User login
Tom Collins is a freelance writer in South Florida who has written about medical topics from nasty infections to ethical dilemmas, runaway tumors to tornado-chasing doctors. He travels the globe gathering conference health news and lives in West Palm Beach.
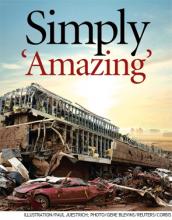
Devastating Superstorm Gone, But Not Forgotten in Moore, Okla.

–Joe R. Womble, MD
The first bit of feedback was fantastic: Everyone who had been inside the hospital—roughly 200 to 300 people, including 30 patients—had survived.
“Everyone was fine,” he said. “All the patients and staff, no one got injured. I was thinking that either the hospital was missed by the storm or that it must not have really damaged it very significantly.”
Unfortunately, the hospital was not OK. He watched as local TV painted a very different picture.
“They started showing aerial shots and I was just shocked. My jaw was just dropped,” Dr. Womble said. “The main entrance that I go in every day was literally stacked with three or four cars deep. A huge stack of about 30 cars was piled up on the main entrance, essentially.”
It was as though they were “toy cars.”
The May 20 tornado, a two-mile-wide superstorm boasting 200-mph winds that struck just south of Oklahoma City, claimed 24 lives and left the regional health system with a void in its network. It also left hospitalists mourning the loss of the place they called a second home several times a week. About a week after the storm, officials announced that Moore Medical Center would have to be demolished.
Miraculous Moments
Despite the terrible events, hospitalists and hospital officials were astounded by the good fortune of the hospital’s inhabitants. Dr. Womble said about 100 people from nearby neighborhoods and businesses used the hospital as shelter.
Senthil Raju, MD, a hospitalist who had done rounds at Moore Medical earlier that day, said the protocol was to take shelter in the hallways. But at some point, probably only minutes before the storm hit, the chief nurse and the house supervisor made the decision to move all the patients to the ground floor because they were in “reasonably stable condition,” according to Dr. Womble, who relayed accounts by staffers who were there. Most of the people in the hospital rode out the storm in the first-floor cafeteria.
After the storm, patient rooms on the second floor were either no longer there or had been reduced to their steel innards.
The decision to move everyone undoubtedly saved lives. “If any of our patients stayed there, they’re probably all dead,” Dr. Raju said.
David Whitaker, CEO of Norman Regional Health System, which includes Moore Medical, marveled at the outcome.
“We had some bumps and bruises, some scratches, but no major lacerations, no broken bones, no injuries that people couldn’t ambulate. It’s totally amazing,” he said. “The leadership that was in place, the employees that were working at that time, they sprang into action, they took command and control of the situation. They got people into the proper areas.”
Dr. Womble said hospital staff at Moore Medical had still more amazing stories of death-defiance. They told him 30 people refused to leave the chapel. Somehow, the chapel remained intact, even though the hospital all around it was destroyed. Whitaker confirmed this.
One woman in active labor was kept in a second-floor operating room—which the medical staff thought was the best place for her, all things considered. Nurses covered the woman with pillows, blankets, and their own bodies as the tornado barreled through the town. She survived and gave birth to a boy several hours later. The parents gave him the middle name Emmanuel, which means “God is with us.”
As the tornado approached, an elderly volunteer had gone outside to get something from a van he used to transport elderly patients to and from a physical therapy program. “Nobody inside knew he had gone outside,” Dr. Womble said. By the time he tried to get back in, the power had gone out, and the doors wouldn’t open. He huddled behind a concrete pillar and ended up with just one minor laceration.
Patients eventually were taken to another hospital, Norman’s HealthPlex, about five miles south. Both Dr. Womble and Dr. Raju have begun working full time at the HealthPlex.
Dr. Raju said that he avoided being at Moore Medical during the tornado only by a turn of luck. He normally rounds at Moore in the afternoon and at the HealthPlex in the morning. But on that day, there were three new admissions at Moore, and only one at HealthPlex. So he went to Moore first, and was gone by the time the tornado hit.
“So lucky,” he said.

–David Whitaker, CEO of Norman Regional Health System
The Aftermath
It remains to be seen what kind of medical facility will be built to replace Moore Medical Center.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” said Dr. Womble, who had worked at Moore Medical Center for four years.
Whitaker said the first priority was to re-establish the clinics located at Moore Medical, and that has been done. The next step is, possibly, a temporary building in Moore for urgent care. The long-term plan remains in the discussion phase.
“We’ve already started having some meetings,” Whitaker said. “We’re going to determine what type of facility, what service levels it will be offering as we go back.”
It’s hard knowing that his hospital is no longer there, Dr. Raju said.
“We are going to miss it,” he said. “It’s unimaginable.”
Dr. Womble said those first few hours, when he wasn’t sure of where he’d be working, were difficult. He struggles to describe the feeling of not being able to provide care at his hospital at the time it’s most needed.
“It’s really hard to put it into words,” he said. “It’s the only hospital in that city, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem. I definitely feel a tie to the community.
“It’s devastating. What is the rest of the city going to do for their hospital care? They essentially will not have a hospital in their city. They’ll have to drive to another city for care.”
Tom Collins is a freelance writer in South Florida.

–Joe R. Womble, MD
The first bit of feedback was fantastic: Everyone who had been inside the hospital—roughly 200 to 300 people, including 30 patients—had survived.
“Everyone was fine,” he said. “All the patients and staff, no one got injured. I was thinking that either the hospital was missed by the storm or that it must not have really damaged it very significantly.”
Unfortunately, the hospital was not OK. He watched as local TV painted a very different picture.
“They started showing aerial shots and I was just shocked. My jaw was just dropped,” Dr. Womble said. “The main entrance that I go in every day was literally stacked with three or four cars deep. A huge stack of about 30 cars was piled up on the main entrance, essentially.”
It was as though they were “toy cars.”
The May 20 tornado, a two-mile-wide superstorm boasting 200-mph winds that struck just south of Oklahoma City, claimed 24 lives and left the regional health system with a void in its network. It also left hospitalists mourning the loss of the place they called a second home several times a week. About a week after the storm, officials announced that Moore Medical Center would have to be demolished.
Miraculous Moments
Despite the terrible events, hospitalists and hospital officials were astounded by the good fortune of the hospital’s inhabitants. Dr. Womble said about 100 people from nearby neighborhoods and businesses used the hospital as shelter.
Senthil Raju, MD, a hospitalist who had done rounds at Moore Medical earlier that day, said the protocol was to take shelter in the hallways. But at some point, probably only minutes before the storm hit, the chief nurse and the house supervisor made the decision to move all the patients to the ground floor because they were in “reasonably stable condition,” according to Dr. Womble, who relayed accounts by staffers who were there. Most of the people in the hospital rode out the storm in the first-floor cafeteria.
After the storm, patient rooms on the second floor were either no longer there or had been reduced to their steel innards.
The decision to move everyone undoubtedly saved lives. “If any of our patients stayed there, they’re probably all dead,” Dr. Raju said.
David Whitaker, CEO of Norman Regional Health System, which includes Moore Medical, marveled at the outcome.
“We had some bumps and bruises, some scratches, but no major lacerations, no broken bones, no injuries that people couldn’t ambulate. It’s totally amazing,” he said. “The leadership that was in place, the employees that were working at that time, they sprang into action, they took command and control of the situation. They got people into the proper areas.”
Dr. Womble said hospital staff at Moore Medical had still more amazing stories of death-defiance. They told him 30 people refused to leave the chapel. Somehow, the chapel remained intact, even though the hospital all around it was destroyed. Whitaker confirmed this.
One woman in active labor was kept in a second-floor operating room—which the medical staff thought was the best place for her, all things considered. Nurses covered the woman with pillows, blankets, and their own bodies as the tornado barreled through the town. She survived and gave birth to a boy several hours later. The parents gave him the middle name Emmanuel, which means “God is with us.”
As the tornado approached, an elderly volunteer had gone outside to get something from a van he used to transport elderly patients to and from a physical therapy program. “Nobody inside knew he had gone outside,” Dr. Womble said. By the time he tried to get back in, the power had gone out, and the doors wouldn’t open. He huddled behind a concrete pillar and ended up with just one minor laceration.
Patients eventually were taken to another hospital, Norman’s HealthPlex, about five miles south. Both Dr. Womble and Dr. Raju have begun working full time at the HealthPlex.
Dr. Raju said that he avoided being at Moore Medical during the tornado only by a turn of luck. He normally rounds at Moore in the afternoon and at the HealthPlex in the morning. But on that day, there were three new admissions at Moore, and only one at HealthPlex. So he went to Moore first, and was gone by the time the tornado hit.
“So lucky,” he said.

–David Whitaker, CEO of Norman Regional Health System
The Aftermath
It remains to be seen what kind of medical facility will be built to replace Moore Medical Center.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” said Dr. Womble, who had worked at Moore Medical Center for four years.
Whitaker said the first priority was to re-establish the clinics located at Moore Medical, and that has been done. The next step is, possibly, a temporary building in Moore for urgent care. The long-term plan remains in the discussion phase.
“We’ve already started having some meetings,” Whitaker said. “We’re going to determine what type of facility, what service levels it will be offering as we go back.”
It’s hard knowing that his hospital is no longer there, Dr. Raju said.
“We are going to miss it,” he said. “It’s unimaginable.”
Dr. Womble said those first few hours, when he wasn’t sure of where he’d be working, were difficult. He struggles to describe the feeling of not being able to provide care at his hospital at the time it’s most needed.
“It’s really hard to put it into words,” he said. “It’s the only hospital in that city, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem. I definitely feel a tie to the community.
“It’s devastating. What is the rest of the city going to do for their hospital care? They essentially will not have a hospital in their city. They’ll have to drive to another city for care.”
Tom Collins is a freelance writer in South Florida.

–Joe R. Womble, MD
The first bit of feedback was fantastic: Everyone who had been inside the hospital—roughly 200 to 300 people, including 30 patients—had survived.
“Everyone was fine,” he said. “All the patients and staff, no one got injured. I was thinking that either the hospital was missed by the storm or that it must not have really damaged it very significantly.”
Unfortunately, the hospital was not OK. He watched as local TV painted a very different picture.
“They started showing aerial shots and I was just shocked. My jaw was just dropped,” Dr. Womble said. “The main entrance that I go in every day was literally stacked with three or four cars deep. A huge stack of about 30 cars was piled up on the main entrance, essentially.”
It was as though they were “toy cars.”
The May 20 tornado, a two-mile-wide superstorm boasting 200-mph winds that struck just south of Oklahoma City, claimed 24 lives and left the regional health system with a void in its network. It also left hospitalists mourning the loss of the place they called a second home several times a week. About a week after the storm, officials announced that Moore Medical Center would have to be demolished.
Miraculous Moments
Despite the terrible events, hospitalists and hospital officials were astounded by the good fortune of the hospital’s inhabitants. Dr. Womble said about 100 people from nearby neighborhoods and businesses used the hospital as shelter.
Senthil Raju, MD, a hospitalist who had done rounds at Moore Medical earlier that day, said the protocol was to take shelter in the hallways. But at some point, probably only minutes before the storm hit, the chief nurse and the house supervisor made the decision to move all the patients to the ground floor because they were in “reasonably stable condition,” according to Dr. Womble, who relayed accounts by staffers who were there. Most of the people in the hospital rode out the storm in the first-floor cafeteria.
After the storm, patient rooms on the second floor were either no longer there or had been reduced to their steel innards.
The decision to move everyone undoubtedly saved lives. “If any of our patients stayed there, they’re probably all dead,” Dr. Raju said.
David Whitaker, CEO of Norman Regional Health System, which includes Moore Medical, marveled at the outcome.
“We had some bumps and bruises, some scratches, but no major lacerations, no broken bones, no injuries that people couldn’t ambulate. It’s totally amazing,” he said. “The leadership that was in place, the employees that were working at that time, they sprang into action, they took command and control of the situation. They got people into the proper areas.”
Dr. Womble said hospital staff at Moore Medical had still more amazing stories of death-defiance. They told him 30 people refused to leave the chapel. Somehow, the chapel remained intact, even though the hospital all around it was destroyed. Whitaker confirmed this.
One woman in active labor was kept in a second-floor operating room—which the medical staff thought was the best place for her, all things considered. Nurses covered the woman with pillows, blankets, and their own bodies as the tornado barreled through the town. She survived and gave birth to a boy several hours later. The parents gave him the middle name Emmanuel, which means “God is with us.”
As the tornado approached, an elderly volunteer had gone outside to get something from a van he used to transport elderly patients to and from a physical therapy program. “Nobody inside knew he had gone outside,” Dr. Womble said. By the time he tried to get back in, the power had gone out, and the doors wouldn’t open. He huddled behind a concrete pillar and ended up with just one minor laceration.
Patients eventually were taken to another hospital, Norman’s HealthPlex, about five miles south. Both Dr. Womble and Dr. Raju have begun working full time at the HealthPlex.
Dr. Raju said that he avoided being at Moore Medical during the tornado only by a turn of luck. He normally rounds at Moore in the afternoon and at the HealthPlex in the morning. But on that day, there were three new admissions at Moore, and only one at HealthPlex. So he went to Moore first, and was gone by the time the tornado hit.
“So lucky,” he said.

