User login
Study identifies predictors of bariatric surgery attrition
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
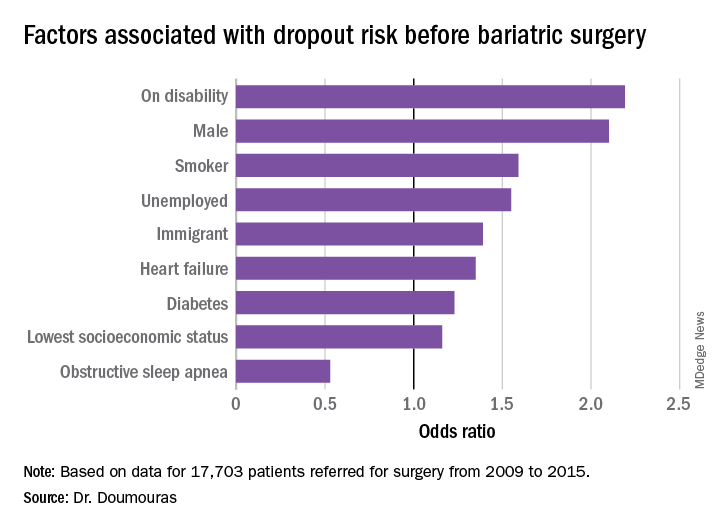
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
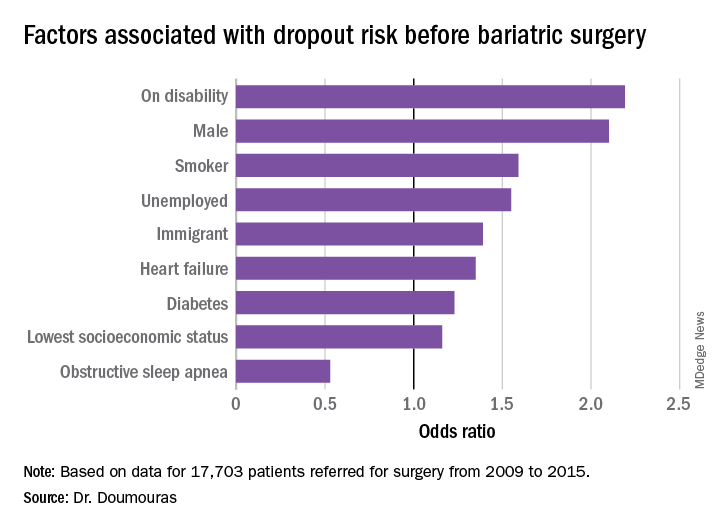
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
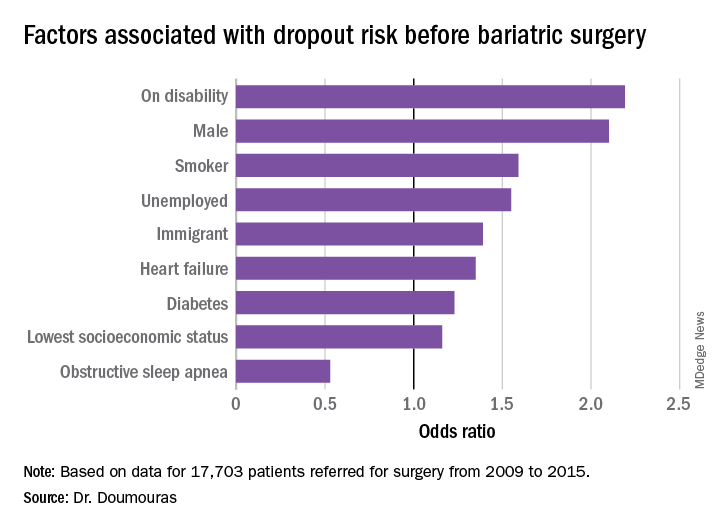
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
REPORTING FROM SAGES 2019
Study finds inconsistencies in MBSAQIP database
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
REPORTING FROM SAGES 2019
Study identifies malpractice causes in hernia repair
BALTIMORE – An and intraoperative damage to surrounding structures was the leading reason for such lawsuits, according to research presented at the annual meeting of the American Gastrointestinal and Endoscopic Surgeons.
