User login
Vesicular rash in a newborn girl
A 3-week-old girl was brought to our pediatric dermatology clinic by her mother for evaluation of a rash on her arms, legs, and trunk that she’d had since birth. The child was otherwise healthy and the mother said she hadn’t experienced any complications during pregnancy or the perinatal period.
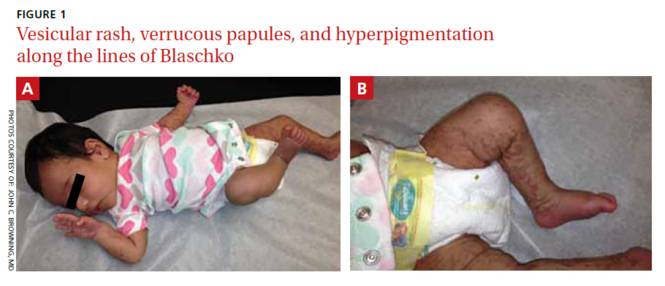
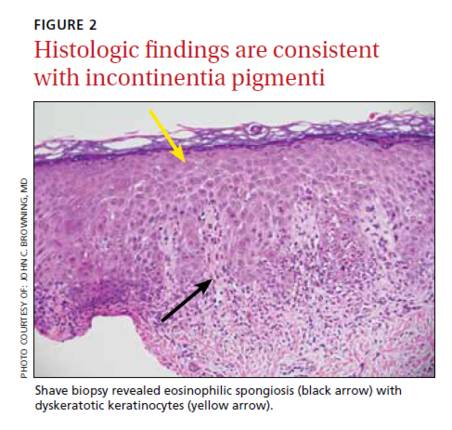
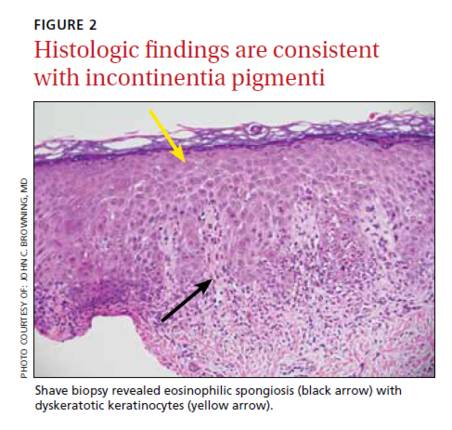
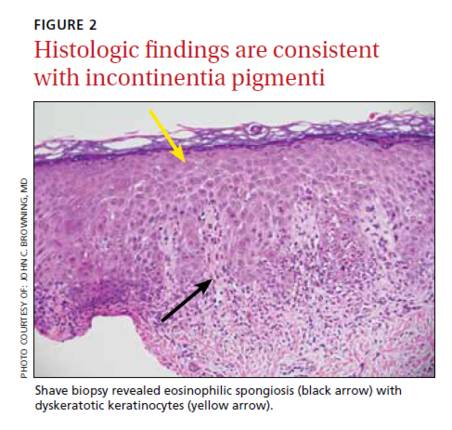
On physical exam, we noted erythematous papules, vesicles, and brown verrucous papules distributed on the newborn’s torso and extremities in a Blaschkoid patter (FIGURE 1). A shave biopsy revealed a mild to moderate hyperplastic epidermis with eosinophilic spongiosis and many scattered necrotic keratinocytes (FIGURE 2).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Incontinentia pigmenti
Based on the appearance and pattern of the rash and histologic findings, we diagnosed incontinentia pigmenti (IP) in this patient. IP is a rare genodermatosis characterized by abnormalities of the tissues and organs derived from the ectoderm and neuroectoderm. It is a type of ectodermal dysplasia that involves the skin, and sometimes other tissues.1
IP is transmitted in an X-linked dominant manner and occurs predominantly in females; it is often lethal in males. It is caused by a mutation of the IKBKG (inhibitor of kappa B kinase gamma) gene, which results in defective activation of nuclear factor-kappa beta (NF-κB), an essential regulator of inflammatory and apoptotic pathways.1 In females, lyonization results in functional mosaicism of X-linked genes, which is manifested by the Blaschkoid distribution of cutaneous lesions.2
In addition to the skin, IP can also affect the eyes, central nervous system (CNS), teeth, hair, and nails.1 Ocular symptoms are present in 35% to 77% of patients with IP.3 Such symptoms are often unilateral, persistent, and may be highly debilitating. The most serious and by far the most common ocular anomalies affect the retina, with possible development of vascular anomalies, pre-retinal fibrosis, retrolental mass, retinal detachment, and a change in the retinal pigment epithelium. Common non-retinal ocular complications of IP include cataracts and strabismus.