–David Whitaker, CEO of Norman Regional Health System
The Aftermath
It remains to be seen what kind of medical facility will be built to replace Moore Medical Center.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” said Dr. Womble, who had worked at Moore Medical Center for four years.
Whitaker said the first priority was to re-establish the clinics located at Moore Medical, and that has been done. The next step is, possibly, a temporary building in Moore for urgent care. The long-term plan remains in the discussion phase.
“We’ve already started having some meetings,” Whitaker said. “We’re going to determine what type of facility, what service levels it will be offering as we go back.”
It’s hard knowing that his hospital is no longer there, Dr. Raju said.
“We are going to miss it,” he said. “It’s unimaginable.”
Dr. Womble said those first few hours, when he wasn’t sure of where he’d be working, were difficult. He struggles to describe the feeling of not being able to provide care at his hospital at the time it’s most needed.
“It’s really hard to put it into words,” he said. “It’s the only hospital in that city, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem. I definitely feel a tie to the community.
“It’s devastating. What is the rest of the city going to do for their hospital care? They essentially will not have a hospital in their city. They’ll have to drive to another city for care.”
Tom Collins is a freelance writer in South Florida.
11 Things Neurologists Think Hospitalists Need To Know
11 Things: At a Glance
- You might be overdiagnosing transient ischemic attacks (TIA).
- Early mobilization after a stroke might be better for some patients.
- MRI is the best tool to evaluate TIA patients.
- Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
- Tracking the time a hospitalized patient was last seen to be normal is crucial.
- Consider neuromuscular disorders when a patient presents with weakness.
- Urinary tract infections (UTIs) are not the only cause of altered mental status.
- Take care in distinguishing aphasia from general confusion.
- A simple checklist might eliminate the need to consult the neurologist.
- Calling a neurologist earlier is way better than calling later.
- Hire a neurohospitalist if your institution doesn’t have one already.
When a patient is admitted to the hospital with neurological symptoms, such as altered mental status, he or she might not be the only one who is confused. Hospitalists might be a little confused, too.
Of all the subspecialties to which hospitalists are exposed, none might make them more uncomfortable than neurology. Because of what often is a dearth of training in this area, and because of the vexing and sometimes fleeting nature of symptoms, hospitalists might be inclined to lean on neurologists more than other specialists.
The Hospitalist spoke with a half-dozen experts, gathering their words of guidance and clinical tips. Here’s hoping they give you a little extra confidence the next time you see a patient with altered mental status.
You might be overdiagnosing transient ischemic attacks (TIA).
Ira Chang, MD, a neurohospitalist with Blue Sky Neurology in Englewood, Colo., and assistant clinical professor at the University of Colorado Health Sciences Center in Denver, says TIA is all too commonly a go-to diagnosis, frequently when there’s another cause.
“I think that hospitalists, and maybe medical internists in general, are very quick to diagnose anything that has a neurologic symptom that comes and goes as a TIA,” she says. “Patients have to have specific neurologic symptoms that we think are due to arterial blood flow or ischemia problems.”
Near-fainting spells and dizzy spells involving confusion commonly are diagnosed as TIA when these symptoms could be due to “a number of other causes,” Dr. Chang adds.
Kevin Barrett, MD, assistant professor of neurology and a neurohospitalist at Mayo Clinic in Jacksonville, Fla., says the suspicion of a TIA should be greater if the patient is older or has traditional cardiovascular risk factors, such as hyptertension, diabetes, hyperlipidemia, or tobacco use.
A TIA typically causes symptoms referable to common arterial distributions. Carotid-distribution TIA often causes ipsilateral loss of vision and contralateral weakness or numbness. Posterior-circulation TIAs bring on symptoms such as ataxia, unilateral or bilateral limb weakness, diplopia, and slurred or slow speech.
TIA diagnoses can be tricky even for those trained in neurology, Dr. Barrett says.
“Even among fellowship-trained vascular neurologists, TIA can be a challenging diagnosis, often with poor inter-observer agreement,” he notes.
Early mobilization after a stroke might be better for some patients.
After receiving tissue plasminogen activator (tPA) therapy for stroke, patients historically were kept on bed rest for 24 hours to reduce the risk of hemorrhage. Evidence now is coming to light that some patients might benefit from getting out of bed sooner, Dr. Barrett says.1
“We’re learning that in selected patients, they can actually be mobilized at 12 hours,” he says. “In some cases, that would not only reduce the risk of complications related to immobilization like DVT but shorten length of stay. These are all important metrics for anybody who practices primarily within an inpatient setting.”
Early mobilization generally is more suitable for patients with less severe deficits and who are hemodynamically stable.
MRI is the best tool to evaluate TIA patients.
TIA patients who have transient symptoms and normal diffusion-weighted imaging (DWI) abnormalities on an MRI are at a very low risk. “Less than 1% of those patients have a stroke within the subsequent seven days,” Dr. Barrett says.2 “But those patients who do have a DWI abnormality, they’re at very high risk: 7.1% at seven days.
“The utility of MRI following TIA is becoming very much apparent. It is something that hospitalists should be aware of.”
Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
Patients experiencing confusion or speech disturbance or altered mentation—particularly if they’re elderly or have dementia—could be having a partial seizure, Dr. Chang says. Dementia patients have a 10% to 15% incidence of complex partial seizures, she says.
“I see that underdiagnosed a lot,” she says. “They keep coming back, and everybody diagnoses them with TIAs. So they keep getting put on aspirin, and they get switched to Aggrenox [to prevent clotting]. They keep coming back with the same symptoms.”
Tracking the time a hospitalized patient was last seen to be normal is crucial.
About 10% to 15% of strokes occur in patients who are in the hospital.
“While a lot of those strokes are perioperative, there also are patients who are going to be on hospitalist services,” says Eric Adelman, MD, assistant professor of neurology at the University of Michigan in Ann Arbor.
Hospitalists should note that patients suffering strokes are found not just in the ED but also on the floor, where all the tools for treatment might not be as readily available. That makes those cases a challenge and makes forethought that much more important, Dr. Adelman says.
“It’s a matter of trying to track down last normal times,” he says. “If they’re eligible for tPA and they’re within the therapeutic window, we should be able to do that within a hospital.”
Establishing a neurological baseline is particularly important for patients who are at higher stroke risk, like those with atrial fibrillation and other cardiovascular risk factors.
“In case something does happen,” Dr. Adelman says, “at least you have a baseline so you can [know that] at time X, we knew they had full strength in their right arm, and now they don’t.”
Consider neuromuscular disorders when a patient presents with weakness.
It’s safe to say some hospitalists might miss a neuromuscular disorder, Dr. Chang says.
“A lot of disorders that are harder for hospitalists to diagnose and that tend to take longer to call a neurologist [on] are things that are due to myasthenia gravis [a breakdown between nerves and muscles leading to muscle fatigue], myopathy, or ALS,” she says. “Many patients present with weakness. I think a lot of times there will be a lot of tests on and a lot of treatment for general medical conditions that can cause weakness.”
And that might be a case of misdirected attention. Patients with weakness accompanied by persistent swallowing problems, slurred speech with no other obvious cause, or the inability to lift their head off the bed without an obvious cause may end up with a neuromuscular diagnosis, she says.
It would be helpful to have a neurologist’s input in these cases, she says, where “nothing’s getting better, and three, four, five days later, the patient’s still weak.
“I think a neurologist would be more in tune with something like that,” she adds.
Urinary tract infections (UTIs) are not the only cause of altered mental status.
That might seem obvious, but too often, a UTI can be pegged as the source of altered mental status when it should not be, Dr. Chang says.
“We get a lot of people who come in with confusion and they have a slightly abnormal urinalysis and they diagnose them with UTI,” Dr. Chang says. “And it turns out that they actually had a stroke or they had a seizure.”
Significantly altered mentation should show a significantly abnormal urine with a positive culture, she says. “They ought to have significant laboratory support for a urinary tract infection.”
Dr. Barrett says a neurologic review of systems, or at least a neurologic exam, should be the physician’s guide.
“Those are key parts of a hospitalist’s practice,” he says, “because that’s what’s truly going to guide them to consider primary neurological causes of altered mental status.”
Take care in distinguishing aphasia from general confusion.
If a patient is still talking and is fairly fluent, that doesn’t mean they aren’t suffering from certain types of aphasia, a disorder caused by damage to parts of the brain that control language, Dr. Adelman says.
“Oftentimes, when you’re dealing with a patient with confusion, you want to make sure that it’s confusion, or encephalopathy, rather than a focal neurologic problem like aphasia,” he says. “Frequently patients with aphasia will have other symptoms such as a facial drop or weakness in the arm, but stroke can present as isolated aphasia.”
A good habit to get into is to determine whether the patient can repeat a phrase, follow a command, or name objects, he says. If they can, they probably do not have aphasia.
“The thing that you worry about with aphasia, particularly acute onset aphasia, is an ischemic stroke,” Dr. Adelman says.
A simple checklist might eliminate the need to consult the neurologist.
When Edgar Kenton, MD, now director of the stroke program at Geisinger Health System in Danville, Pa., was at Emory University Hospital in Atlanta, he found he was getting snowed under with consults from hospitalists. There were about 15 hospitalists for just one or two neurologists.
“There was no way I was able to see these patients, particularly in follow-up, because you might get five consults every day,” he says. “By the middle of the week, that’s 15 consults. You don’t get a chance to go back and see the patients because you’re just going from one consult to the other.”
The situation improved with a checklist of things to consider when a patient presents with altered mental status. Before seeking a consult, neurologists suggested the hospitalists check the electrolytes, blood pressure, and urine, and use CT scans as a screening test. That might uncover the root of the patient’s problems. If those are clear, by all means get the neurologist involved, he says.
“We were able to educate the hospitalists so they knew when to call; they knew when it was beyond their expertise to take care of the patient, so we weren’t getting called for every patient with altered mental status when all they needed to do was to check the electrolytes,” Dr. Kenton says.
Calling a neurologist earlier is way better than calling later.
Once the decision is made to consult with a neurologist, the consult should be done right away, Dr. Kenton says, not after a few days when symptoms don’t appear to be improving.
“We’ll get the call on a Friday afternoon because they thought, finally, ‘Well, you know, we need to get neurology involved because we a) haven’t solved the problem and b) there may be some other tests we should be getting,’” he says of common situations. “That has been a problem. If you don’t have a neurohospitalist involved day by day, working with the patient and the general hospitalist, neurology becomes an afterthought.”
He says accurate and early diagnosis is paramount to the patient.
“If the diagnosis is delayed, obviously there’s more insult to the patients, more persistent insult,” he says, noting the timing is particularly important in neurological conditions “because things can get bad in a hurry.”
He strongly urges hospitalists to consult with a neurologist before ordering an entire battery of tests.
At Geisinger, neurologists are encouraging hospitalists to chat informally with neurosurgeons about cases for guidance at the outset rather than after several days.
Hire a neurohospitalist if your institution doesn’t have one already.
At the top of the list of Dr. Kenton’s suggestions on caring for hospitalized neurology patients is this declaration: “Get a neurohospitalist.”
“It’s important to have the neurologist involved from the time the patient’s admitted,” he says. “That’s the value of connecting the general hospitalist with neurologists.”
S. Andrew Josephson, MD, director of the neurohospitalist program at the University of California at San Francisco, says his colleagues are team players and improve patient care.
“Neurology consultations can be called very quickly, and a nice partnership can develop between internal medicine hospitalists and neurohospitalists to care for those patients who have those medical and neurologic problems,” he says.
He also says having a neurohospitalist on board can ease some of the tension.
“No longer if there’s a neurologic condition does a hospitalist have to think about, ‘Well, does this rise to the level of something that I need to get the neurologist to drive across the city to come see?’” he explains. “‘Or is this something we should try to manage ourselves?’”
Tom Collins is a freelance writer in South Florida.
References
- Bernhardt J, Dewey H, Thrift A, Collier J, Donnan G. A very early rehabilitation trial for stroke (AVERT): phase II safety and feasibility. Stroke. 2008;39;390-396.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs. time-defined TIA: a multicenter study. Neurology. 2011;77(13):1222-1228.
- Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. Attitudes of US medical trainees towards neurology education: “Neurophobia”—a global issue. BMC Med Educ. 2010;10:49.
11 Things: At a Glance
- You might be overdiagnosing transient ischemic attacks (TIA).
- Early mobilization after a stroke might be better for some patients.
- MRI is the best tool to evaluate TIA patients.
- Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
- Tracking the time a hospitalized patient was last seen to be normal is crucial.
- Consider neuromuscular disorders when a patient presents with weakness.
- Urinary tract infections (UTIs) are not the only cause of altered mental status.
- Take care in distinguishing aphasia from general confusion.
- A simple checklist might eliminate the need to consult the neurologist.
- Calling a neurologist earlier is way better than calling later.
- Hire a neurohospitalist if your institution doesn’t have one already.
When a patient is admitted to the hospital with neurological symptoms, such as altered mental status, he or she might not be the only one who is confused. Hospitalists might be a little confused, too.
Of all the subspecialties to which hospitalists are exposed, none might make them more uncomfortable than neurology. Because of what often is a dearth of training in this area, and because of the vexing and sometimes fleeting nature of symptoms, hospitalists might be inclined to lean on neurologists more than other specialists.
The Hospitalist spoke with a half-dozen experts, gathering their words of guidance and clinical tips. Here’s hoping they give you a little extra confidence the next time you see a patient with altered mental status.
You might be overdiagnosing transient ischemic attacks (TIA).
Ira Chang, MD, a neurohospitalist with Blue Sky Neurology in Englewood, Colo., and assistant clinical professor at the University of Colorado Health Sciences Center in Denver, says TIA is all too commonly a go-to diagnosis, frequently when there’s another cause.
“I think that hospitalists, and maybe medical internists in general, are very quick to diagnose anything that has a neurologic symptom that comes and goes as a TIA,” she says. “Patients have to have specific neurologic symptoms that we think are due to arterial blood flow or ischemia problems.”
Near-fainting spells and dizzy spells involving confusion commonly are diagnosed as TIA when these symptoms could be due to “a number of other causes,” Dr. Chang adds.
Kevin Barrett, MD, assistant professor of neurology and a neurohospitalist at Mayo Clinic in Jacksonville, Fla., says the suspicion of a TIA should be greater if the patient is older or has traditional cardiovascular risk factors, such as hyptertension, diabetes, hyperlipidemia, or tobacco use.
A TIA typically causes symptoms referable to common arterial distributions. Carotid-distribution TIA often causes ipsilateral loss of vision and contralateral weakness or numbness. Posterior-circulation TIAs bring on symptoms such as ataxia, unilateral or bilateral limb weakness, diplopia, and slurred or slow speech.
TIA diagnoses can be tricky even for those trained in neurology, Dr. Barrett says.
“Even among fellowship-trained vascular neurologists, TIA can be a challenging diagnosis, often with poor inter-observer agreement,” he notes.
Early mobilization after a stroke might be better for some patients.
After receiving tissue plasminogen activator (tPA) therapy for stroke, patients historically were kept on bed rest for 24 hours to reduce the risk of hemorrhage. Evidence now is coming to light that some patients might benefit from getting out of bed sooner, Dr. Barrett says.1
“We’re learning that in selected patients, they can actually be mobilized at 12 hours,” he says. “In some cases, that would not only reduce the risk of complications related to immobilization like DVT but shorten length of stay. These are all important metrics for anybody who practices primarily within an inpatient setting.”
Early mobilization generally is more suitable for patients with less severe deficits and who are hemodynamically stable.
MRI is the best tool to evaluate TIA patients.
TIA patients who have transient symptoms and normal diffusion-weighted imaging (DWI) abnormalities on an MRI are at a very low risk. “Less than 1% of those patients have a stroke within the subsequent seven days,” Dr. Barrett says.2 “But those patients who do have a DWI abnormality, they’re at very high risk: 7.1% at seven days.
“The utility of MRI following TIA is becoming very much apparent. It is something that hospitalists should be aware of.”
Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
Patients experiencing confusion or speech disturbance or altered mentation—particularly if they’re elderly or have dementia—could be having a partial seizure, Dr. Chang says. Dementia patients have a 10% to 15% incidence of complex partial seizures, she says.
“I see that underdiagnosed a lot,” she says. “They keep coming back, and everybody diagnoses them with TIAs. So they keep getting put on aspirin, and they get switched to Aggrenox [to prevent clotting]. They keep coming back with the same symptoms.”
Tracking the time a hospitalized patient was last seen to be normal is crucial.
About 10% to 15% of strokes occur in patients who are in the hospital.
“While a lot of those strokes are perioperative, there also are patients who are going to be on hospitalist services,” says Eric Adelman, MD, assistant professor of neurology at the University of Michigan in Ann Arbor.
Hospitalists should note that patients suffering strokes are found not just in the ED but also on the floor, where all the tools for treatment might not be as readily available. That makes those cases a challenge and makes forethought that much more important, Dr. Adelman says.
“It’s a matter of trying to track down last normal times,” he says. “If they’re eligible for tPA and they’re within the therapeutic window, we should be able to do that within a hospital.”
Establishing a neurological baseline is particularly important for patients who are at higher stroke risk, like those with atrial fibrillation and other cardiovascular risk factors.
“In case something does happen,” Dr. Adelman says, “at least you have a baseline so you can [know that] at time X, we knew they had full strength in their right arm, and now they don’t.”
Consider neuromuscular disorders when a patient presents with weakness.
It’s safe to say some hospitalists might miss a neuromuscular disorder, Dr. Chang says.
“A lot of disorders that are harder for hospitalists to diagnose and that tend to take longer to call a neurologist [on] are things that are due to myasthenia gravis [a breakdown between nerves and muscles leading to muscle fatigue], myopathy, or ALS,” she says. “Many patients present with weakness. I think a lot of times there will be a lot of tests on and a lot of treatment for general medical conditions that can cause weakness.”
And that might be a case of misdirected attention. Patients with weakness accompanied by persistent swallowing problems, slurred speech with no other obvious cause, or the inability to lift their head off the bed without an obvious cause may end up with a neuromuscular diagnosis, she says.
It would be helpful to have a neurologist’s input in these cases, she says, where “nothing’s getting better, and three, four, five days later, the patient’s still weak.
“I think a neurologist would be more in tune with something like that,” she adds.
Urinary tract infections (UTIs) are not the only cause of altered mental status.
That might seem obvious, but too often, a UTI can be pegged as the source of altered mental status when it should not be, Dr. Chang says.
“We get a lot of people who come in with confusion and they have a slightly abnormal urinalysis and they diagnose them with UTI,” Dr. Chang says. “And it turns out that they actually had a stroke or they had a seizure.”
Significantly altered mentation should show a significantly abnormal urine with a positive culture, she says. “They ought to have significant laboratory support for a urinary tract infection.”
Dr. Barrett says a neurologic review of systems, or at least a neurologic exam, should be the physician’s guide.
“Those are key parts of a hospitalist’s practice,” he says, “because that’s what’s truly going to guide them to consider primary neurological causes of altered mental status.”
Take care in distinguishing aphasia from general confusion.
If a patient is still talking and is fairly fluent, that doesn’t mean they aren’t suffering from certain types of aphasia, a disorder caused by damage to parts of the brain that control language, Dr. Adelman says.
“Oftentimes, when you’re dealing with a patient with confusion, you want to make sure that it’s confusion, or encephalopathy, rather than a focal neurologic problem like aphasia,” he says. “Frequently patients with aphasia will have other symptoms such as a facial drop or weakness in the arm, but stroke can present as isolated aphasia.”
A good habit to get into is to determine whether the patient can repeat a phrase, follow a command, or name objects, he says. If they can, they probably do not have aphasia.
“The thing that you worry about with aphasia, particularly acute onset aphasia, is an ischemic stroke,” Dr. Adelman says.
A simple checklist might eliminate the need to consult the neurologist.
When Edgar Kenton, MD, now director of the stroke program at Geisinger Health System in Danville, Pa., was at Emory University Hospital in Atlanta, he found he was getting snowed under with consults from hospitalists. There were about 15 hospitalists for just one or two neurologists.
“There was no way I was able to see these patients, particularly in follow-up, because you might get five consults every day,” he says. “By the middle of the week, that’s 15 consults. You don’t get a chance to go back and see the patients because you’re just going from one consult to the other.”
The situation improved with a checklist of things to consider when a patient presents with altered mental status. Before seeking a consult, neurologists suggested the hospitalists check the electrolytes, blood pressure, and urine, and use CT scans as a screening test. That might uncover the root of the patient’s problems. If those are clear, by all means get the neurologist involved, he says.
“We were able to educate the hospitalists so they knew when to call; they knew when it was beyond their expertise to take care of the patient, so we weren’t getting called for every patient with altered mental status when all they needed to do was to check the electrolytes,” Dr. Kenton says.
Calling a neurologist earlier is way better than calling later.
Once the decision is made to consult with a neurologist, the consult should be done right away, Dr. Kenton says, not after a few days when symptoms don’t appear to be improving.
“We’ll get the call on a Friday afternoon because they thought, finally, ‘Well, you know, we need to get neurology involved because we a) haven’t solved the problem and b) there may be some other tests we should be getting,’” he says of common situations. “That has been a problem. If you don’t have a neurohospitalist involved day by day, working with the patient and the general hospitalist, neurology becomes an afterthought.”
He says accurate and early diagnosis is paramount to the patient.
“If the diagnosis is delayed, obviously there’s more insult to the patients, more persistent insult,” he says, noting the timing is particularly important in neurological conditions “because things can get bad in a hurry.”
He strongly urges hospitalists to consult with a neurologist before ordering an entire battery of tests.
At Geisinger, neurologists are encouraging hospitalists to chat informally with neurosurgeons about cases for guidance at the outset rather than after several days.
Hire a neurohospitalist if your institution doesn’t have one already.
At the top of the list of Dr. Kenton’s suggestions on caring for hospitalized neurology patients is this declaration: “Get a neurohospitalist.”
“It’s important to have the neurologist involved from the time the patient’s admitted,” he says. “That’s the value of connecting the general hospitalist with neurologists.”
S. Andrew Josephson, MD, director of the neurohospitalist program at the University of California at San Francisco, says his colleagues are team players and improve patient care.
“Neurology consultations can be called very quickly, and a nice partnership can develop between internal medicine hospitalists and neurohospitalists to care for those patients who have those medical and neurologic problems,” he says.
He also says having a neurohospitalist on board can ease some of the tension.
“No longer if there’s a neurologic condition does a hospitalist have to think about, ‘Well, does this rise to the level of something that I need to get the neurologist to drive across the city to come see?’” he explains. “‘Or is this something we should try to manage ourselves?’”
Tom Collins is a freelance writer in South Florida.
References
- Bernhardt J, Dewey H, Thrift A, Collier J, Donnan G. A very early rehabilitation trial for stroke (AVERT): phase II safety and feasibility. Stroke. 2008;39;390-396.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs. time-defined TIA: a multicenter study. Neurology. 2011;77(13):1222-1228.
- Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. Attitudes of US medical trainees towards neurology education: “Neurophobia”—a global issue. BMC Med Educ. 2010;10:49.
11 Things: At a Glance
- You might be overdiagnosing transient ischemic attacks (TIA).
- Early mobilization after a stroke might be better for some patients.
- MRI is the best tool to evaluate TIA patients.
- Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
- Tracking the time a hospitalized patient was last seen to be normal is crucial.
- Consider neuromuscular disorders when a patient presents with weakness.
- Urinary tract infections (UTIs) are not the only cause of altered mental status.
- Take care in distinguishing aphasia from general confusion.
- A simple checklist might eliminate the need to consult the neurologist.
- Calling a neurologist earlier is way better than calling later.
- Hire a neurohospitalist if your institution doesn’t have one already.
When a patient is admitted to the hospital with neurological symptoms, such as altered mental status, he or she might not be the only one who is confused. Hospitalists might be a little confused, too.
Of all the subspecialties to which hospitalists are exposed, none might make them more uncomfortable than neurology. Because of what often is a dearth of training in this area, and because of the vexing and sometimes fleeting nature of symptoms, hospitalists might be inclined to lean on neurologists more than other specialists.
The Hospitalist spoke with a half-dozen experts, gathering their words of guidance and clinical tips. Here’s hoping they give you a little extra confidence the next time you see a patient with altered mental status.
You might be overdiagnosing transient ischemic attacks (TIA).
Ira Chang, MD, a neurohospitalist with Blue Sky Neurology in Englewood, Colo., and assistant clinical professor at the University of Colorado Health Sciences Center in Denver, says TIA is all too commonly a go-to diagnosis, frequently when there’s another cause.
“I think that hospitalists, and maybe medical internists in general, are very quick to diagnose anything that has a neurologic symptom that comes and goes as a TIA,” she says. “Patients have to have specific neurologic symptoms that we think are due to arterial blood flow or ischemia problems.”
Near-fainting spells and dizzy spells involving confusion commonly are diagnosed as TIA when these symptoms could be due to “a number of other causes,” Dr. Chang adds.
Kevin Barrett, MD, assistant professor of neurology and a neurohospitalist at Mayo Clinic in Jacksonville, Fla., says the suspicion of a TIA should be greater if the patient is older or has traditional cardiovascular risk factors, such as hyptertension, diabetes, hyperlipidemia, or tobacco use.
A TIA typically causes symptoms referable to common arterial distributions. Carotid-distribution TIA often causes ipsilateral loss of vision and contralateral weakness or numbness. Posterior-circulation TIAs bring on symptoms such as ataxia, unilateral or bilateral limb weakness, diplopia, and slurred or slow speech.
TIA diagnoses can be tricky even for those trained in neurology, Dr. Barrett says.
“Even among fellowship-trained vascular neurologists, TIA can be a challenging diagnosis, often with poor inter-observer agreement,” he notes.
Early mobilization after a stroke might be better for some patients.
After receiving tissue plasminogen activator (tPA) therapy for stroke, patients historically were kept on bed rest for 24 hours to reduce the risk of hemorrhage. Evidence now is coming to light that some patients might benefit from getting out of bed sooner, Dr. Barrett says.1
“We’re learning that in selected patients, they can actually be mobilized at 12 hours,” he says. “In some cases, that would not only reduce the risk of complications related to immobilization like DVT but shorten length of stay. These are all important metrics for anybody who practices primarily within an inpatient setting.”
Early mobilization generally is more suitable for patients with less severe deficits and who are hemodynamically stable.
MRI is the best tool to evaluate TIA patients.
TIA patients who have transient symptoms and normal diffusion-weighted imaging (DWI) abnormalities on an MRI are at a very low risk. “Less than 1% of those patients have a stroke within the subsequent seven days,” Dr. Barrett says.2 “But those patients who do have a DWI abnormality, they’re at very high risk: 7.1% at seven days.
“The utility of MRI following TIA is becoming very much apparent. It is something that hospitalists should be aware of.”
Consider focal seizure or complex partial seizure as one of the possible causes of confusion or speech disturbance, or both.
Patients experiencing confusion or speech disturbance or altered mentation—particularly if they’re elderly or have dementia—could be having a partial seizure, Dr. Chang says. Dementia patients have a 10% to 15% incidence of complex partial seizures, she says.
“I see that underdiagnosed a lot,” she says. “They keep coming back, and everybody diagnoses them with TIAs. So they keep getting put on aspirin, and they get switched to Aggrenox [to prevent clotting]. They keep coming back with the same symptoms.”
Tracking the time a hospitalized patient was last seen to be normal is crucial.
About 10% to 15% of strokes occur in patients who are in the hospital.
“While a lot of those strokes are perioperative, there also are patients who are going to be on hospitalist services,” says Eric Adelman, MD, assistant professor of neurology at the University of Michigan in Ann Arbor.
Hospitalists should note that patients suffering strokes are found not just in the ED but also on the floor, where all the tools for treatment might not be as readily available. That makes those cases a challenge and makes forethought that much more important, Dr. Adelman says.
“It’s a matter of trying to track down last normal times,” he says. “If they’re eligible for tPA and they’re within the therapeutic window, we should be able to do that within a hospital.”
Establishing a neurological baseline is particularly important for patients who are at higher stroke risk, like those with atrial fibrillation and other cardiovascular risk factors.
“In case something does happen,” Dr. Adelman says, “at least you have a baseline so you can [know that] at time X, we knew they had full strength in their right arm, and now they don’t.”
Consider neuromuscular disorders when a patient presents with weakness.
It’s safe to say some hospitalists might miss a neuromuscular disorder, Dr. Chang says.
“A lot of disorders that are harder for hospitalists to diagnose and that tend to take longer to call a neurologist [on] are things that are due to myasthenia gravis [a breakdown between nerves and muscles leading to muscle fatigue], myopathy, or ALS,” she says. “Many patients present with weakness. I think a lot of times there will be a lot of tests on and a lot of treatment for general medical conditions that can cause weakness.”
And that might be a case of misdirected attention. Patients with weakness accompanied by persistent swallowing problems, slurred speech with no other obvious cause, or the inability to lift their head off the bed without an obvious cause may end up with a neuromuscular diagnosis, she says.
It would be helpful to have a neurologist’s input in these cases, she says, where “nothing’s getting better, and three, four, five days later, the patient’s still weak.
“I think a neurologist would be more in tune with something like that,” she adds.
Urinary tract infections (UTIs) are not the only cause of altered mental status.
That might seem obvious, but too often, a UTI can be pegged as the source of altered mental status when it should not be, Dr. Chang says.
“We get a lot of people who come in with confusion and they have a slightly abnormal urinalysis and they diagnose them with UTI,” Dr. Chang says. “And it turns out that they actually had a stroke or they had a seizure.”
Significantly altered mentation should show a significantly abnormal urine with a positive culture, she says. “They ought to have significant laboratory support for a urinary tract infection.”
Dr. Barrett says a neurologic review of systems, or at least a neurologic exam, should be the physician’s guide.
“Those are key parts of a hospitalist’s practice,” he says, “because that’s what’s truly going to guide them to consider primary neurological causes of altered mental status.”
Take care in distinguishing aphasia from general confusion.
If a patient is still talking and is fairly fluent, that doesn’t mean they aren’t suffering from certain types of aphasia, a disorder caused by damage to parts of the brain that control language, Dr. Adelman says.
“Oftentimes, when you’re dealing with a patient with confusion, you want to make sure that it’s confusion, or encephalopathy, rather than a focal neurologic problem like aphasia,” he says. “Frequently patients with aphasia will have other symptoms such as a facial drop or weakness in the arm, but stroke can present as isolated aphasia.”
A good habit to get into is to determine whether the patient can repeat a phrase, follow a command, or name objects, he says. If they can, they probably do not have aphasia.
“The thing that you worry about with aphasia, particularly acute onset aphasia, is an ischemic stroke,” Dr. Adelman says.
A simple checklist might eliminate the need to consult the neurologist.
When Edgar Kenton, MD, now director of the stroke program at Geisinger Health System in Danville, Pa., was at Emory University Hospital in Atlanta, he found he was getting snowed under with consults from hospitalists. There were about 15 hospitalists for just one or two neurologists.
“There was no way I was able to see these patients, particularly in follow-up, because you might get five consults every day,” he says. “By the middle of the week, that’s 15 consults. You don’t get a chance to go back and see the patients because you’re just going from one consult to the other.”
The situation improved with a checklist of things to consider when a patient presents with altered mental status. Before seeking a consult, neurologists suggested the hospitalists check the electrolytes, blood pressure, and urine, and use CT scans as a screening test. That might uncover the root of the patient’s problems. If those are clear, by all means get the neurologist involved, he says.
“We were able to educate the hospitalists so they knew when to call; they knew when it was beyond their expertise to take care of the patient, so we weren’t getting called for every patient with altered mental status when all they needed to do was to check the electrolytes,” Dr. Kenton says.
Calling a neurologist earlier is way better than calling later.
Once the decision is made to consult with a neurologist, the consult should be done right away, Dr. Kenton says, not after a few days when symptoms don’t appear to be improving.
“We’ll get the call on a Friday afternoon because they thought, finally, ‘Well, you know, we need to get neurology involved because we a) haven’t solved the problem and b) there may be some other tests we should be getting,’” he says of common situations. “That has been a problem. If you don’t have a neurohospitalist involved day by day, working with the patient and the general hospitalist, neurology becomes an afterthought.”
He says accurate and early diagnosis is paramount to the patient.
“If the diagnosis is delayed, obviously there’s more insult to the patients, more persistent insult,” he says, noting the timing is particularly important in neurological conditions “because things can get bad in a hurry.”
He strongly urges hospitalists to consult with a neurologist before ordering an entire battery of tests.
At Geisinger, neurologists are encouraging hospitalists to chat informally with neurosurgeons about cases for guidance at the outset rather than after several days.
Hire a neurohospitalist if your institution doesn’t have one already.
At the top of the list of Dr. Kenton’s suggestions on caring for hospitalized neurology patients is this declaration: “Get a neurohospitalist.”
“It’s important to have the neurologist involved from the time the patient’s admitted,” he says. “That’s the value of connecting the general hospitalist with neurologists.”
S. Andrew Josephson, MD, director of the neurohospitalist program at the University of California at San Francisco, says his colleagues are team players and improve patient care.
“Neurology consultations can be called very quickly, and a nice partnership can develop between internal medicine hospitalists and neurohospitalists to care for those patients who have those medical and neurologic problems,” he says.
He also says having a neurohospitalist on board can ease some of the tension.
“No longer if there’s a neurologic condition does a hospitalist have to think about, ‘Well, does this rise to the level of something that I need to get the neurologist to drive across the city to come see?’” he explains. “‘Or is this something we should try to manage ourselves?’”
Tom Collins is a freelance writer in South Florida.
References
- Bernhardt J, Dewey H, Thrift A, Collier J, Donnan G. A very early rehabilitation trial for stroke (AVERT): phase II safety and feasibility. Stroke. 2008;39;390-396.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs. time-defined TIA: a multicenter study. Neurology. 2011;77(13):1222-1228.
- Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. Attitudes of US medical trainees towards neurology education: “Neurophobia”—a global issue. BMC Med Educ. 2010;10:49.
Boston Marathon Bombing Calls Hospitalists to Duty

