User login
Paranoid delusions • ideas of reference • sleep problems • Dx?
THE CASE
A 58-year-old married Asian woman with no apparent psychiatric history presented to the emergency department (ED) in an acute state with ideas of reference, paranoid delusions, and multiple, vague somatic symptoms.
Based on information in the patient’s medical record, there had been suspicion of an underlying psychiatric disorder 6 years earlier. At that time, the patient had presented to her primary care provider (PCP) with vague somatic complaints, including diffuse body pain, dry cough, chills, weakness, facial numbness, and concerns about infections. A physical examination and work-up did not reveal the source of her complaints. Unfortunately, the patient’s complaints increased in number and severity over time.
Her medical records also indicated that she had been assessed for depression severity using the Patient Health Questionnaire-9 (PHQ-9), with scores of 0 (4 years earlier) and 3 (3 years earlier). The scores suggested that she was not suffering from depression.
During this time, the patient also saw a psychiatrist; however, it was unclear whether her symptoms met the criteria for delusional disorder or schizophrenia because she did not exhibit negative symptoms or sensory hallucinations. In addition, the patient was extremely high-functioning in the community—she participated in dance classes and other social events—and had the equivalent of a medical degree from another country. Based on chart review, when she went to the psychiatrist 3 years prior to her current presentation, there were no antipsychotics prescribed.
In the weeks leading up to her current presentation, the patient reported that she was struggling with sleep, sometimes spending days in bed and other times needing unspecified medication obtained overseas to help her sleep. Her husband reported that she had become increasingly withdrawn and stopped attending her dance classes and social events.
The patient believed the government was trying to poison her via radiation and that unknown people were trying to harm her via an online messaging application. Immediately prior to her arrival in the ED, the police were called to pull her away from oncoming traffic because she ran into the road to find the assassins that were stalking her.
During this recent visit to the ED, the patient presented with labile affect, rapid speech, and anxious and angry mood. She complained about darkened spots on her arm (inflicted through radiation by the media), vaginal bleeding, paralysis below the waist (although she was pacing around), and unspecific pain around her belly. Physical examination revealed no obvious signs of head trauma, intact extraocular movements, no coughing or wheezing, regular heart rate and rhythm, a nontender abdomen to palpation, and normal bowel sounds. No focal neurological deficits were appreciated. She had no rashes, bruises, or skin abrasions on her abdomen or upper extremities.
Continue to: The patient tried to...
The patient tried to leave the ED, saying that her third eye could see the radiation. She required medication and 4-point restraints.
Her initial laboratory work-up for heavy metals, Lyme disease, human immunodeficiency virus (HIV), syphilis, delirium, and drug use were all negative. She also underwent head imaging studies that were also found to be negative. Her mental status exam was notable for a tangential thought process, preservation of delusions with loose associations, labile mood, and dysphoric affect. The patient demonstrated limited insight and judgment, although she was fully oriented to person, place, and time, which suggested against delirium at the time of evaluation.
THE DIAGNOSIS
Based on the patient’s current presentation and in light of her medical history, the health care team arrived at a
DISCUSSION
Schizophrenia is a severe, lifelong mental disorder characterized by at least 2 symptoms of delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, or negative symptoms for at least 6 months, with significant social, occupational, and functional deterioration. Current models attribute the neurodevelopmental deregulation of the brain in patients with schizophrenia to dopaminergic hyperactivity and hypofunction of the glutamatergic neurotransmitter system, explaining why its onset is usually in adolescence or young adulthood.1,2 However, 23% of patients present with symptoms after age 40, with 7% of patients being diagnosed between the ages of 51 and 60.3
Late-onset vs early-onset schizophrenia. LOS is often a missed diagnosis because the clinical presentation is different from early-onset schizophrenia (EOS). Although the prodromal symptoms of EOS and LOS are similar and include marked isolation that subsequently progresses to suspiciousness and ideas of reference,4 patients with EOS often also have prodromal negative symptoms. These prodromal negative symptoms associated with EOS may include loss of motivation, social passivity, and disorganized behavior. These symptoms are hypothesized to be caused by dopaminergic dysregulation in the anterior cingulate cortex. EOS is characterized by the patient experiencing more negative symptoms than LOS, which is characterized by the patient experiencing more positive symptoms.
Continue to: Patients with late-onset schizophrenia...
Patients with LOS typically do not exhibit negative symptoms because remodeling and myelination of neuronal circuitry matures by late adulthood, and thus becomes more resistant to impairment of motivational processes in the anterior cingulate gyrus.4,5,6
LOS is characterized by paranoid personality with predominantly positive symptoms, likely due to disruptions in
Other features of LOS include a high female:male ratio and symptomatic improvement with antipsychotics.7,10 Studies show that the LOS ratio of women:men can range from 2.2:1 to 22.5:1, which could be explained by the effect of dopaminergic-modulating estrogen from different sex-specific aging brain patterns.8,11,12 Finally, patients with LOS are less likely to seek care for sensory deficits than their age-equivalent counterparts.8,10 Fortunately, many of the characteristics of LOS predict good prognosis: Patients are usually female, display positive symptoms, have acute onset of symptoms, and are married with social support.10
Diagnosing LOS
LOS can be challenging to diagnose because of its atypical presentation compared with EOS, relative rarity in the population, and its propensity to be confused with progressive Alzheimer disease/dementia, delusional disorder, and major depressive disorder with psychotic features.3,6 Patients with no prior psychiatric history often do not have ready access to psychiatrists and depend on PCPs and other clinicians to identify mental health issues. A careful history, including familial involvement, utilization of the Montreal Cognitive Assessment (MoCA) test, and evaluation of environmental factors, are crucial to arriving at the proper diagnosis.
