User login
MM patients with concurrent AL show poor survival when coupled to cardiac dysfunction
Cardiac dysfunction is a major determinant of poor survival in multiple myeloma (MM) patients with concurrently developed light chain amyloidosis (AL), according to the results of a small cohort study conducted at a single institution.
A total of 53 patients in whom MM and AL were initially diagnosed from July 2006 to June 2016, The cohort comprised 36 men and 17 women with a median age of 59 years; main organ involvement was kidney (72%) and heart (62%). A bortezomib-based regimen was used in 22 patients whose response rate was better than the other 21 patients who received nonbortezomib-based regimens (64% vs. 29%). The median overall survival for the total cohort was 12 months (P < .05), according to the report published in Clinical Lymphoma, Myeloma & Leukemia.
Of particular note, the researchers found that cardiac involvement significantly and adversely affected overall survival (6 vs. 40 months), as did low systolic blood pressure (<90 mm Hg, 3 vs. 8.5 months), according to Yuanyuan Yu and colleagues at the Multiple Myeloma Medical Center of Beijing, Beijing Chao-yang Hospital.
“Although MM-concurrent AL is rare, AL has a negative impact on survival. This study determined that cardiovascular dysfunction caused by AL is the main determinant of shortening survival in patients with MM complicated with AL, and the necessary interventions should be taken to prevent cardiovascular risk,” the researchers concluded.
The work was supported by the Beijing Municipal Health Commission. The authors reported that they had no disclosures.
SOURCE: Yu Y et al. Clin Lymphoma Myeloma Leuk. 2020;20(8):519-25.
Cardiac dysfunction is a major determinant of poor survival in multiple myeloma (MM) patients with concurrently developed light chain amyloidosis (AL), according to the results of a small cohort study conducted at a single institution.
A total of 53 patients in whom MM and AL were initially diagnosed from July 2006 to June 2016, The cohort comprised 36 men and 17 women with a median age of 59 years; main organ involvement was kidney (72%) and heart (62%). A bortezomib-based regimen was used in 22 patients whose response rate was better than the other 21 patients who received nonbortezomib-based regimens (64% vs. 29%). The median overall survival for the total cohort was 12 months (P < .05), according to the report published in Clinical Lymphoma, Myeloma & Leukemia.
Of particular note, the researchers found that cardiac involvement significantly and adversely affected overall survival (6 vs. 40 months), as did low systolic blood pressure (<90 mm Hg, 3 vs. 8.5 months), according to Yuanyuan Yu and colleagues at the Multiple Myeloma Medical Center of Beijing, Beijing Chao-yang Hospital.
“Although MM-concurrent AL is rare, AL has a negative impact on survival. This study determined that cardiovascular dysfunction caused by AL is the main determinant of shortening survival in patients with MM complicated with AL, and the necessary interventions should be taken to prevent cardiovascular risk,” the researchers concluded.
The work was supported by the Beijing Municipal Health Commission. The authors reported that they had no disclosures.
SOURCE: Yu Y et al. Clin Lymphoma Myeloma Leuk. 2020;20(8):519-25.
Cardiac dysfunction is a major determinant of poor survival in multiple myeloma (MM) patients with concurrently developed light chain amyloidosis (AL), according to the results of a small cohort study conducted at a single institution.
A total of 53 patients in whom MM and AL were initially diagnosed from July 2006 to June 2016, The cohort comprised 36 men and 17 women with a median age of 59 years; main organ involvement was kidney (72%) and heart (62%). A bortezomib-based regimen was used in 22 patients whose response rate was better than the other 21 patients who received nonbortezomib-based regimens (64% vs. 29%). The median overall survival for the total cohort was 12 months (P < .05), according to the report published in Clinical Lymphoma, Myeloma & Leukemia.
Of particular note, the researchers found that cardiac involvement significantly and adversely affected overall survival (6 vs. 40 months), as did low systolic blood pressure (<90 mm Hg, 3 vs. 8.5 months), according to Yuanyuan Yu and colleagues at the Multiple Myeloma Medical Center of Beijing, Beijing Chao-yang Hospital.
