User login
Richard Quinn is an award-winning journalist with 15 years’ experience. He has worked at the Asbury Park Press in New Jersey and The Virginian-Pilot in Norfolk, Va., and currently is managing editor for a leading commercial real estate publication. His freelance work has appeared in The Jewish State, The Hospitalist, The Rheumatologist, ACEP Now, and ENT Today. He lives in New Jersey with his wife and three cats.
Listen Now! American Enterprise Institute's Scott Gottlieb, MD, Talks About the Impact the Affordable Care Act Will Have on Hospitalists
Frustrated with Existing Systems, Hospitalists Collaborate to Improve Health Information Technology
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
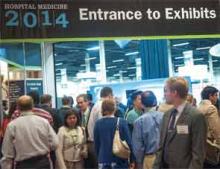
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
Research, Innovation, Clinical Vignette Poster Winners Recognized at HM14
Enter text here
Enter text here
Enter text here
Hospitalists Share Patient Care Tips, Strategies at HM14 Annual RIV Competition
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
Quality Improvement, Patient Safety Top Hospitalists’ Priority Lists at HM14
LAS VEGAS—Hospitalist Ijeoma “Carol” Nwelue, MD, has been more focused on patient readmissions over the past year at her practice in Lansing, Mich. So when the directors at Sparrow Hospitalists told her she had a meeting a few weeks after HM14 to discuss different risk assessment tools that might be used to pre-identify patients at high risk for readmission, she wasn’t nervous.
Instead, she prepped at SHM’s annual meeting at Mandalay Bay Resort and Casino—a veritable three-day crash course in the latest and greatest approaches to preventing readmissions.
“It’s very helpful,” she says. “It helps to see things that I haven’t thought about in our practice that other people are looking into.”
Quality improvement (QI) and patient safety are at the core of what hospitalists do, and the HM14 organizers understand that. From multiple pre-courses on the topics trending today to a dedicated educational track of breakout sessions and expert speakers to hundreds of posters identifying HM-specific QI projects, SHM’s annual meeting is a veritable QI opportunity of its own.
Take the annual pre-course, “ABIM Maintenance of Certification Facilitated Modules.” One attendee told presenter Read Pierce, MD, director of quality improvement and clinical innovation for the hospitalist group at the University of Colorado Denver, that before the session in Las Vegas he had always had “the sense that quality and safety is soft science or fuzzy stuff around the edges, and if you were a smart clinician, that was good enough.”
After some time in the session, Dr. Pierce recounts, the man “realized it’s not just enough to have great intellectual horsepower. You have to have some approach for dealing with these complex systems. And I think that’s the really fun thing....It’s not just about the discreet concepts; it’s about understanding the environment in which we practice, the importance of engaging systems and of using the tools of quality and safety to augment what physicians have always been good at doing.”
John Coppes, MD, FHM, a hospitalist at Mount Nittany Medical Center in State College, Pa., says quality and patient safety are the “most important things that we do.”
“It’s our responsibility to our patients to do the best job we can,” he notes. “It’s our responsibility to society to do it as efficiently as we can.”
Veteran meeting faculty John Bulger, DO, MBA, FACP, SFHM, hospitalist and chief quality officer at Geisinger Health System in Pennsylvania, agrees completely and is one of HM’s biggest proponents of the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely (www.hospitalmedicine.org/choosingwisely) campaign. The national initiative, aimed at educating physicians—and patients—about wasteful medical tests, procedures, and treatments, launched in 2012, but SHM joined the chorus as a strategic partner last year.
“Choosing Wisely is about bending the cost curve,” Dr. Bulger says.
He added that although standardization of care is necessary for Choosing Wisely to work, homogeneity doesn’t mean everybody does everything exactly the same way. It means ensuring that hospitalists adopt “agreed upon best practices” before local variations are added. He compared it to a cookbook of apple pie recipes. All apple pies contain apples and crust, but the tasty treats are tailored differently from there.
“When you come up with guidelines in your hospital, that’s what you’re doing,” Dr. Bulger says. “You’re writing the cookbook and coming up with what works at your hospital. It might not work at [my hospital] at all, but I can look at it and learn.”
In the long-term, SHM hopes to create resources beyond the recommendations themselves—perhaps including a mentored implementation program akin to Project BOOST or pre-packaged order sets and checklists. Whatever the society does, it needs to engage the younger generation of physicians to ensure that quality and safety stay a priority for them, says Darlene Tad-y, MD, chair of SHM’s Physicians in Training Committee.
An assistant professor of medicine and a hospitalist at the University of Colorado Denver, Dr. Tad-y says that getting residents and students involved in quality and safety measures is critical for HM’s future.
“Especially since we want to have hospital medicine be at the forefront,” she explains. “It’s vital for us to have our students and residents taking the lead.”
Younger physicians already see the role quality and safety take in day-to-day practice. So, for them, according to Dr. Tad-y, a focus on making sure patient care is delivered better and more safely isn’t a renewed effort—it’s what they’re taught from the beginning.
“They haven’t been trained in the old way yet,” she says. “They still have an open mind. They see that things can change and things can be better. We don’t have to change old habits. We are just evolving good new habits for them.”
One new perspective was a first-time pre-course, “Cardiology: What Hospitalists Need to Know as Front-Line Providers.” The eight-hour seminar was led by cardiologist Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, who says the time is right for quality-focused hospitalists to devote a full-day pre-course to cardiology.
“Cardiovascular disease is the most common reason we die,” he says. “It’s something hospital-based practitioners see often. Providing a comprehensive, yet simplified, overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The sheer scale of QI initiatives can be daunting, says Michelle Mourad, MD, director of quality and safety at the University of California at San Francisco (UCSF) School of Medicine. She urges her peers to take the proverbial step back, identify a single issue—sepsis mortality or hand hygiene, for example—and then focus on understanding that issue intimately. That way, a hospitalist or HM group can convince other physicians that there is a problem and that it’s worth the work to fix it. Once that’s done, a hospitalist can launch a QI project that devises a measurement strategy to see if change is occurring.
And, while sustaining that change beyond the initial start-up can be difficult, Dr. Mourad believes success breeds success.
