User login
Case Report: An Unusual Case of Arrhythmia
Case
A 3-year-old girl presented to the ED with a 1-week history of cough and new-onset abdominal pain. She was accompanied by her grandfather, who stated that the child had been dropped-off at his house around 5:00 pm the previous day. He noted that after putting his granddaughter to bed, she awoke around 4:30 am complaining of a stomachache. After rocking her, he said she went back to sleep but did not wake up again until 1:00 pm that afternoon. Over the first few hours of awakening, she became less active and had three episodes of posttussive emesis. The grandfather denied the child had any recent nasal congestion, fever, nausea, vomiting, or diarrhea. When questioned about possible toxic ingestion, he said there were no medications in the house and that he did not witness any substance ingestion or trauma.
At presentation, the patient’s vital signs were: blood pressure (BP) 86/49 mm Hg; heart rate (HR), 178 beats/minute and regular; respiratory rate (RR), 26 breaths/minute; temporal artery temperature, 104.7°F. Oxygen saturation was 99% on room air. On physical examination, she was normocephalic; there was no scleral icterus; and the throat and bilateral tympanic membranes were normal. Her extremities were warm and well perfused, with normal capillary refill. Patient’s lungs were clear, and heart sounds were normal with no detection of a murmur. The abdomen was soft and nontender; there was no evidence of organomegaly.
Laboratory evaluation included assessment of sodium, chloride, carbon dioxide, calcium, magnesium, amylase, lipase, and creatine levels; liver function test; complete blood count; and red-cell indices. All of the laboratory values were within normal limits, and urinalysis was negative for infection. Blood and urine cultures were also taken. A chest X-ray showed no acute intrathoracic process (Figure 1).
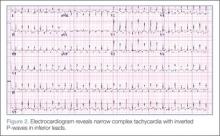
During treatment, the patient became increasingly fussy with new-onset abdominal distension. Repeat physical examination revealed hepatomegaly. A bedside echocardiogram showed hyperdynamic heart with fractional shortening* (FS) of 20% and ejection fraction (EF) of 43%, but no structural abnormalities. An electrocardiogram (ECG) was then ordered, which revealed narrow complex tachycardia with inverted P-waves in inferior leads.
Discussion
Normal cardiac conduction involves an originating impulse from a sinus node followed by atrial muscle activation reaching the atrioventricular (AV) node. There is a necessary delay at the AV node, which is required for ventricular filling and activation of ventricles through the His-Purkinje fiber system and the bundle branches. An abnormality or interruption of this pathway results in an arrhythmia such as supraventricular tachycardia (SVT).
Supraventricular Tachycardia
Supraventricular tachycardia is the most common symptomatic abnormality in the pediatric population.1 Among the various forms of SVT, AV reentrant tachycardia (AVRT) and AV node reentrant tachycardia (AVNRT) account for most case presentations.2 Supraventricular tachycardia may be classified by duration of RP interval compared to PR interval on ECG. Short RP interval SVT includes AVNRT and AVRT through a rapidly conducting accessory path. Long RP interval SVT includes atypical AVNRT, atrial tachycardia, and PJRT.