“Although MM-concurrent AL is rare, AL has a negative impact on survival. This study determined that cardiovascular dysfunction caused by AL is the main determinant of shortening survival in patients with MM complicated with AL, and the necessary interventions should be taken to prevent cardiovascular risk,” the researchers concluded.
The work was supported by the Beijing Municipal Health Commission. The authors reported that they had no disclosures.
SOURCE: Yu Y et al. Clin Lymphoma Myeloma Leuk. 2020;20(8):519-25.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
HSCT or systemic treatment should be offered to HIV+ patients with lymphoma
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Heavy menstrual bleeding difficult to control in young patients with inherited platelet disorders
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
Transitioning regimen may prolong proteasome inhibitor–based therapy for MM
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
FDA approves selinexor for relapsed/refractory DLBCL
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
FROM THE FDA
Oxidatative stress–related genetic variant tied to stroke risk in sickle cell patients
Oxidative stress-related genetic variants, in particular, the according to Igor F. Domingos of the Genetics Postgraduate Program, Federal University of Pernambuco, Recife, Brazil, and colleagues.
The researchers genotyped 499 unrelated adult patients with sickle cell anemia (SCA) for a variety of polymorphisms, along with alpha-thalassemia status and beta-globin gene haplotypes.
They found that SOD2 Val16Ala polymorphism was independently associated with risk of stroke (odds ratio, 1.98; 95% confidence interval, 1.18-3.32; P = .009) and with the long-term cumulative incidence of stroke (hazard ratio, 2.24; 95% CI, 1.3-3.9; P = .004).
A crucial limitation identified by the authors was the inability to replicate their results in a validation cohort. They suggested that there could have been genetic differences between the Brazilian population and the validation cohort of 231 patients followed at King’s College London for whom biological samples was available. They also suggested that patient treatment history between the two countries may be a factor.
“We believe that our study represents an alternative for understudied SCA populations with no access to TCD [transcranial Doppler ultrasound screening] and imaging exams, in which genetic modifiers may be a useful tool for predicting stroke in SCA,” the authors concluded.
The authors reported that they had no competing financial interests.
[email protected]
SOURCE: Domingos IF et al. J Neurol Sci. 2020 Apr 16; doi: 10.1016/j.jns.2020.116839.
Oxidative stress-related genetic variants, in particular, the according to Igor F. Domingos of the Genetics Postgraduate Program, Federal University of Pernambuco, Recife, Brazil, and colleagues.
The researchers genotyped 499 unrelated adult patients with sickle cell anemia (SCA) for a variety of polymorphisms, along with alpha-thalassemia status and beta-globin gene haplotypes.
They found that SOD2 Val16Ala polymorphism was independently associated with risk of stroke (odds ratio, 1.98; 95% confidence interval, 1.18-3.32; P = .009) and with the long-term cumulative incidence of stroke (hazard ratio, 2.24; 95% CI, 1.3-3.9; P = .004).
A crucial limitation identified by the authors was the inability to replicate their results in a validation cohort. They suggested that there could have been genetic differences between the Brazilian population and the validation cohort of 231 patients followed at King’s College London for whom biological samples was available. They also suggested that patient treatment history between the two countries may be a factor.
“We believe that our study represents an alternative for understudied SCA populations with no access to TCD [transcranial Doppler ultrasound screening] and imaging exams, in which genetic modifiers may be a useful tool for predicting stroke in SCA,” the authors concluded.
The authors reported that they had no competing financial interests.
[email protected]
SOURCE: Domingos IF et al. J Neurol Sci. 2020 Apr 16; doi: 10.1016/j.jns.2020.116839.
Oxidative stress-related genetic variants, in particular, the according to Igor F. Domingos of the Genetics Postgraduate Program, Federal University of Pernambuco, Recife, Brazil, and colleagues.
The researchers genotyped 499 unrelated adult patients with sickle cell anemia (SCA) for a variety of polymorphisms, along with alpha-thalassemia status and beta-globin gene haplotypes.
