User login
Strictures in Crohn’s: Balloon dilation avoids later surgery
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
FROM EUROPEAN JOURNAL OF GASTROENTEROLOGY & HEPATOLOGY
Does choice of biologic affect outcomes in perianal Crohn’s disease?
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Pulse oximeters lead to less oxygen supplementation for people of color
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Medicare to cover colonoscopy after positive fecal test
Medicare will cover the full cost of colonoscopy after a positive noninvasive fecal test beginning in 2023, largely in response to a year-long advocacy campaign.
The benefit expansion is a “huge win” for patients, according to the American Gastroenterological Association, because it represents the end of out-of-pocket costs for colorectal cancer (CRC) screening.
“The continuum is complete!” said John Inadomi, MD, AGAF, past president of the AGA and a champion of the initiative within the organization.
Colonoscopy after a positive fecal test was previously considered a diagnostic procedure and therefore not considered part of the screening process by the Affordable Care Act, allowing payers to charge patients. That is, until the AGA and partners, including the American Cancer Society Cancer Action Network and Fight Colorectal Cancer, pushed back. First, the organizations successfully campaigned to ensure that private payers would cover the follow-up procedure. Now, after multiple meetings with the United States Department of Health & Human Services and Centers for Medicare & Medicaid Services, their collaborative efforts will end screening costs for patients with Medicare, pending finalization of the rule this fall. If finalized, it will take effect Jan. 2, 2023.
The policy change will “directly advance health equity” the AGA said, particularly among “rural communities and communities of color,” which are disproportionally affected by CRC.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities,” said David Lieberman, MD, AGAF, who met with the CMS multiple times on behalf of the AGA. “Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test.”
AGA president John Carethers, MD, AGAF, who also met with the CMS, noted that reducing barriers to CRC screening will ultimately reduce CRC mortality.
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives,” he said.
Dr. Inadomi, Dr. Carethers, and Dr. Lieberman serve on the scientific advisory board of Geneoscopy; Dr. Lieberman is also on the scientific advisory board for ColoWrap.
Medicare will cover the full cost of colonoscopy after a positive noninvasive fecal test beginning in 2023, largely in response to a year-long advocacy campaign.
The benefit expansion is a “huge win” for patients, according to the American Gastroenterological Association, because it represents the end of out-of-pocket costs for colorectal cancer (CRC) screening.
“The continuum is complete!” said John Inadomi, MD, AGAF, past president of the AGA and a champion of the initiative within the organization.
Colonoscopy after a positive fecal test was previously considered a diagnostic procedure and therefore not considered part of the screening process by the Affordable Care Act, allowing payers to charge patients. That is, until the AGA and partners, including the American Cancer Society Cancer Action Network and Fight Colorectal Cancer, pushed back. First, the organizations successfully campaigned to ensure that private payers would cover the follow-up procedure. Now, after multiple meetings with the United States Department of Health & Human Services and Centers for Medicare & Medicaid Services, their collaborative efforts will end screening costs for patients with Medicare, pending finalization of the rule this fall. If finalized, it will take effect Jan. 2, 2023.
The policy change will “directly advance health equity” the AGA said, particularly among “rural communities and communities of color,” which are disproportionally affected by CRC.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities,” said David Lieberman, MD, AGAF, who met with the CMS multiple times on behalf of the AGA. “Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test.”
AGA president John Carethers, MD, AGAF, who also met with the CMS, noted that reducing barriers to CRC screening will ultimately reduce CRC mortality.
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives,” he said.
Dr. Inadomi, Dr. Carethers, and Dr. Lieberman serve on the scientific advisory board of Geneoscopy; Dr. Lieberman is also on the scientific advisory board for ColoWrap.
Medicare will cover the full cost of colonoscopy after a positive noninvasive fecal test beginning in 2023, largely in response to a year-long advocacy campaign.
The benefit expansion is a “huge win” for patients, according to the American Gastroenterological Association, because it represents the end of out-of-pocket costs for colorectal cancer (CRC) screening.
“The continuum is complete!” said John Inadomi, MD, AGAF, past president of the AGA and a champion of the initiative within the organization.
Colonoscopy after a positive fecal test was previously considered a diagnostic procedure and therefore not considered part of the screening process by the Affordable Care Act, allowing payers to charge patients. That is, until the AGA and partners, including the American Cancer Society Cancer Action Network and Fight Colorectal Cancer, pushed back. First, the organizations successfully campaigned to ensure that private payers would cover the follow-up procedure. Now, after multiple meetings with the United States Department of Health & Human Services and Centers for Medicare & Medicaid Services, their collaborative efforts will end screening costs for patients with Medicare, pending finalization of the rule this fall. If finalized, it will take effect Jan. 2, 2023.
The policy change will “directly advance health equity” the AGA said, particularly among “rural communities and communities of color,” which are disproportionally affected by CRC.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities,” said David Lieberman, MD, AGAF, who met with the CMS multiple times on behalf of the AGA. “Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test.”
AGA president John Carethers, MD, AGAF, who also met with the CMS, noted that reducing barriers to CRC screening will ultimately reduce CRC mortality.
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives,” he said.
Dr. Inadomi, Dr. Carethers, and Dr. Lieberman serve on the scientific advisory board of Geneoscopy; Dr. Lieberman is also on the scientific advisory board for ColoWrap.
What explains poor adherence to eosinophilic esophagitis therapy?
Almost half of adult patients with eosinophilic esophagitis (EoE) reported poor adherence to long-term medical and dietary therapy, with age younger than 40 years and low necessity beliefs being the strongest predictors, a new study finds.
