User login
UPDATE: INFECTIOUS DISEASE
Six recent articles stand out in the field of infectious disease:
- an assessment of outcomes of seriously ill patients who were hospitalized early in the course of the H1N1 influenza epidemic. The authors highlight major differences in the epidemiology of this infection, compared with regular seasonal flu
- an examination of outcomes of pregnant women who developed H1N1 influenza
- an exploration of the use of blunt needles during cesarean delivery to prevent glove perforation
- an evaluation of the utility of prophylactic antibiotics in ostensibly low-risk women undergoing scheduled cesarean delivery
- a look at the timing of antibiotic prophylaxis for cesarean delivery
- a comparison of skin preparation techniques in the prevention of surgical-site infection.
The focus on cesarean delivery in most of these studies seems particularly appropriate, now that this operation has become the most frequently performed major surgical procedure in US hospitals.
H1N1 virus hits hardest during pregnancy and chronic illness
Jain S, Kamimoto L, Bramley AM, et al, for 2009 Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361(20):1935–1944.
This retrospective survey of patients hospitalized for at least 24 hours for treatment of influenza-like illness included 272 patients who were given a diagnosis of H1N1 influenza, based on real-time, reverse-transcriptase, polymerase chain reaction assay. Sixty-seven (25%) of these patients were admitted to an ICU, and 19 (7%) died. All of the patients who died had been treated in an ICU, and two thirds had an underlying medical condition. Three of the deaths involved pregnant women. None of the patients who died received antiviral therapy within 48 hours of the onset of symptoms. Those who died were also less likely to have been vaccinated against seasonal influenza in 2008–2009.
Details of the trial
The 272 patients included in this study sample represented 25% of the total number of patients hospitalized in the United States for treatment of influenza between April and mid-June 2009. They exhibited the following characteristics:
- median age: 21 years
- race and ethnicity: 30% were Hispanic, and 27% were non-Hispanic white
- most common symptoms: fever and cough, although diarrhea or vomiting was reported in 39% of patients
- underlying medical illness: present in 73% (198 patients), including 60% of children and 83% of adults. At least two underlying medical conditions were present in 32% of patients. Asthma was the most common comorbid condition
- pregnancy: 18 patients were pregnant. Four of the pregnant patients also had asthma, and two had diabetes
- obesity: 29% of adults were obese. Morbid obesity was present in 26%. More than 75% of obese and morbidly obese patients had at least one underlying medical illness
- bloodwork at admission: 20% of patients were leukopenic; 37% were anemic; and 14% were thrombocytopenic
- chest film: 40% of patients who underwent chest radiography had findings consistent with pneumonia. Findings included bilateral infiltrates in 66 patients, a unilobar infiltrate in 26, and multilobar infiltrates in two
- antiviral therapy: 75% ultimately received antiviral drugs, with a median time from onset of illness to initiation of therapy of 3 days (range, 0–29 days). Only 39% received antiviral therapy within 48 hours of the onset of symptoms
- antibiotic therapy: 79% of patients received antibiotics for presumed superimposed bacterial infection. The most commonly used antibiotics were ceftriaxone, azithromycin, vancomycin, and levofloxacin.
Study offers 4 useful lessons
The study by Jain and colleagues offers clinically applicable lessons:
- it reinforces the point that children and young adults, including pregnant women, are at increased risk of serious morbidity and mortality
- it demonstrates that most seriously affected patients have at least one underlying medical condition, such as asthma
- it highlights the importance of pregnancy and morbid obesity as major conditions that contribute to serious complications from influenza. The 7% prevalence of pregnant patients is significantly higher than the 1% prevalence that would typically be expected with seasonal influenza. Similarly, the 26% prevalence of morbid obesity greatly exceeds the estimated 5% prevalence in the adult US population
- it confirms the importance of treating patients early in the course of their illness with antiviral drugs such as oseltamivir. Notably, none of the patients who died received treatment within 48 hours of the onset of illness, when the drugs are most likely to be effective.
How to treat H1N1 influenza
The vast majority of strains of the 2009 H1N1 virus are susceptible to oseltamivir and zanamivir, but essentially all strains are resistant to amantadine and rimantadine.1 Therefore, all individuals who are hospitalized should be treated with one of two regimens:
- oseltamivir, 75 mg orally, twice daily for at least 5 days
- zanamivir, 10 mg by inhalation, twice daily for at least 5 days.
These same regimens should be used for outpatients who are at high risk of complications.
Ideally, antiviral treatment should be administered within 48 hours of the onset of symptoms, but do not withhold treatment even if more than 48 hours have elapsed since the onset of illness.2,3
Both oseltamivir and zanamivir are also effective for prevention of infection in susceptible patients who have been exposed to H1N1 influenza. The appropriate dosage of oseltamivir for prophylaxis is 75 mg orally once daily for 10 days. The corresponding dosage of zanamivir is 10 mg by inhalation once daily for 10 days.1
The most effective method of prophylaxis, of course, is vaccination with the new H1N1 vaccine.4 There are two forms of the vaccine—a live virus nasal vaccine and an inactivated vaccine for intramuscular administration. Pregnant women should receive only the inactivated vaccine.
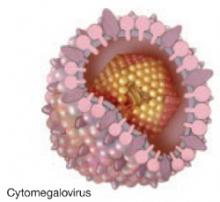
The key reservoirs of all influenza A viruses are migrating waterfowl, pigs, and humans. The current H1N1 strain of virus contains eight unique RNA segments that are a mixture of components from avian, pig, and human influenza viruses.2 The pandemic resulting from this virus is unusual because the continent of origin was North America (Mexico) rather than Asia, the season of origin was spring rather than fall, and the patients at greatest risk of dying have been children and young adults rather than infants and the elderly.3
Women who are pregnant or planning to become pregnant should be vaccinated against H1N1 influenza. Use the inactivated virus if a woman is already pregnant.
After exposure to H1N1 influenza, unvaccinated pregnant women and other patients at high risk of developing the virus should be given oseltamivir or zanamivir prophylactically, using the dosage and route of administration described above for prophylaxis.
Pregnant women and other high-risk patients who exhibit symptoms of H1N1 influenza should be given oseltamivir or zanamivir, using the dosage and route of administration described above for treatment, ideally within 48 hours of the onset of symptoms.
For pregnant and postpartum patients, base treatment of H1N1 flu on symptoms, not rapid tests
Louie JK, Acosta M, Jamieson DJ, et al. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362(1):27–35.
Louie and coworkers describe the outcome of a statewide surveillance program by the California Department of Public Health. They reviewed the medical records of 94 pregnant women, eight women who were within the first 2 weeks postpartum, and 137 nonpregnant women of reproductive age who were hospitalized with confirmed 2009 H1N1 influenza between April 23 and August 11, 2009.
Eighteen pregnant women and four postpartum patients (22%) required intensive care, and 16 (73%) of these women had to be ventilated mechanically. Of the 18 pregnant women who required treatment in the ICU, 12 delivered in the hospital, and four underwent emergent cesarean delivery in the ICU.
Eight (8%) of the 102 pregnant and postpartum patients died. None of these eight women received antiviral therapy within 48 hours of the onset of symptoms. In fact, for pregnant and postpartum patients, a delay in administration of antiviral therapy beyond 48 hours after the onset of symptoms produced a 4.3 relative risk of death (95% confidence interval [CI], 1.4–13.7), compared with patients who were treated early in the course of their infection.
Details of the trial
The women in this trial had the following characteristics:
- gestational age: five (5%) of the 94 pregnant women were in the first trimester, 35 (37%) were in the second trimester, and 54 (57%) were in the third trimester
- underlying conditions were present in 34% of the pregnant and postpartum women and 60% of nonpregnant women. These conditions placed them at increased risk of complications from influenza. The most common underlying condition was asthma
- antiviral therapy was administered to approximately 80% of both pregnant and nonpregnant women. However, only 50% of pregnant women and 34% of nonpregnant women received treatment within 48 hours of the onset of symptoms
- antibiotic therapy was given to 45% of pregnant women and 58% of nonpregnant women for presumed secondary bacterial infection
- false-negative test results: 153 women underwent rapid tests for influenza, 38% of which were falsely negative.
Treat pregnant patients expediently
This article is an excellent complement to the study by Jain and colleagues described on page 37. It strikingly illustrates the heightened risk of morbidity and mortality that pregnant women face when they develop H1N1 influenza. Louie and coworkers documented an influenza-specific mortality ratio (maternal deaths for every 100,000 live births) of 4.3. They also provide clear evidence of the perils of relying on rapid diagnostic tests and withholding antiviral treatment if the rapid test is negative. In their series, 38% of rapid tests were falsely negative. In pregnant women, when antiviral therapy was delayed more than 48 hours, the relative risk of death was 4.3, compared with patients who were treated within 48 hours of the onset of symptoms.
If there is a clinical suspicion of influenza in a pregnant or postpartum patient, treat her immediately with one of the antiviral regimens outlined on page 38—regardless of the outcome of the rapid test for influenza.
Blunt needles reduce needle sticks during cesarean delivery
Sullivan S, Williamson B, Wilson LK, Korde JE, Soper D. Blunt needles for reduction of needlestick injuries during cesarean delivery. Obstet Gynecol. 2009;114 (2 Pt 1):211–216.
Using glove perforation as a proxy for needlestick injuries, Sullivan and colleagues compared blunt needles with sharp needles during cesarean delivery. Ninety-seven women had all anatomic layers reapproximated using blunt needles, and 97 had them reapproximated using sharp needles. The overall glove perforation rate was 12.3%. For sharp needles, the perforation rate was 17.5%, and for blunt needles it was 7.2% (relative risk [RR], 0.66; 95% CI, 0.49–0.89). The key protective effect of the blunt needles was confined to the assistant surgeon (RR, 0.54; 95% CI, 0.41–0.71). The RR for glove perforation involving the primary surgeon was 0.8 (95% CI, 0.53–1.2).
Details of the trial
Glove type, number of gloves, needle size, and type and gauge of suture material were left to the discretion of the surgeon. Glove perforations were identified by filling the gloves with 1,000 mL of water and applying pressure to the palm and each finger. The secondary endpoint of the study was physician satisfaction with the needle. Primary and assistant surgeons reported comparable levels of dissatisfaction with blunt needles, compared with sharp needles (P < .001). However, 92% of primary surgeons and 93% of assistant surgeons rated the blunt needles as at least “acceptable” for use.
Needle stick has led to hepatitis B transmission
Earlier studies reported a rate of glove perforation of 20% to 26% during open abdominal procedures. In an investigation at our center, we noted glove perforation in 13% of cesarean deliveries.5 In this and another investigation, the frequency of perforation did not vary with the level of training of the surgeon or time of day of the procedure.5,6 The most common sites of perforation were the thumb, index finger, and middle finger of the non-dominant hand. The most common mechanism of injury was handling the needle with the operator’s gloved hand rather than with an instrument.
Double-gloving significantly reduces the risk of injury to the inner glove and, subsequently, to the surgeon’s skin. (Note: Double-gloving does not decrease tactile sensation or increase the risk of mishap.6)
The study by Sullivan and colleagues demonstrates that use of blunt needles offers an additional measure of protection against a penetrating injury to the surgeon’s bare skin. Although no surgeon has yet contracted HIV infection from a surgical needle, the transmission of hepatitis B via contaminated surgical needle has been well documented.
Prudence dictates that we use all proven measures to prevent intraoperative blood exposure. Use of blunt needles should be added to interventions such as double-gloving and use of a neutral zone in which to pass sharp objects.
Prophylactic antibiotics reduce postcesarean infection, even in low-risk women
Dinsmoor MJ, Gilbert S, Landon MB, et al, for Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Perioperative antibiotic prophylaxis for nonlaboring cesarean delivery. Obstet Gynecol. 2009;114(4):752–756.
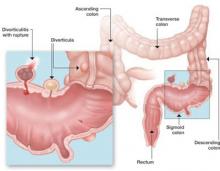
Infection is the most common postoperative complication of cesarean delivery, now the most frequently performed major operation in America. The principal infection is endometritis, followed by wound infection and urinary tract infection. The frequency of wound infection is on the rise because of the steadily increasing prevalence of obesity in the obstetric population.
Dinsmoor and coworkers conducted this secondary analysis using data from an earlier observational study of 9,432 women who underwent cesarean delivery before the onset of labor. Of these women, 6,006 (64%) received antibiotic prophylaxis.
Women treated prophylactically had a significantly lower rate of endometritis (adjusted odds ratio [OR], 0.40; 95% CI, 0.28–0.59) and of wound infection (adjusted OR, 0.49; 95% CI, 0.28–0.86). The frequency of other infection-related complications was not significantly reduced (adjusted OR, 0.39; 95% CI, 0.13–1.12).
Overall, the size of the effect for endometritis was small; endometritis developed in 2.0% of women in the group that received prophylaxis and 2.6% of women in the group that did not. The size of the effect was even smaller for wound infection.
In this uncontrolled series, 113 patients had to be treated to prevent one case of endometritis or wound infection.
Details of the trial
The original observational study from which this analysis derives was performed by the Maternal-Fetal Medicine Units Network at 13 centers in 1999–2000. The choice of antibiotics and the timing of administration were left to the discretion of the attending physician.
Principal endpoints were the occurrence of postoperative endometritis and wound infection. Secondary endpoints were less common infection-related complications such as maternal sepsis, fascial dehiscence or evisceration, necrotizing fasciitis, pelvic abscess, and septic pelvic vein thrombophlebitis.
Of the women who were given prophylactic antibiotics, 88% received only a cephalosporin, 7% received only a broad-spectrum penicillin, and 6% received other regimens. Approximately 1% of patients received more than one antibiotic for prophylaxis.
Averting infection pays dividends
More than 90% of patients who have endometritis respond promptly to broad-spectrum antibiotic therapy. However, some women with postcesarean endometritis develop serious complications such as septic shock, septic pelvic vein thrombophlebitis, and pelvic abscess.
Treatment of wound infection is not so straightforward as treatment of endometritis. Wound infections may well require surgical intervention to drain an incisional abscess. They also necessitate a change in antibiotic therapy, and they are one of the two most important risk factors for fascial dehiscence and intestinal evisceration.
Multiple studies have confirmed that antibiotic prophylaxis significantly reduces the risk of endometritis and wound infection in women who undergo cesarean after the start of labor, with or without ruptured membranes.7,8 Recent publications have also demonstrated that prophylaxis before the start of surgery offers a greater protective effect than administration after the infant’s umbilical cord is clamped.9,10 Other investigations have demonstrated that broader-spectrum prophylaxis further improves outcomes in women undergoing cesarean delivery.11,12
Antibiotic prophylaxis reduces the frequency of postcesarean endometritis and wound infection, even in very low-risk patients. I strongly support the use of prophylactic antibiotics in all women undergoing cesarean delivery. I believe that the best available evidence supports the use of cefazolin (1 g) plus azithromycin (500 mg), administered intravenously before the start of surgery.9-12
Administer antibiotics before making the incision for greatest effectiveness
Owens SM, Brozanski BS, Meyn LA, Wisenfeld HC. Antimicrobial prophylaxis for cesarean delivery before skin incision. Obstet Gynecol. 2009;114(3):573–579.
In this retrospective investigation, Owens and colleagues compared antibiotic prophylaxis in two groups of women undergoing cesarean delivery:
- 4,229 women who received antibiotics after the infant’s umbilical cord was clamped, from July 2002 to November 2004 (Group 1)
- 4,781 women who received antibiotics before the skin was incised, from June 2005 to August 2007 (Group 2).
Both scheduled and unscheduled cesarean deliveries were included, as were women who received antibiotics intrapartum for group B streptococcus prophylaxis and treatment of chorioamnionitis. The most commonly used antibiotic was intravenous cefazolin (1 g).
After excluding women who received group B streptococcus prophylaxis or intrapartum treatment of chorioamnionitis, the authors demonstrated a nearly 50% reduction in the rate of endometritis among women who received antibiotics before surgery (OR, 0.54; 95% CI, 0.38–0.75). They also documented a 30% reduction in the rate of wound infection in these patients (OR, 0.72; 95% CI, 0.55–0.46).
Details of the trial
Principal outcome measures were the rates of maternal endometritis and wound infection and rates of proven and presumed neonatal infection. The mean age and racial distribution were similar in the two groups, but the percentage of patients treated on a resident teaching service was lower in Group 2 (14.9% vs. 18.9%; P < .001). The two groups did not differ in mean body mass index or in the percentage of patients who were in labor before surgery. Colonization with group B streptococcus was more common in Group 2 (24.4% vs. 22.2%; P = .5). However, chorioamnionitis was less prevalent in Group 2 (5.6% vs. 10.3%; P < .001).
The rates of culture-proven neonatal infection within the first 3 days of life (early-onset infection) were similar between groups (1.3% in Group 1 vs. 0.7% in Group 2). Culture-proven late-onset neonatal infection was less common in Group 2 (1.8% vs. 5.7%; P < .001). The groups did not differ in the proportion of newborns treated for presumed infection (24.1% in Group 1 vs. 22.2% in Group 2).
Plentiful data confirm the superiority of preoperative administration
Endometritis is the most common postoperative complication associated with cesarean delivery. Wound infection is less common but more likely to lead to prolonged postoperative morbidity and extended hospitalization. Reducing both of these complications is a critical clinical objective.
Virtually without exception, every investigation has confirmed that prophylactic antibiotics reduce the frequency of postcesarean endometritis and, usually, wound infection as well. One dose of a given antibiotic is clearly as effective as multiple doses.
Classic animal investigations by Burke demonstrated that prophylaxis was most effective when antibiotics were present in tissue prior to the surgical incision.13 Nevertheless, early investigators in obstetrics argued that preoperative exposure to antibiotics increased the likelihood that the neonate would require an evaluation for sepsis and that delaying antibiotics until after cord clamping did not compromise the effectiveness of prophylaxis.14,15
Sullivan and colleagues were the first authors to successfully challenge this dictum.9 In a well-designed investigation, they demonstrated that preoperative administration of antibiotics significantly reduces the frequency of endometritis (RR, 0.22) but not wound infection, and does not increase the need for neonatal sepsis evaluation. Kaimel and coworkers later confirmed these findings,16 and this study by Owen and associates offers additional proof of the effectiveness and safety of preoperative antibiotic administration.
I offer only one addendum to the conclusions presented by Owen and colleagues. Two recent investigations from the University of Alabama conclusively demonstrate that, by extending the spectrum of antibiotic coverage by combining azithromycin and cefazolin, we can further reduce postcesarean endometritis and wound infection.11,17 Accordingly, at our center, we now administer both intravenous (IV) azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Antibiotic prophylaxis reduces the rates of postcesarean endometritis and wound infection, and preoperative administration is superior to administration after cord clamping. Preoperative administration is also safe for the neonate.
Administer IV azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Chlorhexidine solutions are superior to povidone-iodine for surgical-site antisepsis
Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
This report is an excellent complement to the two studies discussed above, which focused on systemic antibiotic prophylaxis for the prevention of postcesarean infection. Here, Darouiche and colleagues conducted a randomized, prospective, unblinded, multi-center comparison of two skin preparations to prevent surgical-site infection:
- 2% chlorhexidine gluconate and 70% isopropyl alcohol (409 patients)
- 10% povidone-iodine solution (440 patients).
Participants underwent a variety of abdominal and nonabdominal (thoracic, gynecologic, and urologic) procedures. All patients received systemic antibiotic prophylaxis within 1 hour before the start of surgery.
The primary outcome measure was the occurrence of any surgical-site infection up to 30 days after surgery. This rate was lower among patients who received chlorhexidine-alcohol skin preparations than among those who received povidone-iodine (9.5% vs. 16.1%; P = .004).
Secondary endpoints were specific types of infection:
- superficial incisional infection (skin and subcutaneous tissue): lower among patients receiving chlorhexidine-alcohol (4.2% vs. 8.6%; P = .008)
- deep incisional infection (involving fascia and muscle): lower among patients receiving chlorhexidine-alcohol (1% vs. 3%; P = .05)
- organ-space infection (any organ or space other than the body wall): no significant difference between women treated with chlorhexidine-alcohol and those treated with povidone-iodine.
Seventeen patients would need to be treated with chlorhexidine-alcohol to prevent one surgical-site infection.
Chlorhexidine has a solid track record
The 41% reduction in the rate of surgical-site infection with chlorhexidine-alcohol (RR, 0.59; 95% CI, 0.41–0.85) is consistent with a 49% reduction in the risk of vascular catheter-related bacteremia using the same formulation.18 The findings are also consistent with a recent report showing that chlorhexidine was more effective than iodine-containing solutions in reducing bacterial concentration in the operative field in women undergoing vaginal hysterectomy.19
Darouiche and coworkers suggest that chlorhexidine is more effective because it has a more rapid onset of action and greater and more persistent antibacterial activity despite exposure to body fluids. Quite appropriately, they indicate that the solution used in their study is flammable, but they observed no adverse effects in a large sample of patients undergoing a variety of procedures.
I strongly recommend that chlorhexidine be used for all surgical skin preparation in obstetric and gynecologic patients. this intervention, along with consistent use of systemic antibiotic prophylaxis, should be highly effective in reducing the risk of superficial and deep abdominal wound infection.
1. Antiviral drugs for influenza. The Medical Letter. 2009;51(1325):89-92.
2. Wenzel RP, Edmond MB. Preparing for 2009 H1N1 influenza. N Engl J Med. 2009;361(20):1991-1993.
3. Perez-Padilla R, Rosa-Zambori D, deLeon SP, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361(7):680-689.
4. H1N1 vaccine for prevention of pandemic influenza. The Medical Letter. 2009;51(1322):77-78.
5. Chapman S, Duff P. Frequency of glove perforations and subsequent blood contact in association with selected obstetric surgical procedures. Am J Obstet Gynecol. 1993;168(5):1354-1357.
6. Lancaster C, Duff P. Single versus double-gloving for obstetric and gynecologic procedures. Am J Obstet Gynecol. 2007;196(5):e36-e37.
7. Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. Cochrane Database of Systematic Reviews. 2002;(3):CD000933.-doi:10/1002/14651858.
8. Prophylactic antibiotics in labor and delivery. ACOG Practice Bulletin No. 47. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2003;102(4):875-882.
9. Sullivan SA, Smith T, Chang F, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized controlled trial. Am J Obstet Gynecol. 2007;196(5):455.e1-e5.
10. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a metaanalysis. Am J Obstet Gynecol. 2008;199(3):301.e1-e6.
11. Tita ATN, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111(1):51-56.
12. Tita AT, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199(3):303.e1-e3.
13. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168.
14. Gordon HR, Phelps D, Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before and after cord clamping. Obstet Gynecol. 1979;53(2):151-156.
15. Cunningham FG, Leveno KJ, DePalma RT, Roark M, Rosenfeld CR. Perioperative antimicrobials for cesarean delivery: before or after cord clamping? Obstet Gynecol. 1983;62(2):151-154.
16. Kaimal AJ, Zlatnik MG, Chang YW, et al. Effect of a change in policy regarding the timing of prophylactic antibiotics on the rate of postcesarean delivery surgical-site infections. Am J Obstet Gynecol. 2008;199(3):310.e1-e5.
17. Tita AT, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systemic review. Obstet Gynecol. 2009;113(3):675-682.
18. Chaiyakunapruk N, Veerstra DI, Lipsky BA, Saint S. Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med. 2002;136(11):792-801.
19. Culligan PJ, Kubik K, Murphy M, Blackwell L, Snyder J. A randomized trial that compared povidone iodine and chlorhexidine as antiseptics for vaginal hysterectomy. Am J Obstet Gynecol. 2005;192(2):422-425.
Six recent articles stand out in the field of infectious disease:
- an assessment of outcomes of seriously ill patients who were hospitalized early in the course of the H1N1 influenza epidemic. The authors highlight major differences in the epidemiology of this infection, compared with regular seasonal flu
- an examination of outcomes of pregnant women who developed H1N1 influenza
- an exploration of the use of blunt needles during cesarean delivery to prevent glove perforation
- an evaluation of the utility of prophylactic antibiotics in ostensibly low-risk women undergoing scheduled cesarean delivery
- a look at the timing of antibiotic prophylaxis for cesarean delivery
- a comparison of skin preparation techniques in the prevention of surgical-site infection.
The focus on cesarean delivery in most of these studies seems particularly appropriate, now that this operation has become the most frequently performed major surgical procedure in US hospitals.
H1N1 virus hits hardest during pregnancy and chronic illness
Jain S, Kamimoto L, Bramley AM, et al, for 2009 Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361(20):1935–1944.
This retrospective survey of patients hospitalized for at least 24 hours for treatment of influenza-like illness included 272 patients who were given a diagnosis of H1N1 influenza, based on real-time, reverse-transcriptase, polymerase chain reaction assay. Sixty-seven (25%) of these patients were admitted to an ICU, and 19 (7%) died. All of the patients who died had been treated in an ICU, and two thirds had an underlying medical condition. Three of the deaths involved pregnant women. None of the patients who died received antiviral therapy within 48 hours of the onset of symptoms. Those who died were also less likely to have been vaccinated against seasonal influenza in 2008–2009.
Details of the trial
The 272 patients included in this study sample represented 25% of the total number of patients hospitalized in the United States for treatment of influenza between April and mid-June 2009. They exhibited the following characteristics:
- median age: 21 years
- race and ethnicity: 30% were Hispanic, and 27% were non-Hispanic white
- most common symptoms: fever and cough, although diarrhea or vomiting was reported in 39% of patients
- underlying medical illness: present in 73% (198 patients), including 60% of children and 83% of adults. At least two underlying medical conditions were present in 32% of patients. Asthma was the most common comorbid condition
- pregnancy: 18 patients were pregnant. Four of the pregnant patients also had asthma, and two had diabetes
- obesity: 29% of adults were obese. Morbid obesity was present in 26%. More than 75% of obese and morbidly obese patients had at least one underlying medical illness
- bloodwork at admission: 20% of patients were leukopenic; 37% were anemic; and 14% were thrombocytopenic
- chest film: 40% of patients who underwent chest radiography had findings consistent with pneumonia. Findings included bilateral infiltrates in 66 patients, a unilobar infiltrate in 26, and multilobar infiltrates in two
- antiviral therapy: 75% ultimately received antiviral drugs, with a median time from onset of illness to initiation of therapy of 3 days (range, 0–29 days). Only 39% received antiviral therapy within 48 hours of the onset of symptoms
- antibiotic therapy: 79% of patients received antibiotics for presumed superimposed bacterial infection. The most commonly used antibiotics were ceftriaxone, azithromycin, vancomycin, and levofloxacin.
Study offers 4 useful lessons
The study by Jain and colleagues offers clinically applicable lessons:
- it reinforces the point that children and young adults, including pregnant women, are at increased risk of serious morbidity and mortality
- it demonstrates that most seriously affected patients have at least one underlying medical condition, such as asthma
- it highlights the importance of pregnancy and morbid obesity as major conditions that contribute to serious complications from influenza. The 7% prevalence of pregnant patients is significantly higher than the 1% prevalence that would typically be expected with seasonal influenza. Similarly, the 26% prevalence of morbid obesity greatly exceeds the estimated 5% prevalence in the adult US population
- it confirms the importance of treating patients early in the course of their illness with antiviral drugs such as oseltamivir. Notably, none of the patients who died received treatment within 48 hours of the onset of illness, when the drugs are most likely to be effective.
How to treat H1N1 influenza
The vast majority of strains of the 2009 H1N1 virus are susceptible to oseltamivir and zanamivir, but essentially all strains are resistant to amantadine and rimantadine.1 Therefore, all individuals who are hospitalized should be treated with one of two regimens:
- oseltamivir, 75 mg orally, twice daily for at least 5 days
- zanamivir, 10 mg by inhalation, twice daily for at least 5 days.
These same regimens should be used for outpatients who are at high risk of complications.
Ideally, antiviral treatment should be administered within 48 hours of the onset of symptoms, but do not withhold treatment even if more than 48 hours have elapsed since the onset of illness.2,3
Both oseltamivir and zanamivir are also effective for prevention of infection in susceptible patients who have been exposed to H1N1 influenza. The appropriate dosage of oseltamivir for prophylaxis is 75 mg orally once daily for 10 days. The corresponding dosage of zanamivir is 10 mg by inhalation once daily for 10 days.1
The most effective method of prophylaxis, of course, is vaccination with the new H1N1 vaccine.4 There are two forms of the vaccine—a live virus nasal vaccine and an inactivated vaccine for intramuscular administration. Pregnant women should receive only the inactivated vaccine.
The key reservoirs of all influenza A viruses are migrating waterfowl, pigs, and humans. The current H1N1 strain of virus contains eight unique RNA segments that are a mixture of components from avian, pig, and human influenza viruses.2 The pandemic resulting from this virus is unusual because the continent of origin was North America (Mexico) rather than Asia, the season of origin was spring rather than fall, and the patients at greatest risk of dying have been children and young adults rather than infants and the elderly.3
Women who are pregnant or planning to become pregnant should be vaccinated against H1N1 influenza. Use the inactivated virus if a woman is already pregnant.
After exposure to H1N1 influenza, unvaccinated pregnant women and other patients at high risk of developing the virus should be given oseltamivir or zanamivir prophylactically, using the dosage and route of administration described above for prophylaxis.
Pregnant women and other high-risk patients who exhibit symptoms of H1N1 influenza should be given oseltamivir or zanamivir, using the dosage and route of administration described above for treatment, ideally within 48 hours of the onset of symptoms.
For pregnant and postpartum patients, base treatment of H1N1 flu on symptoms, not rapid tests
Louie JK, Acosta M, Jamieson DJ, et al. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362(1):27–35.
Louie and coworkers describe the outcome of a statewide surveillance program by the California Department of Public Health. They reviewed the medical records of 94 pregnant women, eight women who were within the first 2 weeks postpartum, and 137 nonpregnant women of reproductive age who were hospitalized with confirmed 2009 H1N1 influenza between April 23 and August 11, 2009.
Eighteen pregnant women and four postpartum patients (22%) required intensive care, and 16 (73%) of these women had to be ventilated mechanically. Of the 18 pregnant women who required treatment in the ICU, 12 delivered in the hospital, and four underwent emergent cesarean delivery in the ICU.
Eight (8%) of the 102 pregnant and postpartum patients died. None of these eight women received antiviral therapy within 48 hours of the onset of symptoms. In fact, for pregnant and postpartum patients, a delay in administration of antiviral therapy beyond 48 hours after the onset of symptoms produced a 4.3 relative risk of death (95% confidence interval [CI], 1.4–13.7), compared with patients who were treated early in the course of their infection.
Details of the trial
The women in this trial had the following characteristics:
- gestational age: five (5%) of the 94 pregnant women were in the first trimester, 35 (37%) were in the second trimester, and 54 (57%) were in the third trimester
- underlying conditions were present in 34% of the pregnant and postpartum women and 60% of nonpregnant women. These conditions placed them at increased risk of complications from influenza. The most common underlying condition was asthma
- antiviral therapy was administered to approximately 80% of both pregnant and nonpregnant women. However, only 50% of pregnant women and 34% of nonpregnant women received treatment within 48 hours of the onset of symptoms
- antibiotic therapy was given to 45% of pregnant women and 58% of nonpregnant women for presumed secondary bacterial infection
- false-negative test results: 153 women underwent rapid tests for influenza, 38% of which were falsely negative.
Treat pregnant patients expediently
This article is an excellent complement to the study by Jain and colleagues described on page 37. It strikingly illustrates the heightened risk of morbidity and mortality that pregnant women face when they develop H1N1 influenza. Louie and coworkers documented an influenza-specific mortality ratio (maternal deaths for every 100,000 live births) of 4.3. They also provide clear evidence of the perils of relying on rapid diagnostic tests and withholding antiviral treatment if the rapid test is negative. In their series, 38% of rapid tests were falsely negative. In pregnant women, when antiviral therapy was delayed more than 48 hours, the relative risk of death was 4.3, compared with patients who were treated within 48 hours of the onset of symptoms.
