User login
Hard nodular lesions over the chest wall
A 56-year-old woman came to our clinic with nodular, indurated, itchy, painful skin lesions over her left anterior chest wall that she had for a month. She was also experiencing lower back pain that had started 2 months before the skin lesions had developed. Thirteen years earlier, the patient had been diagnosed with breast cancer (infiltrating ductal carcinoma stage T2 N1 M0) and had undergone a left modified radical mastectomy. She was advised to receive chemotherapy and radiotherapy after the surgery, but refused further treatment.
During the examination, we noted multiple elevated, nodular, erythematous, indurated skin lesions over the left side of her anterior chest wall near the mastectomy scar that measured approximately 8 × 7 cm (FIGURE 1). The axillary lymph nodes were not swollen and there was no bone tenderness on palpation. The rest of the exam was normal.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cancer-en-cuirasse
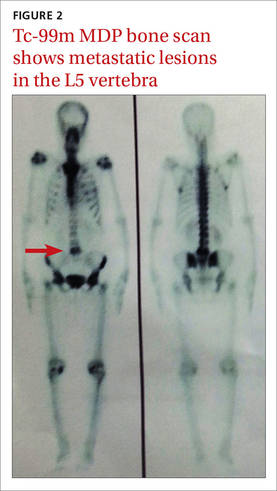
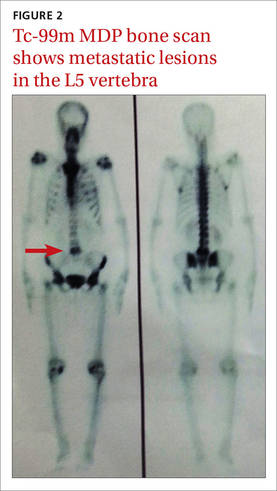
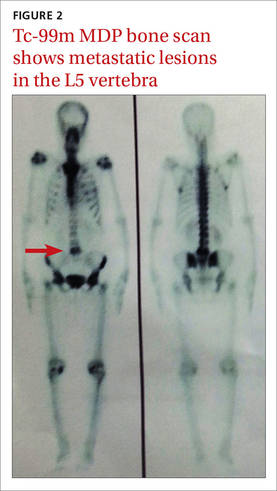
A core biopsy taken from our patient’s nodular region confirmed the presence of a dermal tumor. Review of the histopathologic slide revealed cells that had invaded through the basement membrane. The invasive cells were arranged as either strands or singly placed cells. Signet ring cells and increased mitosis were also seen. The intervening stroma showed desmoplasia and lymphocytic infiltrates. All of this suggested infiltrating ductal carcinoma. Immunohistochemistry was negative for estrogen receptors (ER), progesterone receptors (PR), and HER2 (human epidermal growth factor receptor 2). A bone scan using Tc-99m MDP also showed metastatic lesions in the L5 vertebra (FIGURE 2).
Cancer-en-cuirasse (en cuirasse is French for “in armor”) is a form of cutaneous metastasis that most commonly arises from breast carcinoma (69%). It can also arise from colon carcinoma (9%), melanoma (5%), ovarian carcinoma (4%), and cervical carcinoma (2%).1
The condition is characterized by the invasion of malignant cells into the cutaneous layers of the chest wall—subsequently involving interstitial spaces and lymphatics—resulting in the formation of a tough, fibrotic lesion that’s comparable to an armor or breastplate.2
While cancer-en-cuirasse is usually a local recurrence of carcinoma in patients with a history of breast cancer after mastectomy, it can, on rare occasions, be a clue for the diagnosis of underlying primary breast carcinoma.3
Cancer-en-cuirasse can be mistaken for lymphoma-en-cuirasse or angiosarcoma; a core biopsy is the definitive test to make a diagnosis.
Treatment includes systemic therapy and possibly surgery
The main goal of treatment for patients with metastatic breast cancer is to relieve symptoms and prolong the patient’s life, while ensuring minimal treatment-related adverse effects. The mainstay of treatment is systemic therapy, and in certain circumstances, surgery and/or radiation. Systemic therapy includes endocrine therapy, chemotherapy, and/or biologic agents depending upon the patient’s hormonal receptor status and expression of HER2.
Combination chemotherapy is preferred because it is associated with higher response rates, longer progression-free survival, and a modest improvement in overall survival compared with sequential single-agent chemotherapy.4 According to numerous trials conducted by The French Epirubicin Study Group, the FEC (fluorouracil, epirubicin, and cyclophosphamide) regimen for metastatic breast cancer has been demonstrated to be more effective in terms of response rate, time to progression (TTP), and overall survival compared to the FAC (fluorouracil, doxorubicin, and cyclophosphamide) regimen.5 The FEC regimen also has fewer hematologic, gastrointestinal, and cardiac adverse effects.5 Four initial cycles of FEC should be administered with identical retreatment based on disease progression.5 The duration of chemotherapy is based on how well the patient can tolerate adverse effects and the patient’s informed opinion.