Clinicians need to spend more time discussing the need for EoE therapy with their patients, especially if they are younger, according to lead author Maria L. Haasnoot, MD, of Amsterdam University Medical Center (UMC), the Netherlands, and colleagues.
“Chronic treatment is necessary to maintain suppression of the inflammation and prevent negative outcomes in the long-term,” they write.
Until the recent approval of dupilumab (Dupixent) by the U.S. Food and Drug Administration, patients with EoE relied upon off-label options, including proton pump inhibitors and swallowed topical steroids, as well as dietary interventions for ongoing suppression of inflammation. But only about 1 in 6 patients achieve complete remission at 5 years, according to Dr. Haasnoot and colleagues.
“It is uncertain to what degree limited adherence to treatment [plays] a role in the limited long-term effects of treatment,” they write.
The findings were published online in American Journal of Gastroenterology.
Addressing a knowledge gap
The cross-sectional study involved 177 adult patients with EoE treated at Amsterdam UMC, who were prescribed dietary or medical maintenance therapy. Of note, some patients were treated with budesonide, which is approved for EoE in Europe but not in the United States.
Median participant age was 43 years, with a male-skewed distribution (71% men). Patients had been on EoE treatment for 2-6 years. Most (76%) were on medical treatments. Nearly half were on diets that avoided one to five food groups, with some on both medical treatments and elimination diets.
Using a link sent by mail, participants completed the online Medication Adherence Rating Scale, along with several other questionnaires, such as the Beliefs about Medicine Questionnaire, to measure secondary outcomes, including a patient’s view of how necessary or disruptive maintenance therapy is in their life.
The overall prevalence of poor adherence to therapy was high (41.8%), including a nonsignificant difference in adherence between medical and dietary therapies.
“It might come as a surprise that dietary-treated patients are certainly not less adherent to treatment than medically treated patients,” the authors write, noting that the opposite is usually true.
Multivariate logistic regression showed that patients younger than 40 years were more than twice as likely to be poorly adherent (odds ratio, 2.571; 95% confidence interval, 1.195-5.532). Those with low necessity beliefs were more than four times as likely to be poorly adherent (OR, 4.423; 95% CI, 2.169-9.016). Other factors linked to poor adherence were patients with longer disease duration and more severe symptoms.
“Clinicians should pay more attention to treatment adherence, particularly in younger patients,” the authors conclude. “The necessity of treatment should be actively discussed, and efforts should be done to take doubts away, as this may improve treatment adherence and subsequently may improve treatment effects and long-term outcomes.”
More patient education needed
According to Jennifer L. Horsley-Silva, MD, of Mayo Clinic, Scottsdale, Ariz., “This study is important, as it is one of the first studies to investigate the rate of treatment adherence in EoE patients and attempts to identify factors associated with adherence both in medically and dietary treated patients.”
Dr. Horsley-Silva commented that the findings align with recent research she and her colleagues conducted at the Mayo Clinic, where few patients successfully completed a six-food elimination diet, even when paired with a dietitian. As with the present study, success trended lower among younger adults. “These findings highlight the need for physicians treating EoE to motivate all patients, but especially younger patients, by discussing disease pathophysiology and explaining the reason for maintenance treatment early on,” Dr. Horsley-Silva said.
Conversations should also address the discordance between symptoms and histologic disease, patient doubts and concerns, and other barriers to adherence, she noted.
“Shared decisionmaking is of utmost importance when deciding upon a maintenance treatment strategy and should be readdressed continually,” she added.
Gary W. Falk, MD, of Penn Medicine, Philadelphia, said that patients with EoE may be poorly adherent because therapies tend to be complicated and people often forget to take their medications, especially when their symptoms improve, even though this is a poor indicator of underlying disease. The discordance between symptoms and histology is “not commonly appreciated by the EoE GI community,” he noted.
Patients may benefit from knowing that untreated or undertreated EoE increases the risk for strictures and stenoses, need for dilation, and frequency of food bolus impactions, Dr. Falk said.
“The other thing we know is that once someone is induced into remission, and they stay on therapy ... long-term remission can be maintained,” he added.
The impact of Dupilumab
John Leung, MD, of Boston Food Allergy Center, also cited the complexities of EoE therapies as reason for poor adherence, though he believes this paradigm will shift now that dupilumab has been approved. Dupilumab injections are “just once a week, so it’s much easier in terms of frequency,” Dr. Leung said. “I would expect that the compliance [for dupilumab] will be better” than for older therapies.
Dr. Leung, who helped conduct the dupilumab clinical trials contributing to its approval for EoE and receives speaking honoraria from manufacturer Regeneron/Sanofi, said that dupilumab also overcomes the challenges with elimination diets while offering relief for concomitant conditions, such as “asthma, eczema, food allergies, and seasonal allergies.”
But Dr. Falk, who also worked on the dupilumab clinical trials, said the situation is “not straightforward,” even with FDA approval.
“There are going to be significant costs with [prescribing dupilumab], because it’s a biologic,” Dr. Falk said.
Dr. Falk also pointed out that prior authorization will be required, and until more studies can be conducted, the true impact of once-weekly dosing versus daily dosing remains unknown.
“I would say [dupilumab] has the potential to improve adherence, but we need to see if that’s going to be the case or not,” Dr. Falk said.
The authors disclosed relationships with Dr. Falk Pharma, AstraZeneca, and Sanofi/Regeneron (the manufacturers of Dupixent [dupilumab]), among others. Dr. Horsley-Silva, Dr. Falk, and Dr. Leung conducted clinical trials for dupilumab on behalf of Sanofi/Regeneron, with Dr. Leung also disclosing speaking honoraria from Sanofi/Regeneron. Dr. Horsley-Silva has acted as a clinical trial site principal investigator for Allakos and Celgene/Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Almost half of adult patients with eosinophilic esophagitis (EoE) reported poor adherence to long-term medical and dietary therapy, with age younger than 40 years and low necessity beliefs being the strongest predictors, a new study finds.