“When you work hard at a quality gap that’s in your organization, [when you] actually see the care you provide get better—not just for the patient in front of you, but for all the patients in your organization—it’s extremely powerful and motivating,” she says. “It changes the culture in your institution and convinces other people that they can do the same.”
LAS VEGAS—Hospitalist Ijeoma “Carol” Nwelue, MD, has been more focused on patient readmissions over the past year at her practice in Lansing, Mich. So when the directors at Sparrow Hospitalists told her she had a meeting a few weeks after HM14 to discuss different risk assessment tools that might be used to pre-identify patients at high risk for readmission, she wasn’t nervous.
Instead, she prepped at SHM’s annual meeting at Mandalay Bay Resort and Casino—a veritable three-day crash course in the latest and greatest approaches to preventing readmissions.
“It’s very helpful,” she says. “It helps to see things that I haven’t thought about in our practice that other people are looking into.”
Quality improvement (QI) and patient safety are at the core of what hospitalists do, and the HM14 organizers understand that. From multiple pre-courses on the topics trending today to a dedicated educational track of breakout sessions and expert speakers to hundreds of posters identifying HM-specific QI projects, SHM’s annual meeting is a veritable QI opportunity of its own.
Take the annual pre-course, “ABIM Maintenance of Certification Facilitated Modules.” One attendee told presenter Read Pierce, MD, director of quality improvement and clinical innovation for the hospitalist group at the University of Colorado Denver, that before the session in Las Vegas he had always had “the sense that quality and safety is soft science or fuzzy stuff around the edges, and if you were a smart clinician, that was good enough.”
After some time in the session, Dr. Pierce recounts, the man “realized it’s not just enough to have great intellectual horsepower. You have to have some approach for dealing with these complex systems. And I think that’s the really fun thing....It’s not just about the discreet concepts; it’s about understanding the environment in which we practice, the importance of engaging systems and of using the tools of quality and safety to augment what physicians have always been good at doing.”
John Coppes, MD, FHM, a hospitalist at Mount Nittany Medical Center in State College, Pa., says quality and patient safety are the “most important things that we do.”
“It’s our responsibility to our patients to do the best job we can,” he notes. “It’s our responsibility to society to do it as efficiently as we can.”
Veteran meeting faculty John Bulger, DO, MBA, FACP, SFHM, hospitalist and chief quality officer at Geisinger Health System in Pennsylvania, agrees completely and is one of HM’s biggest proponents of the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely (www.hospitalmedicine.org/choosingwisely) campaign. The national initiative, aimed at educating physicians—and patients—about wasteful medical tests, procedures, and treatments, launched in 2012, but SHM joined the chorus as a strategic partner last year.
“Choosing Wisely is about bending the cost curve,” Dr. Bulger says.
He added that although standardization of care is necessary for Choosing Wisely to work, homogeneity doesn’t mean everybody does everything exactly the same way. It means ensuring that hospitalists adopt “agreed upon best practices” before local variations are added. He compared it to a cookbook of apple pie recipes. All apple pies contain apples and crust, but the tasty treats are tailored differently from there.
“When you come up with guidelines in your hospital, that’s what you’re doing,” Dr. Bulger says. “You’re writing the cookbook and coming up with what works at your hospital. It might not work at [my hospital] at all, but I can look at it and learn.”
In the long-term, SHM hopes to create resources beyond the recommendations themselves—perhaps including a mentored implementation program akin to Project BOOST or pre-packaged order sets and checklists. Whatever the society does, it needs to engage the younger generation of physicians to ensure that quality and safety stay a priority for them, says Darlene Tad-y, MD, chair of SHM’s Physicians in Training Committee.
An assistant professor of medicine and a hospitalist at the University of Colorado Denver, Dr. Tad-y says that getting residents and students involved in quality and safety measures is critical for HM’s future.
“Especially since we want to have hospital medicine be at the forefront,” she explains. “It’s vital for us to have our students and residents taking the lead.”
Younger physicians already see the role quality and safety take in day-to-day practice. So, for them, according to Dr. Tad-y, a focus on making sure patient care is delivered better and more safely isn’t a renewed effort—it’s what they’re taught from the beginning.
“They haven’t been trained in the old way yet,” she says. “They still have an open mind. They see that things can change and things can be better. We don’t have to change old habits. We are just evolving good new habits for them.”
One new perspective was a first-time pre-course, “Cardiology: What Hospitalists Need to Know as Front-Line Providers.” The eight-hour seminar was led by cardiologist Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, who says the time is right for quality-focused hospitalists to devote a full-day pre-course to cardiology.
“Cardiovascular disease is the most common reason we die,” he says. “It’s something hospital-based practitioners see often. Providing a comprehensive, yet simplified, overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The sheer scale of QI initiatives can be daunting, says Michelle Mourad, MD, director of quality and safety at the University of California at San Francisco (UCSF) School of Medicine. She urges her peers to take the proverbial step back, identify a single issue—sepsis mortality or hand hygiene, for example—and then focus on understanding that issue intimately. That way, a hospitalist or HM group can convince other physicians that there is a problem and that it’s worth the work to fix it. Once that’s done, a hospitalist can launch a QI project that devises a measurement strategy to see if change is occurring.
And, while sustaining that change beyond the initial start-up can be difficult, Dr. Mourad believes success breeds success.
“When you work hard at a quality gap that’s in your organization, [when you] actually see the care you provide get better—not just for the patient in front of you, but for all the patients in your organization—it’s extremely powerful and motivating,” she says. “It changes the culture in your institution and convinces other people that they can do the same.”
LAS VEGAS—Hospitalist Ijeoma “Carol” Nwelue, MD, has been more focused on patient readmissions over the past year at her practice in Lansing, Mich. So when the directors at Sparrow Hospitalists told her she had a meeting a few weeks after HM14 to discuss different risk assessment tools that might be used to pre-identify patients at high risk for readmission, she wasn’t nervous.
Instead, she prepped at SHM’s annual meeting at Mandalay Bay Resort and Casino—a veritable three-day crash course in the latest and greatest approaches to preventing readmissions.
“It’s very helpful,” she says. “It helps to see things that I haven’t thought about in our practice that other people are looking into.”