Persistent Junctional Reentrant Tachycardia
Persistent junctional reentrant tachycardia is a rare form of long RP tachycardia, accounting for approximately 1% of SVT in a study review of 21 patients.3 As with the patient in this case, PJRT usually presents in early childhood.3 In a recent review of 194 patients with PJRT, 57% were infants.4 The condition involves an accessory pathway most commonly located in the posterior-superior septal region; conduction involves a retrograde impulse through the decremental accessory pathway.5 On ECG, findings include a negative P wave in inferior leads, a long RP interval, and a 1:1 AV conduction.6
A long-term multicenter follow-up study of 32 patients showed that rates of tachycardia vary among patients, from 100 to 250 beats/minute.7 Tachycardia-induced cardiomyopathy (TIC), which is secondary to the incessant nature of tachycardia, may be present in up to 30% to 50% of patients.3,8 In a recent multicenter study, PJRT was responsible for 23% of cases of TIC.9 Although the exact mechanism of this property is unknown, decremental conduction and unidirectional block of the accessory pathway appear to be contributing factors.6
Treatment
Adenosine is the initial drug of choice for narrow complex tachycardia with stable hemodynamic status and an available intravascular access.10 In a study evaluating the effectiveness of adenosine for managing SVT in the pediatric ED setting, it was more than 70% effective in cardioverting patients presumed to have SVT.11 However, in PJRT, owing to the incessant pattern, adenosine may either terminate the tachycardia (causing asystole) or, as seen in this patient, convert tachycardia to sinus rhythm for only a few seconds.12 Reinitiation of tachycardia in sinus beat without the need for a premature complex contributes to its incessant nature.13
In a multicenter study looking at clinical profile and outcome for PJRT, Vaksmann et al8 found a greater than 80% success rate in controlling the dysrhythmia with amiodarone and verapamil. For long-term management of tachyarrhythmia, medical therapy has been recommended in early childhood compared to older children in whom catheter ablation is an effective approach.7 Spontaneous resolution of PJRT has been documented but is rare.14
Conclusion
Pediatric cardiac emergencies require very specific treatment. As such, it is important that the emergency physician distinguish the different the types of tachyarrhythmias—especially in cases that do not respond to treatment with adenosine. In the pediatric patient, PJRT is a potentially life-threatening arrhythmia that requires a high index of suspicion. Clues to diagnosis include negative P waves in inferior leads, long RP interval, and 1:1 atrioventricular conduction.
Dr Fichadia is a fellow, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan. Dr Perez is a clinical instructor, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan.
- Doniger SJ, Sharieff GQ. Pediatric dysrhythmias. Pediatr Clin North Am. 2006; 53(1):85-105, vi.
- Ko JK, Deal BJ, Strasburger JF, Benson DW Jr. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992;69(12):1028-1032.
- Dorostkar PC, Silka MJ, Morady F, Dick M 2nd. Clinical course of persistent junctional reciprocating tachycardia. J Am Coll Cardiol. 1999;33(2):366-375.
- Kang KT, Potts JE, Radbill AE, et al. Permanent junctional reciprocating tachycardia in children: A multi-center experience: Permanent junctional reciprocating tachycardia [published online ahead of print April 24, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.033.
- Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia: diagnosis and management. Mayo Clin Proc. 2008;83(12):1400-1411.
- O’Neill BJ, Klein GJ, Guiraudon GM, et al. Results of operative therapy in the permanent form of junctional reciprocating tachycardia. Am J Cardiol. 1989;63(15):1074-1079.
- Lindinger A, Heisel A, von Bernuth G, et al., Permanent junctional re-entry tachycardia. A multicentre long-term follow-up study in infants, children and young adults. Eur Heart J. 1998;19(6):936-942.
- Vaksmann G, D’Hoinne C, Lucet V. Permanent junctional reciprocating tachycardia in children: a multicentre study on clinical profile and outcome. Heart. 2006;92(1):101-104.
- Moore JP, Patel PA, Shannon KM, et al. Predictors of Myocardial Recovery in Pediatric Tachycardia-Induced Cardiomyopathy [published online ahead of print April 18, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.023.
- Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S876-S908.
- Losek JD, Endom E, Dietrich A, Stewart G, Zempsky W, Smith K. Adenosine and pediatric supraventricular tachycardia in the emergency department: multicenter study and review. Ann Emerg Med. 1999;33(2):185-191.
- Waisman Y, Berman S, Fogelman R, Zeevi B, Mimouni M. Failure of adenosine to convert subtype of supraventricular tachycardia. Israeli J Emerg Med. 2003;3(2):4-7.
- Ho, Reginald T. Unusual manifestations of accessory pathways. In: Electrophysiology of Arrhythmias: Practical Images for Diagnosis and Ablation. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:167.
- Brugada J, Blom N, Sarquella-Brugada G, et al; European Heart Rhythm Association; Association for European Paediatric and Congenital Cardiology. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace. 2013;15(9):1337-1382.
* Fractional shortening is the percent of shortening of left ventricular diameter between end-diastole to end-systole with a normal range of 28% to 44%. In the presence of myocardial depression, FS values are reduced.