—James Hudspeth, MD, Boston Medical Center

—Dan Hale, MD, Floating Hospital for Children at Tufts Medical Center, Boston
Dan Hale, MD, a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, was doing discharge paperwork when he started getting text messages he couldn’t quite interpret.
“Are you OK?” “Do you need anything?” friends were asking him. Then he heard a page for all anesthesiologists to report to the OR. Immediately, he knew something terrible must have happened. He soon learned about the bombings at the Boston Marathon. He rushed to the pediatric ED to see how he could help.
James Hudspeth, MD, a hospitalist at Boston Medical Center, was meeting with the program director for internal medicine when he read a text message that bombs had just gone off near the finish line. They went online for local news coverage; soon thereafter, a cap on admissions was lifted. Dr. Hudspeth started expediting discharges to make room for what might be coming the hospital’s way.
Sushrut Jangi, MD, a hospitalist at Beth Israel Deaconess Medical Center, was in a medical tent gathering information for an article on treating the health problems of marathoners that he was writing for The Boston Globe when he heard the blasts. Doctors and medical staff there worried about the possibility of a bomb in the tent, he said, but they were instructed to stay with their patients. Dr. Jangi had expected to work as a journalist for the day, but his doctoring skills were needed.
Hospitalists who were working in downtown Boston on April 15, when two bombs exploded 17 seconds apart, all experienced the tragedy in their own ways. But their accounts also resonate within some of the same themes.
They found themselves unsure of their roles, as most of the work inevitably fell to surgeons and trauma specialists. They described the importance of good leadership in times of crisis. And they say that hospitalists should be incorporated to a greater extent into disaster plans.
Dr. Jangi said that before the bombs went off, the medical tent was almost filled with runners who were “quite ill”—hypothermic and shaking, high sodium levels, disoriented. When the blasts occurred, the main instruction was, “Don’t leave your patients behind.” Those who were well enough were released from the tent, and the bomb-blast victims were essentially “whisked through.”
“We just kind of cleared the way and got them into ambulances as soon as possible. We just didn’t have the capacity to take care of such severe injury,” he said. “Why should we? We weren’t expecting a war zone.”
In the tent, Dr. Jangi wrote in an essay for the New England Journal of Medicine, “Many of us barely laid our hands on anyone. We had no trauma surgeons or supplies of blood products; tourniquets had already been applied; CPR had already been performed. Though some patients required bandages, sutures, and dressings, many of us watched these passing victims in a kind of idle horror, with no idea how to help.”
Dr. Hale was not involved in the treatment of bombing victims as the attending of record, but he said that he had a “bird’s-eye view” of the response in the pediatric ED. One child had shrapnel injuries and a ruptured tympanic membrane and was worked on by the team “professionally and efficiently,” Dr. Hale said.
When reports of a possible third bomb blast, at a library, came in, he saw the physician leaders go from team to team, making sure they were prepared.
“There were clear leaders communicating what to do,” said Dr. Hale, a firefighter in his hometown of Kittery in southern Maine. “As patients came in, it was extremely orderly. I saw very few clinical staff who were rattled.”
For his own part, in addition to his medical training, his training as a firefighter helped keep him calm, he said.
At Boston Medical Center, about a mile and a half from the blasts, the admissions that had been worked up over the course of the afternoon were essentially taken all at once so that there was room in the ED, said Dr. Hudspeth, who also does medical work in Haiti and was in New York on 9/11, though not as a doctor.
Focusing, he said, was “definitely a challenge.” Even though he had faith in hospital security, there was still “some notion of ‘You never know exactly what’s going to happen.’”
“You focus on the patient that’s in front of you. You focus on trying to solve the issues that are at hand. You deal with the logistical questions that come up between patients,” he said. “By and large, just put your nose to the grindstone.”
The doctors said that hospitalists had an unclear role in the response effort and hope to have their roles clarified so that they can better put to use their expertise in internal medicine. If hospitalists are monitoring general medical issues, that will help take some of the pressure off the trauma team.
“We know the [general] medicine stuff very well—that is our bread and butter,” said Dr. Hudspeth, who added that steps are being taken as part of Boston Medical Center’s post-response analysis to determine hospitalists’ role in future disaster responses.
They also said they felt fortunate that the bombings had occurred where they did, with so many hospitals close to the scene. It kept the system from becoming overwhelmed. Even so, “at some point, a disaster is so large that it would overwhelm any system, no matter how many resources were available,” Dr. Hale added.
Dr. Jangi said that he thinks his residency training helped him when he found himself having to provide care in a high-pressure situation in the medical tent.
“During residency, there are a lot of situations where you’re responsible for making a decision on your feet,” he said. “That’s a skill that you’re not really exposed to until you do it and that type of fast decision-making. I felt myself drawing on that. Not that I resuscitated anyone in the tent, but I felt more comfortable with uncertainty, with doing your duty in a situation of uncertainty. And I don’t know—maybe if I hadn’t gone through that, I would have just run out of there.”
He said the experience has helped make him more committed as a doctor.
“It makes it easier to remember what my duty is more, and it just gives me more empathy for suffering in general—I feel that very strongly,” he said. “It’s possible that this experience could have numbed me, but it didn’t. It’s made me more acute to the idea of people suffering.”
Tom Collins is a freelance writer in South Florida.
Reference