Quality improvement (QI) and patient safety are at the core of what hospitalists do, and the HM14 organizers understand that. From multiple pre-courses on the topics trending today to a dedicated educational track of breakout sessions and expert speakers to hundreds of posters identifying HM-specific QI projects, SHM’s annual meeting is a veritable QI opportunity of its own.
Take the annual pre-course, “ABIM Maintenance of Certification Facilitated Modules.” One attendee told presenter Read Pierce, MD, director of quality improvement and clinical innovation for the hospitalist group at the University of Colorado Denver, that before the session in Las Vegas he had always had “the sense that quality and safety is soft science or fuzzy stuff around the edges, and if you were a smart clinician, that was good enough.”
After some time in the session, Dr. Pierce recounts, the man “realized it’s not just enough to have great intellectual horsepower. You have to have some approach for dealing with these complex systems. And I think that’s the really fun thing....It’s not just about the discreet concepts; it’s about understanding the environment in which we practice, the importance of engaging systems and of using the tools of quality and safety to augment what physicians have always been good at doing.”
John Coppes, MD, FHM, a hospitalist at Mount Nittany Medical Center in State College, Pa., says quality and patient safety are the “most important things that we do.”
“It’s our responsibility to our patients to do the best job we can,” he notes. “It’s our responsibility to society to do it as efficiently as we can.”
Veteran meeting faculty John Bulger, DO, MBA, FACP, SFHM, hospitalist and chief quality officer at Geisinger Health System in Pennsylvania, agrees completely and is one of HM’s biggest proponents of the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely (www.hospitalmedicine.org/choosingwisely) campaign. The national initiative, aimed at educating physicians—and patients—about wasteful medical tests, procedures, and treatments, launched in 2012, but SHM joined the chorus as a strategic partner last year.
“Choosing Wisely is about bending the cost curve,” Dr. Bulger says.
He added that although standardization of care is necessary for Choosing Wisely to work, homogeneity doesn’t mean everybody does everything exactly the same way. It means ensuring that hospitalists adopt “agreed upon best practices” before local variations are added. He compared it to a cookbook of apple pie recipes. All apple pies contain apples and crust, but the tasty treats are tailored differently from there.
“When you come up with guidelines in your hospital, that’s what you’re doing,” Dr. Bulger says. “You’re writing the cookbook and coming up with what works at your hospital. It might not work at [my hospital] at all, but I can look at it and learn.”
In the long-term, SHM hopes to create resources beyond the recommendations themselves—perhaps including a mentored implementation program akin to Project BOOST or pre-packaged order sets and checklists. Whatever the society does, it needs to engage the younger generation of physicians to ensure that quality and safety stay a priority for them, says Darlene Tad-y, MD, chair of SHM’s Physicians in Training Committee.
An assistant professor of medicine and a hospitalist at the University of Colorado Denver, Dr. Tad-y says that getting residents and students involved in quality and safety measures is critical for HM’s future.
“Especially since we want to have hospital medicine be at the forefront,” she explains. “It’s vital for us to have our students and residents taking the lead.”
Younger physicians already see the role quality and safety take in day-to-day practice. So, for them, according to Dr. Tad-y, a focus on making sure patient care is delivered better and more safely isn’t a renewed effort—it’s what they’re taught from the beginning.
“They haven’t been trained in the old way yet,” she says. “They still have an open mind. They see that things can change and things can be better. We don’t have to change old habits. We are just evolving good new habits for them.”
One new perspective was a first-time pre-course, “Cardiology: What Hospitalists Need to Know as Front-Line Providers.” The eight-hour seminar was led by cardiologist Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, who says the time is right for quality-focused hospitalists to devote a full-day pre-course to cardiology.
“Cardiovascular disease is the most common reason we die,” he says. “It’s something hospital-based practitioners see often. Providing a comprehensive, yet simplified, overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The sheer scale of QI initiatives can be daunting, says Michelle Mourad, MD, director of quality and safety at the University of California at San Francisco (UCSF) School of Medicine. She urges her peers to take the proverbial step back, identify a single issue—sepsis mortality or hand hygiene, for example—and then focus on understanding that issue intimately. That way, a hospitalist or HM group can convince other physicians that there is a problem and that it’s worth the work to fix it. Once that’s done, a hospitalist can launch a QI project that devises a measurement strategy to see if change is occurring.
And, while sustaining that change beyond the initial start-up can be difficult, Dr. Mourad believes success breeds success.
“When you work hard at a quality gap that’s in your organization, [when you] actually see the care you provide get better—not just for the patient in front of you, but for all the patients in your organization—it’s extremely powerful and motivating,” she says. “It changes the culture in your institution and convinces other people that they can do the same.”
Hospital Medicine’s Role in Healthcare System Under Affordable Care Act Takes Shape
LAS VEGAS—As America’s favorite pastime began a new season, hospitalists from all parts of the country engaged in a variety of healthcare policy discussions at HM14. That’s why the baseball analogy that SHM advocacy guru Ron Greeno, MD, MHM, used to describe how far along the industry is in implementing the Affordable Care Act (ACA) was particularly fitting: “We’re in the first inning,” he said.
So, while hospitalists are dealing with myriad policy issues stemming from the generational healthcare reform legislation colloquially referred to as “Obamacare,” policy experts at HM14 noted that hospitalists can help control how changes will be incorporated into day-to-day care delivery.
“I want to decrease people’s fear about the role of hospitalists in the healthcare system of the future,” said Dr. Greeno, chief medical officer of Cogent Healthcare in Brentwood, Tenn., and chair of SHM’s Public Policy Committee. “They should feel just the opposite of fear. There is unbelievable opportunity for hospitalists in the realigned healthcare system.”
At a base level, the ACA is codifying and prodding healthcare’s move away from fee-for-service payments to compensation based on the health of a given population. Over time, that shift will reward value, not simply pay up for procedures and tests, Dr. Greeno said.
As an example, he explained, “If we prevent a readmission in a fee-for-service world, there are hospitals that tell us that that actually hurts them; they need that admission. In a population health environment ... if you prevent a readmission, that’s wonderful thing. That’s a hospitalization that did not occur. That creates tremendous value.”