Case
A 3-year-old girl presented to the ED with a 1-week history of cough and new-onset abdominal pain. She was accompanied by her grandfather, who stated that the child had been dropped-off at his house around 5:00 pm the previous day. He noted that after putting his granddaughter to bed, she awoke around 4:30 am complaining of a stomachache. After rocking her, he said she went back to sleep but did not wake up again until 1:00 pm that afternoon. Over the first few hours of awakening, she became less active and had three episodes of posttussive emesis. The grandfather denied the child had any recent nasal congestion, fever, nausea, vomiting, or diarrhea. When questioned about possible toxic ingestion, he said there were no medications in the house and that he did not witness any substance ingestion or trauma.
At presentation, the patient’s vital signs were: blood pressure (BP) 86/49 mm Hg; heart rate (HR), 178 beats/minute and regular; respiratory rate (RR), 26 breaths/minute; temporal artery temperature, 104.7°F. Oxygen saturation was 99% on room air. On physical examination, she was normocephalic; there was no scleral icterus; and the throat and bilateral tympanic membranes were normal. Her extremities were warm and well perfused, with normal capillary refill. Patient’s lungs were clear, and heart sounds were normal with no detection of a murmur. The abdomen was soft and nontender; there was no evidence of organomegaly.
Laboratory evaluation included assessment of sodium, chloride, carbon dioxide, calcium, magnesium, amylase, lipase, and creatine levels; liver function test; complete blood count; and red-cell indices. All of the laboratory values were within normal limits, and urinalysis was negative for infection. Blood and urine cultures were also taken. A chest X-ray showed no acute intrathoracic process (Figure 1).
During treatment, the patient became increasingly fussy with new-onset abdominal distension. Repeat physical examination revealed hepatomegaly. A bedside echocardiogram showed hyperdynamic heart with fractional shortening* (FS) of 20% and ejection fraction (EF) of 43%, but no structural abnormalities. An electrocardiogram (ECG) was then ordered, which revealed narrow complex tachycardia with inverted P-waves in inferior leads.
Discussion
Normal cardiac conduction involves an originating impulse from a sinus node followed by atrial muscle activation reaching the atrioventricular (AV) node. There is a necessary delay at the AV node, which is required for ventricular filling and activation of ventricles through the His-Purkinje fiber system and the bundle branches. An abnormality or interruption of this pathway results in an arrhythmia such as supraventricular tachycardia (SVT).
Supraventricular Tachycardia
Supraventricular tachycardia is the most common symptomatic abnormality in the pediatric population.1 Among the various forms of SVT, AV reentrant tachycardia (AVRT) and AV node reentrant tachycardia (AVNRT) account for most case presentations.2 Supraventricular tachycardia may be classified by duration of RP interval compared to PR interval on ECG. Short RP interval SVT includes AVNRT and AVRT through a rapidly conducting accessory path. Long RP interval SVT includes atypical AVNRT, atrial tachycardia, and PJRT.
Persistent Junctional Reentrant Tachycardia
Persistent junctional reentrant tachycardia is a rare form of long RP tachycardia, accounting for approximately 1% of SVT in a study review of 21 patients.3 As with the patient in this case, PJRT usually presents in early childhood.3 In a recent review of 194 patients with PJRT, 57% were infants.4 The condition involves an accessory pathway most commonly located in the posterior-superior septal region; conduction involves a retrograde impulse through the decremental accessory pathway.5 On ECG, findings include a negative P wave in inferior leads, a long RP interval, and a 1:1 AV conduction.6
A long-term multicenter follow-up study of 32 patients showed that rates of tachycardia vary among patients, from 100 to 250 beats/minute.7 Tachycardia-induced cardiomyopathy (TIC), which is secondary to the incessant nature of tachycardia, may be present in up to 30% to 50% of patients.3,8 In a recent multicenter study, PJRT was responsible for 23% of cases of TIC.9 Although the exact mechanism of this property is unknown, decremental conduction and unidirectional block of the accessory pathway appear to be contributing factors.6
Treatment
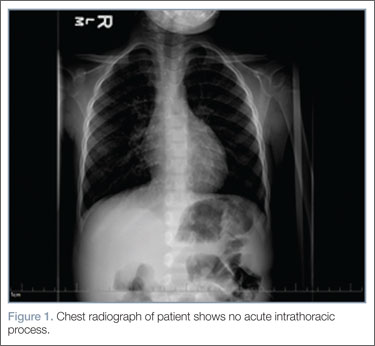