The purpose of the study was to identify leading causes of litigation for hernia repair as the volume of hernia repairs in the United States increases with a trend toward minimally invasive and robotic surgery, said Asad Choudhry, MBBS, of the State University of New York, Syracuse.“In terms of the hernia itself, inguinal hernia operations were found to be the most common hernia procedure that led to pursuance of litigation, and laparoscopy was the most common type of procedure rather than open in terms of patients pursuing litigation.”
The study sampled the WestLawNext legal database for medical malpractice abdominal wall procedures, and evaluated 430 cases of abdominopelvic wall hernias that fit the study criteria – inguinal, femoral, ventral, umbilical, parastomal, spigelian, obturator, epigastric, incisional, paraumbilical, and pantaloon hernias, Dr. Choudhry said. Hiatal, diaphragmatic, sciatic, gluteal, and lumbar hernias were excluded. He noted that abdominal wall hernia have been reported to be the second most common abdominopelvic procedure performed in the United States after C-section, with more than 1 million procedures done annually (Surg Clin N Am. 2003;83:1045-51).
While most malpractice hernia cases were decided in favor of the defendant surgeon, settlements and cases with a jury verdict in favor of the plaintiff were costly. Dr. Choudhry cited awards of $6.8 million, $12 million, and $3 million in specific hernia cases.
“In terms of the type of repair itself, elective operations were more common, and mesh was used in approximately 27% of cases in which there was a defendant verdict and 18% of cases in which there was a plaintiff verdict,” he said.
For inguinal hernia, 61% of cases were decided for the defendant surgeon. With regards to type of procedure, laparoscopic surgery resulted in defendant verdicts in 31% of cases versus 23% for the plaintiff, and open operations resulted in a ruling favoring the defendant surgeon in 26% versus 15% for the plaintiff. (The remainder were lap-converted-to-open operations, with 2% for the defendant and 1% for the plaintiff.)
Mortality was a key determinant of verdict, Dr. Choudhry added. “Cases with no mortality were more likely of having an outcome in favor of the defendant surgeon.”
The researchers also looked at litigation arising from the phase of care – before, during, or after surgery. “In the preoperative time setting, delay or failure to diagnose or manage a hernia was the leading cause of malpractice,” Dr. Choudhry said. “These cases were mainly emergent patients presenting to the emergency department where the intervention was not performed in a timely manner and leading to some form of complication.”
In the intraoperative period, damage to surrounding structures was by far the leading cause of malpractice, but incomplete procedure or improper surgical technique and use of improper surgical materials also were significant causes in this period. Postoperatively, failure to timely detect and/or repair a surgical complication was the most common cause of litigation. “However, it’s important to note that persistent pain, such as nerve entrapment syndrome, is also noted in the postoperative time period as a cause of litigation,” he added.
The study also evaluated injury severity in the context of a claim outcome. “Most claims where there was an insignificant or minor injury were decided for the defendant surgeon,” Dr. Choudhry said. “But as you start moving higher on the injury scale toward death, these cases were more likely to favor the plaintiff, and that’s correlative because patients tend to sue more when there’s a more significant complication, such as when there’s a death of a family member.” In cases involving death, 41% resulted in a verdict for the defendant surgery, 35% in a plaintiff verdict, and 23% in a settlement, whereas in cases involving insignificant temporary injury, 90% were ruled for the defendant surgeon, with none going to settlement.
The research also found another mitigating factor in malpractice lawsuits: the number of lawyers in a state. “We noted that specific states such as California, New York, Texas, and Florida were bound to have a higher number of lawsuits per population, and this was correlative with the number of lawyers practicing within that state,” Dr. Choudhry said. New York led the nation with 46 cases, followed by California with 42, Florida with 27 ,and Texas and Pennsylvania with 17 each.
Session moderator Heather Logghe, MD, of Jefferson Medical College, Philadelphia, questioned Dr. Choudhry on how surgeons can improve their informed consent process to protect against potential litigation.
“The most important thing we can do is document and explain the risk, benefits, and alternatives, and use an inclusive informed consent that will allow the patients to have a complete understanding of the procedure that is to be done and the complications that may result,” he said. This process needs to be tailored to individual hospital systems. “This may allow for better documentation, and it may not decrease the number of malpractice lawsuits but it may decrease the outcomes not in favor of physicians.”
The researchers also identified trends in the broader context of medical malpractice. Citing data from the National Practitioner Data Bank, Dr. Choudhry noted that malpractice payouts have been increasing since 2012 after a steady 9-year decline. In addition, general surgeons are at greater risk than all but two other types of specialists – neurosurgeons and thoracic-cardiovascular surgeons (N Engl J Med. 2011;365:629-36). “Fifteen percent of general surgeons will be facing malpractice claims annually across the United States. Physicians in high-legal-risk specialties, such as the surgical specialties, are 99% likely to face a claim over their careers.”