The skin lesions of IP progress through 4 stages
Cutaneous manifestations of IP follow the lines of Blaschko and occur in a chronological sequence of 4 stages, which may temporarily overlap.4
The first stage (the vesicular stage) is comprised of papules, vesicles, or pustules on an erythematous base. These skin lesions are present at birth or develop in the first few weeks of life in 90% of patients, and typically resolve around 4 months.5
The second stage (the verrucous stage) consists of wart-like papules and plaques. These most commonly develop between 2 to 6 weeks and resolve by 6 months.
The third stage (the hyperpigmented stage) is marked by linear or whorled brown pigmentation. These lesions typically develop during the first 3 to 6 months of life and slowly disappear in adolescence.6
The final stage (the hypopigmented/atrophic stage) develops in adolescence and may be permanent. It often affects the lower extremities with areas of hypopigmentation, atrophy, and an absence of hair.
The diagnosis of IP is made based on the presence of typical cutaneous findings of any stage, most commonly the characteristic vesicular rash and the classic Blaschkoid hyperpigmentation on the trunk that often fades in adolescence.7 Typical features on cutaneous histology, such as eosinophilic spongiosis and dyskeratotic keratinocytes, can support the diagnosis.
Abnormalities of the teeth, eyes, hair, nails, CNS (eg, seizures, mental retardation, or microcephaly), palate, and nipple and breast have also been seen during infancy and are permanent. The mother of a child with IP may have a history of multiple miscarriages of male fetuses.6
Distinguish the rash of IP from other blistering diseases
The differential diagnosis of IP includes other cutaneous blistering diseases, such as herpes simplex virus (HSV) infection and epidermolysis bullosa (EB).8 HSV infection is the most common misdiagnosis in a neonate with vesicles, especially when seizures are also present.6 EB is a rare group of inherited disorders that manifest as blistering of the skin in infants, most commonly affecting the fingers, hands, elbows, feet, legs, and diaper area.
The distribution of skin lesions along the lines of Blaschko, the progression of the rash through different stages, and the possible maternal history of spontaneous abortions can distinguish IP from both HSV infection and EB.6 Cutaneous histopathology is also helpful for differentiating vesicular lesions in infancy and can confirm the diagnosis of IP.
No specific treatment for IP rash; carefully evaluate other symptoms
Because the skin manifestations of IP usually resolve spontaneously, no specific treatment is required. The prognosis of a patient with IP depends on the presence and severity of extracutaneous manifestations of the condition.
A patient with IP who has abnormal findings on a neurologic examination, vascular retinopathy, or both should undergo routine neurodevelopmental assessment and neuroimaging.5 Treatment of neurologic complications is symptomatic. Speech therapy may play an important role in management of these patients because dental and neurologic abnormalities may result in dysfunction of chewing, swallowing, speech, language, and hearing.
Ophthalmology referral is also crucial because untreated retinal disorders have been reported to cause blindness in 7% to 23% of patients with IP.3 Screening is recommended at birth (or at diagnosis), and the child is followed regularly during the first year of life.5
Morbidity and mortality primarily result from neurologic manifestations (most commonly seizures and mental retardation) and ophthalmologic complications, which can result in vision loss.
Our patient presented with a rash in the vesicular stage of IP that was transitioning to the verrucous stage. She was seen by Ophthalmology at 4 weeks of age and there were no concerning findings at that time. She will continue to follow up with Ophthalmology, Dermatology, and her primary care physician.