Adenosine is the initial drug of choice for narrow complex tachycardia with stable hemodynamic status and an available intravascular access.10 In a study evaluating the effectiveness of adenosine for managing SVT in the pediatric ED setting, it was more than 70% effective in cardioverting patients presumed to have SVT.11 However, in PJRT, owing to the incessant pattern, adenosine may either terminate the tachycardia (causing asystole) or, as seen in this patient, convert tachycardia to sinus rhythm for only a few seconds.12 Reinitiation of tachycardia in sinus beat without the need for a premature complex contributes to its incessant nature.13
In a multicenter study looking at clinical profile and outcome for PJRT, Vaksmann et al8 found a greater than 80% success rate in controlling the dysrhythmia with amiodarone and verapamil. For long-term management of tachyarrhythmia, medical therapy has been recommended in early childhood compared to older children in whom catheter ablation is an effective approach.7 Spontaneous resolution of PJRT has been documented but is rare.14
Conclusion
Pediatric cardiac emergencies require very specific treatment. As such, it is important that the emergency physician distinguish the different the types of tachyarrhythmias—especially in cases that do not respond to treatment with adenosine. In the pediatric patient, PJRT is a potentially life-threatening arrhythmia that requires a high index of suspicion. Clues to diagnosis include negative P waves in inferior leads, long RP interval, and 1:1 atrioventricular conduction.
Dr Fichadia is a fellow, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan. Dr Perez is a clinical instructor, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan.
Case
A 3-year-old girl presented to the ED with a 1-week history of cough and new-onset abdominal pain. She was accompanied by her grandfather, who stated that the child had been dropped-off at his house around 5:00 pm the previous day. He noted that after putting his granddaughter to bed, she awoke around 4:30 am complaining of a stomachache. After rocking her, he said she went back to sleep but did not wake up again until 1:00 pm that afternoon. Over the first few hours of awakening, she became less active and had three episodes of posttussive emesis. The grandfather denied the child had any recent nasal congestion, fever, nausea, vomiting, or diarrhea. When questioned about possible toxic ingestion, he said there were no medications in the house and that he did not witness any substance ingestion or trauma.
At presentation, the patient’s vital signs were: blood pressure (BP) 86/49 mm Hg; heart rate (HR), 178 beats/minute and regular; respiratory rate (RR), 26 breaths/minute; temporal artery temperature, 104.7°F. Oxygen saturation was 99% on room air. On physical examination, she was normocephalic; there was no scleral icterus; and the throat and bilateral tympanic membranes were normal. Her extremities were warm and well perfused, with normal capillary refill. Patient’s lungs were clear, and heart sounds were normal with no detection of a murmur. The abdomen was soft and nontender; there was no evidence of organomegaly.
Laboratory evaluation included assessment of sodium, chloride, carbon dioxide, calcium, magnesium, amylase, lipase, and creatine levels; liver function test; complete blood count; and red-cell indices. All of the laboratory values were within normal limits, and urinalysis was negative for infection. Blood and urine cultures were also taken. A chest X-ray showed no acute intrathoracic process (Figure 1).
During treatment, the patient became increasingly fussy with new-onset abdominal distension. Repeat physical examination revealed hepatomegaly. A bedside echocardiogram showed hyperdynamic heart with fractional shortening* (FS) of 20% and ejection fraction (EF) of 43%, but no structural abnormalities. An electrocardiogram (ECG) was then ordered, which revealed narrow complex tachycardia with inverted P-waves in inferior leads.
Discussion
Normal cardiac conduction involves an originating impulse from a sinus node followed by atrial muscle activation reaching the atrioventricular (AV) node. There is a necessary delay at the AV node, which is required for ventricular filling and activation of ventricles through the His-Purkinje fiber system and the bundle branches. An abnormality or interruption of this pathway results in an arrhythmia such as supraventricular tachycardia (SVT).