The next step for the researchers is to use malpractice insurance data to study medical liability on a larger scale and identify methods physicians can use to improve patient care and mitigate risk, Dr. Choudhry said.
Dr. Choudhry had no relevant financial relationships to disclose.
SOURCE: Choudhry A et al. SAGES 2109, Abstract S104.
BALTIMORE – An and intraoperative damage to surrounding structures was the leading reason for such lawsuits, according to research presented at the annual meeting of the American Gastrointestinal and Endoscopic Surgeons.
The purpose of the study was to identify leading causes of litigation for hernia repair as the volume of hernia repairs in the United States increases with a trend toward minimally invasive and robotic surgery, said Asad Choudhry, MBBS, of the State University of New York, Syracuse.“In terms of the hernia itself, inguinal hernia operations were found to be the most common hernia procedure that led to pursuance of litigation, and laparoscopy was the most common type of procedure rather than open in terms of patients pursuing litigation.”
The study sampled the WestLawNext legal database for medical malpractice abdominal wall procedures, and evaluated 430 cases of abdominopelvic wall hernias that fit the study criteria – inguinal, femoral, ventral, umbilical, parastomal, spigelian, obturator, epigastric, incisional, paraumbilical, and pantaloon hernias, Dr. Choudhry said. Hiatal, diaphragmatic, sciatic, gluteal, and lumbar hernias were excluded. He noted that abdominal wall hernia have been reported to be the second most common abdominopelvic procedure performed in the United States after C-section, with more than 1 million procedures done annually (Surg Clin N Am. 2003;83:1045-51).
While most malpractice hernia cases were decided in favor of the defendant surgeon, settlements and cases with a jury verdict in favor of the plaintiff were costly. Dr. Choudhry cited awards of $6.8 million, $12 million, and $3 million in specific hernia cases.
“In terms of the type of repair itself, elective operations were more common, and mesh was used in approximately 27% of cases in which there was a defendant verdict and 18% of cases in which there was a plaintiff verdict,” he said.
For inguinal hernia, 61% of cases were decided for the defendant surgeon. With regards to type of procedure, laparoscopic surgery resulted in defendant verdicts in 31% of cases versus 23% for the plaintiff, and open operations resulted in a ruling favoring the defendant surgeon in 26% versus 15% for the plaintiff. (The remainder were lap-converted-to-open operations, with 2% for the defendant and 1% for the plaintiff.)
Mortality was a key determinant of verdict, Dr. Choudhry added. “Cases with no mortality were more likely of having an outcome in favor of the defendant surgeon.”
The researchers also looked at litigation arising from the phase of care – before, during, or after surgery. “In the preoperative time setting, delay or failure to diagnose or manage a hernia was the leading cause of malpractice,” Dr. Choudhry said. “These cases were mainly emergent patients presenting to the emergency department where the intervention was not performed in a timely manner and leading to some form of complication.”
In the intraoperative period, damage to surrounding structures was by far the leading cause of malpractice, but incomplete procedure or improper surgical technique and use of improper surgical materials also were significant causes in this period. Postoperatively, failure to timely detect and/or repair a surgical complication was the most common cause of litigation. “However, it’s important to note that persistent pain, such as nerve entrapment syndrome, is also noted in the postoperative time period as a cause of litigation,” he added.
The study also evaluated injury severity in the context of a claim outcome. “Most claims where there was an insignificant or minor injury were decided for the defendant surgeon,” Dr. Choudhry said. “But as you start moving higher on the injury scale toward death, these cases were more likely to favor the plaintiff, and that’s correlative because patients tend to sue more when there’s a more significant complication, such as when there’s a death of a family member.” In cases involving death, 41% resulted in a verdict for the defendant surgery, 35% in a plaintiff verdict, and 23% in a settlement, whereas in cases involving insignificant temporary injury, 90% were ruled for the defendant surgeon, with none going to settlement.
The research also found another mitigating factor in malpractice lawsuits: the number of lawyers in a state. “We noted that specific states such as California, New York, Texas, and Florida were bound to have a higher number of lawsuits per population, and this was correlative with the number of lawyers practicing within that state,” Dr. Choudhry said. New York led the nation with 46 cases, followed by California with 42, Florida with 27 ,and Texas and Pennsylvania with 17 each.
