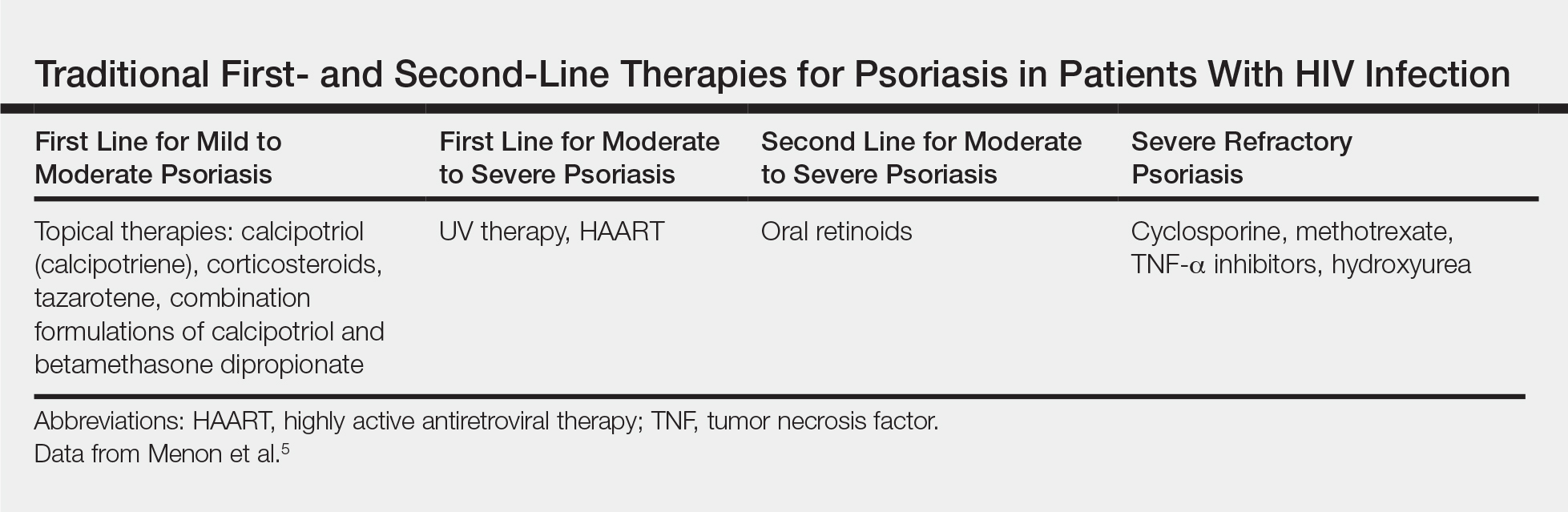
Topical Therapy
As in the general population, targeted therapies such as topical agents are recommended as first-line treatment of mild HIV-associated psoriasis.12 Topical corticosteroids, calcipotriol, tazarotene, and formulations combining 2 of these medications form the cornerstone of topical therapies for mild psoriasis in patients with HIV infection. These agents have the advantage of possessing limited and localized effects, making it unlikely for them to increase immunosuppression in patients with HIV infection. They generally can be safely used in patients with HIV infection, and their side-effect profile in patients with HIV infection is similar to the general population.12 However, calcipotriol is the least desirable for use in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4
UV Phototherapy
Topical therapy is limited by its lack of potency; limited field coverage; and the inconvenience of application, particularly in patients with more widespread disease.12 Therefore, UV phototherapy is preferred as first-line treatment of moderate to severe psoriasis. UV phototherapy has been shown to inhibit cell proliferation and inflammation and result in clinical improvement of HIV-associated psoriasis; moreover, most of the reports in the literature support it as an option that will not increase immunocompromise in patients with HIV infection.12
Caution is warranted, however, regarding the immunomodulatory effects of UV therapies, which may result in an increased risk for skin cancer and diminished resistance to infection, which can be of particular concern in immunocompromised patients who are already at risk.7,13,14 In patients who are candidates for phototherapy, HIV serology and close monitoring of viral load and CD4 lymphocyte count before treatment, at monthly interludes throughout treatment, and 3 months following the cessation of treatment have been recommended.7,15 Careful consideration of the risk-benefit ratio of phototherapy for individual patients, including the patient’s stage of HIV disease, the degree of discomfort, disfigurement, and disability caused by the psoriasis (or other dermatologic condition), as well as the availability of alternative treatment options is essential.7,16
Systemic Agents
In patients who are intolerant of or unresponsive to antiretroviral therapy, topical therapies, and phototherapy, traditional systemic agents may be considered,12 including acitretin, methotrexate, and cyclosporine. However, updated guidelines indicate that methotrexate and cyclosporine should be avoided in this population given the risk for increased immunosuppression with these agents.4,17
Oral retinoids, such as acitretin, continue to be important options for second-line psoriasis treatment in patients with comorbid HIV infection, either as monotherapy or in association with phototherapy.3 Acitretin has the notable benefit of not causing or worsening immune compromise; however, its use is less than desirable in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4,12 Providers also must be aware of the possible association between acitretin (and other antiretrovirals) and pancreatitis, remaining vigilant in monitoring patients for this adverse effect.3
Biologics
