User login
Osteoporosis: A quick update
Researchers estimate that approximately 10.2 million Americans have osteoporosis, and an additional 43 million have low bone density.1 Equally stark are the ramifications of these numbers. About one out of every 2 Caucasian women will experience an osteoporosis-related fracture at some point in their lifetime, as will approximately one in 5 men.2 Although African American women tend to have a higher bone mineral density (BMD) than white women throughout their lives, those who have osteoporosis have the same elevated risk for fractures as Caucasians.
Osteoporotic fractures are associated with increased risk of disability, mortality, and nursing home placement. Given the aging population, researchers expect annual direct costs from osteoporosis to reach $25.3 billion by 2025.3
Family physicians (FPs) can have a meaningful impact on the extent to which this condition affects the population. To that end, we’ve put together a brief summary of the screening recommendations to keep in mind and a comparison of the different agents used to treat and prevent osteoporosis. The reference tables throughout will put these details at your fingertips.
Screening recommendations vary, Dx doesn’t require BMD testing
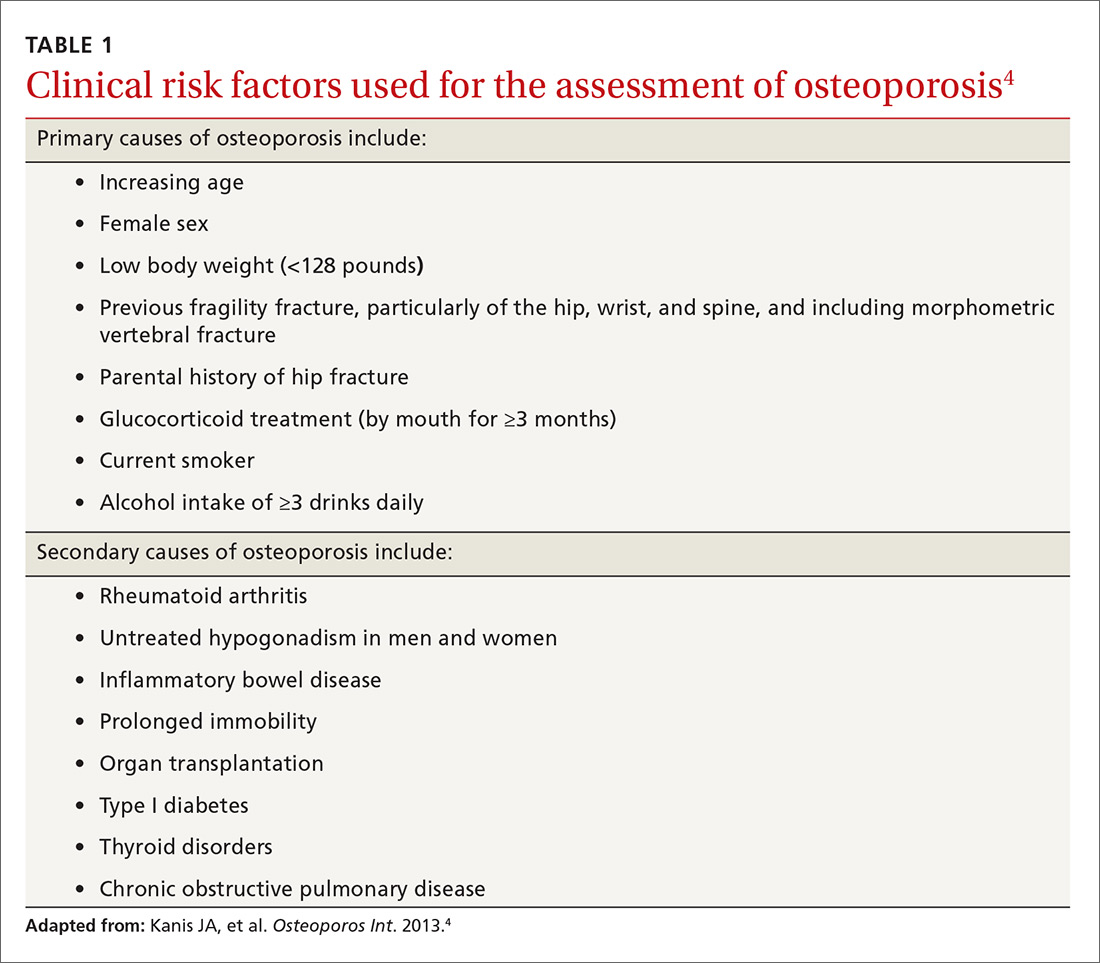
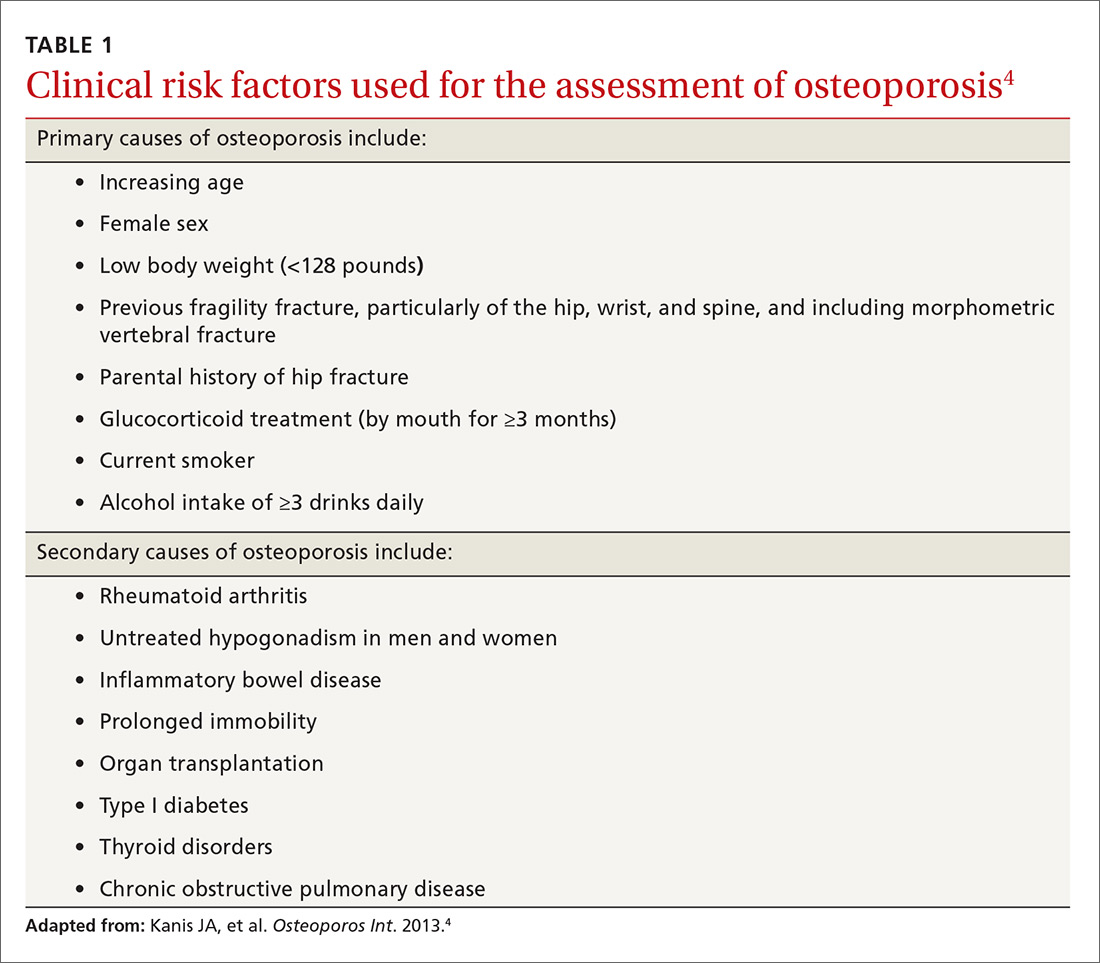
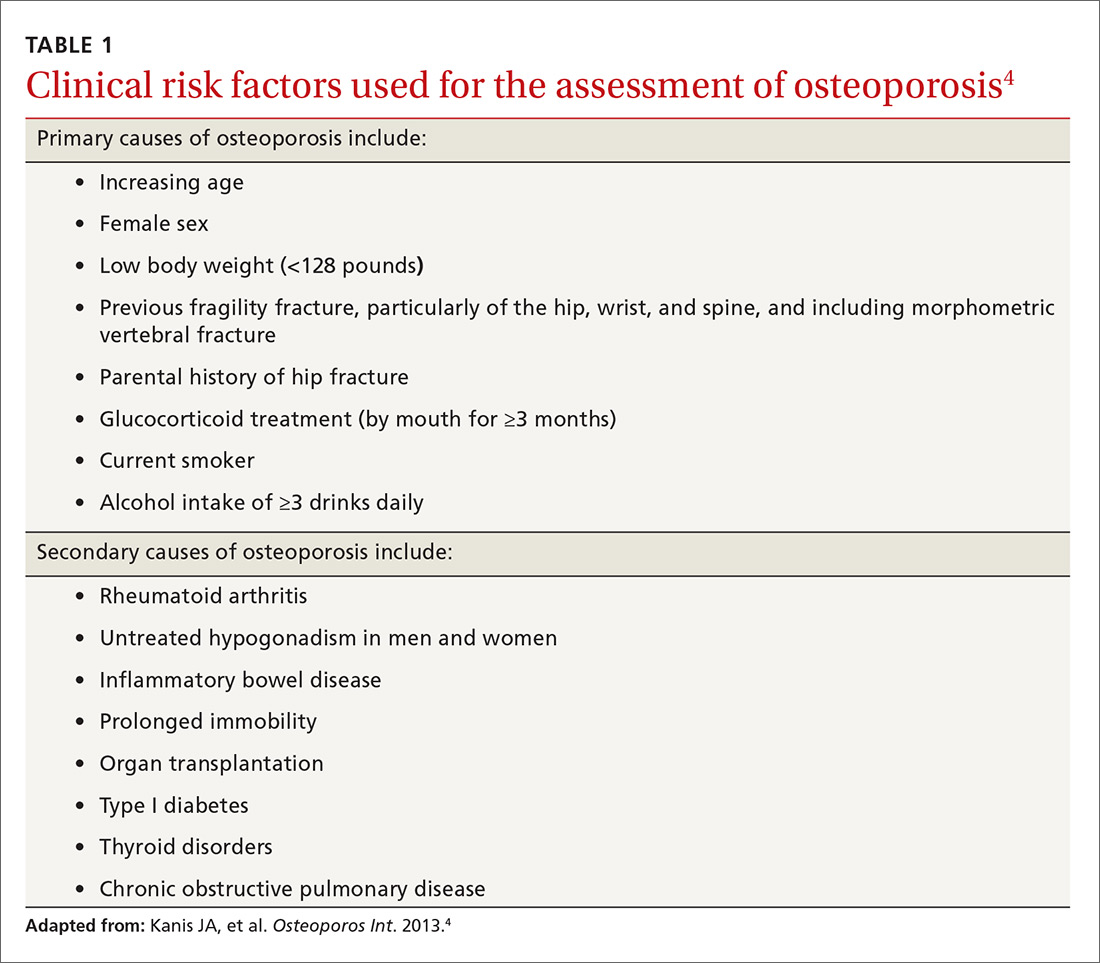
Guidelines for screening for osteoporosis vary considerably by professional organization. For example, the US Preventive Services Task Force (USPSTF) recommends screening all women ≥65 years, and younger women whose fracture risk is the same, or greater than, that of a 65-year-old white woman who has no additional risk factors (TABLE 14).5 In addition, the USPSTF concludes that the current evidence is insufficient to recommend routine screening for osteoporosis in men.5