Session moderator Heather Logghe, MD, of Jefferson Medical College, Philadelphia, questioned Dr. Choudhry on how surgeons can improve their informed consent process to protect against potential litigation.
“The most important thing we can do is document and explain the risk, benefits, and alternatives, and use an inclusive informed consent that will allow the patients to have a complete understanding of the procedure that is to be done and the complications that may result,” he said. This process needs to be tailored to individual hospital systems. “This may allow for better documentation, and it may not decrease the number of malpractice lawsuits but it may decrease the outcomes not in favor of physicians.”
The researchers also identified trends in the broader context of medical malpractice. Citing data from the National Practitioner Data Bank, Dr. Choudhry noted that malpractice payouts have been increasing since 2012 after a steady 9-year decline. In addition, general surgeons are at greater risk than all but two other types of specialists – neurosurgeons and thoracic-cardiovascular surgeons (N Engl J Med. 2011;365:629-36). “Fifteen percent of general surgeons will be facing malpractice claims annually across the United States. Physicians in high-legal-risk specialties, such as the surgical specialties, are 99% likely to face a claim over their careers.”
The next step for the researchers is to use malpractice insurance data to study medical liability on a larger scale and identify methods physicians can use to improve patient care and mitigate risk, Dr. Choudhry said.
Dr. Choudhry had no relevant financial relationships to disclose.
SOURCE: Choudhry A et al. SAGES 2109, Abstract S104.
BALTIMORE – An and intraoperative damage to surrounding structures was the leading reason for such lawsuits, according to research presented at the annual meeting of the American Gastrointestinal and Endoscopic Surgeons.
The purpose of the study was to identify leading causes of litigation for hernia repair as the volume of hernia repairs in the United States increases with a trend toward minimally invasive and robotic surgery, said Asad Choudhry, MBBS, of the State University of New York, Syracuse.“In terms of the hernia itself, inguinal hernia operations were found to be the most common hernia procedure that led to pursuance of litigation, and laparoscopy was the most common type of procedure rather than open in terms of patients pursuing litigation.”
The study sampled the WestLawNext legal database for medical malpractice abdominal wall procedures, and evaluated 430 cases of abdominopelvic wall hernias that fit the study criteria – inguinal, femoral, ventral, umbilical, parastomal, spigelian, obturator, epigastric, incisional, paraumbilical, and pantaloon hernias, Dr. Choudhry said. Hiatal, diaphragmatic, sciatic, gluteal, and lumbar hernias were excluded. He noted that abdominal wall hernia have been reported to be the second most common abdominopelvic procedure performed in the United States after C-section, with more than 1 million procedures done annually (Surg Clin N Am. 2003;83:1045-51).
While most malpractice hernia cases were decided in favor of the defendant surgeon, settlements and cases with a jury verdict in favor of the plaintiff were costly. Dr. Choudhry cited awards of $6.8 million, $12 million, and $3 million in specific hernia cases.
“In terms of the type of repair itself, elective operations were more common, and mesh was used in approximately 27% of cases in which there was a defendant verdict and 18% of cases in which there was a plaintiff verdict,” he said.
For inguinal hernia, 61% of cases were decided for the defendant surgeon. With regards to type of procedure, laparoscopic surgery resulted in defendant verdicts in 31% of cases versus 23% for the plaintiff, and open operations resulted in a ruling favoring the defendant surgeon in 26% versus 15% for the plaintiff. (The remainder were lap-converted-to-open operations, with 2% for the defendant and 1% for the plaintiff.)
Mortality was a key determinant of verdict, Dr. Choudhry added. “Cases with no mortality were more likely of having an outcome in favor of the defendant surgeon.”
The researchers also looked at litigation arising from the phase of care – before, during, or after surgery. “In the preoperative time setting, delay or failure to diagnose or manage a hernia was the leading cause of malpractice,” Dr. Choudhry said. “These cases were mainly emergent patients presenting to the emergency department where the intervention was not performed in a timely manner and leading to some form of complication.”
In the intraoperative period, damage to surrounding structures was by far the leading cause of malpractice, but incomplete procedure or improper surgical technique and use of improper surgical materials also were significant causes in this period. Postoperatively, failure to timely detect and/or repair a surgical complication was the most common cause of litigation. “However, it’s important to note that persistent pain, such as nerve entrapment syndrome, is also noted in the postoperative time period as a cause of litigation,” he added.