Clinicians need to spend more time discussing the need for EoE therapy with their patients, especially if they are younger, according to lead author Maria L. Haasnoot, MD, of Amsterdam University Medical Center (UMC), the Netherlands, and colleagues.
“Chronic treatment is necessary to maintain suppression of the inflammation and prevent negative outcomes in the long-term,” they write.
Until the recent approval of dupilumab (Dupixent) by the U.S. Food and Drug Administration, patients with EoE relied upon off-label options, including proton pump inhibitors and swallowed topical steroids, as well as dietary interventions for ongoing suppression of inflammation. But only about 1 in 6 patients achieve complete remission at 5 years, according to Dr. Haasnoot and colleagues.
“It is uncertain to what degree limited adherence to treatment [plays] a role in the limited long-term effects of treatment,” they write.
The findings were published online in American Journal of Gastroenterology.
Addressing a knowledge gap
The cross-sectional study involved 177 adult patients with EoE treated at Amsterdam UMC, who were prescribed dietary or medical maintenance therapy. Of note, some patients were treated with budesonide, which is approved for EoE in Europe but not in the United States.
Median participant age was 43 years, with a male-skewed distribution (71% men). Patients had been on EoE treatment for 2-6 years. Most (76%) were on medical treatments. Nearly half were on diets that avoided one to five food groups, with some on both medical treatments and elimination diets.
Using a link sent by mail, participants completed the online Medication Adherence Rating Scale, along with several other questionnaires, such as the Beliefs about Medicine Questionnaire, to measure secondary outcomes, including a patient’s view of how necessary or disruptive maintenance therapy is in their life.
The overall prevalence of poor adherence to therapy was high (41.8%), including a nonsignificant difference in adherence between medical and dietary therapies.
“It might come as a surprise that dietary-treated patients are certainly not less adherent to treatment than medically treated patients,” the authors write, noting that the opposite is usually true.
Multivariate logistic regression showed that patients younger than 40 years were more than twice as likely to be poorly adherent (odds ratio, 2.571; 95% confidence interval, 1.195-5.532). Those with low necessity beliefs were more than four times as likely to be poorly adherent (OR, 4.423; 95% CI, 2.169-9.016). Other factors linked to poor adherence were patients with longer disease duration and more severe symptoms.
“Clinicians should pay more attention to treatment adherence, particularly in younger patients,” the authors conclude. “The necessity of treatment should be actively discussed, and efforts should be done to take doubts away, as this may improve treatment adherence and subsequently may improve treatment effects and long-term outcomes.”
More patient education needed
According to Jennifer L. Horsley-Silva, MD, of Mayo Clinic, Scottsdale, Ariz., “This study is important, as it is one of the first studies to investigate the rate of treatment adherence in EoE patients and attempts to identify factors associated with adherence both in medically and dietary treated patients.”
Dr. Horsley-Silva commented that the findings align with recent research she and her colleagues conducted at the Mayo Clinic, where few patients successfully completed a six-food elimination diet, even when paired with a dietitian. As with the present study, success trended lower among younger adults. “These findings highlight the need for physicians treating EoE to motivate all patients, but especially younger patients, by discussing disease pathophysiology and explaining the reason for maintenance treatment early on,” Dr. Horsley-Silva said.
Conversations should also address the discordance between symptoms and histologic disease, patient doubts and concerns, and other barriers to adherence, she noted.
“Shared decisionmaking is of utmost importance when deciding upon a maintenance treatment strategy and should be readdressed continually,” she added.
Gary W. Falk, MD, of Penn Medicine, Philadelphia, said that patients with EoE may be poorly adherent because therapies tend to be complicated and people often forget to take their medications, especially when their symptoms improve, even though this is a poor indicator of underlying disease. The discordance between symptoms and histology is “not commonly appreciated by the EoE GI community,” he noted.
Patients may benefit from knowing that untreated or undertreated EoE increases the risk for strictures and stenoses, need for dilation, and frequency of food bolus impactions, Dr. Falk said.
“The other thing we know is that once someone is induced into remission, and they stay on therapy ... long-term remission can be maintained,” he added.
The impact of Dupilumab
John Leung, MD, of Boston Food Allergy Center, also cited the complexities of EoE therapies as reason for poor adherence, though he believes this paradigm will shift now that dupilumab has been approved. Dupilumab injections are “just once a week, so it’s much easier in terms of frequency,” Dr. Leung said. “I would expect that the compliance [for dupilumab] will be better” than for older therapies.
Dr. Leung, who helped conduct the dupilumab clinical trials contributing to its approval for EoE and receives speaking honoraria from manufacturer Regeneron/Sanofi, said that dupilumab also overcomes the challenges with elimination diets while offering relief for concomitant conditions, such as “asthma, eczema, food allergies, and seasonal allergies.”
But Dr. Falk, who also worked on the dupilumab clinical trials, said the situation is “not straightforward,” even with FDA approval.
“There are going to be significant costs with [prescribing dupilumab], because it’s a biologic,” Dr. Falk said.
Dr. Falk also pointed out that prior authorization will be required, and until more studies can be conducted, the true impact of once-weekly dosing versus daily dosing remains unknown.
“I would say [dupilumab] has the potential to improve adherence, but we need to see if that’s going to be the case or not,” Dr. Falk said.