If there is a clinical suspicion of influenza in a pregnant or postpartum patient, treat her immediately with one of the antiviral regimens outlined on page 38—regardless of the outcome of the rapid test for influenza.
Blunt needles reduce needle sticks during cesarean delivery
Sullivan S, Williamson B, Wilson LK, Korde JE, Soper D. Blunt needles for reduction of needlestick injuries during cesarean delivery. Obstet Gynecol. 2009;114 (2 Pt 1):211–216.
Using glove perforation as a proxy for needlestick injuries, Sullivan and colleagues compared blunt needles with sharp needles during cesarean delivery. Ninety-seven women had all anatomic layers reapproximated using blunt needles, and 97 had them reapproximated using sharp needles. The overall glove perforation rate was 12.3%. For sharp needles, the perforation rate was 17.5%, and for blunt needles it was 7.2% (relative risk [RR], 0.66; 95% CI, 0.49–0.89). The key protective effect of the blunt needles was confined to the assistant surgeon (RR, 0.54; 95% CI, 0.41–0.71). The RR for glove perforation involving the primary surgeon was 0.8 (95% CI, 0.53–1.2).
Details of the trial
Glove type, number of gloves, needle size, and type and gauge of suture material were left to the discretion of the surgeon. Glove perforations were identified by filling the gloves with 1,000 mL of water and applying pressure to the palm and each finger. The secondary endpoint of the study was physician satisfaction with the needle. Primary and assistant surgeons reported comparable levels of dissatisfaction with blunt needles, compared with sharp needles (P < .001). However, 92% of primary surgeons and 93% of assistant surgeons rated the blunt needles as at least “acceptable” for use.
Needle stick has led to hepatitis B transmission
Earlier studies reported a rate of glove perforation of 20% to 26% during open abdominal procedures. In an investigation at our center, we noted glove perforation in 13% of cesarean deliveries.5 In this and another investigation, the frequency of perforation did not vary with the level of training of the surgeon or time of day of the procedure.5,6 The most common sites of perforation were the thumb, index finger, and middle finger of the non-dominant hand. The most common mechanism of injury was handling the needle with the operator’s gloved hand rather than with an instrument.
Double-gloving significantly reduces the risk of injury to the inner glove and, subsequently, to the surgeon’s skin. (Note: Double-gloving does not decrease tactile sensation or increase the risk of mishap.6)
The study by Sullivan and colleagues demonstrates that use of blunt needles offers an additional measure of protection against a penetrating injury to the surgeon’s bare skin. Although no surgeon has yet contracted HIV infection from a surgical needle, the transmission of hepatitis B via contaminated surgical needle has been well documented.
Prudence dictates that we use all proven measures to prevent intraoperative blood exposure. Use of blunt needles should be added to interventions such as double-gloving and use of a neutral zone in which to pass sharp objects.
Prophylactic antibiotics reduce postcesarean infection, even in low-risk women
Dinsmoor MJ, Gilbert S, Landon MB, et al, for Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Perioperative antibiotic prophylaxis for nonlaboring cesarean delivery. Obstet Gynecol. 2009;114(4):752–756.
Infection is the most common postoperative complication of cesarean delivery, now the most frequently performed major operation in America. The principal infection is endometritis, followed by wound infection and urinary tract infection. The frequency of wound infection is on the rise because of the steadily increasing prevalence of obesity in the obstetric population.
Dinsmoor and coworkers conducted this secondary analysis using data from an earlier observational study of 9,432 women who underwent cesarean delivery before the onset of labor. Of these women, 6,006 (64%) received antibiotic prophylaxis.
Women treated prophylactically had a significantly lower rate of endometritis (adjusted odds ratio [OR], 0.40; 95% CI, 0.28–0.59) and of wound infection (adjusted OR, 0.49; 95% CI, 0.28–0.86). The frequency of other infection-related complications was not significantly reduced (adjusted OR, 0.39; 95% CI, 0.13–1.12).
Overall, the size of the effect for endometritis was small; endometritis developed in 2.0% of women in the group that received prophylaxis and 2.6% of women in the group that did not. The size of the effect was even smaller for wound infection.
In this uncontrolled series, 113 patients had to be treated to prevent one case of endometritis or wound infection.
Details of the trial
The original observational study from which this analysis derives was performed by the Maternal-Fetal Medicine Units Network at 13 centers in 1999–2000. The choice of antibiotics and the timing of administration were left to the discretion of the attending physician.
Principal endpoints were the occurrence of postoperative endometritis and wound infection. Secondary endpoints were less common infection-related complications such as maternal sepsis, fascial dehiscence or evisceration, necrotizing fasciitis, pelvic abscess, and septic pelvic vein thrombophlebitis.
Of the women who were given prophylactic antibiotics, 88% received only a cephalosporin, 7% received only a broad-spectrum penicillin, and 6% received other regimens. Approximately 1% of patients received more than one antibiotic for prophylaxis.
Averting infection pays dividends
More than 90% of patients who have endometritis respond promptly to broad-spectrum antibiotic therapy. However, some women with postcesarean endometritis develop serious complications such as septic shock, septic pelvic vein thrombophlebitis, and pelvic abscess.
Treatment of wound infection is not so straightforward as treatment of endometritis. Wound infections may well require surgical intervention to drain an incisional abscess. They also necessitate a change in antibiotic therapy, and they are one of the two most important risk factors for fascial dehiscence and intestinal evisceration.
Multiple studies have confirmed that antibiotic prophylaxis significantly reduces the risk of endometritis and wound infection in women who undergo cesarean after the start of labor, with or without ruptured membranes.7,8 Recent publications have also demonstrated that prophylaxis before the start of surgery offers a greater protective effect than administration after the infant’s umbilical cord is clamped.9,10 Other investigations have demonstrated that broader-spectrum prophylaxis further improves outcomes in women undergoing cesarean delivery.11,12
Antibiotic prophylaxis reduces the frequency of postcesarean endometritis and wound infection, even in very low-risk patients. I strongly support the use of prophylactic antibiotics in all women undergoing cesarean delivery. I believe that the best available evidence supports the use of cefazolin (1 g) plus azithromycin (500 mg), administered intravenously before the start of surgery.9-12
Administer antibiotics before making the incision for greatest effectiveness
Owens SM, Brozanski BS, Meyn LA, Wisenfeld HC. Antimicrobial prophylaxis for cesarean delivery before skin incision. Obstet Gynecol. 2009;114(3):573–579.
In this retrospective investigation, Owens and colleagues compared antibiotic prophylaxis in two groups of women undergoing cesarean delivery:
- 4,229 women who received antibiotics after the infant’s umbilical cord was clamped, from July 2002 to November 2004 (Group 1)
- 4,781 women who received antibiotics before the skin was incised, from June 2005 to August 2007 (Group 2).
Both scheduled and unscheduled cesarean deliveries were included, as were women who received antibiotics intrapartum for group B streptococcus prophylaxis and treatment of chorioamnionitis. The most commonly used antibiotic was intravenous cefazolin (1 g).
After excluding women who received group B streptococcus prophylaxis or intrapartum treatment of chorioamnionitis, the authors demonstrated a nearly 50% reduction in the rate of endometritis among women who received antibiotics before surgery (OR, 0.54; 95% CI, 0.38–0.75). They also documented a 30% reduction in the rate of wound infection in these patients (OR, 0.72; 95% CI, 0.55–0.46).
Details of the trial
Principal outcome measures were the rates of maternal endometritis and wound infection and rates of proven and presumed neonatal infection. The mean age and racial distribution were similar in the two groups, but the percentage of patients treated on a resident teaching service was lower in Group 2 (14.9% vs. 18.9%; P < .001). The two groups did not differ in mean body mass index or in the percentage of patients who were in labor before surgery. Colonization with group B streptococcus was more common in Group 2 (24.4% vs. 22.2%; P = .5). However, chorioamnionitis was less prevalent in Group 2 (5.6% vs. 10.3%; P < .001).
The rates of culture-proven neonatal infection within the first 3 days of life (early-onset infection) were similar between groups (1.3% in Group 1 vs. 0.7% in Group 2). Culture-proven late-onset neonatal infection was less common in Group 2 (1.8% vs. 5.7%; P < .001). The groups did not differ in the proportion of newborns treated for presumed infection (24.1% in Group 1 vs. 22.2% in Group 2).
Plentiful data confirm the superiority of preoperative administration
Endometritis is the most common postoperative complication associated with cesarean delivery. Wound infection is less common but more likely to lead to prolonged postoperative morbidity and extended hospitalization. Reducing both of these complications is a critical clinical objective.
Virtually without exception, every investigation has confirmed that prophylactic antibiotics reduce the frequency of postcesarean endometritis and, usually, wound infection as well. One dose of a given antibiotic is clearly as effective as multiple doses.
Classic animal investigations by Burke demonstrated that prophylaxis was most effective when antibiotics were present in tissue prior to the surgical incision.13 Nevertheless, early investigators in obstetrics argued that preoperative exposure to antibiotics increased the likelihood that the neonate would require an evaluation for sepsis and that delaying antibiotics until after cord clamping did not compromise the effectiveness of prophylaxis.14,15
Sullivan and colleagues were the first authors to successfully challenge this dictum.9 In a well-designed investigation, they demonstrated that preoperative administration of antibiotics significantly reduces the frequency of endometritis (RR, 0.22) but not wound infection, and does not increase the need for neonatal sepsis evaluation. Kaimel and coworkers later confirmed these findings,16 and this study by Owen and associates offers additional proof of the effectiveness and safety of preoperative antibiotic administration.
I offer only one addendum to the conclusions presented by Owen and colleagues. Two recent investigations from the University of Alabama conclusively demonstrate that, by extending the spectrum of antibiotic coverage by combining azithromycin and cefazolin, we can further reduce postcesarean endometritis and wound infection.11,17 Accordingly, at our center, we now administer both intravenous (IV) azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Antibiotic prophylaxis reduces the rates of postcesarean endometritis and wound infection, and preoperative administration is superior to administration after cord clamping. Preoperative administration is also safe for the neonate.
Administer IV azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Chlorhexidine solutions are superior to povidone-iodine for surgical-site antisepsis
Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
This report is an excellent complement to the two studies discussed above, which focused on systemic antibiotic prophylaxis for the prevention of postcesarean infection. Here, Darouiche and colleagues conducted a randomized, prospective, unblinded, multi-center comparison of two skin preparations to prevent surgical-site infection:
- 2% chlorhexidine gluconate and 70% isopropyl alcohol (409 patients)
- 10% povidone-iodine solution (440 patients).
Participants underwent a variety of abdominal and nonabdominal (thoracic, gynecologic, and urologic) procedures. All patients received systemic antibiotic prophylaxis within 1 hour before the start of surgery.
The primary outcome measure was the occurrence of any surgical-site infection up to 30 days after surgery. This rate was lower among patients who received chlorhexidine-alcohol skin preparations than among those who received povidone-iodine (9.5% vs. 16.1%; P = .004).
Secondary endpoints were specific types of infection:
- superficial incisional infection (skin and subcutaneous tissue): lower among patients receiving chlorhexidine-alcohol (4.2% vs. 8.6%; P = .008)
- deep incisional infection (involving fascia and muscle): lower among patients receiving chlorhexidine-alcohol (1% vs. 3%; P = .05)
- organ-space infection (any organ or space other than the body wall): no significant difference between women treated with chlorhexidine-alcohol and those treated with povidone-iodine.
Seventeen patients would need to be treated with chlorhexidine-alcohol to prevent one surgical-site infection.
Chlorhexidine has a solid track record
The 41% reduction in the rate of surgical-site infection with chlorhexidine-alcohol (RR, 0.59; 95% CI, 0.41–0.85) is consistent with a 49% reduction in the risk of vascular catheter-related bacteremia using the same formulation.18 The findings are also consistent with a recent report showing that chlorhexidine was more effective than iodine-containing solutions in reducing bacterial concentration in the operative field in women undergoing vaginal hysterectomy.19
Darouiche and coworkers suggest that chlorhexidine is more effective because it has a more rapid onset of action and greater and more persistent antibacterial activity despite exposure to body fluids. Quite appropriately, they indicate that the solution used in their study is flammable, but they observed no adverse effects in a large sample of patients undergoing a variety of procedures.
I strongly recommend that chlorhexidine be used for all surgical skin preparation in obstetric and gynecologic patients. this intervention, along with consistent use of systemic antibiotic prophylaxis, should be highly effective in reducing the risk of superficial and deep abdominal wound infection.
Six recent articles stand out in the field of infectious disease:
- an assessment of outcomes of seriously ill patients who were hospitalized early in the course of the H1N1 influenza epidemic. The authors highlight major differences in the epidemiology of this infection, compared with regular seasonal flu
- an examination of outcomes of pregnant women who developed H1N1 influenza
- an exploration of the use of blunt needles during cesarean delivery to prevent glove perforation
- an evaluation of the utility of prophylactic antibiotics in ostensibly low-risk women undergoing scheduled cesarean delivery
- a look at the timing of antibiotic prophylaxis for cesarean delivery
- a comparison of skin preparation techniques in the prevention of surgical-site infection.
The focus on cesarean delivery in most of these studies seems particularly appropriate, now that this operation has become the most frequently performed major surgical procedure in US hospitals.
H1N1 virus hits hardest during pregnancy and chronic illness
Jain S, Kamimoto L, Bramley AM, et al, for 2009 Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361(20):1935–1944.
This retrospective survey of patients hospitalized for at least 24 hours for treatment of influenza-like illness included 272 patients who were given a diagnosis of H1N1 influenza, based on real-time, reverse-transcriptase, polymerase chain reaction assay. Sixty-seven (25%) of these patients were admitted to an ICU, and 19 (7%) died. All of the patients who died had been treated in an ICU, and two thirds had an underlying medical condition. Three of the deaths involved pregnant women. None of the patients who died received antiviral therapy within 48 hours of the onset of symptoms. Those who died were also less likely to have been vaccinated against seasonal influenza in 2008–2009.
Details of the trial
The 272 patients included in this study sample represented 25% of the total number of patients hospitalized in the United States for treatment of influenza between April and mid-June 2009. They exhibited the following characteristics:
- median age: 21 years
- race and ethnicity: 30% were Hispanic, and 27% were non-Hispanic white
- most common symptoms: fever and cough, although diarrhea or vomiting was reported in 39% of patients
- underlying medical illness: present in 73% (198 patients), including 60% of children and 83% of adults. At least two underlying medical conditions were present in 32% of patients. Asthma was the most common comorbid condition
- pregnancy: 18 patients were pregnant. Four of the pregnant patients also had asthma, and two had diabetes
- obesity: 29% of adults were obese. Morbid obesity was present in 26%. More than 75% of obese and morbidly obese patients had at least one underlying medical illness
- bloodwork at admission: 20% of patients were leukopenic; 37% were anemic; and 14% were thrombocytopenic
- chest film: 40% of patients who underwent chest radiography had findings consistent with pneumonia. Findings included bilateral infiltrates in 66 patients, a unilobar infiltrate in 26, and multilobar infiltrates in two
- antiviral therapy: 75% ultimately received antiviral drugs, with a median time from onset of illness to initiation of therapy of 3 days (range, 0–29 days). Only 39% received antiviral therapy within 48 hours of the onset of symptoms
- antibiotic therapy: 79% of patients received antibiotics for presumed superimposed bacterial infection. The most commonly used antibiotics were ceftriaxone, azithromycin, vancomycin, and levofloxacin.
Study offers 4 useful lessons
The study by Jain and colleagues offers clinically applicable lessons:
- it reinforces the point that children and young adults, including pregnant women, are at increased risk of serious morbidity and mortality
- it demonstrates that most seriously affected patients have at least one underlying medical condition, such as asthma
- it highlights the importance of pregnancy and morbid obesity as major conditions that contribute to serious complications from influenza. The 7% prevalence of pregnant patients is significantly higher than the 1% prevalence that would typically be expected with seasonal influenza. Similarly, the 26% prevalence of morbid obesity greatly exceeds the estimated 5% prevalence in the adult US population
- it confirms the importance of treating patients early in the course of their illness with antiviral drugs such as oseltamivir. Notably, none of the patients who died received treatment within 48 hours of the onset of illness, when the drugs are most likely to be effective.
How to treat H1N1 influenza
The vast majority of strains of the 2009 H1N1 virus are susceptible to oseltamivir and zanamivir, but essentially all strains are resistant to amantadine and rimantadine.1 Therefore, all individuals who are hospitalized should be treated with one of two regimens:
- oseltamivir, 75 mg orally, twice daily for at least 5 days
- zanamivir, 10 mg by inhalation, twice daily for at least 5 days.
These same regimens should be used for outpatients who are at high risk of complications.
Ideally, antiviral treatment should be administered within 48 hours of the onset of symptoms, but do not withhold treatment even if more than 48 hours have elapsed since the onset of illness.2,3
Both oseltamivir and zanamivir are also effective for prevention of infection in susceptible patients who have been exposed to H1N1 influenza. The appropriate dosage of oseltamivir for prophylaxis is 75 mg orally once daily for 10 days. The corresponding dosage of zanamivir is 10 mg by inhalation once daily for 10 days.1
The most effective method of prophylaxis, of course, is vaccination with the new H1N1 vaccine.4 There are two forms of the vaccine—a live virus nasal vaccine and an inactivated vaccine for intramuscular administration. Pregnant women should receive only the inactivated vaccine.
The key reservoirs of all influenza A viruses are migrating waterfowl, pigs, and humans. The current H1N1 strain of virus contains eight unique RNA segments that are a mixture of components from avian, pig, and human influenza viruses.2 The pandemic resulting from this virus is unusual because the continent of origin was North America (Mexico) rather than Asia, the season of origin was spring rather than fall, and the patients at greatest risk of dying have been children and young adults rather than infants and the elderly.3
Women who are pregnant or planning to become pregnant should be vaccinated against H1N1 influenza. Use the inactivated virus if a woman is already pregnant.
After exposure to H1N1 influenza, unvaccinated pregnant women and other patients at high risk of developing the virus should be given oseltamivir or zanamivir prophylactically, using the dosage and route of administration described above for prophylaxis.
Pregnant women and other high-risk patients who exhibit symptoms of H1N1 influenza should be given oseltamivir or zanamivir, using the dosage and route of administration described above for treatment, ideally within 48 hours of the onset of symptoms.
For pregnant and postpartum patients, base treatment of H1N1 flu on symptoms, not rapid tests
Louie JK, Acosta M, Jamieson DJ, et al. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362(1):27–35.
Louie and coworkers describe the outcome of a statewide surveillance program by the California Department of Public Health. They reviewed the medical records of 94 pregnant women, eight women who were within the first 2 weeks postpartum, and 137 nonpregnant women of reproductive age who were hospitalized with confirmed 2009 H1N1 influenza between April 23 and August 11, 2009.
Eighteen pregnant women and four postpartum patients (22%) required intensive care, and 16 (73%) of these women had to be ventilated mechanically. Of the 18 pregnant women who required treatment in the ICU, 12 delivered in the hospital, and four underwent emergent cesarean delivery in the ICU.
Eight (8%) of the 102 pregnant and postpartum patients died. None of these eight women received antiviral therapy within 48 hours of the onset of symptoms. In fact, for pregnant and postpartum patients, a delay in administration of antiviral therapy beyond 48 hours after the onset of symptoms produced a 4.3 relative risk of death (95% confidence interval [CI], 1.4–13.7), compared with patients who were treated early in the course of their infection.
Details of the trial
The women in this trial had the following characteristics:
- gestational age: five (5%) of the 94 pregnant women were in the first trimester, 35 (37%) were in the second trimester, and 54 (57%) were in the third trimester
- underlying conditions were present in 34% of the pregnant and postpartum women and 60% of nonpregnant women. These conditions placed them at increased risk of complications from influenza. The most common underlying condition was asthma
- antiviral therapy was administered to approximately 80% of both pregnant and nonpregnant women. However, only 50% of pregnant women and 34% of nonpregnant women received treatment within 48 hours of the onset of symptoms
- antibiotic therapy was given to 45% of pregnant women and 58% of nonpregnant women for presumed secondary bacterial infection
- false-negative test results: 153 women underwent rapid tests for influenza, 38% of which were falsely negative.
Treat pregnant patients expediently
This article is an excellent complement to the study by Jain and colleagues described on page 37. It strikingly illustrates the heightened risk of morbidity and mortality that pregnant women face when they develop H1N1 influenza. Louie and coworkers documented an influenza-specific mortality ratio (maternal deaths for every 100,000 live births) of 4.3. They also provide clear evidence of the perils of relying on rapid diagnostic tests and withholding antiviral treatment if the rapid test is negative. In their series, 38% of rapid tests were falsely negative. In pregnant women, when antiviral therapy was delayed more than 48 hours, the relative risk of death was 4.3, compared with patients who were treated within 48 hours of the onset of symptoms.
If there is a clinical suspicion of influenza in a pregnant or postpartum patient, treat her immediately with one of the antiviral regimens outlined on page 38—regardless of the outcome of the rapid test for influenza.
Blunt needles reduce needle sticks during cesarean delivery
Sullivan S, Williamson B, Wilson LK, Korde JE, Soper D. Blunt needles for reduction of needlestick injuries during cesarean delivery. Obstet Gynecol. 2009;114 (2 Pt 1):211–216.
Using glove perforation as a proxy for needlestick injuries, Sullivan and colleagues compared blunt needles with sharp needles during cesarean delivery. Ninety-seven women had all anatomic layers reapproximated using blunt needles, and 97 had them reapproximated using sharp needles. The overall glove perforation rate was 12.3%. For sharp needles, the perforation rate was 17.5%, and for blunt needles it was 7.2% (relative risk [RR], 0.66; 95% CI, 0.49–0.89). The key protective effect of the blunt needles was confined to the assistant surgeon (RR, 0.54; 95% CI, 0.41–0.71). The RR for glove perforation involving the primary surgeon was 0.8 (95% CI, 0.53–1.2).
Details of the trial
Glove type, number of gloves, needle size, and type and gauge of suture material were left to the discretion of the surgeon. Glove perforations were identified by filling the gloves with 1,000 mL of water and applying pressure to the palm and each finger. The secondary endpoint of the study was physician satisfaction with the needle. Primary and assistant surgeons reported comparable levels of dissatisfaction with blunt needles, compared with sharp needles (P < .001). However, 92% of primary surgeons and 93% of assistant surgeons rated the blunt needles as at least “acceptable” for use.
Needle stick has led to hepatitis B transmission
Earlier studies reported a rate of glove perforation of 20% to 26% during open abdominal procedures. In an investigation at our center, we noted glove perforation in 13% of cesarean deliveries.5 In this and another investigation, the frequency of perforation did not vary with the level of training of the surgeon or time of day of the procedure.5,6 The most common sites of perforation were the thumb, index finger, and middle finger of the non-dominant hand. The most common mechanism of injury was handling the needle with the operator’s gloved hand rather than with an instrument.
Double-gloving significantly reduces the risk of injury to the inner glove and, subsequently, to the surgeon’s skin. (Note: Double-gloving does not decrease tactile sensation or increase the risk of mishap.6)
The study by Sullivan and colleagues demonstrates that use of blunt needles offers an additional measure of protection against a penetrating injury to the surgeon’s bare skin. Although no surgeon has yet contracted HIV infection from a surgical needle, the transmission of hepatitis B via contaminated surgical needle has been well documented.
Prudence dictates that we use all proven measures to prevent intraoperative blood exposure. Use of blunt needles should be added to interventions such as double-gloving and use of a neutral zone in which to pass sharp objects.
Prophylactic antibiotics reduce postcesarean infection, even in low-risk women
Dinsmoor MJ, Gilbert S, Landon MB, et al, for Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Perioperative antibiotic prophylaxis for nonlaboring cesarean delivery. Obstet Gynecol. 2009;114(4):752–756.
Infection is the most common postoperative complication of cesarean delivery, now the most frequently performed major operation in America. The principal infection is endometritis, followed by wound infection and urinary tract infection. The frequency of wound infection is on the rise because of the steadily increasing prevalence of obesity in the obstetric population.
Dinsmoor and coworkers conducted this secondary analysis using data from an earlier observational study of 9,432 women who underwent cesarean delivery before the onset of labor. Of these women, 6,006 (64%) received antibiotic prophylaxis.
Women treated prophylactically had a significantly lower rate of endometritis (adjusted odds ratio [OR], 0.40; 95% CI, 0.28–0.59) and of wound infection (adjusted OR, 0.49; 95% CI, 0.28–0.86). The frequency of other infection-related complications was not significantly reduced (adjusted OR, 0.39; 95% CI, 0.13–1.12).
Overall, the size of the effect for endometritis was small; endometritis developed in 2.0% of women in the group that received prophylaxis and 2.6% of women in the group that did not. The size of the effect was even smaller for wound infection.
In this uncontrolled series, 113 patients had to be treated to prevent one case of endometritis or wound infection.
Details of the trial
The original observational study from which this analysis derives was performed by the Maternal-Fetal Medicine Units Network at 13 centers in 1999–2000. The choice of antibiotics and the timing of administration were left to the discretion of the attending physician.
Principal endpoints were the occurrence of postoperative endometritis and wound infection. Secondary endpoints were less common infection-related complications such as maternal sepsis, fascial dehiscence or evisceration, necrotizing fasciitis, pelvic abscess, and septic pelvic vein thrombophlebitis.
Of the women who were given prophylactic antibiotics, 88% received only a cephalosporin, 7% received only a broad-spectrum penicillin, and 6% received other regimens. Approximately 1% of patients received more than one antibiotic for prophylaxis.
Averting infection pays dividends
More than 90% of patients who have endometritis respond promptly to broad-spectrum antibiotic therapy. However, some women with postcesarean endometritis develop serious complications such as septic shock, septic pelvic vein thrombophlebitis, and pelvic abscess.
Treatment of wound infection is not so straightforward as treatment of endometritis. Wound infections may well require surgical intervention to drain an incisional abscess. They also necessitate a change in antibiotic therapy, and they are one of the two most important risk factors for fascial dehiscence and intestinal evisceration.
Multiple studies have confirmed that antibiotic prophylaxis significantly reduces the risk of endometritis and wound infection in women who undergo cesarean after the start of labor, with or without ruptured membranes.7,8 Recent publications have also demonstrated that prophylaxis before the start of surgery offers a greater protective effect than administration after the infant’s umbilical cord is clamped.9,10 Other investigations have demonstrated that broader-spectrum prophylaxis further improves outcomes in women undergoing cesarean delivery.11,12
Antibiotic prophylaxis reduces the frequency of postcesarean endometritis and wound infection, even in very low-risk patients. I strongly support the use of prophylactic antibiotics in all women undergoing cesarean delivery. I believe that the best available evidence supports the use of cefazolin (1 g) plus azithromycin (500 mg), administered intravenously before the start of surgery.9-12
Administer antibiotics before making the incision for greatest effectiveness
Owens SM, Brozanski BS, Meyn LA, Wisenfeld HC. Antimicrobial prophylaxis for cesarean delivery before skin incision. Obstet Gynecol. 2009;114(3):573–579.
In this retrospective investigation, Owens and colleagues compared antibiotic prophylaxis in two groups of women undergoing cesarean delivery:
- 4,229 women who received antibiotics after the infant’s umbilical cord was clamped, from July 2002 to November 2004 (Group 1)
- 4,781 women who received antibiotics before the skin was incised, from June 2005 to August 2007 (Group 2).
Both scheduled and unscheduled cesarean deliveries were included, as were women who received antibiotics intrapartum for group B streptococcus prophylaxis and treatment of chorioamnionitis. The most commonly used antibiotic was intravenous cefazolin (1 g).
After excluding women who received group B streptococcus prophylaxis or intrapartum treatment of chorioamnionitis, the authors demonstrated a nearly 50% reduction in the rate of endometritis among women who received antibiotics before surgery (OR, 0.54; 95% CI, 0.38–0.75). They also documented a 30% reduction in the rate of wound infection in these patients (OR, 0.72; 95% CI, 0.55–0.46).
Details of the trial
Principal outcome measures were the rates of maternal endometritis and wound infection and rates of proven and presumed neonatal infection. The mean age and racial distribution were similar in the two groups, but the percentage of patients treated on a resident teaching service was lower in Group 2 (14.9% vs. 18.9%; P < .001). The two groups did not differ in mean body mass index or in the percentage of patients who were in labor before surgery. Colonization with group B streptococcus was more common in Group 2 (24.4% vs. 22.2%; P = .5). However, chorioamnionitis was less prevalent in Group 2 (5.6% vs. 10.3%; P < .001).
The rates of culture-proven neonatal infection within the first 3 days of life (early-onset infection) were similar between groups (1.3% in Group 1 vs. 0.7% in Group 2). Culture-proven late-onset neonatal infection was less common in Group 2 (1.8% vs. 5.7%; P < .001). The groups did not differ in the proportion of newborns treated for presumed infection (24.1% in Group 1 vs. 22.2% in Group 2).
Plentiful data confirm the superiority of preoperative administration
Endometritis is the most common postoperative complication associated with cesarean delivery. Wound infection is less common but more likely to lead to prolonged postoperative morbidity and extended hospitalization. Reducing both of these complications is a critical clinical objective.
Virtually without exception, every investigation has confirmed that prophylactic antibiotics reduce the frequency of postcesarean endometritis and, usually, wound infection as well. One dose of a given antibiotic is clearly as effective as multiple doses.
Classic animal investigations by Burke demonstrated that prophylaxis was most effective when antibiotics were present in tissue prior to the surgical incision.13 Nevertheless, early investigators in obstetrics argued that preoperative exposure to antibiotics increased the likelihood that the neonate would require an evaluation for sepsis and that delaying antibiotics until after cord clamping did not compromise the effectiveness of prophylaxis.14,15
Sullivan and colleagues were the first authors to successfully challenge this dictum.9 In a well-designed investigation, they demonstrated that preoperative administration of antibiotics significantly reduces the frequency of endometritis (RR, 0.22) but not wound infection, and does not increase the need for neonatal sepsis evaluation. Kaimel and coworkers later confirmed these findings,16 and this study by Owen and associates offers additional proof of the effectiveness and safety of preoperative antibiotic administration.
I offer only one addendum to the conclusions presented by Owen and colleagues. Two recent investigations from the University of Alabama conclusively demonstrate that, by extending the spectrum of antibiotic coverage by combining azithromycin and cefazolin, we can further reduce postcesarean endometritis and wound infection.11,17 Accordingly, at our center, we now administer both intravenous (IV) azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Antibiotic prophylaxis reduces the rates of postcesarean endometritis and wound infection, and preoperative administration is superior to administration after cord clamping. Preoperative administration is also safe for the neonate.
Administer IV azithromycin (500 mg over 1 hour) and IV cefazolin (1 g) approximately 30 to 60 minutes before the start of surgery.
Chlorhexidine solutions are superior to povidone-iodine for surgical-site antisepsis
Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
This report is an excellent complement to the two studies discussed above, which focused on systemic antibiotic prophylaxis for the prevention of postcesarean infection. Here, Darouiche and colleagues conducted a randomized, prospective, unblinded, multi-center comparison of two skin preparations to prevent surgical-site infection:
- 2% chlorhexidine gluconate and 70% isopropyl alcohol (409 patients)
- 10% povidone-iodine solution (440 patients).
Participants underwent a variety of abdominal and nonabdominal (thoracic, gynecologic, and urologic) procedures. All patients received systemic antibiotic prophylaxis within 1 hour before the start of surgery.
The primary outcome measure was the occurrence of any surgical-site infection up to 30 days after surgery. This rate was lower among patients who received chlorhexidine-alcohol skin preparations than among those who received povidone-iodine (9.5% vs. 16.1%; P = .004).