The National Osteoporosis Foundation (NOF) recommends that BMD testing be performed in all women ≥65 years and in men ≥70 years.6 In terms of frequency, NOF recommends BMD testing one to 2 years after initiating therapy to reduce fracture risk and every 2 years thereafter. The American College of Obstetricians and Gynecologists recommends BMD screening for women no more than every 2 years starting at age 65 years.7 It also recommends selective screening in women younger than 65 years of age if they are postmenopausal and have other risk factors for osteoporosis.7
The most recent guideline regarding osteoporosis was published in May 2017 by the American College of Physicians (ACP) and endorsed by the American Academy of Family Physicians.8 But the guideline focuses on treatment rather than screening.
Although guidelines vary by society, most experts agree with BMD assessment in all women ≥65 years and postmenopausal women <65 years if one or more of the risk factors identified in TABLE 14 are present.
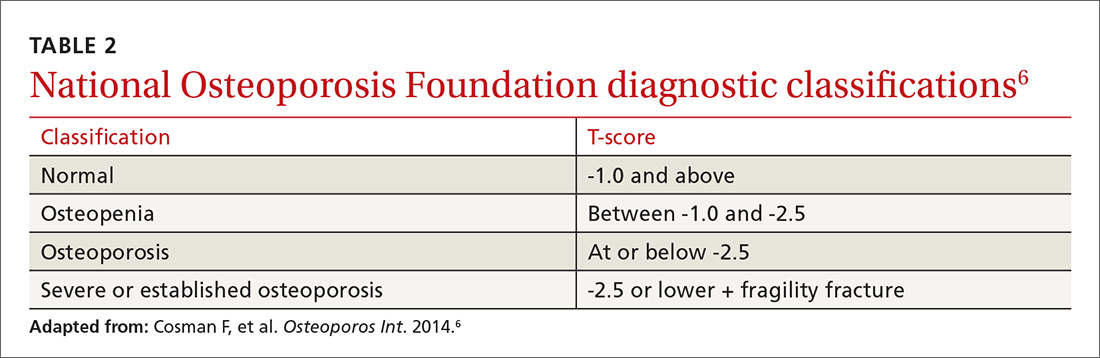
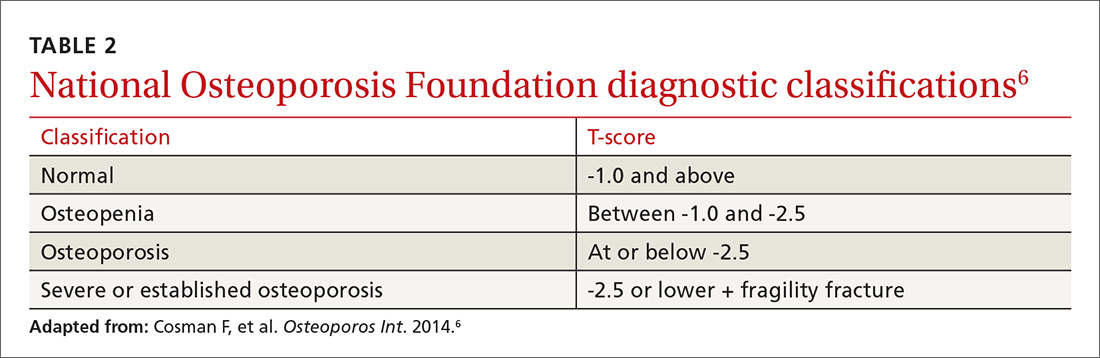
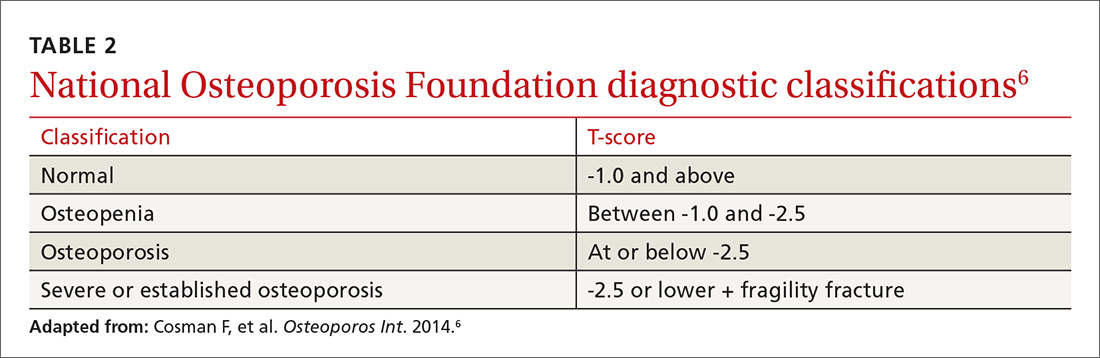
Diagnosis. Osteoporosis can be diagnosed using dual energy x-ray absorptiometry (DXA) and T-score (TABLE 26),9 but BMD testing is not always necessary to establish the diagnosis. For example, osteoporosis can be diagnosed clinically in both men and women who have sustained a hip fracture (with or without BMD testing). Osteoporosis may also be diagnosed in patients with osteopenia (determined by DXA and T-score) who have had a vertebral, proximal humeral, or pelvic fracture. Generally speaking, a detailed history and physical together with BMD assessment, vertebral imaging to diagnose vertebral fractures, and, when appropriate, the World Health Organization’s 10-year estimated fracture probability, are all utilized to establish patients’ fracture risk.6,10
Treatment: Which agents and for how long?