The study also evaluated injury severity in the context of a claim outcome. “Most claims where there was an insignificant or minor injury were decided for the defendant surgeon,” Dr. Choudhry said. “But as you start moving higher on the injury scale toward death, these cases were more likely to favor the plaintiff, and that’s correlative because patients tend to sue more when there’s a more significant complication, such as when there’s a death of a family member.” In cases involving death, 41% resulted in a verdict for the defendant surgery, 35% in a plaintiff verdict, and 23% in a settlement, whereas in cases involving insignificant temporary injury, 90% were ruled for the defendant surgeon, with none going to settlement.
The research also found another mitigating factor in malpractice lawsuits: the number of lawyers in a state. “We noted that specific states such as California, New York, Texas, and Florida were bound to have a higher number of lawsuits per population, and this was correlative with the number of lawyers practicing within that state,” Dr. Choudhry said. New York led the nation with 46 cases, followed by California with 42, Florida with 27 ,and Texas and Pennsylvania with 17 each.
Session moderator Heather Logghe, MD, of Jefferson Medical College, Philadelphia, questioned Dr. Choudhry on how surgeons can improve their informed consent process to protect against potential litigation.
“The most important thing we can do is document and explain the risk, benefits, and alternatives, and use an inclusive informed consent that will allow the patients to have a complete understanding of the procedure that is to be done and the complications that may result,” he said. This process needs to be tailored to individual hospital systems. “This may allow for better documentation, and it may not decrease the number of malpractice lawsuits but it may decrease the outcomes not in favor of physicians.”
The researchers also identified trends in the broader context of medical malpractice. Citing data from the National Practitioner Data Bank, Dr. Choudhry noted that malpractice payouts have been increasing since 2012 after a steady 9-year decline. In addition, general surgeons are at greater risk than all but two other types of specialists – neurosurgeons and thoracic-cardiovascular surgeons (N Engl J Med. 2011;365:629-36). “Fifteen percent of general surgeons will be facing malpractice claims annually across the United States. Physicians in high-legal-risk specialties, such as the surgical specialties, are 99% likely to face a claim over their careers.”
The next step for the researchers is to use malpractice insurance data to study medical liability on a larger scale and identify methods physicians can use to improve patient care and mitigate risk, Dr. Choudhry said.
Dr. Choudhry had no relevant financial relationships to disclose.
SOURCE: Choudhry A et al. SAGES 2109, Abstract S104.
REPORTING FROM SAGES 2019
Study: Surgeon post-SG reflux rates vary widely
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
REPORTING FROM SAGES 2019
Robotic and lap surgery achieve similar negative margins for rectal resection
BALTIMORE – A head-to-head comparison of robotic and laparoscopic surgery for locally advanced rectal cancer has found that the operations achieve similar outcomes in terms of composite negative margins, overall survival, and readmissions, but that robotic surgery is associated with lower rates of conversion to open surgery and shorter hospital stays, according to an analysis of cases in the National Cancer Database presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The gold standard for how we’re taking care of our patients, of course, is how we’re doing with the cancer survival, and we found no difference for overall survival in the robotic arm and the laparoscopic arm,” said M. Benjamin Hopkins, MD, of Vanderbilt University, Nashville, Tenn. He reported on a retrospective review of 7,616 operations for rectal adenocarcinoma in the National Cancer Database from 2010 to 2014. The study population included 2,472 (32%) robotic procedures. The hazard ratio for 5-year overall survival was 0.87 (P = .18), Dr. Hopkins noted, with virtually identical Kaplan-Meier survival curves between the two approaches.
The negative margin rates were also similar between the two groups: 93.7% for the robotic patients and 92.9% for the laparoscopic cohort (odds ratio 0.86, P = .23), Dr. Hopkins noted. Readmission rates were 9% and 8%, respectively (odds ratio 1.02, P = .44).
There were two significant differences in outcomes between the two groups: The conversion rate to open surgery for the robotic group “was about half that from what we saw with laparoscopic surgery,” he said – 8% vs. 15%; and “a slightly decreased length of stay” in the robotic group – 6.3 vs. 6.7 days (P less than .001).