They found that SOD2 Val16Ala polymorphism was independently associated with risk of stroke (odds ratio, 1.98; 95% confidence interval, 1.18-3.32; P = .009) and with the long-term cumulative incidence of stroke (hazard ratio, 2.24; 95% CI, 1.3-3.9; P = .004).
A crucial limitation identified by the authors was the inability to replicate their results in a validation cohort. They suggested that there could have been genetic differences between the Brazilian population and the validation cohort of 231 patients followed at King’s College London for whom biological samples was available. They also suggested that patient treatment history between the two countries may be a factor.
“We believe that our study represents an alternative for understudied SCA populations with no access to TCD [transcranial Doppler ultrasound screening] and imaging exams, in which genetic modifiers may be a useful tool for predicting stroke in SCA,” the authors concluded.
The authors reported that they had no competing financial interests.
[email protected]
SOURCE: Domingos IF et al. J Neurol Sci. 2020 Apr 16; doi: 10.1016/j.jns.2020.116839.
FROM THE JOURNAL OF NEUROLOGICAL SCIENCES
Key clinical point: SOD2 Val16Ala polymorphism may represent a simple and inexpensive alternative for identifying sickle cell patients at risk of stroke.
Major finding: SOD2 Val16Ala polymorphism was independently associated with an increased risk of stroke (odds ratio, 1.98; P = .009).
Study details: A total of 499 unrelated adult patients with sickle cell disease were genotyped.
Disclosures: The authors reported that they had no competing financial interests.
Source: Domingos IF et al. J Neurol Sci. 2020 Apr 16. doi: org/10.1016/j.jns.2020.116839.
First-in-kind anti-CD47 antibody shows promise for MDS and AML treatment
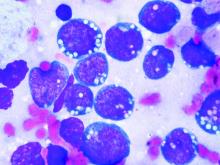
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
FROM ASCO 2020
Subcutaneous hep A vaccination as effective as intramuscular for bleeding disorder patients
Subcutaneous hepatitis A vaccination is as effective and may be safer for patients with bleeding disorders, according to a study by Mayumi Nakasone, MD, and colleagues.
The large number of donor exposures in bleeding disorder patients who require routine use of clotting factor concentrates remains a concern with regard to the risk of virus infection. Therefore, vaccinations for viruses such as hepatitis A are recommended. Although the intramuscular (IM) route is recommended for hepatitis A vaccination, patients with bleeding disorders have been advised to avoid IM injections because of the risk of bleeding and bruising of muscles, requiring infusion of clotting factor concentrates or other blood products for its treatment, according to Dr. Nakasone of the University of São Paulo and colleagues. They assessed 78 adult and pediatric patients with blood disorders randomized to vaccination for hepatitis A either subcutaneously (SC) or IM, according their study published on Vaccine.
The study was conducted at a single hemophilia center between May 2006 and February 2017.
Among the 78 patients, 58 (74.4%) presented hemophilia A (34 of the SC group and 24 of the IM group), 13 (16.7%) hemophilia B (4 of the SC group and 9 of the IM group) and 7 (8.9%) other bleeding disorders. There were no statistically significant differences between the SC and the IM groups in patients diagnosis or sex.
A total of 38 patients had serology performed after the first vaccine dose, determining seroconversion rates of 83.3% and 90.0% for the SC and the IM group, respectively, a nonsignificant difference. After the second vaccine dose, the seroconversion rate for the SC group was 97.5% and for the IM group was 97.4%, also a nonsignificant difference.
At a median of 9 years after a second vaccine dose, antibody titers for the SC group were slightly greater than the IM group (7.6 vs. 7.4), but this was also not a significant difference. There were no serious adverse events in both groups, according to Dr. Nakasone and colleagues. And although twice as many patients of the IM group required clotting factor concentrates for adverse events, compared with the SC group (15.8% vs. 7.5%), the difference was not significant.
“Hepatitis A vaccine administered subcutaneously is as immunogenic, long-term protective, and even safer as the intramuscular route for both children and adults not only with hemophilia, but also with other bleeding disorders,” the researchers concluded.