Once a patient is diagnosed with osteoporosis, answering the following questions will help with selection of the best therapy for the patient:
- Where on the body is BMD the lowest (vertebral, nonvertebral, or hip) and, consequently, at highest risk for a fracture?
- Does the patient have any conditions that would interfere with therapy (difficulty swallowing, esophageal/gastrointestinal irritation)? This is important, as certain agents are associated with severe esophagitis.
- Does the patient have any issues that would prevent adherence? Adherence may improve with therapy that is administered less frequently (weekly, monthly, once every 3 months, or annually).
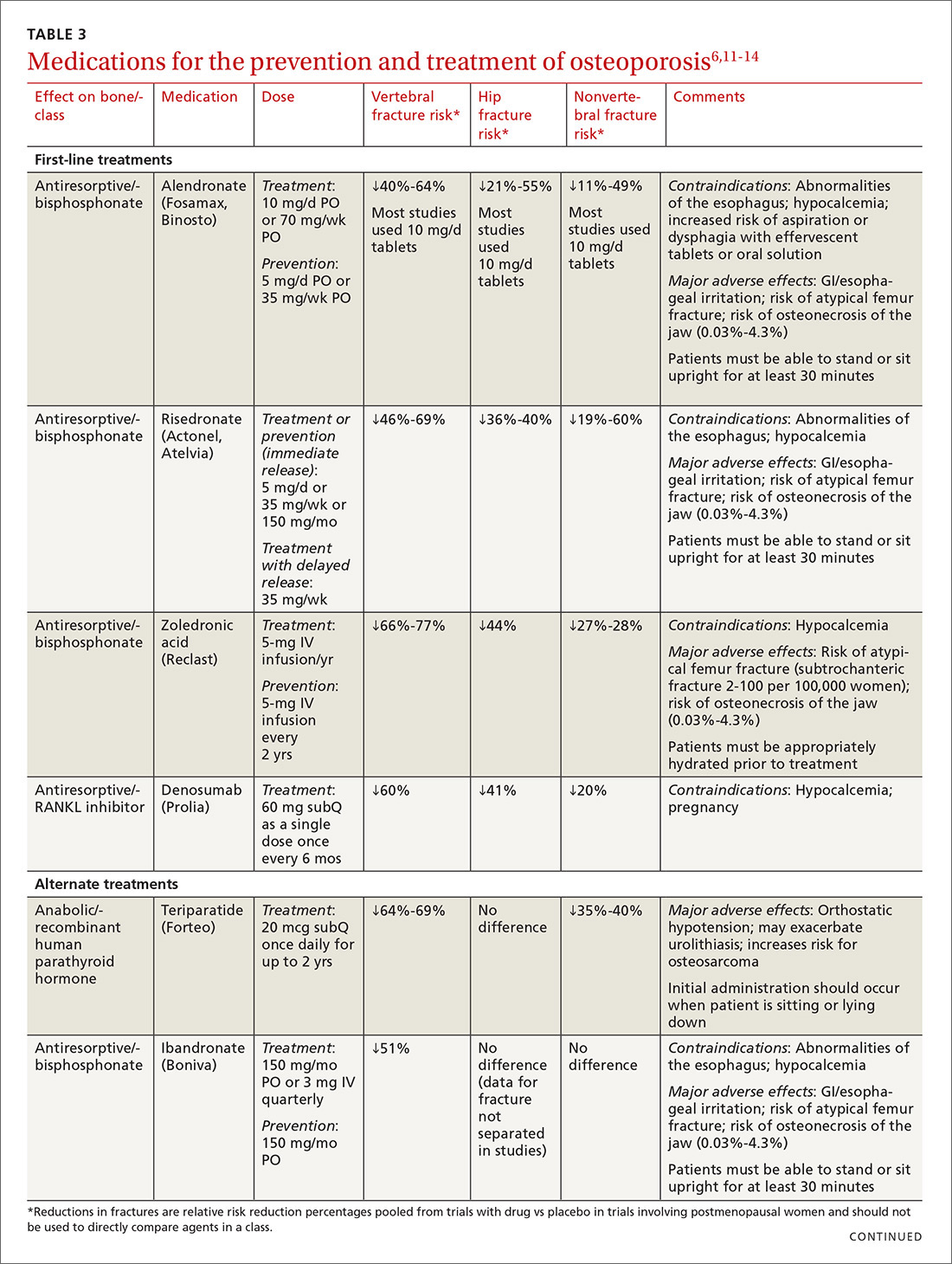
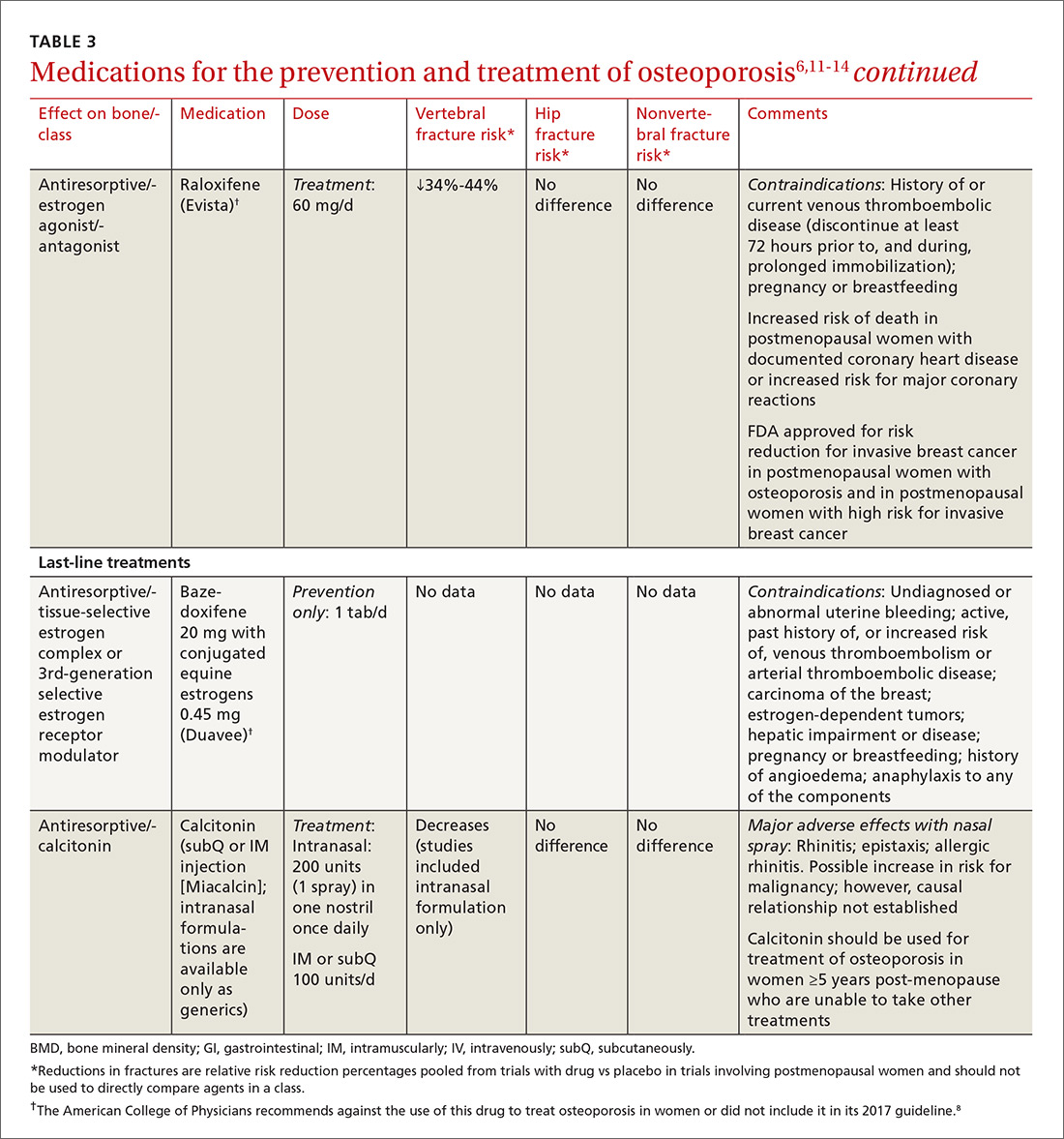
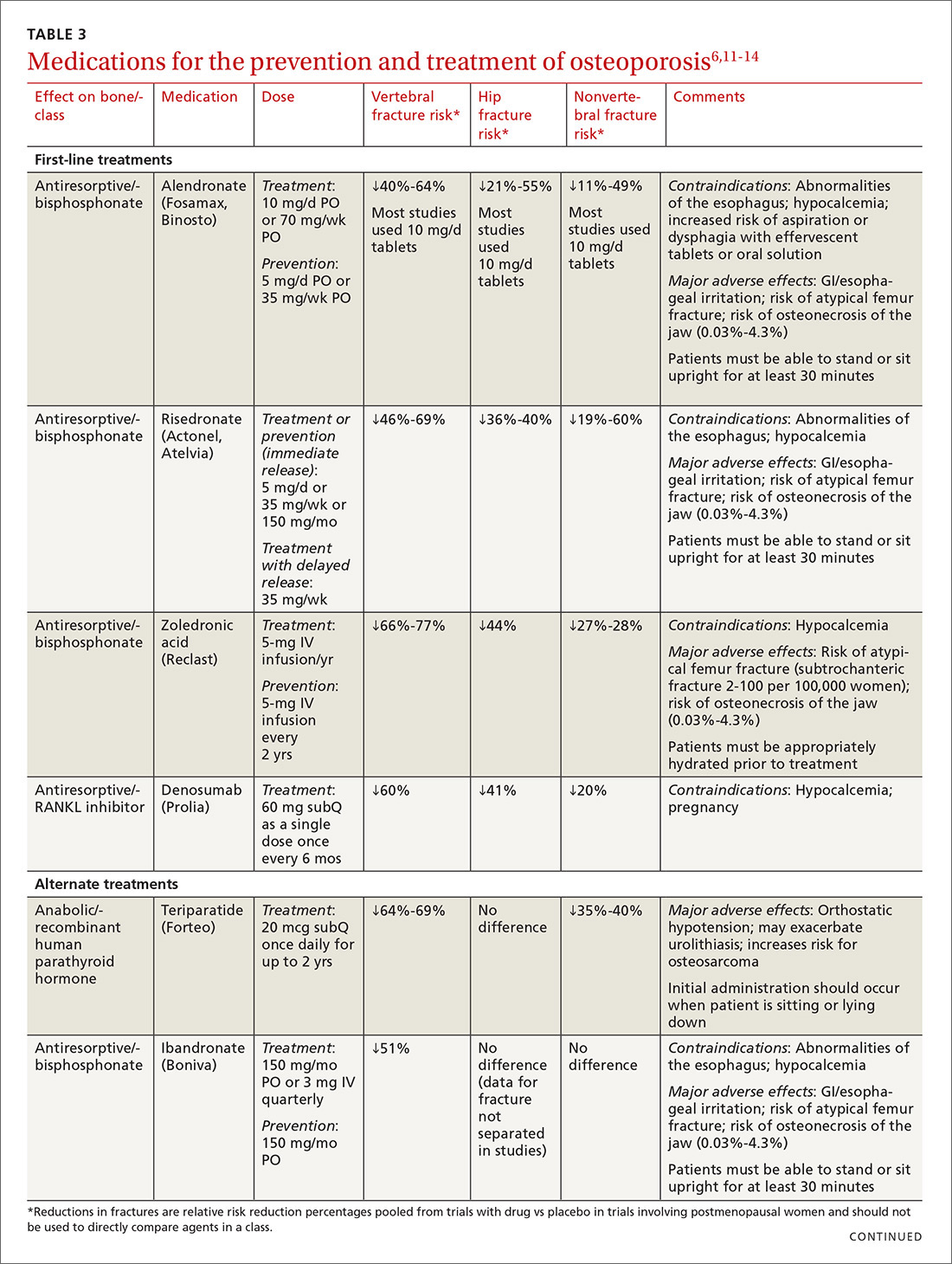
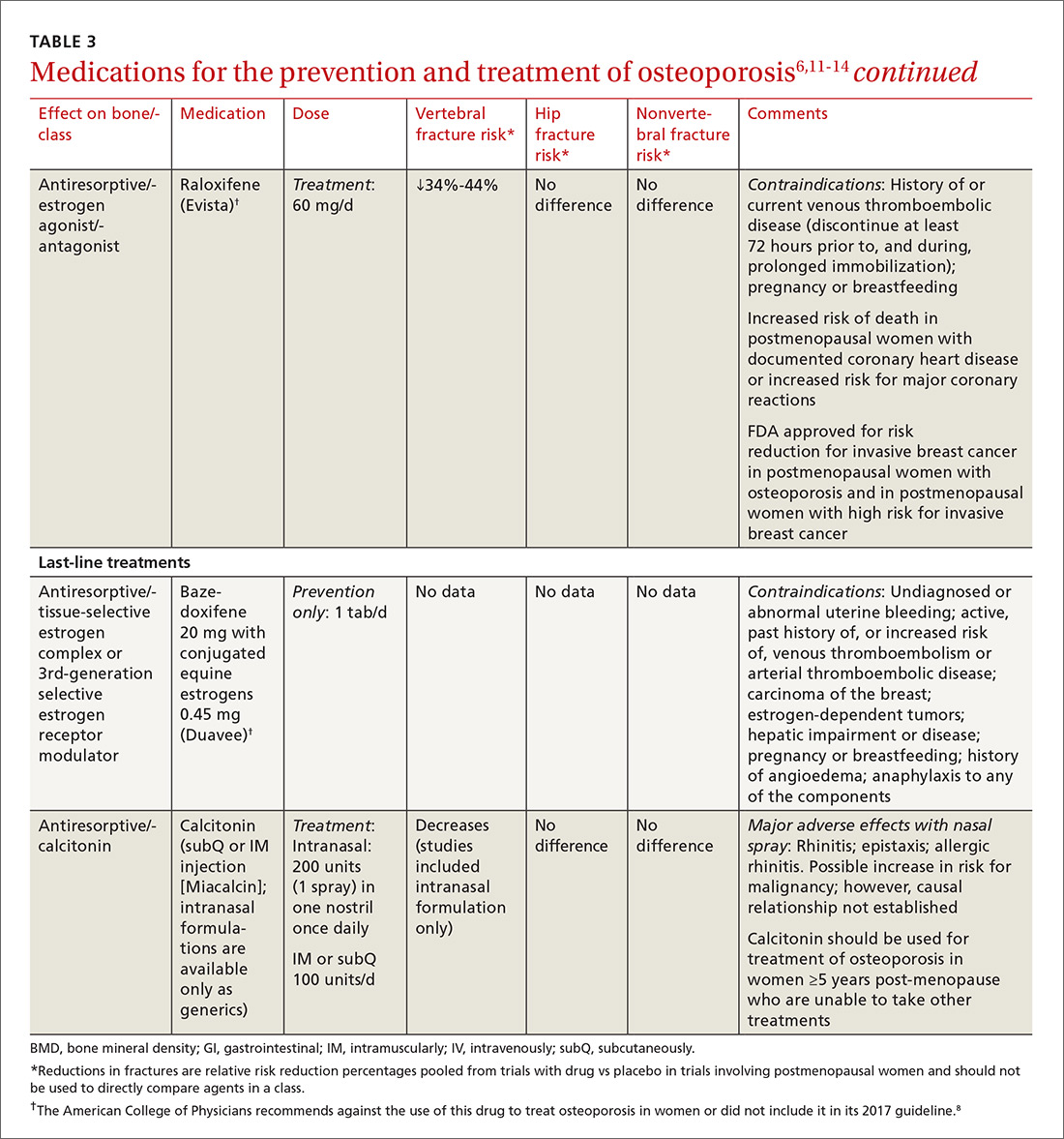
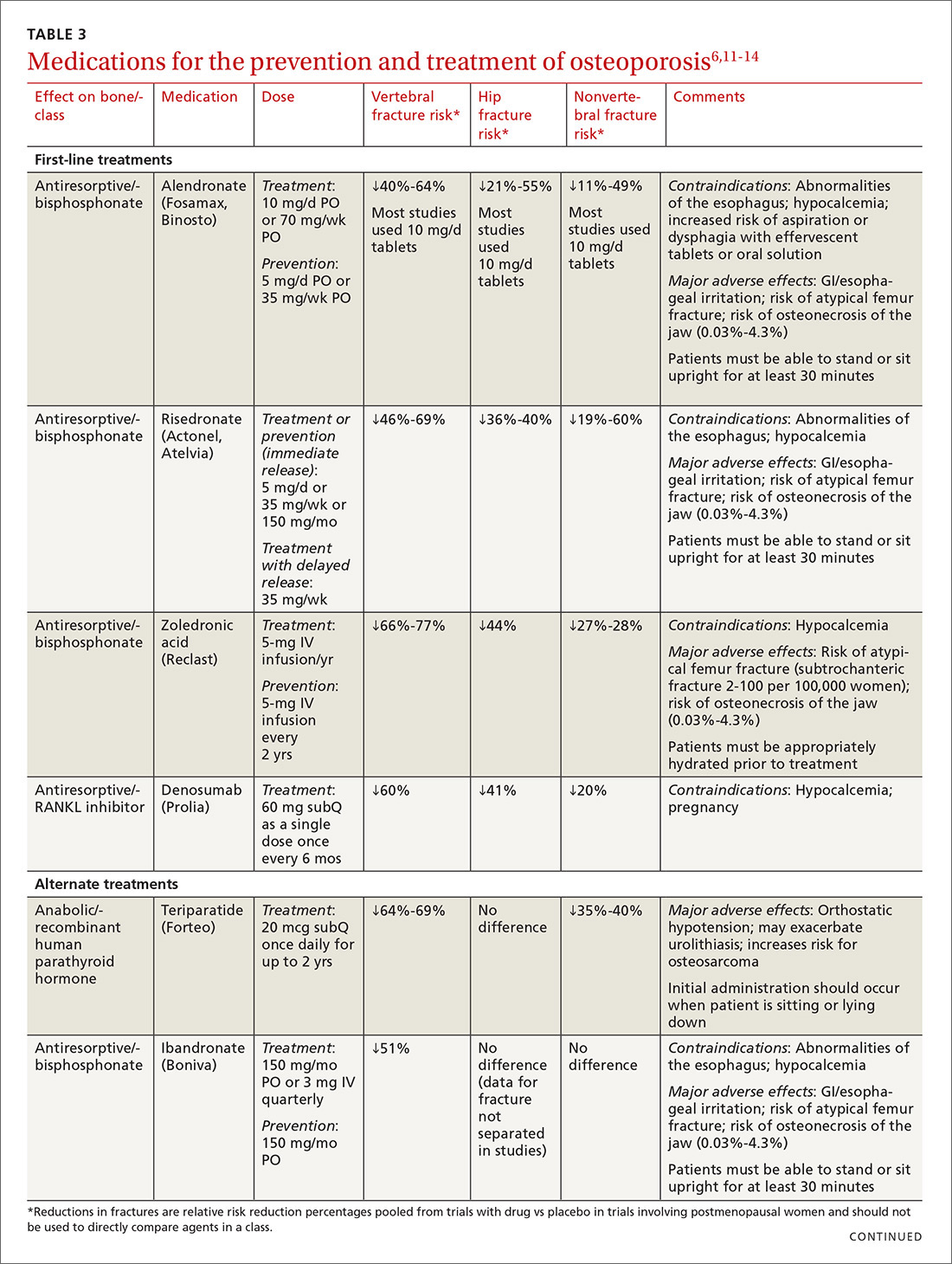
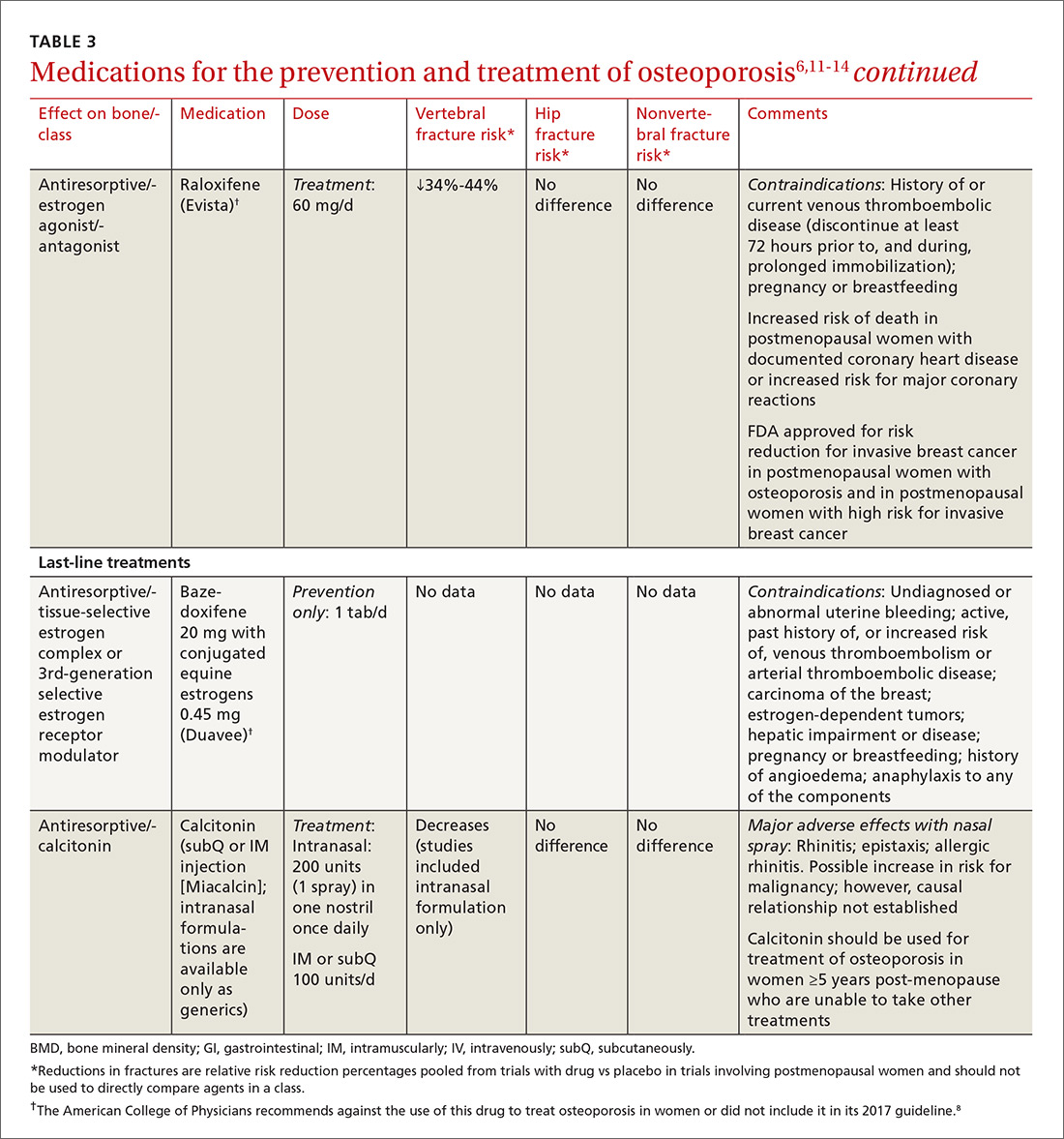
TABLE 36,11-14 lists the prescription medications used to treat and prevent osteoporosis, their effect on the risk of vertebral, hip, and nonvertebral fractures, and contraindications/major adverse effects. First-line therapies are recommended based on clinical trials comparing the medication to placebo and evaluating their effectiveness in lowering the risk of vertebral, hip, and nonvertebral fractures.15 Given the absence of studies comparing these drugs to one another, TABLE 36,11-14 should not be used to make direct comparisons.
A new monoclonal antibody, romosozumab, has shown statistically significant decreases in the risk of new vertebral and nonvertebral fractures compared to alendronate after 12 months of use.16 However, there was a statistically significant higher number of patients who had a cardiac ischemic event or revascularization while taking romosozumab compared with those taking alendronate in the one-year double-blind period of the study.16 As of press time, the US Food and Drug Administration has not approved romosozumab.