SHM CEO Larry Wellikson, MD, SFHM, said hospitalists not only provide that value on the ground, but also have a strong voice in Washington, D.C. That is especially true with hospitalist Patrick Conway, MD, MSc, FAAP, MHM, who serves as chief medical officer for the Centers for Medicare & Medicaid Services (CMS). Dr. Conway is the former chair of SHM’s Public Policy Committee.
“We’re a young organization with no budget and no power, and we get to have a face-to-face conversation with the guy that’s running Medicare,” Dr. Wellikson said. “Five or six hospitalists from SHM sit on our Public Policy Committee and think about how to fix the observation unit, and the next thing you know it becomes [part] of the regulations and changes things. We’re not your ordinary society.”
Robert Wachter, MD, MHM, also noted that the specialty is waiting to see if the U.S. Senate will approve President Obama’s nomination of Boston hospitalist Vivek Murthy, MD, MBA, as surgeon general of the United States. Dr. Murthy has been a strong supporter of the ACA, but a vote on his approval is being held up by Congress members who are concerned he will use the position as a bully pulpit against gun control, a claim he has denied.
Dr. Wellikson added that when lobbying for continued changes to healthcare rules, SHM tries to focus on providing assistance, not asking for handouts. That will likely be a big focus next year, as the annual meeting returns to a suburb of Washington, D.C., with an expectation that hundreds of hospitalists will participate in the “Hospitalists on the Hill” advocacy event.
“We never go to Washington and ask for more power for hospitals or more money for hospitalists,” Dr. Wellikson said. “When we go to Washington, we say, ‘Things are changing in the system. How can we be a part of that change?’
“And that makes us very, very different.”
To be sure, not everyone at HM14 had the rosiest view on Obamacare and how it will play out in the next few years from a policy perspective. Scott Gottlieb, MD, a practicing physician, U.S. Food and Drug Administration alumni, and American Enterprise Institute fellow, said that the financial repercussions of reforms will reduce costs.
“That might affect hospitalist employment, or the hospitalists are going to have to take on new responsibilities to try to make up for services that hospitals might be shedding,” Dr. Gottlieb said. “But if I were trying to pick a growth industry right now, it would be restructuring distressed hospitals. That’s what’s going to happen in five years.”
Dr. Gottlieb, a frequent contributor to Fox News, said that while many political conservatives argue that Obamacare is driving all of the healthcare problems, many underlying components of the ACA have support from Republicans and Democrats, including proposed reforms to Medicare’s sustainable growth rate (SGR) formula.
“It’s hard to just blame Obamacare for this,” he said. “The SGR bill, which is coming out of a Republican-led House and has bipartisan support, codifies major elements of Obamacare that, frankly, I’ve been criticizing for the last four years.”
Dr. Gottlieb believes that risk sharing has to improve for healthcare reform to be embraced by the best-performing doctors. Bundled payments, for example, shift nearly all of the payment risk onto physicians, because their revenue will be capped at a point, regardless of the cost of services rendered, Dr. Gottlieb said.
“I think, ultimately, as physicians, we should be fearful of payment models that put a lot of the financial risk on physicians without ways to offset some of that risk and without tools to manage it well,” he added.

—Dr. Greeno
HM14 keynote speaker and healthcare futurist Ian Morrison, PhD, said he believes that Obamacare will spur local health systems to merge, until just 100 to 200 regional or super-regional systems exist. Consolidation, he noted, ultimately will reduce the number of health systems to between 50 and 75 nationwide.
“Everybody understands we need to reform the delivery system,” Dr. Morrison said, adding that he wants hospitalists to “have an increased interest in public policy and advocate for the things that we believe in, which is better patient care and better outcomes for patients.”
With reference to Dr. Greeno’s analogy that Obamacare is a baseball game in the first inning, Dr. Morrison said he believes that all HM14 attendees will deal with policy implications of the ACA until the end of their careers. And while those changes are often frustrating, he said one of the core themes—a more unified healthcare delivery system focused on value—is for the greater good.
“The unintended consequences are going to be felt for decades,” he said. “But there are parts of it that would be very hard for anybody to disagree with: that we need to have more alignment in terms of other providers and with hospitals.”
LAS VEGAS—As America’s favorite pastime began a new season, hospitalists from all parts of the country engaged in a variety of healthcare policy discussions at HM14. That’s why the baseball analogy that SHM advocacy guru Ron Greeno, MD, MHM, used to describe how far along the industry is in implementing the Affordable Care Act (ACA) was particularly fitting: “We’re in the first inning,” he said.
So, while hospitalists are dealing with myriad policy issues stemming from the generational healthcare reform legislation colloquially referred to as “Obamacare,” policy experts at HM14 noted that hospitalists can help control how changes will be incorporated into day-to-day care delivery.
“I want to decrease people’s fear about the role of hospitalists in the healthcare system of the future,” said Dr. Greeno, chief medical officer of Cogent Healthcare in Brentwood, Tenn., and chair of SHM’s Public Policy Committee. “They should feel just the opposite of fear. There is unbelievable opportunity for hospitalists in the realigned healthcare system.”
At a base level, the ACA is codifying and prodding healthcare’s move away from fee-for-service payments to compensation based on the health of a given population. Over time, that shift will reward value, not simply pay up for procedures and tests, Dr. Greeno said.
As an example, he explained, “If we prevent a readmission in a fee-for-service world, there are hospitals that tell us that that actually hurts them; they need that admission. In a population health environment ... if you prevent a readmission, that’s wonderful thing. That’s a hospitalization that did not occur. That creates tremendous value.”
SHM CEO Larry Wellikson, MD, SFHM, said hospitalists not only provide that value on the ground, but also have a strong voice in Washington, D.C. That is especially true with hospitalist Patrick Conway, MD, MSc, FAAP, MHM, who serves as chief medical officer for the Centers for Medicare & Medicaid Services (CMS). Dr. Conway is the former chair of SHM’s Public Policy Committee.
“We’re a young organization with no budget and no power, and we get to have a face-to-face conversation with the guy that’s running Medicare,” Dr. Wellikson said. “Five or six hospitalists from SHM sit on our Public Policy Committee and think about how to fix the observation unit, and the next thing you know it becomes [part] of the regulations and changes things. We’re not your ordinary society.”