Secondary endpoints were specific types of infection:
- superficial incisional infection (skin and subcutaneous tissue): lower among patients receiving chlorhexidine-alcohol (4.2% vs. 8.6%; P = .008)
- deep incisional infection (involving fascia and muscle): lower among patients receiving chlorhexidine-alcohol (1% vs. 3%; P = .05)
- organ-space infection (any organ or space other than the body wall): no significant difference between women treated with chlorhexidine-alcohol and those treated with povidone-iodine.
Seventeen patients would need to be treated with chlorhexidine-alcohol to prevent one surgical-site infection.
Chlorhexidine has a solid track record
The 41% reduction in the rate of surgical-site infection with chlorhexidine-alcohol (RR, 0.59; 95% CI, 0.41–0.85) is consistent with a 49% reduction in the risk of vascular catheter-related bacteremia using the same formulation.18 The findings are also consistent with a recent report showing that chlorhexidine was more effective than iodine-containing solutions in reducing bacterial concentration in the operative field in women undergoing vaginal hysterectomy.19
Darouiche and coworkers suggest that chlorhexidine is more effective because it has a more rapid onset of action and greater and more persistent antibacterial activity despite exposure to body fluids. Quite appropriately, they indicate that the solution used in their study is flammable, but they observed no adverse effects in a large sample of patients undergoing a variety of procedures.
I strongly recommend that chlorhexidine be used for all surgical skin preparation in obstetric and gynecologic patients. this intervention, along with consistent use of systemic antibiotic prophylaxis, should be highly effective in reducing the risk of superficial and deep abdominal wound infection.
1. Antiviral drugs for influenza. The Medical Letter. 2009;51(1325):89-92.
2. Wenzel RP, Edmond MB. Preparing for 2009 H1N1 influenza. N Engl J Med. 2009;361(20):1991-1993.
3. Perez-Padilla R, Rosa-Zambori D, deLeon SP, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361(7):680-689.
4. H1N1 vaccine for prevention of pandemic influenza. The Medical Letter. 2009;51(1322):77-78.
5. Chapman S, Duff P. Frequency of glove perforations and subsequent blood contact in association with selected obstetric surgical procedures. Am J Obstet Gynecol. 1993;168(5):1354-1357.
6. Lancaster C, Duff P. Single versus double-gloving for obstetric and gynecologic procedures. Am J Obstet Gynecol. 2007;196(5):e36-e37.
7. Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. Cochrane Database of Systematic Reviews. 2002;(3):CD000933.-doi:10/1002/14651858.
8. Prophylactic antibiotics in labor and delivery. ACOG Practice Bulletin No. 47. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2003;102(4):875-882.
9. Sullivan SA, Smith T, Chang F, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized controlled trial. Am J Obstet Gynecol. 2007;196(5):455.e1-e5.
10. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a metaanalysis. Am J Obstet Gynecol. 2008;199(3):301.e1-e6.
11. Tita ATN, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111(1):51-56.
12. Tita AT, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199(3):303.e1-e3.
13. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168.
14. Gordon HR, Phelps D, Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before and after cord clamping. Obstet Gynecol. 1979;53(2):151-156.
15. Cunningham FG, Leveno KJ, DePalma RT, Roark M, Rosenfeld CR. Perioperative antimicrobials for cesarean delivery: before or after cord clamping? Obstet Gynecol. 1983;62(2):151-154.
16. Kaimal AJ, Zlatnik MG, Chang YW, et al. Effect of a change in policy regarding the timing of prophylactic antibiotics on the rate of postcesarean delivery surgical-site infections. Am J Obstet Gynecol. 2008;199(3):310.e1-e5.
17. Tita AT, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systemic review. Obstet Gynecol. 2009;113(3):675-682.
18. Chaiyakunapruk N, Veerstra DI, Lipsky BA, Saint S. Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med. 2002;136(11):792-801.
19. Culligan PJ, Kubik K, Murphy M, Blackwell L, Snyder J. A randomized trial that compared povidone iodine and chlorhexidine as antiseptics for vaginal hysterectomy. Am J Obstet Gynecol. 2005;192(2):422-425.
1. Antiviral drugs for influenza. The Medical Letter. 2009;51(1325):89-92.
2. Wenzel RP, Edmond MB. Preparing for 2009 H1N1 influenza. N Engl J Med. 2009;361(20):1991-1993.
3. Perez-Padilla R, Rosa-Zambori D, deLeon SP, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361(7):680-689.
4. H1N1 vaccine for prevention of pandemic influenza. The Medical Letter. 2009;51(1322):77-78.
5. Chapman S, Duff P. Frequency of glove perforations and subsequent blood contact in association with selected obstetric surgical procedures. Am J Obstet Gynecol. 1993;168(5):1354-1357.
6. Lancaster C, Duff P. Single versus double-gloving for obstetric and gynecologic procedures. Am J Obstet Gynecol. 2007;196(5):e36-e37.
7. Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. Cochrane Database of Systematic Reviews. 2002;(3):CD000933.-doi:10/1002/14651858.
8. Prophylactic antibiotics in labor and delivery. ACOG Practice Bulletin No. 47. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2003;102(4):875-882.
9. Sullivan SA, Smith T, Chang F, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized controlled trial. Am J Obstet Gynecol. 2007;196(5):455.e1-e5.
10. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a metaanalysis. Am J Obstet Gynecol. 2008;199(3):301.e1-e6.
11. Tita ATN, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111(1):51-56.
12. Tita AT, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199(3):303.e1-e3.
13. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168.
14. Gordon HR, Phelps D, Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before and after cord clamping. Obstet Gynecol. 1979;53(2):151-156.
15. Cunningham FG, Leveno KJ, DePalma RT, Roark M, Rosenfeld CR. Perioperative antimicrobials for cesarean delivery: before or after cord clamping? Obstet Gynecol. 1983;62(2):151-154.
16. Kaimal AJ, Zlatnik MG, Chang YW, et al. Effect of a change in policy regarding the timing of prophylactic antibiotics on the rate of postcesarean delivery surgical-site infections. Am J Obstet Gynecol. 2008;199(3):310.e1-e5.
17. Tita AT, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systemic review. Obstet Gynecol. 2009;113(3):675-682.
18. Chaiyakunapruk N, Veerstra DI, Lipsky BA, Saint S. Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med. 2002;136(11):792-801.
19. Culligan PJ, Kubik K, Murphy M, Blackwell L, Snyder J. A randomized trial that compared povidone iodine and chlorhexidine as antiseptics for vaginal hysterectomy. Am J Obstet Gynecol. 2005;192(2):422-425.
INFECTIOUS DISEASE
Dr. Duff reports no financial relationships relevant to this article.
Four important developments have marked the past year in infectious disease:
- A promising vaccine against cytomegalovirus (CMV) was tested in women of reproductive age
- Extended-spectrum antibiotic prophylaxis proved to be effective in reducing the incidence of wound infection following cesarean delivery
- Investigators developed a simple but effective method to prevent wound complications following repair of a third- or fourth-degree perineal laceration
- The incidence of severe Clostridium difficile-associated diarrhea crept upward, emerging as a threat to pregnant women.
CMV vaccine makes an auspicious debut—but isn’t ready for practice
Pass RF, Zhang C, Evans A, et al. Vaccine prevention of maternal cytomegalovirus infection. N Engl J Med. 2009; 360:1191–1199 [Classification of evidence – Level I].
This Phase-2, randomized, double-blind, placebo-controlled trial of a new cytomegalovirus (CMV) vaccine in women found an overall efficacy rate of 50% (95% confidence interval, 7% to 73%), with no unusually serious reactions among women who were vaccinated. This efficacy rate is disappointing, but it isn’t entirely surprising; even the immune response resulting from natural infection is not fully protective against reactivated infection or recurrent infection with a different strain of virus. Nor is natural immunity completely effective in preventing severe fetal injury in recurrent infection.1
Virus poses greatest risk to pregnant women and their fetuses
CMV is the most common perinatally transmitted infection, affecting 0.6% to 0.7% of infants ( FIGURE 1 ). The greatest risk of fetal injury occurs when the mother develops primary infection during pregnancy, which raises her infant’s risk of infection to 40% to 50%. Of infants delivered to mothers with primary infection, approximately 10% to 15% will be acutely symptomatic at birth.
Clinical manifestations of severe congenital CMV infection include growth restriction, microcephaly, ventriculomegaly, intracranial calcification, chorioretinitis, hearing impairment, hepatitis, and thrombocytopenia.
Because the morbidity and mortality associated with these conditions are alarmingly high, development of a safe, effective vaccine against CMV would be most welcome.2,3
Recurrent or reactivated maternal CMV infection poses a much lower risk to the fetus. Infected infants are rarely symptomatic at birth. Clinical manifestations of infection typically occur later in childhood and include hearing and visual deficits, dental anomalies, and learning or behavioral disorders.2,3
FIGURE 1 Cytomegalovirus
Cytomegalovirus is a member of the herpesvirus family. It is shed intermittently in bodily fluids, without detectable signs and symptoms.
Details of the trial
Women were eligible for the study if they were seronegative for CMV antibody, in good health, 14 to 40 years old, and not pregnant or lactating. Participants received three doses of vaccine or placebo at 0, 1, and 6 months. (The vaccine was composed of CMV envelope glycoprotein B with MF59 adjuvant.) The women were then tested for CMV infection every 3 months for as long as 42 months, using an assay for IgG antibodies directed against viral proteins other than glycoprotein B. Infection was confirmed by viral culture or immuno blotting. The primary endpoint was time until detection of CMV infection.
The vaccine was given to 234 patients, and 230 received placebo. Eighteen infections occurred in the vaccine group, compared with 31 in the placebo group. Vaccinated patients were more likely to remain uninfected during follow-up (p=.02).
One of 81 infants (1%) born to mothers in the vaccinated group had congenital CMV infection, compared with three of 97 (3%) infants born to mothers in the placebo group (p=.41). One infant in the placebo group had severe infection that was evident at birth. The other three infants were asymptomatic at birth and free of sequelae 3 to 5 years later.
The most promising preventive remains experimental
No drug is uniformly effective in treating maternal CMV infection and preventing congenital infection. The most promising intervention for prevention of congenital CMV infection is administration of hyperimmune anti-CMV antibody to the mother. A recent report by Nigro and colleagues4 found this agent to be of great value for both treating and preventing congenital CMV. However, because of limitations in the design of this study, administration of hyperimmune globulin still must be regarded as experimental.3
Key questions remain unanswered
The goal of a large-scale vaccination program is to ensure that women enter reproductive age with preexisting immunity to infection. In that light, the study by Pass and colleagues is only partially encouraging. Despite vaccination, 18 infections occurred, and the follow-up period was relatively short. We do not yet know whether the protective effect of the vaccine will be of extended duration. Moreover, one vaccinated mother delivered an infant who had congenital CMV infection.
Until additional trials of the CMV vaccine are reported, we must focus on helping patients prevent acquisition of infection during pregnancy. Preventive measures include:
- safe sex practices
- use of CMV-negative blood for transfusion to pregnant women and their fetuses
- strict hand-washing procedures for mothers when changing diapers and caring for young children.
Extended-spectrum antibiotics reduce the rate of postcesarean wound infection
Tita ATN, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199:303e.1–303e.3 [Classification of evidence – Level II].
This prospective study describes surveillance for postcesarean wound infection during three different periods at the University of Alabama:
- 1992–1996, during which patients undergoing cesarean delivery routinely received prophylaxis with a first- or second-generation cephalosporin. Overall incidence of wound infection: 3.1%
- 1997–1999, during which patients were randomized to standard prophylaxis with cefazolin or to cefazolin plus either intravenous (IV) doxycycline or oral azithromycin. Overall incidence of wound infection: 2.4%
- 2001–2006, during which patients routinely received IV cefazolin plus IV azithromycin. Overall incidence of wound infection: 1.3%.
In each time period, the prophylactic antibiotics were administered after the infant’s umbilical cord was clamped. The p value for test of trend was highly significant (p<.002). The same significant trend was noted when superficial and deep wound infections were examined separately.
This evidence is a “practice changer”
For almost 20 years, the standard of practice has been to routinely administer prophylactic antibiotics to all women having cesarean delivery. Essentially, every published study has demonstrated a highly significant reduction in the frequency of postcesarean endometritis when patients received prophylaxis. Multiple studies also confirmed that a more limited-spectrum cephalosporin was as effective as an extended-spectrum agent in reducing the frequency of endometritis.5
Many of these earlier reports were unable to demonstrate a consistently beneficial effect of prophylaxis on the incidence of postoperative wound infection. That is why the present study is of such interest and importance. Tita and colleagues previously demonstrated an improved effect of extended-spectrum prophylaxis on the incidence of postcesarean endometritis.6 Now they have confirmed that this method of prophylaxis is also effective in lowering the rate of surgical wound infection.
Wound infections are more troublesome than endometritis
Wound infections—either incisional abscess or cellulitis—are even more likely than post-cesarean endometritis to prolong a patient’s postoperative stay and create the potential for severe morbidity, such as fascial dehiscence and necrotizing fasciitis. With the increasing prevalence of obesity in the US population, wound infections are likely to become even more frequent.
These infections typically are caused by aerobic streptococci and staphylococci from the skin, combined with coliform organisms and anaerobes from the pelvic flora. Incisional abscesses require surgical drainage; cellulitis usually will respond to a change in antibiotic therapy that specifically targets streptococci and staphylococci, along with the coliforms and anaerobes.
I strongly recommend routine prophylaxis with IV cefazolin (1 g) plus azithromycin (500 mg) in all women having cesarean delivery. Moreover, in view of several recent investigations that evaluated the timing of antibiotic administration (immediately preoperative versus after the umbilical cord is clamped), I recommend that extended-spectrum prophylaxis be given before the start of surgery.7
Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized control trial. Obstet Gynecol. 2008;111:1268–1273 [Classification of evidence – Level I].
Take note of this prospective, randomized, placebo-controlled trial of prophylactic antibiotics in women who sustained a third-or fourth-degree perineal laceration during vaginal delivery: It is the first, and only, well-designed trial of antibiotic prophylaxis for prevention of complications after repair of a major perineal laceration. Among patients in the study, 8% who received antibiotics developed a wound complication, compared with 24% of patients who received placebo, a statistically and clinically significant difference.
Details of the study
Eighty-three women received placebo, and 64 received a single IV dose of either cefotetan (1 g) or cefoxitin (1 g) before their perineal laceration was repaired. Patients who were allergic to penicillin received clindamycin (900 mg). The primary endpoints of the study were gross disruption of the wound or purulent drainage from the wound site 2 weeks after delivery.
Forty patients (27%) did not return for their post-partum appointment. Of the remaining patients, four of 49 (8%) who received antibiotics developed a wound complication, compared with 14 of 58 (24%) of those who received placebo (p=.037).
Sequelae of major perineal laceration can be severe
Major perineal laceration occurs in approximately 2% to 20% of vaginal deliveries in the United States. The principal risk factors for third- and fourth-degree lacerations are nulliparity, midline episiotomy, and operative vaginal delivery, especially forceps extraction. Both types of laceration may lead to serious morbidity, such as prolonged pain, fecal incontinence, and perineal infection, including necrotizing fasciitis. These infections typically are polymicrobial, mixed aerobic–anaerobic. Moreover, fourth-degree lacerations may result in rectovaginal fistula if they are not repaired properly. This complication causes considerable debility and major social inconvenience for the patient.
Although the sample size was relatively small, this study clearly demonstrated that a single dose of extended-spectrum cephalosporin (cefotetan or cefoxitin) was highly effective in reducing the rate of perineal infection and perineal wound disruption. Whether a more limited-spectrum agent such as cefazolin would be as effective is not certain.
I strongly recommend routine antibiotic prophylaxis for any patient who sustains a third- or fourth-degree perineal laceration.
If the patient has a mild allergy to penicillin (morbilliform rash), I would administer cefotetan because it is less expensive than cefoxitin. If the patient has a severe reaction to penicillin (urticaria, anaphylaxis), I would administer both clindamycin and gentamicin in order to ensure adequate coverage of the multiple organisms likely to cause soft-tissue infection of the genital tract.
Clindamycin alone covers only aerobic gram-positive cocci and offers no protection against the coliform organisms that are so prevalent in perineal wound infection.8
Diarrhea linked to Clostridium difficile emerges as a potent threat to pregnant women
Rouphael NG, O’Donnell JA, Bhatnagar J, et al. Clostridium difficile-associated diarrhea: an emerging threat to pregnant women. Am J Obstet Gynecol. 2008;198:635.e1–635.e6 [Classification of evidence – Level III].
This report describes 10 cases of severe Clostridium difficile-associated diarrhea (CDAD) in pregnant women during 2005 and 2006. CDAD usually affects elderly debilitated patients in hospitals and nursing homes. This report is of great concern because the affected patients were otherwise healthy, young, pregnant women. The observations are even more alarming because the mortality rate in this small series was 30% for both mothers and babies.
Details of the series
The women developed signs of severe CDAD 3 to 60 days after receiving antibiotics; the median was 5 days. CDAD was considered severe if the patient required hospitalization, ICU admission, or colectomy, or if she died. These cases occurred in California, Georgia, Oklahoma, and Pennsylvania and were reported to the Centers for Disease Control and Prevention (CDC).
Six women became ill before delivery, and four developed symptoms postpartum. The most common manifestations of infection were diarrhea, abdominal pain and distention, and fever. The peripheral white blood cell count was in the range of 11–72 × 103/μL. In nine patients, the diagnosis was confirmed by a positive test for toxin A/B; seven of these patients also had visible pseudomembranes in the colon. One patient had a positive stool sample for C difficile ( FIGURE 2 ).
Six patients required admission to the ICU. Six developed toxic megacolon, and five required subtotal colectomy. Three had sepsis; three had acute renal failure; two had disseminated intravascular coagulation. Three patients died, and three had stillbirths. Two patients relapsed following treatment.
One patient had no treatment and died. The others received either metronidazole or vancomycin or a combination of the two. One of the patients who died received metronidazole, vancomycin, and cholestyramine.
FIGURE 2 Clostridium difficile
C difficile is a spore-forming, gram-positive anaerobic bacillus that is a common cause of antibiotic-associated diarrhea.
An epidemic strain appears
The incidence of C difficile infection in acute care US hospitals has increased to 84 for every 100,000 patients in recent years, about three times the rate of 31 for every 100,000 that was reported in 1996, as the authors note. Many of the most severe cases of CDAD are caused by a new epidemic strain of bacteria, termed North American Pulsed Field type 1 (NAP1) and PCR ribotype 027.
This new strain is characterized by three key virulence factors:
- increased production of toxins A and B
- resistance to fluoroquinolones
- production of binary toxin.
Toxins A and B bind to the surface of intestinal epithelial cells, stimulate tissue injury and inflammation, and, ultimately, lead to cell death. Binary toxin appears to act synergistically with toxins A and B to cause severe colitis.9
Metronidazole is no longer the treatment of choice for severe CDAD
Before 2000, treatment of CDAD with vancomycin or metronidazole was 97% to 98% effective.9 In recent years, however, a failure rate as high as 26% has been reported among patients who are treated with metronidazole.10 One prospective, randomized clinical trial demonstrated that, in patients who had severe CDAD, vancomycin, 125 mg four times daily, was superior to metronidazole, 250 mg four times daily (97% success rate vs 76%; p=.02).11 The efficacy of the two drugs was comparable in treating milder cases of CDAD (98% for vancomycin, 90% for metronidazole; p=.36).
The clinical implications of this case series and the reports cited above are clear: When we administer broad-spectrum antibiotics to our patients, we must be ever watchful for signs of toxicity. If the patient develops diarrhea, the offending drug should be discontinued. If the diarrhea does not promptly resolve, tests to isolate C difficile in the stool and identify toxins unique to this organism are advised.
In addition, anoscopy or sigmoidoscopy should be performed to assess the patient for pseudomembranes.
If mild CDAD is confirmed, the patient may be treated with vancomycin or metronidazole. If severe CDAD is identified, vancomycin should be administered, and the patient should be transferred to the ICU for close monitoring and supportive care.
1. Dekker CL, Arvin AM. One step closer to a CMV vaccine. N Engl J Med. 2009;360:1250-1252.
2. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
3. Nigro G, Adler SP, LaTorre RL, Best AM. Congenital Cytomegalovirus Collaborating Group. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
4. Duff P, Barth WH, Jr, Post MD. Case records of the Massachusetts General Hospital. Case 4-2009: A 39-year-old pregnant woman with fever after a trip to Africa. N Engl J Med. 2009;360:508-516.
5. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157(4 Pt 1):794-798.
6. Tita AT, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
7. Tita ATN, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systematic review. Obstet Gynecol. 2009;113:675-682.
8. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
9. Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. N Engl J Med. 2008;359:1932-1940.
10. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
11. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
Dr. Duff reports no financial relationships relevant to this article.
Four important developments have marked the past year in infectious disease:
- A promising vaccine against cytomegalovirus (CMV) was tested in women of reproductive age
- Extended-spectrum antibiotic prophylaxis proved to be effective in reducing the incidence of wound infection following cesarean delivery
- Investigators developed a simple but effective method to prevent wound complications following repair of a third- or fourth-degree perineal laceration
- The incidence of severe Clostridium difficile-associated diarrhea crept upward, emerging as a threat to pregnant women.
CMV vaccine makes an auspicious debut—but isn’t ready for practice
Pass RF, Zhang C, Evans A, et al. Vaccine prevention of maternal cytomegalovirus infection. N Engl J Med. 2009; 360:1191–1199 [Classification of evidence – Level I].
This Phase-2, randomized, double-blind, placebo-controlled trial of a new cytomegalovirus (CMV) vaccine in women found an overall efficacy rate of 50% (95% confidence interval, 7% to 73%), with no unusually serious reactions among women who were vaccinated. This efficacy rate is disappointing, but it isn’t entirely surprising; even the immune response resulting from natural infection is not fully protective against reactivated infection or recurrent infection with a different strain of virus. Nor is natural immunity completely effective in preventing severe fetal injury in recurrent infection.1
Virus poses greatest risk to pregnant women and their fetuses
CMV is the most common perinatally transmitted infection, affecting 0.6% to 0.7% of infants ( FIGURE 1 ). The greatest risk of fetal injury occurs when the mother develops primary infection during pregnancy, which raises her infant’s risk of infection to 40% to 50%. Of infants delivered to mothers with primary infection, approximately 10% to 15% will be acutely symptomatic at birth.
Clinical manifestations of severe congenital CMV infection include growth restriction, microcephaly, ventriculomegaly, intracranial calcification, chorioretinitis, hearing impairment, hepatitis, and thrombocytopenia.
Because the morbidity and mortality associated with these conditions are alarmingly high, development of a safe, effective vaccine against CMV would be most welcome.2,3
Recurrent or reactivated maternal CMV infection poses a much lower risk to the fetus. Infected infants are rarely symptomatic at birth. Clinical manifestations of infection typically occur later in childhood and include hearing and visual deficits, dental anomalies, and learning or behavioral disorders.2,3
FIGURE 1 Cytomegalovirus
Cytomegalovirus is a member of the herpesvirus family. It is shed intermittently in bodily fluids, without detectable signs and symptoms.
Details of the trial
Women were eligible for the study if they were seronegative for CMV antibody, in good health, 14 to 40 years old, and not pregnant or lactating. Participants received three doses of vaccine or placebo at 0, 1, and 6 months. (The vaccine was composed of CMV envelope glycoprotein B with MF59 adjuvant.) The women were then tested for CMV infection every 3 months for as long as 42 months, using an assay for IgG antibodies directed against viral proteins other than glycoprotein B. Infection was confirmed by viral culture or immuno blotting. The primary endpoint was time until detection of CMV infection.
The vaccine was given to 234 patients, and 230 received placebo. Eighteen infections occurred in the vaccine group, compared with 31 in the placebo group. Vaccinated patients were more likely to remain uninfected during follow-up (p=.02).
One of 81 infants (1%) born to mothers in the vaccinated group had congenital CMV infection, compared with three of 97 (3%) infants born to mothers in the placebo group (p=.41). One infant in the placebo group had severe infection that was evident at birth. The other three infants were asymptomatic at birth and free of sequelae 3 to 5 years later.
The most promising preventive remains experimental
No drug is uniformly effective in treating maternal CMV infection and preventing congenital infection. The most promising intervention for prevention of congenital CMV infection is administration of hyperimmune anti-CMV antibody to the mother. A recent report by Nigro and colleagues4 found this agent to be of great value for both treating and preventing congenital CMV. However, because of limitations in the design of this study, administration of hyperimmune globulin still must be regarded as experimental.3
Key questions remain unanswered
The goal of a large-scale vaccination program is to ensure that women enter reproductive age with preexisting immunity to infection. In that light, the study by Pass and colleagues is only partially encouraging. Despite vaccination, 18 infections occurred, and the follow-up period was relatively short. We do not yet know whether the protective effect of the vaccine will be of extended duration. Moreover, one vaccinated mother delivered an infant who had congenital CMV infection.
Until additional trials of the CMV vaccine are reported, we must focus on helping patients prevent acquisition of infection during pregnancy. Preventive measures include:
- safe sex practices
- use of CMV-negative blood for transfusion to pregnant women and their fetuses
- strict hand-washing procedures for mothers when changing diapers and caring for young children.
Extended-spectrum antibiotics reduce the rate of postcesarean wound infection
Tita ATN, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199:303e.1–303e.3 [Classification of evidence – Level II].
This prospective study describes surveillance for postcesarean wound infection during three different periods at the University of Alabama:
- 1992–1996, during which patients undergoing cesarean delivery routinely received prophylaxis with a first- or second-generation cephalosporin. Overall incidence of wound infection: 3.1%
- 1997–1999, during which patients were randomized to standard prophylaxis with cefazolin or to cefazolin plus either intravenous (IV) doxycycline or oral azithromycin. Overall incidence of wound infection: 2.4%
- 2001–2006, during which patients routinely received IV cefazolin plus IV azithromycin. Overall incidence of wound infection: 1.3%.
In each time period, the prophylactic antibiotics were administered after the infant’s umbilical cord was clamped. The p value for test of trend was highly significant (p<.002). The same significant trend was noted when superficial and deep wound infections were examined separately.
This evidence is a “practice changer”
For almost 20 years, the standard of practice has been to routinely administer prophylactic antibiotics to all women having cesarean delivery. Essentially, every published study has demonstrated a highly significant reduction in the frequency of postcesarean endometritis when patients received prophylaxis. Multiple studies also confirmed that a more limited-spectrum cephalosporin was as effective as an extended-spectrum agent in reducing the frequency of endometritis.5
Many of these earlier reports were unable to demonstrate a consistently beneficial effect of prophylaxis on the incidence of postoperative wound infection. That is why the present study is of such interest and importance. Tita and colleagues previously demonstrated an improved effect of extended-spectrum prophylaxis on the incidence of postcesarean endometritis.6 Now they have confirmed that this method of prophylaxis is also effective in lowering the rate of surgical wound infection.
Wound infections are more troublesome than endometritis
Wound infections—either incisional abscess or cellulitis—are even more likely than post-cesarean endometritis to prolong a patient’s postoperative stay and create the potential for severe morbidity, such as fascial dehiscence and necrotizing fasciitis. With the increasing prevalence of obesity in the US population, wound infections are likely to become even more frequent.
These infections typically are caused by aerobic streptococci and staphylococci from the skin, combined with coliform organisms and anaerobes from the pelvic flora. Incisional abscesses require surgical drainage; cellulitis usually will respond to a change in antibiotic therapy that specifically targets streptococci and staphylococci, along with the coliforms and anaerobes.
I strongly recommend routine prophylaxis with IV cefazolin (1 g) plus azithromycin (500 mg) in all women having cesarean delivery. Moreover, in view of several recent investigations that evaluated the timing of antibiotic administration (immediately preoperative versus after the umbilical cord is clamped), I recommend that extended-spectrum prophylaxis be given before the start of surgery.7
Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized control trial. Obstet Gynecol. 2008;111:1268–1273 [Classification of evidence – Level I].
Take note of this prospective, randomized, placebo-controlled trial of prophylactic antibiotics in women who sustained a third-or fourth-degree perineal laceration during vaginal delivery: It is the first, and only, well-designed trial of antibiotic prophylaxis for prevention of complications after repair of a major perineal laceration. Among patients in the study, 8% who received antibiotics developed a wound complication, compared with 24% of patients who received placebo, a statistically and clinically significant difference.
Details of the study
Eighty-three women received placebo, and 64 received a single IV dose of either cefotetan (1 g) or cefoxitin (1 g) before their perineal laceration was repaired. Patients who were allergic to penicillin received clindamycin (900 mg). The primary endpoints of the study were gross disruption of the wound or purulent drainage from the wound site 2 weeks after delivery.
Forty patients (27%) did not return for their post-partum appointment. Of the remaining patients, four of 49 (8%) who received antibiotics developed a wound complication, compared with 14 of 58 (24%) of those who received placebo (p=.037).
Sequelae of major perineal laceration can be severe
Major perineal laceration occurs in approximately 2% to 20% of vaginal deliveries in the United States. The principal risk factors for third- and fourth-degree lacerations are nulliparity, midline episiotomy, and operative vaginal delivery, especially forceps extraction. Both types of laceration may lead to serious morbidity, such as prolonged pain, fecal incontinence, and perineal infection, including necrotizing fasciitis. These infections typically are polymicrobial, mixed aerobic–anaerobic. Moreover, fourth-degree lacerations may result in rectovaginal fistula if they are not repaired properly. This complication causes considerable debility and major social inconvenience for the patient.
Although the sample size was relatively small, this study clearly demonstrated that a single dose of extended-spectrum cephalosporin (cefotetan or cefoxitin) was highly effective in reducing the rate of perineal infection and perineal wound disruption. Whether a more limited-spectrum agent such as cefazolin would be as effective is not certain.
I strongly recommend routine antibiotic prophylaxis for any patient who sustains a third- or fourth-degree perineal laceration.
If the patient has a mild allergy to penicillin (morbilliform rash), I would administer cefotetan because it is less expensive than cefoxitin. If the patient has a severe reaction to penicillin (urticaria, anaphylaxis), I would administer both clindamycin and gentamicin in order to ensure adequate coverage of the multiple organisms likely to cause soft-tissue infection of the genital tract.
Clindamycin alone covers only aerobic gram-positive cocci and offers no protection against the coliform organisms that are so prevalent in perineal wound infection.8
Diarrhea linked to Clostridium difficile emerges as a potent threat to pregnant women
Rouphael NG, O’Donnell JA, Bhatnagar J, et al. Clostridium difficile-associated diarrhea: an emerging threat to pregnant women. Am J Obstet Gynecol. 2008;198:635.e1–635.e6 [Classification of evidence – Level III].
This report describes 10 cases of severe Clostridium difficile-associated diarrhea (CDAD) in pregnant women during 2005 and 2006. CDAD usually affects elderly debilitated patients in hospitals and nursing homes. This report is of great concern because the affected patients were otherwise healthy, young, pregnant women. The observations are even more alarming because the mortality rate in this small series was 30% for both mothers and babies.
Details of the series
The women developed signs of severe CDAD 3 to 60 days after receiving antibiotics; the median was 5 days. CDAD was considered severe if the patient required hospitalization, ICU admission, or colectomy, or if she died. These cases occurred in California, Georgia, Oklahoma, and Pennsylvania and were reported to the Centers for Disease Control and Prevention (CDC).
Six women became ill before delivery, and four developed symptoms postpartum. The most common manifestations of infection were diarrhea, abdominal pain and distention, and fever. The peripheral white blood cell count was in the range of 11–72 × 103/μL. In nine patients, the diagnosis was confirmed by a positive test for toxin A/B; seven of these patients also had visible pseudomembranes in the colon. One patient had a positive stool sample for C difficile ( FIGURE 2 ).