—James Hudspeth, MD, Boston Medical Center

—Dan Hale, MD, Floating Hospital for Children at Tufts Medical Center, Boston
Dan Hale, MD, a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, was doing discharge paperwork when he started getting text messages he couldn’t quite interpret.
“Are you OK?” “Do you need anything?” friends were asking him. Then he heard a page for all anesthesiologists to report to the OR. Immediately, he knew something terrible must have happened. He soon learned about the bombings at the Boston Marathon. He rushed to the pediatric ED to see how he could help.
James Hudspeth, MD, a hospitalist at Boston Medical Center, was meeting with the program director for internal medicine when he read a text message that bombs had just gone off near the finish line. They went online for local news coverage; soon thereafter, a cap on admissions was lifted. Dr. Hudspeth started expediting discharges to make room for what might be coming the hospital’s way.
Sushrut Jangi, MD, a hospitalist at Beth Israel Deaconess Medical Center, was in a medical tent gathering information for an article on treating the health problems of marathoners that he was writing for The Boston Globe when he heard the blasts. Doctors and medical staff there worried about the possibility of a bomb in the tent, he said, but they were instructed to stay with their patients. Dr. Jangi had expected to work as a journalist for the day, but his doctoring skills were needed.
Hospitalists who were working in downtown Boston on April 15, when two bombs exploded 17 seconds apart, all experienced the tragedy in their own ways. But their accounts also resonate within some of the same themes.
They found themselves unsure of their roles, as most of the work inevitably fell to surgeons and trauma specialists. They described the importance of good leadership in times of crisis. And they say that hospitalists should be incorporated to a greater extent into disaster plans.
Dr. Jangi said that before the bombs went off, the medical tent was almost filled with runners who were “quite ill”—hypothermic and shaking, high sodium levels, disoriented. When the blasts occurred, the main instruction was, “Don’t leave your patients behind.” Those who were well enough were released from the tent, and the bomb-blast victims were essentially “whisked through.”
“We just kind of cleared the way and got them into ambulances as soon as possible. We just didn’t have the capacity to take care of such severe injury,” he said. “Why should we? We weren’t expecting a war zone.”
In the tent, Dr. Jangi wrote in an essay for the New England Journal of Medicine, “Many of us barely laid our hands on anyone. We had no trauma surgeons or supplies of blood products; tourniquets had already been applied; CPR had already been performed. Though some patients required bandages, sutures, and dressings, many of us watched these passing victims in a kind of idle horror, with no idea how to help.”
Dr. Hale was not involved in the treatment of bombing victims as the attending of record, but he said that he had a “bird’s-eye view” of the response in the pediatric ED. One child had shrapnel injuries and a ruptured tympanic membrane and was worked on by the team “professionally and efficiently,” Dr. Hale said.
When reports of a possible third bomb blast, at a library, came in, he saw the physician leaders go from team to team, making sure they were prepared.
“There were clear leaders communicating what to do,” said Dr. Hale, a firefighter in his hometown of Kittery in southern Maine. “As patients came in, it was extremely orderly. I saw very few clinical staff who were rattled.”
For his own part, in addition to his medical training, his training as a firefighter helped keep him calm, he said.
At Boston Medical Center, about a mile and a half from the blasts, the admissions that had been worked up over the course of the afternoon were essentially taken all at once so that there was room in the ED, said Dr. Hudspeth, who also does medical work in Haiti and was in New York on 9/11, though not as a doctor.
Focusing, he said, was “definitely a challenge.” Even though he had faith in hospital security, there was still “some notion of ‘You never know exactly what’s going to happen.’”
“You focus on the patient that’s in front of you. You focus on trying to solve the issues that are at hand. You deal with the logistical questions that come up between patients,” he said. “By and large, just put your nose to the grindstone.”
The doctors said that hospitalists had an unclear role in the response effort and hope to have their roles clarified so that they can better put to use their expertise in internal medicine. If hospitalists are monitoring general medical issues, that will help take some of the pressure off the trauma team.
“We know the [general] medicine stuff very well—that is our bread and butter,” said Dr. Hudspeth, who added that steps are being taken as part of Boston Medical Center’s post-response analysis to determine hospitalists’ role in future disaster responses.
They also said they felt fortunate that the bombings had occurred where they did, with so many hospitals close to the scene. It kept the system from becoming overwhelmed. Even so, “at some point, a disaster is so large that it would overwhelm any system, no matter how many resources were available,” Dr. Hale added.
Dr. Jangi said that he thinks his residency training helped him when he found himself having to provide care in a high-pressure situation in the medical tent.
“During residency, there are a lot of situations where you’re responsible for making a decision on your feet,” he said. “That’s a skill that you’re not really exposed to until you do it and that type of fast decision-making. I felt myself drawing on that. Not that I resuscitated anyone in the tent, but I felt more comfortable with uncertainty, with doing your duty in a situation of uncertainty. And I don’t know—maybe if I hadn’t gone through that, I would have just run out of there.”
He said the experience has helped make him more committed as a doctor.
“It makes it easier to remember what my duty is more, and it just gives me more empathy for suffering in general—I feel that very strongly,” he said. “It’s possible that this experience could have numbed me, but it didn’t. It’s made me more acute to the idea of people suffering.”
Tom Collins is a freelance writer in South Florida.
Reference

—James Hudspeth, MD, Boston Medical Center

—Dan Hale, MD, Floating Hospital for Children at Tufts Medical Center, Boston
Dan Hale, MD, a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston, was doing discharge paperwork when he started getting text messages he couldn’t quite interpret.
“Are you OK?” “Do you need anything?” friends were asking him. Then he heard a page for all anesthesiologists to report to the OR. Immediately, he knew something terrible must have happened. He soon learned about the bombings at the Boston Marathon. He rushed to the pediatric ED to see how he could help.
James Hudspeth, MD, a hospitalist at Boston Medical Center, was meeting with the program director for internal medicine when he read a text message that bombs had just gone off near the finish line. They went online for local news coverage; soon thereafter, a cap on admissions was lifted. Dr. Hudspeth started expediting discharges to make room for what might be coming the hospital’s way.
Sushrut Jangi, MD, a hospitalist at Beth Israel Deaconess Medical Center, was in a medical tent gathering information for an article on treating the health problems of marathoners that he was writing for The Boston Globe when he heard the blasts. Doctors and medical staff there worried about the possibility of a bomb in the tent, he said, but they were instructed to stay with their patients. Dr. Jangi had expected to work as a journalist for the day, but his doctoring skills were needed.
Hospitalists who were working in downtown Boston on April 15, when two bombs exploded 17 seconds apart, all experienced the tragedy in their own ways. But their accounts also resonate within some of the same themes.
They found themselves unsure of their roles, as most of the work inevitably fell to surgeons and trauma specialists. They described the importance of good leadership in times of crisis. And they say that hospitalists should be incorporated to a greater extent into disaster plans.
Dr. Jangi said that before the bombs went off, the medical tent was almost filled with runners who were “quite ill”—hypothermic and shaking, high sodium levels, disoriented. When the blasts occurred, the main instruction was, “Don’t leave your patients behind.” Those who were well enough were released from the tent, and the bomb-blast victims were essentially “whisked through.”
“We just kind of cleared the way and got them into ambulances as soon as possible. We just didn’t have the capacity to take care of such severe injury,” he said. “Why should we? We weren’t expecting a war zone.”
In the tent, Dr. Jangi wrote in an essay for the New England Journal of Medicine, “Many of us barely laid our hands on anyone. We had no trauma surgeons or supplies of blood products; tourniquets had already been applied; CPR had already been performed. Though some patients required bandages, sutures, and dressings, many of us watched these passing victims in a kind of idle horror, with no idea how to help.”
Dr. Hale was not involved in the treatment of bombing victims as the attending of record, but he said that he had a “bird’s-eye view” of the response in the pediatric ED. One child had shrapnel injuries and a ruptured tympanic membrane and was worked on by the team “professionally and efficiently,” Dr. Hale said.
When reports of a possible third bomb blast, at a library, came in, he saw the physician leaders go from team to team, making sure they were prepared.
“There were clear leaders communicating what to do,” said Dr. Hale, a firefighter in his hometown of Kittery in southern Maine. “As patients came in, it was extremely orderly. I saw very few clinical staff who were rattled.”
For his own part, in addition to his medical training, his training as a firefighter helped keep him calm, he said.
At Boston Medical Center, about a mile and a half from the blasts, the admissions that had been worked up over the course of the afternoon were essentially taken all at once so that there was room in the ED, said Dr. Hudspeth, who also does medical work in Haiti and was in New York on 9/11, though not as a doctor.
Focusing, he said, was “definitely a challenge.” Even though he had faith in hospital security, there was still “some notion of ‘You never know exactly what’s going to happen.’”
“You focus on the patient that’s in front of you. You focus on trying to solve the issues that are at hand. You deal with the logistical questions that come up between patients,” he said. “By and large, just put your nose to the grindstone.”
The doctors said that hospitalists had an unclear role in the response effort and hope to have their roles clarified so that they can better put to use their expertise in internal medicine. If hospitalists are monitoring general medical issues, that will help take some of the pressure off the trauma team.
“We know the [general] medicine stuff very well—that is our bread and butter,” said Dr. Hudspeth, who added that steps are being taken as part of Boston Medical Center’s post-response analysis to determine hospitalists’ role in future disaster responses.
They also said they felt fortunate that the bombings had occurred where they did, with so many hospitals close to the scene. It kept the system from becoming overwhelmed. Even so, “at some point, a disaster is so large that it would overwhelm any system, no matter how many resources were available,” Dr. Hale added.
Dr. Jangi said that he thinks his residency training helped him when he found himself having to provide care in a high-pressure situation in the medical tent.
“During residency, there are a lot of situations where you’re responsible for making a decision on your feet,” he said. “That’s a skill that you’re not really exposed to until you do it and that type of fast decision-making. I felt myself drawing on that. Not that I resuscitated anyone in the tent, but I felt more comfortable with uncertainty, with doing your duty in a situation of uncertainty. And I don’t know—maybe if I hadn’t gone through that, I would have just run out of there.”
He said the experience has helped make him more committed as a doctor.
“It makes it easier to remember what my duty is more, and it just gives me more empathy for suffering in general—I feel that very strongly,” he said. “It’s possible that this experience could have numbed me, but it didn’t. It’s made me more acute to the idea of people suffering.”
Tom Collins is a freelance writer in South Florida.
Reference
Moore Medical Center a Casualty of Tornado’s Fury
After a monstrous tornado roared through Moore, Okla., chewing up and spitting out everything in its path, hospitalist Joe R. Womble, MD, who was off that day, wondered what had become of his colleagues, his patients, and his hospital, Moore Medical Center.
The initial news was encouraging: Everyone who had been inside the hospital—roughly 200 to 300 people, including a few dozen patients—had survived. He thought that boded well for the hospital as well.
“When I was getting information back from people who were there and I was hearing that everyone was fine, all the patients and staff, and no one got injured, I was thinking that either the hospital was missed by the storm, or that it must not have really damaged it very significantly,” says Dr. Womble. “And then they started showing aerial shots [on TV] and I was just shocked. My jaw was just dropped. The main entrance that I would go in every day was literally stacked three or four cars deep with … about 30 cars.” Likewise, the storm ripped through patient rooms on the second floor, obliterating some and reducing others to their steel innards.
About a week after the storm, word came back that Moore Medical Center will have to be demolished.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” says Dr. Womble. “It’s the only hospital in that city of Moore, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem.
“And so I definitely feel a tie to the community. … Now that it’s gone, it’s just hard to put into words,” he says. “I would just say devastating, I guess.”
After a monstrous tornado roared through Moore, Okla., chewing up and spitting out everything in its path, hospitalist Joe R. Womble, MD, who was off that day, wondered what had become of his colleagues, his patients, and his hospital, Moore Medical Center.
The initial news was encouraging: Everyone who had been inside the hospital—roughly 200 to 300 people, including a few dozen patients—had survived. He thought that boded well for the hospital as well.
“When I was getting information back from people who were there and I was hearing that everyone was fine, all the patients and staff, and no one got injured, I was thinking that either the hospital was missed by the storm, or that it must not have really damaged it very significantly,” says Dr. Womble. “And then they started showing aerial shots [on TV] and I was just shocked. My jaw was just dropped. The main entrance that I would go in every day was literally stacked three or four cars deep with … about 30 cars.” Likewise, the storm ripped through patient rooms on the second floor, obliterating some and reducing others to their steel innards.
About a week after the storm, word came back that Moore Medical Center will have to be demolished.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” says Dr. Womble. “It’s the only hospital in that city of Moore, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem.
“And so I definitely feel a tie to the community. … Now that it’s gone, it’s just hard to put into words,” he says. “I would just say devastating, I guess.”
After a monstrous tornado roared through Moore, Okla., chewing up and spitting out everything in its path, hospitalist Joe R. Womble, MD, who was off that day, wondered what had become of his colleagues, his patients, and his hospital, Moore Medical Center.
The initial news was encouraging: Everyone who had been inside the hospital—roughly 200 to 300 people, including a few dozen patients—had survived. He thought that boded well for the hospital as well.
“When I was getting information back from people who were there and I was hearing that everyone was fine, all the patients and staff, and no one got injured, I was thinking that either the hospital was missed by the storm, or that it must not have really damaged it very significantly,” says Dr. Womble. “And then they started showing aerial shots [on TV] and I was just shocked. My jaw was just dropped. The main entrance that I would go in every day was literally stacked three or four cars deep with … about 30 cars.” Likewise, the storm ripped through patient rooms on the second floor, obliterating some and reducing others to their steel innards.
About a week after the storm, word came back that Moore Medical Center will have to be demolished.
“Nobody knows what will happen next, but a lot of us speculate that they will not rebuild an inpatient facility,” says Dr. Womble. “It’s the only hospital in that city of Moore, and it’s just me and my partner to take care of virtually everyone that comes in with any kind of medical problem.
“And so I definitely feel a tie to the community. … Now that it’s gone, it’s just hard to put into words,” he says. “I would just say devastating, I guess.”
We Welcome the Newest SHM Members
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
Report: Hospitals Show Improvement on Infection Rates, but Progress Slows on CAUTIs
U.S. hospitals in 2011 showed improvements in their rates of central line-associated bloodstream infections (CLABSI) and in some surgical-site infections, compared with 2010, but the rate essentially hit a plateau for catheter-associated urinary tract infections (CAUTI), according to a new CDC report.
“Reductions in some of the deadliest healthcare-associated infections are encouraging, especially when you consider the costs to both patients and the health care system,” CDC director Thomas R. Frieden, MD, MPH, says. “However, the slower progress in reducing catheter-associated urinary tract infections is a call to action for hospitals to redouble their efforts to track these infections and implement control strategies we know that work.”
The report showed a 41% reduction in 2011 central-line infections compared with 2008, the baseline year for the report. In 2010, the reduction was 32% over the 2008 baseline. The improvement was seen across ICUs, general wards, and neonatal ICUs.