Supraventricular Tachycardia
Supraventricular tachycardia is the most common symptomatic abnormality in the pediatric population.1 Among the various forms of SVT, AV reentrant tachycardia (AVRT) and AV node reentrant tachycardia (AVNRT) account for most case presentations.2 Supraventricular tachycardia may be classified by duration of RP interval compared to PR interval on ECG. Short RP interval SVT includes AVNRT and AVRT through a rapidly conducting accessory path. Long RP interval SVT includes atypical AVNRT, atrial tachycardia, and PJRT.
Persistent Junctional Reentrant Tachycardia
Persistent junctional reentrant tachycardia is a rare form of long RP tachycardia, accounting for approximately 1% of SVT in a study review of 21 patients.3 As with the patient in this case, PJRT usually presents in early childhood.3 In a recent review of 194 patients with PJRT, 57% were infants.4 The condition involves an accessory pathway most commonly located in the posterior-superior septal region; conduction involves a retrograde impulse through the decremental accessory pathway.5 On ECG, findings include a negative P wave in inferior leads, a long RP interval, and a 1:1 AV conduction.6
A long-term multicenter follow-up study of 32 patients showed that rates of tachycardia vary among patients, from 100 to 250 beats/minute.7 Tachycardia-induced cardiomyopathy (TIC), which is secondary to the incessant nature of tachycardia, may be present in up to 30% to 50% of patients.3,8 In a recent multicenter study, PJRT was responsible for 23% of cases of TIC.9 Although the exact mechanism of this property is unknown, decremental conduction and unidirectional block of the accessory pathway appear to be contributing factors.6
Treatment
Adenosine is the initial drug of choice for narrow complex tachycardia with stable hemodynamic status and an available intravascular access.10 In a study evaluating the effectiveness of adenosine for managing SVT in the pediatric ED setting, it was more than 70% effective in cardioverting patients presumed to have SVT.11 However, in PJRT, owing to the incessant pattern, adenosine may either terminate the tachycardia (causing asystole) or, as seen in this patient, convert tachycardia to sinus rhythm for only a few seconds.12 Reinitiation of tachycardia in sinus beat without the need for a premature complex contributes to its incessant nature.13
In a multicenter study looking at clinical profile and outcome for PJRT, Vaksmann et al8 found a greater than 80% success rate in controlling the dysrhythmia with amiodarone and verapamil. For long-term management of tachyarrhythmia, medical therapy has been recommended in early childhood compared to older children in whom catheter ablation is an effective approach.7 Spontaneous resolution of PJRT has been documented but is rare.14
Conclusion
Pediatric cardiac emergencies require very specific treatment. As such, it is important that the emergency physician distinguish the different the types of tachyarrhythmias—especially in cases that do not respond to treatment with adenosine. In the pediatric patient, PJRT is a potentially life-threatening arrhythmia that requires a high index of suspicion. Clues to diagnosis include negative P waves in inferior leads, long RP interval, and 1:1 atrioventricular conduction.
Dr Fichadia is a fellow, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan. Dr Perez is a clinical instructor, pediatric emergency medicine, Wayne State University, Children’s Hospital of Michigan.
- Doniger SJ, Sharieff GQ. Pediatric dysrhythmias. Pediatr Clin North Am. 2006; 53(1):85-105, vi.
- Ko JK, Deal BJ, Strasburger JF, Benson DW Jr. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992;69(12):1028-1032.
- Dorostkar PC, Silka MJ, Morady F, Dick M 2nd. Clinical course of persistent junctional reciprocating tachycardia. J Am Coll Cardiol. 1999;33(2):366-375.
- Kang KT, Potts JE, Radbill AE, et al. Permanent junctional reciprocating tachycardia in children: A multi-center experience: Permanent junctional reciprocating tachycardia [published online ahead of print April 24, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.033.
- Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia: diagnosis and management. Mayo Clin Proc. 2008;83(12):1400-1411.
- O’Neill BJ, Klein GJ, Guiraudon GM, et al. Results of operative therapy in the permanent form of junctional reciprocating tachycardia. Am J Cardiol. 1989;63(15):1074-1079.
- Lindinger A, Heisel A, von Bernuth G, et al., Permanent junctional re-entry tachycardia. A multicentre long-term follow-up study in infants, children and young adults. Eur Heart J. 1998;19(6):936-942.