Duration of treatment should be individualized based on specific patient factors, the pharmacologic agent, and, of course, adverse effects. However, no pharmacologic agent should be used indefinitely.6 In its clinical practice guidelines, the ACP recommends that patients be treated for 5 years with an appropriate pharmacologic therapy.8 The American Society for Bone and Mineral Research (ASBMR) Task Force recommends a review of therapy after 3 years with an intravenous bisphosphonate (BP; strength of recommendation [SOR]=C).17
A review of 2 recent long-term trials analyzing the effects of BPs offers some additional guidance regarding duration of therapy in Caucasian postmenopausal women.18 In one study, women who received 10 years of therapy with alendronate reported fewer vertebral fractures than those who were switched to placebo after 5 years of treatment.19
In the second trial, which studied zoledronic acid, there were fewer morphometric vertebral fractures for those participants given annual injections for 6 years vs 3 years.20 This trial found a significant transient increase in serum creatinine >0.5 mg/dL in the zoledronic acid treatment group.
These findings have prompted some experts in the field of osteoporosis to call for physicians to consider longer therapy with a BP (10 years with oral therapy or 6 years with intravenous therapy) in high-risk postmenopausal women (older women, those with a low hip T-score or high fracture risk score, those with a previous major osteoporotic fracture, and those who experienced fracture while on therapy) (SOR=B).18
Two rare adverse effects to keep in mind
The incidence of atypical femoral fracture, although rare (2-100 per 100,000 women), increases with duration of BP use. As a result, a drug holiday of 2 to 3 years should be considered for women with a low risk for fracture after 3 to 5 years of BP therapy (SOR=C).18
Osteonecrosis of the jaw (ONJ), also known as antiresorptive-associated osteonecrosis of the jaw, is a rare adverse effect of BPs that is associated with higher drug potency, higher cumulative dose, and parenteral route of administration, as well as other risk factors.17,21 The American Association of Maxillofacial Surgeons (AAOMS) states that the risk of developing ONJ increases with use of oral BPs for more than 4 years;22 however, the Task Force of the ASBMR states that the evidence to support this is of poor quality.18 No recommendations on duration of therapy based on risk for ONJ have been made; however, AAOMS recommends discontinuation of oral BPs for a period of 2 months prior to, and 3 months following (or until osseous healing has occurred), elective invasive dental surgery for patients who have been taking an oral BP ≥4 years (SOR=C).22
If a long-term drug holiday is selected, patients should be reassessed in 2 years. Shorter duration of follow-up is warranted for patients taking denosumab, teriparatide, or raloxifene, since bone loss will resume once therapy is discontinued.18
Because the benefits of BPs (in terms of reducing the risk of vertebral fracture) are significantly greater than the risks of an atypical fracture or ONJ, therapy should be started in appropriate patients, but duration of therapy should be monitored closely.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CORRESPONDENCE
Lovedhi Aggarwal, MD, 95-390 Kuahelani Avenue, Mililani, HI 96789; [email protected].
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520-2526.
2. Office of the Surgeon General (US). Bone health and osteoporosis: a report of the Surgeon General. Rockville (MD); 2004.
3. Dempster DW. Osteoporosis and the burden of osteoporosis-related fractures. Am J Manag Care. 2011;17 Suppl 6:S164-S169.
4. Kanis JA, McCloskey EV, Johansson H, et al, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23-57.
5. Screening for Osteoporosis: U.S. Preventive Services Task Force Final Recommendation Statement. Ann Intern Med. 2011;154:356-364.
6. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis (National Osteoporosis Foundation). Osteoporos Int. 2014;25:2359-2381.
7. Committee on Practice Bulletins-Gynecology, The American College of Obstetricians and Gynecologists. ACOG Practice Bulletin N. 129. Osteoporosis. Obstet Gynecol. 2012;120:718-734.
8. Qaseem A, Forciea MA, McLean RM, et al. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166:818-839.
9. Jeremiah MP, Unwin BK, Greenawald MH, et al. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92:261-268.
10. Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395-2411.
11. Lexicomp Online. Clinical Drug Information. Available at: https://online.lexi.com/lco/action/home. Accessed June 30, 2016.
12. Crandall CJ, Newberry SJ, Diamant A, et al. Treatment to Prevent Fractures in Men and Women with Low Bone Density and Osteoporosis: Update of a 2007 Report. Comparative Effectiveness Review No. 53. Rockville, MD: Agency for Healthcare Research and Quality; March 2012. Available at: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/osteoporosis-bone-fracture_research.pdf. Accessed January 10, 2018.
13. O’Connell MB, Borchert JS. Chapter 73. Osteoporosis and other metabolic bone diseases. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy: a pathophysiologic approach. 9th ed. McGraw-Hill Education; 2014.
14. Crandall CJ, Newberry SJ, Diamant A, et al. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014;161:711-723.
15. Watts NB, Bilezikian JP, Camacho PM, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16(Supp 3):1-37. Available at: https://www.aace.com/files/osteo-guidelines-2010.pdf. Accessed June 17, 2016.
16. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427.
17. Adler RA, El-Hajj Fuleihan G, Bauer DC, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: Report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31:16-35.
18. Adler RA. Duration of anti-resorptive therapy for osteoporosis. Endocrine. 2015;51:222-224.
19. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927-2938.
20. Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27:243-254.
21. Denosumab (Xgeva, Prolia); intravenous bisphosphonates: osteonecrosis of the jaw—further measures to minimise risk. 2015. Available at: https://www.gov.uk/drug-safety-update/denosumab-xgeva-prolia-intravenous-bisphosphonates-osteonecrosis-of-the-jaw-further-measures-to-minimise-risk. Accessed June 30, 2016.
22. Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938-1956.
Researchers estimate that approximately 10.2 million Americans have osteoporosis, and an additional 43 million have low bone density.1 Equally stark are the ramifications of these numbers. About one out of every 2 Caucasian women will experience an osteoporosis-related fracture at some point in their lifetime, as will approximately one in 5 men.2 Although African American women tend to have a higher bone mineral density (BMD) than white women throughout their lives, those who have osteoporosis have the same elevated risk for fractures as Caucasians.
Osteoporotic fractures are associated with increased risk of disability, mortality, and nursing home placement. Given the aging population, researchers expect annual direct costs from osteoporosis to reach $25.3 billion by 2025.3
Family physicians (FPs) can have a meaningful impact on the extent to which this condition affects the population. To that end, we’ve put together a brief summary of the screening recommendations to keep in mind and a comparison of the different agents used to treat and prevent osteoporosis. The reference tables throughout will put these details at your fingertips.
Screening recommendations vary, Dx doesn’t require BMD testing
Guidelines for screening for osteoporosis vary considerably by professional organization. For example, the US Preventive Services Task Force (USPSTF) recommends screening all women ≥65 years, and younger women whose fracture risk is the same, or greater than, that of a 65-year-old white woman who has no additional risk factors (TABLE 14).5 In addition, the USPSTF concludes that the current evidence is insufficient to recommend routine screening for osteoporosis in men.5
The National Osteoporosis Foundation (NOF) recommends that BMD testing be performed in all women ≥65 years and in men ≥70 years.6 In terms of frequency, NOF recommends BMD testing one to 2 years after initiating therapy to reduce fracture risk and every 2 years thereafter. The American College of Obstetricians and Gynecologists recommends BMD screening for women no more than every 2 years starting at age 65 years.7 It also recommends selective screening in women younger than 65 years of age if they are postmenopausal and have other risk factors for osteoporosis.7
The most recent guideline regarding osteoporosis was published in May 2017 by the American College of Physicians (ACP) and endorsed by the American Academy of Family Physicians.8 But the guideline focuses on treatment rather than screening.
Although guidelines vary by society, most experts agree with BMD assessment in all women ≥65 years and postmenopausal women <65 years if one or more of the risk factors identified in TABLE 14 are present.
Diagnosis. Osteoporosis can be diagnosed using dual energy x-ray absorptiometry (DXA) and T-score (TABLE 26),9 but BMD testing is not always necessary to establish the diagnosis. For example, osteoporosis can be diagnosed clinically in both men and women who have sustained a hip fracture (with or without BMD testing). Osteoporosis may also be diagnosed in patients with osteopenia (determined by DXA and T-score) who have had a vertebral, proximal humeral, or pelvic fracture. Generally speaking, a detailed history and physical together with BMD assessment, vertebral imaging to diagnose vertebral fractures, and, when appropriate, the World Health Organization’s 10-year estimated fracture probability, are all utilized to establish patients’ fracture risk.6,10
Treatment: Which agents and for how long?
Once a patient is diagnosed with osteoporosis, answering the following questions will help with selection of the best therapy for the patient:
- Where on the body is BMD the lowest (vertebral, nonvertebral, or hip) and, consequently, at highest risk for a fracture?
- Does the patient have any conditions that would interfere with therapy (difficulty swallowing, esophageal/gastrointestinal irritation)? This is important, as certain agents are associated with severe esophagitis.