The authors declared that they had no disclosures.
SOURCE: Nakasone M et al. Vaccine 2020;38:4162-6.
Subcutaneous hepatitis A vaccination is as effective and may be safer for patients with bleeding disorders, according to a study by Mayumi Nakasone, MD, and colleagues.
The large number of donor exposures in bleeding disorder patients who require routine use of clotting factor concentrates remains a concern with regard to the risk of virus infection. Therefore, vaccinations for viruses such as hepatitis A are recommended. Although the intramuscular (IM) route is recommended for hepatitis A vaccination, patients with bleeding disorders have been advised to avoid IM injections because of the risk of bleeding and bruising of muscles, requiring infusion of clotting factor concentrates or other blood products for its treatment, according to Dr. Nakasone of the University of São Paulo and colleagues. They assessed 78 adult and pediatric patients with blood disorders randomized to vaccination for hepatitis A either subcutaneously (SC) or IM, according their study published on Vaccine.
The study was conducted at a single hemophilia center between May 2006 and February 2017.
Among the 78 patients, 58 (74.4%) presented hemophilia A (34 of the SC group and 24 of the IM group), 13 (16.7%) hemophilia B (4 of the SC group and 9 of the IM group) and 7 (8.9%) other bleeding disorders. There were no statistically significant differences between the SC and the IM groups in patients diagnosis or sex.
A total of 38 patients had serology performed after the first vaccine dose, determining seroconversion rates of 83.3% and 90.0% for the SC and the IM group, respectively, a nonsignificant difference. After the second vaccine dose, the seroconversion rate for the SC group was 97.5% and for the IM group was 97.4%, also a nonsignificant difference.
At a median of 9 years after a second vaccine dose, antibody titers for the SC group were slightly greater than the IM group (7.6 vs. 7.4), but this was also not a significant difference. There were no serious adverse events in both groups, according to Dr. Nakasone and colleagues. And although twice as many patients of the IM group required clotting factor concentrates for adverse events, compared with the SC group (15.8% vs. 7.5%), the difference was not significant.
“Hepatitis A vaccine administered subcutaneously is as immunogenic, long-term protective, and even safer as the intramuscular route for both children and adults not only with hemophilia, but also with other bleeding disorders,” the researchers concluded.
The authors declared that they had no disclosures.
SOURCE: Nakasone M et al. Vaccine 2020;38:4162-6.
Subcutaneous hepatitis A vaccination is as effective and may be safer for patients with bleeding disorders, according to a study by Mayumi Nakasone, MD, and colleagues.
The large number of donor exposures in bleeding disorder patients who require routine use of clotting factor concentrates remains a concern with regard to the risk of virus infection. Therefore, vaccinations for viruses such as hepatitis A are recommended. Although the intramuscular (IM) route is recommended for hepatitis A vaccination, patients with bleeding disorders have been advised to avoid IM injections because of the risk of bleeding and bruising of muscles, requiring infusion of clotting factor concentrates or other blood products for its treatment, according to Dr. Nakasone of the University of São Paulo and colleagues. They assessed 78 adult and pediatric patients with blood disorders randomized to vaccination for hepatitis A either subcutaneously (SC) or IM, according their study published on Vaccine.
The study was conducted at a single hemophilia center between May 2006 and February 2017.
Among the 78 patients, 58 (74.4%) presented hemophilia A (34 of the SC group and 24 of the IM group), 13 (16.7%) hemophilia B (4 of the SC group and 9 of the IM group) and 7 (8.9%) other bleeding disorders. There were no statistically significant differences between the SC and the IM groups in patients diagnosis or sex.
A total of 38 patients had serology performed after the first vaccine dose, determining seroconversion rates of 83.3% and 90.0% for the SC and the IM group, respectively, a nonsignificant difference. After the second vaccine dose, the seroconversion rate for the SC group was 97.5% and for the IM group was 97.4%, also a nonsignificant difference.