CORRESPONDENCE
John C. Browning, MD, Chief of Dermatology, Children’s Hospital of San Antonio, 333 N. Santa Rosa, San Antonio, TX, 78207; [email protected]
1. Landy SJ, Donnai D. Incontinentia pigmenti (Bloch-Sulzberger syndrome). J Med Genet. 1993;30:53-59.
2. Migeon BR, Axelman J, Jan de Beur S, et al. Selection against lethal alleles in females heterozygous for incontinentia pigmenti. Am J Hum Genet. 1989;44:100-106.
3. Minic S, Obradovic M, Kovacevic I, et al. Ocular anomalies in incontinentia pigmenti: literature review and meta-analysis. Srp Arh Celok Lek. 2010;138:408-413.
4. Poziomczyk CS, Recuero JK, Bringhenti L, et al. Incontinentia pigmenti. An Bras Dermatol. 2014;89:26-36.
5. Hadj-Rabia S, Froidevaux D, Bodak N, et al. Clinical study of 40 cases of incontinentia pigmenti. Arch Dermatol. 2003;139:1163-1170.
6. Faloyin M, Levitt J, Bercowitz E, et al. All that is vesicular is not herpes: incontinentia pigmenti masquerading as herpes simplex virus in a newborn. Pediatrics. 2004;114:e270-e272.
7. Minic S, Trpinac D, Obradovic M. Incontinentia pigmenti diagnostic criteria update. Clin Genet. 2014;85:536-542.
8. Cohen PR. Incontinentia pigmenti: clinicopathologic characteristics and differential diagnosis. Cutis. 1994;54:161-166.
A 3-week-old girl was brought to our pediatric dermatology clinic by her mother for evaluation of a rash on her arms, legs, and trunk that she’d had since birth. The child was otherwise healthy and the mother said she hadn’t experienced any complications during pregnancy or the perinatal period.
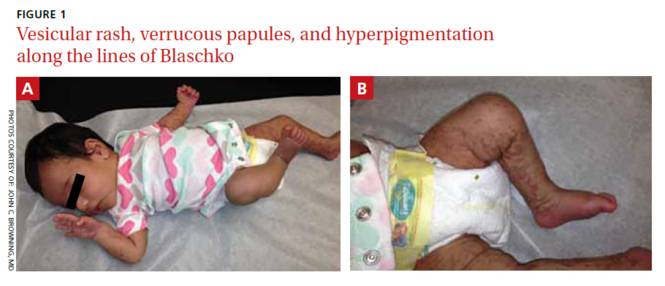
On physical exam, we noted erythematous papules, vesicles, and brown verrucous papules distributed on the newborn’s torso and extremities in a Blaschkoid patter (FIGURE 1). A shave biopsy revealed a mild to moderate hyperplastic epidermis with eosinophilic spongiosis and many scattered necrotic keratinocytes (FIGURE 2).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Incontinentia pigmenti
Based on the appearance and pattern of the rash and histologic findings, we diagnosed incontinentia pigmenti (IP) in this patient. IP is a rare genodermatosis characterized by abnormalities of the tissues and organs derived from the ectoderm and neuroectoderm. It is a type of ectodermal dysplasia that involves the skin, and sometimes other tissues.1
IP is transmitted in an X-linked dominant manner and occurs predominantly in females; it is often lethal in males. It is caused by a mutation of the IKBKG (inhibitor of kappa B kinase gamma) gene, which results in defective activation of nuclear factor-kappa beta (NF-κB), an essential regulator of inflammatory and apoptotic pathways.1 In females, lyonization results in functional mosaicism of X-linked genes, which is manifested by the Blaschkoid distribution of cutaneous lesions.2
In addition to the skin, IP can also affect the eyes, central nervous system (CNS), teeth, hair, and nails.1 Ocular symptoms are present in 35% to 77% of patients with IP.3 Such symptoms are often unilateral, persistent, and may be highly debilitating. The most serious and by far the most common ocular anomalies affect the retina, with possible development of vascular anomalies, pre-retinal fibrosis, retrolental mass, retinal detachment, and a change in the retinal pigment epithelium. Common non-retinal ocular complications of IP include cataracts and strabismus.