The relatively recent addition of cytokine-suppressive biologic agents to the treatment armamentarium has transformed the management of psoriasis in otherwise healthy individuals. These agents have been shown to possess an excellent safety and efficacy profile.12 However, their use in patients with HIV infection has been mired in concerns regarding a potential increase in the risk for opportunistic infections, sepsis, and HIV disease progression in this patient population.7,12
Case reports have detailed the safe treatment of recalcitrant HIV-associated psoriasis with tumor necrosis factor (TNF) blockers, such as etanercept.7,12 In most of these case reports, no harm to CD4 lymphocyte counts, serum viral loads, overall immune status, and susceptibility to infection have been noted; on the contrary, CD4 count increased in most patients following treatment with biologic agents.12 Because patients with HIV infection tend to be excluded from clinical trials, anecdotal evidence derived from case reports and case series often provides clinically relevant information and often forms the basis for treatment recommendations in this patient population.12 Indeed, in the wake of positive case reports, TNF-α inhibitors are now recommended for highly selected patients with refractory chronic psoriatic disease, including those with incapacitating joint pain.7,18
When TNF-α inhibitors are used in patients with HIV infection and psoriasis, optimal antiretroviral therapy and exceedingly close monitoring of clinical and laboratory parameters are of the utmost importance; Pneumocystis jiroveci prophylaxis also is recommended in patients with low CD4 counts.7,18
In 2014, the oral phosphodiesterase 4 inhibitor apremilast was approved for the treatment of moderate to severe plaque psoriasis and PsA. Recent case reports have described its successful use in patients with HIV infection and psoriasis, including the case reported herein, with no reports of opportunistic infections.4,19 Furthermore, HIV infection is not listed as a contraindication on its label.20
Apremilast is thought to increase intracellular cyclic adenosine monophosphate, thereby helping to attain improved homeostasis between proinflammatory and anti-inflammatory mediators.4,19 Several of the proinflammatory mediators that are indirectly targeted by apremilast, including TNF-α and IL-23, are explicitly inhibited by other biologics. It is this equilibrium between proinflammatory and anti-inflammatory mediators that most markedly differentiates apremilast from most other available biologic therapies for psoriasis, which typically have a specific proinflammatory target.4,21 As with other systemic therapies, close monitoring of CD4 levels and viral loads, as well as use of relevant prophylactic agents, is essential when apremilast is used in the setting of HIV infection, making coordination with infectious disease specialists essential.19
Bottom Line
Management of psoriasis in patients with HIV infection represents a clinical challenge. Case reports suggest a role for apremilast as an adjuvant to first-line therapy such as UV phototherapy in the setting of HIV infection in a patient with moderate to severe psoriasis, but close monitoring of CD4 count and viral load in these patients is needed in collaboration with infectious disease specialists. Updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population are needed.