Dr. Hopkins noted that the science supporting robotic surgery for rectal resection is still somewhat nascent, pointing to the ROLARR randomized trial, which showed conversion rates similar to those of open between the two minimally invasive approaches (8.1% for robotic and 12.2% for laparoscopy [P = .16] JAMA. 2017; 318[16]:1569-80). “Surgeons in this study were still on their learning curve, and what the results showed was that among surgeons, even with varied experience, robotic surgery was [equal] to laparoscopic surgery in relation to conversion rates and composite margin for cancer specimens,” he said of the ROLARR trial.
That led to the premise for his group’s study. “The hypothesis that we had going into this study was that we are able to get a better composite negative margin with robotic surgery as opposed to laparoscopic surgery, which would then translate into improved cancer survival for our patients,” he said. Like the ROLARR trial, the 2010-2014 National Cancer Database dataset Dr. Hopkins and colleagues used includes a window for the learning curve, he added.
“One of the questions that always comes at us from hospital administration and from insurance companies is whether or not there’s a cost benefit for the patient: What is the value to the patient?” Dr. Hopkins noted. “I’d like to see future studies where we’re looking at this value and, as we decrease our operative time and anesthesia costs, and hopefully some decreased cost in the instrumentation, we start to see some more benefits as we get more facile with robotic surgery.”
Dr. Hopkins has no financial relationships to disclose.
SOURCE: Hopkins B et al. SAGES 2019. Session SS13; abstract S058
CORRECTION 5/14/2109 : The hazard ratio for 5-year overall survival and p-value were updated.
BALTIMORE – A head-to-head comparison of robotic and laparoscopic surgery for locally advanced rectal cancer has found that the operations achieve similar outcomes in terms of composite negative margins, overall survival, and readmissions, but that robotic surgery is associated with lower rates of conversion to open surgery and shorter hospital stays, according to an analysis of cases in the National Cancer Database presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The gold standard for how we’re taking care of our patients, of course, is how we’re doing with the cancer survival, and we found no difference for overall survival in the robotic arm and the laparoscopic arm,” said M. Benjamin Hopkins, MD, of Vanderbilt University, Nashville, Tenn. He reported on a retrospective review of 7,616 operations for rectal adenocarcinoma in the National Cancer Database from 2010 to 2014. The study population included 2,472 (32%) robotic procedures. The hazard ratio for 5-year overall survival was 0.87 (P = .18), Dr. Hopkins noted, with virtually identical Kaplan-Meier survival curves between the two approaches.
The negative margin rates were also similar between the two groups: 93.7% for the robotic patients and 92.9% for the laparoscopic cohort (odds ratio 0.86, P = .23), Dr. Hopkins noted. Readmission rates were 9% and 8%, respectively (odds ratio 1.02, P = .44).
There were two significant differences in outcomes between the two groups: The conversion rate to open surgery for the robotic group “was about half that from what we saw with laparoscopic surgery,” he said – 8% vs. 15%; and “a slightly decreased length of stay” in the robotic group – 6.3 vs. 6.7 days (P less than .001).
Dr. Hopkins noted that the science supporting robotic surgery for rectal resection is still somewhat nascent, pointing to the ROLARR randomized trial, which showed conversion rates similar to those of open between the two minimally invasive approaches (8.1% for robotic and 12.2% for laparoscopy [P = .16] JAMA. 2017; 318[16]:1569-80). “Surgeons in this study were still on their learning curve, and what the results showed was that among surgeons, even with varied experience, robotic surgery was [equal] to laparoscopic surgery in relation to conversion rates and composite margin for cancer specimens,” he said of the ROLARR trial.
That led to the premise for his group’s study. “The hypothesis that we had going into this study was that we are able to get a better composite negative margin with robotic surgery as opposed to laparoscopic surgery, which would then translate into improved cancer survival for our patients,” he said. Like the ROLARR trial, the 2010-2014 National Cancer Database dataset Dr. Hopkins and colleagues used includes a window for the learning curve, he added.
“One of the questions that always comes at us from hospital administration and from insurance companies is whether or not there’s a cost benefit for the patient: What is the value to the patient?” Dr. Hopkins noted. “I’d like to see future studies where we’re looking at this value and, as we decrease our operative time and anesthesia costs, and hopefully some decreased cost in the instrumentation, we start to see some more benefits as we get more facile with robotic surgery.”
Dr. Hopkins has no financial relationships to disclose.
SOURCE: Hopkins B et al. SAGES 2019. Session SS13; abstract S058
CORRECTION 5/14/2109 : The hazard ratio for 5-year overall survival and p-value were updated.