Six patients required admission to the ICU. Six developed toxic megacolon, and five required subtotal colectomy. Three had sepsis; three had acute renal failure; two had disseminated intravascular coagulation. Three patients died, and three had stillbirths. Two patients relapsed following treatment.
One patient had no treatment and died. The others received either metronidazole or vancomycin or a combination of the two. One of the patients who died received metronidazole, vancomycin, and cholestyramine.
FIGURE 2 Clostridium difficile
C difficile is a spore-forming, gram-positive anaerobic bacillus that is a common cause of antibiotic-associated diarrhea.
An epidemic strain appears
The incidence of C difficile infection in acute care US hospitals has increased to 84 for every 100,000 patients in recent years, about three times the rate of 31 for every 100,000 that was reported in 1996, as the authors note. Many of the most severe cases of CDAD are caused by a new epidemic strain of bacteria, termed North American Pulsed Field type 1 (NAP1) and PCR ribotype 027.
This new strain is characterized by three key virulence factors:
- increased production of toxins A and B
- resistance to fluoroquinolones
- production of binary toxin.
Toxins A and B bind to the surface of intestinal epithelial cells, stimulate tissue injury and inflammation, and, ultimately, lead to cell death. Binary toxin appears to act synergistically with toxins A and B to cause severe colitis.9
Metronidazole is no longer the treatment of choice for severe CDAD
Before 2000, treatment of CDAD with vancomycin or metronidazole was 97% to 98% effective.9 In recent years, however, a failure rate as high as 26% has been reported among patients who are treated with metronidazole.10 One prospective, randomized clinical trial demonstrated that, in patients who had severe CDAD, vancomycin, 125 mg four times daily, was superior to metronidazole, 250 mg four times daily (97% success rate vs 76%; p=.02).11 The efficacy of the two drugs was comparable in treating milder cases of CDAD (98% for vancomycin, 90% for metronidazole; p=.36).
The clinical implications of this case series and the reports cited above are clear: When we administer broad-spectrum antibiotics to our patients, we must be ever watchful for signs of toxicity. If the patient develops diarrhea, the offending drug should be discontinued. If the diarrhea does not promptly resolve, tests to isolate C difficile in the stool and identify toxins unique to this organism are advised.
In addition, anoscopy or sigmoidoscopy should be performed to assess the patient for pseudomembranes.
If mild CDAD is confirmed, the patient may be treated with vancomycin or metronidazole. If severe CDAD is identified, vancomycin should be administered, and the patient should be transferred to the ICU for close monitoring and supportive care.
Dr. Duff reports no financial relationships relevant to this article.
Four important developments have marked the past year in infectious disease:
- A promising vaccine against cytomegalovirus (CMV) was tested in women of reproductive age
- Extended-spectrum antibiotic prophylaxis proved to be effective in reducing the incidence of wound infection following cesarean delivery
- Investigators developed a simple but effective method to prevent wound complications following repair of a third- or fourth-degree perineal laceration
- The incidence of severe Clostridium difficile-associated diarrhea crept upward, emerging as a threat to pregnant women.
CMV vaccine makes an auspicious debut—but isn’t ready for practice
Pass RF, Zhang C, Evans A, et al. Vaccine prevention of maternal cytomegalovirus infection. N Engl J Med. 2009; 360:1191–1199 [Classification of evidence – Level I].
This Phase-2, randomized, double-blind, placebo-controlled trial of a new cytomegalovirus (CMV) vaccine in women found an overall efficacy rate of 50% (95% confidence interval, 7% to 73%), with no unusually serious reactions among women who were vaccinated. This efficacy rate is disappointing, but it isn’t entirely surprising; even the immune response resulting from natural infection is not fully protective against reactivated infection or recurrent infection with a different strain of virus. Nor is natural immunity completely effective in preventing severe fetal injury in recurrent infection.1
Virus poses greatest risk to pregnant women and their fetuses
CMV is the most common perinatally transmitted infection, affecting 0.6% to 0.7% of infants ( FIGURE 1 ). The greatest risk of fetal injury occurs when the mother develops primary infection during pregnancy, which raises her infant’s risk of infection to 40% to 50%. Of infants delivered to mothers with primary infection, approximately 10% to 15% will be acutely symptomatic at birth.
Clinical manifestations of severe congenital CMV infection include growth restriction, microcephaly, ventriculomegaly, intracranial calcification, chorioretinitis, hearing impairment, hepatitis, and thrombocytopenia.
Because the morbidity and mortality associated with these conditions are alarmingly high, development of a safe, effective vaccine against CMV would be most welcome.2,3
Recurrent or reactivated maternal CMV infection poses a much lower risk to the fetus. Infected infants are rarely symptomatic at birth. Clinical manifestations of infection typically occur later in childhood and include hearing and visual deficits, dental anomalies, and learning or behavioral disorders.2,3
FIGURE 1 Cytomegalovirus
Cytomegalovirus is a member of the herpesvirus family. It is shed intermittently in bodily fluids, without detectable signs and symptoms.
Details of the trial
Women were eligible for the study if they were seronegative for CMV antibody, in good health, 14 to 40 years old, and not pregnant or lactating. Participants received three doses of vaccine or placebo at 0, 1, and 6 months. (The vaccine was composed of CMV envelope glycoprotein B with MF59 adjuvant.) The women were then tested for CMV infection every 3 months for as long as 42 months, using an assay for IgG antibodies directed against viral proteins other than glycoprotein B. Infection was confirmed by viral culture or immuno blotting. The primary endpoint was time until detection of CMV infection.
The vaccine was given to 234 patients, and 230 received placebo. Eighteen infections occurred in the vaccine group, compared with 31 in the placebo group. Vaccinated patients were more likely to remain uninfected during follow-up (p=.02).
One of 81 infants (1%) born to mothers in the vaccinated group had congenital CMV infection, compared with three of 97 (3%) infants born to mothers in the placebo group (p=.41). One infant in the placebo group had severe infection that was evident at birth. The other three infants were asymptomatic at birth and free of sequelae 3 to 5 years later.
The most promising preventive remains experimental
No drug is uniformly effective in treating maternal CMV infection and preventing congenital infection. The most promising intervention for prevention of congenital CMV infection is administration of hyperimmune anti-CMV antibody to the mother. A recent report by Nigro and colleagues4 found this agent to be of great value for both treating and preventing congenital CMV. However, because of limitations in the design of this study, administration of hyperimmune globulin still must be regarded as experimental.3
Key questions remain unanswered
The goal of a large-scale vaccination program is to ensure that women enter reproductive age with preexisting immunity to infection. In that light, the study by Pass and colleagues is only partially encouraging. Despite vaccination, 18 infections occurred, and the follow-up period was relatively short. We do not yet know whether the protective effect of the vaccine will be of extended duration. Moreover, one vaccinated mother delivered an infant who had congenital CMV infection.
Until additional trials of the CMV vaccine are reported, we must focus on helping patients prevent acquisition of infection during pregnancy. Preventive measures include:
- safe sex practices
- use of CMV-negative blood for transfusion to pregnant women and their fetuses
- strict hand-washing procedures for mothers when changing diapers and caring for young children.
Extended-spectrum antibiotics reduce the rate of postcesarean wound infection
Tita ATN, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199:303e.1–303e.3 [Classification of evidence – Level II].
This prospective study describes surveillance for postcesarean wound infection during three different periods at the University of Alabama:
- 1992–1996, during which patients undergoing cesarean delivery routinely received prophylaxis with a first- or second-generation cephalosporin. Overall incidence of wound infection: 3.1%
- 1997–1999, during which patients were randomized to standard prophylaxis with cefazolin or to cefazolin plus either intravenous (IV) doxycycline or oral azithromycin. Overall incidence of wound infection: 2.4%
- 2001–2006, during which patients routinely received IV cefazolin plus IV azithromycin. Overall incidence of wound infection: 1.3%.
In each time period, the prophylactic antibiotics were administered after the infant’s umbilical cord was clamped. The p value for test of trend was highly significant (p<.002). The same significant trend was noted when superficial and deep wound infections were examined separately.
This evidence is a “practice changer”
For almost 20 years, the standard of practice has been to routinely administer prophylactic antibiotics to all women having cesarean delivery. Essentially, every published study has demonstrated a highly significant reduction in the frequency of postcesarean endometritis when patients received prophylaxis. Multiple studies also confirmed that a more limited-spectrum cephalosporin was as effective as an extended-spectrum agent in reducing the frequency of endometritis.5
Many of these earlier reports were unable to demonstrate a consistently beneficial effect of prophylaxis on the incidence of postoperative wound infection. That is why the present study is of such interest and importance. Tita and colleagues previously demonstrated an improved effect of extended-spectrum prophylaxis on the incidence of postcesarean endometritis.6 Now they have confirmed that this method of prophylaxis is also effective in lowering the rate of surgical wound infection.
Wound infections are more troublesome than endometritis
Wound infections—either incisional abscess or cellulitis—are even more likely than post-cesarean endometritis to prolong a patient’s postoperative stay and create the potential for severe morbidity, such as fascial dehiscence and necrotizing fasciitis. With the increasing prevalence of obesity in the US population, wound infections are likely to become even more frequent.
These infections typically are caused by aerobic streptococci and staphylococci from the skin, combined with coliform organisms and anaerobes from the pelvic flora. Incisional abscesses require surgical drainage; cellulitis usually will respond to a change in antibiotic therapy that specifically targets streptococci and staphylococci, along with the coliforms and anaerobes.
I strongly recommend routine prophylaxis with IV cefazolin (1 g) plus azithromycin (500 mg) in all women having cesarean delivery. Moreover, in view of several recent investigations that evaluated the timing of antibiotic administration (immediately preoperative versus after the umbilical cord is clamped), I recommend that extended-spectrum prophylaxis be given before the start of surgery.7
Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized control trial. Obstet Gynecol. 2008;111:1268–1273 [Classification of evidence – Level I].
Take note of this prospective, randomized, placebo-controlled trial of prophylactic antibiotics in women who sustained a third-or fourth-degree perineal laceration during vaginal delivery: It is the first, and only, well-designed trial of antibiotic prophylaxis for prevention of complications after repair of a major perineal laceration. Among patients in the study, 8% who received antibiotics developed a wound complication, compared with 24% of patients who received placebo, a statistically and clinically significant difference.
Details of the study
Eighty-three women received placebo, and 64 received a single IV dose of either cefotetan (1 g) or cefoxitin (1 g) before their perineal laceration was repaired. Patients who were allergic to penicillin received clindamycin (900 mg). The primary endpoints of the study were gross disruption of the wound or purulent drainage from the wound site 2 weeks after delivery.
Forty patients (27%) did not return for their post-partum appointment. Of the remaining patients, four of 49 (8%) who received antibiotics developed a wound complication, compared with 14 of 58 (24%) of those who received placebo (p=.037).
Sequelae of major perineal laceration can be severe
Major perineal laceration occurs in approximately 2% to 20% of vaginal deliveries in the United States. The principal risk factors for third- and fourth-degree lacerations are nulliparity, midline episiotomy, and operative vaginal delivery, especially forceps extraction. Both types of laceration may lead to serious morbidity, such as prolonged pain, fecal incontinence, and perineal infection, including necrotizing fasciitis. These infections typically are polymicrobial, mixed aerobic–anaerobic. Moreover, fourth-degree lacerations may result in rectovaginal fistula if they are not repaired properly. This complication causes considerable debility and major social inconvenience for the patient.
Although the sample size was relatively small, this study clearly demonstrated that a single dose of extended-spectrum cephalosporin (cefotetan or cefoxitin) was highly effective in reducing the rate of perineal infection and perineal wound disruption. Whether a more limited-spectrum agent such as cefazolin would be as effective is not certain.
I strongly recommend routine antibiotic prophylaxis for any patient who sustains a third- or fourth-degree perineal laceration.
If the patient has a mild allergy to penicillin (morbilliform rash), I would administer cefotetan because it is less expensive than cefoxitin. If the patient has a severe reaction to penicillin (urticaria, anaphylaxis), I would administer both clindamycin and gentamicin in order to ensure adequate coverage of the multiple organisms likely to cause soft-tissue infection of the genital tract.
Clindamycin alone covers only aerobic gram-positive cocci and offers no protection against the coliform organisms that are so prevalent in perineal wound infection.8
Diarrhea linked to Clostridium difficile emerges as a potent threat to pregnant women
Rouphael NG, O’Donnell JA, Bhatnagar J, et al. Clostridium difficile-associated diarrhea: an emerging threat to pregnant women. Am J Obstet Gynecol. 2008;198:635.e1–635.e6 [Classification of evidence – Level III].
This report describes 10 cases of severe Clostridium difficile-associated diarrhea (CDAD) in pregnant women during 2005 and 2006. CDAD usually affects elderly debilitated patients in hospitals and nursing homes. This report is of great concern because the affected patients were otherwise healthy, young, pregnant women. The observations are even more alarming because the mortality rate in this small series was 30% for both mothers and babies.
Details of the series
The women developed signs of severe CDAD 3 to 60 days after receiving antibiotics; the median was 5 days. CDAD was considered severe if the patient required hospitalization, ICU admission, or colectomy, or if she died. These cases occurred in California, Georgia, Oklahoma, and Pennsylvania and were reported to the Centers for Disease Control and Prevention (CDC).
Six women became ill before delivery, and four developed symptoms postpartum. The most common manifestations of infection were diarrhea, abdominal pain and distention, and fever. The peripheral white blood cell count was in the range of 11–72 × 103/μL. In nine patients, the diagnosis was confirmed by a positive test for toxin A/B; seven of these patients also had visible pseudomembranes in the colon. One patient had a positive stool sample for C difficile ( FIGURE 2 ).
Six patients required admission to the ICU. Six developed toxic megacolon, and five required subtotal colectomy. Three had sepsis; three had acute renal failure; two had disseminated intravascular coagulation. Three patients died, and three had stillbirths. Two patients relapsed following treatment.
One patient had no treatment and died. The others received either metronidazole or vancomycin or a combination of the two. One of the patients who died received metronidazole, vancomycin, and cholestyramine.
FIGURE 2 Clostridium difficile
C difficile is a spore-forming, gram-positive anaerobic bacillus that is a common cause of antibiotic-associated diarrhea.
An epidemic strain appears
The incidence of C difficile infection in acute care US hospitals has increased to 84 for every 100,000 patients in recent years, about three times the rate of 31 for every 100,000 that was reported in 1996, as the authors note. Many of the most severe cases of CDAD are caused by a new epidemic strain of bacteria, termed North American Pulsed Field type 1 (NAP1) and PCR ribotype 027.
This new strain is characterized by three key virulence factors:
- increased production of toxins A and B
- resistance to fluoroquinolones
- production of binary toxin.
Toxins A and B bind to the surface of intestinal epithelial cells, stimulate tissue injury and inflammation, and, ultimately, lead to cell death. Binary toxin appears to act synergistically with toxins A and B to cause severe colitis.9
Metronidazole is no longer the treatment of choice for severe CDAD
Before 2000, treatment of CDAD with vancomycin or metronidazole was 97% to 98% effective.9 In recent years, however, a failure rate as high as 26% has been reported among patients who are treated with metronidazole.10 One prospective, randomized clinical trial demonstrated that, in patients who had severe CDAD, vancomycin, 125 mg four times daily, was superior to metronidazole, 250 mg four times daily (97% success rate vs 76%; p=.02).11 The efficacy of the two drugs was comparable in treating milder cases of CDAD (98% for vancomycin, 90% for metronidazole; p=.36).
The clinical implications of this case series and the reports cited above are clear: When we administer broad-spectrum antibiotics to our patients, we must be ever watchful for signs of toxicity. If the patient develops diarrhea, the offending drug should be discontinued. If the diarrhea does not promptly resolve, tests to isolate C difficile in the stool and identify toxins unique to this organism are advised.
In addition, anoscopy or sigmoidoscopy should be performed to assess the patient for pseudomembranes.
If mild CDAD is confirmed, the patient may be treated with vancomycin or metronidazole. If severe CDAD is identified, vancomycin should be administered, and the patient should be transferred to the ICU for close monitoring and supportive care.
1. Dekker CL, Arvin AM. One step closer to a CMV vaccine. N Engl J Med. 2009;360:1250-1252.
2. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
3. Nigro G, Adler SP, LaTorre RL, Best AM. Congenital Cytomegalovirus Collaborating Group. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
4. Duff P, Barth WH, Jr, Post MD. Case records of the Massachusetts General Hospital. Case 4-2009: A 39-year-old pregnant woman with fever after a trip to Africa. N Engl J Med. 2009;360:508-516.
5. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157(4 Pt 1):794-798.
6. Tita AT, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
7. Tita ATN, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systematic review. Obstet Gynecol. 2009;113:675-682.
8. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
9. Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. N Engl J Med. 2008;359:1932-1940.
10. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
11. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
1. Dekker CL, Arvin AM. One step closer to a CMV vaccine. N Engl J Med. 2009;360:1250-1252.
2. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
3. Nigro G, Adler SP, LaTorre RL, Best AM. Congenital Cytomegalovirus Collaborating Group. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
4. Duff P, Barth WH, Jr, Post MD. Case records of the Massachusetts General Hospital. Case 4-2009: A 39-year-old pregnant woman with fever after a trip to Africa. N Engl J Med. 2009;360:508-516.
5. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157(4 Pt 1):794-798.
6. Tita AT, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
7. Tita ATN, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systematic review. Obstet Gynecol. 2009;113:675-682.
8. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
9. Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. N Engl J Med. 2008;359:1932-1940.
10. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
11. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
UPDATE: INFECTIOUS DISEASE
- important new information regarding the effectiveness of hepatitis A vaccine for postexposure prophylaxis
- the need to confirm antimicrobial susceptibility of group B streptococcus (GBS) isolates in pregnant women who are allergic to penicillin
- a new guideline on administering antibiotic prophylaxis for cesarean delivery
- a valuable overview of diverticulitis, a disease that we will all see with increasing regularity as the US population ages
For most, the best hepatitis A postexposure prophylaxis is vaccination
Victor JC, Monto AS, Surdina TY, et al. Hepatitis A vaccine versus immune globulin for postexposure prophylaxis. N Engl J Med. 2007;357:1685–1694.
The objective of this investigation, conducted in Almaty, Kazakhstan, was to compare the relative effectiveness of hepatitis A vaccine with that of immune globulin for prophylaxis after exposure to the hepatitis A virus. Participants were 2 to 40 years old and were household or day-care contacts of people who had hepatitis A. Five hundred sixty-eight susceptible patients received hepatitis A vaccine within 14 days of exposure; 522 susceptible patients received an age-appropriate dose of immune globulin. The primary endpoint was laboratoryconfirmed, symptomatic hepatitis A within 15 to 56 days of exposure.
FIGURE 1 Hepatitis A virus
Hepatitis A virus has single-stranded RNA, no envelope, and is approximately 27–30 nm in diameter.Symptomatic infection occurred in 25 of 568 (4.4%) vaccine recipients and 17 of 522 (3.3%) recipients of immune globulin. The relative risk of infection after the vaccine was 1.35 (95% confidence interval [CI], 0.70–2.67). No serious adverse effects occurred as the result of administration of either the vaccine or immune globulin. The authors concluded that both agents provide effective postexposure prophylaxis against hepatitis A infection.
Hepatitis A is caused by an RNA virus that is transmitted by fecal–oral contact. It is highly contagious and endemic in areas of the world where poverty, poor sanitation, and overcrowded living conditions prevail. Hepatitis A usually causes a symptomatic illness characterized by fever, malaise, anorexia, jaundice, acholic stools, darkened urine, and hepatic pain and tenderness. In poorly nourished or immunocompromised patients, severe morbidity and, rarely, mortality, may occur. Unlike other forms of hepatitis, hepatitis A does not cause a chronic carrier state, and perinatal transmission is extremely unlikely.
Best strategy? Prevention
At present, there is no specific antiviral therapy that is routinely used for treatment of hepatitis A. However, highly effective preventive measures are available. For preexposure prophylaxis, time permitting, the ideal agent is inactivated hepatitis A vaccine.1
The vaccine is usually given in two doses separated by 6 to 12 months and is highly immunogenic. In the United States, key candidates for vaccination are
- gay men
- residents and staff of chronic care facilities
- intravenous drug users
- individuals who live in areas where hepatitis A is endemic
- primate laboratory workers
- people 30 years of age and older who have chronic liver disease
- international travelers
- people who have received a liver transplant or are awaiting one.
The vaccine is safe for administration in pregnancy and is now recommended for children.
After exposure, vaccine trumps immune globulin in healthy patients
The standard agent for prophylaxis after exposure to the hepatitis A virus has been immune globulin 0.02 mL/kg, administered intramuscularly. Immune globulin is highly effective in this application and, in the present investigation, it was slightly more effective than the vaccine.
Despite the modest difference in effectiveness, however, hepatitis A vaccine offers several unique advantages for postexposure prophylaxis:
- It confers long-term immunity rather than just temporary protection.
- Because the volume of fluid injected is lower, the vaccine causes less pain upon administration.
- Immune globulin is now produced by a single manufacturer, and its supply has been limited. Its price also approaches that of the vaccine.
- Administration of immune globulin to a child may disrupt the normal childhood immunization schedule.
In older and immunocompromised patients, use immune globulin
For most patients, hepatitis A vaccine is the indicated method of postexposure immunoprophylaxis.
Because it is slightly more effective, however, immune globulin probably should remain the preferred agent for hepatitis A postexposure prophylaxis in older or immunocompromised patients who are more likely to develop severe illness if they be-come infected.
REFERENCES
We’re not following guidelines on GBS prophylaxis in penicillin allergy
Matheson KA, Lievense SP, Catanzaro B, Phipps MG. Intrapartum group B streptococci prophylaxis in patients reporting a penicillin allergy. Obstet Gynecol. 2008;111:356–364.
In this study, conducted at a single institution (Brown University), Matheson and colleagues sought to assess the adequacy of prophylaxis for GBS infection in women who had an allergy to penicillin. Specifically, the authors sought to determine how well practitioners at their institution adhered to the 2002 Centers for Disease Control and Prevention (CDC) guidelines, which specify that cefazolin should be used for prophylaxis in patients who are penicillin-allergic but not at high risk for anaphylaxis.1 For patients at high risk for anaphylaxis, clindamycin may be used for prophylaxis if the organism is known to be susceptible. If susceptibility has not been documented, vancomycin should be administered.1
Overall, 95% of GBS-positive, penicillin-allergic patients received prophylaxis (95% CI, 91–97). However, only 15% of these women received appropriate prophylaxis as defined by the CDC (95% CI, 11–12). Clindamycin was administered to 83% of patients, but susceptibility testing was performed in only 11%. At the time of this study, 26% of all GBS isolates at Brown were resistant to clindamycin; 37% were resistant to erythromycin.
The authors concluded that adherence to CDC guidelines was clearly less than optimal. Even at 1 year after adoption of the guidelines, only 20% of patients received appropriate prophylaxis.
Type of allergic reaction is key to selection of prophylactic agent
GBS is uniformly sensitive to penicillin and ampicillin. It also is 100% sensitive to cefazolin, the preferred drug for intrapartum prophylaxis in penicillin-allergic women who have a low risk of anaphylactic reaction to penicillin.
FIGURE 2 Group B streptococcus
A clear zone of hemolysis on blood agar is a key characteristic of group B streptococcus.However, it probably is better to avoid cephalosporins in patients who report a previous anaphylactic reaction to penicillin or ampicillin, even though the risk of cross-reactivity between penicillin and cephalosporin is low. In such patients, possible alternatives include erythromycin, clindamycin, and vancomycin.
Erythromycin is no longer recommended
At the University of Florida, we reported that 21% of GBS strains were resistant to erythromycin.2 At Brown University, Matheson and colleagues reported that 37% of GBS isolates were resistant to erythromycin. On the basis of similar reports, the CDC has concluded that erythromycin no longer should be used for GBS prophylaxis.
At our institution, we also have noted a disturbing trend of increased GBS resistance to clindamycin. In our recent report, 9% of GBS strains were resistant to this antibiotic. Similarly, Matheson and coworkers observed that 26% of GBS isolates in their center were resistant to clindamycin.
Neonatal GBS infection is now one of the leading causes for malpractice suits in obstetrics. Key issues presented in these suits include:
- failure to screen
- failure to use the correct culture medium for screening
- failure to obtain test results in a timely manner
- failure to use the correct drug for prophylaxis.
In GBS-positive patients, practitioners should inquire about penicillin allergy and document the exact type of reaction experienced by the patient, if it is accurately known. If the reported reaction to penicillin was not life-threatening, patients should receive cefazolin, 2 g IV initially, then 1 g every 8 hours until delivery. If the reaction to penicillin was immediate and life-threatening, the patient should receive clindamycin, 900 mg IV every 8 hours, if the organism is confirmed to be susceptible. Susceptibility testing should be documented in the medical record.
If such testing is unavailable, vancomycin is the drug of choice.
Susceptibility testing is vital in penicillin-allergic women
Because of observations such as these, the CDC now recommends that clindamycin be used for GBS prophylaxis only if antimicrobial susceptibility tests have confirmed that the organism is sensitive. If susceptibility testing cannot easily be performed, practitioners should use intravenous (IV) vancomycin, 1 g every 12 hours, for prophylaxis. Potential side effects of vancomycin include allergic reactions, gastrointestinal irritation, ototoxicity, and nephrotoxicity. The latter two effects are extremely unlikely in patients who receive only one or two IV doses of the drug.
20% to 30% of gravidas are colonized with GBS
GBS is one of the two major causes of pneumonia, meningitis, and sepsis in both pre-term and term newborns. Approximately 20% to 30% of women are colonized with the organism at some point during pregnancy. Universal screening for GBS at 35 to 37 weeks’ gestation, combined with intrapartum antibiotic prophylaxis, has been highly effective in reducing the frequency of invasive GBS infection.
REFERENCES
1. Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002;51:1-24
2. Edwards RK, Clark P, Sistrom CL, Duff P. Intrapartum antibiotic prophylaxis 1: relative effects of recommended antibiotics on gram-negative pathogens. Obstet Gynecol. 2002;100:534-539
New data suggest that preincision prophylaxis is best for C-section
Sullivan SA, Smith T, Chang E, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized, controlled trial. Am J Obstet Gynecol. 2007;196:455.e1–455.e5.
Is preoperative antibiotic prophylaxis superior to intraoperative prophylaxis in preventing postcesarean infection? Sullivan and colleagues set out to answer this question in a prospective, randomized, double-blinded, placebo-controlled study at the Medical University of South Carolina.
In the study group, 175 women undergoing cesarean delivery were randomized to receive 1 g of IV cefazolin 15 to 60 minutes before surgery, followed by a placebo infusion immediately after the umbilical cord was clamped. In the control group, 182 women received preoperative placebo, followed by 1 g of cefazolin immediately after cord clamping.
Two patients in the study group developed endomyometritis, compared with 10 in the control group (relative risk [RR], 0.2; 95% CI, 0.15–0.94). Five patients in the study group developed a wound infection, compared with 10 in the control group (RR, 0.52; 95% CI, 0.18–1.5, not significant). Overall, eight women in the study group and 21 women in the control group met the criteria for infectious morbidity (RR, 0.4; 95% CI, 0.18–0.87).
There were no differences between the groups in the frequency of neonatal sepsis, neonatal intensive care unit (NICU) admission, total length of hospital stay, metabolic acidosis, or sepsis evaluation. Infants in the study group had significantly fewer days in the NICU (P<.01).
How this study differs from earlier investigations
The classic studies of antibiotic prophylaxis were performed in an animal model by Burke.1 He demonstrated that prophylaxis had its greatest effect when the antibiotic was administered before the surgical incision. Essentially, no effect of prophylaxis was evident when antibiotic administration was delayed more than 4 hours beyond the start of surgery.
Early studies of antibiotic prophylaxis for cesarean delivery, conducted in the 1970s, administered antibiotics preoperatively and continued administration for several days after surgery. In 1979, Gordon and colleagues published an important investigation demonstrating that delay in administration of antibiotics until after the umbilical cord was clamped did not compromise the effectiveness of prophylaxis and significantly decreased the number of infants who required sepsis evaluations.2
This latter effect presumably occurred because infants were not exposed to antibiotics before delivery. Gordon’s investigation and subsequent reports also demonstrated that effective prophylaxis could be achieved with one to three doses of antibiotics.3
Why this new study may alter practice
Before Sullivan and colleagues published their findings, I believe that the best available evidence supported the use of a single dose of antibiotic, such as cefazolin, immediately after cord clamping. There are no convincing data that demonstrate an advantage for extended-spectrum agents (second- and third-generation cephalosporins, broad-spectrum penicillins, or carbapenems) over cefazolin.3
However, if the findings of Sullivan and coworkers are confirmed by other investigations in different patient populations, they definitely should lead to a change in the standard of care for prophylaxis. This investigation was exceptionally well designed and executed. The reduction in the frequency of endomyometritis and overall rate of infectious morbidity was impressive. This advantage was achieved without increasing the rate of neonatal sepsis evaluation.
REFERENCES
1. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168
2. Gordon HR, Phelps D. Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before or after cord clamping. Surgery. 1979;53:151-156
3. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157:794-798
Expect to see more women with diverticulitis as the population ages
Jacobs DO. Diverticulitis. N Engl J Med. 2007;357:2057–2066.
ObGyns continue to play a major role in providing primary care to women. With the steady aging of the American population, practitioners certainly can expect to care for more and more women who are 50 years of age or older, and diverticulitis is likely to turn up in an increasing number of these patients.
Diverticulitis is a relatively common condition in older patients and must consistently be considered in the differential diagnosis of women with acute abdominal pain—particularly left-sided pain.
It is present in approximately 10% of adults younger than 40 years of age and in 40 to 70% of people 80 years of age or older. It primarily affects the sigmoid and descending colon and is associated with diets that are low in fiber and high in refined carbohydrates.
The condition probably results from stasis or obstruction in the narrow neck of a diverticulum, which, in turn, leads to an overgrowth of bacteria. The principal micro-organisms isolated from affected patients are anaerobes, gram-negative aerobes, and some facultative gram-positive bacteria.
Range of severity can be wide
Presentation of diverticulitis may range in severity from mild to moderate lower abdominal pain associated with anorexia, nausea, and vomiting to abscess and fistula formation, colonic stricture, bowel obstruction, and peritonitis (“complicated diverticulitis”). Peritonitis may arise from rupture of a peridiverticular abscess or free rupture of an uninflamed diverticulum. Diverticulitis may be particularly severe in immunocompromised patients.
Classification of disease
The most accepted classification system for diverticulitis is the Hinchey system:
- in stage 1 disease, patients have small and confined pericolic or mesenteric abscesses
- in stage 2, the abscesses are larger but usually remain confined to the pelvis
- in stage 3, an abscess ruptures and causes purulent peritonitis
- stage 4 disease is distinguished by rupture of an uninflamed and unobstructed diverticulum (known as “free rupture”); this stage has the highest risk of adverse outcomes.
CT is best for diagnosis
The most useful diagnostic test for diverticulitis is a computed tomography (CT) scan. As a general rule, endoscopy should be avoided because of the risk of intestinal perforation.
Most patients can be treated as outpatients
Patients who have mild disease usually can be treated as outpatients. They should receive a 7- to 10-day course of oral antibiotics such as ciprofloxacin, 500 to 750 mg every 12 hours, plus metronidazole, 500 mg every 6 to 8 hours.
Alternate oral regimens include metronidazole, 500 mg every 6 to 8 hours, plus trimethoprim-sulfamethoxazole, double-strength, every 12 hours, or amoxicillin-clavulanate, 875 mg every 12 hours.
For seriously ill patients, hospitalization is warranted
Seriously ill patients—particularly those who are immunocompromised—should be hospitalized. If bowel obstruction is present, a nasogastric tube should be inserted. Appropriate IV antibiotic regimens for hospitalized patients include:
- metronidazole, 500 mg every 6 to 8 hours, plus ciprofloxacin, 400 mg every 12 hours
- metronidazole, 500 mg every 6 to 8 hours, plus ceftriaxone, 1 to 2 g every 24 hours
- ampicillin–sulbactam, 3 g every 6 hours
- piperacillin–tazobactam, 3.375 g every 6 hours
- ticarcillin–clavulanate, 3.1 g every 6 hours.
FIGURE 3 Consider diverticulitis in older women who complain of acute abdominal pain
Diverticulitis generally affects the sigmoid colon and descending colon and probably arises from stasis or obstruction in the narrow neck of a diverticulum, which leads to an overgrowth of bacteria and possible rupture.If an abscess is present and fails to respond promptly to medical therapy, drainage may be necessary. Some abscesses can be drained percutaneously under CT guidance. Large abscesses, in association with signs of generalized peritonitis, uncontrolled sepsis, or intestinal perforation, require surgical intervention, either via laparoscopy or open laparotomy. Preliminary data suggest that the laparoscopic approach may result in a shorter hospital stay, decreased postoperative pain, and an overall reduced rate of perioperative complication.
Diverticulitis may mimic appendicitis
The clinical presentation of diverticulitis is similar to that of appendicitis, except that the pain is usually on the left. Perforation, with resulting peritonitis, is an ever-present and potentially life-threatening complication. The dominant organisms are anaerobes and coliforms. The best diagnostic test is CT.
Patients in the early stages of disease can usually be treated as outpatients with antibiotics that are quite familiar to all ObGyns— i.e., metronidazole and a quinolone. More seriously ill patients should be hospitalized and treated with IV antibiotics and nasogastric suctioning.
Consultation with an interventional radiologist and general surgeon is recommended if operative intervention is necessary.
- important new information regarding the effectiveness of hepatitis A vaccine for postexposure prophylaxis
- the need to confirm antimicrobial susceptibility of group B streptococcus (GBS) isolates in pregnant women who are allergic to penicillin
- a new guideline on administering antibiotic prophylaxis for cesarean delivery
- a valuable overview of diverticulitis, a disease that we will all see with increasing regularity as the US population ages
For most, the best hepatitis A postexposure prophylaxis is vaccination
Victor JC, Monto AS, Surdina TY, et al. Hepatitis A vaccine versus immune globulin for postexposure prophylaxis. N Engl J Med. 2007;357:1685–1694.
The objective of this investigation, conducted in Almaty, Kazakhstan, was to compare the relative effectiveness of hepatitis A vaccine with that of immune globulin for prophylaxis after exposure to the hepatitis A virus. Participants were 2 to 40 years old and were household or day-care contacts of people who had hepatitis A. Five hundred sixty-eight susceptible patients received hepatitis A vaccine within 14 days of exposure; 522 susceptible patients received an age-appropriate dose of immune globulin. The primary endpoint was laboratoryconfirmed, symptomatic hepatitis A within 15 to 56 days of exposure.
FIGURE 1 Hepatitis A virus
Hepatitis A virus has single-stranded RNA, no envelope, and is approximately 27–30 nm in diameter.Symptomatic infection occurred in 25 of 568 (4.4%) vaccine recipients and 17 of 522 (3.3%) recipients of immune globulin. The relative risk of infection after the vaccine was 1.35 (95% confidence interval [CI], 0.70–2.67). No serious adverse effects occurred as the result of administration of either the vaccine or immune globulin. The authors concluded that both agents provide effective postexposure prophylaxis against hepatitis A infection.
Hepatitis A is caused by an RNA virus that is transmitted by fecal–oral contact. It is highly contagious and endemic in areas of the world where poverty, poor sanitation, and overcrowded living conditions prevail. Hepatitis A usually causes a symptomatic illness characterized by fever, malaise, anorexia, jaundice, acholic stools, darkened urine, and hepatic pain and tenderness. In poorly nourished or immunocompromised patients, severe morbidity and, rarely, mortality, may occur. Unlike other forms of hepatitis, hepatitis A does not cause a chronic carrier state, and perinatal transmission is extremely unlikely.
Best strategy? Prevention
At present, there is no specific antiviral therapy that is routinely used for treatment of hepatitis A. However, highly effective preventive measures are available. For preexposure prophylaxis, time permitting, the ideal agent is inactivated hepatitis A vaccine.1
The vaccine is usually given in two doses separated by 6 to 12 months and is highly immunogenic. In the United States, key candidates for vaccination are
- gay men
- residents and staff of chronic care facilities
- intravenous drug users
- individuals who live in areas where hepatitis A is endemic
- primate laboratory workers
- people 30 years of age and older who have chronic liver disease
- international travelers
- people who have received a liver transplant or are awaiting one.
The vaccine is safe for administration in pregnancy and is now recommended for children.
After exposure, vaccine trumps immune globulin in healthy patients
The standard agent for prophylaxis after exposure to the hepatitis A virus has been immune globulin 0.02 mL/kg, administered intramuscularly. Immune globulin is highly effective in this application and, in the present investigation, it was slightly more effective than the vaccine.
Despite the modest difference in effectiveness, however, hepatitis A vaccine offers several unique advantages for postexposure prophylaxis:
- It confers long-term immunity rather than just temporary protection.
- Because the volume of fluid injected is lower, the vaccine causes less pain upon administration.
- Immune globulin is now produced by a single manufacturer, and its supply has been limited. Its price also approaches that of the vaccine.
- Administration of immune globulin to a child may disrupt the normal childhood immunization schedule.
In older and immunocompromised patients, use immune globulin
For most patients, hepatitis A vaccine is the indicated method of postexposure immunoprophylaxis.
Because it is slightly more effective, however, immune globulin probably should remain the preferred agent for hepatitis A postexposure prophylaxis in older or immunocompromised patients who are more likely to develop severe illness if they be-come infected.
REFERENCES
We’re not following guidelines on GBS prophylaxis in penicillin allergy
Matheson KA, Lievense SP, Catanzaro B, Phipps MG. Intrapartum group B streptococci prophylaxis in patients reporting a penicillin allergy. Obstet Gynecol. 2008;111:356–364.
In this study, conducted at a single institution (Brown University), Matheson and colleagues sought to assess the adequacy of prophylaxis for GBS infection in women who had an allergy to penicillin. Specifically, the authors sought to determine how well practitioners at their institution adhered to the 2002 Centers for Disease Control and Prevention (CDC) guidelines, which specify that cefazolin should be used for prophylaxis in patients who are penicillin-allergic but not at high risk for anaphylaxis.1 For patients at high risk for anaphylaxis, clindamycin may be used for prophylaxis if the organism is known to be susceptible. If susceptibility has not been documented, vancomycin should be administered.1
Overall, 95% of GBS-positive, penicillin-allergic patients received prophylaxis (95% CI, 91–97). However, only 15% of these women received appropriate prophylaxis as defined by the CDC (95% CI, 11–12). Clindamycin was administered to 83% of patients, but susceptibility testing was performed in only 11%. At the time of this study, 26% of all GBS isolates at Brown were resistant to clindamycin; 37% were resistant to erythromycin.
The authors concluded that adherence to CDC guidelines was clearly less than optimal. Even at 1 year after adoption of the guidelines, only 20% of patients received appropriate prophylaxis.
Type of allergic reaction is key to selection of prophylactic agent
GBS is uniformly sensitive to penicillin and ampicillin. It also is 100% sensitive to cefazolin, the preferred drug for intrapartum prophylaxis in penicillin-allergic women who have a low risk of anaphylactic reaction to penicillin.
FIGURE 2 Group B streptococcus
A clear zone of hemolysis on blood agar is a key characteristic of group B streptococcus.However, it probably is better to avoid cephalosporins in patients who report a previous anaphylactic reaction to penicillin or ampicillin, even though the risk of cross-reactivity between penicillin and cephalosporin is low. In such patients, possible alternatives include erythromycin, clindamycin, and vancomycin.
Erythromycin is no longer recommended
At the University of Florida, we reported that 21% of GBS strains were resistant to erythromycin.2 At Brown University, Matheson and colleagues reported that 37% of GBS isolates were resistant to erythromycin. On the basis of similar reports, the CDC has concluded that erythromycin no longer should be used for GBS prophylaxis.
At our institution, we also have noted a disturbing trend of increased GBS resistance to clindamycin. In our recent report, 9% of GBS strains were resistant to this antibiotic. Similarly, Matheson and coworkers observed that 26% of GBS isolates in their center were resistant to clindamycin.
Neonatal GBS infection is now one of the leading causes for malpractice suits in obstetrics. Key issues presented in these suits include:
- failure to screen
- failure to use the correct culture medium for screening
- failure to obtain test results in a timely manner
- failure to use the correct drug for prophylaxis.
In GBS-positive patients, practitioners should inquire about penicillin allergy and document the exact type of reaction experienced by the patient, if it is accurately known. If the reported reaction to penicillin was not life-threatening, patients should receive cefazolin, 2 g IV initially, then 1 g every 8 hours until delivery. If the reaction to penicillin was immediate and life-threatening, the patient should receive clindamycin, 900 mg IV every 8 hours, if the organism is confirmed to be susceptible. Susceptibility testing should be documented in the medical record.
If such testing is unavailable, vancomycin is the drug of choice.
Susceptibility testing is vital in penicillin-allergic women
Because of observations such as these, the CDC now recommends that clindamycin be used for GBS prophylaxis only if antimicrobial susceptibility tests have confirmed that the organism is sensitive. If susceptibility testing cannot easily be performed, practitioners should use intravenous (IV) vancomycin, 1 g every 12 hours, for prophylaxis. Potential side effects of vancomycin include allergic reactions, gastrointestinal irritation, ototoxicity, and nephrotoxicity. The latter two effects are extremely unlikely in patients who receive only one or two IV doses of the drug.
20% to 30% of gravidas are colonized with GBS
GBS is one of the two major causes of pneumonia, meningitis, and sepsis in both pre-term and term newborns. Approximately 20% to 30% of women are colonized with the organism at some point during pregnancy. Universal screening for GBS at 35 to 37 weeks’ gestation, combined with intrapartum antibiotic prophylaxis, has been highly effective in reducing the frequency of invasive GBS infection.
REFERENCES
1. Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002;51:1-24
2. Edwards RK, Clark P, Sistrom CL, Duff P. Intrapartum antibiotic prophylaxis 1: relative effects of recommended antibiotics on gram-negative pathogens. Obstet Gynecol. 2002;100:534-539
New data suggest that preincision prophylaxis is best for C-section
Sullivan SA, Smith T, Chang E, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized, controlled trial. Am J Obstet Gynecol. 2007;196:455.e1–455.e5.
Is preoperative antibiotic prophylaxis superior to intraoperative prophylaxis in preventing postcesarean infection? Sullivan and colleagues set out to answer this question in a prospective, randomized, double-blinded, placebo-controlled study at the Medical University of South Carolina.
In the study group, 175 women undergoing cesarean delivery were randomized to receive 1 g of IV cefazolin 15 to 60 minutes before surgery, followed by a placebo infusion immediately after the umbilical cord was clamped. In the control group, 182 women received preoperative placebo, followed by 1 g of cefazolin immediately after cord clamping.
Two patients in the study group developed endomyometritis, compared with 10 in the control group (relative risk [RR], 0.2; 95% CI, 0.15–0.94). Five patients in the study group developed a wound infection, compared with 10 in the control group (RR, 0.52; 95% CI, 0.18–1.5, not significant). Overall, eight women in the study group and 21 women in the control group met the criteria for infectious morbidity (RR, 0.4; 95% CI, 0.18–0.87).
There were no differences between the groups in the frequency of neonatal sepsis, neonatal intensive care unit (NICU) admission, total length of hospital stay, metabolic acidosis, or sepsis evaluation. Infants in the study group had significantly fewer days in the NICU (P<.01).
How this study differs from earlier investigations
The classic studies of antibiotic prophylaxis were performed in an animal model by Burke.1 He demonstrated that prophylaxis had its greatest effect when the antibiotic was administered before the surgical incision. Essentially, no effect of prophylaxis was evident when antibiotic administration was delayed more than 4 hours beyond the start of surgery.
Early studies of antibiotic prophylaxis for cesarean delivery, conducted in the 1970s, administered antibiotics preoperatively and continued administration for several days after surgery. In 1979, Gordon and colleagues published an important investigation demonstrating that delay in administration of antibiotics until after the umbilical cord was clamped did not compromise the effectiveness of prophylaxis and significantly decreased the number of infants who required sepsis evaluations.2
This latter effect presumably occurred because infants were not exposed to antibiotics before delivery. Gordon’s investigation and subsequent reports also demonstrated that effective prophylaxis could be achieved with one to three doses of antibiotics.3
Why this new study may alter practice
Before Sullivan and colleagues published their findings, I believe that the best available evidence supported the use of a single dose of antibiotic, such as cefazolin, immediately after cord clamping. There are no convincing data that demonstrate an advantage for extended-spectrum agents (second- and third-generation cephalosporins, broad-spectrum penicillins, or carbapenems) over cefazolin.3
However, if the findings of Sullivan and coworkers are confirmed by other investigations in different patient populations, they definitely should lead to a change in the standard of care for prophylaxis. This investigation was exceptionally well designed and executed. The reduction in the frequency of endomyometritis and overall rate of infectious morbidity was impressive. This advantage was achieved without increasing the rate of neonatal sepsis evaluation.
REFERENCES
1. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168
2. Gordon HR, Phelps D. Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before or after cord clamping. Surgery. 1979;53:151-156
3. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157:794-798
Expect to see more women with diverticulitis as the population ages
Jacobs DO. Diverticulitis. N Engl J Med. 2007;357:2057–2066.
ObGyns continue to play a major role in providing primary care to women. With the steady aging of the American population, practitioners certainly can expect to care for more and more women who are 50 years of age or older, and diverticulitis is likely to turn up in an increasing number of these patients.
Diverticulitis is a relatively common condition in older patients and must consistently be considered in the differential diagnosis of women with acute abdominal pain—particularly left-sided pain.
It is present in approximately 10% of adults younger than 40 years of age and in 40 to 70% of people 80 years of age or older. It primarily affects the sigmoid and descending colon and is associated with diets that are low in fiber and high in refined carbohydrates.
The condition probably results from stasis or obstruction in the narrow neck of a diverticulum, which, in turn, leads to an overgrowth of bacteria. The principal micro-organisms isolated from affected patients are anaerobes, gram-negative aerobes, and some facultative gram-positive bacteria.
Range of severity can be wide
Presentation of diverticulitis may range in severity from mild to moderate lower abdominal pain associated with anorexia, nausea, and vomiting to abscess and fistula formation, colonic stricture, bowel obstruction, and peritonitis (“complicated diverticulitis”). Peritonitis may arise from rupture of a peridiverticular abscess or free rupture of an uninflamed diverticulum. Diverticulitis may be particularly severe in immunocompromised patients.
Classification of disease
The most accepted classification system for diverticulitis is the Hinchey system:
- in stage 1 disease, patients have small and confined pericolic or mesenteric abscesses
- in stage 2, the abscesses are larger but usually remain confined to the pelvis
- in stage 3, an abscess ruptures and causes purulent peritonitis
- stage 4 disease is distinguished by rupture of an uninflamed and unobstructed diverticulum (known as “free rupture”); this stage has the highest risk of adverse outcomes.
CT is best for diagnosis
The most useful diagnostic test for diverticulitis is a computed tomography (CT) scan. As a general rule, endoscopy should be avoided because of the risk of intestinal perforation.
Most patients can be treated as outpatients
Patients who have mild disease usually can be treated as outpatients. They should receive a 7- to 10-day course of oral antibiotics such as ciprofloxacin, 500 to 750 mg every 12 hours, plus metronidazole, 500 mg every 6 to 8 hours.
Alternate oral regimens include metronidazole, 500 mg every 6 to 8 hours, plus trimethoprim-sulfamethoxazole, double-strength, every 12 hours, or amoxicillin-clavulanate, 875 mg every 12 hours.
For seriously ill patients, hospitalization is warranted
Seriously ill patients—particularly those who are immunocompromised—should be hospitalized. If bowel obstruction is present, a nasogastric tube should be inserted. Appropriate IV antibiotic regimens for hospitalized patients include:
- metronidazole, 500 mg every 6 to 8 hours, plus ciprofloxacin, 400 mg every 12 hours
- metronidazole, 500 mg every 6 to 8 hours, plus ceftriaxone, 1 to 2 g every 24 hours
- ampicillin–sulbactam, 3 g every 6 hours
- piperacillin–tazobactam, 3.375 g every 6 hours
- ticarcillin–clavulanate, 3.1 g every 6 hours.
FIGURE 3 Consider diverticulitis in older women who complain of acute abdominal pain
Diverticulitis generally affects the sigmoid colon and descending colon and probably arises from stasis or obstruction in the narrow neck of a diverticulum, which leads to an overgrowth of bacteria and possible rupture.If an abscess is present and fails to respond promptly to medical therapy, drainage may be necessary. Some abscesses can be drained percutaneously under CT guidance. Large abscesses, in association with signs of generalized peritonitis, uncontrolled sepsis, or intestinal perforation, require surgical intervention, either via laparoscopy or open laparotomy. Preliminary data suggest that the laparoscopic approach may result in a shorter hospital stay, decreased postoperative pain, and an overall reduced rate of perioperative complication.
Diverticulitis may mimic appendicitis
The clinical presentation of diverticulitis is similar to that of appendicitis, except that the pain is usually on the left. Perforation, with resulting peritonitis, is an ever-present and potentially life-threatening complication. The dominant organisms are anaerobes and coliforms. The best diagnostic test is CT.
Patients in the early stages of disease can usually be treated as outpatients with antibiotics that are quite familiar to all ObGyns— i.e., metronidazole and a quinolone. More seriously ill patients should be hospitalized and treated with IV antibiotics and nasogastric suctioning.
Consultation with an interventional radiologist and general surgeon is recommended if operative intervention is necessary.
- important new information regarding the effectiveness of hepatitis A vaccine for postexposure prophylaxis
- the need to confirm antimicrobial susceptibility of group B streptococcus (GBS) isolates in pregnant women who are allergic to penicillin
- a new guideline on administering antibiotic prophylaxis for cesarean delivery
- a valuable overview of diverticulitis, a disease that we will all see with increasing regularity as the US population ages
For most, the best hepatitis A postexposure prophylaxis is vaccination
Victor JC, Monto AS, Surdina TY, et al. Hepatitis A vaccine versus immune globulin for postexposure prophylaxis. N Engl J Med. 2007;357:1685–1694.
The objective of this investigation, conducted in Almaty, Kazakhstan, was to compare the relative effectiveness of hepatitis A vaccine with that of immune globulin for prophylaxis after exposure to the hepatitis A virus. Participants were 2 to 40 years old and were household or day-care contacts of people who had hepatitis A. Five hundred sixty-eight susceptible patients received hepatitis A vaccine within 14 days of exposure; 522 susceptible patients received an age-appropriate dose of immune globulin. The primary endpoint was laboratoryconfirmed, symptomatic hepatitis A within 15 to 56 days of exposure.
FIGURE 1 Hepatitis A virus
Hepatitis A virus has single-stranded RNA, no envelope, and is approximately 27–30 nm in diameter.Symptomatic infection occurred in 25 of 568 (4.4%) vaccine recipients and 17 of 522 (3.3%) recipients of immune globulin. The relative risk of infection after the vaccine was 1.35 (95% confidence interval [CI], 0.70–2.67). No serious adverse effects occurred as the result of administration of either the vaccine or immune globulin. The authors concluded that both agents provide effective postexposure prophylaxis against hepatitis A infection.
Hepatitis A is caused by an RNA virus that is transmitted by fecal–oral contact. It is highly contagious and endemic in areas of the world where poverty, poor sanitation, and overcrowded living conditions prevail. Hepatitis A usually causes a symptomatic illness characterized by fever, malaise, anorexia, jaundice, acholic stools, darkened urine, and hepatic pain and tenderness. In poorly nourished or immunocompromised patients, severe morbidity and, rarely, mortality, may occur. Unlike other forms of hepatitis, hepatitis A does not cause a chronic carrier state, and perinatal transmission is extremely unlikely.
Best strategy? Prevention
At present, there is no specific antiviral therapy that is routinely used for treatment of hepatitis A. However, highly effective preventive measures are available. For preexposure prophylaxis, time permitting, the ideal agent is inactivated hepatitis A vaccine.1
The vaccine is usually given in two doses separated by 6 to 12 months and is highly immunogenic. In the United States, key candidates for vaccination are
- gay men
- residents and staff of chronic care facilities
- intravenous drug users
- individuals who live in areas where hepatitis A is endemic
- primate laboratory workers
- people 30 years of age and older who have chronic liver disease
- international travelers
- people who have received a liver transplant or are awaiting one.
The vaccine is safe for administration in pregnancy and is now recommended for children.
After exposure, vaccine trumps immune globulin in healthy patients
The standard agent for prophylaxis after exposure to the hepatitis A virus has been immune globulin 0.02 mL/kg, administered intramuscularly. Immune globulin is highly effective in this application and, in the present investigation, it was slightly more effective than the vaccine.
Despite the modest difference in effectiveness, however, hepatitis A vaccine offers several unique advantages for postexposure prophylaxis:
- It confers long-term immunity rather than just temporary protection.
- Because the volume of fluid injected is lower, the vaccine causes less pain upon administration.
- Immune globulin is now produced by a single manufacturer, and its supply has been limited. Its price also approaches that of the vaccine.
- Administration of immune globulin to a child may disrupt the normal childhood immunization schedule.
In older and immunocompromised patients, use immune globulin
For most patients, hepatitis A vaccine is the indicated method of postexposure immunoprophylaxis.
Because it is slightly more effective, however, immune globulin probably should remain the preferred agent for hepatitis A postexposure prophylaxis in older or immunocompromised patients who are more likely to develop severe illness if they be-come infected.
REFERENCES
We’re not following guidelines on GBS prophylaxis in penicillin allergy
Matheson KA, Lievense SP, Catanzaro B, Phipps MG. Intrapartum group B streptococci prophylaxis in patients reporting a penicillin allergy. Obstet Gynecol. 2008;111:356–364.
In this study, conducted at a single institution (Brown University), Matheson and colleagues sought to assess the adequacy of prophylaxis for GBS infection in women who had an allergy to penicillin. Specifically, the authors sought to determine how well practitioners at their institution adhered to the 2002 Centers for Disease Control and Prevention (CDC) guidelines, which specify that cefazolin should be used for prophylaxis in patients who are penicillin-allergic but not at high risk for anaphylaxis.1 For patients at high risk for anaphylaxis, clindamycin may be used for prophylaxis if the organism is known to be susceptible. If susceptibility has not been documented, vancomycin should be administered.1
Overall, 95% of GBS-positive, penicillin-allergic patients received prophylaxis (95% CI, 91–97). However, only 15% of these women received appropriate prophylaxis as defined by the CDC (95% CI, 11–12). Clindamycin was administered to 83% of patients, but susceptibility testing was performed in only 11%. At the time of this study, 26% of all GBS isolates at Brown were resistant to clindamycin; 37% were resistant to erythromycin.
The authors concluded that adherence to CDC guidelines was clearly less than optimal. Even at 1 year after adoption of the guidelines, only 20% of patients received appropriate prophylaxis.
Type of allergic reaction is key to selection of prophylactic agent
GBS is uniformly sensitive to penicillin and ampicillin. It also is 100% sensitive to cefazolin, the preferred drug for intrapartum prophylaxis in penicillin-allergic women who have a low risk of anaphylactic reaction to penicillin.
FIGURE 2 Group B streptococcus
A clear zone of hemolysis on blood agar is a key characteristic of group B streptococcus.However, it probably is better to avoid cephalosporins in patients who report a previous anaphylactic reaction to penicillin or ampicillin, even though the risk of cross-reactivity between penicillin and cephalosporin is low. In such patients, possible alternatives include erythromycin, clindamycin, and vancomycin.
Erythromycin is no longer recommended
At the University of Florida, we reported that 21% of GBS strains were resistant to erythromycin.2 At Brown University, Matheson and colleagues reported that 37% of GBS isolates were resistant to erythromycin. On the basis of similar reports, the CDC has concluded that erythromycin no longer should be used for GBS prophylaxis.
At our institution, we also have noted a disturbing trend of increased GBS resistance to clindamycin. In our recent report, 9% of GBS strains were resistant to this antibiotic. Similarly, Matheson and coworkers observed that 26% of GBS isolates in their center were resistant to clindamycin.
Neonatal GBS infection is now one of the leading causes for malpractice suits in obstetrics. Key issues presented in these suits include:
- failure to screen
- failure to use the correct culture medium for screening
- failure to obtain test results in a timely manner
- failure to use the correct drug for prophylaxis.
In GBS-positive patients, practitioners should inquire about penicillin allergy and document the exact type of reaction experienced by the patient, if it is accurately known. If the reported reaction to penicillin was not life-threatening, patients should receive cefazolin, 2 g IV initially, then 1 g every 8 hours until delivery. If the reaction to penicillin was immediate and life-threatening, the patient should receive clindamycin, 900 mg IV every 8 hours, if the organism is confirmed to be susceptible. Susceptibility testing should be documented in the medical record.
If such testing is unavailable, vancomycin is the drug of choice.
Susceptibility testing is vital in penicillin-allergic women
Because of observations such as these, the CDC now recommends that clindamycin be used for GBS prophylaxis only if antimicrobial susceptibility tests have confirmed that the organism is sensitive. If susceptibility testing cannot easily be performed, practitioners should use intravenous (IV) vancomycin, 1 g every 12 hours, for prophylaxis. Potential side effects of vancomycin include allergic reactions, gastrointestinal irritation, ototoxicity, and nephrotoxicity. The latter two effects are extremely unlikely in patients who receive only one or two IV doses of the drug.
20% to 30% of gravidas are colonized with GBS
GBS is one of the two major causes of pneumonia, meningitis, and sepsis in both pre-term and term newborns. Approximately 20% to 30% of women are colonized with the organism at some point during pregnancy. Universal screening for GBS at 35 to 37 weeks’ gestation, combined with intrapartum antibiotic prophylaxis, has been highly effective in reducing the frequency of invasive GBS infection.
REFERENCES
1. Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002;51:1-24
2. Edwards RK, Clark P, Sistrom CL, Duff P. Intrapartum antibiotic prophylaxis 1: relative effects of recommended antibiotics on gram-negative pathogens. Obstet Gynecol. 2002;100:534-539
New data suggest that preincision prophylaxis is best for C-section
Sullivan SA, Smith T, Chang E, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized, controlled trial. Am J Obstet Gynecol. 2007;196:455.e1–455.e5.
Is preoperative antibiotic prophylaxis superior to intraoperative prophylaxis in preventing postcesarean infection? Sullivan and colleagues set out to answer this question in a prospective, randomized, double-blinded, placebo-controlled study at the Medical University of South Carolina.
In the study group, 175 women undergoing cesarean delivery were randomized to receive 1 g of IV cefazolin 15 to 60 minutes before surgery, followed by a placebo infusion immediately after the umbilical cord was clamped. In the control group, 182 women received preoperative placebo, followed by 1 g of cefazolin immediately after cord clamping.
Two patients in the study group developed endomyometritis, compared with 10 in the control group (relative risk [RR], 0.2; 95% CI, 0.15–0.94). Five patients in the study group developed a wound infection, compared with 10 in the control group (RR, 0.52; 95% CI, 0.18–1.5, not significant). Overall, eight women in the study group and 21 women in the control group met the criteria for infectious morbidity (RR, 0.4; 95% CI, 0.18–0.87).
There were no differences between the groups in the frequency of neonatal sepsis, neonatal intensive care unit (NICU) admission, total length of hospital stay, metabolic acidosis, or sepsis evaluation. Infants in the study group had significantly fewer days in the NICU (P<.01).
How this study differs from earlier investigations
The classic studies of antibiotic prophylaxis were performed in an animal model by Burke.1 He demonstrated that prophylaxis had its greatest effect when the antibiotic was administered before the surgical incision. Essentially, no effect of prophylaxis was evident when antibiotic administration was delayed more than 4 hours beyond the start of surgery.
Early studies of antibiotic prophylaxis for cesarean delivery, conducted in the 1970s, administered antibiotics preoperatively and continued administration for several days after surgery. In 1979, Gordon and colleagues published an important investigation demonstrating that delay in administration of antibiotics until after the umbilical cord was clamped did not compromise the effectiveness of prophylaxis and significantly decreased the number of infants who required sepsis evaluations.2
This latter effect presumably occurred because infants were not exposed to antibiotics before delivery. Gordon’s investigation and subsequent reports also demonstrated that effective prophylaxis could be achieved with one to three doses of antibiotics.3
Why this new study may alter practice
Before Sullivan and colleagues published their findings, I believe that the best available evidence supported the use of a single dose of antibiotic, such as cefazolin, immediately after cord clamping. There are no convincing data that demonstrate an advantage for extended-spectrum agents (second- and third-generation cephalosporins, broad-spectrum penicillins, or carbapenems) over cefazolin.3
However, if the findings of Sullivan and coworkers are confirmed by other investigations in different patient populations, they definitely should lead to a change in the standard of care for prophylaxis. This investigation was exceptionally well designed and executed. The reduction in the frequency of endomyometritis and overall rate of infectious morbidity was impressive. This advantage was achieved without increasing the rate of neonatal sepsis evaluation.
REFERENCES
1. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161-168
2. Gordon HR, Phelps D. Blanchard K. Prophylactic cesarean section antibiotics: maternal and neonatal morbidity before or after cord clamping. Surgery. 1979;53:151-156
3. Duff P. Prophylactic antibiotics for cesarean delivery: a simple cost-effective strategy for prevention of postoperative morbidity. Am J Obstet Gynecol. 1987;157:794-798
Expect to see more women with diverticulitis as the population ages
Jacobs DO. Diverticulitis. N Engl J Med. 2007;357:2057–2066.
ObGyns continue to play a major role in providing primary care to women. With the steady aging of the American population, practitioners certainly can expect to care for more and more women who are 50 years of age or older, and diverticulitis is likely to turn up in an increasing number of these patients.
Diverticulitis is a relatively common condition in older patients and must consistently be considered in the differential diagnosis of women with acute abdominal pain—particularly left-sided pain.
It is present in approximately 10% of adults younger than 40 years of age and in 40 to 70% of people 80 years of age or older. It primarily affects the sigmoid and descending colon and is associated with diets that are low in fiber and high in refined carbohydrates.
The condition probably results from stasis or obstruction in the narrow neck of a diverticulum, which, in turn, leads to an overgrowth of bacteria. The principal micro-organisms isolated from affected patients are anaerobes, gram-negative aerobes, and some facultative gram-positive bacteria.
Range of severity can be wide
Presentation of diverticulitis may range in severity from mild to moderate lower abdominal pain associated with anorexia, nausea, and vomiting to abscess and fistula formation, colonic stricture, bowel obstruction, and peritonitis (“complicated diverticulitis”). Peritonitis may arise from rupture of a peridiverticular abscess or free rupture of an uninflamed diverticulum. Diverticulitis may be particularly severe in immunocompromised patients.
Classification of disease
The most accepted classification system for diverticulitis is the Hinchey system:
- in stage 1 disease, patients have small and confined pericolic or mesenteric abscesses
- in stage 2, the abscesses are larger but usually remain confined to the pelvis
- in stage 3, an abscess ruptures and causes purulent peritonitis
- stage 4 disease is distinguished by rupture of an uninflamed and unobstructed diverticulum (known as “free rupture”); this stage has the highest risk of adverse outcomes.