The treatment of psoriasis in patients with HIV infection represents a clinical challenge.1,2 Up to 3% of patients with HIV infection are estimated to have psoriasis. Although this prevalence is similar to the general population, psoriatic disease in patients with HIV tends to be more severe, refractory, and more difficult to treat.3-5 Additionally, up to half of patients with comorbid HIV and psoriasis also have substantial psoriatic arthritis (PsA).1,6
Drug treatments for psoriasis and PsA often are immunosuppressive; as such, the treatment of psoriasis in this patient population requires careful consideration of the potential risks and benefits of treatment as well as fastidious monitoring for the emergence of potentially adverse treatment effects.1 A careful diagnostic process to determine the severity of HIV-associated psoriasis and to select the appropriate treatment relative to the patient’s immunologic status is of critical importance.3
Presentation of Psoriasis in Patients With HIV Infection
The presentation and severity of psoriasis in patients with HIV infection is highly variable and is often related to the degree of immune suppression experienced by the patient.3,7 In some individuals, psoriasis may be the first outward manifestation of HIV, whereas in others, it only manifests after HIV has progressed to AIDS.7
Recognition of the atypical presentations of psoriasis that are frequently seen in patients with HIV infection can help to facilitate early diagnosis and treatment to improve patient outcomes.3,8 Psoriasis vulgaris, for example, typically presents as erythematous plaques with silvery-white scales on extensor surfaces of the body such as the knees and elbows. However, in patients with HIV, psoriasis vulgaris may present with scales that appear thick and oyster shell–like instead of silvery-white; these lesions also may occur on flexural areas rather than extensor surfaces.8 Similarly, the sudden onset of widespread psoriasis in otherwise healthy persons should trigger suspicion for HIV infection and recommendations for appropriate testing, even when no risk factors are present.8

Guttate, inverse, and erythrodermic psoriasis are the most common subtypes in patients with HIV infection, though all clinical subtypes may occur. Overlapping of psoriasis subtypes often occurs in individuals with HIV infection and should serve as a red flag to recommend screening for HIV.5,8 Acral involvement, frequently with pustules and occasionally with severe destructive nail changes, is commonly seen in patients with HIV-associated psoriasis.7,9 In cases involving severe psoriatic exacerbations among individuals with AIDS, there is a heightened risk of developing systemic infections, including superinfection of Staphylococcus aureus, which is a rare occurrence in immunocompetent patients with psoriasis.7,10,11
Therapeutic Options
Because the clinical course of psoriasis in patients with HIV infection is frequently progressive and refractory to treatment, traditional first- and second-line therapies (Table) including topical agents, phototherapy, and oral retinoids may be unable to achieve lasting control of both skin and joint manifestations.1
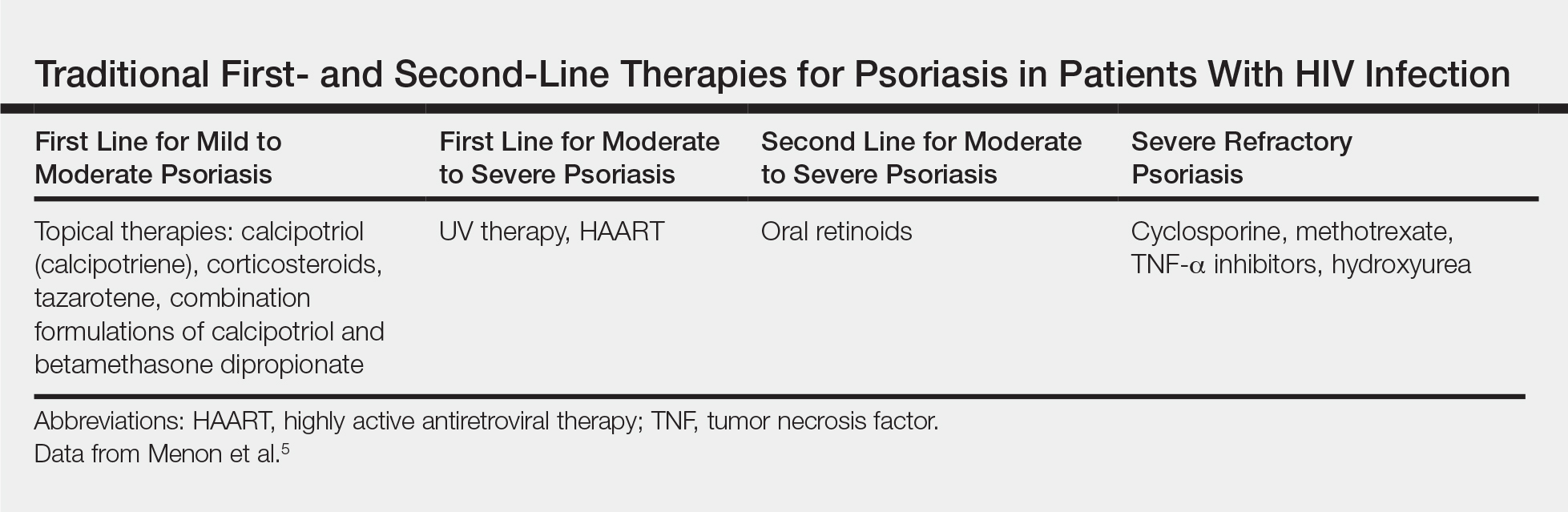
Topical Therapy
As in the general population, targeted therapies such as topical agents are recommended as first-line treatment of mild HIV-associated psoriasis.12 Topical corticosteroids, calcipotriol, tazarotene, and formulations combining 2 of these medications form the cornerstone of topical therapies for mild psoriasis in patients with HIV infection. These agents have the advantage of possessing limited and localized effects, making it unlikely for them to increase immunosuppression in patients with HIV infection. They generally can be safely used in patients with HIV infection, and their side-effect profile in patients with HIV infection is similar to the general population.12 However, calcipotriol is the least desirable for use in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4
UV Phototherapy