The skin lesions of IP progress through 4 stages
Cutaneous manifestations of IP follow the lines of Blaschko and occur in a chronological sequence of 4 stages, which may temporarily overlap.4
The first stage (the vesicular stage) is comprised of papules, vesicles, or pustules on an erythematous base. These skin lesions are present at birth or develop in the first few weeks of life in 90% of patients, and typically resolve around 4 months.5
The second stage (the verrucous stage) consists of wart-like papules and plaques. These most commonly develop between 2 to 6 weeks and resolve by 6 months.
The third stage (the hyperpigmented stage) is marked by linear or whorled brown pigmentation. These lesions typically develop during the first 3 to 6 months of life and slowly disappear in adolescence.6
The final stage (the hypopigmented/atrophic stage) develops in adolescence and may be permanent. It often affects the lower extremities with areas of hypopigmentation, atrophy, and an absence of hair.
The diagnosis of IP is made based on the presence of typical cutaneous findings of any stage, most commonly the characteristic vesicular rash and the classic Blaschkoid hyperpigmentation on the trunk that often fades in adolescence.7 Typical features on cutaneous histology, such as eosinophilic spongiosis and dyskeratotic keratinocytes, can support the diagnosis.
Abnormalities of the teeth, eyes, hair, nails, CNS (eg, seizures, mental retardation, or microcephaly), palate, and nipple and breast have also been seen during infancy and are permanent. The mother of a child with IP may have a history of multiple miscarriages of male fetuses.6
Distinguish the rash of IP from other blistering diseases
The differential diagnosis of IP includes other cutaneous blistering diseases, such as herpes simplex virus (HSV) infection and epidermolysis bullosa (EB).8 HSV infection is the most common misdiagnosis in a neonate with vesicles, especially when seizures are also present.6 EB is a rare group of inherited disorders that manifest as blistering of the skin in infants, most commonly affecting the fingers, hands, elbows, feet, legs, and diaper area.
The distribution of skin lesions along the lines of Blaschko, the progression of the rash through different stages, and the possible maternal history of spontaneous abortions can distinguish IP from both HSV infection and EB.6 Cutaneous histopathology is also helpful for differentiating vesicular lesions in infancy and can confirm the diagnosis of IP.
No specific treatment for IP rash; carefully evaluate other symptoms
Because the skin manifestations of IP usually resolve spontaneously, no specific treatment is required. The prognosis of a patient with IP depends on the presence and severity of extracutaneous manifestations of the condition.
A patient with IP who has abnormal findings on a neurologic examination, vascular retinopathy, or both should undergo routine neurodevelopmental assessment and neuroimaging.5 Treatment of neurologic complications is symptomatic. Speech therapy may play an important role in management of these patients because dental and neurologic abnormalities may result in dysfunction of chewing, swallowing, speech, language, and hearing.
Ophthalmology referral is also crucial because untreated retinal disorders have been reported to cause blindness in 7% to 23% of patients with IP.3 Screening is recommended at birth (or at diagnosis), and the child is followed regularly during the first year of life.5
Morbidity and mortality primarily result from neurologic manifestations (most commonly seizures and mental retardation) and ophthalmologic complications, which can result in vision loss.
Our patient presented with a rash in the vesicular stage of IP that was transitioning to the verrucous stage. She was seen by Ophthalmology at 4 weeks of age and there were no concerning findings at that time. She will continue to follow up with Ophthalmology, Dermatology, and her primary care physician.
CORRESPONDENCE
John C. Browning, MD, Chief of Dermatology, Children’s Hospital of San Antonio, 333 N. Santa Rosa, San Antonio, TX, 78207; [email protected]
A 3-week-old girl was brought to our pediatric dermatology clinic by her mother for evaluation of a rash on her arms, legs, and trunk that she’d had since birth. The child was otherwise healthy and the mother said she hadn’t experienced any complications during pregnancy or the perinatal period.