CT is best for diagnosis
The most useful diagnostic test for diverticulitis is a computed tomography (CT) scan. As a general rule, endoscopy should be avoided because of the risk of intestinal perforation.
Most patients can be treated as outpatients
Patients who have mild disease usually can be treated as outpatients. They should receive a 7- to 10-day course of oral antibiotics such as ciprofloxacin, 500 to 750 mg every 12 hours, plus metronidazole, 500 mg every 6 to 8 hours.
Alternate oral regimens include metronidazole, 500 mg every 6 to 8 hours, plus trimethoprim-sulfamethoxazole, double-strength, every 12 hours, or amoxicillin-clavulanate, 875 mg every 12 hours.
For seriously ill patients, hospitalization is warranted
Seriously ill patients—particularly those who are immunocompromised—should be hospitalized. If bowel obstruction is present, a nasogastric tube should be inserted. Appropriate IV antibiotic regimens for hospitalized patients include:
- metronidazole, 500 mg every 6 to 8 hours, plus ciprofloxacin, 400 mg every 12 hours
- metronidazole, 500 mg every 6 to 8 hours, plus ceftriaxone, 1 to 2 g every 24 hours
- ampicillin–sulbactam, 3 g every 6 hours
- piperacillin–tazobactam, 3.375 g every 6 hours
- ticarcillin–clavulanate, 3.1 g every 6 hours.
FIGURE 3 Consider diverticulitis in older women who complain of acute abdominal pain
Diverticulitis generally affects the sigmoid colon and descending colon and probably arises from stasis or obstruction in the narrow neck of a diverticulum, which leads to an overgrowth of bacteria and possible rupture.If an abscess is present and fails to respond promptly to medical therapy, drainage may be necessary. Some abscesses can be drained percutaneously under CT guidance. Large abscesses, in association with signs of generalized peritonitis, uncontrolled sepsis, or intestinal perforation, require surgical intervention, either via laparoscopy or open laparotomy. Preliminary data suggest that the laparoscopic approach may result in a shorter hospital stay, decreased postoperative pain, and an overall reduced rate of perioperative complication.
Diverticulitis may mimic appendicitis
The clinical presentation of diverticulitis is similar to that of appendicitis, except that the pain is usually on the left. Perforation, with resulting peritonitis, is an ever-present and potentially life-threatening complication. The dominant organisms are anaerobes and coliforms. The best diagnostic test is CT.
Patients in the early stages of disease can usually be treated as outpatients with antibiotics that are quite familiar to all ObGyns— i.e., metronidazole and a quinolone. More seriously ill patients should be hospitalized and treated with IV antibiotics and nasogastric suctioning.
Consultation with an interventional radiologist and general surgeon is recommended if operative intervention is necessary.
INFECTIOUS DISEASE
Four studies caught my eye this past year. The first describes the use of systematic methodology to confirm the diagnosis of primary cytomegalovirus (CMV) infection in pregnancy and lower the rate of unnecessary pregnancy termination. Investigators were able to reclassify approximately 70% of women who had been diagnosed with CMV infection and reduce the number of pregnancy terminations by 73%.
Two other studies help define the emerging problem of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection, when to look for it, and how to treat it. In the first, researchers isolated S. aureus from the wounds of 320 patients with community-acquired infection and tested the samples for methicillin resistance, finding a prevalence of 59%. In the second study, investigators analyzed culture specimens from pregnant women for the presence of group B streptococci and S. aureus colonization. They found colonization with group B streptococci to be significantly associated with S. aureus colonization, with a prevalence odds ratio of 2.1.
The fourth study concerns the human papillomavirus (HPV) vaccine. Women given an HPV-16 L1 virus-like particle vaccine and followed for 4 years remained 100% free of cervical intraepithelial neoplasia (CIN) grades 2 and 3, unlike women who received placebo.
I believe these 4 studies represent the most significant developments of the past year in the field of infectious disease.
Don’t rush a diagnosis of CMV infection in pregnancy
Guerra B, Simonazzi G, Banfi A, et al. Impact of diagnostic and confirmatory tests and prenatal counseling on the rate of pregnancy termination among women with positive cytomegalovirus immunoglobulin M antibody titers. Am J Obstet Gynecol. 2007;196:221.e1–6.
CMV infection is a common and important perinatal pathogen. Each year in the United States, approximately 1% of gravidas acquire primary infection. Of these, about 40% transmit infection to the fetus. The rate of transmission is highest when maternal infection occurs in the third trimester, but the risk of serious fetal injury is greatest when maternal infection occurs in the first trimester. Ten percent to 20% of congenitally infected infants are acutely symptomatic at birth. Approximately 20% of these newborns die; most survivors have serious long-term complications. In contrast, CMV infection that recurs during pregnancy poses only minimal risk to the baby.1
Many women choose to have their pregnancy terminated when they learn they have a primary CMV infection.
Details of the study
This retrospective study was designed to determine whether a systematic diagnostic algorithm reduces the rate of unnecessary abortion in women who have apparent acute CMV infection during pregnancy. Guerra and colleagues evaluated 1,857 consecutive patients in practices in Italy who had a positive anti-CMV immunoglobulin M (IgM) antibody assay in the first or second trimester and were referred to a tertiary care facility for further diagnostic testing. Universal screening for CMV is now common among practitioners in Italy, and virtually all of these patients were completely asymptomatic.
At the tertiary facility, investigators tested again for CMV-specific IgM, as well as IgG, by enzyme immunoassay. They also tested for IgM by immunoblot and determined the avidity of anti-CMV IgG. Women who had IgG of low or moderate avidity with confirmed IgM, and those who clearly seroconverted to IgG were assumed to have a primary infection.
Women who were positive for IgM with high-avidity IgG were assumed to have nonprimary infection. Women who were seronegative for both antibodies were classified as uninfected. Those who were IgM-negative with high-avidity IgG were classified as previously infected. Women with an acute infection were then counseled by a specialist and offered amniocentesis and targeted ultrasonography.
Only 11.9% of women with primary infection chose abortion
Of the 1,857 women in this study, 445 were classified as having primary infection (group 1); 53 (11.9%) women elected to terminate their pregnancy. At autopsy, 38 of the 53 fetuses were found to be infected. In the other 15 cases, the pregnancy was terminated in the first trimester, and postmortem examination was not performed.
In the 1,205 women found to have nonprimary infection or previous infection (group 2), only 5 (0.4%) had the pregnancy terminated in the first trimester, and no postmortem examinations were performed. The difference in the observed rates of abortion between groups 1 and 2 was highly significant (P<.001).
Given their observations in group 1, the authors estimated that, on the basis of the initial screening tests at the referring institutions, approximately 196 (11.9%) of all patients in groups 1 and 2 would have elected abortion. By using confirmatory tests combined with counseling by a specialist, the authors were able to reduce the number of abortions from 196 to 53, a 73% decrease.
Always confirm an initial diagnosis
Given the ominous prognosis for congenital CMV infection and the major psychological implications and sobering finality of abortion, it is imperative that clinicians confirm the diagnosis of primary CMV infection. Because most cases of CMV infection in immunocompetent adults are asymptomatic, the diagnosis is typically confirmed by serology. Unfortunately, the serologic tests for CMV are not as straight-forward and reliable as tests for other viral infections such as rubella. Commercially available tests for anti-CMV IgM often have false-positive and false-negative results. In addition, IgM antibody may be detected as long as 9 months after a primary infection and may subsequently re-appear during reactivation of a latent infection or reinfection.2,3
Be selective, on the basis of risk factors and clinical manifestations, when screening pregnant women for cytomegalovirus infection.
Routine screening is not necessary
The authors’ findings vividly illustrate the potential errors that can occur when a large number of asymptomatic patients are routinely screened for CMV. Because of these pitfalls, I do not recommend routine screening. Rather, screening should be selective, directed at women who:
- have clinical manifestations of CMV infection
- are immunosuppressed
- have small children in daycare or work in daycare themselves or
- have documented exposure to someone with CMV infection.
If the initial immunoassay for CMV IgM is positive, a confirmatory immunoblot test for IgM should be performed, as well as avidity testing for IgG.
If primary infection is confirmed, the patient should undergo targeted ultrasonography and amniocentesis to assess for manifestations of congenital infection and to detect CMV in amniotic fluid by culture or polymerase chain reaction (PCR) testing. If the sonogram shows signs of fetal injury, or the PCR test is positive, the woman should be counseled about the options, which include experimental immunotherapy with hyperimmune anti-CMV globulin4 and pregnancy termination.
The study by Guerra and colleagues is a welcome addition to the obstetric literature. By using a systematic diagnostic algorithm that included an enzyme-linked immunosorbent assay and an immunoblot assay for IgM antibody and avidity testing for IgG antibody, the authors were able to reclassify approximately 70% of patients as either uninfected or previously infected. As a result, they reduced the number of pregnancy terminations by 73%, an objective end-point that clearly has great social, economic, and medical impact.
Most community S. aureus infections are methicillin-resistant
Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666–674.
Moran and colleagues reviewed the records of 422 adults with acute purulent and soft-tissue infections who were evaluated in 11 university-affiliated emergency departments in August 2004. Wounds were routinely cultured. When S. aureus was isolated, the organisms were tested for antimicrobial susceptibility to identify those that were methicillin-resistant. The PCR test was used to identify genes for staphylococcal enterotoxins A through E and H, toxic shock syndrome toxin, and Panton–Valentin leukocidin. The same methodology was used to identify the gene complex staphylococcal cassette chromosome mec (SCCmec). This complex contains the mecA gene that confers methicillin resistance.
Of the 422 patients, 320 (76%) had S. aureus isolated from their wound. The prevalence of methicillin resistance was 59%. Ninety-seven percent of MRSA isolates were pulsed-field type USA 300. SCCmec type IV and the Panton–Valentin leukocidin gene were detected in 98% of MRSA isolates. Other toxin genes were rare.
Only 2 drugs were 100% effective
Among MRSA isolates, 100% were susceptible to rifampin and trimethoprim-sulfamethoxazole (TMP-SMX), 95% were susceptible to clindamycin, and 92% were sensitive to tetracycline. Only 60% were sensitive to fluoroquinolones, and only 6% were sensitive to erythromycin. Only 43% of patients received initial empiric therapy with antibiotics to which their organisms were sensitive.
Reason to worry
S. aureus is an important pathogen in obstetric patients. It is the causative organism of toxic shock syndrome and the dominant pathogen in patients with puerperal mastitis, as well as one of the key causes of postoperative wound infection. When penicillin was developed in 1941, all strains of S. aureus were sensitive to the drug. Within a few short years, however, most hospital-acquired strains became resistant.
Methicillin was introduced in 1961 to treat these resistant staphylococcal species. Unfortunately, by the mid-1960s, methicillin-resistant S. aureus (MRSA) infections began to appear. By the 1990s, MRSA infections were common in hospitalized patients, particularly in intensive care units. Hospital-acquired MRSA isolates are often sensitive to only a few select antibiotics such as vancomycin, linezolid, and quinupristin/dalfopristin.5
In the late 1990s and early 2000s, MRSA began to appear in community-acquired infections in both adults and children. Most of these isolates have been implicated in skin and soft-tissue infections, but some have been responsible for invasive infection, bacteremia, and even death.6 Compared with hospital-acquired MRSA, these community isolates are more likely to be sensitive to commonly used antibiotics.
Always culture an infected wound
Knowledge of these sensitivity patterns is of great importance. Regrettably, as noted by Moran and associates, more than half of the patients (57%) were initially treated with antibiotics to which their infecting organism was resistant.
The clinical implications are clear:
- We must be aware that many community-acquired soft-tissue infections will be caused by drug-resistant staphylococci.
- Because antibiotic resistance is so prevalent, a culture of the infected wound should be obtained routinely so that antimicrobial therapy can be modified if the patient fails to respond to initial treatment.
- Antibiotic therapy alone is rarely sufficient for abscesses in the soft tissue and skin; adequate surgical drainage is essential.
- Fundamental infection-control measures, such as careful handwashing, adequate skin preparation prior to surgery, and local wound care, are of greater importance than ever.
Most cases of community-acquired MRSA have been isolated from skin and soft tissue; surgical drainage is necessary when infection advances to abscess in those sites.
In gravidas with group B strep, look for S. aureus
Chen KT, Huard RC, Della-Latta P, Saiman L. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet Gynecol. 2006;108:482–487.
To assess the prevalence of methicillin-sensitive and community-acquired methicillin-resistant S. aureus colonization in pregnant women, Chen and colleagues evaluated de-identified culture specimens that had originally been submitted to the microbiology laboratory for identification of group B streptococcal infection. As opposed to hospital-associated MRSA isolates, community-associated methicillin-resistant strains were defined as those possessing the type IV or V staphylococcal chromosomal cassette mec element and lacking a multi-drug-resistant phenotype.
Of the 2,963 culture specimens in the prospective surveillance study, 743 (25%) were positive for group B streptococci, and 507 (17%) were positive for S. aureus. Group B streptococcal colonization was significantly associated with S. aureus colonization; the prevalence odds ratio was 2.1. Fourteen of the 507 S. aureus isolates were methicillin-resistant (2.8%; 95% confidence interval [CI] 1.4–4.2%). Thirteen of the 14 strains (93%) were community-acquired.
S. aureus may cause sepsis, wound infection, bacteremia, and other ills
The unique feature of this study is the observation that vaginal colonization with group B streptococci was significantly associated with colonization with S. aureus—one of the possible causative pathogens in chorioamnionitis, endometritis, wound infection, bacteremia, puerperal mastitis, and toxic shock syndrome. The organism also may cause serious neonatal infection, particularly sepsis.
The prevalence of group B streptococcal colonization in this study (25.1%, 95% CI 23.5–26.7%) is comparable to data reported from several other investigators.7 Colonized women are at increased risk for chorioamnionitis and puerperal endometritis, and their infants are at increased risk of sepsis, pneumonia, and meningitis. Fortunately, intrapartum antibiotic prophylaxis significantly reduces the risk of both maternal and neonatal group B streptococcal infection.8
As I noted earlier in this update, the antimicrobial susceptibility of S. aureus has become increasingly limited, particularly in light of the recent increase in both hospital- and community-acquired methicillin-resistant strains. In this study by Chen and colleagues, 2.8% of S. aureus isolates were methicillin-resistant. Of these, all but one were community-acquired.
Clinical suggestions
These findings certainly do not indicate the need for routine cultures for S. aureus vaginal colonization in all pregnant women. Nor are cultures needed in women who test positive for group B streptococci at 35 to 37 weeks. However, clinicians should be alert for possible staphylococcal infections, such as wound abscess, furuncle, carbuncle, or mastitis, in these women. If such an infection appears, obtain a culture of the purulent collection. Pending the result, treat the patient empirically with a drug that is likely to be effective against community-acquired MRSA. One hundred percent of these strains are sensitive to rifampin and TMP-SMX, and 90% to 95% are sensitive to tetracycline.9
Univalent HPV vaccine is 100% effective against CIN grades 2, 3
Mao C, Koutsky LA, Ault KA, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia. Obstet Gynecol. 2006;107:18–27.
Mao and colleagues set out to assess the long-term protection of a univalent HPV vaccine against CIN grades 2, 3. Their prospective, randomized, double-blind, placebo-controlled trial involved 2,391 women, aged 16 to 23 years, who received either 40 μg of HPV-16 L1 virus-like particle vaccine or placebo intramuscularly at day 1, month 2, and month 6. Genital samples for HPV-16 DNA and cervical cytology specimens were collected at day 1, month 7, and then every 6 months for 48 months. A radioimmunoassay was used to assess antibody titers to HPV-16.
Of the 750 women who received placebo, 6 developed HPV-16–related CIN 2, and 6 developed CIN 3. Among the 755 vaccinated women, no cases of CIN occurred. Thus, the vaccine was 100% effective in this trial (95% CI 65–100%).
Among women who received placebo, 111 cases of persistent HPV-16 infection occurred, compared with 7 cases in vaccinated women (vaccine efficacy 94%; 95% CI 88–98%).
Following immunization, antibody to HPV-16 peaked at month 7, declined through month 18, and remained stable between months 30 and 48.
Any effective vaccine is important
Because 3,500 to 4,000 women still die from cervical cancer each year in the United States, and almost 274,000 die worldwide, the development of any HPV vaccine that provides lasting protection against CIN is important.
The vaccine evaluated by Mao and colleagues targeted a single strain of HPV, genotype 16. The recently approved quadrivalent vaccine, Gardasil, targets types 6, 11, 16, and 18. Of the more than 100 genotypes of HPV that have been discovered, approximately 30 are present in the mucosa of the genital tract, and 15 of these 30 are associated with cervical cancer. However, 2 HPV strains—types 16 and 18—are responsible for about two thirds of all cases of cervical cancer; 90% of genital warts cases result from infection with types 6 and 11.10
Emphasize to patients that preexisting cytologic abnormalities and genital warts don’t respond to vaccination against human papillomavirus.The Advisory Committee on Immunization Practices recommends that the quadrivalent vaccine be given to girls at age 11 or 12 years, prior to the onset of sexual activity, to be maximally effective against all 4 genotypes included in the vaccine.10
If a woman is infected with HPV prior to vaccination, she may develop abnormal cervical cytology related to the genotypes in the vaccine, as well as genotypes not included. Nevertheless, ACOG recommends that the vaccine be considered in all females ages 9 to 26.11 HPV genotyping is not recommended before giving the vaccine because any type of routine screening reduces the cost-effectiveness of the vaccination program.10
Fundamentals of vaccination
The quadrivalent vaccine must be administered intramuscularly (0.5 mL) in 3 doses on day 1 and at 2 and 6 months. The principal adverse effect is a local reaction such as pain, swelling, or pruritus at the injection site. Low-grade fever occurs in approximately 10% of patients.
Although the vaccine is classified by the FDA as pregnancy category B, the manufacturer recommends against its use during pregnancy. It may be administered to lactating women, however. The approximate cost of the 3-dose series, including administration fees, is $400 to $500.
It’s a vaccine, not a treatment
Patients need to understand that vaccination is not a treatment for preexisting cytologic abnormalities or genital warts. Nor can it be expected to be perfectly protective over a person’s lifetime against infection caused by genotypes 6, 11, 16, and 18. Women must continue to have regular cytologic screening. No reliable scientific data suggest that vaccination of young girls will increase sexual promiscuity in the adolescent population.10
The author reports no financial relationships relevant to this article.
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Munro SC, Hall B, Whybin LR, et al. Diagnosis of and screening for cytomegalovirus infection in pregnant women. J Clin Microbiol. 2005;431:4713-4718.
3. Lazzarotto T, Gabrielli L, Lanari M, et al. Congenital cytomegalovirus infection: recent advances in the diagnosis of maternal infection. Hum Immunol. 2004;65:410-415.
4. Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
5. Gibbs RS. Emerging infections in obstetric and gynecologic practice. Obstet Gynecol. 2006;108:480-481.
6. Laible VR, Sheffield JS, Roberts S, McIntire DD, Trevino S, Wendel GD. Clinical presentation of community-acquired methicillin-resistant Staphylococcus aureus in pregnancy. Obstet Gynecol. 2005;106:461-465.
7. Edwards RK, Clark P, Duff P. Intrapartum antibiotic prophylaxis 2: positive predictive value of antenatal group B streptococcal cultures and antibiotic susceptibility of clinical isolates. Obstet Gynecol. 2002;100:590-594.
8. Locksmith GJ, Clark P, Duff P. Maternal and neonatal infection rates with three different protocols for prevention of group B streptococcal disease. Am J Obstet Gynecol. 1999;180:416-422.
9. Moran GJ, Krisnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666-674.
10. Monk BJ, Wiley DJ. Will human papillomavirus prophylactic vaccination change sexual practices of adolescent and young adult women in America? Obstet Gynecol. 2006;108:420-424.
11. Human papillomavirus vaccination. ACOG Committee Opinion #344. Washington, DC: American College of Obstetricians and Gynecologists; September 2006.
Four studies caught my eye this past year. The first describes the use of systematic methodology to confirm the diagnosis of primary cytomegalovirus (CMV) infection in pregnancy and lower the rate of unnecessary pregnancy termination. Investigators were able to reclassify approximately 70% of women who had been diagnosed with CMV infection and reduce the number of pregnancy terminations by 73%.
Two other studies help define the emerging problem of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection, when to look for it, and how to treat it. In the first, researchers isolated S. aureus from the wounds of 320 patients with community-acquired infection and tested the samples for methicillin resistance, finding a prevalence of 59%. In the second study, investigators analyzed culture specimens from pregnant women for the presence of group B streptococci and S. aureus colonization. They found colonization with group B streptococci to be significantly associated with S. aureus colonization, with a prevalence odds ratio of 2.1.
The fourth study concerns the human papillomavirus (HPV) vaccine. Women given an HPV-16 L1 virus-like particle vaccine and followed for 4 years remained 100% free of cervical intraepithelial neoplasia (CIN) grades 2 and 3, unlike women who received placebo.
I believe these 4 studies represent the most significant developments of the past year in the field of infectious disease.
Don’t rush a diagnosis of CMV infection in pregnancy
Guerra B, Simonazzi G, Banfi A, et al. Impact of diagnostic and confirmatory tests and prenatal counseling on the rate of pregnancy termination among women with positive cytomegalovirus immunoglobulin M antibody titers. Am J Obstet Gynecol. 2007;196:221.e1–6.
CMV infection is a common and important perinatal pathogen. Each year in the United States, approximately 1% of gravidas acquire primary infection. Of these, about 40% transmit infection to the fetus. The rate of transmission is highest when maternal infection occurs in the third trimester, but the risk of serious fetal injury is greatest when maternal infection occurs in the first trimester. Ten percent to 20% of congenitally infected infants are acutely symptomatic at birth. Approximately 20% of these newborns die; most survivors have serious long-term complications. In contrast, CMV infection that recurs during pregnancy poses only minimal risk to the baby.1
Many women choose to have their pregnancy terminated when they learn they have a primary CMV infection.
Details of the study
This retrospective study was designed to determine whether a systematic diagnostic algorithm reduces the rate of unnecessary abortion in women who have apparent acute CMV infection during pregnancy. Guerra and colleagues evaluated 1,857 consecutive patients in practices in Italy who had a positive anti-CMV immunoglobulin M (IgM) antibody assay in the first or second trimester and were referred to a tertiary care facility for further diagnostic testing. Universal screening for CMV is now common among practitioners in Italy, and virtually all of these patients were completely asymptomatic.
At the tertiary facility, investigators tested again for CMV-specific IgM, as well as IgG, by enzyme immunoassay. They also tested for IgM by immunoblot and determined the avidity of anti-CMV IgG. Women who had IgG of low or moderate avidity with confirmed IgM, and those who clearly seroconverted to IgG were assumed to have a primary infection.
Women who were positive for IgM with high-avidity IgG were assumed to have nonprimary infection. Women who were seronegative for both antibodies were classified as uninfected. Those who were IgM-negative with high-avidity IgG were classified as previously infected. Women with an acute infection were then counseled by a specialist and offered amniocentesis and targeted ultrasonography.
Only 11.9% of women with primary infection chose abortion
Of the 1,857 women in this study, 445 were classified as having primary infection (group 1); 53 (11.9%) women elected to terminate their pregnancy. At autopsy, 38 of the 53 fetuses were found to be infected. In the other 15 cases, the pregnancy was terminated in the first trimester, and postmortem examination was not performed.
In the 1,205 women found to have nonprimary infection or previous infection (group 2), only 5 (0.4%) had the pregnancy terminated in the first trimester, and no postmortem examinations were performed. The difference in the observed rates of abortion between groups 1 and 2 was highly significant (P<.001).
Given their observations in group 1, the authors estimated that, on the basis of the initial screening tests at the referring institutions, approximately 196 (11.9%) of all patients in groups 1 and 2 would have elected abortion. By using confirmatory tests combined with counseling by a specialist, the authors were able to reduce the number of abortions from 196 to 53, a 73% decrease.
Always confirm an initial diagnosis
Given the ominous prognosis for congenital CMV infection and the major psychological implications and sobering finality of abortion, it is imperative that clinicians confirm the diagnosis of primary CMV infection. Because most cases of CMV infection in immunocompetent adults are asymptomatic, the diagnosis is typically confirmed by serology. Unfortunately, the serologic tests for CMV are not as straight-forward and reliable as tests for other viral infections such as rubella. Commercially available tests for anti-CMV IgM often have false-positive and false-negative results. In addition, IgM antibody may be detected as long as 9 months after a primary infection and may subsequently re-appear during reactivation of a latent infection or reinfection.2,3
Be selective, on the basis of risk factors and clinical manifestations, when screening pregnant women for cytomegalovirus infection.
Routine screening is not necessary
The authors’ findings vividly illustrate the potential errors that can occur when a large number of asymptomatic patients are routinely screened for CMV. Because of these pitfalls, I do not recommend routine screening. Rather, screening should be selective, directed at women who:
- have clinical manifestations of CMV infection
- are immunosuppressed
- have small children in daycare or work in daycare themselves or
- have documented exposure to someone with CMV infection.
If the initial immunoassay for CMV IgM is positive, a confirmatory immunoblot test for IgM should be performed, as well as avidity testing for IgG.
If primary infection is confirmed, the patient should undergo targeted ultrasonography and amniocentesis to assess for manifestations of congenital infection and to detect CMV in amniotic fluid by culture or polymerase chain reaction (PCR) testing. If the sonogram shows signs of fetal injury, or the PCR test is positive, the woman should be counseled about the options, which include experimental immunotherapy with hyperimmune anti-CMV globulin4 and pregnancy termination.
The study by Guerra and colleagues is a welcome addition to the obstetric literature. By using a systematic diagnostic algorithm that included an enzyme-linked immunosorbent assay and an immunoblot assay for IgM antibody and avidity testing for IgG antibody, the authors were able to reclassify approximately 70% of patients as either uninfected or previously infected. As a result, they reduced the number of pregnancy terminations by 73%, an objective end-point that clearly has great social, economic, and medical impact.
Most community S. aureus infections are methicillin-resistant
Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666–674.
Moran and colleagues reviewed the records of 422 adults with acute purulent and soft-tissue infections who were evaluated in 11 university-affiliated emergency departments in August 2004. Wounds were routinely cultured. When S. aureus was isolated, the organisms were tested for antimicrobial susceptibility to identify those that were methicillin-resistant. The PCR test was used to identify genes for staphylococcal enterotoxins A through E and H, toxic shock syndrome toxin, and Panton–Valentin leukocidin. The same methodology was used to identify the gene complex staphylococcal cassette chromosome mec (SCCmec). This complex contains the mecA gene that confers methicillin resistance.
Of the 422 patients, 320 (76%) had S. aureus isolated from their wound. The prevalence of methicillin resistance was 59%. Ninety-seven percent of MRSA isolates were pulsed-field type USA 300. SCCmec type IV and the Panton–Valentin leukocidin gene were detected in 98% of MRSA isolates. Other toxin genes were rare.
Only 2 drugs were 100% effective
Among MRSA isolates, 100% were susceptible to rifampin and trimethoprim-sulfamethoxazole (TMP-SMX), 95% were susceptible to clindamycin, and 92% were sensitive to tetracycline. Only 60% were sensitive to fluoroquinolones, and only 6% were sensitive to erythromycin. Only 43% of patients received initial empiric therapy with antibiotics to which their organisms were sensitive.
Reason to worry
S. aureus is an important pathogen in obstetric patients. It is the causative organism of toxic shock syndrome and the dominant pathogen in patients with puerperal mastitis, as well as one of the key causes of postoperative wound infection. When penicillin was developed in 1941, all strains of S. aureus were sensitive to the drug. Within a few short years, however, most hospital-acquired strains became resistant.
Methicillin was introduced in 1961 to treat these resistant staphylococcal species. Unfortunately, by the mid-1960s, methicillin-resistant S. aureus (MRSA) infections began to appear. By the 1990s, MRSA infections were common in hospitalized patients, particularly in intensive care units. Hospital-acquired MRSA isolates are often sensitive to only a few select antibiotics such as vancomycin, linezolid, and quinupristin/dalfopristin.5
In the late 1990s and early 2000s, MRSA began to appear in community-acquired infections in both adults and children. Most of these isolates have been implicated in skin and soft-tissue infections, but some have been responsible for invasive infection, bacteremia, and even death.6 Compared with hospital-acquired MRSA, these community isolates are more likely to be sensitive to commonly used antibiotics.
Always culture an infected wound
Knowledge of these sensitivity patterns is of great importance. Regrettably, as noted by Moran and associates, more than half of the patients (57%) were initially treated with antibiotics to which their infecting organism was resistant.
The clinical implications are clear:
- We must be aware that many community-acquired soft-tissue infections will be caused by drug-resistant staphylococci.
- Because antibiotic resistance is so prevalent, a culture of the infected wound should be obtained routinely so that antimicrobial therapy can be modified if the patient fails to respond to initial treatment.
- Antibiotic therapy alone is rarely sufficient for abscesses in the soft tissue and skin; adequate surgical drainage is essential.
- Fundamental infection-control measures, such as careful handwashing, adequate skin preparation prior to surgery, and local wound care, are of greater importance than ever.
Most cases of community-acquired MRSA have been isolated from skin and soft tissue; surgical drainage is necessary when infection advances to abscess in those sites.
In gravidas with group B strep, look for S. aureus
Chen KT, Huard RC, Della-Latta P, Saiman L. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet Gynecol. 2006;108:482–487.
To assess the prevalence of methicillin-sensitive and community-acquired methicillin-resistant S. aureus colonization in pregnant women, Chen and colleagues evaluated de-identified culture specimens that had originally been submitted to the microbiology laboratory for identification of group B streptococcal infection. As opposed to hospital-associated MRSA isolates, community-associated methicillin-resistant strains were defined as those possessing the type IV or V staphylococcal chromosomal cassette mec element and lacking a multi-drug-resistant phenotype.
Of the 2,963 culture specimens in the prospective surveillance study, 743 (25%) were positive for group B streptococci, and 507 (17%) were positive for S. aureus. Group B streptococcal colonization was significantly associated with S. aureus colonization; the prevalence odds ratio was 2.1. Fourteen of the 507 S. aureus isolates were methicillin-resistant (2.8%; 95% confidence interval [CI] 1.4–4.2%). Thirteen of the 14 strains (93%) were community-acquired.
S. aureus may cause sepsis, wound infection, bacteremia, and other ills
The unique feature of this study is the observation that vaginal colonization with group B streptococci was significantly associated with colonization with S. aureus—one of the possible causative pathogens in chorioamnionitis, endometritis, wound infection, bacteremia, puerperal mastitis, and toxic shock syndrome. The organism also may cause serious neonatal infection, particularly sepsis.
The prevalence of group B streptococcal colonization in this study (25.1%, 95% CI 23.5–26.7%) is comparable to data reported from several other investigators.7 Colonized women are at increased risk for chorioamnionitis and puerperal endometritis, and their infants are at increased risk of sepsis, pneumonia, and meningitis. Fortunately, intrapartum antibiotic prophylaxis significantly reduces the risk of both maternal and neonatal group B streptococcal infection.8
As I noted earlier in this update, the antimicrobial susceptibility of S. aureus has become increasingly limited, particularly in light of the recent increase in both hospital- and community-acquired methicillin-resistant strains. In this study by Chen and colleagues, 2.8% of S. aureus isolates were methicillin-resistant. Of these, all but one were community-acquired.
Clinical suggestions
These findings certainly do not indicate the need for routine cultures for S. aureus vaginal colonization in all pregnant women. Nor are cultures needed in women who test positive for group B streptococci at 35 to 37 weeks. However, clinicians should be alert for possible staphylococcal infections, such as wound abscess, furuncle, carbuncle, or mastitis, in these women. If such an infection appears, obtain a culture of the purulent collection. Pending the result, treat the patient empirically with a drug that is likely to be effective against community-acquired MRSA. One hundred percent of these strains are sensitive to rifampin and TMP-SMX, and 90% to 95% are sensitive to tetracycline.9
Univalent HPV vaccine is 100% effective against CIN grades 2, 3
Mao C, Koutsky LA, Ault KA, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia. Obstet Gynecol. 2006;107:18–27.