- Does the patient have any issues that would prevent adherence? Adherence may improve with therapy that is administered less frequently (weekly, monthly, once every 3 months, or annually).
TABLE 36,11-14 lists the prescription medications used to treat and prevent osteoporosis, their effect on the risk of vertebral, hip, and nonvertebral fractures, and contraindications/major adverse effects. First-line therapies are recommended based on clinical trials comparing the medication to placebo and evaluating their effectiveness in lowering the risk of vertebral, hip, and nonvertebral fractures.15 Given the absence of studies comparing these drugs to one another, TABLE 36,11-14 should not be used to make direct comparisons.
A new monoclonal antibody, romosozumab, has shown statistically significant decreases in the risk of new vertebral and nonvertebral fractures compared to alendronate after 12 months of use.16 However, there was a statistically significant higher number of patients who had a cardiac ischemic event or revascularization while taking romosozumab compared with those taking alendronate in the one-year double-blind period of the study.16 As of press time, the US Food and Drug Administration has not approved romosozumab.
Duration of treatment should be individualized based on specific patient factors, the pharmacologic agent, and, of course, adverse effects. However, no pharmacologic agent should be used indefinitely.6 In its clinical practice guidelines, the ACP recommends that patients be treated for 5 years with an appropriate pharmacologic therapy.8 The American Society for Bone and Mineral Research (ASBMR) Task Force recommends a review of therapy after 3 years with an intravenous bisphosphonate (BP; strength of recommendation [SOR]=C).17
A review of 2 recent long-term trials analyzing the effects of BPs offers some additional guidance regarding duration of therapy in Caucasian postmenopausal women.18 In one study, women who received 10 years of therapy with alendronate reported fewer vertebral fractures than those who were switched to placebo after 5 years of treatment.19
In the second trial, which studied zoledronic acid, there were fewer morphometric vertebral fractures for those participants given annual injections for 6 years vs 3 years.20 This trial found a significant transient increase in serum creatinine >0.5 mg/dL in the zoledronic acid treatment group.
These findings have prompted some experts in the field of osteoporosis to call for physicians to consider longer therapy with a BP (10 years with oral therapy or 6 years with intravenous therapy) in high-risk postmenopausal women (older women, those with a low hip T-score or high fracture risk score, those with a previous major osteoporotic fracture, and those who experienced fracture while on therapy) (SOR=B).18
Two rare adverse effects to keep in mind
The incidence of atypical femoral fracture, although rare (2-100 per 100,000 women), increases with duration of BP use. As a result, a drug holiday of 2 to 3 years should be considered for women with a low risk for fracture after 3 to 5 years of BP therapy (SOR=C).18
Osteonecrosis of the jaw (ONJ), also known as antiresorptive-associated osteonecrosis of the jaw, is a rare adverse effect of BPs that is associated with higher drug potency, higher cumulative dose, and parenteral route of administration, as well as other risk factors.17,21 The American Association of Maxillofacial Surgeons (AAOMS) states that the risk of developing ONJ increases with use of oral BPs for more than 4 years;22 however, the Task Force of the ASBMR states that the evidence to support this is of poor quality.18 No recommendations on duration of therapy based on risk for ONJ have been made; however, AAOMS recommends discontinuation of oral BPs for a period of 2 months prior to, and 3 months following (or until osseous healing has occurred), elective invasive dental surgery for patients who have been taking an oral BP ≥4 years (SOR=C).22
If a long-term drug holiday is selected, patients should be reassessed in 2 years. Shorter duration of follow-up is warranted for patients taking denosumab, teriparatide, or raloxifene, since bone loss will resume once therapy is discontinued.18
Because the benefits of BPs (in terms of reducing the risk of vertebral fracture) are significantly greater than the risks of an atypical fracture or ONJ, therapy should be started in appropriate patients, but duration of therapy should be monitored closely.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CORRESPONDENCE
Lovedhi Aggarwal, MD, 95-390 Kuahelani Avenue, Mililani, HI 96789; [email protected].
Researchers estimate that approximately 10.2 million Americans have osteoporosis, and an additional 43 million have low bone density.1 Equally stark are the ramifications of these numbers. About one out of every 2 Caucasian women will experience an osteoporosis-related fracture at some point in their lifetime, as will approximately one in 5 men.2 Although African American women tend to have a higher bone mineral density (BMD) than white women throughout their lives, those who have osteoporosis have the same elevated risk for fractures as Caucasians.
Osteoporotic fractures are associated with increased risk of disability, mortality, and nursing home placement. Given the aging population, researchers expect annual direct costs from osteoporosis to reach $25.3 billion by 2025.3
Family physicians (FPs) can have a meaningful impact on the extent to which this condition affects the population. To that end, we’ve put together a brief summary of the screening recommendations to keep in mind and a comparison of the different agents used to treat and prevent osteoporosis. The reference tables throughout will put these details at your fingertips.
Screening recommendations vary, Dx doesn’t require BMD testing
Guidelines for screening for osteoporosis vary considerably by professional organization. For example, the US Preventive Services Task Force (USPSTF) recommends screening all women ≥65 years, and younger women whose fracture risk is the same, or greater than, that of a 65-year-old white woman who has no additional risk factors (TABLE 14).5 In addition, the USPSTF concludes that the current evidence is insufficient to recommend routine screening for osteoporosis in men.5
The National Osteoporosis Foundation (NOF) recommends that BMD testing be performed in all women ≥65 years and in men ≥70 years.6 In terms of frequency, NOF recommends BMD testing one to 2 years after initiating therapy to reduce fracture risk and every 2 years thereafter. The American College of Obstetricians and Gynecologists recommends BMD screening for women no more than every 2 years starting at age 65 years.7 It also recommends selective screening in women younger than 65 years of age if they are postmenopausal and have other risk factors for osteoporosis.7
The most recent guideline regarding osteoporosis was published in May 2017 by the American College of Physicians (ACP) and endorsed by the American Academy of Family Physicians.8 But the guideline focuses on treatment rather than screening.
Although guidelines vary by society, most experts agree with BMD assessment in all women ≥65 years and postmenopausal women <65 years if one or more of the risk factors identified in TABLE 14 are present.
Diagnosis. Osteoporosis can be diagnosed using dual energy x-ray absorptiometry (DXA) and T-score (TABLE 26),9 but BMD testing is not always necessary to establish the diagnosis. For example, osteoporosis can be diagnosed clinically in both men and women who have sustained a hip fracture (with or without BMD testing). Osteoporosis may also be diagnosed in patients with osteopenia (determined by DXA and T-score) who have had a vertebral, proximal humeral, or pelvic fracture. Generally speaking, a detailed history and physical together with BMD assessment, vertebral imaging to diagnose vertebral fractures, and, when appropriate, the World Health Organization’s 10-year estimated fracture probability, are all utilized to establish patients’ fracture risk.6,10
Treatment: Which agents and for how long?
Once a patient is diagnosed with osteoporosis, answering the following questions will help with selection of the best therapy for the patient:
- Where on the body is BMD the lowest (vertebral, nonvertebral, or hip) and, consequently, at highest risk for a fracture?
- Does the patient have any conditions that would interfere with therapy (difficulty swallowing, esophageal/gastrointestinal irritation)? This is important, as certain agents are associated with severe esophagitis.
- Does the patient have any issues that would prevent adherence? Adherence may improve with therapy that is administered less frequently (weekly, monthly, once every 3 months, or annually).
TABLE 36,11-14 lists the prescription medications used to treat and prevent osteoporosis, their effect on the risk of vertebral, hip, and nonvertebral fractures, and contraindications/major adverse effects. First-line therapies are recommended based on clinical trials comparing the medication to placebo and evaluating their effectiveness in lowering the risk of vertebral, hip, and nonvertebral fractures.15 Given the absence of studies comparing these drugs to one another, TABLE 36,11-14 should not be used to make direct comparisons.
A new monoclonal antibody, romosozumab, has shown statistically significant decreases in the risk of new vertebral and nonvertebral fractures compared to alendronate after 12 months of use.16 However, there was a statistically significant higher number of patients who had a cardiac ischemic event or revascularization while taking romosozumab compared with those taking alendronate in the one-year double-blind period of the study.16 As of press time, the US Food and Drug Administration has not approved romosozumab.