The authors disclosed relationships with Dr. Falk Pharma, AstraZeneca, and Sanofi/Regeneron (the manufacturers of Dupixent [dupilumab]), among others. Dr. Horsley-Silva, Dr. Falk, and Dr. Leung conducted clinical trials for dupilumab on behalf of Sanofi/Regeneron, with Dr. Leung also disclosing speaking honoraria from Sanofi/Regeneron. Dr. Horsley-Silva has acted as a clinical trial site principal investigator for Allakos and Celgene/Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Almost half of adult patients with eosinophilic esophagitis (EoE) reported poor adherence to long-term medical and dietary therapy, with age younger than 40 years and low necessity beliefs being the strongest predictors, a new study finds.
Clinicians need to spend more time discussing the need for EoE therapy with their patients, especially if they are younger, according to lead author Maria L. Haasnoot, MD, of Amsterdam University Medical Center (UMC), the Netherlands, and colleagues.
“Chronic treatment is necessary to maintain suppression of the inflammation and prevent negative outcomes in the long-term,” they write.
Until the recent approval of dupilumab (Dupixent) by the U.S. Food and Drug Administration, patients with EoE relied upon off-label options, including proton pump inhibitors and swallowed topical steroids, as well as dietary interventions for ongoing suppression of inflammation. But only about 1 in 6 patients achieve complete remission at 5 years, according to Dr. Haasnoot and colleagues.
“It is uncertain to what degree limited adherence to treatment [plays] a role in the limited long-term effects of treatment,” they write.
The findings were published online in American Journal of Gastroenterology.
Addressing a knowledge gap
The cross-sectional study involved 177 adult patients with EoE treated at Amsterdam UMC, who were prescribed dietary or medical maintenance therapy. Of note, some patients were treated with budesonide, which is approved for EoE in Europe but not in the United States.
Median participant age was 43 years, with a male-skewed distribution (71% men). Patients had been on EoE treatment for 2-6 years. Most (76%) were on medical treatments. Nearly half were on diets that avoided one to five food groups, with some on both medical treatments and elimination diets.
Using a link sent by mail, participants completed the online Medication Adherence Rating Scale, along with several other questionnaires, such as the Beliefs about Medicine Questionnaire, to measure secondary outcomes, including a patient’s view of how necessary or disruptive maintenance therapy is in their life.
The overall prevalence of poor adherence to therapy was high (41.8%), including a nonsignificant difference in adherence between medical and dietary therapies.
“It might come as a surprise that dietary-treated patients are certainly not less adherent to treatment than medically treated patients,” the authors write, noting that the opposite is usually true.
Multivariate logistic regression showed that patients younger than 40 years were more than twice as likely to be poorly adherent (odds ratio, 2.571; 95% confidence interval, 1.195-5.532). Those with low necessity beliefs were more than four times as likely to be poorly adherent (OR, 4.423; 95% CI, 2.169-9.016). Other factors linked to poor adherence were patients with longer disease duration and more severe symptoms.
“Clinicians should pay more attention to treatment adherence, particularly in younger patients,” the authors conclude. “The necessity of treatment should be actively discussed, and efforts should be done to take doubts away, as this may improve treatment adherence and subsequently may improve treatment effects and long-term outcomes.”
More patient education needed
According to Jennifer L. Horsley-Silva, MD, of Mayo Clinic, Scottsdale, Ariz., “This study is important, as it is one of the first studies to investigate the rate of treatment adherence in EoE patients and attempts to identify factors associated with adherence both in medically and dietary treated patients.”
Dr. Horsley-Silva commented that the findings align with recent research she and her colleagues conducted at the Mayo Clinic, where few patients successfully completed a six-food elimination diet, even when paired with a dietitian. As with the present study, success trended lower among younger adults. “These findings highlight the need for physicians treating EoE to motivate all patients, but especially younger patients, by discussing disease pathophysiology and explaining the reason for maintenance treatment early on,” Dr. Horsley-Silva said.
Conversations should also address the discordance between symptoms and histologic disease, patient doubts and concerns, and other barriers to adherence, she noted.
“Shared decisionmaking is of utmost importance when deciding upon a maintenance treatment strategy and should be readdressed continually,” she added.
Gary W. Falk, MD, of Penn Medicine, Philadelphia, said that patients with EoE may be poorly adherent because therapies tend to be complicated and people often forget to take their medications, especially when their symptoms improve, even though this is a poor indicator of underlying disease. The discordance between symptoms and histology is “not commonly appreciated by the EoE GI community,” he noted.
Patients may benefit from knowing that untreated or undertreated EoE increases the risk for strictures and stenoses, need for dilation, and frequency of food bolus impactions, Dr. Falk said.
“The other thing we know is that once someone is induced into remission, and they stay on therapy ... long-term remission can be maintained,” he added.
The impact of Dupilumab
John Leung, MD, of Boston Food Allergy Center, also cited the complexities of EoE therapies as reason for poor adherence, though he believes this paradigm will shift now that dupilumab has been approved. Dupilumab injections are “just once a week, so it’s much easier in terms of frequency,” Dr. Leung said. “I would expect that the compliance [for dupilumab] will be better” than for older therapies.
Dr. Leung, who helped conduct the dupilumab clinical trials contributing to its approval for EoE and receives speaking honoraria from manufacturer Regeneron/Sanofi, said that dupilumab also overcomes the challenges with elimination diets while offering relief for concomitant conditions, such as “asthma, eczema, food allergies, and seasonal allergies.”
But Dr. Falk, who also worked on the dupilumab clinical trials, said the situation is “not straightforward,” even with FDA approval.
“There are going to be significant costs with [prescribing dupilumab], because it’s a biologic,” Dr. Falk said.