Mao and colleagues set out to assess the long-term protection of a univalent HPV vaccine against CIN grades 2, 3. Their prospective, randomized, double-blind, placebo-controlled trial involved 2,391 women, aged 16 to 23 years, who received either 40 μg of HPV-16 L1 virus-like particle vaccine or placebo intramuscularly at day 1, month 2, and month 6. Genital samples for HPV-16 DNA and cervical cytology specimens were collected at day 1, month 7, and then every 6 months for 48 months. A radioimmunoassay was used to assess antibody titers to HPV-16.
Of the 750 women who received placebo, 6 developed HPV-16–related CIN 2, and 6 developed CIN 3. Among the 755 vaccinated women, no cases of CIN occurred. Thus, the vaccine was 100% effective in this trial (95% CI 65–100%).
Among women who received placebo, 111 cases of persistent HPV-16 infection occurred, compared with 7 cases in vaccinated women (vaccine efficacy 94%; 95% CI 88–98%).
Following immunization, antibody to HPV-16 peaked at month 7, declined through month 18, and remained stable between months 30 and 48.
Any effective vaccine is important
Because 3,500 to 4,000 women still die from cervical cancer each year in the United States, and almost 274,000 die worldwide, the development of any HPV vaccine that provides lasting protection against CIN is important.
The vaccine evaluated by Mao and colleagues targeted a single strain of HPV, genotype 16. The recently approved quadrivalent vaccine, Gardasil, targets types 6, 11, 16, and 18. Of the more than 100 genotypes of HPV that have been discovered, approximately 30 are present in the mucosa of the genital tract, and 15 of these 30 are associated with cervical cancer. However, 2 HPV strains—types 16 and 18—are responsible for about two thirds of all cases of cervical cancer; 90% of genital warts cases result from infection with types 6 and 11.10
Emphasize to patients that preexisting cytologic abnormalities and genital warts don’t respond to vaccination against human papillomavirus.The Advisory Committee on Immunization Practices recommends that the quadrivalent vaccine be given to girls at age 11 or 12 years, prior to the onset of sexual activity, to be maximally effective against all 4 genotypes included in the vaccine.10
If a woman is infected with HPV prior to vaccination, she may develop abnormal cervical cytology related to the genotypes in the vaccine, as well as genotypes not included. Nevertheless, ACOG recommends that the vaccine be considered in all females ages 9 to 26.11 HPV genotyping is not recommended before giving the vaccine because any type of routine screening reduces the cost-effectiveness of the vaccination program.10
Fundamentals of vaccination
The quadrivalent vaccine must be administered intramuscularly (0.5 mL) in 3 doses on day 1 and at 2 and 6 months. The principal adverse effect is a local reaction such as pain, swelling, or pruritus at the injection site. Low-grade fever occurs in approximately 10% of patients.
Although the vaccine is classified by the FDA as pregnancy category B, the manufacturer recommends against its use during pregnancy. It may be administered to lactating women, however. The approximate cost of the 3-dose series, including administration fees, is $400 to $500.
It’s a vaccine, not a treatment
Patients need to understand that vaccination is not a treatment for preexisting cytologic abnormalities or genital warts. Nor can it be expected to be perfectly protective over a person’s lifetime against infection caused by genotypes 6, 11, 16, and 18. Women must continue to have regular cytologic screening. No reliable scientific data suggest that vaccination of young girls will increase sexual promiscuity in the adolescent population.10
The author reports no financial relationships relevant to this article.
Four studies caught my eye this past year. The first describes the use of systematic methodology to confirm the diagnosis of primary cytomegalovirus (CMV) infection in pregnancy and lower the rate of unnecessary pregnancy termination. Investigators were able to reclassify approximately 70% of women who had been diagnosed with CMV infection and reduce the number of pregnancy terminations by 73%.
Two other studies help define the emerging problem of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection, when to look for it, and how to treat it. In the first, researchers isolated S. aureus from the wounds of 320 patients with community-acquired infection and tested the samples for methicillin resistance, finding a prevalence of 59%. In the second study, investigators analyzed culture specimens from pregnant women for the presence of group B streptococci and S. aureus colonization. They found colonization with group B streptococci to be significantly associated with S. aureus colonization, with a prevalence odds ratio of 2.1.
The fourth study concerns the human papillomavirus (HPV) vaccine. Women given an HPV-16 L1 virus-like particle vaccine and followed for 4 years remained 100% free of cervical intraepithelial neoplasia (CIN) grades 2 and 3, unlike women who received placebo.
I believe these 4 studies represent the most significant developments of the past year in the field of infectious disease.
Don’t rush a diagnosis of CMV infection in pregnancy
Guerra B, Simonazzi G, Banfi A, et al. Impact of diagnostic and confirmatory tests and prenatal counseling on the rate of pregnancy termination among women with positive cytomegalovirus immunoglobulin M antibody titers. Am J Obstet Gynecol. 2007;196:221.e1–6.
CMV infection is a common and important perinatal pathogen. Each year in the United States, approximately 1% of gravidas acquire primary infection. Of these, about 40% transmit infection to the fetus. The rate of transmission is highest when maternal infection occurs in the third trimester, but the risk of serious fetal injury is greatest when maternal infection occurs in the first trimester. Ten percent to 20% of congenitally infected infants are acutely symptomatic at birth. Approximately 20% of these newborns die; most survivors have serious long-term complications. In contrast, CMV infection that recurs during pregnancy poses only minimal risk to the baby.1
Many women choose to have their pregnancy terminated when they learn they have a primary CMV infection.
Details of the study
This retrospective study was designed to determine whether a systematic diagnostic algorithm reduces the rate of unnecessary abortion in women who have apparent acute CMV infection during pregnancy. Guerra and colleagues evaluated 1,857 consecutive patients in practices in Italy who had a positive anti-CMV immunoglobulin M (IgM) antibody assay in the first or second trimester and were referred to a tertiary care facility for further diagnostic testing. Universal screening for CMV is now common among practitioners in Italy, and virtually all of these patients were completely asymptomatic.
At the tertiary facility, investigators tested again for CMV-specific IgM, as well as IgG, by enzyme immunoassay. They also tested for IgM by immunoblot and determined the avidity of anti-CMV IgG. Women who had IgG of low or moderate avidity with confirmed IgM, and those who clearly seroconverted to IgG were assumed to have a primary infection.
Women who were positive for IgM with high-avidity IgG were assumed to have nonprimary infection. Women who were seronegative for both antibodies were classified as uninfected. Those who were IgM-negative with high-avidity IgG were classified as previously infected. Women with an acute infection were then counseled by a specialist and offered amniocentesis and targeted ultrasonography.
Only 11.9% of women with primary infection chose abortion
Of the 1,857 women in this study, 445 were classified as having primary infection (group 1); 53 (11.9%) women elected to terminate their pregnancy. At autopsy, 38 of the 53 fetuses were found to be infected. In the other 15 cases, the pregnancy was terminated in the first trimester, and postmortem examination was not performed.
In the 1,205 women found to have nonprimary infection or previous infection (group 2), only 5 (0.4%) had the pregnancy terminated in the first trimester, and no postmortem examinations were performed. The difference in the observed rates of abortion between groups 1 and 2 was highly significant (P<.001).
Given their observations in group 1, the authors estimated that, on the basis of the initial screening tests at the referring institutions, approximately 196 (11.9%) of all patients in groups 1 and 2 would have elected abortion. By using confirmatory tests combined with counseling by a specialist, the authors were able to reduce the number of abortions from 196 to 53, a 73% decrease.
Always confirm an initial diagnosis
Given the ominous prognosis for congenital CMV infection and the major psychological implications and sobering finality of abortion, it is imperative that clinicians confirm the diagnosis of primary CMV infection. Because most cases of CMV infection in immunocompetent adults are asymptomatic, the diagnosis is typically confirmed by serology. Unfortunately, the serologic tests for CMV are not as straight-forward and reliable as tests for other viral infections such as rubella. Commercially available tests for anti-CMV IgM often have false-positive and false-negative results. In addition, IgM antibody may be detected as long as 9 months after a primary infection and may subsequently re-appear during reactivation of a latent infection or reinfection.2,3
Be selective, on the basis of risk factors and clinical manifestations, when screening pregnant women for cytomegalovirus infection.
Routine screening is not necessary
The authors’ findings vividly illustrate the potential errors that can occur when a large number of asymptomatic patients are routinely screened for CMV. Because of these pitfalls, I do not recommend routine screening. Rather, screening should be selective, directed at women who:
- have clinical manifestations of CMV infection
- are immunosuppressed
- have small children in daycare or work in daycare themselves or
- have documented exposure to someone with CMV infection.
If the initial immunoassay for CMV IgM is positive, a confirmatory immunoblot test for IgM should be performed, as well as avidity testing for IgG.
If primary infection is confirmed, the patient should undergo targeted ultrasonography and amniocentesis to assess for manifestations of congenital infection and to detect CMV in amniotic fluid by culture or polymerase chain reaction (PCR) testing. If the sonogram shows signs of fetal injury, or the PCR test is positive, the woman should be counseled about the options, which include experimental immunotherapy with hyperimmune anti-CMV globulin4 and pregnancy termination.
The study by Guerra and colleagues is a welcome addition to the obstetric literature. By using a systematic diagnostic algorithm that included an enzyme-linked immunosorbent assay and an immunoblot assay for IgM antibody and avidity testing for IgG antibody, the authors were able to reclassify approximately 70% of patients as either uninfected or previously infected. As a result, they reduced the number of pregnancy terminations by 73%, an objective end-point that clearly has great social, economic, and medical impact.
Most community S. aureus infections are methicillin-resistant
Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666–674.
Moran and colleagues reviewed the records of 422 adults with acute purulent and soft-tissue infections who were evaluated in 11 university-affiliated emergency departments in August 2004. Wounds were routinely cultured. When S. aureus was isolated, the organisms were tested for antimicrobial susceptibility to identify those that were methicillin-resistant. The PCR test was used to identify genes for staphylococcal enterotoxins A through E and H, toxic shock syndrome toxin, and Panton–Valentin leukocidin. The same methodology was used to identify the gene complex staphylococcal cassette chromosome mec (SCCmec). This complex contains the mecA gene that confers methicillin resistance.
Of the 422 patients, 320 (76%) had S. aureus isolated from their wound. The prevalence of methicillin resistance was 59%. Ninety-seven percent of MRSA isolates were pulsed-field type USA 300. SCCmec type IV and the Panton–Valentin leukocidin gene were detected in 98% of MRSA isolates. Other toxin genes were rare.
Only 2 drugs were 100% effective
Among MRSA isolates, 100% were susceptible to rifampin and trimethoprim-sulfamethoxazole (TMP-SMX), 95% were susceptible to clindamycin, and 92% were sensitive to tetracycline. Only 60% were sensitive to fluoroquinolones, and only 6% were sensitive to erythromycin. Only 43% of patients received initial empiric therapy with antibiotics to which their organisms were sensitive.
Reason to worry
S. aureus is an important pathogen in obstetric patients. It is the causative organism of toxic shock syndrome and the dominant pathogen in patients with puerperal mastitis, as well as one of the key causes of postoperative wound infection. When penicillin was developed in 1941, all strains of S. aureus were sensitive to the drug. Within a few short years, however, most hospital-acquired strains became resistant.
Methicillin was introduced in 1961 to treat these resistant staphylococcal species. Unfortunately, by the mid-1960s, methicillin-resistant S. aureus (MRSA) infections began to appear. By the 1990s, MRSA infections were common in hospitalized patients, particularly in intensive care units. Hospital-acquired MRSA isolates are often sensitive to only a few select antibiotics such as vancomycin, linezolid, and quinupristin/dalfopristin.5
In the late 1990s and early 2000s, MRSA began to appear in community-acquired infections in both adults and children. Most of these isolates have been implicated in skin and soft-tissue infections, but some have been responsible for invasive infection, bacteremia, and even death.6 Compared with hospital-acquired MRSA, these community isolates are more likely to be sensitive to commonly used antibiotics.
Always culture an infected wound
Knowledge of these sensitivity patterns is of great importance. Regrettably, as noted by Moran and associates, more than half of the patients (57%) were initially treated with antibiotics to which their infecting organism was resistant.
The clinical implications are clear:
- We must be aware that many community-acquired soft-tissue infections will be caused by drug-resistant staphylococci.
- Because antibiotic resistance is so prevalent, a culture of the infected wound should be obtained routinely so that antimicrobial therapy can be modified if the patient fails to respond to initial treatment.
- Antibiotic therapy alone is rarely sufficient for abscesses in the soft tissue and skin; adequate surgical drainage is essential.
- Fundamental infection-control measures, such as careful handwashing, adequate skin preparation prior to surgery, and local wound care, are of greater importance than ever.
Most cases of community-acquired MRSA have been isolated from skin and soft tissue; surgical drainage is necessary when infection advances to abscess in those sites.
In gravidas with group B strep, look for S. aureus
Chen KT, Huard RC, Della-Latta P, Saiman L. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet Gynecol. 2006;108:482–487.
To assess the prevalence of methicillin-sensitive and community-acquired methicillin-resistant S. aureus colonization in pregnant women, Chen and colleagues evaluated de-identified culture specimens that had originally been submitted to the microbiology laboratory for identification of group B streptococcal infection. As opposed to hospital-associated MRSA isolates, community-associated methicillin-resistant strains were defined as those possessing the type IV or V staphylococcal chromosomal cassette mec element and lacking a multi-drug-resistant phenotype.
Of the 2,963 culture specimens in the prospective surveillance study, 743 (25%) were positive for group B streptococci, and 507 (17%) were positive for S. aureus. Group B streptococcal colonization was significantly associated with S. aureus colonization; the prevalence odds ratio was 2.1. Fourteen of the 507 S. aureus isolates were methicillin-resistant (2.8%; 95% confidence interval [CI] 1.4–4.2%). Thirteen of the 14 strains (93%) were community-acquired.
S. aureus may cause sepsis, wound infection, bacteremia, and other ills
The unique feature of this study is the observation that vaginal colonization with group B streptococci was significantly associated with colonization with S. aureus—one of the possible causative pathogens in chorioamnionitis, endometritis, wound infection, bacteremia, puerperal mastitis, and toxic shock syndrome. The organism also may cause serious neonatal infection, particularly sepsis.
The prevalence of group B streptococcal colonization in this study (25.1%, 95% CI 23.5–26.7%) is comparable to data reported from several other investigators.7 Colonized women are at increased risk for chorioamnionitis and puerperal endometritis, and their infants are at increased risk of sepsis, pneumonia, and meningitis. Fortunately, intrapartum antibiotic prophylaxis significantly reduces the risk of both maternal and neonatal group B streptococcal infection.8
As I noted earlier in this update, the antimicrobial susceptibility of S. aureus has become increasingly limited, particularly in light of the recent increase in both hospital- and community-acquired methicillin-resistant strains. In this study by Chen and colleagues, 2.8% of S. aureus isolates were methicillin-resistant. Of these, all but one were community-acquired.
Clinical suggestions
These findings certainly do not indicate the need for routine cultures for S. aureus vaginal colonization in all pregnant women. Nor are cultures needed in women who test positive for group B streptococci at 35 to 37 weeks. However, clinicians should be alert for possible staphylococcal infections, such as wound abscess, furuncle, carbuncle, or mastitis, in these women. If such an infection appears, obtain a culture of the purulent collection. Pending the result, treat the patient empirically with a drug that is likely to be effective against community-acquired MRSA. One hundred percent of these strains are sensitive to rifampin and TMP-SMX, and 90% to 95% are sensitive to tetracycline.9
Univalent HPV vaccine is 100% effective against CIN grades 2, 3
Mao C, Koutsky LA, Ault KA, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia. Obstet Gynecol. 2006;107:18–27.
Mao and colleagues set out to assess the long-term protection of a univalent HPV vaccine against CIN grades 2, 3. Their prospective, randomized, double-blind, placebo-controlled trial involved 2,391 women, aged 16 to 23 years, who received either 40 μg of HPV-16 L1 virus-like particle vaccine or placebo intramuscularly at day 1, month 2, and month 6. Genital samples for HPV-16 DNA and cervical cytology specimens were collected at day 1, month 7, and then every 6 months for 48 months. A radioimmunoassay was used to assess antibody titers to HPV-16.
Of the 750 women who received placebo, 6 developed HPV-16–related CIN 2, and 6 developed CIN 3. Among the 755 vaccinated women, no cases of CIN occurred. Thus, the vaccine was 100% effective in this trial (95% CI 65–100%).
Among women who received placebo, 111 cases of persistent HPV-16 infection occurred, compared with 7 cases in vaccinated women (vaccine efficacy 94%; 95% CI 88–98%).
Following immunization, antibody to HPV-16 peaked at month 7, declined through month 18, and remained stable between months 30 and 48.
Any effective vaccine is important
Because 3,500 to 4,000 women still die from cervical cancer each year in the United States, and almost 274,000 die worldwide, the development of any HPV vaccine that provides lasting protection against CIN is important.
The vaccine evaluated by Mao and colleagues targeted a single strain of HPV, genotype 16. The recently approved quadrivalent vaccine, Gardasil, targets types 6, 11, 16, and 18. Of the more than 100 genotypes of HPV that have been discovered, approximately 30 are present in the mucosa of the genital tract, and 15 of these 30 are associated with cervical cancer. However, 2 HPV strains—types 16 and 18—are responsible for about two thirds of all cases of cervical cancer; 90% of genital warts cases result from infection with types 6 and 11.10
Emphasize to patients that preexisting cytologic abnormalities and genital warts don’t respond to vaccination against human papillomavirus.The Advisory Committee on Immunization Practices recommends that the quadrivalent vaccine be given to girls at age 11 or 12 years, prior to the onset of sexual activity, to be maximally effective against all 4 genotypes included in the vaccine.10
If a woman is infected with HPV prior to vaccination, she may develop abnormal cervical cytology related to the genotypes in the vaccine, as well as genotypes not included. Nevertheless, ACOG recommends that the vaccine be considered in all females ages 9 to 26.11 HPV genotyping is not recommended before giving the vaccine because any type of routine screening reduces the cost-effectiveness of the vaccination program.10
Fundamentals of vaccination
The quadrivalent vaccine must be administered intramuscularly (0.5 mL) in 3 doses on day 1 and at 2 and 6 months. The principal adverse effect is a local reaction such as pain, swelling, or pruritus at the injection site. Low-grade fever occurs in approximately 10% of patients.
Although the vaccine is classified by the FDA as pregnancy category B, the manufacturer recommends against its use during pregnancy. It may be administered to lactating women, however. The approximate cost of the 3-dose series, including administration fees, is $400 to $500.
It’s a vaccine, not a treatment
Patients need to understand that vaccination is not a treatment for preexisting cytologic abnormalities or genital warts. Nor can it be expected to be perfectly protective over a person’s lifetime against infection caused by genotypes 6, 11, 16, and 18. Women must continue to have regular cytologic screening. No reliable scientific data suggest that vaccination of young girls will increase sexual promiscuity in the adolescent population.10
The author reports no financial relationships relevant to this article.
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Munro SC, Hall B, Whybin LR, et al. Diagnosis of and screening for cytomegalovirus infection in pregnant women. J Clin Microbiol. 2005;431:4713-4718.
3. Lazzarotto T, Gabrielli L, Lanari M, et al. Congenital cytomegalovirus infection: recent advances in the diagnosis of maternal infection. Hum Immunol. 2004;65:410-415.
4. Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
5. Gibbs RS. Emerging infections in obstetric and gynecologic practice. Obstet Gynecol. 2006;108:480-481.
6. Laible VR, Sheffield JS, Roberts S, McIntire DD, Trevino S, Wendel GD. Clinical presentation of community-acquired methicillin-resistant Staphylococcus aureus in pregnancy. Obstet Gynecol. 2005;106:461-465.
7. Edwards RK, Clark P, Duff P. Intrapartum antibiotic prophylaxis 2: positive predictive value of antenatal group B streptococcal cultures and antibiotic susceptibility of clinical isolates. Obstet Gynecol. 2002;100:590-594.
8. Locksmith GJ, Clark P, Duff P. Maternal and neonatal infection rates with three different protocols for prevention of group B streptococcal disease. Am J Obstet Gynecol. 1999;180:416-422.
9. Moran GJ, Krisnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666-674.
10. Monk BJ, Wiley DJ. Will human papillomavirus prophylactic vaccination change sexual practices of adolescent and young adult women in America? Obstet Gynecol. 2006;108:420-424.
11. Human papillomavirus vaccination. ACOG Committee Opinion #344. Washington, DC: American College of Obstetricians and Gynecologists; September 2006.
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Munro SC, Hall B, Whybin LR, et al. Diagnosis of and screening for cytomegalovirus infection in pregnant women. J Clin Microbiol. 2005;431:4713-4718.
3. Lazzarotto T, Gabrielli L, Lanari M, et al. Congenital cytomegalovirus infection: recent advances in the diagnosis of maternal infection. Hum Immunol. 2004;65:410-415.
4. Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350-1362.
5. Gibbs RS. Emerging infections in obstetric and gynecologic practice. Obstet Gynecol. 2006;108:480-481.
6. Laible VR, Sheffield JS, Roberts S, McIntire DD, Trevino S, Wendel GD. Clinical presentation of community-acquired methicillin-resistant Staphylococcus aureus in pregnancy. Obstet Gynecol. 2005;106:461-465.
7. Edwards RK, Clark P, Duff P. Intrapartum antibiotic prophylaxis 2: positive predictive value of antenatal group B streptococcal cultures and antibiotic susceptibility of clinical isolates. Obstet Gynecol. 2002;100:590-594.
8. Locksmith GJ, Clark P, Duff P. Maternal and neonatal infection rates with three different protocols for prevention of group B streptococcal disease. Am J Obstet Gynecol. 1999;180:416-422.
9. Moran GJ, Krisnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666-674.
10. Monk BJ, Wiley DJ. Will human papillomavirus prophylactic vaccination change sexual practices of adolescent and young adult women in America? Obstet Gynecol. 2006;108:420-424.
11. Human papillomavirus vaccination. ACOG Committee Opinion #344. Washington, DC: American College of Obstetricians and Gynecologists; September 2006.
INFECTIOUS DISEASES
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
INFECTIOUS DISEASE
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
Q Can screening for vaginitis reduce preterm birth?
<huc>A</huc> Perhaps. Women treated for subclinical infection had significantly fewer preterm births than controls, Kiss et al found. However, I am not yet ready to embrace routine screening of all gravidas for asymptomatic candidiasis, trichomoniasis, and bacterial vaginosis (BV), though I strongly recommend treating symptomatic infections.
Expert Commentary
Before you embrace the screening program recommended by Kiss et al, be aware that their observations are inconsistent with other published reports and with our understanding of the pathophysiology of preterm delivery related to genital tract infection.
In this prospective, randomized trial, more than 4,000 asymptomatic gravidas were screened for vaginal candidiasis, trichomoniasis, and BV. When infection was detected, the intervention group was treated and the control group was not. The frequency of preterm birth was 3.0% in the intervention group (P=.0001) and 5.3% in the control group. The intervention group also had significantly fewer infants weighing less than 2,500 g.
How the findings contradict other data
I question these findings due to the following:
- To my knowledge, the study is unique in suggesting an association between vaginal candidiasis and preterm delivery.
- In a large multicenter US study,1 treating gravidas with asymptomatic trichomoniasis did not prevent preterm delivery. In fact, treated women had a higher frequency of preterm delivery (19.0% versus 10.7%, P=.004).
- In another large multicenter US study,2 treating asymptomatic BV did not reduce the frequency of preterm delivery or other adverse outcomes.
The regimens Kiss et al used for trichomoniasis and BV are not standard in the United States. They administered topical metronidazole to treat trichomoniasis and topical clindamycin for BV. The current recommendation for treating trichomoniasis in pregnancy is a single 2-g oral dose of metronidazole.3 For BV, recommended treatment is oral metronidazole, 250 mg three times daily for 7 days.3
Systemic regimens are based on the hypothesis that organisms ascend from the lower genital tract through the endocervical canal and colonize the membranes, causing inflammation and activating the prostaglandin cascade. Presumably, topical vaginal therapy will not eradicate organisms colonizing the upper genital tract.
These results may not be widely applicable, since the women treated by Kiss et al were extremely low-risk. Ninety-eight percent of the women were white, and the total prevalence of the 3 vaginal infections was only 20%. In many US sectors, the prevalence of BV alone exceeds 30%. Unfortunately, based on results of the studies cited above, I do not believe US obstetricians should anticipate the favorable results noted by Kiss et al.
1. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487M-493.
2. Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vagnonsis. N Engl J Med. 2000;342:534-540.
3. Sexually transmitted diseases treatment guidelines— 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51:1-78.
<huc>A</huc> Perhaps. Women treated for subclinical infection had significantly fewer preterm births than controls, Kiss et al found. However, I am not yet ready to embrace routine screening of all gravidas for asymptomatic candidiasis, trichomoniasis, and bacterial vaginosis (BV), though I strongly recommend treating symptomatic infections.
Expert Commentary
Before you embrace the screening program recommended by Kiss et al, be aware that their observations are inconsistent with other published reports and with our understanding of the pathophysiology of preterm delivery related to genital tract infection.
In this prospective, randomized trial, more than 4,000 asymptomatic gravidas were screened for vaginal candidiasis, trichomoniasis, and BV. When infection was detected, the intervention group was treated and the control group was not. The frequency of preterm birth was 3.0% in the intervention group (P=.0001) and 5.3% in the control group. The intervention group also had significantly fewer infants weighing less than 2,500 g.
How the findings contradict other data
I question these findings due to the following:
- To my knowledge, the study is unique in suggesting an association between vaginal candidiasis and preterm delivery.
- In a large multicenter US study,1 treating gravidas with asymptomatic trichomoniasis did not prevent preterm delivery. In fact, treated women had a higher frequency of preterm delivery (19.0% versus 10.7%, P=.004).
- In another large multicenter US study,2 treating asymptomatic BV did not reduce the frequency of preterm delivery or other adverse outcomes.
The regimens Kiss et al used for trichomoniasis and BV are not standard in the United States. They administered topical metronidazole to treat trichomoniasis and topical clindamycin for BV. The current recommendation for treating trichomoniasis in pregnancy is a single 2-g oral dose of metronidazole.3 For BV, recommended treatment is oral metronidazole, 250 mg three times daily for 7 days.3
Systemic regimens are based on the hypothesis that organisms ascend from the lower genital tract through the endocervical canal and colonize the membranes, causing inflammation and activating the prostaglandin cascade. Presumably, topical vaginal therapy will not eradicate organisms colonizing the upper genital tract.
These results may not be widely applicable, since the women treated by Kiss et al were extremely low-risk. Ninety-eight percent of the women were white, and the total prevalence of the 3 vaginal infections was only 20%. In many US sectors, the prevalence of BV alone exceeds 30%. Unfortunately, based on results of the studies cited above, I do not believe US obstetricians should anticipate the favorable results noted by Kiss et al.
<huc>A</huc> Perhaps. Women treated for subclinical infection had significantly fewer preterm births than controls, Kiss et al found. However, I am not yet ready to embrace routine screening of all gravidas for asymptomatic candidiasis, trichomoniasis, and bacterial vaginosis (BV), though I strongly recommend treating symptomatic infections.
Expert Commentary
Before you embrace the screening program recommended by Kiss et al, be aware that their observations are inconsistent with other published reports and with our understanding of the pathophysiology of preterm delivery related to genital tract infection.
In this prospective, randomized trial, more than 4,000 asymptomatic gravidas were screened for vaginal candidiasis, trichomoniasis, and BV. When infection was detected, the intervention group was treated and the control group was not. The frequency of preterm birth was 3.0% in the intervention group (P=.0001) and 5.3% in the control group. The intervention group also had significantly fewer infants weighing less than 2,500 g.
How the findings contradict other data
I question these findings due to the following:
- To my knowledge, the study is unique in suggesting an association between vaginal candidiasis and preterm delivery.
- In a large multicenter US study,1 treating gravidas with asymptomatic trichomoniasis did not prevent preterm delivery. In fact, treated women had a higher frequency of preterm delivery (19.0% versus 10.7%, P=.004).
- In another large multicenter US study,2 treating asymptomatic BV did not reduce the frequency of preterm delivery or other adverse outcomes.
The regimens Kiss et al used for trichomoniasis and BV are not standard in the United States. They administered topical metronidazole to treat trichomoniasis and topical clindamycin for BV. The current recommendation for treating trichomoniasis in pregnancy is a single 2-g oral dose of metronidazole.3 For BV, recommended treatment is oral metronidazole, 250 mg three times daily for 7 days.3
Systemic regimens are based on the hypothesis that organisms ascend from the lower genital tract through the endocervical canal and colonize the membranes, causing inflammation and activating the prostaglandin cascade. Presumably, topical vaginal therapy will not eradicate organisms colonizing the upper genital tract.
These results may not be widely applicable, since the women treated by Kiss et al were extremely low-risk. Ninety-eight percent of the women were white, and the total prevalence of the 3 vaginal infections was only 20%. In many US sectors, the prevalence of BV alone exceeds 30%. Unfortunately, based on results of the studies cited above, I do not believe US obstetricians should anticipate the favorable results noted by Kiss et al.
1. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487M-493.
2. Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vagnonsis. N Engl J Med. 2000;342:534-540.
3. Sexually transmitted diseases treatment guidelines— 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51:1-78.
1. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487M-493.
2. Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vagnonsis. N Engl J Med. 2000;342:534-540.
3. Sexually transmitted diseases treatment guidelines— 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51:1-78.
Evaluation and management of preterm premature rupture of membranes
Management of preterm premature rupture of membranes (PPROM) is the most controversial of all obstetric problems. This article describes an algorithmic approach (FIGURE) to evaluation and treatment.
PPROM refers to rupture of membranes before onset of contractions at a gestational age less than 37 weeks. Approximately 30% to 40% of preterm deliveries are associated with PPROM.1 In turn, preterm delivery is responsible for approximately 75% of all neonatal deaths, excluding infants with anomalies incompatible with life.2
PPROM is multifactorial and complex
PPROM may occur in patients with an incompetent cervix, which can result from previous genital tract surgery or laceration. PPROM occurs with increased frequency in women who smoke or who have multiple gestation, polyhydramnios, or antepartum hemorrhage. Some women with PPROM also appear to have inherent deficiencies in collagen synthesis, which may predispose to weakening of the membranes.1
Infection link confirmed. Of greatest interest in recent years has been the confirmation that PPROM is associated with lower and upper genital tract infection; there are 3 major lines of supporting evidence:
- Many of the bacteria that inhabit the lower genital tract can produce phospholipase A, an enzyme that can trigger the arachidonic acid cascade that leads to the synthesis of prostaglandins. These same bacteria also are able to produce a variety of proteolytic enzymes that can degrade the collagen matrix of the chorioamniotic membranes.
- Compared to women with uncomplicated gestation, those with PPROM are more likely to have lower genital tract infections (such as group B streptococcal colonization or bacterial vaginosis).
- Compared to women with preterm labor and intact membranes, women with PPROM are more likely to have clinical and subclinical chorioamnionitis and inflammatory cytokines in the amniotic fluid.2
The following conclusions are based on good and consistent evidence (level A recommendations) on management of patients with PPROM.
- As a rule, at a gestational age of less than 32 weeks, the greatest threat to the fetus is preterm delivery.
- If the gestational age is 32 weeks or more and fetal lung maturity is confirmed, the risks of expectant management usually exceed the risks of delivery.
- Outpatient management is appropriate only in a highly select group of women.