BALTIMORE – A head-to-head comparison of robotic and laparoscopic surgery for locally advanced rectal cancer has found that the operations achieve similar outcomes in terms of composite negative margins, overall survival, and readmissions, but that robotic surgery is associated with lower rates of conversion to open surgery and shorter hospital stays, according to an analysis of cases in the National Cancer Database presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The gold standard for how we’re taking care of our patients, of course, is how we’re doing with the cancer survival, and we found no difference for overall survival in the robotic arm and the laparoscopic arm,” said M. Benjamin Hopkins, MD, of Vanderbilt University, Nashville, Tenn. He reported on a retrospective review of 7,616 operations for rectal adenocarcinoma in the National Cancer Database from 2010 to 2014. The study population included 2,472 (32%) robotic procedures. The hazard ratio for 5-year overall survival was 0.87 (P = .18), Dr. Hopkins noted, with virtually identical Kaplan-Meier survival curves between the two approaches.
The negative margin rates were also similar between the two groups: 93.7% for the robotic patients and 92.9% for the laparoscopic cohort (odds ratio 0.86, P = .23), Dr. Hopkins noted. Readmission rates were 9% and 8%, respectively (odds ratio 1.02, P = .44).
There were two significant differences in outcomes between the two groups: The conversion rate to open surgery for the robotic group “was about half that from what we saw with laparoscopic surgery,” he said – 8% vs. 15%; and “a slightly decreased length of stay” in the robotic group – 6.3 vs. 6.7 days (P less than .001).
Dr. Hopkins noted that the science supporting robotic surgery for rectal resection is still somewhat nascent, pointing to the ROLARR randomized trial, which showed conversion rates similar to those of open between the two minimally invasive approaches (8.1% for robotic and 12.2% for laparoscopy [P = .16] JAMA. 2017; 318[16]:1569-80). “Surgeons in this study were still on their learning curve, and what the results showed was that among surgeons, even with varied experience, robotic surgery was [equal] to laparoscopic surgery in relation to conversion rates and composite margin for cancer specimens,” he said of the ROLARR trial.
That led to the premise for his group’s study. “The hypothesis that we had going into this study was that we are able to get a better composite negative margin with robotic surgery as opposed to laparoscopic surgery, which would then translate into improved cancer survival for our patients,” he said. Like the ROLARR trial, the 2010-2014 National Cancer Database dataset Dr. Hopkins and colleagues used includes a window for the learning curve, he added.
“One of the questions that always comes at us from hospital administration and from insurance companies is whether or not there’s a cost benefit for the patient: What is the value to the patient?” Dr. Hopkins noted. “I’d like to see future studies where we’re looking at this value and, as we decrease our operative time and anesthesia costs, and hopefully some decreased cost in the instrumentation, we start to see some more benefits as we get more facile with robotic surgery.”
Dr. Hopkins has no financial relationships to disclose.
SOURCE: Hopkins B et al. SAGES 2019. Session SS13; abstract S058
CORRECTION 5/14/2109 : The hazard ratio for 5-year overall survival and p-value were updated.
REPORTING FROM SAGES 2019
Machine learning tool may predict LSG outcomes
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
REPORTING FROM SAGES 2019
Laparoscopic magnetic sphincter augmentation may accrue savings over time
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
REPORTING FROM SAGES 2019
Report card may foretell achalasia surgery outcomes
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
REPORTING FROM SAGES 2019
Novel strategies may help curb bariatric SSI
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
REPORTING FROM SAGES 2019
Key clinical point: .
Major findings: The BariWound predictive model had an accuracy of area under the curve of 0.73; wound infection rates decreased from 6% to 1.3% after the change in practice.
Study details: Analysis of 274,187 cases from the 2015 MBSAQIP database; and a retrospective analysis of 333 bariatric cases performed from January 2016 to March 2018 at a single center.
Disclosures: Dr. Dang has no relationships to disclose. Dr. Weber has no disclosures, although coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
Sources: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
Staging tool predicts post-RYGB complications
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
REPORTING FROM SAGES 2019
Key clinical point: The Edmonton Obesity Staging System is predictive of complications after Roux-en-Y gastric bypass surgery.
Major finding: Patients with a score greater than 3 had a threefold greater incidence of complications at 1 year.
Study details: Retrospective chart review of 378 patients who had RYGB at a single center from 2009 through 2015.
Disclosures: Mr. Skulsky has no financial relationships to disclose.
Source: Skulsky SL et al. SAGES 2018, Session SS12.