Topical therapy is limited by its lack of potency; limited field coverage; and the inconvenience of application, particularly in patients with more widespread disease.12 Therefore, UV phototherapy is preferred as first-line treatment of moderate to severe psoriasis. UV phototherapy has been shown to inhibit cell proliferation and inflammation and result in clinical improvement of HIV-associated psoriasis; moreover, most of the reports in the literature support it as an option that will not increase immunocompromise in patients with HIV infection.12
Caution is warranted, however, regarding the immunomodulatory effects of UV therapies, which may result in an increased risk for skin cancer and diminished resistance to infection, which can be of particular concern in immunocompromised patients who are already at risk.7,13,14 In patients who are candidates for phototherapy, HIV serology and close monitoring of viral load and CD4 lymphocyte count before treatment, at monthly interludes throughout treatment, and 3 months following the cessation of treatment have been recommended.7,15 Careful consideration of the risk-benefit ratio of phototherapy for individual patients, including the patient’s stage of HIV disease, the degree of discomfort, disfigurement, and disability caused by the psoriasis (or other dermatologic condition), as well as the availability of alternative treatment options is essential.7,16
Systemic Agents
In patients who are intolerant of or unresponsive to antiretroviral therapy, topical therapies, and phototherapy, traditional systemic agents may be considered,12 including acitretin, methotrexate, and cyclosporine. However, updated guidelines indicate that methotrexate and cyclosporine should be avoided in this population given the risk for increased immunosuppression with these agents.4,17
Oral retinoids, such as acitretin, continue to be important options for second-line psoriasis treatment in patients with comorbid HIV infection, either as monotherapy or in association with phototherapy.3 Acitretin has the notable benefit of not causing or worsening immune compromise; however, its use is less than desirable in patients with hypertriglyceridemia, which can be a side effect of antiretroviral drugs.4,12 Providers also must be aware of the possible association between acitretin (and other antiretrovirals) and pancreatitis, remaining vigilant in monitoring patients for this adverse effect.3
Biologics
The relatively recent addition of cytokine-suppressive biologic agents to the treatment armamentarium has transformed the management of psoriasis in otherwise healthy individuals. These agents have been shown to possess an excellent safety and efficacy profile.12 However, their use in patients with HIV infection has been mired in concerns regarding a potential increase in the risk for opportunistic infections, sepsis, and HIV disease progression in this patient population.7,12
Case reports have detailed the safe treatment of recalcitrant HIV-associated psoriasis with tumor necrosis factor (TNF) blockers, such as etanercept.7,12 In most of these case reports, no harm to CD4 lymphocyte counts, serum viral loads, overall immune status, and susceptibility to infection have been noted; on the contrary, CD4 count increased in most patients following treatment with biologic agents.12 Because patients with HIV infection tend to be excluded from clinical trials, anecdotal evidence derived from case reports and case series often provides clinically relevant information and often forms the basis for treatment recommendations in this patient population.12 Indeed, in the wake of positive case reports, TNF-α inhibitors are now recommended for highly selected patients with refractory chronic psoriatic disease, including those with incapacitating joint pain.7,18
When TNF-α inhibitors are used in patients with HIV infection and psoriasis, optimal antiretroviral therapy and exceedingly close monitoring of clinical and laboratory parameters are of the utmost importance; Pneumocystis jiroveci prophylaxis also is recommended in patients with low CD4 counts.7,18