Dr. Falk also pointed out that prior authorization will be required, and until more studies can be conducted, the true impact of once-weekly dosing versus daily dosing remains unknown.
“I would say [dupilumab] has the potential to improve adherence, but we need to see if that’s going to be the case or not,” Dr. Falk said.
The authors disclosed relationships with Dr. Falk Pharma, AstraZeneca, and Sanofi/Regeneron (the manufacturers of Dupixent [dupilumab]), among others. Dr. Horsley-Silva, Dr. Falk, and Dr. Leung conducted clinical trials for dupilumab on behalf of Sanofi/Regeneron, with Dr. Leung also disclosing speaking honoraria from Sanofi/Regeneron. Dr. Horsley-Silva has acted as a clinical trial site principal investigator for Allakos and Celgene/Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
AGA Clinical Practice Guidelines: Pharmacologic treatment of IBS
The American Gastroenterological Association has issued new guidelines for the medical treatment of irritable bowel syndrome (IBS).
The guidelines, which are separated into one publication for IBS with constipation (IBS-C) and another for IBS with diarrhea (IBS-D), are the first to advise clinicians in the usage of new, old, and over-the-counter drugs for IBS, according to a press release from the AGA.
“With more treatments available, physicians can tailor a personalized approach based on the symptoms a patient with IBS is experiencing,” AGA said.
Published simultaneously in Gastroenterology, the two guidelines describe a shared rationale for their creation, noting how the treatment landscape has changed since the AGA last issued IBS guidelines in 2014.
“New pharmacological treatments have become available and new evidence has accumulated about established treatments,” both guidelines stated. “The purpose of these guidelines is to provide evidence-based recommendations for the pharmacologic management” of individuals with IBS “based on a systematic and comprehensive synthesis of the literature.”
IBS-C
In the IBS-C guidelines, co–first authors Lin Chang, MD, AGAF, of the University of Los Angeles, and Shahnaz Sultan, MD, MHSc, AGAF, of the Minneapolis Veterans Affairs Healthcare System, noted that IBS-C accounts for “more than a third of IBS cases,” with patients frequently reporting “feeling self-conscious, avoiding sex, difficulty concentrating, [and] not feeling able to reach one’s full potential.”
They offered nine pharmacologic recommendations, eight of which are conditional, with certainty in evidence ranging from low to high.
The only strong recommendation with a high certainty in evidence is for linaclotide.
“Across four RCTs [randomized controlled trials], linaclotide improved global assessment of IBS-C symptoms (FDA responder), abdominal pain, complete spontaneous bowel movement response, as well as adequate global response,” Dr. Chang and colleagues wrote.
Conditional recommendations with moderate certainty in evidence are provided for tenapanor, plecanatide, tegaserod, and lubiprostone. Recommendations for polyethylene glycol laxatives, tricyclic antidepressants and antispasmodics are conditional and based on low-certainty evidence, as well as a conditional recommendation against selective serotonin reuptake inhibitors, also based on low-certainty evidence.
IBS-D
The IBS-D guidelines, led by co–first authors Anthony Lembo, MD, AGAF, of Beth Israel Deaconess Medical Center, Boston, and Dr. Sultan, includes eight conditional recommendations with certainty in evidence ranging from very low to moderate.
Drugs recommended based on moderate-certainty evidence include eluxadoline, alosetron, and rifaximin, with the added note that patients who respond to rifaximin but have recurrence should be treated again with rifaximin. Low-certainty evidence supported recommendations for tricyclic antidepressants, and antispasmodics. Very low–certainty evidence stands behind a recommendation for loperamide. Again, the panel made a conditional recommendation against SSRIs, also based on low-certainty evidence.
Shared decision-making
Both publications concluded with similar statements about the importance of shared decision-making, plus a practical mindset, in management of IBS.
“Acknowledging that multimodal treatments that include dietary and behavioral approaches in conjunction with drug therapy may provide maximal benefits and that treatment choices may be influenced by patient preferences, practitioners should engage in shared decision-making with patients when choosing the best therapy,” Dr. Lembo and colleagues wrote. “The importance of the patient-physician relationship is paramount in caring for individuals with IBS, and understanding patient preferences (for side-effect tolerability as well as cost) is valuable in choosing the right therapy.”
Both guidelines noted that some newer drugs for IBS have no generic alternative, and preauthorization may be required. Payer approval may depend on previous treatment failure with generic alternatives, they added.
The guidelines were commissioned and funded by the AGA Institute. The authors disclosed relationships with Ardelyx, Immunic, Protagonist, and others.
The American Gastroenterological Association has issued new guidelines for the medical treatment of irritable bowel syndrome (IBS).
The guidelines, which are separated into one publication for IBS with constipation (IBS-C) and another for IBS with diarrhea (IBS-D), are the first to advise clinicians in the usage of new, old, and over-the-counter drugs for IBS, according to a press release from the AGA.
“With more treatments available, physicians can tailor a personalized approach based on the symptoms a patient with IBS is experiencing,” AGA said.
Published simultaneously in Gastroenterology, the two guidelines describe a shared rationale for their creation, noting how the treatment landscape has changed since the AGA last issued IBS guidelines in 2014.
“New pharmacological treatments have become available and new evidence has accumulated about established treatments,” both guidelines stated. “The purpose of these guidelines is to provide evidence-based recommendations for the pharmacologic management” of individuals with IBS “based on a systematic and comprehensive synthesis of the literature.”