Zoledronic acid has been shown to directly inhibit cell proliferation and induce apoptosis of metastatic/highly tumorigenic cancer cells.6 It also interferes with osteoclast function, slows bone resorption, and thus prevents future skeletal morbidity from the bone lesion.6 Zoledronic acid is administered along with chemotherapy for one year. It is administered continuously for 3 weeks, followed by a one-week break before the next cycle.
Our patient was ER, PR, and HER2 negative, and that limited our treatment options. Based on the National Comprehensive Cancer Network guidelines and our patient’s financial status, we decided on a course of treatment that included 6 cycles of FEC with zoledronic acid, followed by external beam radiotherapy.7
Fifteen days after the third cycle, our patient developed pleural effusion and a pigtail catheter was placed for drainage. Fluid cytology revealed no evidence of malignant cells. We resumed and completed the 6 cycles of chemotherapy. The patient did not receive radiation therapy and was lost to follow-up.
CORRESPONDENCE
Raghunath Prabhu, MD, Department of Surgery, Kasturba Medical College, Manipal University, Manipal, Karnataka, India 576104; [email protected].
1. McKee PH, Calonje E, Granter SR. Cutaneous metastases and Paget’s disease of the skin. In: Pathology of the skin with clinical correlations. Philadelphia, PA: Elsevier Mosby;2005:1514-1518.
2. Handley WS. Cancer of the breast and its treatment. 2nd ed. London, England: John Murray;1922:17.
3. Mahore SD, Bothale KA, Patrikar AD, et al. Carcinoma en cuirasse: a rare presentation of breast cancer. Indian J Pathol Microbiol. 2010;53:351-358.
4. Carrick S, Parker S, Wilcken N, et al. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane Database Syst Rev. 2005;CD003372.
5. French Epirubicin Study Group. Epirubicin-based chemotherapy in metastatic breast cancer patients: role of dose-intensity and duration of treatment. J Clin Oncol. 2000;18:3115-3124.
6. Almubarak H, Jones A, Chaisuparat R, et al. Zoledronic acid directly suppresses cell proliferation and induces apoptosis in highly tumorigenic prostate and breast cancers. J Carcinog. 2011;10:2.
7. National Comprehensive Cancer Network. Clinical practice guidelines in oncology. Breast cancer. Version 3. National Comprehensive Cancer Network Web site. Available at: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 2014.
A 56-year-old woman came to our clinic with nodular, indurated, itchy, painful skin lesions over her left anterior chest wall that she had for a month. She was also experiencing lower back pain that had started 2 months before the skin lesions had developed. Thirteen years earlier, the patient had been diagnosed with breast cancer (infiltrating ductal carcinoma stage T2 N1 M0) and had undergone a left modified radical mastectomy. She was advised to receive chemotherapy and radiotherapy after the surgery, but refused further treatment.
During the examination, we noted multiple elevated, nodular, erythematous, indurated skin lesions over the left side of her anterior chest wall near the mastectomy scar that measured approximately 8 × 7 cm (FIGURE 1). The axillary lymph nodes were not swollen and there was no bone tenderness on palpation. The rest of the exam was normal.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cancer-en-cuirasse
A core biopsy taken from our patient’s nodular region confirmed the presence of a dermal tumor. Review of the histopathologic slide revealed cells that had invaded through the basement membrane. The invasive cells were arranged as either strands or singly placed cells. Signet ring cells and increased mitosis were also seen. The intervening stroma showed desmoplasia and lymphocytic infiltrates. All of this suggested infiltrating ductal carcinoma. Immunohistochemistry was negative for estrogen receptors (ER), progesterone receptors (PR), and HER2 (human epidermal growth factor receptor 2). A bone scan using Tc-99m MDP also showed metastatic lesions in the L5 vertebra (FIGURE 2).
Cancer-en-cuirasse (en cuirasse is French for “in armor”) is a form of cutaneous metastasis that most commonly arises from breast carcinoma (69%). It can also arise from colon carcinoma (9%), melanoma (5%), ovarian carcinoma (4%), and cervical carcinoma (2%).1
The condition is characterized by the invasion of malignant cells into the cutaneous layers of the chest wall—subsequently involving interstitial spaces and lymphatics—resulting in the formation of a tough, fibrotic lesion that’s comparable to an armor or breastplate.2
While cancer-en-cuirasse is usually a local recurrence of carcinoma in patients with a history of breast cancer after mastectomy, it can, on rare occasions, be a clue for the diagnosis of underlying primary breast carcinoma.3
Cancer-en-cuirasse can be mistaken for lymphoma-en-cuirasse or angiosarcoma; a core biopsy is the definitive test to make a diagnosis.
Treatment includes systemic therapy and possibly surgery
The main goal of treatment for patients with metastatic breast cancer is to relieve symptoms and prolong the patient’s life, while ensuring minimal treatment-related adverse effects. The mainstay of treatment is systemic therapy, and in certain circumstances, surgery and/or radiation. Systemic therapy includes endocrine therapy, chemotherapy, and/or biologic agents depending upon the patient’s hormonal receptor status and expression of HER2.
Combination chemotherapy is preferred because it is associated with higher response rates, longer progression-free survival, and a modest improvement in overall survival compared with sequential single-agent chemotherapy.4 According to numerous trials conducted by The French Epirubicin Study Group, the FEC (fluorouracil, epirubicin, and cyclophosphamide) regimen for metastatic breast cancer has been demonstrated to be more effective in terms of response rate, time to progression (TTP), and overall survival compared to the FAC (fluorouracil, doxorubicin, and cyclophosphamide) regimen.5 The FEC regimen also has fewer hematologic, gastrointestinal, and cardiac adverse effects.5 Four initial cycles of FEC should be administered with identical retreatment based on disease progression.5 The duration of chemotherapy is based on how well the patient can tolerate adverse effects and the patient’s informed opinion.
Zoledronic acid has been shown to directly inhibit cell proliferation and induce apoptosis of metastatic/highly tumorigenic cancer cells.6 It also interferes with osteoclast function, slows bone resorption, and thus prevents future skeletal morbidity from the bone lesion.6 Zoledronic acid is administered along with chemotherapy for one year. It is administered continuously for 3 weeks, followed by a one-week break before the next cycle.
Our patient was ER, PR, and HER2 negative, and that limited our treatment options. Based on the National Comprehensive Cancer Network guidelines and our patient’s financial status, we decided on a course of treatment that included 6 cycles of FEC with zoledronic acid, followed by external beam radiotherapy.7
Fifteen days after the third cycle, our patient developed pleural effusion and a pigtail catheter was placed for drainage. Fluid cytology revealed no evidence of malignant cells. We resumed and completed the 6 cycles of chemotherapy. The patient did not receive radiation therapy and was lost to follow-up.
CORRESPONDENCE
Raghunath Prabhu, MD, Department of Surgery, Kasturba Medical College, Manipal University, Manipal, Karnataka, India 576104; [email protected].
A 56-year-old woman came to our clinic with nodular, indurated, itchy, painful skin lesions over her left anterior chest wall that she had for a month. She was also experiencing lower back pain that had started 2 months before the skin lesions had developed. Thirteen years earlier, the patient had been diagnosed with breast cancer (infiltrating ductal carcinoma stage T2 N1 M0) and had undergone a left modified radical mastectomy. She was advised to receive chemotherapy and radiotherapy after the surgery, but refused further treatment.
During the examination, we noted multiple elevated, nodular, erythematous, indurated skin lesions over the left side of her anterior chest wall near the mastectomy scar that measured approximately 8 × 7 cm (FIGURE 1). The axillary lymph nodes were not swollen and there was no bone tenderness on palpation. The rest of the exam was normal.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cancer-en-cuirasse
A core biopsy taken from our patient’s nodular region confirmed the presence of a dermal tumor. Review of the histopathologic slide revealed cells that had invaded through the basement membrane. The invasive cells were arranged as either strands or singly placed cells. Signet ring cells and increased mitosis were also seen. The intervening stroma showed desmoplasia and lymphocytic infiltrates. All of this suggested infiltrating ductal carcinoma. Immunohistochemistry was negative for estrogen receptors (ER), progesterone receptors (PR), and HER2 (human epidermal growth factor receptor 2). A bone scan using Tc-99m MDP also showed metastatic lesions in the L5 vertebra (FIGURE 2).
Cancer-en-cuirasse (en cuirasse is French for “in armor”) is a form of cutaneous metastasis that most commonly arises from breast carcinoma (69%). It can also arise from colon carcinoma (9%), melanoma (5%), ovarian carcinoma (4%), and cervical carcinoma (2%).1
The condition is characterized by the invasion of malignant cells into the cutaneous layers of the chest wall—subsequently involving interstitial spaces and lymphatics—resulting in the formation of a tough, fibrotic lesion that’s comparable to an armor or breastplate.2
While cancer-en-cuirasse is usually a local recurrence of carcinoma in patients with a history of breast cancer after mastectomy, it can, on rare occasions, be a clue for the diagnosis of underlying primary breast carcinoma.3
Cancer-en-cuirasse can be mistaken for lymphoma-en-cuirasse or angiosarcoma; a core biopsy is the definitive test to make a diagnosis.
Treatment includes systemic therapy and possibly surgery
The main goal of treatment for patients with metastatic breast cancer is to relieve symptoms and prolong the patient’s life, while ensuring minimal treatment-related adverse effects. The mainstay of treatment is systemic therapy, and in certain circumstances, surgery and/or radiation. Systemic therapy includes endocrine therapy, chemotherapy, and/or biologic agents depending upon the patient’s hormonal receptor status and expression of HER2.
Combination chemotherapy is preferred because it is associated with higher response rates, longer progression-free survival, and a modest improvement in overall survival compared with sequential single-agent chemotherapy.4 According to numerous trials conducted by The French Epirubicin Study Group, the FEC (fluorouracil, epirubicin, and cyclophosphamide) regimen for metastatic breast cancer has been demonstrated to be more effective in terms of response rate, time to progression (TTP), and overall survival compared to the FAC (fluorouracil, doxorubicin, and cyclophosphamide) regimen.5 The FEC regimen also has fewer hematologic, gastrointestinal, and cardiac adverse effects.5 Four initial cycles of FEC should be administered with identical retreatment based on disease progression.5 The duration of chemotherapy is based on how well the patient can tolerate adverse effects and the patient’s informed opinion.
Zoledronic acid has been shown to directly inhibit cell proliferation and induce apoptosis of metastatic/highly tumorigenic cancer cells.6 It also interferes with osteoclast function, slows bone resorption, and thus prevents future skeletal morbidity from the bone lesion.6 Zoledronic acid is administered along with chemotherapy for one year. It is administered continuously for 3 weeks, followed by a one-week break before the next cycle.
Our patient was ER, PR, and HER2 negative, and that limited our treatment options. Based on the National Comprehensive Cancer Network guidelines and our patient’s financial status, we decided on a course of treatment that included 6 cycles of FEC with zoledronic acid, followed by external beam radiotherapy.7
Fifteen days after the third cycle, our patient developed pleural effusion and a pigtail catheter was placed for drainage. Fluid cytology revealed no evidence of malignant cells. We resumed and completed the 6 cycles of chemotherapy. The patient did not receive radiation therapy and was lost to follow-up.
CORRESPONDENCE
Raghunath Prabhu, MD, Department of Surgery, Kasturba Medical College, Manipal University, Manipal, Karnataka, India 576104; [email protected].
1. McKee PH, Calonje E, Granter SR. Cutaneous metastases and Paget’s disease of the skin. In: Pathology of the skin with clinical correlations. Philadelphia, PA: Elsevier Mosby;2005:1514-1518.
2. Handley WS. Cancer of the breast and its treatment. 2nd ed. London, England: John Murray;1922:17.
3. Mahore SD, Bothale KA, Patrikar AD, et al. Carcinoma en cuirasse: a rare presentation of breast cancer. Indian J Pathol Microbiol. 2010;53:351-358.
4. Carrick S, Parker S, Wilcken N, et al. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane Database Syst Rev. 2005;CD003372.
5. French Epirubicin Study Group. Epirubicin-based chemotherapy in metastatic breast cancer patients: role of dose-intensity and duration of treatment. J Clin Oncol. 2000;18:3115-3124.
6. Almubarak H, Jones A, Chaisuparat R, et al. Zoledronic acid directly suppresses cell proliferation and induces apoptosis in highly tumorigenic prostate and breast cancers. J Carcinog. 2011;10:2.
7. National Comprehensive Cancer Network. Clinical practice guidelines in oncology. Breast cancer. Version 3. National Comprehensive Cancer Network Web site. Available at: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 2014.
1. McKee PH, Calonje E, Granter SR. Cutaneous metastases and Paget’s disease of the skin. In: Pathology of the skin with clinical correlations. Philadelphia, PA: Elsevier Mosby;2005:1514-1518.
2. Handley WS. Cancer of the breast and its treatment. 2nd ed. London, England: John Murray;1922:17.
3. Mahore SD, Bothale KA, Patrikar AD, et al. Carcinoma en cuirasse: a rare presentation of breast cancer. Indian J Pathol Microbiol. 2010;53:351-358.
4. Carrick S, Parker S, Wilcken N, et al. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane Database Syst Rev. 2005;CD003372.
5. French Epirubicin Study Group. Epirubicin-based chemotherapy in metastatic breast cancer patients: role of dose-intensity and duration of treatment. J Clin Oncol. 2000;18:3115-3124.
6. Almubarak H, Jones A, Chaisuparat R, et al. Zoledronic acid directly suppresses cell proliferation and induces apoptosis in highly tumorigenic prostate and breast cancers. J Carcinog. 2011;10:2.
7. National Comprehensive Cancer Network. Clinical practice guidelines in oncology. Breast cancer. Version 3. National Comprehensive Cancer Network Web site. Available at: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 2014.