In 2014, the oral phosphodiesterase 4 inhibitor apremilast was approved for the treatment of moderate to severe plaque psoriasis and PsA. Recent case reports have described its successful use in patients with HIV infection and psoriasis, including the case reported herein, with no reports of opportunistic infections.4,19 Furthermore, HIV infection is not listed as a contraindication on its label.20
Apremilast is thought to increase intracellular cyclic adenosine monophosphate, thereby helping to attain improved homeostasis between proinflammatory and anti-inflammatory mediators.4,19 Several of the proinflammatory mediators that are indirectly targeted by apremilast, including TNF-α and IL-23, are explicitly inhibited by other biologics. It is this equilibrium between proinflammatory and anti-inflammatory mediators that most markedly differentiates apremilast from most other available biologic therapies for psoriasis, which typically have a specific proinflammatory target.4,21 As with other systemic therapies, close monitoring of CD4 levels and viral loads, as well as use of relevant prophylactic agents, is essential when apremilast is used in the setting of HIV infection, making coordination with infectious disease specialists essential.19
Bottom Line
Management of psoriasis in patients with HIV infection represents a clinical challenge. Case reports suggest a role for apremilast as an adjuvant to first-line therapy such as UV phototherapy in the setting of HIV infection in a patient with moderate to severe psoriasis, but close monitoring of CD4 count and viral load in these patients is needed in collaboration with infectious disease specialists. Updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population are needed.
- Nakamura M, Abrouk M, Farahnik B, et al. Psoriasis treatment in HIV-positive patients: a systematic review of systemic immunosuppressive therapies. Cutis. 2018;101:38, 42, 56.
- Patel RV, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 2: review of treatment. Cutis. 2008;82:202-210.
- Ceccarelli M, Venanzi Rullo E, Vaccaro M, et al. HIV‐associated psoriasis: epidemiology, pathogenesis, and management [published online January 6, 2019]. Dermatol Ther. 2019;32:e12806. doi:10.1111/dth.12806.
- Zarbafian M, Richer V. Treatment of moderate to severe psoriasis with apremilast over 2 years in the context of long-term treated HIV infection: a case report. SAGE Open Med Case Rep. 2019;7:2050313X19845193. doi:10.1177/2050313X19845193.
- Menon K, Van Vorhees AS, Bebo, BF, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Mallon E, Bunker CB. HIV-associated psoriasis. AIDS Patient Care STDS. 2000;14:239-246.
- Patel VA, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 1: review of pathogenesis. Cutis. 2008;82:117-122.
- Castillo RL, Racaza GZ, Dela Cruz Roa F. Ostraceous and inverse psoriasis with psoriatic arthritis as the presenting features of advanced HIV infection. Singapore Med J. 2014;55:e60-e63.
- Duvic M, Crane MM, Conant M, et al. Zidovudine improves psoriasis in human immunodeficiency virus- positive males. Arch Dermatol. 1994;130:447.
- Jaffee D, May LP, Sanchez M, et al. Staphylococcal sepsis in HIV antibody seropositive psoriasis patients. J Am Acad Dermatol. 1991;24:970-972.
- King LE, Dufresne RG, Lovette GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
- Kaminetsky J, Aziz M, Kaushik S. A review of biologics and other treatment modalities in HIV-associated psoriasis. Skin. 2018;2:389-401.
- Wolff K. Side effects of psoralen photochemotherapy (PUVA). Br J Dermatol. 1990;122:117-125.
- Stern RS, Mills DK, Krell K, et al. HIV-positive patients differ from HIV-negative patients in indications for and type of UV therapy used. J Am Acad Dermatol. 1998;39:48-55.
- Oracion RM, Skiest DJ, Keiser PH, et al. HIV-related skin diseases. Prog Dermatol. 1999;33:1-6.
- Finkelstein M, Berman B. HIV and AIDS in inpatient dermatology: approach to the consultation. Dermatol Clin. 2000;18:509-520.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections. J Am Acad Dermatol. 2019;80:43-53.
- Sellam J, Bouvard B, Masson C, et al. Use of infliximab to treat psoriatic arthritis in HIV-positive patients. Joint Bone Spine. 2007;74:197-200.
- Reddy SP, Lee E, Wu JJ. Apremilast and phototherapy for treatment of psoriasis in a patient with human immunodeficiency virus. Cutis. 2019;103:E1-E7.