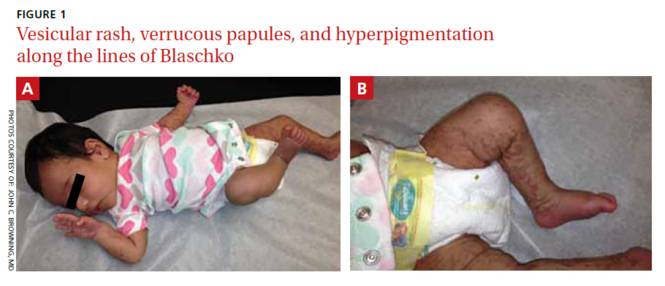
On physical exam, we noted erythematous papules, vesicles, and brown verrucous papules distributed on the newborn’s torso and extremities in a Blaschkoid patter (FIGURE 1). A shave biopsy revealed a mild to moderate hyperplastic epidermis with eosinophilic spongiosis and many scattered necrotic keratinocytes (FIGURE 2).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Incontinentia pigmenti
Based on the appearance and pattern of the rash and histologic findings, we diagnosed incontinentia pigmenti (IP) in this patient. IP is a rare genodermatosis characterized by abnormalities of the tissues and organs derived from the ectoderm and neuroectoderm. It is a type of ectodermal dysplasia that involves the skin, and sometimes other tissues.1
IP is transmitted in an X-linked dominant manner and occurs predominantly in females; it is often lethal in males. It is caused by a mutation of the IKBKG (inhibitor of kappa B kinase gamma) gene, which results in defective activation of nuclear factor-kappa beta (NF-κB), an essential regulator of inflammatory and apoptotic pathways.1 In females, lyonization results in functional mosaicism of X-linked genes, which is manifested by the Blaschkoid distribution of cutaneous lesions.2
In addition to the skin, IP can also affect the eyes, central nervous system (CNS), teeth, hair, and nails.1 Ocular symptoms are present in 35% to 77% of patients with IP.3 Such symptoms are often unilateral, persistent, and may be highly debilitating. The most serious and by far the most common ocular anomalies affect the retina, with possible development of vascular anomalies, pre-retinal fibrosis, retrolental mass, retinal detachment, and a change in the retinal pigment epithelium. Common non-retinal ocular complications of IP include cataracts and strabismus.
The skin lesions of IP progress through 4 stages
Cutaneous manifestations of IP follow the lines of Blaschko and occur in a chronological sequence of 4 stages, which may temporarily overlap.4
The first stage (the vesicular stage) is comprised of papules, vesicles, or pustules on an erythematous base. These skin lesions are present at birth or develop in the first few weeks of life in 90% of patients, and typically resolve around 4 months.5
The second stage (the verrucous stage) consists of wart-like papules and plaques. These most commonly develop between 2 to 6 weeks and resolve by 6 months.
The third stage (the hyperpigmented stage) is marked by linear or whorled brown pigmentation. These lesions typically develop during the first 3 to 6 months of life and slowly disappear in adolescence.6
The final stage (the hypopigmented/atrophic stage) develops in adolescence and may be permanent. It often affects the lower extremities with areas of hypopigmentation, atrophy, and an absence of hair.
The diagnosis of IP is made based on the presence of typical cutaneous findings of any stage, most commonly the characteristic vesicular rash and the classic Blaschkoid hyperpigmentation on the trunk that often fades in adolescence.7 Typical features on cutaneous histology, such as eosinophilic spongiosis and dyskeratotic keratinocytes, can support the diagnosis.
Abnormalities of the teeth, eyes, hair, nails, CNS (eg, seizures, mental retardation, or microcephaly), palate, and nipple and breast have also been seen during infancy and are permanent. The mother of a child with IP may have a history of multiple miscarriages of male fetuses.6
Distinguish the rash of IP from other blistering diseases
The differential diagnosis of IP includes other cutaneous blistering diseases, such as herpes simplex virus (HSV) infection and epidermolysis bullosa (EB).8 HSV infection is the most common misdiagnosis in a neonate with vesicles, especially when seizures are also present.6 EB is a rare group of inherited disorders that manifest as blistering of the skin in infants, most commonly affecting the fingers, hands, elbows, feet, legs, and diaper area.
The distribution of skin lesions along the lines of Blaschko, the progression of the rash through different stages, and the possible maternal history of spontaneous abortions can distinguish IP from both HSV infection and EB.6 Cutaneous histopathology is also helpful for differentiating vesicular lesions in infancy and can confirm the diagnosis of IP.