- Vaksmann G, D’Hoinne C, Lucet V. Permanent junctional reciprocating tachycardia in children: a multicentre study on clinical profile and outcome. Heart. 2006;92(1):101-104.
- Moore JP, Patel PA, Shannon KM, et al. Predictors of Myocardial Recovery in Pediatric Tachycardia-Induced Cardiomyopathy [published online ahead of print April 18, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.023.
- Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S876-S908.
- Losek JD, Endom E, Dietrich A, Stewart G, Zempsky W, Smith K. Adenosine and pediatric supraventricular tachycardia in the emergency department: multicenter study and review. Ann Emerg Med. 1999;33(2):185-191.
- Waisman Y, Berman S, Fogelman R, Zeevi B, Mimouni M. Failure of adenosine to convert subtype of supraventricular tachycardia. Israeli J Emerg Med. 2003;3(2):4-7.
- Ho, Reginald T. Unusual manifestations of accessory pathways. In: Electrophysiology of Arrhythmias: Practical Images for Diagnosis and Ablation. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:167.
- Brugada J, Blom N, Sarquella-Brugada G, et al; European Heart Rhythm Association; Association for European Paediatric and Congenital Cardiology. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace. 2013;15(9):1337-1382.
* Fractional shortening is the percent of shortening of left ventricular diameter between end-diastole to end-systole with a normal range of 28% to 44%. In the presence of myocardial depression, FS values are reduced.
- Doniger SJ, Sharieff GQ. Pediatric dysrhythmias. Pediatr Clin North Am. 2006; 53(1):85-105, vi.
- Ko JK, Deal BJ, Strasburger JF, Benson DW Jr. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992;69(12):1028-1032.
- Dorostkar PC, Silka MJ, Morady F, Dick M 2nd. Clinical course of persistent junctional reciprocating tachycardia. J Am Coll Cardiol. 1999;33(2):366-375.
- Kang KT, Potts JE, Radbill AE, et al. Permanent junctional reciprocating tachycardia in children: A multi-center experience: Permanent junctional reciprocating tachycardia [published online ahead of print April 24, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.033.
- Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia: diagnosis and management. Mayo Clin Proc. 2008;83(12):1400-1411.
- O’Neill BJ, Klein GJ, Guiraudon GM, et al. Results of operative therapy in the permanent form of junctional reciprocating tachycardia. Am J Cardiol. 1989;63(15):1074-1079.
- Lindinger A, Heisel A, von Bernuth G, et al., Permanent junctional re-entry tachycardia. A multicentre long-term follow-up study in infants, children and young adults. Eur Heart J. 1998;19(6):936-942.
- Vaksmann G, D’Hoinne C, Lucet V. Permanent junctional reciprocating tachycardia in children: a multicentre study on clinical profile and outcome. Heart. 2006;92(1):101-104.
- Moore JP, Patel PA, Shannon KM, et al. Predictors of Myocardial Recovery in Pediatric Tachycardia-Induced Cardiomyopathy [published online ahead of print April 18, 2014]. Heart Rhythm. doi:10.1016/j.hrthm.2014.04.023.
- Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S876-S908.
- Losek JD, Endom E, Dietrich A, Stewart G, Zempsky W, Smith K. Adenosine and pediatric supraventricular tachycardia in the emergency department: multicenter study and review. Ann Emerg Med. 1999;33(2):185-191.
- Waisman Y, Berman S, Fogelman R, Zeevi B, Mimouni M. Failure of adenosine to convert subtype of supraventricular tachycardia. Israeli J Emerg Med. 2003;3(2):4-7.
- Ho, Reginald T. Unusual manifestations of accessory pathways. In: Electrophysiology of Arrhythmias: Practical Images for Diagnosis and Ablation. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:167.
- Brugada J, Blom N, Sarquella-Brugada G, et al; European Heart Rhythm Association; Association for European Paediatric and Congenital Cardiology. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace. 2013;15(9):1337-1382.
* Fractional shortening is the percent of shortening of left ventricular diameter between end-diastole to end-systole with a normal range of 28% to 44%. In the presence of myocardial depression, FS values are reduced.