—Scott Flanders, MD, SFHM, professor of medicine, director of hospital medicine, University of Michigan Health System, Ann Arbor, former SHM president
The CDC also reported a 17% drop in surgical-site infections since 2008, better than the 7% reduction in 2010. The biggest reductions were seen in coronary artery bypass graft surgery and cardiac surgery; little improvement was seen in infections from hip arthroplasty and vaginal hysterectomy procedures.
The rate of infections from CAUTIs was 7%, nearly the same as the 6% rate in 2010 data. The infection rate in ICUs actually went up—a 1% drop in 2011 compared with a 3% drop from baseline in 2010.
SHM is a partner in two initiatives that aim to reduce CAUTI infections: the University HealthSystems Consortium’s Partnership for Patients project and On the CUSP: STOP CAUTI, an American Hospital Association HRET effort that’s funded by the Agency for Healthcare Research and Quality-funded project.
Gregory Maynard, MD, SFHM, director of hospital medicine at the University of San Diego Medical Center and senior vice president of SHM’s Center for Healthcare Improvement and Innovation is encouraged by the CLABSI and SSI figures. The report highlights the need for more effort on CAUTI.
“I think all the tools and information are available for improvement teams,” he says. “The CDC, the HRET On the CUSP group, and others all have great toolkits.”
He also says it was telling that the CAUTI numbers were worse in the ICU than in general wards.
“The more complex the environment, the easier it is for those things to get lost,” he says. “It just will probably take more attention to it and making it more of a priority.
“The more complex the environment, the easier it is for those things to get lost. It just will probably take more attention to it and making it more of a priority…. We’re supposed to reduce these adverse events by a very significant amount and obviously we’re not getting there based on this report. We have to do a better job. Reducing CAUTI by 40% is one of goals for the $500 million Partnerships for Patients effort. With that much money involved, it should increase the pressure to get this done.”
Click here to hear more of Dr. Maynard's interview with The Hospitalist
Scott Flanders, MD, SFHM, a former SHM president and SHM’s physician leader for STOP CAUTI, says the report shows that CAUTIs may be more difficult to prevent. In part, that is because catheters are used more broadly throughout a hospital than, say, central lines, which are most common in ICUs.
It takes a multi-disciplinary team implementing a variety of tools: critieria for putting catheters in, managing them appropriately once they are in, and developing protocols for removing them as quickly as possible, he adds.
“Having all those elements in place are critical to preventing CAUTI and I think many hospitals around the country have not implemented all of those strategies to reduce CAUTI,” says Dr. Flanders, professor of medicine and director of hospital medicine at the University of Michigan Health System in Ann Arbor. “No single strategy used in isolation is going to be effective.”
Efforts to reduce CAUTIs have been launched more recently than efforts to reduce other infection types, he says.
“There’s been less of a drive for CAUTI,” he says. “It’s a tougher problem to tackle than some of these other issues, which is a contributing factor in the lower rate of improvement.” TH
Tom Collins is a freelance writer in South Florida.
U.S. hospitals in 2011 showed improvements in their rates of central line-associated bloodstream infections (CLABSI) and in some surgical-site infections, compared with 2010, but the rate essentially hit a plateau for catheter-associated urinary tract infections (CAUTI), according to a new CDC report.
“Reductions in some of the deadliest healthcare-associated infections are encouraging, especially when you consider the costs to both patients and the health care system,” CDC director Thomas R. Frieden, MD, MPH, says. “However, the slower progress in reducing catheter-associated urinary tract infections is a call to action for hospitals to redouble their efforts to track these infections and implement control strategies we know that work.”
The report showed a 41% reduction in 2011 central-line infections compared with 2008, the baseline year for the report. In 2010, the reduction was 32% over the 2008 baseline. The improvement was seen across ICUs, general wards, and neonatal ICUs.

—Scott Flanders, MD, SFHM, professor of medicine, director of hospital medicine, University of Michigan Health System, Ann Arbor, former SHM president
The CDC also reported a 17% drop in surgical-site infections since 2008, better than the 7% reduction in 2010. The biggest reductions were seen in coronary artery bypass graft surgery and cardiac surgery; little improvement was seen in infections from hip arthroplasty and vaginal hysterectomy procedures.
The rate of infections from CAUTIs was 7%, nearly the same as the 6% rate in 2010 data. The infection rate in ICUs actually went up—a 1% drop in 2011 compared with a 3% drop from baseline in 2010.
SHM is a partner in two initiatives that aim to reduce CAUTI infections: the University HealthSystems Consortium’s Partnership for Patients project and On the CUSP: STOP CAUTI, an American Hospital Association HRET effort that’s funded by the Agency for Healthcare Research and Quality-funded project.
Gregory Maynard, MD, SFHM, director of hospital medicine at the University of San Diego Medical Center and senior vice president of SHM’s Center for Healthcare Improvement and Innovation is encouraged by the CLABSI and SSI figures. The report highlights the need for more effort on CAUTI.
“I think all the tools and information are available for improvement teams,” he says. “The CDC, the HRET On the CUSP group, and others all have great toolkits.”
He also says it was telling that the CAUTI numbers were worse in the ICU than in general wards.
“The more complex the environment, the easier it is for those things to get lost,” he says. “It just will probably take more attention to it and making it more of a priority.
“The more complex the environment, the easier it is for those things to get lost. It just will probably take more attention to it and making it more of a priority…. We’re supposed to reduce these adverse events by a very significant amount and obviously we’re not getting there based on this report. We have to do a better job. Reducing CAUTI by 40% is one of goals for the $500 million Partnerships for Patients effort. With that much money involved, it should increase the pressure to get this done.”
Click here to hear more of Dr. Maynard's interview with The Hospitalist
Scott Flanders, MD, SFHM, a former SHM president and SHM’s physician leader for STOP CAUTI, says the report shows that CAUTIs may be more difficult to prevent. In part, that is because catheters are used more broadly throughout a hospital than, say, central lines, which are most common in ICUs.
It takes a multi-disciplinary team implementing a variety of tools: critieria for putting catheters in, managing them appropriately once they are in, and developing protocols for removing them as quickly as possible, he adds.
“Having all those elements in place are critical to preventing CAUTI and I think many hospitals around the country have not implemented all of those strategies to reduce CAUTI,” says Dr. Flanders, professor of medicine and director of hospital medicine at the University of Michigan Health System in Ann Arbor. “No single strategy used in isolation is going to be effective.”
Efforts to reduce CAUTIs have been launched more recently than efforts to reduce other infection types, he says.
“There’s been less of a drive for CAUTI,” he says. “It’s a tougher problem to tackle than some of these other issues, which is a contributing factor in the lower rate of improvement.” TH
Tom Collins is a freelance writer in South Florida.
U.S. hospitals in 2011 showed improvements in their rates of central line-associated bloodstream infections (CLABSI) and in some surgical-site infections, compared with 2010, but the rate essentially hit a plateau for catheter-associated urinary tract infections (CAUTI), according to a new CDC report.
“Reductions in some of the deadliest healthcare-associated infections are encouraging, especially when you consider the costs to both patients and the health care system,” CDC director Thomas R. Frieden, MD, MPH, says. “However, the slower progress in reducing catheter-associated urinary tract infections is a call to action for hospitals to redouble their efforts to track these infections and implement control strategies we know that work.”
The report showed a 41% reduction in 2011 central-line infections compared with 2008, the baseline year for the report. In 2010, the reduction was 32% over the 2008 baseline. The improvement was seen across ICUs, general wards, and neonatal ICUs.