- Otezla (apremilast). Summit, NJ: Celgene Corporation; 2017.
- Schafer P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem Pharmacol. 2012;83:1583-1590.
- Nakamura M, Abrouk M, Farahnik B, et al. Psoriasis treatment in HIV-positive patients: a systematic review of systemic immunosuppressive therapies. Cutis. 2018;101:38, 42, 56.
- Patel RV, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 2: review of treatment. Cutis. 2008;82:202-210.
- Ceccarelli M, Venanzi Rullo E, Vaccaro M, et al. HIV‐associated psoriasis: epidemiology, pathogenesis, and management [published online January 6, 2019]. Dermatol Ther. 2019;32:e12806. doi:10.1111/dth.12806.
- Zarbafian M, Richer V. Treatment of moderate to severe psoriasis with apremilast over 2 years in the context of long-term treated HIV infection: a case report. SAGE Open Med Case Rep. 2019;7:2050313X19845193. doi:10.1177/2050313X19845193.
- Menon K, Van Vorhees AS, Bebo, BF, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Mallon E, Bunker CB. HIV-associated psoriasis. AIDS Patient Care STDS. 2000;14:239-246.
- Patel VA, Weinberg JM. Psoriasis in the patient with human immunodeficiency virus, part 1: review of pathogenesis. Cutis. 2008;82:117-122.
- Castillo RL, Racaza GZ, Dela Cruz Roa F. Ostraceous and inverse psoriasis with psoriatic arthritis as the presenting features of advanced HIV infection. Singapore Med J. 2014;55:e60-e63.
- Duvic M, Crane MM, Conant M, et al. Zidovudine improves psoriasis in human immunodeficiency virus- positive males. Arch Dermatol. 1994;130:447.
- Jaffee D, May LP, Sanchez M, et al. Staphylococcal sepsis in HIV antibody seropositive psoriasis patients. J Am Acad Dermatol. 1991;24:970-972.
- King LE, Dufresne RG, Lovette GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
- Kaminetsky J, Aziz M, Kaushik S. A review of biologics and other treatment modalities in HIV-associated psoriasis. Skin. 2018;2:389-401.
- Wolff K. Side effects of psoralen photochemotherapy (PUVA). Br J Dermatol. 1990;122:117-125.
- Stern RS, Mills DK, Krell K, et al. HIV-positive patients differ from HIV-negative patients in indications for and type of UV therapy used. J Am Acad Dermatol. 1998;39:48-55.
- Oracion RM, Skiest DJ, Keiser PH, et al. HIV-related skin diseases. Prog Dermatol. 1999;33:1-6.
- Finkelstein M, Berman B. HIV and AIDS in inpatient dermatology: approach to the consultation. Dermatol Clin. 2000;18:509-520.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections. J Am Acad Dermatol. 2019;80:43-53.
- Sellam J, Bouvard B, Masson C, et al. Use of infliximab to treat psoriatic arthritis in HIV-positive patients. Joint Bone Spine. 2007;74:197-200.
- Reddy SP, Lee E, Wu JJ. Apremilast and phototherapy for treatment of psoriasis in a patient with human immunodeficiency virus. Cutis. 2019;103:E1-E7.
- Otezla (apremilast). Summit, NJ: Celgene Corporation; 2017.
- Schafer P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem Pharmacol. 2012;83:1583-1590.
A 50-year-old man with Fitzpatrick skin type IV presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. The patient’s medical history was positive for human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected), for which clobetasol spray and calcitriol ointment had been prescribed. The patient’s CD4 count was 460 at presentation, and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to presentation. For the last 5 months, the patient had been undergoing phototherapy 3 times weekly for treatment of psoriasis.
An apremilast starter pack was initiated with the dosage titrated from 10 mg to 30 mg over the course of 1 week. The patient was maintained on a dose of 30 mg twice daily after 1 week, while continuing clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the patient’s affected BSA was 0%. Apremilast was continued, and phototherapy was reduced to once weekly. After 7 months of concomitant treatment with apremilast, phototherapy was discontinued after clearance was maintained. Phototherapy was reinitiated twice weekly after a mild flare (3% BSA affected).
The patient continued apremilast for a total of 20 months until it became cost prohibitive. After discontinuing apremilast for 4 months, he presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with intention to apply for an apremilast financial assistance program.