IBS-C
In the IBS-C guidelines, co–first authors Lin Chang, MD, AGAF, of the University of Los Angeles, and Shahnaz Sultan, MD, MHSc, AGAF, of the Minneapolis Veterans Affairs Healthcare System, noted that IBS-C accounts for “more than a third of IBS cases,” with patients frequently reporting “feeling self-conscious, avoiding sex, difficulty concentrating, [and] not feeling able to reach one’s full potential.”
They offered nine pharmacologic recommendations, eight of which are conditional, with certainty in evidence ranging from low to high.
The only strong recommendation with a high certainty in evidence is for linaclotide.
“Across four RCTs [randomized controlled trials], linaclotide improved global assessment of IBS-C symptoms (FDA responder), abdominal pain, complete spontaneous bowel movement response, as well as adequate global response,” Dr. Chang and colleagues wrote.
Conditional recommendations with moderate certainty in evidence are provided for tenapanor, plecanatide, tegaserod, and lubiprostone. Recommendations for polyethylene glycol laxatives, tricyclic antidepressants and antispasmodics are conditional and based on low-certainty evidence, as well as a conditional recommendation against selective serotonin reuptake inhibitors, also based on low-certainty evidence.
IBS-D
The IBS-D guidelines, led by co–first authors Anthony Lembo, MD, AGAF, of Beth Israel Deaconess Medical Center, Boston, and Dr. Sultan, includes eight conditional recommendations with certainty in evidence ranging from very low to moderate.
Drugs recommended based on moderate-certainty evidence include eluxadoline, alosetron, and rifaximin, with the added note that patients who respond to rifaximin but have recurrence should be treated again with rifaximin. Low-certainty evidence supported recommendations for tricyclic antidepressants, and antispasmodics. Very low–certainty evidence stands behind a recommendation for loperamide. Again, the panel made a conditional recommendation against SSRIs, also based on low-certainty evidence.
Shared decision-making
Both publications concluded with similar statements about the importance of shared decision-making, plus a practical mindset, in management of IBS.
“Acknowledging that multimodal treatments that include dietary and behavioral approaches in conjunction with drug therapy may provide maximal benefits and that treatment choices may be influenced by patient preferences, practitioners should engage in shared decision-making with patients when choosing the best therapy,” Dr. Lembo and colleagues wrote. “The importance of the patient-physician relationship is paramount in caring for individuals with IBS, and understanding patient preferences (for side-effect tolerability as well as cost) is valuable in choosing the right therapy.”
Both guidelines noted that some newer drugs for IBS have no generic alternative, and preauthorization may be required. Payer approval may depend on previous treatment failure with generic alternatives, they added.
The guidelines were commissioned and funded by the AGA Institute. The authors disclosed relationships with Ardelyx, Immunic, Protagonist, and others.
The American Gastroenterological Association has issued new guidelines for the medical treatment of irritable bowel syndrome (IBS).
The guidelines, which are separated into one publication for IBS with constipation (IBS-C) and another for IBS with diarrhea (IBS-D), are the first to advise clinicians in the usage of new, old, and over-the-counter drugs for IBS, according to a press release from the AGA.
“With more treatments available, physicians can tailor a personalized approach based on the symptoms a patient with IBS is experiencing,” AGA said.
Published simultaneously in Gastroenterology, the two guidelines describe a shared rationale for their creation, noting how the treatment landscape has changed since the AGA last issued IBS guidelines in 2014.
“New pharmacological treatments have become available and new evidence has accumulated about established treatments,” both guidelines stated. “The purpose of these guidelines is to provide evidence-based recommendations for the pharmacologic management” of individuals with IBS “based on a systematic and comprehensive synthesis of the literature.”
IBS-C
In the IBS-C guidelines, co–first authors Lin Chang, MD, AGAF, of the University of Los Angeles, and Shahnaz Sultan, MD, MHSc, AGAF, of the Minneapolis Veterans Affairs Healthcare System, noted that IBS-C accounts for “more than a third of IBS cases,” with patients frequently reporting “feeling self-conscious, avoiding sex, difficulty concentrating, [and] not feeling able to reach one’s full potential.”
They offered nine pharmacologic recommendations, eight of which are conditional, with certainty in evidence ranging from low to high.
The only strong recommendation with a high certainty in evidence is for linaclotide.
“Across four RCTs [randomized controlled trials], linaclotide improved global assessment of IBS-C symptoms (FDA responder), abdominal pain, complete spontaneous bowel movement response, as well as adequate global response,” Dr. Chang and colleagues wrote.
Conditional recommendations with moderate certainty in evidence are provided for tenapanor, plecanatide, tegaserod, and lubiprostone. Recommendations for polyethylene glycol laxatives, tricyclic antidepressants and antispasmodics are conditional and based on low-certainty evidence, as well as a conditional recommendation against selective serotonin reuptake inhibitors, also based on low-certainty evidence.
IBS-D
The IBS-D guidelines, led by co–first authors Anthony Lembo, MD, AGAF, of Beth Israel Deaconess Medical Center, Boston, and Dr. Sultan, includes eight conditional recommendations with certainty in evidence ranging from very low to moderate.
Drugs recommended based on moderate-certainty evidence include eluxadoline, alosetron, and rifaximin, with the added note that patients who respond to rifaximin but have recurrence should be treated again with rifaximin. Low-certainty evidence supported recommendations for tricyclic antidepressants, and antispasmodics. Very low–certainty evidence stands behind a recommendation for loperamide. Again, the panel made a conditional recommendation against SSRIs, also based on low-certainty evidence.
Shared decision-making
Both publications concluded with similar statements about the importance of shared decision-making, plus a practical mindset, in management of IBS.