—Scott Flanders, MD, SFHM, professor of medicine, director of hospital medicine, University of Michigan Health System, Ann Arbor, former SHM president
The CDC also reported a 17% drop in surgical-site infections since 2008, better than the 7% reduction in 2010. The biggest reductions were seen in coronary artery bypass graft surgery and cardiac surgery; little improvement was seen in infections from hip arthroplasty and vaginal hysterectomy procedures.
The rate of infections from CAUTIs was 7%, nearly the same as the 6% rate in 2010 data. The infection rate in ICUs actually went up—a 1% drop in 2011 compared with a 3% drop from baseline in 2010.
SHM is a partner in two initiatives that aim to reduce CAUTI infections: the University HealthSystems Consortium’s Partnership for Patients project and On the CUSP: STOP CAUTI, an American Hospital Association HRET effort that’s funded by the Agency for Healthcare Research and Quality-funded project.
Gregory Maynard, MD, SFHM, director of hospital medicine at the University of San Diego Medical Center and senior vice president of SHM’s Center for Healthcare Improvement and Innovation is encouraged by the CLABSI and SSI figures. The report highlights the need for more effort on CAUTI.
“I think all the tools and information are available for improvement teams,” he says. “The CDC, the HRET On the CUSP group, and others all have great toolkits.”
He also says it was telling that the CAUTI numbers were worse in the ICU than in general wards.
“The more complex the environment, the easier it is for those things to get lost,” he says. “It just will probably take more attention to it and making it more of a priority.
“The more complex the environment, the easier it is for those things to get lost. It just will probably take more attention to it and making it more of a priority…. We’re supposed to reduce these adverse events by a very significant amount and obviously we’re not getting there based on this report. We have to do a better job. Reducing CAUTI by 40% is one of goals for the $500 million Partnerships for Patients effort. With that much money involved, it should increase the pressure to get this done.”
Click here to hear more of Dr. Maynard's interview with The Hospitalist
Scott Flanders, MD, SFHM, a former SHM president and SHM’s physician leader for STOP CAUTI, says the report shows that CAUTIs may be more difficult to prevent. In part, that is because catheters are used more broadly throughout a hospital than, say, central lines, which are most common in ICUs.
It takes a multi-disciplinary team implementing a variety of tools: critieria for putting catheters in, managing them appropriately once they are in, and developing protocols for removing them as quickly as possible, he adds.
“Having all those elements in place are critical to preventing CAUTI and I think many hospitals around the country have not implemented all of those strategies to reduce CAUTI,” says Dr. Flanders, professor of medicine and director of hospital medicine at the University of Michigan Health System in Ann Arbor. “No single strategy used in isolation is going to be effective.”
Efforts to reduce CAUTIs have been launched more recently than efforts to reduce other infection types, he says.
“There’s been less of a drive for CAUTI,” he says. “It’s a tougher problem to tackle than some of these other issues, which is a contributing factor in the lower rate of improvement.” TH
Tom Collins is a freelance writer in South Florida.
New Oral Anticoagulants Advance Treatment Options, Create Complications for Hospitalists
New oral anticoagulants promise to impact hospitalists and their patients—but the question is how much
When the FDA gave the nod to factor Xa-inhibitor rivaroxaban in November for use in treating acute DVT and pulmonary embolism (PE), it was just the latest development in the swiftly evolving world of oral anticoagulants—a world that hospitalists had better get used to living in, and quick.
As many as 80% of the patients that hospitalists encounter are on some kind of anticoagulant, experts say. But the extent to which the emergence of the new drugs— particularly rivaroxaban, which also is approved for stroke prevention in nonvalvular atrial fibrillation (afib) and for DVT and PE prevention in knee and hip replacement patients—will affect the daily routines of hospitalists remains to be seen.
Hospitalists specializing in VTE prevention and vascular experts say that the new drugs will make life simpler for hospitalists in some ways, mainly because for some patients, a pill will replace the injectable enoxaparin that has been used to bridge patients to warfarin. But with more options available, things will become more complicated as well, they say.
Approvals for the new agents, which aim to replace warfarin and its need for constant monitoring and concern over drug and food interactions, have been coming rapid-fire. Along with rivaroxaban in the new oral anticoagulant group are dabigatran, approved in late 2010 for stroke prevention in nonvalvular afib, and apixaban, which is expected to be approved for the same indication this year.
“Of all three drugs, [rivaroxaban] has the broadest indications for use,” said Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago. “Because of that, it’s likely that it’s going to be the agent that will be adopted much more broadly and more easily than dabigatran.”
But apixaban might come on strong in the U.S. when it’s approved because it shows better promise for patients with renal impairment and has a lower risk of intracranial hemorrhage, says Geno Merli, MD, director of the Jefferson Center for Vascular Disease and chief medical officer at Thomas Jefferson University Hospital in Philadelphia.
“I think the two other [manufacturers] are afraid of apixaban because apixaban’s safety profile was much better,” he says.
Steven Deitelzweig, MD, FACP, SFHM, secretary of the Gulf State chapter of SHM and a DVT prevention specialist at Ochsner Health System New Orleans, says hurdles to adoption of the new agents will include whether a system is integrated and can assure appropriate follow-up and concerns over proper patient selection and cost, as the cost-benefit analyses haven’t been done yet.
“The learning curve, or the adoption curve, is really going to be very variable around the country,” he says.
Experts agree changes are on the way as the new anticoagulants gain more traction. Here are some things they say hospitalists should watch out for.
Care and Discharge
Dr. Shah says the availability of the oral agents will streamline care and discharge of patients.
“The care and coordination process that needs to occur with the use of parenteral agents and warfarin is significantly more complex than the patient education and care coordination that will be required with the new oral anticoagulants,” he says. “That’s where there’s a significant time savings.”
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says the windfall of time saved might not hit hospitalists directly, at least at some centers.
“The education is being done by pharmacy here for warfarin, and nurses handle enoxaparin injection teaching,” he says. “So the workload that benefits may be that of our colleagues.”
Dr. Shah notes that the responsibility in patient counseling ultimately falls within hospitalists’ purview, so he predicts that any greater simplicity in that regard would help hospitalists.
Who Ends up Hospitalized?
The option of oral agents might help diminish the number of patients who have to stay in the hospital for enoxaparin injections that bridge them to warfarin, a topic at a recent roundtable discussion Dr. Shah attended.
“It was shocking to me that I have many colleagues throughout the country who have patients who are in the hospital simply to get parenteral injections because they can’t take them themselves at home and have no loved ones or friends to help them,” he says.
Dr. Merli agrees that the new agents might affect hospitalists’ patient census. Many patients, he says, will be discharged straight from the ED.
“The DVT patients probably won’t get [admitted]. You’re going to put them on rivaroxaban and send them home,” he says. “You’re not going to get [admitted] with a DVT anymore, unless it’s extensive. And if it’s an extensive DVT, you’re not going to get rivaroxaban. You’re going to get enoxaparin or you’re going to get thrombolytics therapy followed by IV heparin followed by enoxaparin. So I don’t see rivaroxaban jumping into the marketplace and being a boon to hospitalists immediately.”
If patients skip hospitalization and are discharged straight from the ED, Dr. Deitelzweig says, “there will be patients who will backfill those spots.”
“I think most of the people will come in as observation status, if not inpatient,” he says, although simpler DVT patients will be likelier candidates for discharge from the ER. He predicts that stays might be shorter, though.
But Dr. Merli says hospitalists shouldn’t expect a big effect on length of stay.
“I don’t think you’re going to reduce dramatically length of stay because you have an oral pill,” he says.
QI Initiatives
What might be a boon, though, are opportunities for quality-improvement (QI) initiatives related to the new therapies, Dr. Jenkins says. “Many of these projects that are being done with anticoagulants … do focus on warfarin safety; it’s a frequent part of readmission and patient harm,” he says. “Having it much simpler to treat and educate these patients is actually going to be a boon, I think, for hospitalists working on quality-improvement projects, and for people who do that education, whether that is a hospitalist or a pharmacist or some other member of the staff.”
There are downsides, though, he notes. One is cost. Another is reversibility. Warfarin can be easily reversed in the event of a bleed, but that’s not the case with rivaroxaban and dabigatran. And none of the new therapies are suitable for patients with renal failure.
“Right now, we’re stuck with IV heparin and Coumadin in the hospital, and rivaroxaban won’t change this,” he says. “Rivaroxaban patients one might help with PCC; but with dabigatran, I don’t think much will help besides time and dialysis, which is dangerous in unstable anticoagulated patients.”
Dr. Shah, though, says he’s aware of only two times that bleeding reversal protocols—based on anecdotal evidence, because no method has been scientifically proven—had to be invoked at Northwestern in the past year.
It might be “more of a theoretical problem than one in reality,” he explains, “simply because we have not found the need to reverse oral anticoagulants very often given their short half-lives.”
The new agents, all the experts agree, will require hospitalists to stay on their toes.
“There are so many different facets in each case, whether it’s the age or the renal function or whether there’s a fall risk and what their compliance is, what their funding is, what the exact indication is,” Dr. Jenkins says. “Keeping up with those things is actually quite challenging.”
His main resources are the American College of Chest Physicians’ guidelines on anticoagulants, his center’s own protocols, and the primary literature for the main trials (see “Additional Reading,” right). He also looks to the inpatient pharmacist for guidance.
Dr. Shah says it is important to be aware of the patient-inclusion criteria, study design, and outcomes measured for each agent through their trials.
“There is a lot of information out there, and there are very subtle aspects of some of these trials and you’ve got to really understand: Does it apply to the patient that is front of me?” he said. “There’s a lot to know, there’s no doubt about it.”
Thomas R. Collins is a freelance writer in South Florida.
New oral anticoagulants promise to impact hospitalists and their patients—but the question is how much
When the FDA gave the nod to factor Xa-inhibitor rivaroxaban in November for use in treating acute DVT and pulmonary embolism (PE), it was just the latest development in the swiftly evolving world of oral anticoagulants—a world that hospitalists had better get used to living in, and quick.
As many as 80% of the patients that hospitalists encounter are on some kind of anticoagulant, experts say. But the extent to which the emergence of the new drugs— particularly rivaroxaban, which also is approved for stroke prevention in nonvalvular atrial fibrillation (afib) and for DVT and PE prevention in knee and hip replacement patients—will affect the daily routines of hospitalists remains to be seen.
Hospitalists specializing in VTE prevention and vascular experts say that the new drugs will make life simpler for hospitalists in some ways, mainly because for some patients, a pill will replace the injectable enoxaparin that has been used to bridge patients to warfarin. But with more options available, things will become more complicated as well, they say.
Approvals for the new agents, which aim to replace warfarin and its need for constant monitoring and concern over drug and food interactions, have been coming rapid-fire. Along with rivaroxaban in the new oral anticoagulant group are dabigatran, approved in late 2010 for stroke prevention in nonvalvular afib, and apixaban, which is expected to be approved for the same indication this year.
“Of all three drugs, [rivaroxaban] has the broadest indications for use,” said Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago. “Because of that, it’s likely that it’s going to be the agent that will be adopted much more broadly and more easily than dabigatran.”
But apixaban might come on strong in the U.S. when it’s approved because it shows better promise for patients with renal impairment and has a lower risk of intracranial hemorrhage, says Geno Merli, MD, director of the Jefferson Center for Vascular Disease and chief medical officer at Thomas Jefferson University Hospital in Philadelphia.
“I think the two other [manufacturers] are afraid of apixaban because apixaban’s safety profile was much better,” he says.
Steven Deitelzweig, MD, FACP, SFHM, secretary of the Gulf State chapter of SHM and a DVT prevention specialist at Ochsner Health System New Orleans, says hurdles to adoption of the new agents will include whether a system is integrated and can assure appropriate follow-up and concerns over proper patient selection and cost, as the cost-benefit analyses haven’t been done yet.
“The learning curve, or the adoption curve, is really going to be very variable around the country,” he says.
Experts agree changes are on the way as the new anticoagulants gain more traction. Here are some things they say hospitalists should watch out for.
Care and Discharge
Dr. Shah says the availability of the oral agents will streamline care and discharge of patients.
“The care and coordination process that needs to occur with the use of parenteral agents and warfarin is significantly more complex than the patient education and care coordination that will be required with the new oral anticoagulants,” he says. “That’s where there’s a significant time savings.”
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says the windfall of time saved might not hit hospitalists directly, at least at some centers.
“The education is being done by pharmacy here for warfarin, and nurses handle enoxaparin injection teaching,” he says. “So the workload that benefits may be that of our colleagues.”
Dr. Shah notes that the responsibility in patient counseling ultimately falls within hospitalists’ purview, so he predicts that any greater simplicity in that regard would help hospitalists.
Who Ends up Hospitalized?
The option of oral agents might help diminish the number of patients who have to stay in the hospital for enoxaparin injections that bridge them to warfarin, a topic at a recent roundtable discussion Dr. Shah attended.
“It was shocking to me that I have many colleagues throughout the country who have patients who are in the hospital simply to get parenteral injections because they can’t take them themselves at home and have no loved ones or friends to help them,” he says.
Dr. Merli agrees that the new agents might affect hospitalists’ patient census. Many patients, he says, will be discharged straight from the ED.
“The DVT patients probably won’t get [admitted]. You’re going to put them on rivaroxaban and send them home,” he says. “You’re not going to get [admitted] with a DVT anymore, unless it’s extensive. And if it’s an extensive DVT, you’re not going to get rivaroxaban. You’re going to get enoxaparin or you’re going to get thrombolytics therapy followed by IV heparin followed by enoxaparin. So I don’t see rivaroxaban jumping into the marketplace and being a boon to hospitalists immediately.”
If patients skip hospitalization and are discharged straight from the ED, Dr. Deitelzweig says, “there will be patients who will backfill those spots.”
“I think most of the people will come in as observation status, if not inpatient,” he says, although simpler DVT patients will be likelier candidates for discharge from the ER. He predicts that stays might be shorter, though.
But Dr. Merli says hospitalists shouldn’t expect a big effect on length of stay.
“I don’t think you’re going to reduce dramatically length of stay because you have an oral pill,” he says.
QI Initiatives
What might be a boon, though, are opportunities for quality-improvement (QI) initiatives related to the new therapies, Dr. Jenkins says. “Many of these projects that are being done with anticoagulants … do focus on warfarin safety; it’s a frequent part of readmission and patient harm,” he says. “Having it much simpler to treat and educate these patients is actually going to be a boon, I think, for hospitalists working on quality-improvement projects, and for people who do that education, whether that is a hospitalist or a pharmacist or some other member of the staff.”
There are downsides, though, he notes. One is cost. Another is reversibility. Warfarin can be easily reversed in the event of a bleed, but that’s not the case with rivaroxaban and dabigatran. And none of the new therapies are suitable for patients with renal failure.
“Right now, we’re stuck with IV heparin and Coumadin in the hospital, and rivaroxaban won’t change this,” he says. “Rivaroxaban patients one might help with PCC; but with dabigatran, I don’t think much will help besides time and dialysis, which is dangerous in unstable anticoagulated patients.”
Dr. Shah, though, says he’s aware of only two times that bleeding reversal protocols—based on anecdotal evidence, because no method has been scientifically proven—had to be invoked at Northwestern in the past year.
It might be “more of a theoretical problem than one in reality,” he explains, “simply because we have not found the need to reverse oral anticoagulants very often given their short half-lives.”
The new agents, all the experts agree, will require hospitalists to stay on their toes.
“There are so many different facets in each case, whether it’s the age or the renal function or whether there’s a fall risk and what their compliance is, what their funding is, what the exact indication is,” Dr. Jenkins says. “Keeping up with those things is actually quite challenging.”
His main resources are the American College of Chest Physicians’ guidelines on anticoagulants, his center’s own protocols, and the primary literature for the main trials (see “Additional Reading,” right). He also looks to the inpatient pharmacist for guidance.
Dr. Shah says it is important to be aware of the patient-inclusion criteria, study design, and outcomes measured for each agent through their trials.
“There is a lot of information out there, and there are very subtle aspects of some of these trials and you’ve got to really understand: Does it apply to the patient that is front of me?” he said. “There’s a lot to know, there’s no doubt about it.”
Thomas R. Collins is a freelance writer in South Florida.
New oral anticoagulants promise to impact hospitalists and their patients—but the question is how much
When the FDA gave the nod to factor Xa-inhibitor rivaroxaban in November for use in treating acute DVT and pulmonary embolism (PE), it was just the latest development in the swiftly evolving world of oral anticoagulants—a world that hospitalists had better get used to living in, and quick.
As many as 80% of the patients that hospitalists encounter are on some kind of anticoagulant, experts say. But the extent to which the emergence of the new drugs— particularly rivaroxaban, which also is approved for stroke prevention in nonvalvular atrial fibrillation (afib) and for DVT and PE prevention in knee and hip replacement patients—will affect the daily routines of hospitalists remains to be seen.
Hospitalists specializing in VTE prevention and vascular experts say that the new drugs will make life simpler for hospitalists in some ways, mainly because for some patients, a pill will replace the injectable enoxaparin that has been used to bridge patients to warfarin. But with more options available, things will become more complicated as well, they say.
Approvals for the new agents, which aim to replace warfarin and its need for constant monitoring and concern over drug and food interactions, have been coming rapid-fire. Along with rivaroxaban in the new oral anticoagulant group are dabigatran, approved in late 2010 for stroke prevention in nonvalvular afib, and apixaban, which is expected to be approved for the same indication this year.
“Of all three drugs, [rivaroxaban] has the broadest indications for use,” said Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago. “Because of that, it’s likely that it’s going to be the agent that will be adopted much more broadly and more easily than dabigatran.”
But apixaban might come on strong in the U.S. when it’s approved because it shows better promise for patients with renal impairment and has a lower risk of intracranial hemorrhage, says Geno Merli, MD, director of the Jefferson Center for Vascular Disease and chief medical officer at Thomas Jefferson University Hospital in Philadelphia.
“I think the two other [manufacturers] are afraid of apixaban because apixaban’s safety profile was much better,” he says.
Steven Deitelzweig, MD, FACP, SFHM, secretary of the Gulf State chapter of SHM and a DVT prevention specialist at Ochsner Health System New Orleans, says hurdles to adoption of the new agents will include whether a system is integrated and can assure appropriate follow-up and concerns over proper patient selection and cost, as the cost-benefit analyses haven’t been done yet.
“The learning curve, or the adoption curve, is really going to be very variable around the country,” he says.
Experts agree changes are on the way as the new anticoagulants gain more traction. Here are some things they say hospitalists should watch out for.
Care and Discharge
Dr. Shah says the availability of the oral agents will streamline care and discharge of patients.
“The care and coordination process that needs to occur with the use of parenteral agents and warfarin is significantly more complex than the patient education and care coordination that will be required with the new oral anticoagulants,” he says. “That’s where there’s a significant time savings.”
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says the windfall of time saved might not hit hospitalists directly, at least at some centers.
“The education is being done by pharmacy here for warfarin, and nurses handle enoxaparin injection teaching,” he says. “So the workload that benefits may be that of our colleagues.”
Dr. Shah notes that the responsibility in patient counseling ultimately falls within hospitalists’ purview, so he predicts that any greater simplicity in that regard would help hospitalists.
Who Ends up Hospitalized?
The option of oral agents might help diminish the number of patients who have to stay in the hospital for enoxaparin injections that bridge them to warfarin, a topic at a recent roundtable discussion Dr. Shah attended.
“It was shocking to me that I have many colleagues throughout the country who have patients who are in the hospital simply to get parenteral injections because they can’t take them themselves at home and have no loved ones or friends to help them,” he says.
Dr. Merli agrees that the new agents might affect hospitalists’ patient census. Many patients, he says, will be discharged straight from the ED.
“The DVT patients probably won’t get [admitted]. You’re going to put them on rivaroxaban and send them home,” he says. “You’re not going to get [admitted] with a DVT anymore, unless it’s extensive. And if it’s an extensive DVT, you’re not going to get rivaroxaban. You’re going to get enoxaparin or you’re going to get thrombolytics therapy followed by IV heparin followed by enoxaparin. So I don’t see rivaroxaban jumping into the marketplace and being a boon to hospitalists immediately.”
If patients skip hospitalization and are discharged straight from the ED, Dr. Deitelzweig says, “there will be patients who will backfill those spots.”