At a median of 9 years after a second vaccine dose, antibody titers for the SC group were slightly greater than the IM group (7.6 vs. 7.4), but this was also not a significant difference. There were no serious adverse events in both groups, according to Dr. Nakasone and colleagues. And although twice as many patients of the IM group required clotting factor concentrates for adverse events, compared with the SC group (15.8% vs. 7.5%), the difference was not significant.
“Hepatitis A vaccine administered subcutaneously is as immunogenic, long-term protective, and even safer as the intramuscular route for both children and adults not only with hemophilia, but also with other bleeding disorders,” the researchers concluded.
The authors declared that they had no disclosures.
SOURCE: Nakasone M et al. Vaccine 2020;38:4162-6.
FROM VACCINE
Key clinical point: Subcutaneous hepatitis A vaccination is as immunogenic, but appeared safer than intramuscular injections for bleeding disorder patients.
Major finding: A total of 38 patients assessed after first vaccine dose showed seroconversion rates of 83.3% and 90.0% for the subcutaneous versus the intramuscular group, respectively.
Study details: A comparison of hepatitis A vaccination administered subcutaneously or intramuscularly in 78 children and adults with hemophilia and other bleeding disorders.
Disclosures: The authors declared that they had no disclosures.
Source: Nakasone M et al. Vaccine. 2020;38:4162-6.
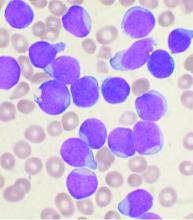
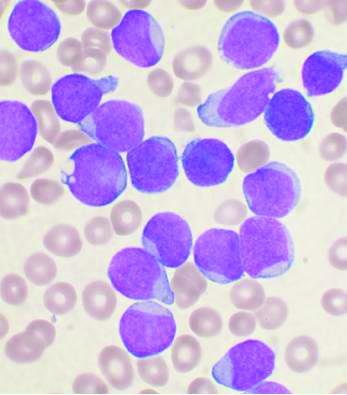
Added rituximab was effective in children and adolescents with high-risk B-cell NHL
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Adding rituximab to chemotherapy was effective in children and adolescents with high-risk, high-grade, mature B-cell non-Hodgkin lymphoma.
Major finding: Higher 3-year overall survival was observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group).
Study details: Analysis of 328 patients who underwent randomization to standard chemotherapy vs. chemo plus rituximab (164 patients per group).
Disclosures: The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
Source: Minard-Colin V et al. N Engl J Med. 2020; 382:2207-19.
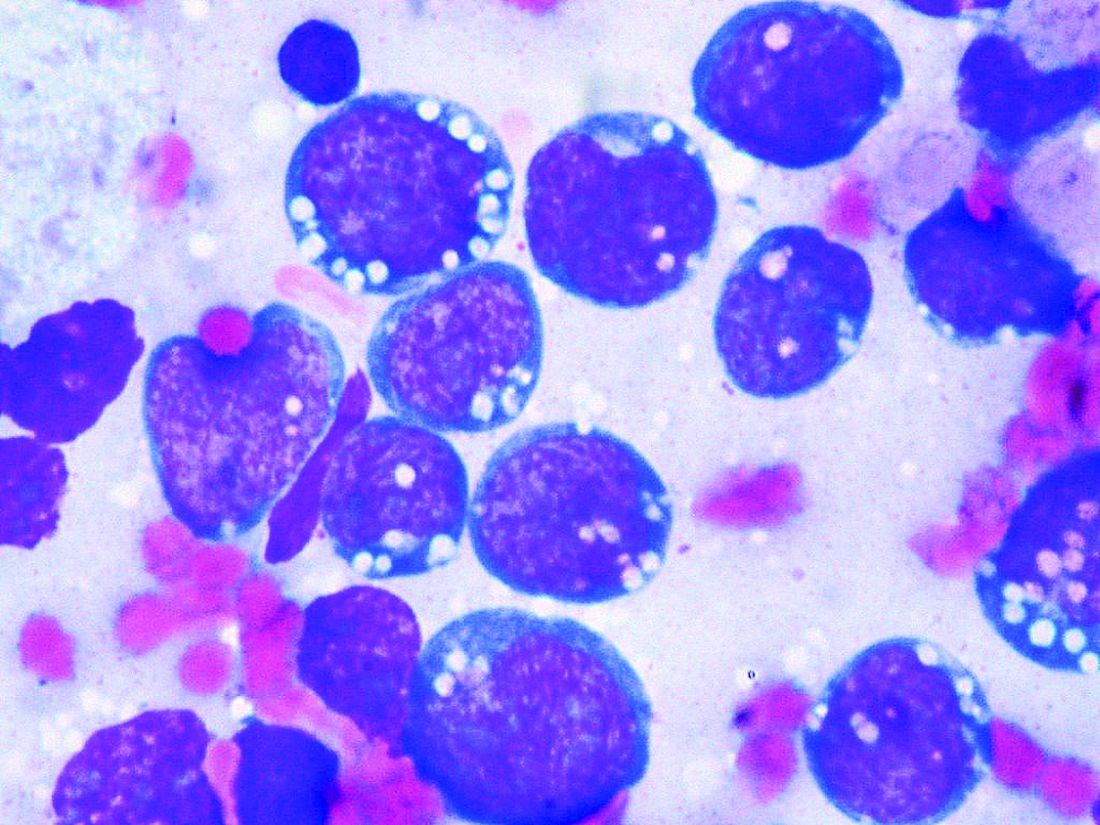
Acute lymphoblastic leukemia can be successfully treated in the frail elderly
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
A treatment schedule of very attenuated chemotherapy using standard drugs is feasible and effective in frail and elderly patients with acute lymphoblastic leukemia (ALL), according to a prospective study published in Clinical Lymphoma, Myeloma & Leukemia.