“Acknowledging that multimodal treatments that include dietary and behavioral approaches in conjunction with drug therapy may provide maximal benefits and that treatment choices may be influenced by patient preferences, practitioners should engage in shared decision-making with patients when choosing the best therapy,” Dr. Lembo and colleagues wrote. “The importance of the patient-physician relationship is paramount in caring for individuals with IBS, and understanding patient preferences (for side-effect tolerability as well as cost) is valuable in choosing the right therapy.”
Both guidelines noted that some newer drugs for IBS have no generic alternative, and preauthorization may be required. Payer approval may depend on previous treatment failure with generic alternatives, they added.
The guidelines were commissioned and funded by the AGA Institute. The authors disclosed relationships with Ardelyx, Immunic, Protagonist, and others.
FROM GASTROENTEROLOGY
Center-based childcare associated with healthier body weight
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
FROM NUTRITION 2022
AGA issues position statements on reducing CRC burden
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”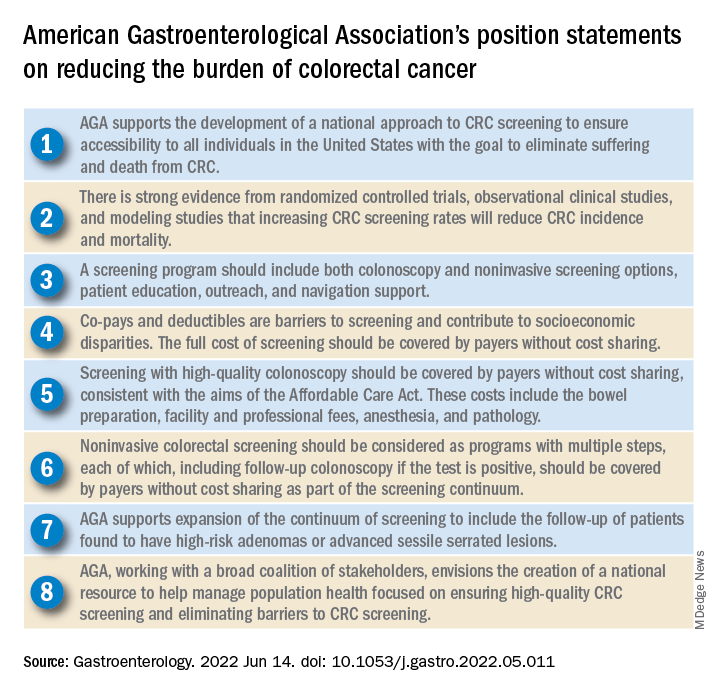
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
Groups interested in collaborating with AGA should contact Kathleen Teixeira, AGA Vice President, Public Policy and Advocacy, at [email protected].
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”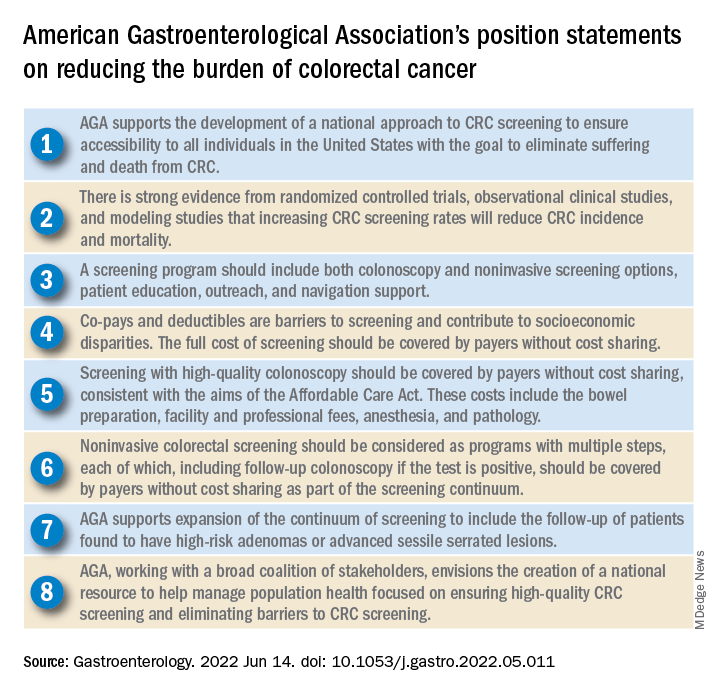
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
Groups interested in collaborating with AGA should contact Kathleen Teixeira, AGA Vice President, Public Policy and Advocacy, at [email protected].
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”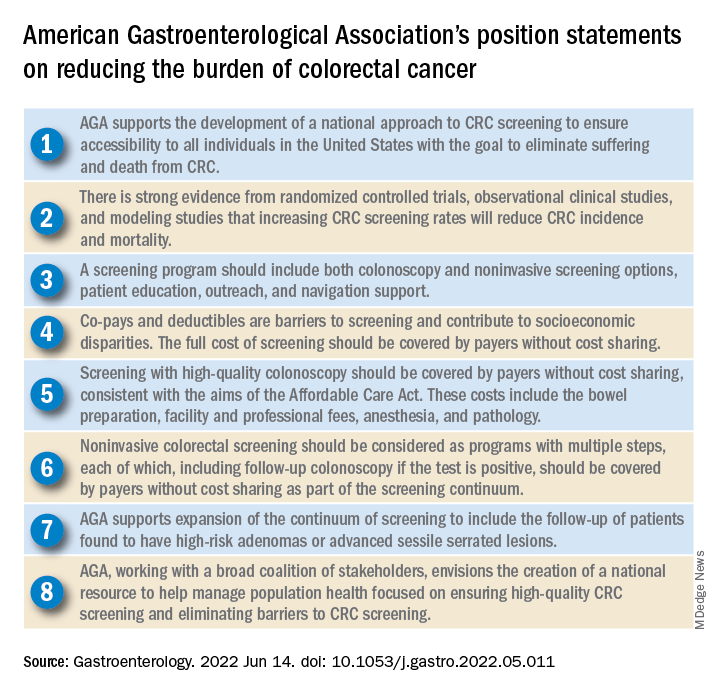
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
Groups interested in collaborating with AGA should contact Kathleen Teixeira, AGA Vice President, Public Policy and Advocacy, at [email protected].