“I think most of the people will come in as observation status, if not inpatient,” he says, although simpler DVT patients will be likelier candidates for discharge from the ER. He predicts that stays might be shorter, though.
But Dr. Merli says hospitalists shouldn’t expect a big effect on length of stay.
“I don’t think you’re going to reduce dramatically length of stay because you have an oral pill,” he says.
QI Initiatives
What might be a boon, though, are opportunities for quality-improvement (QI) initiatives related to the new therapies, Dr. Jenkins says. “Many of these projects that are being done with anticoagulants … do focus on warfarin safety; it’s a frequent part of readmission and patient harm,” he says. “Having it much simpler to treat and educate these patients is actually going to be a boon, I think, for hospitalists working on quality-improvement projects, and for people who do that education, whether that is a hospitalist or a pharmacist or some other member of the staff.”
There are downsides, though, he notes. One is cost. Another is reversibility. Warfarin can be easily reversed in the event of a bleed, but that’s not the case with rivaroxaban and dabigatran. And none of the new therapies are suitable for patients with renal failure.
“Right now, we’re stuck with IV heparin and Coumadin in the hospital, and rivaroxaban won’t change this,” he says. “Rivaroxaban patients one might help with PCC; but with dabigatran, I don’t think much will help besides time and dialysis, which is dangerous in unstable anticoagulated patients.”
Dr. Shah, though, says he’s aware of only two times that bleeding reversal protocols—based on anecdotal evidence, because no method has been scientifically proven—had to be invoked at Northwestern in the past year.
It might be “more of a theoretical problem than one in reality,” he explains, “simply because we have not found the need to reverse oral anticoagulants very often given their short half-lives.”
The new agents, all the experts agree, will require hospitalists to stay on their toes.
“There are so many different facets in each case, whether it’s the age or the renal function or whether there’s a fall risk and what their compliance is, what their funding is, what the exact indication is,” Dr. Jenkins says. “Keeping up with those things is actually quite challenging.”
His main resources are the American College of Chest Physicians’ guidelines on anticoagulants, his center’s own protocols, and the primary literature for the main trials (see “Additional Reading,” right). He also looks to the inpatient pharmacist for guidance.
Dr. Shah says it is important to be aware of the patient-inclusion criteria, study design, and outcomes measured for each agent through their trials.
“There is a lot of information out there, and there are very subtle aspects of some of these trials and you’ve got to really understand: Does it apply to the patient that is front of me?” he said. “There’s a lot to know, there’s no doubt about it.”
Thomas R. Collins is a freelance writer in South Florida.
Why Hospitalists Should Pay Special Attention to Kidney Disease
Need another reason to hone your skills in treating people with kidney disease?
Take a look at a study out of the University of Washington: Kidney disease, researchers there found, is the diagnosis associated with the highest rate of readmission to the hospital and the emergency room and hospital mortality—controlling for cardiovascular disease, infection, sepsis, encephalopathy and “all the usual suspects associated with readmission,” says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington Division of Nephrology.
The reasons are not known.
“One reason we think is really important is this issue of medication management,” Dr. Tuttle says.
Researchers then did a pilot study showing that, at the time of discharge, if a pharmacist visited within the first week, the rates of readmission were reduced by 50 percent. “The goal of that visit was basically do what probably should have been done through the hospital, which is adjust drug doses properly for kidney function and address drug interaction,” Dr. Tuttle says.
The research team is working on a large study funded by the National Institutes of Health to validate those findings and look at a broader population of patients. This is more evidence pointing to the importance of handoffs, she says.
"These transitions in care are dangerous situations,” Dr. Tuttle says. “But they’re also opportunities for improvement. And I think anything we can do to enhance education management is likely to be very beneficial in people with chronic kidney disease.”
Hospitalists have "serious work to do in improving continuity in care, and handoffs in general,” she adds.
“So much of what they do in the hospital is influenced by kidney function, whether it’s the drugs they give or the diagnostic tests that they want to do,” she says. “I’m not being critical at all. It’s a new area, relatively speaking, and there are lots of opportunities for improvement in the system.”
Tom Collins is a freelance writer in South Florida.
Reference
1. Risks of subsequent hospitalization and death in patients with kidney disease. Clin J Am Soc Nephrol. 2012;7(3):409-416.
Need another reason to hone your skills in treating people with kidney disease?
Take a look at a study out of the University of Washington: Kidney disease, researchers there found, is the diagnosis associated with the highest rate of readmission to the hospital and the emergency room and hospital mortality—controlling for cardiovascular disease, infection, sepsis, encephalopathy and “all the usual suspects associated with readmission,” says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington Division of Nephrology.
The reasons are not known.
“One reason we think is really important is this issue of medication management,” Dr. Tuttle says.
Researchers then did a pilot study showing that, at the time of discharge, if a pharmacist visited within the first week, the rates of readmission were reduced by 50 percent. “The goal of that visit was basically do what probably should have been done through the hospital, which is adjust drug doses properly for kidney function and address drug interaction,” Dr. Tuttle says.
The research team is working on a large study funded by the National Institutes of Health to validate those findings and look at a broader population of patients. This is more evidence pointing to the importance of handoffs, she says.
"These transitions in care are dangerous situations,” Dr. Tuttle says. “But they’re also opportunities for improvement. And I think anything we can do to enhance education management is likely to be very beneficial in people with chronic kidney disease.”
Hospitalists have "serious work to do in improving continuity in care, and handoffs in general,” she adds.
“So much of what they do in the hospital is influenced by kidney function, whether it’s the drugs they give or the diagnostic tests that they want to do,” she says. “I’m not being critical at all. It’s a new area, relatively speaking, and there are lots of opportunities for improvement in the system.”
Tom Collins is a freelance writer in South Florida.
Reference
1. Risks of subsequent hospitalization and death in patients with kidney disease. Clin J Am Soc Nephrol. 2012;7(3):409-416.
Need another reason to hone your skills in treating people with kidney disease?
Take a look at a study out of the University of Washington: Kidney disease, researchers there found, is the diagnosis associated with the highest rate of readmission to the hospital and the emergency room and hospital mortality—controlling for cardiovascular disease, infection, sepsis, encephalopathy and “all the usual suspects associated with readmission,” says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington Division of Nephrology.
The reasons are not known.
“One reason we think is really important is this issue of medication management,” Dr. Tuttle says.
Researchers then did a pilot study showing that, at the time of discharge, if a pharmacist visited within the first week, the rates of readmission were reduced by 50 percent. “The goal of that visit was basically do what probably should have been done through the hospital, which is adjust drug doses properly for kidney function and address drug interaction,” Dr. Tuttle says.
The research team is working on a large study funded by the National Institutes of Health to validate those findings and look at a broader population of patients. This is more evidence pointing to the importance of handoffs, she says.
"These transitions in care are dangerous situations,” Dr. Tuttle says. “But they’re also opportunities for improvement. And I think anything we can do to enhance education management is likely to be very beneficial in people with chronic kidney disease.”
Hospitalists have "serious work to do in improving continuity in care, and handoffs in general,” she adds.
“So much of what they do in the hospital is influenced by kidney function, whether it’s the drugs they give or the diagnostic tests that they want to do,” she says. “I’m not being critical at all. It’s a new area, relatively speaking, and there are lots of opportunities for improvement in the system.”
Tom Collins is a freelance writer in South Florida.
Reference
1. Risks of subsequent hospitalization and death in patients with kidney disease. Clin J Am Soc Nephrol. 2012;7(3):409-416.
ONLINE EXCLUSIVE: Nephrologist Acknowledges Hospitalist Evolution, Importance to Patient Care
Listent to Dr. Shaikewitz talk about hospitalists and patient care.
Listent to Dr. Shaikewitz talk about hospitalists and patient care.
Listent to Dr. Shaikewitz talk about hospitalists and patient care.
12 Things Hospitalists Need to Know About Nephrology
One number alone should be enough for hospitalists to want to know everything they can about kidney disease: 26 million. It’s the number of Americans that the National Kidney Foundation estimates to have chronic kidney disease (CKD). That’s about the same number as the American Diabetes Association’s estimate for Americans battling diabetes.
And a lot of people who have CKD don’t even know they have it, kidney specialists warn, making it that much more important to be a knowledgeable watchdog looking out for people admitted to the hospital.
The Hospitalist talked to a half-dozen experts on kidney disease, requesting their words of wisdom for hospitalists. The following are 12 things the experts believe hospitalists should keep in mind as they care for patients with kidney disease.
1) Coordination is key, especially with regard to medications and dialysis after discharge.
A goal should be to develop a “tacit understanding of who does what and just trying to see each day that everyone’s working toward the same goal, so I’m not stopping fluids and then you’re starting fluids, or vice versa,” says Ted Shaikewitz, MD, attending nephrologist at Durham (N.C.) Regional Medical Center and a nephrologist at Durham Nephrology Associates.
A key component of hospitalist-nephrologist collaboration is examining and reconciling medications.
“If it looks like they’re on too many medications, then call the specialist, as opposed to each of you expecting the other one to do it,” he says. “Just pare things down and get rid of things that are unnecessary.”
Often, Dr. Shaikewitz says, the hospitalist and the nephrologist both are reluctant to stop or tweak a medication because someone else started the patient on it. He stresses that the more a medication regimen can be simplified, the better.
Coordination is especially important for dialysis patients who are being sent home, says Ruben Velez, MD, president of the Renal Physicians Association (RPA) and president of Dallas Nephrology Associates. If a nephrologist hasn’t been contacted at discharge, the nephrologist hasn’t contacted the patient’s dialysis center to arrange treatment after the hospitalization. And that treatment likely needs to be altered from what it was before the hospitalization, Dr. Velez explains.
The dialysis center needs to get a small discharge summary, so it’s important to get that ball rolling right away, he adds.
“It’s not uncommon for a nephrologist to round in the morning and suddenly realize that the patient was sent home last night,” he says. “We go, ‘Oops. Did somebody call the dialysis center?’ and we don’t know.”
Informing the nephrologist about discharge helps them do their jobs better, he says.
“My job and my clinical responsibility is, I need to contact the treating nephrologist. I need to contact the dialysis clinic,” he says. “I need to tell them, ‘Change your medications.’ I need to tell them there’s been added antibiotics or other things. I need to tell them what they came in with and what was done. And I need to tell them if there has been a change in their weight....The dialysis clinic has difficulty in dialyzing that patient unless they get this information.”
2) Acknowledge the significance of small, early changes.
A jump in serum creatinine levels at the lower end of the range is far more serious than jumps when the creatinine already is at higher levels, says Lynda Szczech, MD, president of the National Kidney Foundation and medical director at Pharmaceutical Product Development.
“The amount of kidney function that’s described by a [serum creatinine] change of 0.1 when that 0.1” is between 1 and 2, “meaning going from 1.1 to 1.2 or 1.3 to 1.4, is huge compared to the amount of kidney function that is described by a change of 0.1 when you’re higher, when you’re going from 3.0 to 3.1,” Dr. Szczech says. “That’s important, because the earlier changes of going from 0.9 to 1.1 might not trigger a cause for concern, but they actually should be the biggest concern. When you go from a creatinine of 1 to 2, you’ve lost 50 percent of your kidney function. When you go from a creatinine of 3 to 4, you’ve probably lost about 10 percent.”
Hospitalists need to understand both the significance of the change and know “how to jump on something,” Dr. Szczech says. “That is probably the most important thing.”
3) Avoid NSAIDs in patients with advanced CKD and transplant patients.
“The nonsteroidal anti-inflammatory drugs can make your renal function much worse,” Dr. Velez says. “Those can finish your kidneys off, and you end up on dialysis.”
That concept is so simple that it’s commonly forgotten, he adds. Patients come to the hospital and are put on an NSAID and the kidneys are damaged.
“It’s horrible,” Dr. Velez says. “That’s one of the worst, and we want to avoid more damage to their kidney function.”
It’s such a common occurrence that the American Society of Nephrology (ASN) included it on their short list of suggestions for the American Board of Internal Medicine’s (ABIM) Choosing Wisely campaign, which aims to arm patients and providers with better information, promote evidence-based care, and reduce unnecessary testing and cost.
4) Don’t place PICC lines in advanced CKD and ESRD patients.
Placement of peripheral intravenous central catheter (PICC) lines in advanced CKD and end-stage renal disease (ESRD) patients is something hospitalists should “avoid as much as possible,” Dr. Velez says, “or forever.”
“PICC lines will destroy veins that we will need to use to create fistulas” needed for dialysis or potential dialysis, he explains.
This item also appears on the Choosing Wisely list.
—Michael Shapiro, MD, MBA, FACP, CPE, president, Denver Nephrology
5) Take basic steps in cases of acute kidney injury (AKI), but be careful about ordering too many tests.
Dr. Shaikewitz says there is little point in hospitalists “ordering everything they can” before the nephrologist is even consulted. That said, certain basic steps—ultrasound, urinalysis, stopping NSAIDs, stopping angiotensin-converting enzyme inhibitors, and hydration—should be taken very early, he says.
But hydrating the patient really means achieving a “euvolemic state,” he explains.
“You don’t want to drown the patient,” Dr. Shaikewitz says. Once patients “clearly have enough fluid on board, then you can stop.”
Plus, while it might sound basic, looking back at old creatinine levels is crucial.
“Oftentimes, a lot of what is going on with a patient will become obvious, and the differential will become obvious, when you have more data,” he says.
He also says it’s important to keep in mind that “patients who are in flux with kidney issues often times can tolerate higher blood pressures,” and the goal should be to get it going in the right direction, not necessarily hitting a specific number.
6) Don’t wait for AKI to progress to needing dialysis before consulting the nephrologist.
As Michael Shapiro, MD, MBA, FACP, CPE, president of Denver Nephrology, puts it, “it doesn’t have to be a catastrophe or an emergency for us to be there within a very quick period of time.”
Nephrologists would rather help out earlier than later.
“What we hate to do is have [hospitalists] spend most of the day trying to manage a problem and then calling us late in the day or in the evening, especially if a procedure like dialysis would be needed at that point in time,” he says. “It’s a lot harder to manage those troops, so to speak, once we let the day go. It’s a little bit more of a crash as opposed to a nice plan.”
Hospitalists should adopt the “earlier is better” mantra for cases of electrolyte problems, such as hypokalemia, hyperkalemia, and significant hyponatremia, or low salt levels, he notes.
“We don’t mind being curb-sided,” Dr. Shapiro says. If the specialist gets a simple heads-up about a patient on the fourth floor—even if it doesn’t require immediate action—he can then pop in and check on the status of that patient when he’s there on his rounds, he says.
Dr. Shaikewitz admits that some kidney specialists prefer not to be called in very early; therefore, it’s important for hospitalists to develop relationships and understand individual preferences. But in his case, an early referral is favorable.
“When in doubt, refer a little bit on the early side,” he says. “It’s actually kind of a fun teamwork with the hospitalists, trying to manage the patient and doing everything as a group.”
—Ruben Velez, MD, president, Renal Physicians Association, president, Dallas Nephrology Associates
7) Always call a nephrologist when a kidney transplant patient is admitted.
Robert Kossmann, MD, president-elect of the RPA, and other experts agree that it’s a good idea to at least call and inform a nephrologist that a transplant patient has been admitted. The call can go something like, “I have this patient coming in to the hospital, their kidney transplant function is fine, but they’re here with X, Y, or Z,” he says. “Is there something that we should be paying particular attention to or do you need to come see that patient?”
Dr. Kossmann says hospitalists don’t need to automatically consult a nephrologist every time, but “it’s probably a good idea to call and talk to the nephrologist every time.”
Dr. Velez says he’s seen a lot of unnecessary mistakes around transplant patients.
“There’s a lot of drug interactions with immunosuppressive drugs that these patients take that could have been prevented or avoided,” he says. “Even on patients that have fantastic renal function up to transplant … these patients can turn sour on a dime.”
8) Don’t forget the power of a simple urinalysis.
You can get a lot of diagnostic information from the urinalysis—“from a simple dipstick,” Dr. Szczech says. She points out the value of the specific gravity reading.
“A specific gravity of 1.010 in the setting of a rising creatinine [level] probably means you’ve got injury to the tubule,” she says.
The power of this simple tool can sometimes be overlooked, she says, as clinicians seek to understand how to use the newer biomarkers.
“In nephrology, we can make things quite complicated,” she adds. “We can’t forget about the low-tech stuff that we just take for granted.”
9) Simply looking at serum creatinine level is not enough.
It’s extremely important to calculate the glomerular filtration rate (GFR), says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington’s division of nephrology. Some hospital labs will do this, but hospitalists need to “make sure they review the GFR values, not just the serum creatinine,” she says.
And those readings have important ripple effects.
“Everything from need for adjustment of drugs for low GFR to drug interactions to caution about, for example, using iodinated contrasts because of risk of acute kidney injury, increased risk of infection, increased risk of cardiovascular complications,” she says. “So it’s a very important part of the clinical assessment.”
10) Know the potential benefits of isolated ultrafiltration.
This dialysis-like procedure is becoming more widely recognized as helpful for patients with congestive heart failure who have recurrent readmissions.
“This is a very small group, but a very complicated group,” Dr. Kossmann says. “You can’t keep them out of the hospital.”
Isolated ultrafiltration can help “pull off quite a lot of fluid while they’re in the hospital or in a setting where you can do that,” he adds. “That’s something that I think hospitalists may be seeing more of as this unfolds into the future. It’s a small group of people, but there’s so much heart disease in this country that it winds up being a significant increase in number.”
11) Avoid using low-molecular-weight heparins, especially Lovenox, in advanced kidney disease and dialysis patients.
Don’t just follow the protocols for preventing thromboembolic events, says Dr. Velez, who adds it’s done “very frequently.”
“In this day and age of preventing thromboembolic [events], they have protocols where they just put them on it and they don’t realize they have advanced kidney disease or end-stage renal disease,” he says. “Heparin is fine. Lovenox should be avoided.”
Such mistakes are, in part, a product of operating within a protocol-driven environment.
“Dealing with a lot of protocols and algorithms and pressure from the hospital and you name it—and we’re all busy—we want to do the right thing,” Dr. Velez says. “But we don’t apply it to individual patients, and that’s a concern of having too many protocols and trying to treat everybody the same.”
Dr. Tuttle says the risk of “over-reliance” on protocols and guidelines is real.
“The problem with guidelines is people extrapolate them too far and they overinterpret them,” she says. “That happens in the hospital all the time.”
12) Take a moment and ask: Am I really comfortable handling this patient?
“It’s worth pausing at some point with yourself and sort of taking a self-assessment and saying—whether it’s nephrology, cardiology, or something else—‘Where do I feel confident and strong?’” Dr. Kossmann says. “Although it sounds overly basic, that’s an important starting point.”
He says he’s witnessed hospitalists with a wide range of comfort levels handle cases involving kidney dysfunction.
“There’s no one-size-fits-all,” he says. “Sometimes the question I get asked is, ‘Rob, what’s the general rule? When should a nephrologist be called for a consult?’ And that’s a terrible question, because it depends on the doctor who’s seeing the patient.”
Thomas Collins is a freelance writer in South Florida.
One number alone should be enough for hospitalists to want to know everything they can about kidney disease: 26 million. It’s the number of Americans that the National Kidney Foundation estimates to have chronic kidney disease (CKD). That’s about the same number as the American Diabetes Association’s estimate for Americans battling diabetes.
And a lot of people who have CKD don’t even know they have it, kidney specialists warn, making it that much more important to be a knowledgeable watchdog looking out for people admitted to the hospital.
The Hospitalist talked to a half-dozen experts on kidney disease, requesting their words of wisdom for hospitalists. The following are 12 things the experts believe hospitalists should keep in mind as they care for patients with kidney disease.
1) Coordination is key, especially with regard to medications and dialysis after discharge.
A goal should be to develop a “tacit understanding of who does what and just trying to see each day that everyone’s working toward the same goal, so I’m not stopping fluids and then you’re starting fluids, or vice versa,” says Ted Shaikewitz, MD, attending nephrologist at Durham (N.C.) Regional Medical Center and a nephrologist at Durham Nephrology Associates.
A key component of hospitalist-nephrologist collaboration is examining and reconciling medications.
“If it looks like they’re on too many medications, then call the specialist, as opposed to each of you expecting the other one to do it,” he says. “Just pare things down and get rid of things that are unnecessary.”
Often, Dr. Shaikewitz says, the hospitalist and the nephrologist both are reluctant to stop or tweak a medication because someone else started the patient on it. He stresses that the more a medication regimen can be simplified, the better.