No specific treatment for IP rash; carefully evaluate other symptoms
Because the skin manifestations of IP usually resolve spontaneously, no specific treatment is required. The prognosis of a patient with IP depends on the presence and severity of extracutaneous manifestations of the condition.
A patient with IP who has abnormal findings on a neurologic examination, vascular retinopathy, or both should undergo routine neurodevelopmental assessment and neuroimaging.5 Treatment of neurologic complications is symptomatic. Speech therapy may play an important role in management of these patients because dental and neurologic abnormalities may result in dysfunction of chewing, swallowing, speech, language, and hearing.
Ophthalmology referral is also crucial because untreated retinal disorders have been reported to cause blindness in 7% to 23% of patients with IP.3 Screening is recommended at birth (or at diagnosis), and the child is followed regularly during the first year of life.5
Morbidity and mortality primarily result from neurologic manifestations (most commonly seizures and mental retardation) and ophthalmologic complications, which can result in vision loss.
Our patient presented with a rash in the vesicular stage of IP that was transitioning to the verrucous stage. She was seen by Ophthalmology at 4 weeks of age and there were no concerning findings at that time. She will continue to follow up with Ophthalmology, Dermatology, and her primary care physician.
CORRESPONDENCE
John C. Browning, MD, Chief of Dermatology, Children’s Hospital of San Antonio, 333 N. Santa Rosa, San Antonio, TX, 78207; [email protected]
1. Landy SJ, Donnai D. Incontinentia pigmenti (Bloch-Sulzberger syndrome). J Med Genet. 1993;30:53-59.
2. Migeon BR, Axelman J, Jan de Beur S, et al. Selection against lethal alleles in females heterozygous for incontinentia pigmenti. Am J Hum Genet. 1989;44:100-106.
3. Minic S, Obradovic M, Kovacevic I, et al. Ocular anomalies in incontinentia pigmenti: literature review and meta-analysis. Srp Arh Celok Lek. 2010;138:408-413.
4. Poziomczyk CS, Recuero JK, Bringhenti L, et al. Incontinentia pigmenti. An Bras Dermatol. 2014;89:26-36.
5. Hadj-Rabia S, Froidevaux D, Bodak N, et al. Clinical study of 40 cases of incontinentia pigmenti. Arch Dermatol. 2003;139:1163-1170.
6. Faloyin M, Levitt J, Bercowitz E, et al. All that is vesicular is not herpes: incontinentia pigmenti masquerading as herpes simplex virus in a newborn. Pediatrics. 2004;114:e270-e272.
7. Minic S, Trpinac D, Obradovic M. Incontinentia pigmenti diagnostic criteria update. Clin Genet. 2014;85:536-542.
8. Cohen PR. Incontinentia pigmenti: clinicopathologic characteristics and differential diagnosis. Cutis. 1994;54:161-166.
1. Landy SJ, Donnai D. Incontinentia pigmenti (Bloch-Sulzberger syndrome). J Med Genet. 1993;30:53-59.
2. Migeon BR, Axelman J, Jan de Beur S, et al. Selection against lethal alleles in females heterozygous for incontinentia pigmenti. Am J Hum Genet. 1989;44:100-106.
3. Minic S, Obradovic M, Kovacevic I, et al. Ocular anomalies in incontinentia pigmenti: literature review and meta-analysis. Srp Arh Celok Lek. 2010;138:408-413.
4. Poziomczyk CS, Recuero JK, Bringhenti L, et al. Incontinentia pigmenti. An Bras Dermatol. 2014;89:26-36.
5. Hadj-Rabia S, Froidevaux D, Bodak N, et al. Clinical study of 40 cases of incontinentia pigmenti. Arch Dermatol. 2003;139:1163-1170.
6. Faloyin M, Levitt J, Bercowitz E, et al. All that is vesicular is not herpes: incontinentia pigmenti masquerading as herpes simplex virus in a newborn. Pediatrics. 2004;114:e270-e272.
7. Minic S, Trpinac D, Obradovic M. Incontinentia pigmenti diagnostic criteria update. Clin Genet. 2014;85:536-542.
8. Cohen PR. Incontinentia pigmenti: clinicopathologic characteristics and differential diagnosis. Cutis. 1994;54:161-166.