Duration of treatment should be individualized based on specific patient factors, the pharmacologic agent, and, of course, adverse effects. However, no pharmacologic agent should be used indefinitely.6 In its clinical practice guidelines, the ACP recommends that patients be treated for 5 years with an appropriate pharmacologic therapy.8 The American Society for Bone and Mineral Research (ASBMR) Task Force recommends a review of therapy after 3 years with an intravenous bisphosphonate (BP; strength of recommendation [SOR]=C).17
A review of 2 recent long-term trials analyzing the effects of BPs offers some additional guidance regarding duration of therapy in Caucasian postmenopausal women.18 In one study, women who received 10 years of therapy with alendronate reported fewer vertebral fractures than those who were switched to placebo after 5 years of treatment.19
In the second trial, which studied zoledronic acid, there were fewer morphometric vertebral fractures for those participants given annual injections for 6 years vs 3 years.20 This trial found a significant transient increase in serum creatinine >0.5 mg/dL in the zoledronic acid treatment group.
These findings have prompted some experts in the field of osteoporosis to call for physicians to consider longer therapy with a BP (10 years with oral therapy or 6 years with intravenous therapy) in high-risk postmenopausal women (older women, those with a low hip T-score or high fracture risk score, those with a previous major osteoporotic fracture, and those who experienced fracture while on therapy) (SOR=B).18
Two rare adverse effects to keep in mind
The incidence of atypical femoral fracture, although rare (2-100 per 100,000 women), increases with duration of BP use. As a result, a drug holiday of 2 to 3 years should be considered for women with a low risk for fracture after 3 to 5 years of BP therapy (SOR=C).18
Osteonecrosis of the jaw (ONJ), also known as antiresorptive-associated osteonecrosis of the jaw, is a rare adverse effect of BPs that is associated with higher drug potency, higher cumulative dose, and parenteral route of administration, as well as other risk factors.17,21 The American Association of Maxillofacial Surgeons (AAOMS) states that the risk of developing ONJ increases with use of oral BPs for more than 4 years;22 however, the Task Force of the ASBMR states that the evidence to support this is of poor quality.18 No recommendations on duration of therapy based on risk for ONJ have been made; however, AAOMS recommends discontinuation of oral BPs for a period of 2 months prior to, and 3 months following (or until osseous healing has occurred), elective invasive dental surgery for patients who have been taking an oral BP ≥4 years (SOR=C).22
If a long-term drug holiday is selected, patients should be reassessed in 2 years. Shorter duration of follow-up is warranted for patients taking denosumab, teriparatide, or raloxifene, since bone loss will resume once therapy is discontinued.18
Because the benefits of BPs (in terms of reducing the risk of vertebral fracture) are significantly greater than the risks of an atypical fracture or ONJ, therapy should be started in appropriate patients, but duration of therapy should be monitored closely.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CORRESPONDENCE
Lovedhi Aggarwal, MD, 95-390 Kuahelani Avenue, Mililani, HI 96789; [email protected].
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520-2526.
2. Office of the Surgeon General (US). Bone health and osteoporosis: a report of the Surgeon General. Rockville (MD); 2004.
3. Dempster DW. Osteoporosis and the burden of osteoporosis-related fractures. Am J Manag Care. 2011;17 Suppl 6:S164-S169.
4. Kanis JA, McCloskey EV, Johansson H, et al, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23-57.
5. Screening for Osteoporosis: U.S. Preventive Services Task Force Final Recommendation Statement. Ann Intern Med. 2011;154:356-364.
6. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis (National Osteoporosis Foundation). Osteoporos Int. 2014;25:2359-2381.
7. Committee on Practice Bulletins-Gynecology, The American College of Obstetricians and Gynecologists. ACOG Practice Bulletin N. 129. Osteoporosis. Obstet Gynecol. 2012;120:718-734.
8. Qaseem A, Forciea MA, McLean RM, et al. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166:818-839.
9. Jeremiah MP, Unwin BK, Greenawald MH, et al. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92:261-268.
10. Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395-2411.
11. Lexicomp Online. Clinical Drug Information. Available at: https://online.lexi.com/lco/action/home. Accessed June 30, 2016.
12. Crandall CJ, Newberry SJ, Diamant A, et al. Treatment to Prevent Fractures in Men and Women with Low Bone Density and Osteoporosis: Update of a 2007 Report. Comparative Effectiveness Review No. 53. Rockville, MD: Agency for Healthcare Research and Quality; March 2012. Available at: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/osteoporosis-bone-fracture_research.pdf. Accessed January 10, 2018.
13. O’Connell MB, Borchert JS. Chapter 73. Osteoporosis and other metabolic bone diseases. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy: a pathophysiologic approach. 9th ed. McGraw-Hill Education; 2014.
14. Crandall CJ, Newberry SJ, Diamant A, et al. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014;161:711-723.
15. Watts NB, Bilezikian JP, Camacho PM, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16(Supp 3):1-37. Available at: https://www.aace.com/files/osteo-guidelines-2010.pdf. Accessed June 17, 2016.
16. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427.
17. Adler RA, El-Hajj Fuleihan G, Bauer DC, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: Report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31:16-35.
18. Adler RA. Duration of anti-resorptive therapy for osteoporosis. Endocrine. 2015;51:222-224.
19. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927-2938.
20. Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27:243-254.
21. Denosumab (Xgeva, Prolia); intravenous bisphosphonates: osteonecrosis of the jaw—further measures to minimise risk. 2015. Available at: https://www.gov.uk/drug-safety-update/denosumab-xgeva-prolia-intravenous-bisphosphonates-osteonecrosis-of-the-jaw-further-measures-to-minimise-risk. Accessed June 30, 2016.
22. Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938-1956.
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520-2526.
2. Office of the Surgeon General (US). Bone health and osteoporosis: a report of the Surgeon General. Rockville (MD); 2004.
3. Dempster DW. Osteoporosis and the burden of osteoporosis-related fractures. Am J Manag Care. 2011;17 Suppl 6:S164-S169.
4. Kanis JA, McCloskey EV, Johansson H, et al, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23-57.
5. Screening for Osteoporosis: U.S. Preventive Services Task Force Final Recommendation Statement. Ann Intern Med. 2011;154:356-364.
6. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis (National Osteoporosis Foundation). Osteoporos Int. 2014;25:2359-2381.
7. Committee on Practice Bulletins-Gynecology, The American College of Obstetricians and Gynecologists. ACOG Practice Bulletin N. 129. Osteoporosis. Obstet Gynecol. 2012;120:718-734.
8. Qaseem A, Forciea MA, McLean RM, et al. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166:818-839.
9. Jeremiah MP, Unwin BK, Greenawald MH, et al. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92:261-268.
10. Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395-2411.
11. Lexicomp Online. Clinical Drug Information. Available at: https://online.lexi.com/lco/action/home. Accessed June 30, 2016.
12. Crandall CJ, Newberry SJ, Diamant A, et al. Treatment to Prevent Fractures in Men and Women with Low Bone Density and Osteoporosis: Update of a 2007 Report. Comparative Effectiveness Review No. 53. Rockville, MD: Agency for Healthcare Research and Quality; March 2012. Available at: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/osteoporosis-bone-fracture_research.pdf. Accessed January 10, 2018.
13. O’Connell MB, Borchert JS. Chapter 73. Osteoporosis and other metabolic bone diseases. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy: a pathophysiologic approach. 9th ed. McGraw-Hill Education; 2014.
14. Crandall CJ, Newberry SJ, Diamant A, et al. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014;161:711-723.
15. Watts NB, Bilezikian JP, Camacho PM, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16(Supp 3):1-37. Available at: https://www.aace.com/files/osteo-guidelines-2010.pdf. Accessed June 17, 2016.
16. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427.
17. Adler RA, El-Hajj Fuleihan G, Bauer DC, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: Report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31:16-35.
18. Adler RA. Duration of anti-resorptive therapy for osteoporosis. Endocrine. 2015;51:222-224.
19. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927-2938.
20. Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27:243-254.
21. Denosumab (Xgeva, Prolia); intravenous bisphosphonates: osteonecrosis of the jaw—further measures to minimise risk. 2015. Available at: https://www.gov.uk/drug-safety-update/denosumab-xgeva-prolia-intravenous-bisphosphonates-osteonecrosis-of-the-jaw-further-measures-to-minimise-risk. Accessed June 30, 2016.
22. Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938-1956.
From The Journal of Family Practice | 2018;67(2):59-62,64-65.
PRACTICE RECOMMENDATIONS
› Use bisphosphonates (except ibandronate) and denosumab as first-line pharmacologic treatment for osteoporosis. A
› Treat patients for 5 years with oral bisphosphonates and 3 years with intravenous bisphosphonates before reviewing therapy, unless there are complications. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series