Coordination is especially important for dialysis patients who are being sent home, says Ruben Velez, MD, president of the Renal Physicians Association (RPA) and president of Dallas Nephrology Associates. If a nephrologist hasn’t been contacted at discharge, the nephrologist hasn’t contacted the patient’s dialysis center to arrange treatment after the hospitalization. And that treatment likely needs to be altered from what it was before the hospitalization, Dr. Velez explains.
The dialysis center needs to get a small discharge summary, so it’s important to get that ball rolling right away, he adds.
“It’s not uncommon for a nephrologist to round in the morning and suddenly realize that the patient was sent home last night,” he says. “We go, ‘Oops. Did somebody call the dialysis center?’ and we don’t know.”
Informing the nephrologist about discharge helps them do their jobs better, he says.
“My job and my clinical responsibility is, I need to contact the treating nephrologist. I need to contact the dialysis clinic,” he says. “I need to tell them, ‘Change your medications.’ I need to tell them there’s been added antibiotics or other things. I need to tell them what they came in with and what was done. And I need to tell them if there has been a change in their weight....The dialysis clinic has difficulty in dialyzing that patient unless they get this information.”
2) Acknowledge the significance of small, early changes.
A jump in serum creatinine levels at the lower end of the range is far more serious than jumps when the creatinine already is at higher levels, says Lynda Szczech, MD, president of the National Kidney Foundation and medical director at Pharmaceutical Product Development.
“The amount of kidney function that’s described by a [serum creatinine] change of 0.1 when that 0.1” is between 1 and 2, “meaning going from 1.1 to 1.2 or 1.3 to 1.4, is huge compared to the amount of kidney function that is described by a change of 0.1 when you’re higher, when you’re going from 3.0 to 3.1,” Dr. Szczech says. “That’s important, because the earlier changes of going from 0.9 to 1.1 might not trigger a cause for concern, but they actually should be the biggest concern. When you go from a creatinine of 1 to 2, you’ve lost 50 percent of your kidney function. When you go from a creatinine of 3 to 4, you’ve probably lost about 10 percent.”
Hospitalists need to understand both the significance of the change and know “how to jump on something,” Dr. Szczech says. “That is probably the most important thing.”
3) Avoid NSAIDs in patients with advanced CKD and transplant patients.
“The nonsteroidal anti-inflammatory drugs can make your renal function much worse,” Dr. Velez says. “Those can finish your kidneys off, and you end up on dialysis.”
That concept is so simple that it’s commonly forgotten, he adds. Patients come to the hospital and are put on an NSAID and the kidneys are damaged.
“It’s horrible,” Dr. Velez says. “That’s one of the worst, and we want to avoid more damage to their kidney function.”
It’s such a common occurrence that the American Society of Nephrology (ASN) included it on their short list of suggestions for the American Board of Internal Medicine’s (ABIM) Choosing Wisely campaign, which aims to arm patients and providers with better information, promote evidence-based care, and reduce unnecessary testing and cost.
4) Don’t place PICC lines in advanced CKD and ESRD patients.
Placement of peripheral intravenous central catheter (PICC) lines in advanced CKD and end-stage renal disease (ESRD) patients is something hospitalists should “avoid as much as possible,” Dr. Velez says, “or forever.”
“PICC lines will destroy veins that we will need to use to create fistulas” needed for dialysis or potential dialysis, he explains.
This item also appears on the Choosing Wisely list.
—Michael Shapiro, MD, MBA, FACP, CPE, president, Denver Nephrology
5) Take basic steps in cases of acute kidney injury (AKI), but be careful about ordering too many tests.
Dr. Shaikewitz says there is little point in hospitalists “ordering everything they can” before the nephrologist is even consulted. That said, certain basic steps—ultrasound, urinalysis, stopping NSAIDs, stopping angiotensin-converting enzyme inhibitors, and hydration—should be taken very early, he says.
But hydrating the patient really means achieving a “euvolemic state,” he explains.
“You don’t want to drown the patient,” Dr. Shaikewitz says. Once patients “clearly have enough fluid on board, then you can stop.”
Plus, while it might sound basic, looking back at old creatinine levels is crucial.
“Oftentimes, a lot of what is going on with a patient will become obvious, and the differential will become obvious, when you have more data,” he says.
He also says it’s important to keep in mind that “patients who are in flux with kidney issues often times can tolerate higher blood pressures,” and the goal should be to get it going in the right direction, not necessarily hitting a specific number.
6) Don’t wait for AKI to progress to needing dialysis before consulting the nephrologist.
As Michael Shapiro, MD, MBA, FACP, CPE, president of Denver Nephrology, puts it, “it doesn’t have to be a catastrophe or an emergency for us to be there within a very quick period of time.”
Nephrologists would rather help out earlier than later.
“What we hate to do is have [hospitalists] spend most of the day trying to manage a problem and then calling us late in the day or in the evening, especially if a procedure like dialysis would be needed at that point in time,” he says. “It’s a lot harder to manage those troops, so to speak, once we let the day go. It’s a little bit more of a crash as opposed to a nice plan.”
Hospitalists should adopt the “earlier is better” mantra for cases of electrolyte problems, such as hypokalemia, hyperkalemia, and significant hyponatremia, or low salt levels, he notes.
“We don’t mind being curb-sided,” Dr. Shapiro says. If the specialist gets a simple heads-up about a patient on the fourth floor—even if it doesn’t require immediate action—he can then pop in and check on the status of that patient when he’s there on his rounds, he says.
Dr. Shaikewitz admits that some kidney specialists prefer not to be called in very early; therefore, it’s important for hospitalists to develop relationships and understand individual preferences. But in his case, an early referral is favorable.
“When in doubt, refer a little bit on the early side,” he says. “It’s actually kind of a fun teamwork with the hospitalists, trying to manage the patient and doing everything as a group.”
—Ruben Velez, MD, president, Renal Physicians Association, president, Dallas Nephrology Associates
7) Always call a nephrologist when a kidney transplant patient is admitted.
Robert Kossmann, MD, president-elect of the RPA, and other experts agree that it’s a good idea to at least call and inform a nephrologist that a transplant patient has been admitted. The call can go something like, “I have this patient coming in to the hospital, their kidney transplant function is fine, but they’re here with X, Y, or Z,” he says. “Is there something that we should be paying particular attention to or do you need to come see that patient?”
Dr. Kossmann says hospitalists don’t need to automatically consult a nephrologist every time, but “it’s probably a good idea to call and talk to the nephrologist every time.”
Dr. Velez says he’s seen a lot of unnecessary mistakes around transplant patients.
“There’s a lot of drug interactions with immunosuppressive drugs that these patients take that could have been prevented or avoided,” he says. “Even on patients that have fantastic renal function up to transplant … these patients can turn sour on a dime.”
8) Don’t forget the power of a simple urinalysis.
You can get a lot of diagnostic information from the urinalysis—“from a simple dipstick,” Dr. Szczech says. She points out the value of the specific gravity reading.
“A specific gravity of 1.010 in the setting of a rising creatinine [level] probably means you’ve got injury to the tubule,” she says.
The power of this simple tool can sometimes be overlooked, she says, as clinicians seek to understand how to use the newer biomarkers.
“In nephrology, we can make things quite complicated,” she adds. “We can’t forget about the low-tech stuff that we just take for granted.”
9) Simply looking at serum creatinine level is not enough.
It’s extremely important to calculate the glomerular filtration rate (GFR), says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington’s division of nephrology. Some hospital labs will do this, but hospitalists need to “make sure they review the GFR values, not just the serum creatinine,” she says.
And those readings have important ripple effects.
“Everything from need for adjustment of drugs for low GFR to drug interactions to caution about, for example, using iodinated contrasts because of risk of acute kidney injury, increased risk of infection, increased risk of cardiovascular complications,” she says. “So it’s a very important part of the clinical assessment.”
10) Know the potential benefits of isolated ultrafiltration.
This dialysis-like procedure is becoming more widely recognized as helpful for patients with congestive heart failure who have recurrent readmissions.
“This is a very small group, but a very complicated group,” Dr. Kossmann says. “You can’t keep them out of the hospital.”
Isolated ultrafiltration can help “pull off quite a lot of fluid while they’re in the hospital or in a setting where you can do that,” he adds. “That’s something that I think hospitalists may be seeing more of as this unfolds into the future. It’s a small group of people, but there’s so much heart disease in this country that it winds up being a significant increase in number.”
11) Avoid using low-molecular-weight heparins, especially Lovenox, in advanced kidney disease and dialysis patients.
Don’t just follow the protocols for preventing thromboembolic events, says Dr. Velez, who adds it’s done “very frequently.”
“In this day and age of preventing thromboembolic [events], they have protocols where they just put them on it and they don’t realize they have advanced kidney disease or end-stage renal disease,” he says. “Heparin is fine. Lovenox should be avoided.”
Such mistakes are, in part, a product of operating within a protocol-driven environment.
“Dealing with a lot of protocols and algorithms and pressure from the hospital and you name it—and we’re all busy—we want to do the right thing,” Dr. Velez says. “But we don’t apply it to individual patients, and that’s a concern of having too many protocols and trying to treat everybody the same.”
Dr. Tuttle says the risk of “over-reliance” on protocols and guidelines is real.
“The problem with guidelines is people extrapolate them too far and they overinterpret them,” she says. “That happens in the hospital all the time.”
12) Take a moment and ask: Am I really comfortable handling this patient?
“It’s worth pausing at some point with yourself and sort of taking a self-assessment and saying—whether it’s nephrology, cardiology, or something else—‘Where do I feel confident and strong?’” Dr. Kossmann says. “Although it sounds overly basic, that’s an important starting point.”
He says he’s witnessed hospitalists with a wide range of comfort levels handle cases involving kidney dysfunction.
“There’s no one-size-fits-all,” he says. “Sometimes the question I get asked is, ‘Rob, what’s the general rule? When should a nephrologist be called for a consult?’ And that’s a terrible question, because it depends on the doctor who’s seeing the patient.”
Thomas Collins is a freelance writer in South Florida.
One number alone should be enough for hospitalists to want to know everything they can about kidney disease: 26 million. It’s the number of Americans that the National Kidney Foundation estimates to have chronic kidney disease (CKD). That’s about the same number as the American Diabetes Association’s estimate for Americans battling diabetes.
And a lot of people who have CKD don’t even know they have it, kidney specialists warn, making it that much more important to be a knowledgeable watchdog looking out for people admitted to the hospital.
The Hospitalist talked to a half-dozen experts on kidney disease, requesting their words of wisdom for hospitalists. The following are 12 things the experts believe hospitalists should keep in mind as they care for patients with kidney disease.
1) Coordination is key, especially with regard to medications and dialysis after discharge.
A goal should be to develop a “tacit understanding of who does what and just trying to see each day that everyone’s working toward the same goal, so I’m not stopping fluids and then you’re starting fluids, or vice versa,” says Ted Shaikewitz, MD, attending nephrologist at Durham (N.C.) Regional Medical Center and a nephrologist at Durham Nephrology Associates.
A key component of hospitalist-nephrologist collaboration is examining and reconciling medications.
“If it looks like they’re on too many medications, then call the specialist, as opposed to each of you expecting the other one to do it,” he says. “Just pare things down and get rid of things that are unnecessary.”
Often, Dr. Shaikewitz says, the hospitalist and the nephrologist both are reluctant to stop or tweak a medication because someone else started the patient on it. He stresses that the more a medication regimen can be simplified, the better.
Coordination is especially important for dialysis patients who are being sent home, says Ruben Velez, MD, president of the Renal Physicians Association (RPA) and president of Dallas Nephrology Associates. If a nephrologist hasn’t been contacted at discharge, the nephrologist hasn’t contacted the patient’s dialysis center to arrange treatment after the hospitalization. And that treatment likely needs to be altered from what it was before the hospitalization, Dr. Velez explains.
The dialysis center needs to get a small discharge summary, so it’s important to get that ball rolling right away, he adds.
“It’s not uncommon for a nephrologist to round in the morning and suddenly realize that the patient was sent home last night,” he says. “We go, ‘Oops. Did somebody call the dialysis center?’ and we don’t know.”
Informing the nephrologist about discharge helps them do their jobs better, he says.
“My job and my clinical responsibility is, I need to contact the treating nephrologist. I need to contact the dialysis clinic,” he says. “I need to tell them, ‘Change your medications.’ I need to tell them there’s been added antibiotics or other things. I need to tell them what they came in with and what was done. And I need to tell them if there has been a change in their weight....The dialysis clinic has difficulty in dialyzing that patient unless they get this information.”
2) Acknowledge the significance of small, early changes.
A jump in serum creatinine levels at the lower end of the range is far more serious than jumps when the creatinine already is at higher levels, says Lynda Szczech, MD, president of the National Kidney Foundation and medical director at Pharmaceutical Product Development.
“The amount of kidney function that’s described by a [serum creatinine] change of 0.1 when that 0.1” is between 1 and 2, “meaning going from 1.1 to 1.2 or 1.3 to 1.4, is huge compared to the amount of kidney function that is described by a change of 0.1 when you’re higher, when you’re going from 3.0 to 3.1,” Dr. Szczech says. “That’s important, because the earlier changes of going from 0.9 to 1.1 might not trigger a cause for concern, but they actually should be the biggest concern. When you go from a creatinine of 1 to 2, you’ve lost 50 percent of your kidney function. When you go from a creatinine of 3 to 4, you’ve probably lost about 10 percent.”
Hospitalists need to understand both the significance of the change and know “how to jump on something,” Dr. Szczech says. “That is probably the most important thing.”
3) Avoid NSAIDs in patients with advanced CKD and transplant patients.
“The nonsteroidal anti-inflammatory drugs can make your renal function much worse,” Dr. Velez says. “Those can finish your kidneys off, and you end up on dialysis.”
That concept is so simple that it’s commonly forgotten, he adds. Patients come to the hospital and are put on an NSAID and the kidneys are damaged.
“It’s horrible,” Dr. Velez says. “That’s one of the worst, and we want to avoid more damage to their kidney function.”
It’s such a common occurrence that the American Society of Nephrology (ASN) included it on their short list of suggestions for the American Board of Internal Medicine’s (ABIM) Choosing Wisely campaign, which aims to arm patients and providers with better information, promote evidence-based care, and reduce unnecessary testing and cost.
4) Don’t place PICC lines in advanced CKD and ESRD patients.
Placement of peripheral intravenous central catheter (PICC) lines in advanced CKD and end-stage renal disease (ESRD) patients is something hospitalists should “avoid as much as possible,” Dr. Velez says, “or forever.”
“PICC lines will destroy veins that we will need to use to create fistulas” needed for dialysis or potential dialysis, he explains.
This item also appears on the Choosing Wisely list.
—Michael Shapiro, MD, MBA, FACP, CPE, president, Denver Nephrology
5) Take basic steps in cases of acute kidney injury (AKI), but be careful about ordering too many tests.
Dr. Shaikewitz says there is little point in hospitalists “ordering everything they can” before the nephrologist is even consulted. That said, certain basic steps—ultrasound, urinalysis, stopping NSAIDs, stopping angiotensin-converting enzyme inhibitors, and hydration—should be taken very early, he says.
But hydrating the patient really means achieving a “euvolemic state,” he explains.
“You don’t want to drown the patient,” Dr. Shaikewitz says. Once patients “clearly have enough fluid on board, then you can stop.”
Plus, while it might sound basic, looking back at old creatinine levels is crucial.
“Oftentimes, a lot of what is going on with a patient will become obvious, and the differential will become obvious, when you have more data,” he says.
He also says it’s important to keep in mind that “patients who are in flux with kidney issues often times can tolerate higher blood pressures,” and the goal should be to get it going in the right direction, not necessarily hitting a specific number.
6) Don’t wait for AKI to progress to needing dialysis before consulting the nephrologist.
As Michael Shapiro, MD, MBA, FACP, CPE, president of Denver Nephrology, puts it, “it doesn’t have to be a catastrophe or an emergency for us to be there within a very quick period of time.”
Nephrologists would rather help out earlier than later.
“What we hate to do is have [hospitalists] spend most of the day trying to manage a problem and then calling us late in the day or in the evening, especially if a procedure like dialysis would be needed at that point in time,” he says. “It’s a lot harder to manage those troops, so to speak, once we let the day go. It’s a little bit more of a crash as opposed to a nice plan.”
Hospitalists should adopt the “earlier is better” mantra for cases of electrolyte problems, such as hypokalemia, hyperkalemia, and significant hyponatremia, or low salt levels, he notes.
“We don’t mind being curb-sided,” Dr. Shapiro says. If the specialist gets a simple heads-up about a patient on the fourth floor—even if it doesn’t require immediate action—he can then pop in and check on the status of that patient when he’s there on his rounds, he says.
Dr. Shaikewitz admits that some kidney specialists prefer not to be called in very early; therefore, it’s important for hospitalists to develop relationships and understand individual preferences. But in his case, an early referral is favorable.
“When in doubt, refer a little bit on the early side,” he says. “It’s actually kind of a fun teamwork with the hospitalists, trying to manage the patient and doing everything as a group.”
—Ruben Velez, MD, president, Renal Physicians Association, president, Dallas Nephrology Associates
7) Always call a nephrologist when a kidney transplant patient is admitted.
Robert Kossmann, MD, president-elect of the RPA, and other experts agree that it’s a good idea to at least call and inform a nephrologist that a transplant patient has been admitted. The call can go something like, “I have this patient coming in to the hospital, their kidney transplant function is fine, but they’re here with X, Y, or Z,” he says. “Is there something that we should be paying particular attention to or do you need to come see that patient?”
Dr. Kossmann says hospitalists don’t need to automatically consult a nephrologist every time, but “it’s probably a good idea to call and talk to the nephrologist every time.”
Dr. Velez says he’s seen a lot of unnecessary mistakes around transplant patients.
“There’s a lot of drug interactions with immunosuppressive drugs that these patients take that could have been prevented or avoided,” he says. “Even on patients that have fantastic renal function up to transplant … these patients can turn sour on a dime.”
8) Don’t forget the power of a simple urinalysis.
You can get a lot of diagnostic information from the urinalysis—“from a simple dipstick,” Dr. Szczech says. She points out the value of the specific gravity reading.
“A specific gravity of 1.010 in the setting of a rising creatinine [level] probably means you’ve got injury to the tubule,” she says.
The power of this simple tool can sometimes be overlooked, she says, as clinicians seek to understand how to use the newer biomarkers.
“In nephrology, we can make things quite complicated,” she adds. “We can’t forget about the low-tech stuff that we just take for granted.”
9) Simply looking at serum creatinine level is not enough.
It’s extremely important to calculate the glomerular filtration rate (GFR), says Katherine Tuttle, MD, clinical professor of medicine in the University of Washington’s division of nephrology. Some hospital labs will do this, but hospitalists need to “make sure they review the GFR values, not just the serum creatinine,” she says.
And those readings have important ripple effects.
“Everything from need for adjustment of drugs for low GFR to drug interactions to caution about, for example, using iodinated contrasts because of risk of acute kidney injury, increased risk of infection, increased risk of cardiovascular complications,” she says. “So it’s a very important part of the clinical assessment.”
10) Know the potential benefits of isolated ultrafiltration.
This dialysis-like procedure is becoming more widely recognized as helpful for patients with congestive heart failure who have recurrent readmissions.
“This is a very small group, but a very complicated group,” Dr. Kossmann says. “You can’t keep them out of the hospital.”
Isolated ultrafiltration can help “pull off quite a lot of fluid while they’re in the hospital or in a setting where you can do that,” he adds. “That’s something that I think hospitalists may be seeing more of as this unfolds into the future. It’s a small group of people, but there’s so much heart disease in this country that it winds up being a significant increase in number.”
11) Avoid using low-molecular-weight heparins, especially Lovenox, in advanced kidney disease and dialysis patients.
Don’t just follow the protocols for preventing thromboembolic events, says Dr. Velez, who adds it’s done “very frequently.”
“In this day and age of preventing thromboembolic [events], they have protocols where they just put them on it and they don’t realize they have advanced kidney disease or end-stage renal disease,” he says. “Heparin is fine. Lovenox should be avoided.”
Such mistakes are, in part, a product of operating within a protocol-driven environment.
“Dealing with a lot of protocols and algorithms and pressure from the hospital and you name it—and we’re all busy—we want to do the right thing,” Dr. Velez says. “But we don’t apply it to individual patients, and that’s a concern of having too many protocols and trying to treat everybody the same.”
Dr. Tuttle says the risk of “over-reliance” on protocols and guidelines is real.
“The problem with guidelines is people extrapolate them too far and they overinterpret them,” she says. “That happens in the hospital all the time.”
12) Take a moment and ask: Am I really comfortable handling this patient?
“It’s worth pausing at some point with yourself and sort of taking a self-assessment and saying—whether it’s nephrology, cardiology, or something else—‘Where do I feel confident and strong?’” Dr. Kossmann says. “Although it sounds overly basic, that’s an important starting point.”
He says he’s witnessed hospitalists with a wide range of comfort levels handle cases involving kidney dysfunction.
“There’s no one-size-fits-all,” he says. “Sometimes the question I get asked is, ‘Rob, what’s the general rule? When should a nephrologist be called for a consult?’ And that’s a terrible question, because it depends on the doctor who’s seeing the patient.”
Thomas Collins is a freelance writer in South Florida.