Continue to: Differential diagnosis
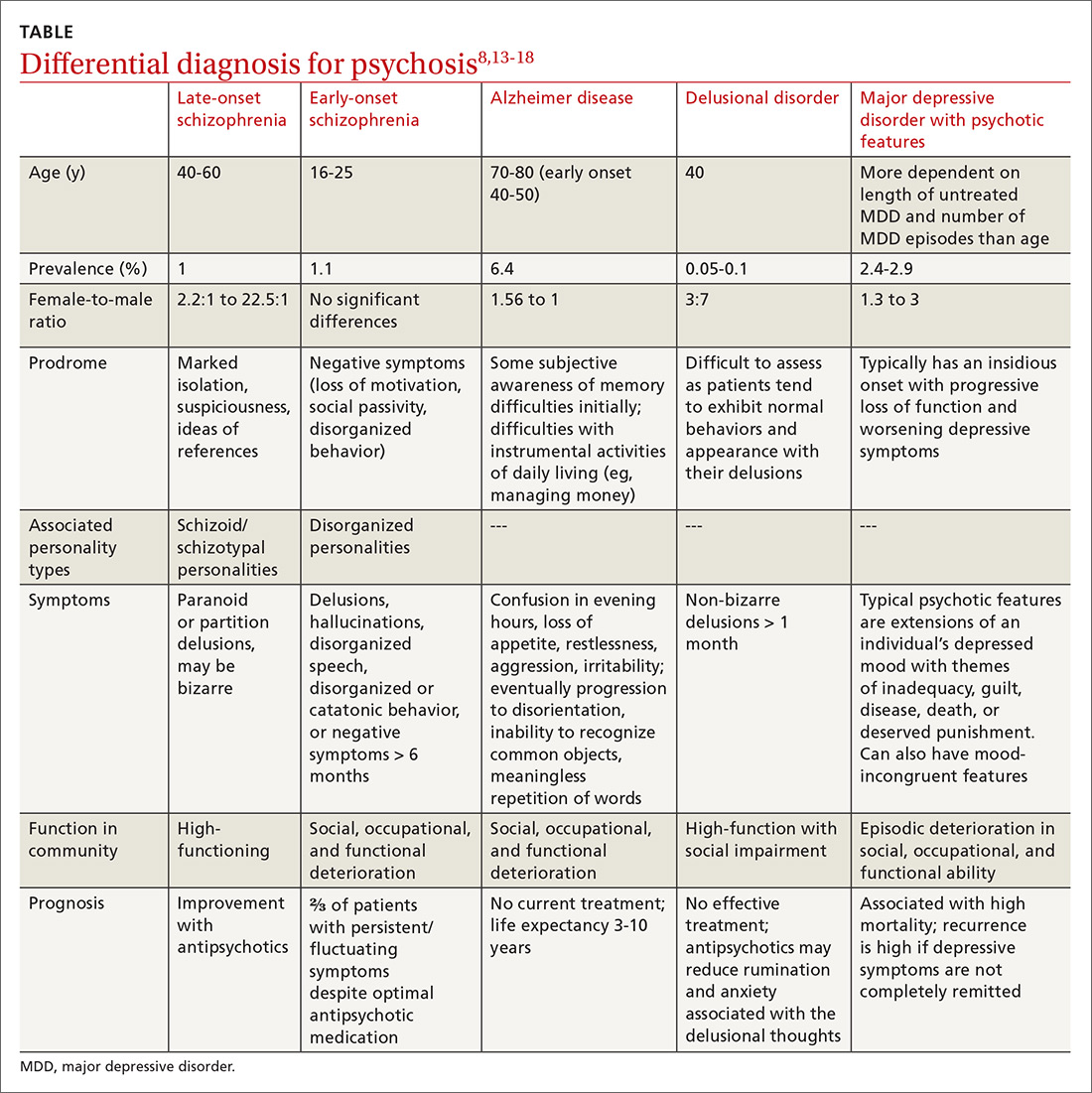
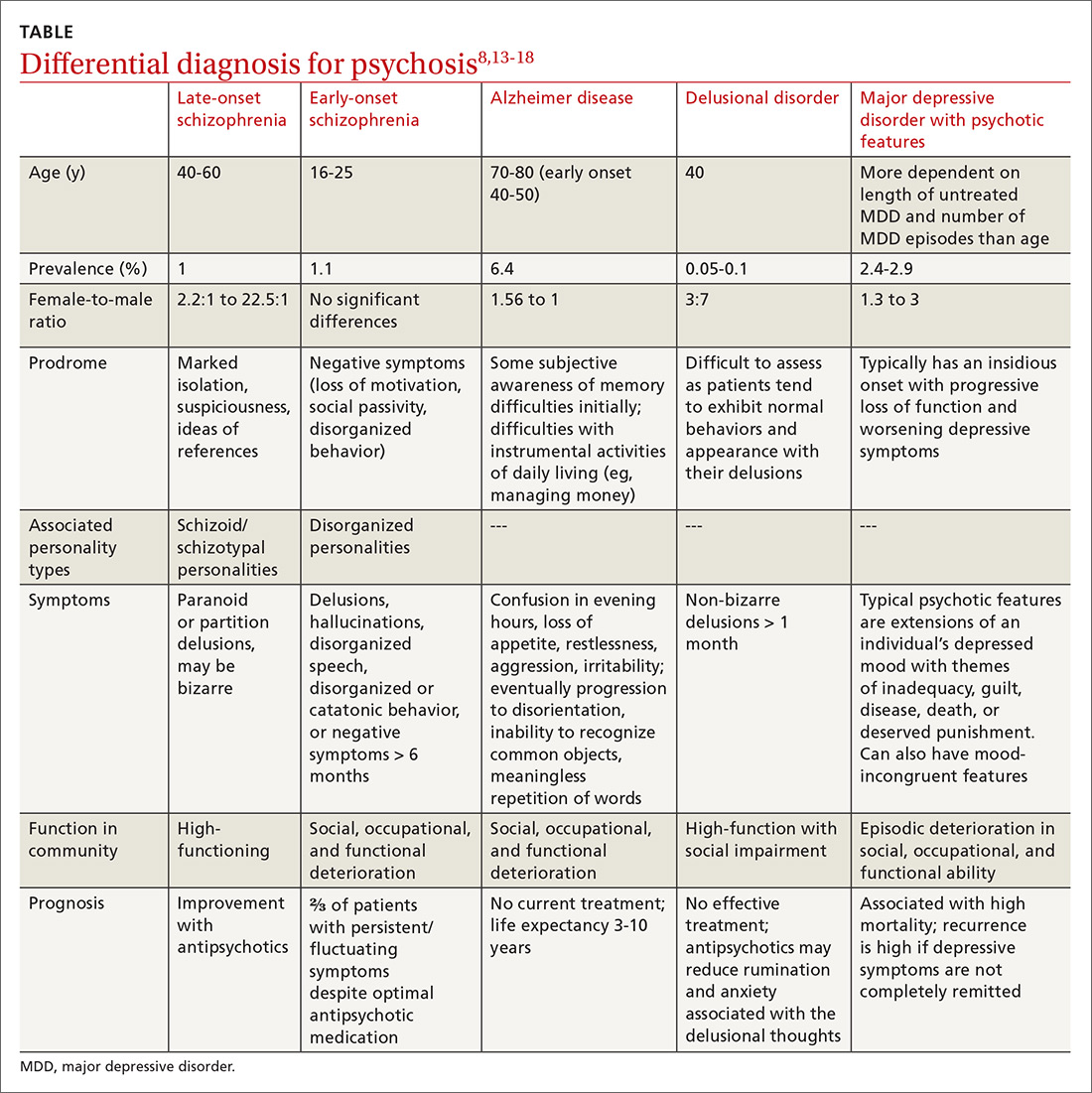
Differential diagnosis. When psychosis appears later in life, it is important to consider a broad differential (TABLE13-18), which includes the following:
Alzheimer disease. LOS can be easily differentiated from psychosis associated with Alzheimer disease or dementia through findings from neuropsychologic assessments and brain imaging. The initial first-line assessment for Alzheimer disease includes determining time course of daily living impairment and memory with follow-up brain imaging. Magnetic resonance imaging of patients with Alzheimer disease shows clear atrophy of the medial temporal lobes and general brain atrophy.19 Other than hypoperfusion in the frontal and temporal area, brain imaging of patients with LOS will not reveal any pathology.1
Delusional disorder and LOS are often more challenging to differentiate because symptoms can overlap, and many of the negative symptoms that would otherwise help clinicians diagnose schizophrenia in a younger population are absent in LOS. The milder symptoms of LOS may also lead clinicians to favor a diagnosis of delusional disorder. However, the following differences can help physicians differentiate between LOS and delusional disorder. Delusional disorder20-22:
- often will include paranoid beliefs, but these beliefs will not be bizarre, and the patient’s daily functioning will not be impaired, whereas patients with schizophrenia would have an increase in isolation and impairment in functioning that tends to be distinct from baseline.
- is more rare than schizophrenia. Delusional disorder has a prevalence of 0.05% to 0.1% compared to 1% for schizophrenia.
Major depressive disorder (MDD) with psychotic features. Major depressive disorder with psychotic features is an important differential to consider in this setting because the treatment intervention can be considerably different. Among patients who have MDD with psychotic features, a significant mood component is present, and treatment typically focuses on optimizing a selective serotonin reuptake inhibitor (SSRI); depending on severity, electroconvulsive therapy (ECT) also may be warranted.19
Continue to: For patients with LOS...
For patients with LOS, optimizing an antipsychotic medication is the typical course of treatment, and ECT would likely have less of an impact than it does with MDD with psychotic features.
Other. Finally, in an acute setting, other differential diagnoses for mental status changes (depending on clinical findings) might include:
- drug/medication use
- delirium
- nutrient deficiencies
- acute head trauma
- chronic subdural hematoma
- syphilis
- Lyme disease
- HIV encephalitis
- heavy metal toxicity.
Treatment involves antipsychotics—especially certain ones
Antipsychotic medications are utilized for the treatment of patients with LOS. A Cochrane review concluded that there are no trial-based evidence guidelines for the treatment of patients with LOS, and that physicians should continue with their current practice and use clinical judgment and prescribing patterns to guide their selection of antipsychotic medications.22,23 Pearlson et al24 found that 76% of patients with schizophrenia achieved at least partial remission and 48% achieved full remission with antipsychotic treatment.
The preferred treatment for patients with schizophrenia is low doses of newer antipsychotics (atypical or second-generation antipsychotics [SGAs]) because they are less likely to cause extrapyramidal symptoms/adverse effects than first-generation antipsychotics. Examples of SGAs include aripiprazole, risperidone, olanzapine, quetiapine, and ziprasidone.
Effective treatment for LOS includes antipsychotics at a quarter to one-half of the usual therapeutic doses. In patients with very late-onset schizophrenia, doses should be started at a tenth of therapeutic dose.1,23 Physicians should titrate up carefully, as needed.
Continue to: As with any significant mental illness...
As with any significant mental illness, to improve clinical outcomes, family support may help patients’ medication adherence and ensure they attend scheduled medical appointments.
Our patient was eventually stabilized on long-acting injectable risperidone, 25 mg, with improvement in symptoms. Unfortunately, she was not convinced that her symptoms were psychiatric in nature and did not continue with her medications as an outpatient.
The patient’s nonadherence to her medication regimen led to 2 more hospitalizations with similar presentations over the following 2 years. On her most recent discharge, she was stabilized on oral olanzapine, 10 mg every night at bedtime, with close outpatient follow-up and family education.
THE TAKEAWAY
The prodromal phase of patients with LOS is similar to patients with EOS and includes withdrawal and isolation from others, making it difficult for physicians to evaluate and treat patients. Patients with LOS predominantly experience positive symptoms that may include delusions and hallucinations. Brain imaging studies can help rule out progressive dementia diseases. A neuropsychological evaluation can assess the patient’s functional level and types of delusions, which helps to differentiate LOS from other late-age psychoses. Treatment with SGAs make for a good prognosis; however, this requires patients to be adherent to treatment.
CORRESPONDENCE
Sandy Chan, MD, Department of Internal Medicine, UMass Memorial Medical Center, 55N Lake Avenue, Worcester, MA 01605; [email protected]
1. Howard R, Rabins P, Seeman M, et al. Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international crisis. Am J Psychiatry 2000;157:172-178.
2. Pickard B. Progress in defining the biological causes of schizophrenia. Expert Rev Mol Med. 2011;13:e25.
3. Jeste D, Symonds L, Harris M, et al. Nondementia nonpraecox dementia praecox? Am J Geriatr Psychiatry. 1997;5:302-317.
4. Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase of schizophrenia. Schizophr Bull. 2002;28:415-429.
5. Dolan R, Fletcher P, Frith C, et al. Dopaminergic modulation of impaired cognitive activation in the anterior cingulate cortex in schizophrenia. Nature. 1995;378:180-182.
6. Skokou M, Katrivanou A, Andriopoulos I, et al. Active and prodromal phase symptomatology of young-onset and late-onset paranoid schizophrenia. Rev Psiquiatr Salud Ment. 2012;5:150-159.
7. Riecher-Rossler A, Loffler W, Munk-Jorgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
8. Lubman D, Castle D. Late-onset schizophrenia: make the right diagnosis when psychosis emerges after age 60. Current Psychiatry. 2002;1:35-44.
9. Howard R, Castle D, Wessely S, et al. A comparative study of 470 cases of early-onset and late-onset schizophrenia. British Journal of Psychiatry. 1993;163:352-357.
10. Harris M, Jeste D. Late-onset schizophrenia: an overview. Schizophr Bull. 1988;14:39-55.
11. Castle D, Murray R. The epidemiology of late-onset schizophrenia. Schizophr Bull. 1993;19:691-700.
12. Lindamer L, Lohr J, Harris M, Jeste D. Gender, estrogen, and schizophrenia. Psychopharmacol Bull. 1997;33:221-228.
13. Gaudiano BA, Dalrymple KL, Zimmerman M. Prevalence and clinical characteristics of psychotic versus non-psychotic major depression in a general psychiatric outpatient clinic. Depress Anxiety. 2009;26:54-64.
14. Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141.
15. Gao S, Hendrie H, Hall K. The relationships between age, sex, and the incidence of dementia and Alzheimer Disease. JAMA Psychiatry. 1998;55:809-815.
16. Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer Disease. Nature Reviews Neurology. 2011;7:137-152
17. Winokur G. Delusional Disorder (Paranoia). Comprehensive Psychiatry. 1977;18:511-521.
18. Scheltens P, Leys D, Huglo D, et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol, Neurosurg Psychiatry. 1992;55:967-972.
19. Copeland J, Dewey M, Scott A, et al. Schizophrenia and delusional disorder in older age: community prevalence, incidence, comorbidity, and outcome. Schizophr Bull. 1998;24:153-161.
20. Kendler K. Demography of paranoid psychosis (delusional disorder): a review and comparison with schizophrenia and affective illness. Arch Gen Psychiatry 1982;39:890-902.
21. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67.
22. Essali A, Ali G. Antipsychotic drug treatment for elderly people with late-onset schizophrenia. Cochrane Database Syst Rev. 2012;(2):CD004162.
23. Sweet R, Pollock B. New atypical antipsychotics- experience and utility in the elderly. Drugs Aging. 1998;12:115-127.
24. Pearlson G, Kreger L, Rabins P, et al. A chart review study of late-onset and early-onset schizophrenia. Am J Psychiatry.1989;146:1568-1574.
THE CASE
A 58-year-old married Asian woman with no apparent psychiatric history presented to the emergency department (ED) in an acute state with ideas of reference, paranoid delusions, and multiple, vague somatic symptoms.
Based on information in the patient’s medical record, there had been suspicion of an underlying psychiatric disorder 6 years earlier. At that time, the patient had presented to her primary care provider (PCP) with vague somatic complaints, including diffuse body pain, dry cough, chills, weakness, facial numbness, and concerns about infections. A physical examination and work-up did not reveal the source of her complaints. Unfortunately, the patient’s complaints increased in number and severity over time.
Her medical records also indicated that she had been assessed for depression severity using the Patient Health Questionnaire-9 (PHQ-9), with scores of 0 (4 years earlier) and 3 (3 years earlier). The scores suggested that she was not suffering from depression.
During this time, the patient also saw a psychiatrist; however, it was unclear whether her symptoms met the criteria for delusional disorder or schizophrenia because she did not exhibit negative symptoms or sensory hallucinations. In addition, the patient was extremely high-functioning in the community—she participated in dance classes and other social events—and had the equivalent of a medical degree from another country. Based on chart review, when she went to the psychiatrist 3 years prior to her current presentation, there were no antipsychotics prescribed.
In the weeks leading up to her current presentation, the patient reported that she was struggling with sleep, sometimes spending days in bed and other times needing unspecified medication obtained overseas to help her sleep. Her husband reported that she had become increasingly withdrawn and stopped attending her dance classes and social events.
The patient believed the government was trying to poison her via radiation and that unknown people were trying to harm her via an online messaging application. Immediately prior to her arrival in the ED, the police were called to pull her away from oncoming traffic because she ran into the road to find the assassins that were stalking her.
During this recent visit to the ED, the patient presented with labile affect, rapid speech, and anxious and angry mood. She complained about darkened spots on her arm (inflicted through radiation by the media), vaginal bleeding, paralysis below the waist (although she was pacing around), and unspecific pain around her belly. Physical examination revealed no obvious signs of head trauma, intact extraocular movements, no coughing or wheezing, regular heart rate and rhythm, a nontender abdomen to palpation, and normal bowel sounds. No focal neurological deficits were appreciated. She had no rashes, bruises, or skin abrasions on her abdomen or upper extremities.
Continue to: The patient tried to...
The patient tried to leave the ED, saying that her third eye could see the radiation. She required medication and 4-point restraints.
Her initial laboratory work-up for heavy metals, Lyme disease, human immunodeficiency virus (HIV), syphilis, delirium, and drug use were all negative. She also underwent head imaging studies that were also found to be negative. Her mental status exam was notable for a tangential thought process, preservation of delusions with loose associations, labile mood, and dysphoric affect. The patient demonstrated limited insight and judgment, although she was fully oriented to person, place, and time, which suggested against delirium at the time of evaluation.
THE DIAGNOSIS
Based on the patient’s current presentation and in light of her medical history, the health care team arrived at a
DISCUSSION
Schizophrenia is a severe, lifelong mental disorder characterized by at least 2 symptoms of delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, or negative symptoms for at least 6 months, with significant social, occupational, and functional deterioration. Current models attribute the neurodevelopmental deregulation of the brain in patients with schizophrenia to dopaminergic hyperactivity and hypofunction of the glutamatergic neurotransmitter system, explaining why its onset is usually in adolescence or young adulthood.1,2 However, 23% of patients present with symptoms after age 40, with 7% of patients being diagnosed between the ages of 51 and 60.3
Late-onset vs early-onset schizophrenia. LOS is often a missed diagnosis because the clinical presentation is different from early-onset schizophrenia (EOS). Although the prodromal symptoms of EOS and LOS are similar and include marked isolation that subsequently progresses to suspiciousness and ideas of reference,4 patients with EOS often also have prodromal negative symptoms. These prodromal negative symptoms associated with EOS may include loss of motivation, social passivity, and disorganized behavior. These symptoms are hypothesized to be caused by dopaminergic dysregulation in the anterior cingulate cortex. EOS is characterized by the patient experiencing more negative symptoms than LOS, which is characterized by the patient experiencing more positive symptoms.
Continue to: Patients with late-onset schizophrenia...
Patients with LOS typically do not exhibit negative symptoms because remodeling and myelination of neuronal circuitry matures by late adulthood, and thus becomes more resistant to impairment of motivational processes in the anterior cingulate gyrus.4,5,6
LOS is characterized by paranoid personality with predominantly positive symptoms, likely due to disruptions in
Other features of LOS include a high female:male ratio and symptomatic improvement with antipsychotics.7,10 Studies show that the LOS ratio of women:men can range from 2.2:1 to 22.5:1, which could be explained by the effect of dopaminergic-modulating estrogen from different sex-specific aging brain patterns.8,11,12 Finally, patients with LOS are less likely to seek care for sensory deficits than their age-equivalent counterparts.8,10 Fortunately, many of the characteristics of LOS predict good prognosis: Patients are usually female, display positive symptoms, have acute onset of symptoms, and are married with social support.10
Diagnosing LOS
LOS can be challenging to diagnose because of its atypical presentation compared with EOS, relative rarity in the population, and its propensity to be confused with progressive Alzheimer disease/dementia, delusional disorder, and major depressive disorder with psychotic features.3,6 Patients with no prior psychiatric history often do not have ready access to psychiatrists and depend on PCPs and other clinicians to identify mental health issues. A careful history, including familial involvement, utilization of the Montreal Cognitive Assessment (MoCA) test, and evaluation of environmental factors, are crucial to arriving at the proper diagnosis.
Continue to: Differential diagnosis
Differential diagnosis. When psychosis appears later in life, it is important to consider a broad differential (TABLE13-18), which includes the following:
Alzheimer disease. LOS can be easily differentiated from psychosis associated with Alzheimer disease or dementia through findings from neuropsychologic assessments and brain imaging. The initial first-line assessment for Alzheimer disease includes determining time course of daily living impairment and memory with follow-up brain imaging. Magnetic resonance imaging of patients with Alzheimer disease shows clear atrophy of the medial temporal lobes and general brain atrophy.19 Other than hypoperfusion in the frontal and temporal area, brain imaging of patients with LOS will not reveal any pathology.1
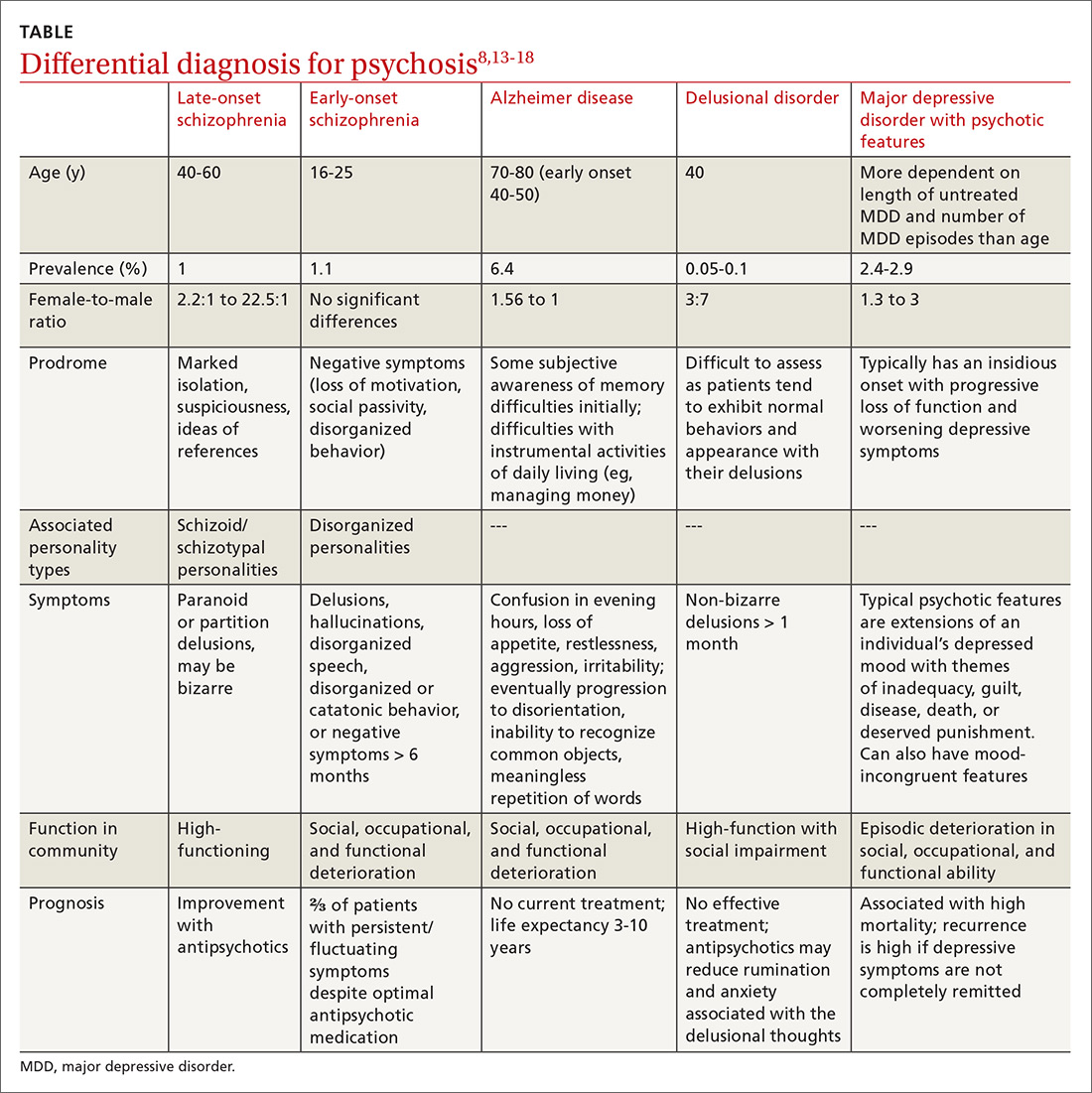
Delusional disorder and LOS are often more challenging to differentiate because symptoms can overlap, and many of the negative symptoms that would otherwise help clinicians diagnose schizophrenia in a younger population are absent in LOS. The milder symptoms of LOS may also lead clinicians to favor a diagnosis of delusional disorder. However, the following differences can help physicians differentiate between LOS and delusional disorder. Delusional disorder20-22:
- often will include paranoid beliefs, but these beliefs will not be bizarre, and the patient’s daily functioning will not be impaired, whereas patients with schizophrenia would have an increase in isolation and impairment in functioning that tends to be distinct from baseline.
- is more rare than schizophrenia. Delusional disorder has a prevalence of 0.05% to 0.1% compared to 1% for schizophrenia.
Major depressive disorder (MDD) with psychotic features. Major depressive disorder with psychotic features is an important differential to consider in this setting because the treatment intervention can be considerably different. Among patients who have MDD with psychotic features, a significant mood component is present, and treatment typically focuses on optimizing a selective serotonin reuptake inhibitor (SSRI); depending on severity, electroconvulsive therapy (ECT) also may be warranted.19
Continue to: For patients with LOS...
For patients with LOS, optimizing an antipsychotic medication is the typical course of treatment, and ECT would likely have less of an impact than it does with MDD with psychotic features.
Other. Finally, in an acute setting, other differential diagnoses for mental status changes (depending on clinical findings) might include:
- drug/medication use
- delirium
- nutrient deficiencies
- acute head trauma
- chronic subdural hematoma
- syphilis
- Lyme disease
- HIV encephalitis
- heavy metal toxicity.
Treatment involves antipsychotics—especially certain ones
Antipsychotic medications are utilized for the treatment of patients with LOS. A Cochrane review concluded that there are no trial-based evidence guidelines for the treatment of patients with LOS, and that physicians should continue with their current practice and use clinical judgment and prescribing patterns to guide their selection of antipsychotic medications.22,23 Pearlson et al24 found that 76% of patients with schizophrenia achieved at least partial remission and 48% achieved full remission with antipsychotic treatment.
The preferred treatment for patients with schizophrenia is low doses of newer antipsychotics (atypical or second-generation antipsychotics [SGAs]) because they are less likely to cause extrapyramidal symptoms/adverse effects than first-generation antipsychotics. Examples of SGAs include aripiprazole, risperidone, olanzapine, quetiapine, and ziprasidone.
Effective treatment for LOS includes antipsychotics at a quarter to one-half of the usual therapeutic doses. In patients with very late-onset schizophrenia, doses should be started at a tenth of therapeutic dose.1,23 Physicians should titrate up carefully, as needed.
Continue to: As with any significant mental illness...
As with any significant mental illness, to improve clinical outcomes, family support may help patients’ medication adherence and ensure they attend scheduled medical appointments.
Our patient was eventually stabilized on long-acting injectable risperidone, 25 mg, with improvement in symptoms. Unfortunately, she was not convinced that her symptoms were psychiatric in nature and did not continue with her medications as an outpatient.
The patient’s nonadherence to her medication regimen led to 2 more hospitalizations with similar presentations over the following 2 years. On her most recent discharge, she was stabilized on oral olanzapine, 10 mg every night at bedtime, with close outpatient follow-up and family education.
THE TAKEAWAY
The prodromal phase of patients with LOS is similar to patients with EOS and includes withdrawal and isolation from others, making it difficult for physicians to evaluate and treat patients. Patients with LOS predominantly experience positive symptoms that may include delusions and hallucinations. Brain imaging studies can help rule out progressive dementia diseases. A neuropsychological evaluation can assess the patient’s functional level and types of delusions, which helps to differentiate LOS from other late-age psychoses. Treatment with SGAs make for a good prognosis; however, this requires patients to be adherent to treatment.
CORRESPONDENCE
Sandy Chan, MD, Department of Internal Medicine, UMass Memorial Medical Center, 55N Lake Avenue, Worcester, MA 01605; [email protected]
THE CASE
A 58-year-old married Asian woman with no apparent psychiatric history presented to the emergency department (ED) in an acute state with ideas of reference, paranoid delusions, and multiple, vague somatic symptoms.
Based on information in the patient’s medical record, there had been suspicion of an underlying psychiatric disorder 6 years earlier. At that time, the patient had presented to her primary care provider (PCP) with vague somatic complaints, including diffuse body pain, dry cough, chills, weakness, facial numbness, and concerns about infections. A physical examination and work-up did not reveal the source of her complaints. Unfortunately, the patient’s complaints increased in number and severity over time.
Her medical records also indicated that she had been assessed for depression severity using the Patient Health Questionnaire-9 (PHQ-9), with scores of 0 (4 years earlier) and 3 (3 years earlier). The scores suggested that she was not suffering from depression.
During this time, the patient also saw a psychiatrist; however, it was unclear whether her symptoms met the criteria for delusional disorder or schizophrenia because she did not exhibit negative symptoms or sensory hallucinations. In addition, the patient was extremely high-functioning in the community—she participated in dance classes and other social events—and had the equivalent of a medical degree from another country. Based on chart review, when she went to the psychiatrist 3 years prior to her current presentation, there were no antipsychotics prescribed.
In the weeks leading up to her current presentation, the patient reported that she was struggling with sleep, sometimes spending days in bed and other times needing unspecified medication obtained overseas to help her sleep. Her husband reported that she had become increasingly withdrawn and stopped attending her dance classes and social events.
The patient believed the government was trying to poison her via radiation and that unknown people were trying to harm her via an online messaging application. Immediately prior to her arrival in the ED, the police were called to pull her away from oncoming traffic because she ran into the road to find the assassins that were stalking her.
During this recent visit to the ED, the patient presented with labile affect, rapid speech, and anxious and angry mood. She complained about darkened spots on her arm (inflicted through radiation by the media), vaginal bleeding, paralysis below the waist (although she was pacing around), and unspecific pain around her belly. Physical examination revealed no obvious signs of head trauma, intact extraocular movements, no coughing or wheezing, regular heart rate and rhythm, a nontender abdomen to palpation, and normal bowel sounds. No focal neurological deficits were appreciated. She had no rashes, bruises, or skin abrasions on her abdomen or upper extremities.
Continue to: The patient tried to...
The patient tried to leave the ED, saying that her third eye could see the radiation. She required medication and 4-point restraints.
Her initial laboratory work-up for heavy metals, Lyme disease, human immunodeficiency virus (HIV), syphilis, delirium, and drug use were all negative. She also underwent head imaging studies that were also found to be negative. Her mental status exam was notable for a tangential thought process, preservation of delusions with loose associations, labile mood, and dysphoric affect. The patient demonstrated limited insight and judgment, although she was fully oriented to person, place, and time, which suggested against delirium at the time of evaluation.
THE DIAGNOSIS
Based on the patient’s current presentation and in light of her medical history, the health care team arrived at a
DISCUSSION
Schizophrenia is a severe, lifelong mental disorder characterized by at least 2 symptoms of delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, or negative symptoms for at least 6 months, with significant social, occupational, and functional deterioration. Current models attribute the neurodevelopmental deregulation of the brain in patients with schizophrenia to dopaminergic hyperactivity and hypofunction of the glutamatergic neurotransmitter system, explaining why its onset is usually in adolescence or young adulthood.1,2 However, 23% of patients present with symptoms after age 40, with 7% of patients being diagnosed between the ages of 51 and 60.3
Late-onset vs early-onset schizophrenia. LOS is often a missed diagnosis because the clinical presentation is different from early-onset schizophrenia (EOS). Although the prodromal symptoms of EOS and LOS are similar and include marked isolation that subsequently progresses to suspiciousness and ideas of reference,4 patients with EOS often also have prodromal negative symptoms. These prodromal negative symptoms associated with EOS may include loss of motivation, social passivity, and disorganized behavior. These symptoms are hypothesized to be caused by dopaminergic dysregulation in the anterior cingulate cortex. EOS is characterized by the patient experiencing more negative symptoms than LOS, which is characterized by the patient experiencing more positive symptoms.
Continue to: Patients with late-onset schizophrenia...
Patients with LOS typically do not exhibit negative symptoms because remodeling and myelination of neuronal circuitry matures by late adulthood, and thus becomes more resistant to impairment of motivational processes in the anterior cingulate gyrus.4,5,6
LOS is characterized by paranoid personality with predominantly positive symptoms, likely due to disruptions in
Other features of LOS include a high female:male ratio and symptomatic improvement with antipsychotics.7,10 Studies show that the LOS ratio of women:men can range from 2.2:1 to 22.5:1, which could be explained by the effect of dopaminergic-modulating estrogen from different sex-specific aging brain patterns.8,11,12 Finally, patients with LOS are less likely to seek care for sensory deficits than their age-equivalent counterparts.8,10 Fortunately, many of the characteristics of LOS predict good prognosis: Patients are usually female, display positive symptoms, have acute onset of symptoms, and are married with social support.10
Diagnosing LOS
LOS can be challenging to diagnose because of its atypical presentation compared with EOS, relative rarity in the population, and its propensity to be confused with progressive Alzheimer disease/dementia, delusional disorder, and major depressive disorder with psychotic features.3,6 Patients with no prior psychiatric history often do not have ready access to psychiatrists and depend on PCPs and other clinicians to identify mental health issues. A careful history, including familial involvement, utilization of the Montreal Cognitive Assessment (MoCA) test, and evaluation of environmental factors, are crucial to arriving at the proper diagnosis.
Continue to: Differential diagnosis
Differential diagnosis. When psychosis appears later in life, it is important to consider a broad differential (TABLE13-18), which includes the following:
Alzheimer disease. LOS can be easily differentiated from psychosis associated with Alzheimer disease or dementia through findings from neuropsychologic assessments and brain imaging. The initial first-line assessment for Alzheimer disease includes determining time course of daily living impairment and memory with follow-up brain imaging. Magnetic resonance imaging of patients with Alzheimer disease shows clear atrophy of the medial temporal lobes and general brain atrophy.19 Other than hypoperfusion in the frontal and temporal area, brain imaging of patients with LOS will not reveal any pathology.1
Delusional disorder and LOS are often more challenging to differentiate because symptoms can overlap, and many of the negative symptoms that would otherwise help clinicians diagnose schizophrenia in a younger population are absent in LOS. The milder symptoms of LOS may also lead clinicians to favor a diagnosis of delusional disorder. However, the following differences can help physicians differentiate between LOS and delusional disorder. Delusional disorder20-22:
- often will include paranoid beliefs, but these beliefs will not be bizarre, and the patient’s daily functioning will not be impaired, whereas patients with schizophrenia would have an increase in isolation and impairment in functioning that tends to be distinct from baseline.
- is more rare than schizophrenia. Delusional disorder has a prevalence of 0.05% to 0.1% compared to 1% for schizophrenia.
Major depressive disorder (MDD) with psychotic features. Major depressive disorder with psychotic features is an important differential to consider in this setting because the treatment intervention can be considerably different. Among patients who have MDD with psychotic features, a significant mood component is present, and treatment typically focuses on optimizing a selective serotonin reuptake inhibitor (SSRI); depending on severity, electroconvulsive therapy (ECT) also may be warranted.19
Continue to: For patients with LOS...
For patients with LOS, optimizing an antipsychotic medication is the typical course of treatment, and ECT would likely have less of an impact than it does with MDD with psychotic features.
Other. Finally, in an acute setting, other differential diagnoses for mental status changes (depending on clinical findings) might include:
- drug/medication use
- delirium
- nutrient deficiencies
- acute head trauma
- chronic subdural hematoma
- syphilis
- Lyme disease
- HIV encephalitis
- heavy metal toxicity.
Treatment involves antipsychotics—especially certain ones
Antipsychotic medications are utilized for the treatment of patients with LOS. A Cochrane review concluded that there are no trial-based evidence guidelines for the treatment of patients with LOS, and that physicians should continue with their current practice and use clinical judgment and prescribing patterns to guide their selection of antipsychotic medications.22,23 Pearlson et al24 found that 76% of patients with schizophrenia achieved at least partial remission and 48% achieved full remission with antipsychotic treatment.
The preferred treatment for patients with schizophrenia is low doses of newer antipsychotics (atypical or second-generation antipsychotics [SGAs]) because they are less likely to cause extrapyramidal symptoms/adverse effects than first-generation antipsychotics. Examples of SGAs include aripiprazole, risperidone, olanzapine, quetiapine, and ziprasidone.
Effective treatment for LOS includes antipsychotics at a quarter to one-half of the usual therapeutic doses. In patients with very late-onset schizophrenia, doses should be started at a tenth of therapeutic dose.1,23 Physicians should titrate up carefully, as needed.
Continue to: As with any significant mental illness...
As with any significant mental illness, to improve clinical outcomes, family support may help patients’ medication adherence and ensure they attend scheduled medical appointments.
Our patient was eventually stabilized on long-acting injectable risperidone, 25 mg, with improvement in symptoms. Unfortunately, she was not convinced that her symptoms were psychiatric in nature and did not continue with her medications as an outpatient.
The patient’s nonadherence to her medication regimen led to 2 more hospitalizations with similar presentations over the following 2 years. On her most recent discharge, she was stabilized on oral olanzapine, 10 mg every night at bedtime, with close outpatient follow-up and family education.
THE TAKEAWAY
The prodromal phase of patients with LOS is similar to patients with EOS and includes withdrawal and isolation from others, making it difficult for physicians to evaluate and treat patients. Patients with LOS predominantly experience positive symptoms that may include delusions and hallucinations. Brain imaging studies can help rule out progressive dementia diseases. A neuropsychological evaluation can assess the patient’s functional level and types of delusions, which helps to differentiate LOS from other late-age psychoses. Treatment with SGAs make for a good prognosis; however, this requires patients to be adherent to treatment.
CORRESPONDENCE
Sandy Chan, MD, Department of Internal Medicine, UMass Memorial Medical Center, 55N Lake Avenue, Worcester, MA 01605; [email protected]
1. Howard R, Rabins P, Seeman M, et al. Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international crisis. Am J Psychiatry 2000;157:172-178.
2. Pickard B. Progress in defining the biological causes of schizophrenia. Expert Rev Mol Med. 2011;13:e25.
3. Jeste D, Symonds L, Harris M, et al. Nondementia nonpraecox dementia praecox? Am J Geriatr Psychiatry. 1997;5:302-317.
4. Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase of schizophrenia. Schizophr Bull. 2002;28:415-429.
5. Dolan R, Fletcher P, Frith C, et al. Dopaminergic modulation of impaired cognitive activation in the anterior cingulate cortex in schizophrenia. Nature. 1995;378:180-182.
6. Skokou M, Katrivanou A, Andriopoulos I, et al. Active and prodromal phase symptomatology of young-onset and late-onset paranoid schizophrenia. Rev Psiquiatr Salud Ment. 2012;5:150-159.
7. Riecher-Rossler A, Loffler W, Munk-Jorgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
8. Lubman D, Castle D. Late-onset schizophrenia: make the right diagnosis when psychosis emerges after age 60. Current Psychiatry. 2002;1:35-44.
9. Howard R, Castle D, Wessely S, et al. A comparative study of 470 cases of early-onset and late-onset schizophrenia. British Journal of Psychiatry. 1993;163:352-357.
10. Harris M, Jeste D. Late-onset schizophrenia: an overview. Schizophr Bull. 1988;14:39-55.
11. Castle D, Murray R. The epidemiology of late-onset schizophrenia. Schizophr Bull. 1993;19:691-700.
12. Lindamer L, Lohr J, Harris M, Jeste D. Gender, estrogen, and schizophrenia. Psychopharmacol Bull. 1997;33:221-228.
13. Gaudiano BA, Dalrymple KL, Zimmerman M. Prevalence and clinical characteristics of psychotic versus non-psychotic major depression in a general psychiatric outpatient clinic. Depress Anxiety. 2009;26:54-64.
14. Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141.
15. Gao S, Hendrie H, Hall K. The relationships between age, sex, and the incidence of dementia and Alzheimer Disease. JAMA Psychiatry. 1998;55:809-815.
16. Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer Disease. Nature Reviews Neurology. 2011;7:137-152
17. Winokur G. Delusional Disorder (Paranoia). Comprehensive Psychiatry. 1977;18:511-521.
18. Scheltens P, Leys D, Huglo D, et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol, Neurosurg Psychiatry. 1992;55:967-972.
19. Copeland J, Dewey M, Scott A, et al. Schizophrenia and delusional disorder in older age: community prevalence, incidence, comorbidity, and outcome. Schizophr Bull. 1998;24:153-161.
20. Kendler K. Demography of paranoid psychosis (delusional disorder): a review and comparison with schizophrenia and affective illness. Arch Gen Psychiatry 1982;39:890-902.
21. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67.
22. Essali A, Ali G. Antipsychotic drug treatment for elderly people with late-onset schizophrenia. Cochrane Database Syst Rev. 2012;(2):CD004162.
23. Sweet R, Pollock B. New atypical antipsychotics- experience and utility in the elderly. Drugs Aging. 1998;12:115-127.
24. Pearlson G, Kreger L, Rabins P, et al. A chart review study of late-onset and early-onset schizophrenia. Am J Psychiatry.1989;146:1568-1574.
1. Howard R, Rabins P, Seeman M, et al. Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international crisis. Am J Psychiatry 2000;157:172-178.
2. Pickard B. Progress in defining the biological causes of schizophrenia. Expert Rev Mol Med. 2011;13:e25.
3. Jeste D, Symonds L, Harris M, et al. Nondementia nonpraecox dementia praecox? Am J Geriatr Psychiatry. 1997;5:302-317.
4. Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase of schizophrenia. Schizophr Bull. 2002;28:415-429.
5. Dolan R, Fletcher P, Frith C, et al. Dopaminergic modulation of impaired cognitive activation in the anterior cingulate cortex in schizophrenia. Nature. 1995;378:180-182.
6. Skokou M, Katrivanou A, Andriopoulos I, et al. Active and prodromal phase symptomatology of young-onset and late-onset paranoid schizophrenia. Rev Psiquiatr Salud Ment. 2012;5:150-159.
7. Riecher-Rossler A, Loffler W, Munk-Jorgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
8. Lubman D, Castle D. Late-onset schizophrenia: make the right diagnosis when psychosis emerges after age 60. Current Psychiatry. 2002;1:35-44.
9. Howard R, Castle D, Wessely S, et al. A comparative study of 470 cases of early-onset and late-onset schizophrenia. British Journal of Psychiatry. 1993;163:352-357.
10. Harris M, Jeste D. Late-onset schizophrenia: an overview. Schizophr Bull. 1988;14:39-55.
11. Castle D, Murray R. The epidemiology of late-onset schizophrenia. Schizophr Bull. 1993;19:691-700.
12. Lindamer L, Lohr J, Harris M, Jeste D. Gender, estrogen, and schizophrenia. Psychopharmacol Bull. 1997;33:221-228.
13. Gaudiano BA, Dalrymple KL, Zimmerman M. Prevalence and clinical characteristics of psychotic versus non-psychotic major depression in a general psychiatric outpatient clinic. Depress Anxiety. 2009;26:54-64.
14. Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141.
15. Gao S, Hendrie H, Hall K. The relationships between age, sex, and the incidence of dementia and Alzheimer Disease. JAMA Psychiatry. 1998;55:809-815.
16. Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer Disease. Nature Reviews Neurology. 2011;7:137-152
17. Winokur G. Delusional Disorder (Paranoia). Comprehensive Psychiatry. 1977;18:511-521.
18. Scheltens P, Leys D, Huglo D, et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol, Neurosurg Psychiatry. 1992;55:967-972.
19. Copeland J, Dewey M, Scott A, et al. Schizophrenia and delusional disorder in older age: community prevalence, incidence, comorbidity, and outcome. Schizophr Bull. 1998;24:153-161.
20. Kendler K. Demography of paranoid psychosis (delusional disorder): a review and comparison with schizophrenia and affective illness. Arch Gen Psychiatry 1982;39:890-902.
21. McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67.
22. Essali A, Ali G. Antipsychotic drug treatment for elderly people with late-onset schizophrenia. Cochrane Database Syst Rev. 2012;(2):CD004162.
23. Sweet R, Pollock B. New atypical antipsychotics- experience and utility in the elderly. Drugs Aging. 1998;12:115-127.
24. Pearlson G, Kreger L, Rabins P, et al. A chart review study of late-onset and early-onset schizophrenia. Am J Psychiatry.1989;146:1568-1574.