The study comprised 67 previously untreated patients with B- or T-lineage Philadelphia chromosome–negative ALL from 30 Spanish hospitals who were enrolled in the prospective, multicenter ALL-07FRAIL trial (NCT01358201) from the Spanish PETHEMA (Programa Español de Tratamientos en Hematologia) group from January 2008 to October 2019.
The median patient age in this analysis was 67 years and 51 patients (76%) were older than 70 years. The median Charlson Comorbidity Index was 5, with the main comorbidities being cardiovascular (47 patients), other neoplasia (24), diabetes (17), and very advanced age (>80 years; 12).
The attenuated treatment regimen consisted of a prephase with dexamethasone and intrathecal therapy with methotrexate was given for a maximum of 1 week. Then weekly induction therapy consisted of weekly vincristine (capped at 1 mg/week) and daily dexamethasone with a progressively decreasing dose along 4 weeks, as well as two additional doses of intrathecal methotrexate.
Those patients who achieved complete remission received maintenance therapy with mercaptopurine and methotrexate to complete 2 years of treatment. In addition, reinduction pulses with vincristine and dexamethasone were given every 3 months during the first year, according to Josep-Maria Ribera, MD, of the Universitat Autònoma de Barcelona, Badalona, Spain and colleagues on behalf of the PETHEMA group of the Spanish Society of Hematology.
The complete remission rate was 54% (36/67 patients). The median disease-free survival and overall survival were 6.9 months and 7.6 months, respectively.
Of the 32 patients who initiated maintenance therapy, 5 patients died of infection (2), hemorrhage (2), and acute cognitive impairment (1), and 23 relapsed, with a cumulative incidence of relapse of 74% and a median time to relapse of 12.3 months.
The most frequent toxic events reported were hematologic (neutropenia 77% and thrombocytopenia 54%, of grade III-IV in all cases) followed by infections, metabolic (mainly hyperglycemia), and neurologic, according to the researchers.
“The lack of similar trials specifically directed to this frail population is one of the major strengths of this study, and we consider that this minimal chemotherapy approach could be used as a backbone for addition of immuno/targeted therapy in this subset of infirm patients,” the researchers concluded.
The study was supported by the CERCA Program/Generalitat de Catalunya and the Josep Carreras Leukemia Research Institute. The authors reported having no disclosures.
SOURCE: Ribera J-M et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 5. doi: 10.1016/j.clml.2020.03.011.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA