User login
Double Sequential Defibrillation for Refractory Ventricular Fibrillation and Pulseless Ventricular Tachycardia
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
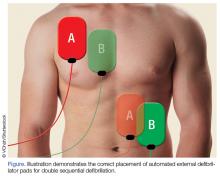
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.