Robert Wachter, MD, MHM, also noted that the specialty is waiting to see if the U.S. Senate will approve President Obama’s nomination of Boston hospitalist Vivek Murthy, MD, MBA, as surgeon general of the United States. Dr. Murthy has been a strong supporter of the ACA, but a vote on his approval is being held up by Congress members who are concerned he will use the position as a bully pulpit against gun control, a claim he has denied.
Dr. Wellikson added that when lobbying for continued changes to healthcare rules, SHM tries to focus on providing assistance, not asking for handouts. That will likely be a big focus next year, as the annual meeting returns to a suburb of Washington, D.C., with an expectation that hundreds of hospitalists will participate in the “Hospitalists on the Hill” advocacy event.
“We never go to Washington and ask for more power for hospitals or more money for hospitalists,” Dr. Wellikson said. “When we go to Washington, we say, ‘Things are changing in the system. How can we be a part of that change?’
“And that makes us very, very different.”
To be sure, not everyone at HM14 had the rosiest view on Obamacare and how it will play out in the next few years from a policy perspective. Scott Gottlieb, MD, a practicing physician, U.S. Food and Drug Administration alumni, and American Enterprise Institute fellow, said that the financial repercussions of reforms will reduce costs.
“That might affect hospitalist employment, or the hospitalists are going to have to take on new responsibilities to try to make up for services that hospitals might be shedding,” Dr. Gottlieb said. “But if I were trying to pick a growth industry right now, it would be restructuring distressed hospitals. That’s what’s going to happen in five years.”
Dr. Gottlieb, a frequent contributor to Fox News, said that while many political conservatives argue that Obamacare is driving all of the healthcare problems, many underlying components of the ACA have support from Republicans and Democrats, including proposed reforms to Medicare’s sustainable growth rate (SGR) formula.
“It’s hard to just blame Obamacare for this,” he said. “The SGR bill, which is coming out of a Republican-led House and has bipartisan support, codifies major elements of Obamacare that, frankly, I’ve been criticizing for the last four years.”
Dr. Gottlieb believes that risk sharing has to improve for healthcare reform to be embraced by the best-performing doctors. Bundled payments, for example, shift nearly all of the payment risk onto physicians, because their revenue will be capped at a point, regardless of the cost of services rendered, Dr. Gottlieb said.
“I think, ultimately, as physicians, we should be fearful of payment models that put a lot of the financial risk on physicians without ways to offset some of that risk and without tools to manage it well,” he added.

—Dr. Greeno
HM14 keynote speaker and healthcare futurist Ian Morrison, PhD, said he believes that Obamacare will spur local health systems to merge, until just 100 to 200 regional or super-regional systems exist. Consolidation, he noted, ultimately will reduce the number of health systems to between 50 and 75 nationwide.
“Everybody understands we need to reform the delivery system,” Dr. Morrison said, adding that he wants hospitalists to “have an increased interest in public policy and advocate for the things that we believe in, which is better patient care and better outcomes for patients.”
With reference to Dr. Greeno’s analogy that Obamacare is a baseball game in the first inning, Dr. Morrison said he believes that all HM14 attendees will deal with policy implications of the ACA until the end of their careers. And while those changes are often frustrating, he said one of the core themes—a more unified healthcare delivery system focused on value—is for the greater good.
“The unintended consequences are going to be felt for decades,” he said. “But there are parts of it that would be very hard for anybody to disagree with: that we need to have more alignment in terms of other providers and with hospitals.”
LAS VEGAS—As America’s favorite pastime began a new season, hospitalists from all parts of the country engaged in a variety of healthcare policy discussions at HM14. That’s why the baseball analogy that SHM advocacy guru Ron Greeno, MD, MHM, used to describe how far along the industry is in implementing the Affordable Care Act (ACA) was particularly fitting: “We’re in the first inning,” he said.
So, while hospitalists are dealing with myriad policy issues stemming from the generational healthcare reform legislation colloquially referred to as “Obamacare,” policy experts at HM14 noted that hospitalists can help control how changes will be incorporated into day-to-day care delivery.
“I want to decrease people’s fear about the role of hospitalists in the healthcare system of the future,” said Dr. Greeno, chief medical officer of Cogent Healthcare in Brentwood, Tenn., and chair of SHM’s Public Policy Committee. “They should feel just the opposite of fear. There is unbelievable opportunity for hospitalists in the realigned healthcare system.”
At a base level, the ACA is codifying and prodding healthcare’s move away from fee-for-service payments to compensation based on the health of a given population. Over time, that shift will reward value, not simply pay up for procedures and tests, Dr. Greeno said.
As an example, he explained, “If we prevent a readmission in a fee-for-service world, there are hospitals that tell us that that actually hurts them; they need that admission. In a population health environment ... if you prevent a readmission, that’s wonderful thing. That’s a hospitalization that did not occur. That creates tremendous value.”
SHM CEO Larry Wellikson, MD, SFHM, said hospitalists not only provide that value on the ground, but also have a strong voice in Washington, D.C. That is especially true with hospitalist Patrick Conway, MD, MSc, FAAP, MHM, who serves as chief medical officer for the Centers for Medicare & Medicaid Services (CMS). Dr. Conway is the former chair of SHM’s Public Policy Committee.
“We’re a young organization with no budget and no power, and we get to have a face-to-face conversation with the guy that’s running Medicare,” Dr. Wellikson said. “Five or six hospitalists from SHM sit on our Public Policy Committee and think about how to fix the observation unit, and the next thing you know it becomes [part] of the regulations and changes things. We’re not your ordinary society.”
Robert Wachter, MD, MHM, also noted that the specialty is waiting to see if the U.S. Senate will approve President Obama’s nomination of Boston hospitalist Vivek Murthy, MD, MBA, as surgeon general of the United States. Dr. Murthy has been a strong supporter of the ACA, but a vote on his approval is being held up by Congress members who are concerned he will use the position as a bully pulpit against gun control, a claim he has denied.
Dr. Wellikson added that when lobbying for continued changes to healthcare rules, SHM tries to focus on providing assistance, not asking for handouts. That will likely be a big focus next year, as the annual meeting returns to a suburb of Washington, D.C., with an expectation that hundreds of hospitalists will participate in the “Hospitalists on the Hill” advocacy event.
“We never go to Washington and ask for more power for hospitals or more money for hospitalists,” Dr. Wellikson said. “When we go to Washington, we say, ‘Things are changing in the system. How can we be a part of that change?’
“And that makes us very, very different.”
To be sure, not everyone at HM14 had the rosiest view on Obamacare and how it will play out in the next few years from a policy perspective. Scott Gottlieb, MD, a practicing physician, U.S. Food and Drug Administration alumni, and American Enterprise Institute fellow, said that the financial repercussions of reforms will reduce costs.
“That might affect hospitalist employment, or the hospitalists are going to have to take on new responsibilities to try to make up for services that hospitals might be shedding,” Dr. Gottlieb said. “But if I were trying to pick a growth industry right now, it would be restructuring distressed hospitals. That’s what’s going to happen in five years.”
Dr. Gottlieb, a frequent contributor to Fox News, said that while many political conservatives argue that Obamacare is driving all of the healthcare problems, many underlying components of the ACA have support from Republicans and Democrats, including proposed reforms to Medicare’s sustainable growth rate (SGR) formula.
“It’s hard to just blame Obamacare for this,” he said. “The SGR bill, which is coming out of a Republican-led House and has bipartisan support, codifies major elements of Obamacare that, frankly, I’ve been criticizing for the last four years.”
Dr. Gottlieb believes that risk sharing has to improve for healthcare reform to be embraced by the best-performing doctors. Bundled payments, for example, shift nearly all of the payment risk onto physicians, because their revenue will be capped at a point, regardless of the cost of services rendered, Dr. Gottlieb said.
“I think, ultimately, as physicians, we should be fearful of payment models that put a lot of the financial risk on physicians without ways to offset some of that risk and without tools to manage it well,” he added.

—Dr. Greeno
HM14 keynote speaker and healthcare futurist Ian Morrison, PhD, said he believes that Obamacare will spur local health systems to merge, until just 100 to 200 regional or super-regional systems exist. Consolidation, he noted, ultimately will reduce the number of health systems to between 50 and 75 nationwide.
“Everybody understands we need to reform the delivery system,” Dr. Morrison said, adding that he wants hospitalists to “have an increased interest in public policy and advocate for the things that we believe in, which is better patient care and better outcomes for patients.”
With reference to Dr. Greeno’s analogy that Obamacare is a baseball game in the first inning, Dr. Morrison said he believes that all HM14 attendees will deal with policy implications of the ACA until the end of their careers. And while those changes are often frustrating, he said one of the core themes—a more unified healthcare delivery system focused on value—is for the greater good.
“The unintended consequences are going to be felt for decades,” he said. “But there are parts of it that would be very hard for anybody to disagree with: that we need to have more alignment in terms of other providers and with hospitals.”
Hospital Medicine Leaders Share Practice Management Pearls at HM14
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”
Hospital Medicine Pioneer Bob Wachter, MD, MHM, Hits High Note at HM14
"“Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice."
LAS VEGAS—Bob Wachter, MD, MHM, hyped the final six minutes of his annual meeting address as something hospitalists at HM14 conference wouldn’t forget. As usual, he was right.
The man who helped coin the term “hospitalist,” and whose penultimate pep talk has come to signal the unofficial end of SHM’s annual meeting, finished his plenary on the confab’s last day and returned minutes later in a white suit, yellowed wig, and sunglasses worthy of the man he was portraying: Elton John.
After enjoying Dr. Wachter’s retooled lyrics—in which “Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice.
“That was just phenomenal,” said hospitalist Kevin Gilroy, MD, of Greenville, S.C. “What other conference does that? You find another society that is that down to Earth.”—RQ
"“Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice."
LAS VEGAS—Bob Wachter, MD, MHM, hyped the final six minutes of his annual meeting address as something hospitalists at HM14 conference wouldn’t forget. As usual, he was right.
The man who helped coin the term “hospitalist,” and whose penultimate pep talk has come to signal the unofficial end of SHM’s annual meeting, finished his plenary on the confab’s last day and returned minutes later in a white suit, yellowed wig, and sunglasses worthy of the man he was portraying: Elton John.
After enjoying Dr. Wachter’s retooled lyrics—in which “Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice.
“That was just phenomenal,” said hospitalist Kevin Gilroy, MD, of Greenville, S.C. “What other conference does that? You find another society that is that down to Earth.”—RQ
"“Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice."
LAS VEGAS—Bob Wachter, MD, MHM, hyped the final six minutes of his annual meeting address as something hospitalists at HM14 conference wouldn’t forget. As usual, he was right.
The man who helped coin the term “hospitalist,” and whose penultimate pep talk has come to signal the unofficial end of SHM’s annual meeting, finished his plenary on the confab’s last day and returned minutes later in a white suit, yellowed wig, and sunglasses worthy of the man he was portraying: Elton John.
After enjoying Dr. Wachter’s retooled lyrics—in which “Your Song” became “Your Hospitalist Song”—the crowd gave him a standing ovation, perhaps as much for his chutzpah and piano playing as for his voice.
“That was just phenomenal,” said hospitalist Kevin Gilroy, MD, of Greenville, S.C. “What other conference does that? You find another society that is that down to Earth.”—RQ
HM14 Keynote Speakers Encourage Hospitalists to Deliver High-Quality, Low-Cost Patient Care
LAS VEGAS—A record 3,600 hospitalists swarmed the Mandalay Bay Resort and Casino for four days of education and networking that wrapped with the “father of HM,” Bob Wachter, MD, MHM, dressed as Elton John, warbling a hospitalist-centric version of Sir Elton’s chart topper, “Your Song,” to a packed ballroom.
“[HM14] is just intoxicating,” said hospitalist Kevin Gilroy, MD, of Greenville (S.C.) Health System. “And it ends with our daddy getting up there and lighting it up as Elton John. What other conference does that?”
In perhaps the most tweeted line from HM14, keynote speaker Ian Morrison, PhD, compared the addictiveness of crack cocaine with physicians’ dedication to the fee-for-service payment system.
“It’s really hard to get off of it,” the national healthcare expert deadpanned to a packed ballroom at the Mandalay Bay Resort and Casino.
The zinger was one of the highlights of the annual meeting’s three plenary addresses, which alternately gave the record 3,600 hospitalists in attendance doses of sobriety about the difficulty of healthcare reform and comedy bits from Dr. Morrison and HM dean Robert Wachter, MD, MHM.
The keynote titled “Obamacare Is Here: What Does It Mean for You and Your Hospital?” featured a panel discussion among Centers for Medicare & Medicaid Services (CMS) chief medical officer Patrick Conway, MD, MSc, MHM, FAAP; executive director and CEO of the Medical University of South Carolina in Charleston and former SHM president Patrick Cawley, MD, MBA, MHM, FACP, FACHE; veteran healthcare executive Patrick Courneya, MD; and American Enterprise Institute resident fellow Scott Gottlieb, MD. The quartet—dubbed the Patricks and Scott by several emcees—followed their hour-long plenary with a question-and-answer session.
“I think this is ultimately going to hurt the financial standing of the hospital industry,” said Dr. Gottlieb, a newcomer to SHM’s annual meeting. “A lot of these hospitals that are taking on these capitated contracts, taking on risk, consolidating physicians, I think they’re going to get themselves into financial trouble in the next five years. That’s going to put pressure on the hospitalists.”

–Dr. Gottlieb
Dr. Cawley said that just a few years ago, his institution subsidized five medical groups. Now it’s 25. He has a simple message for hospitalists not committed to providing better care at lower costs: “You’re not going to be on my good side.”
Dr. Wachter told medical students and residents that he sees no end in sight to the unrelenting pressure to provide that high-quality, low-cost care, while also making sure patient satisfaction rises. And he’s more than OK with that.
“It’s important to recognize that the goal we’re being asked to achieve—to deliver high-quality, satisfying, evidence-based care without undue variations, where we’re not harming people and doing it at a cost that doesn’t bankrupt society—is unambiguously right,” he said. “It’s such an obviously right goal that what is odd is that this was not our goal until recently. So the fact that our field has taken this on as our mantra is very satisfying and completely appropriate.”
The keynote addresses also highlighted another satisfying result: Immediate past SHM President Eric Howell, MD, SFHM, reached the goal he set at 2013’s annual meeting to double the society’s number of student and housestaff members from 500 to 1,000.
Newly minted SHM President Burke Kealey, MD, SFHM, has a goal that is a bit more abstract: He wants hospitalists to look at improving healthcare affordability, patient health, and the patient experience—as a single goal.
“We put the energy and the effort of the moment behind the squeaky wheel,” said Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey’s tack for his one-year term is borrowed from the Institute of Healthcare Improvement, whose “triple aim” initiative has the same goals. But Dr. Kealey believes that focusing on any of the three areas while giving short shrift to the others misses the point of bettering the overall healthcare system.
“To improve health, but then people can’t afford that healthcare, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”

–Dr. Kealey
And hospitalists are in the perfect position to do it, said Dr. Morrison, a founding partner of Strategic Health Perspectives, a forecasting service for the healthcare industry that includes joint venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management. He sees hospitalist leaders as change agents, as the rigmarole of healthcare reform shakes out over the next few years.
Dr. Morrison, a native of Scotland whose delivery was half stand-up comic, half policy wonk (he introduced himself as Dr. Wachter’s Scottish caddy), said that while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients’ needs.
“This is the work of the future,” he said, “and it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future.
“We’ve got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver. This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at.”
LAS VEGAS—A record 3,600 hospitalists swarmed the Mandalay Bay Resort and Casino for four days of education and networking that wrapped with the “father of HM,” Bob Wachter, MD, MHM, dressed as Elton John, warbling a hospitalist-centric version of Sir Elton’s chart topper, “Your Song,” to a packed ballroom.
“[HM14] is just intoxicating,” said hospitalist Kevin Gilroy, MD, of Greenville (S.C.) Health System. “And it ends with our daddy getting up there and lighting it up as Elton John. What other conference does that?”
In perhaps the most tweeted line from HM14, keynote speaker Ian Morrison, PhD, compared the addictiveness of crack cocaine with physicians’ dedication to the fee-for-service payment system.
“It’s really hard to get off of it,” the national healthcare expert deadpanned to a packed ballroom at the Mandalay Bay Resort and Casino.
The zinger was one of the highlights of the annual meeting’s three plenary addresses, which alternately gave the record 3,600 hospitalists in attendance doses of sobriety about the difficulty of healthcare reform and comedy bits from Dr. Morrison and HM dean Robert Wachter, MD, MHM.
The keynote titled “Obamacare Is Here: What Does It Mean for You and Your Hospital?” featured a panel discussion among Centers for Medicare & Medicaid Services (CMS) chief medical officer Patrick Conway, MD, MSc, MHM, FAAP; executive director and CEO of the Medical University of South Carolina in Charleston and former SHM president Patrick Cawley, MD, MBA, MHM, FACP, FACHE; veteran healthcare executive Patrick Courneya, MD; and American Enterprise Institute resident fellow Scott Gottlieb, MD. The quartet—dubbed the Patricks and Scott by several emcees—followed their hour-long plenary with a question-and-answer session.
“I think this is ultimately going to hurt the financial standing of the hospital industry,” said Dr. Gottlieb, a newcomer to SHM’s annual meeting. “A lot of these hospitals that are taking on these capitated contracts, taking on risk, consolidating physicians, I think they’re going to get themselves into financial trouble in the next five years. That’s going to put pressure on the hospitalists.”

–Dr. Gottlieb
Dr. Cawley said that just a few years ago, his institution subsidized five medical groups. Now it’s 25. He has a simple message for hospitalists not committed to providing better care at lower costs: “You’re not going to be on my good side.”
Dr. Wachter told medical students and residents that he sees no end in sight to the unrelenting pressure to provide that high-quality, low-cost care, while also making sure patient satisfaction rises. And he’s more than OK with that.
“It’s important to recognize that the goal we’re being asked to achieve—to deliver high-quality, satisfying, evidence-based care without undue variations, where we’re not harming people and doing it at a cost that doesn’t bankrupt society—is unambiguously right,” he said. “It’s such an obviously right goal that what is odd is that this was not our goal until recently. So the fact that our field has taken this on as our mantra is very satisfying and completely appropriate.”
The keynote addresses also highlighted another satisfying result: Immediate past SHM President Eric Howell, MD, SFHM, reached the goal he set at 2013’s annual meeting to double the society’s number of student and housestaff members from 500 to 1,000.
Newly minted SHM President Burke Kealey, MD, SFHM, has a goal that is a bit more abstract: He wants hospitalists to look at improving healthcare affordability, patient health, and the patient experience—as a single goal.
“We put the energy and the effort of the moment behind the squeaky wheel,” said Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey’s tack for his one-year term is borrowed from the Institute of Healthcare Improvement, whose “triple aim” initiative has the same goals. But Dr. Kealey believes that focusing on any of the three areas while giving short shrift to the others misses the point of bettering the overall healthcare system.
“To improve health, but then people can’t afford that healthcare, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”

–Dr. Kealey
And hospitalists are in the perfect position to do it, said Dr. Morrison, a founding partner of Strategic Health Perspectives, a forecasting service for the healthcare industry that includes joint venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management. He sees hospitalist leaders as change agents, as the rigmarole of healthcare reform shakes out over the next few years.
Dr. Morrison, a native of Scotland whose delivery was half stand-up comic, half policy wonk (he introduced himself as Dr. Wachter’s Scottish caddy), said that while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients’ needs.
“This is the work of the future,” he said, “and it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future.
“We’ve got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver. This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at.”
LAS VEGAS—A record 3,600 hospitalists swarmed the Mandalay Bay Resort and Casino for four days of education and networking that wrapped with the “father of HM,” Bob Wachter, MD, MHM, dressed as Elton John, warbling a hospitalist-centric version of Sir Elton’s chart topper, “Your Song,” to a packed ballroom.
“[HM14] is just intoxicating,” said hospitalist Kevin Gilroy, MD, of Greenville (S.C.) Health System. “And it ends with our daddy getting up there and lighting it up as Elton John. What other conference does that?”
In perhaps the most tweeted line from HM14, keynote speaker Ian Morrison, PhD, compared the addictiveness of crack cocaine with physicians’ dedication to the fee-for-service payment system.
“It’s really hard to get off of it,” the national healthcare expert deadpanned to a packed ballroom at the Mandalay Bay Resort and Casino.
The zinger was one of the highlights of the annual meeting’s three plenary addresses, which alternately gave the record 3,600 hospitalists in attendance doses of sobriety about the difficulty of healthcare reform and comedy bits from Dr. Morrison and HM dean Robert Wachter, MD, MHM.
The keynote titled “Obamacare Is Here: What Does It Mean for You and Your Hospital?” featured a panel discussion among Centers for Medicare & Medicaid Services (CMS) chief medical officer Patrick Conway, MD, MSc, MHM, FAAP; executive director and CEO of the Medical University of South Carolina in Charleston and former SHM president Patrick Cawley, MD, MBA, MHM, FACP, FACHE; veteran healthcare executive Patrick Courneya, MD; and American Enterprise Institute resident fellow Scott Gottlieb, MD. The quartet—dubbed the Patricks and Scott by several emcees—followed their hour-long plenary with a question-and-answer session.
“I think this is ultimately going to hurt the financial standing of the hospital industry,” said Dr. Gottlieb, a newcomer to SHM’s annual meeting. “A lot of these hospitals that are taking on these capitated contracts, taking on risk, consolidating physicians, I think they’re going to get themselves into financial trouble in the next five years. That’s going to put pressure on the hospitalists.”

–Dr. Gottlieb
Dr. Cawley said that just a few years ago, his institution subsidized five medical groups. Now it’s 25. He has a simple message for hospitalists not committed to providing better care at lower costs: “You’re not going to be on my good side.”
Dr. Wachter told medical students and residents that he sees no end in sight to the unrelenting pressure to provide that high-quality, low-cost care, while also making sure patient satisfaction rises. And he’s more than OK with that.
“It’s important to recognize that the goal we’re being asked to achieve—to deliver high-quality, satisfying, evidence-based care without undue variations, where we’re not harming people and doing it at a cost that doesn’t bankrupt society—is unambiguously right,” he said. “It’s such an obviously right goal that what is odd is that this was not our goal until recently. So the fact that our field has taken this on as our mantra is very satisfying and completely appropriate.”
The keynote addresses also highlighted another satisfying result: Immediate past SHM President Eric Howell, MD, SFHM, reached the goal he set at 2013’s annual meeting to double the society’s number of student and housestaff members from 500 to 1,000.
Newly minted SHM President Burke Kealey, MD, SFHM, has a goal that is a bit more abstract: He wants hospitalists to look at improving healthcare affordability, patient health, and the patient experience—as a single goal.
“We put the energy and the effort of the moment behind the squeaky wheel,” said Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey’s tack for his one-year term is borrowed from the Institute of Healthcare Improvement, whose “triple aim” initiative has the same goals. But Dr. Kealey believes that focusing on any of the three areas while giving short shrift to the others misses the point of bettering the overall healthcare system.
“To improve health, but then people can’t afford that healthcare, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”

–Dr. Kealey
And hospitalists are in the perfect position to do it, said Dr. Morrison, a founding partner of Strategic Health Perspectives, a forecasting service for the healthcare industry that includes joint venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management. He sees hospitalist leaders as change agents, as the rigmarole of healthcare reform shakes out over the next few years.
Dr. Morrison, a native of Scotland whose delivery was half stand-up comic, half policy wonk (he introduced himself as Dr. Wachter’s Scottish caddy), said that while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients’ needs.
“This is the work of the future,” he said, “and it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future.
“We’ve got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver. This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at.”
Listen Now! Ron Greeno Discusses Policy Issues Facing Hospitalists
Click here to listen to excerpts of our interview with SHM Public Policy Committee Chair Ron Greeno, MD, MHM
Click here to listen to excerpts of our interview with SHM Public Policy Committee Chair Ron Greeno, MD, MHM
Click here to listen to excerpts of our interview with SHM Public Policy Committee Chair Ron Greeno, MD, MHM