- In properly selected patients, the benefits of a single course of corticosteroids outweigh the risks.
- Tocolytics are effective in delaying delivery for 48 hours—a critical interval for the administration of corticosteroids.
- Prophylactic antibiotics prolong the latent period and reduce maternal and neonatal infection. These benefits clearly outweigh any risks such as allergic drug reaction or development of resistant organisms.
Direct observation is the best diagnostic test
Patients with PPROM usually note a sudden “gush” of fluid from the vagina. They also may experience a “constant leakage” of fluid or a sensation of “wetness” in the vagina or on the perineum.
The single best test to confirm the diagnosis is direct observation of amniotic fluid in the vaginal vault. Demonstration of severe oligo-hydramnios by ultrasound in a patient with a suggestive history also is helpful.
Although widely used, both the fern test and nitrazine test have pitfalls. The former may be falsely positive in the presence of highly estrogenized cervical mucus or extraneous saline on the glass side (e.g., from a fingerprint). The nitrazine test may be falsely positive in the presence of blood or seminal fluid.
Neonatal and maternal factors guide the management plan
The most important of several factors that must be considered in developing a management plan for PPROM are gestational age and availability of neonatal intensive care. For most patients at less than 36 weeks’ gestation, the prudent course at a hospital with only a level 1 nursery is transfer to a tertiary care facility. If a level 2 nursery is available, the clinician may have sufficient support from neonatology staff to manage patients at 34 weeks’ gestation.
Other important considerations include:
- the presence or absence of labor
- the presence of overt or subclinical infection,
- the stability of the fetal presentation and heart-rate tracing,
- the degree of fetal lung maturation, and
- the degree of cervical effacement and dilation.
- Expectant management. The principal hazards are the risks of ascending infection, umbilical cord prolapse, umbilical cord compression due to oligohydramnios, and abruptio placentae.
- Immediate delivery. The major risks are the well-recognized complications of prema-turity, including respiratory distress syndrome (RDS), intraventricular hemorrhage (IVH), sepsis, necrotizing enterocolitis (NEC), thermal instability, metabolic derangements, apnea and bradycardia, patent ductus arteriosus, and poor feeding. Of these, the 4 most likely to result in neonatal death are RDS, IVH, sepsis, and NEC, all of which are significantly more likely at gestational ages below 32 weeks than at 32 weeks or more.
Algorithmic management approach Assess stability of fetal presentation.
After confirming the diagnosis of PPROM, the clinician should assess gestational age on the basis of history, physical examination, and ultrasound. The fetal presentation and estimated fetal weight should be determined, and the fetal heart rate should be monitored for evidence of recurrent variable decelerations. The mother should be evaluated for chorioamnionitis, primarily by assessment of temperature and maternal and fetal heart rate.
If the fetal presentation is unstable, thus predisposing to umbilical cord prolapse, or if the fetal heart rate tracing is worrisome, the patient should be delivered. If the gravida initially is admitted to a facility with only a level 1 nursery and maternal transfer is impractical, neonatal transfer should take place immediately after the birth.
Assess fetal lung maturity. At a gestational age of less than 32 weeks, lung maturity is very unlikely, and testing is not cost-effective. However, at 32 to 34 weeks, testing should be performed routinely. Amniotic fluid may be obtained by transabdominal amniocentesis or by aspiration of fluid pooled in the vaginal vault. Edwards et al3 recently confirmed the reliability of this sampling method. Lung maturity may be assessed by means of the lecithin:sphingomyelin ratio, lamellar body count, or fetal lung maturity test.
If the fetal presentation is unstable or the fetal heart rate tracing is worrisome, the patient should be delivered.
The decision to deliver. If the gestational age is 32 weeks or more, fetal lung maturity is confirmed, and a neonatal intensive care unit is available, both mother and baby usally will fare better if delivered.
Patients should be treated intrapartum with antibiotics to prevent perinatal transmission of group B streptocol infection. Appropriate regimens include penicillin, then 2.5 million units IV every 4 hours; or ampicillin, 2 g IV initially, then I g every 4 hours.
A recent study confirmed the value of this treatment plan.4 In it, 164 patients at 32 to weeks’ gestation with confirmed fetal lung maturity were randomly assigned to delivery or expectant management. The mean gestational ages in the two groups were similar: 34.1 weeks in the former and 34.3 weeks in the latter group. The expectant management group had a longer duration of hospitalization for the mother and baby, and an increased rate of maternal infection and fetal heart rate abnormalities. In addition, the infants in this group received more frequent, prolonged antibiotic therapy.
Expectant management is appropriate for some patients. If gestational age is less than 32 weeks and the mother and fetus are stable, expectant management is appropriate.
If the patient is at 32 to 34 weeks’ gestation and amniotic fluid cannot be obtained, she should be managed expectantly until 34 weeks. At 34 weeks, she should be delivered.
A recent study by Naef et al5 confirmed the value of delivery at 34 weeks or more. In this investigation, 120 patients at 34 to 36 6/7 weeks’ gestation were randomly assigned to oxytocin induction (n = 57) or expectant management (n = 63). Fetal lung maturity studies were not done. In the expectant management group, chorioamnionitis occurred more often (16% versus 2%, P = .007), maternal hospitalization was prolonged (5.2±6.8 days versus 2.6±1.6 days, P = .006), and there was a trend toward an increased rate of neonatal infection.
- Corticosterioids. A single course of corticosteroids should be administered to reduce the risk of neonatal RDS, IVH, and NEC.2 Dosage regimens include 2 intramuscular (IM) doses of betamethasone, 12 mg, at 24-hour intervals, or 4 IM doses of dexamethasone, 6 mg, at 12-hour intervals. Tocolytics should be administered to delay delivery for 48 hours, thus permitting administration of corticosteroids.3 Prolonged administration of tocolytics is not justified.
- Testing for infection. The patient should be tested for gonorrhea, chlamydia, bacterial vaginosis, and group B streptococcal colonization. If the test for bacterial vaginosis is positive, the patient should be treated with metronidazole, 250 mg orally, 3 times daily, for 7 days. If gonorrhea is present, she should receive either cefixime, 400 mg orally in a single dose, or ceftriaxone, 125 mg IM in a single dose.6
- Prophylactic antibiotics. Even in the absence of obvious lower genital tract infection, patients with PPROM benefit from antibiotic prophylaxis. Many studies investigating the role of prophylactic antibiotics in women with PPROM have been published.7
The largest and most strictly conducted trial was reported by Mercer et al8 on behalf of the Maternal-Fetal Medicine Units Network. Participants—all women with PPROM between 24 and 32 weeks gestation—were randomly assigned to treatment with placebo or IV ampicillin plus erythromycin for 48 hours, followed by oral amoxicillin plus erythromycin for an additional 5 days. The main outcome measure was composite morbidity—at least 1 of the following complications: fetal or infant death, RDS, IVH, NEC, or sepsis within 72 hours of birth. (Researchers also looked at these morbidities individually.) Antibiotic prophylaxis significantly reduced the risk of composite morbidity (44.1% versus 52.9%, P = .04), RDS (40.5% versus 48.7%, P = .04), and NEC (2.3% versus 5.8%, P = .03). Among women who tested negative for group B streptococci, prophylactic antibiotics also significantly prolonged the latent period between PPROM and onset of labor (P <.001>
- Monitoring. Patients selected for expectant management should be observed for evidence of maternal infection. Although a variety of laboratory tests have been proposed for the early diagnosis of infection (white blood cell count, C-reactive protein, nonstress test, biophysical profile, amniotic fluid glucose, or Gram stain), probably the most cost-effective method is monitoring maternal temperature and heart rate and fetal heart rate.
- Outpatient versus inpatient. With rare exceptions, expectant management should take place in the hospital. Carlan et al9 reported a randomized trial of outpatient management of PPROM, in which patients were included if they were judged to be compliant and met all of the following criteria: no evidence of cervical or intra-amniotic infection, minimal cervical dilation, stable fetal presentation, no sign of labor, reassuring heart-rate tracing, and easy access to the hospital. Patients initially were observed for 72 hours in the hospital.
Dr. Duff reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Duff P. Management of premature rupture of membranes in term patients. In: Sciarra JJ, ed. Gynecology and Obstetrics. Chicago, Ill: JB Lippincott; 1997.
2. Mercer B. ACOG Practice Bulletin #1: premature rupture of membranes. Washington, DC: ACOG; June 1998.
3. Edwards RK, Duff P, Ross KC. Amniotic fluid indices of fetal lung maturity with preterm premature rupture of membranes. Obstet Gynecol. 2000;96:102-105.
4. Mercer BM, Crocker LG, Boe NM, Sibai BM. Induction versus expectant management in premature rupture of the membranes with mature amniotic fluid at 32–36 weeks: a randomized trial. Am J Obstet Gynecol. 1993;169:775-782.
5. Naef RW, Albert JR, Ross EL, et al. Premature rupture of membranes at 34 to 37 weeks’ gestation: aggressive versus conservative management. Am J Obstet Gynecol. 1998;178:126-130.
6. Duff P. Maternal and perinatal infection. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics. Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2001.
7. Duff P. Antibiotic treatment in patients with preterm premature rupture of membranes. OBG Management. 2001;13:54-66.
8. Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. JAMA. 1997;278:989-995.
9. Carlan SJ, O’Brien WF, Parsons MT, Lense JJ. Preterm premature rupture of membranes: a randomized study of home versus hospital management. Obstet Gynecol. 1993;81:61-64.
Management of preterm premature rupture of membranes (PPROM) is the most controversial of all obstetric problems. This article describes an algorithmic approach (FIGURE) to evaluation and treatment.
PPROM refers to rupture of membranes before onset of contractions at a gestational age less than 37 weeks. Approximately 30% to 40% of preterm deliveries are associated with PPROM.1 In turn, preterm delivery is responsible for approximately 75% of all neonatal deaths, excluding infants with anomalies incompatible with life.2
PPROM is multifactorial and complex
PPROM may occur in patients with an incompetent cervix, which can result from previous genital tract surgery or laceration. PPROM occurs with increased frequency in women who smoke or who have multiple gestation, polyhydramnios, or antepartum hemorrhage. Some women with PPROM also appear to have inherent deficiencies in collagen synthesis, which may predispose to weakening of the membranes.1
Infection link confirmed. Of greatest interest in recent years has been the confirmation that PPROM is associated with lower and upper genital tract infection; there are 3 major lines of supporting evidence:
- Many of the bacteria that inhabit the lower genital tract can produce phospholipase A, an enzyme that can trigger the arachidonic acid cascade that leads to the synthesis of prostaglandins. These same bacteria also are able to produce a variety of proteolytic enzymes that can degrade the collagen matrix of the chorioamniotic membranes.
- Compared to women with uncomplicated gestation, those with PPROM are more likely to have lower genital tract infections (such as group B streptococcal colonization or bacterial vaginosis).
- Compared to women with preterm labor and intact membranes, women with PPROM are more likely to have clinical and subclinical chorioamnionitis and inflammatory cytokines in the amniotic fluid.2
The following conclusions are based on good and consistent evidence (level A recommendations) on management of patients with PPROM.
- As a rule, at a gestational age of less than 32 weeks, the greatest threat to the fetus is preterm delivery.
- If the gestational age is 32 weeks or more and fetal lung maturity is confirmed, the risks of expectant management usually exceed the risks of delivery.
- Outpatient management is appropriate only in a highly select group of women.
- In properly selected patients, the benefits of a single course of corticosteroids outweigh the risks.
- Tocolytics are effective in delaying delivery for 48 hours—a critical interval for the administration of corticosteroids.
- Prophylactic antibiotics prolong the latent period and reduce maternal and neonatal infection. These benefits clearly outweigh any risks such as allergic drug reaction or development of resistant organisms.
Direct observation is the best diagnostic test
Patients with PPROM usually note a sudden “gush” of fluid from the vagina. They also may experience a “constant leakage” of fluid or a sensation of “wetness” in the vagina or on the perineum.
The single best test to confirm the diagnosis is direct observation of amniotic fluid in the vaginal vault. Demonstration of severe oligo-hydramnios by ultrasound in a patient with a suggestive history also is helpful.
Although widely used, both the fern test and nitrazine test have pitfalls. The former may be falsely positive in the presence of highly estrogenized cervical mucus or extraneous saline on the glass side (e.g., from a fingerprint). The nitrazine test may be falsely positive in the presence of blood or seminal fluid.
Neonatal and maternal factors guide the management plan
The most important of several factors that must be considered in developing a management plan for PPROM are gestational age and availability of neonatal intensive care. For most patients at less than 36 weeks’ gestation, the prudent course at a hospital with only a level 1 nursery is transfer to a tertiary care facility. If a level 2 nursery is available, the clinician may have sufficient support from neonatology staff to manage patients at 34 weeks’ gestation.
Other important considerations include:
- the presence or absence of labor
- the presence of overt or subclinical infection,
- the stability of the fetal presentation and heart-rate tracing,
- the degree of fetal lung maturation, and
- the degree of cervical effacement and dilation.
- Expectant management. The principal hazards are the risks of ascending infection, umbilical cord prolapse, umbilical cord compression due to oligohydramnios, and abruptio placentae.
- Immediate delivery. The major risks are the well-recognized complications of prema-turity, including respiratory distress syndrome (RDS), intraventricular hemorrhage (IVH), sepsis, necrotizing enterocolitis (NEC), thermal instability, metabolic derangements, apnea and bradycardia, patent ductus arteriosus, and poor feeding. Of these, the 4 most likely to result in neonatal death are RDS, IVH, sepsis, and NEC, all of which are significantly more likely at gestational ages below 32 weeks than at 32 weeks or more.
Algorithmic management approach Assess stability of fetal presentation.
After confirming the diagnosis of PPROM, the clinician should assess gestational age on the basis of history, physical examination, and ultrasound. The fetal presentation and estimated fetal weight should be determined, and the fetal heart rate should be monitored for evidence of recurrent variable decelerations. The mother should be evaluated for chorioamnionitis, primarily by assessment of temperature and maternal and fetal heart rate.
If the fetal presentation is unstable, thus predisposing to umbilical cord prolapse, or if the fetal heart rate tracing is worrisome, the patient should be delivered. If the gravida initially is admitted to a facility with only a level 1 nursery and maternal transfer is impractical, neonatal transfer should take place immediately after the birth.
Assess fetal lung maturity. At a gestational age of less than 32 weeks, lung maturity is very unlikely, and testing is not cost-effective. However, at 32 to 34 weeks, testing should be performed routinely. Amniotic fluid may be obtained by transabdominal amniocentesis or by aspiration of fluid pooled in the vaginal vault. Edwards et al3 recently confirmed the reliability of this sampling method. Lung maturity may be assessed by means of the lecithin:sphingomyelin ratio, lamellar body count, or fetal lung maturity test.
If the fetal presentation is unstable or the fetal heart rate tracing is worrisome, the patient should be delivered.
The decision to deliver. If the gestational age is 32 weeks or more, fetal lung maturity is confirmed, and a neonatal intensive care unit is available, both mother and baby usally will fare better if delivered.
Patients should be treated intrapartum with antibiotics to prevent perinatal transmission of group B streptocol infection. Appropriate regimens include penicillin, then 2.5 million units IV every 4 hours; or ampicillin, 2 g IV initially, then I g every 4 hours.
A recent study confirmed the value of this treatment plan.4 In it, 164 patients at 32 to weeks’ gestation with confirmed fetal lung maturity were randomly assigned to delivery or expectant management. The mean gestational ages in the two groups were similar: 34.1 weeks in the former and 34.3 weeks in the latter group. The expectant management group had a longer duration of hospitalization for the mother and baby, and an increased rate of maternal infection and fetal heart rate abnormalities. In addition, the infants in this group received more frequent, prolonged antibiotic therapy.
Expectant management is appropriate for some patients. If gestational age is less than 32 weeks and the mother and fetus are stable, expectant management is appropriate.
If the patient is at 32 to 34 weeks’ gestation and amniotic fluid cannot be obtained, she should be managed expectantly until 34 weeks. At 34 weeks, she should be delivered.
A recent study by Naef et al5 confirmed the value of delivery at 34 weeks or more. In this investigation, 120 patients at 34 to 36 6/7 weeks’ gestation were randomly assigned to oxytocin induction (n = 57) or expectant management (n = 63). Fetal lung maturity studies were not done. In the expectant management group, chorioamnionitis occurred more often (16% versus 2%, P = .007), maternal hospitalization was prolonged (5.2±6.8 days versus 2.6±1.6 days, P = .006), and there was a trend toward an increased rate of neonatal infection.
- Corticosterioids. A single course of corticosteroids should be administered to reduce the risk of neonatal RDS, IVH, and NEC.2 Dosage regimens include 2 intramuscular (IM) doses of betamethasone, 12 mg, at 24-hour intervals, or 4 IM doses of dexamethasone, 6 mg, at 12-hour intervals. Tocolytics should be administered to delay delivery for 48 hours, thus permitting administration of corticosteroids.3 Prolonged administration of tocolytics is not justified.
- Testing for infection. The patient should be tested for gonorrhea, chlamydia, bacterial vaginosis, and group B streptococcal colonization. If the test for bacterial vaginosis is positive, the patient should be treated with metronidazole, 250 mg orally, 3 times daily, for 7 days. If gonorrhea is present, she should receive either cefixime, 400 mg orally in a single dose, or ceftriaxone, 125 mg IM in a single dose.6
- Prophylactic antibiotics. Even in the absence of obvious lower genital tract infection, patients with PPROM benefit from antibiotic prophylaxis. Many studies investigating the role of prophylactic antibiotics in women with PPROM have been published.7
The largest and most strictly conducted trial was reported by Mercer et al8 on behalf of the Maternal-Fetal Medicine Units Network. Participants—all women with PPROM between 24 and 32 weeks gestation—were randomly assigned to treatment with placebo or IV ampicillin plus erythromycin for 48 hours, followed by oral amoxicillin plus erythromycin for an additional 5 days. The main outcome measure was composite morbidity—at least 1 of the following complications: fetal or infant death, RDS, IVH, NEC, or sepsis within 72 hours of birth. (Researchers also looked at these morbidities individually.) Antibiotic prophylaxis significantly reduced the risk of composite morbidity (44.1% versus 52.9%, P = .04), RDS (40.5% versus 48.7%, P = .04), and NEC (2.3% versus 5.8%, P = .03). Among women who tested negative for group B streptococci, prophylactic antibiotics also significantly prolonged the latent period between PPROM and onset of labor (P <.001>
- Monitoring. Patients selected for expectant management should be observed for evidence of maternal infection. Although a variety of laboratory tests have been proposed for the early diagnosis of infection (white blood cell count, C-reactive protein, nonstress test, biophysical profile, amniotic fluid glucose, or Gram stain), probably the most cost-effective method is monitoring maternal temperature and heart rate and fetal heart rate.
- Outpatient versus inpatient. With rare exceptions, expectant management should take place in the hospital. Carlan et al9 reported a randomized trial of outpatient management of PPROM, in which patients were included if they were judged to be compliant and met all of the following criteria: no evidence of cervical or intra-amniotic infection, minimal cervical dilation, stable fetal presentation, no sign of labor, reassuring heart-rate tracing, and easy access to the hospital. Patients initially were observed for 72 hours in the hospital.
Dr. Duff reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
Management of preterm premature rupture of membranes (PPROM) is the most controversial of all obstetric problems. This article describes an algorithmic approach (FIGURE) to evaluation and treatment.
PPROM refers to rupture of membranes before onset of contractions at a gestational age less than 37 weeks. Approximately 30% to 40% of preterm deliveries are associated with PPROM.1 In turn, preterm delivery is responsible for approximately 75% of all neonatal deaths, excluding infants with anomalies incompatible with life.2
PPROM is multifactorial and complex
PPROM may occur in patients with an incompetent cervix, which can result from previous genital tract surgery or laceration. PPROM occurs with increased frequency in women who smoke or who have multiple gestation, polyhydramnios, or antepartum hemorrhage. Some women with PPROM also appear to have inherent deficiencies in collagen synthesis, which may predispose to weakening of the membranes.1
Infection link confirmed. Of greatest interest in recent years has been the confirmation that PPROM is associated with lower and upper genital tract infection; there are 3 major lines of supporting evidence:
- Many of the bacteria that inhabit the lower genital tract can produce phospholipase A, an enzyme that can trigger the arachidonic acid cascade that leads to the synthesis of prostaglandins. These same bacteria also are able to produce a variety of proteolytic enzymes that can degrade the collagen matrix of the chorioamniotic membranes.
- Compared to women with uncomplicated gestation, those with PPROM are more likely to have lower genital tract infections (such as group B streptococcal colonization or bacterial vaginosis).
- Compared to women with preterm labor and intact membranes, women with PPROM are more likely to have clinical and subclinical chorioamnionitis and inflammatory cytokines in the amniotic fluid.2
The following conclusions are based on good and consistent evidence (level A recommendations) on management of patients with PPROM.
- As a rule, at a gestational age of less than 32 weeks, the greatest threat to the fetus is preterm delivery.
- If the gestational age is 32 weeks or more and fetal lung maturity is confirmed, the risks of expectant management usually exceed the risks of delivery.
- Outpatient management is appropriate only in a highly select group of women.
- In properly selected patients, the benefits of a single course of corticosteroids outweigh the risks.
- Tocolytics are effective in delaying delivery for 48 hours—a critical interval for the administration of corticosteroids.
- Prophylactic antibiotics prolong the latent period and reduce maternal and neonatal infection. These benefits clearly outweigh any risks such as allergic drug reaction or development of resistant organisms.
Direct observation is the best diagnostic test
Patients with PPROM usually note a sudden “gush” of fluid from the vagina. They also may experience a “constant leakage” of fluid or a sensation of “wetness” in the vagina or on the perineum.
The single best test to confirm the diagnosis is direct observation of amniotic fluid in the vaginal vault. Demonstration of severe oligo-hydramnios by ultrasound in a patient with a suggestive history also is helpful.
Although widely used, both the fern test and nitrazine test have pitfalls. The former may be falsely positive in the presence of highly estrogenized cervical mucus or extraneous saline on the glass side (e.g., from a fingerprint). The nitrazine test may be falsely positive in the presence of blood or seminal fluid.
Neonatal and maternal factors guide the management plan
The most important of several factors that must be considered in developing a management plan for PPROM are gestational age and availability of neonatal intensive care. For most patients at less than 36 weeks’ gestation, the prudent course at a hospital with only a level 1 nursery is transfer to a tertiary care facility. If a level 2 nursery is available, the clinician may have sufficient support from neonatology staff to manage patients at 34 weeks’ gestation.
Other important considerations include:
- the presence or absence of labor
- the presence of overt or subclinical infection,
- the stability of the fetal presentation and heart-rate tracing,
- the degree of fetal lung maturation, and
- the degree of cervical effacement and dilation.
- Expectant management. The principal hazards are the risks of ascending infection, umbilical cord prolapse, umbilical cord compression due to oligohydramnios, and abruptio placentae.
- Immediate delivery. The major risks are the well-recognized complications of prema-turity, including respiratory distress syndrome (RDS), intraventricular hemorrhage (IVH), sepsis, necrotizing enterocolitis (NEC), thermal instability, metabolic derangements, apnea and bradycardia, patent ductus arteriosus, and poor feeding. Of these, the 4 most likely to result in neonatal death are RDS, IVH, sepsis, and NEC, all of which are significantly more likely at gestational ages below 32 weeks than at 32 weeks or more.
Algorithmic management approach Assess stability of fetal presentation.
After confirming the diagnosis of PPROM, the clinician should assess gestational age on the basis of history, physical examination, and ultrasound. The fetal presentation and estimated fetal weight should be determined, and the fetal heart rate should be monitored for evidence of recurrent variable decelerations. The mother should be evaluated for chorioamnionitis, primarily by assessment of temperature and maternal and fetal heart rate.
If the fetal presentation is unstable, thus predisposing to umbilical cord prolapse, or if the fetal heart rate tracing is worrisome, the patient should be delivered. If the gravida initially is admitted to a facility with only a level 1 nursery and maternal transfer is impractical, neonatal transfer should take place immediately after the birth.
Assess fetal lung maturity. At a gestational age of less than 32 weeks, lung maturity is very unlikely, and testing is not cost-effective. However, at 32 to 34 weeks, testing should be performed routinely. Amniotic fluid may be obtained by transabdominal amniocentesis or by aspiration of fluid pooled in the vaginal vault. Edwards et al3 recently confirmed the reliability of this sampling method. Lung maturity may be assessed by means of the lecithin:sphingomyelin ratio, lamellar body count, or fetal lung maturity test.
If the fetal presentation is unstable or the fetal heart rate tracing is worrisome, the patient should be delivered.
The decision to deliver. If the gestational age is 32 weeks or more, fetal lung maturity is confirmed, and a neonatal intensive care unit is available, both mother and baby usally will fare better if delivered.
Patients should be treated intrapartum with antibiotics to prevent perinatal transmission of group B streptocol infection. Appropriate regimens include penicillin, then 2.5 million units IV every 4 hours; or ampicillin, 2 g IV initially, then I g every 4 hours.
A recent study confirmed the value of this treatment plan.4 In it, 164 patients at 32 to weeks’ gestation with confirmed fetal lung maturity were randomly assigned to delivery or expectant management. The mean gestational ages in the two groups were similar: 34.1 weeks in the former and 34.3 weeks in the latter group. The expectant management group had a longer duration of hospitalization for the mother and baby, and an increased rate of maternal infection and fetal heart rate abnormalities. In addition, the infants in this group received more frequent, prolonged antibiotic therapy.
Expectant management is appropriate for some patients. If gestational age is less than 32 weeks and the mother and fetus are stable, expectant management is appropriate.
If the patient is at 32 to 34 weeks’ gestation and amniotic fluid cannot be obtained, she should be managed expectantly until 34 weeks. At 34 weeks, she should be delivered.
A recent study by Naef et al5 confirmed the value of delivery at 34 weeks or more. In this investigation, 120 patients at 34 to 36 6/7 weeks’ gestation were randomly assigned to oxytocin induction (n = 57) or expectant management (n = 63). Fetal lung maturity studies were not done. In the expectant management group, chorioamnionitis occurred more often (16% versus 2%, P = .007), maternal hospitalization was prolonged (5.2±6.8 days versus 2.6±1.6 days, P = .006), and there was a trend toward an increased rate of neonatal infection.
- Corticosterioids. A single course of corticosteroids should be administered to reduce the risk of neonatal RDS, IVH, and NEC.2 Dosage regimens include 2 intramuscular (IM) doses of betamethasone, 12 mg, at 24-hour intervals, or 4 IM doses of dexamethasone, 6 mg, at 12-hour intervals. Tocolytics should be administered to delay delivery for 48 hours, thus permitting administration of corticosteroids.3 Prolonged administration of tocolytics is not justified.
- Testing for infection. The patient should be tested for gonorrhea, chlamydia, bacterial vaginosis, and group B streptococcal colonization. If the test for bacterial vaginosis is positive, the patient should be treated with metronidazole, 250 mg orally, 3 times daily, for 7 days. If gonorrhea is present, she should receive either cefixime, 400 mg orally in a single dose, or ceftriaxone, 125 mg IM in a single dose.6
- Prophylactic antibiotics. Even in the absence of obvious lower genital tract infection, patients with PPROM benefit from antibiotic prophylaxis. Many studies investigating the role of prophylactic antibiotics in women with PPROM have been published.7
The largest and most strictly conducted trial was reported by Mercer et al8 on behalf of the Maternal-Fetal Medicine Units Network. Participants—all women with PPROM between 24 and 32 weeks gestation—were randomly assigned to treatment with placebo or IV ampicillin plus erythromycin for 48 hours, followed by oral amoxicillin plus erythromycin for an additional 5 days. The main outcome measure was composite morbidity—at least 1 of the following complications: fetal or infant death, RDS, IVH, NEC, or sepsis within 72 hours of birth. (Researchers also looked at these morbidities individually.) Antibiotic prophylaxis significantly reduced the risk of composite morbidity (44.1% versus 52.9%, P = .04), RDS (40.5% versus 48.7%, P = .04), and NEC (2.3% versus 5.8%, P = .03). Among women who tested negative for group B streptococci, prophylactic antibiotics also significantly prolonged the latent period between PPROM and onset of labor (P <.001>
- Monitoring. Patients selected for expectant management should be observed for evidence of maternal infection. Although a variety of laboratory tests have been proposed for the early diagnosis of infection (white blood cell count, C-reactive protein, nonstress test, biophysical profile, amniotic fluid glucose, or Gram stain), probably the most cost-effective method is monitoring maternal temperature and heart rate and fetal heart rate.
- Outpatient versus inpatient. With rare exceptions, expectant management should take place in the hospital. Carlan et al9 reported a randomized trial of outpatient management of PPROM, in which patients were included if they were judged to be compliant and met all of the following criteria: no evidence of cervical or intra-amniotic infection, minimal cervical dilation, stable fetal presentation, no sign of labor, reassuring heart-rate tracing, and easy access to the hospital. Patients initially were observed for 72 hours in the hospital.
Dr. Duff reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Duff P. Management of premature rupture of membranes in term patients. In: Sciarra JJ, ed. Gynecology and Obstetrics. Chicago, Ill: JB Lippincott; 1997.
2. Mercer B. ACOG Practice Bulletin #1: premature rupture of membranes. Washington, DC: ACOG; June 1998.
3. Edwards RK, Duff P, Ross KC. Amniotic fluid indices of fetal lung maturity with preterm premature rupture of membranes. Obstet Gynecol. 2000;96:102-105.
4. Mercer BM, Crocker LG, Boe NM, Sibai BM. Induction versus expectant management in premature rupture of the membranes with mature amniotic fluid at 32–36 weeks: a randomized trial. Am J Obstet Gynecol. 1993;169:775-782.
5. Naef RW, Albert JR, Ross EL, et al. Premature rupture of membranes at 34 to 37 weeks’ gestation: aggressive versus conservative management. Am J Obstet Gynecol. 1998;178:126-130.
6. Duff P. Maternal and perinatal infection. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics. Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2001.
7. Duff P. Antibiotic treatment in patients with preterm premature rupture of membranes. OBG Management. 2001;13:54-66.
8. Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. JAMA. 1997;278:989-995.
9. Carlan SJ, O’Brien WF, Parsons MT, Lense JJ. Preterm premature rupture of membranes: a randomized study of home versus hospital management. Obstet Gynecol. 1993;81:61-64.
1. Duff P. Management of premature rupture of membranes in term patients. In: Sciarra JJ, ed. Gynecology and Obstetrics. Chicago, Ill: JB Lippincott; 1997.
2. Mercer B. ACOG Practice Bulletin #1: premature rupture of membranes. Washington, DC: ACOG; June 1998.
3. Edwards RK, Duff P, Ross KC. Amniotic fluid indices of fetal lung maturity with preterm premature rupture of membranes. Obstet Gynecol. 2000;96:102-105.
4. Mercer BM, Crocker LG, Boe NM, Sibai BM. Induction versus expectant management in premature rupture of the membranes with mature amniotic fluid at 32–36 weeks: a randomized trial. Am J Obstet Gynecol. 1993;169:775-782.
5. Naef RW, Albert JR, Ross EL, et al. Premature rupture of membranes at 34 to 37 weeks’ gestation: aggressive versus conservative management. Am J Obstet Gynecol. 1998;178:126-130.
6. Duff P. Maternal and perinatal infection. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics. Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2001.
7. Duff P. Antibiotic treatment in patients with preterm premature rupture of membranes. OBG Management. 2001;13:54-66.
8. Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. JAMA. 1997;278:989-995.
9. Carlan SJ, O’Brien WF, Parsons MT, Lense JJ. Preterm premature rupture of membranes: a randomized study of home versus hospital management. Obstet Gynecol. 1993;81:61-64.