FROM GASTROENTEROLOGY
AGA issues position statements on reducing CRC burden
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
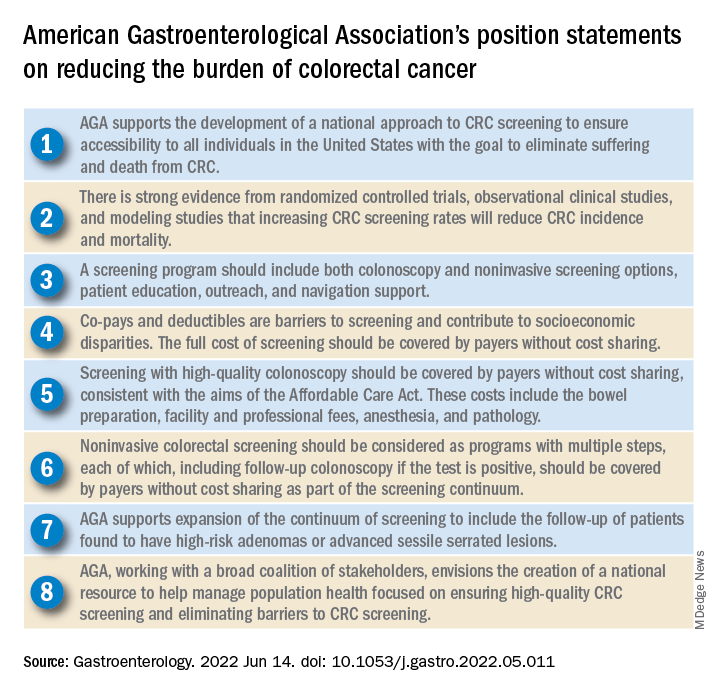
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
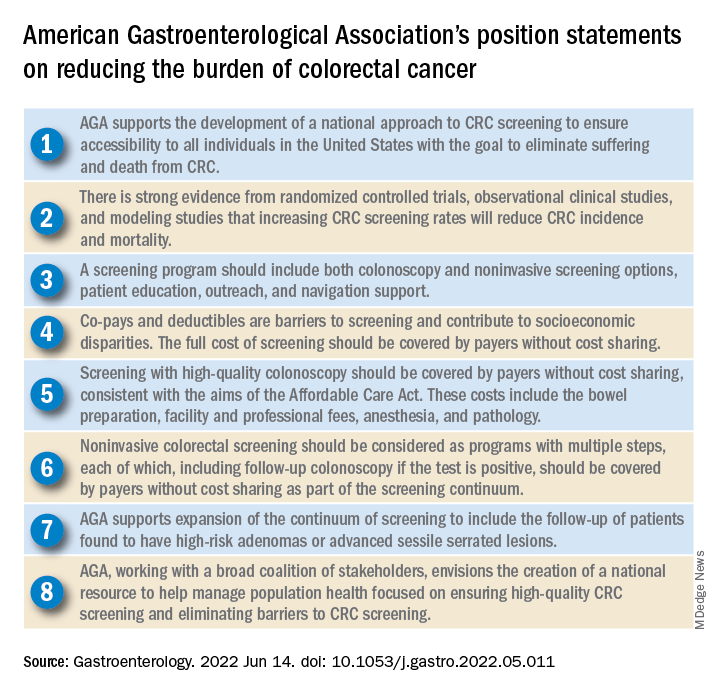
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
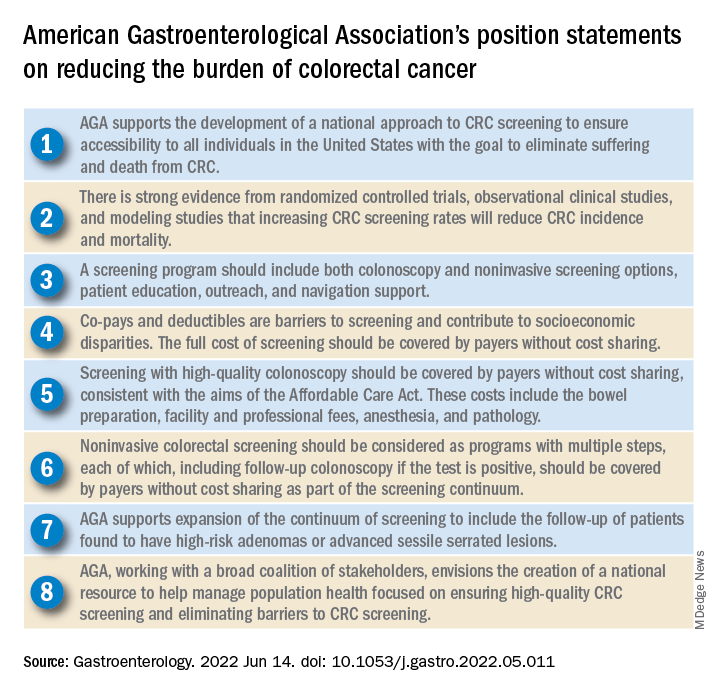
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
FROM GASTROENTEROLOGY
Cannabis may relieve pain as effectively as opioids, but more research is needed
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE