User login
Key 2010 publications in behavioral medicine
The effect of emotion on the heart is not confined to depression, but extends to a variety of mental states; as William Harvey described in 1628, “A mental disturbance provoking pain, excessive joy, hope or anxiety extends to the heart, where it affects its temper and rate, impairing general nutrition and vigor.”
In going beyond the well-established role of depression as a risk factor for heart disease, 2010 delivered several important publications recognizing anxiety, anger, and other forms of distress as key factors in the etiology of coronary heart disease (CHD). Other papers of merit elucidated new and overlooked insights into the pathways linking psychosocial stress and cardiovascular risk, and also considered psychologic states that appear to promote healthy functioning.
IMPACT OF NEGATIVE EMOTIONS ON RISK OF INCIDENT CORONARY HEART DISEASE
In a meta-analysis of 20 prospective studies that included 249,846 persons with a mean follow-up of 11.2 years, Roest et al1 examined the impact of anxiety characterized by the presence of anxiety symptoms or a diagnosis of anxiety disorder on incident CHD. Most of the studies adjusted for a broad array of relevant potential confounders. Findings suggest the presence of anxiety increases the risk of incident CHD by 26% (P P = .003).
In a meta-analysis of 25 prospective studies of 7,160 persons with a mean follow-up exceeding 10 years, Chida and Steptoe2 found that anger increased the risk of incident CHD by 19%, after adjustment for standard coronary risk factors. The effect was less stable than that associated with anxiety and depression, and when stratified by gender, the harmful effects of anger were more evident in men than in women. The effect of anger was attenuated when controlling for behavioral covariates. The association between anger and CHD did not hold for all ways of measuring anger, which suggests that the type of anger or the ability to regulate anger may be relevant to the relationship.
A study that did account for the type of anger expression on the risk of incident CHD was conducted by Davidson and Mostofsky.3 The independent effect of three distinct types of anger expression (constructive anger, destructive anger justification, and destructive anger rumination) on 10-year incident CHD was examined, controlling for other psychosocial factors. In men, higher scores for constructive anger were associated with a lower rate of CHD; in both men and women, higher scores for destructive anger justification were associated with an increased risk of CHD.
Insights gained from these studies are as follows:
- The impact of anxiety appears to be comparable to depression, and the effects of anxiety and depression are largely independent.
- If anxiety and depression co-occur, the effect on CHD is synergistic.
- The effects of anger are less clear; its impact may be independent of or dependent on other forms of psychologic distress.
- Distress in general appears to serve as a signal that something is wrong and needs to be addressed. If ignored, it may become chronic and unremitting; because symptoms of distress may lead to systemic dysregulation and increased CHD risk, they may indicate the need for increased surveillance and intervention.
WHY FOCUS ON THE BIOLOGY OF EMOTIONS?
A clear biologic explanation for the influence of emotional factors on physical health would serve to assuage skeptics who doubt that such a link exists or who attribute a common underlying genetic trait to both negative affect and heart disease. Further, focusing on the biology may help answer key questions with respect to emotions and disease processes: What is the damage incurred by negative emotional states and is it reversible? Can compensatory pathways be activated to bypass the mechanisms causing damage or slow the progression of disease?
Cardiac response to worry and stress
In one study attempting to shed light on relevant emotion-related biologic process, the prolonged physiologic effects of worry were examined. Worry episodes and stressful events were recorded hourly along with ambulatory heart rate and heart rate variability in 73 teachers for 4 days.4 Autonomic activity, as reflected by a concurrent elevation in heart rate and a decrease in heart rate variability, was increased up to 2 hours after a worry episode. The findings also suggested that the prolonged cardiac effects of separate worry episodes were independent.
Another study sought to determine whether heightened reactivity or delayed recovery to acute stress increases risk of cardiovascular disease.5 This meta-analysis included 36 studies to assess whether acute cardiovascular response to various laboratory stressors (ie, cognitive tasks, stress interviews, public speaking). Findings indicated that heightened cardiovascular reactivity was associated with worse cardiovascular outcomes, such as incident hypertension, coronary calcification, carotid intima-media thickness, and cardiovascular events over time.
Role of aldosterone overlooked
WHY CONSIDER RESILIENCE?
Because the absence of a deficit is not the same as the presence of an asset, greater insight into dysfunction may be gained by explicitly considering what promotes healthy functioning. Ameliorating distress has proven difficult; so, in studying resilience (including the ability to regulate affect), new targets for prevention and intervention may be identified. Although no meta-analysis of resilience factors has been published to date owing to the paucity of data, the studies that have been performed are generally rigorous and have demonstrated consistent findings.
For example, one prospective, well-controlled study of 1,739 men and women demonstrated a protective effect of positive affect (as ascertained by structured interview) against 10-year incident CHD.6 The risk of fatal or nonfatal ischemic heart disease events was reduced by 22% (P = .02) for each 1-point increase in positive affect, even after controlling for depression and negative emotions.
Biology of resilience: Counteracting cellular damage
Genomic changes can be induced by the relaxation response, as evidenced by the differential gene expression profiles of long-term daily practitioners of relaxation (ie, meditation, yoga), short-term (8-week) practitioners of relaxation, and healthy controls.8 Alterations in cellular metabolism, oxidative phosphorylation, and generation of reactive oxygen species that counteract proinflammatory responses, indicative of an adaptive response, were observed in both groups that practiced relaxation.
FUTURE DIRECTIONS
Whether and how the sources and effects of psychosocial stress and response to treatment differ across men and women deserves closer examination. A review by Low et al9 summarizes the current state of knowledge with respect to psychosocial factors and heart disease in women, noting that the sources of stress associated with increased CHD risk differ across men and women; psychosocial risk factors like depression and anxiety appear to increase risk for both men and women; work-related stress has larger effects in men while stress related to relationships and family responsibilities appear to have larger effects in women.
Although responses to psychosocial stress are not clearly different between men and women, intervention targeted at reducing distress is much less effective in reducing the risk of adverse events in women versus men. The mechanism to explain this difference in effectiveness of intervention urgently requires further exploration.
In conducting this work, several factors are important. The best time to intervene to reduce psychosocial distress is unknown; a key consideration will be, what is the best etiologic window for intervention? Perhaps a life-course approach that targets individuals with chronically high levels of emotional distress who also have multiple coronary risk factors, and that enhances their capacity to regulate emotions would prove superior to waiting until late in the disease process.
Another area that may prove fruitful is to consider in more depth the biology of the placebo effect and whether and how it may inform our understanding of resilience.
More generally, considering why interventions seem to influence outcomes so differently across men and women, applying a life course approach to determine the best etiologic window for prevention and intervention strategies, and conducting a more in-depth exploration of the biology of resilience may lead to improved capacity for population-based approaches to reducing the burden of CHD.
- Roest AM, Martens E, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010; 56:38–46.
- Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol 2009; 53:936–946.
- Davidson KW, Mostofsky E. Anger expression and risk of coronary heart disease: evidence from the Nova Scotia Health Survey. Am Heart J 2010; 159:199–206.
- Pieper S, Brosschot JF, van der Leeden R, Thayer J. Prolonged cardiac effects of momentary assessed stressful events and worry episodes. Psychosom Med 2010; 72:570–577.
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension 2010; 55:1026–1032.
- Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J 2010; 31:1065–1070.
- Kubzansky LD, Park N, Peterson C, Vokonas P, Sparrow D. Healthy psychological functioning and incident coronary heart disease. Arch Gen Psychiatry 2000; 68:400–408.
- Dusek JA, Out HH, Wohlhueter AL, et al Genomic counterstress changes induced by the relaxation response. PLoS One 2008; 3:e2576.
- Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: current research and future directions. Psychosom Med 2010; 72:842–854.
The effect of emotion on the heart is not confined to depression, but extends to a variety of mental states; as William Harvey described in 1628, “A mental disturbance provoking pain, excessive joy, hope or anxiety extends to the heart, where it affects its temper and rate, impairing general nutrition and vigor.”
In going beyond the well-established role of depression as a risk factor for heart disease, 2010 delivered several important publications recognizing anxiety, anger, and other forms of distress as key factors in the etiology of coronary heart disease (CHD). Other papers of merit elucidated new and overlooked insights into the pathways linking psychosocial stress and cardiovascular risk, and also considered psychologic states that appear to promote healthy functioning.
IMPACT OF NEGATIVE EMOTIONS ON RISK OF INCIDENT CORONARY HEART DISEASE
In a meta-analysis of 20 prospective studies that included 249,846 persons with a mean follow-up of 11.2 years, Roest et al1 examined the impact of anxiety characterized by the presence of anxiety symptoms or a diagnosis of anxiety disorder on incident CHD. Most of the studies adjusted for a broad array of relevant potential confounders. Findings suggest the presence of anxiety increases the risk of incident CHD by 26% (P P = .003).
In a meta-analysis of 25 prospective studies of 7,160 persons with a mean follow-up exceeding 10 years, Chida and Steptoe2 found that anger increased the risk of incident CHD by 19%, after adjustment for standard coronary risk factors. The effect was less stable than that associated with anxiety and depression, and when stratified by gender, the harmful effects of anger were more evident in men than in women. The effect of anger was attenuated when controlling for behavioral covariates. The association between anger and CHD did not hold for all ways of measuring anger, which suggests that the type of anger or the ability to regulate anger may be relevant to the relationship.
A study that did account for the type of anger expression on the risk of incident CHD was conducted by Davidson and Mostofsky.3 The independent effect of three distinct types of anger expression (constructive anger, destructive anger justification, and destructive anger rumination) on 10-year incident CHD was examined, controlling for other psychosocial factors. In men, higher scores for constructive anger were associated with a lower rate of CHD; in both men and women, higher scores for destructive anger justification were associated with an increased risk of CHD.
Insights gained from these studies are as follows:
- The impact of anxiety appears to be comparable to depression, and the effects of anxiety and depression are largely independent.
- If anxiety and depression co-occur, the effect on CHD is synergistic.
- The effects of anger are less clear; its impact may be independent of or dependent on other forms of psychologic distress.
- Distress in general appears to serve as a signal that something is wrong and needs to be addressed. If ignored, it may become chronic and unremitting; because symptoms of distress may lead to systemic dysregulation and increased CHD risk, they may indicate the need for increased surveillance and intervention.
WHY FOCUS ON THE BIOLOGY OF EMOTIONS?
A clear biologic explanation for the influence of emotional factors on physical health would serve to assuage skeptics who doubt that such a link exists or who attribute a common underlying genetic trait to both negative affect and heart disease. Further, focusing on the biology may help answer key questions with respect to emotions and disease processes: What is the damage incurred by negative emotional states and is it reversible? Can compensatory pathways be activated to bypass the mechanisms causing damage or slow the progression of disease?
Cardiac response to worry and stress
In one study attempting to shed light on relevant emotion-related biologic process, the prolonged physiologic effects of worry were examined. Worry episodes and stressful events were recorded hourly along with ambulatory heart rate and heart rate variability in 73 teachers for 4 days.4 Autonomic activity, as reflected by a concurrent elevation in heart rate and a decrease in heart rate variability, was increased up to 2 hours after a worry episode. The findings also suggested that the prolonged cardiac effects of separate worry episodes were independent.
Another study sought to determine whether heightened reactivity or delayed recovery to acute stress increases risk of cardiovascular disease.5 This meta-analysis included 36 studies to assess whether acute cardiovascular response to various laboratory stressors (ie, cognitive tasks, stress interviews, public speaking). Findings indicated that heightened cardiovascular reactivity was associated with worse cardiovascular outcomes, such as incident hypertension, coronary calcification, carotid intima-media thickness, and cardiovascular events over time.
Role of aldosterone overlooked
WHY CONSIDER RESILIENCE?
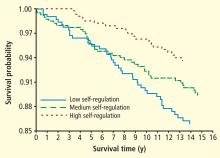
Because the absence of a deficit is not the same as the presence of an asset, greater insight into dysfunction may be gained by explicitly considering what promotes healthy functioning. Ameliorating distress has proven difficult; so, in studying resilience (including the ability to regulate affect), new targets for prevention and intervention may be identified. Although no meta-analysis of resilience factors has been published to date owing to the paucity of data, the studies that have been performed are generally rigorous and have demonstrated consistent findings.
For example, one prospective, well-controlled study of 1,739 men and women demonstrated a protective effect of positive affect (as ascertained by structured interview) against 10-year incident CHD.6 The risk of fatal or nonfatal ischemic heart disease events was reduced by 22% (P = .02) for each 1-point increase in positive affect, even after controlling for depression and negative emotions.
Biology of resilience: Counteracting cellular damage
Genomic changes can be induced by the relaxation response, as evidenced by the differential gene expression profiles of long-term daily practitioners of relaxation (ie, meditation, yoga), short-term (8-week) practitioners of relaxation, and healthy controls.8 Alterations in cellular metabolism, oxidative phosphorylation, and generation of reactive oxygen species that counteract proinflammatory responses, indicative of an adaptive response, were observed in both groups that practiced relaxation.
FUTURE DIRECTIONS
Whether and how the sources and effects of psychosocial stress and response to treatment differ across men and women deserves closer examination. A review by Low et al9 summarizes the current state of knowledge with respect to psychosocial factors and heart disease in women, noting that the sources of stress associated with increased CHD risk differ across men and women; psychosocial risk factors like depression and anxiety appear to increase risk for both men and women; work-related stress has larger effects in men while stress related to relationships and family responsibilities appear to have larger effects in women.
Although responses to psychosocial stress are not clearly different between men and women, intervention targeted at reducing distress is much less effective in reducing the risk of adverse events in women versus men. The mechanism to explain this difference in effectiveness of intervention urgently requires further exploration.
In conducting this work, several factors are important. The best time to intervene to reduce psychosocial distress is unknown; a key consideration will be, what is the best etiologic window for intervention? Perhaps a life-course approach that targets individuals with chronically high levels of emotional distress who also have multiple coronary risk factors, and that enhances their capacity to regulate emotions would prove superior to waiting until late in the disease process.
Another area that may prove fruitful is to consider in more depth the biology of the placebo effect and whether and how it may inform our understanding of resilience.
More generally, considering why interventions seem to influence outcomes so differently across men and women, applying a life course approach to determine the best etiologic window for prevention and intervention strategies, and conducting a more in-depth exploration of the biology of resilience may lead to improved capacity for population-based approaches to reducing the burden of CHD.
The effect of emotion on the heart is not confined to depression, but extends to a variety of mental states; as William Harvey described in 1628, “A mental disturbance provoking pain, excessive joy, hope or anxiety extends to the heart, where it affects its temper and rate, impairing general nutrition and vigor.”
In going beyond the well-established role of depression as a risk factor for heart disease, 2010 delivered several important publications recognizing anxiety, anger, and other forms of distress as key factors in the etiology of coronary heart disease (CHD). Other papers of merit elucidated new and overlooked insights into the pathways linking psychosocial stress and cardiovascular risk, and also considered psychologic states that appear to promote healthy functioning.
IMPACT OF NEGATIVE EMOTIONS ON RISK OF INCIDENT CORONARY HEART DISEASE
In a meta-analysis of 20 prospective studies that included 249,846 persons with a mean follow-up of 11.2 years, Roest et al1 examined the impact of anxiety characterized by the presence of anxiety symptoms or a diagnosis of anxiety disorder on incident CHD. Most of the studies adjusted for a broad array of relevant potential confounders. Findings suggest the presence of anxiety increases the risk of incident CHD by 26% (P P = .003).
In a meta-analysis of 25 prospective studies of 7,160 persons with a mean follow-up exceeding 10 years, Chida and Steptoe2 found that anger increased the risk of incident CHD by 19%, after adjustment for standard coronary risk factors. The effect was less stable than that associated with anxiety and depression, and when stratified by gender, the harmful effects of anger were more evident in men than in women. The effect of anger was attenuated when controlling for behavioral covariates. The association between anger and CHD did not hold for all ways of measuring anger, which suggests that the type of anger or the ability to regulate anger may be relevant to the relationship.
A study that did account for the type of anger expression on the risk of incident CHD was conducted by Davidson and Mostofsky.3 The independent effect of three distinct types of anger expression (constructive anger, destructive anger justification, and destructive anger rumination) on 10-year incident CHD was examined, controlling for other psychosocial factors. In men, higher scores for constructive anger were associated with a lower rate of CHD; in both men and women, higher scores for destructive anger justification were associated with an increased risk of CHD.
Insights gained from these studies are as follows:
- The impact of anxiety appears to be comparable to depression, and the effects of anxiety and depression are largely independent.
- If anxiety and depression co-occur, the effect on CHD is synergistic.
- The effects of anger are less clear; its impact may be independent of or dependent on other forms of psychologic distress.
- Distress in general appears to serve as a signal that something is wrong and needs to be addressed. If ignored, it may become chronic and unremitting; because symptoms of distress may lead to systemic dysregulation and increased CHD risk, they may indicate the need for increased surveillance and intervention.
WHY FOCUS ON THE BIOLOGY OF EMOTIONS?
A clear biologic explanation for the influence of emotional factors on physical health would serve to assuage skeptics who doubt that such a link exists or who attribute a common underlying genetic trait to both negative affect and heart disease. Further, focusing on the biology may help answer key questions with respect to emotions and disease processes: What is the damage incurred by negative emotional states and is it reversible? Can compensatory pathways be activated to bypass the mechanisms causing damage or slow the progression of disease?
Cardiac response to worry and stress
In one study attempting to shed light on relevant emotion-related biologic process, the prolonged physiologic effects of worry were examined. Worry episodes and stressful events were recorded hourly along with ambulatory heart rate and heart rate variability in 73 teachers for 4 days.4 Autonomic activity, as reflected by a concurrent elevation in heart rate and a decrease in heart rate variability, was increased up to 2 hours after a worry episode. The findings also suggested that the prolonged cardiac effects of separate worry episodes were independent.
Another study sought to determine whether heightened reactivity or delayed recovery to acute stress increases risk of cardiovascular disease.5 This meta-analysis included 36 studies to assess whether acute cardiovascular response to various laboratory stressors (ie, cognitive tasks, stress interviews, public speaking). Findings indicated that heightened cardiovascular reactivity was associated with worse cardiovascular outcomes, such as incident hypertension, coronary calcification, carotid intima-media thickness, and cardiovascular events over time.
Role of aldosterone overlooked
WHY CONSIDER RESILIENCE?
Because the absence of a deficit is not the same as the presence of an asset, greater insight into dysfunction may be gained by explicitly considering what promotes healthy functioning. Ameliorating distress has proven difficult; so, in studying resilience (including the ability to regulate affect), new targets for prevention and intervention may be identified. Although no meta-analysis of resilience factors has been published to date owing to the paucity of data, the studies that have been performed are generally rigorous and have demonstrated consistent findings.
For example, one prospective, well-controlled study of 1,739 men and women demonstrated a protective effect of positive affect (as ascertained by structured interview) against 10-year incident CHD.6 The risk of fatal or nonfatal ischemic heart disease events was reduced by 22% (P = .02) for each 1-point increase in positive affect, even after controlling for depression and negative emotions.
Biology of resilience: Counteracting cellular damage
Genomic changes can be induced by the relaxation response, as evidenced by the differential gene expression profiles of long-term daily practitioners of relaxation (ie, meditation, yoga), short-term (8-week) practitioners of relaxation, and healthy controls.8 Alterations in cellular metabolism, oxidative phosphorylation, and generation of reactive oxygen species that counteract proinflammatory responses, indicative of an adaptive response, were observed in both groups that practiced relaxation.
FUTURE DIRECTIONS
Whether and how the sources and effects of psychosocial stress and response to treatment differ across men and women deserves closer examination. A review by Low et al9 summarizes the current state of knowledge with respect to psychosocial factors and heart disease in women, noting that the sources of stress associated with increased CHD risk differ across men and women; psychosocial risk factors like depression and anxiety appear to increase risk for both men and women; work-related stress has larger effects in men while stress related to relationships and family responsibilities appear to have larger effects in women.
Although responses to psychosocial stress are not clearly different between men and women, intervention targeted at reducing distress is much less effective in reducing the risk of adverse events in women versus men. The mechanism to explain this difference in effectiveness of intervention urgently requires further exploration.
In conducting this work, several factors are important. The best time to intervene to reduce psychosocial distress is unknown; a key consideration will be, what is the best etiologic window for intervention? Perhaps a life-course approach that targets individuals with chronically high levels of emotional distress who also have multiple coronary risk factors, and that enhances their capacity to regulate emotions would prove superior to waiting until late in the disease process.
Another area that may prove fruitful is to consider in more depth the biology of the placebo effect and whether and how it may inform our understanding of resilience.
More generally, considering why interventions seem to influence outcomes so differently across men and women, applying a life course approach to determine the best etiologic window for prevention and intervention strategies, and conducting a more in-depth exploration of the biology of resilience may lead to improved capacity for population-based approaches to reducing the burden of CHD.
- Roest AM, Martens E, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010; 56:38–46.
- Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol 2009; 53:936–946.
- Davidson KW, Mostofsky E. Anger expression and risk of coronary heart disease: evidence from the Nova Scotia Health Survey. Am Heart J 2010; 159:199–206.
- Pieper S, Brosschot JF, van der Leeden R, Thayer J. Prolonged cardiac effects of momentary assessed stressful events and worry episodes. Psychosom Med 2010; 72:570–577.
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension 2010; 55:1026–1032.
- Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J 2010; 31:1065–1070.
- Kubzansky LD, Park N, Peterson C, Vokonas P, Sparrow D. Healthy psychological functioning and incident coronary heart disease. Arch Gen Psychiatry 2000; 68:400–408.
- Dusek JA, Out HH, Wohlhueter AL, et al Genomic counterstress changes induced by the relaxation response. PLoS One 2008; 3:e2576.
- Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: current research and future directions. Psychosom Med 2010; 72:842–854.
- Roest AM, Martens E, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010; 56:38–46.
- Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol 2009; 53:936–946.
- Davidson KW, Mostofsky E. Anger expression and risk of coronary heart disease: evidence from the Nova Scotia Health Survey. Am Heart J 2010; 159:199–206.
- Pieper S, Brosschot JF, van der Leeden R, Thayer J. Prolonged cardiac effects of momentary assessed stressful events and worry episodes. Psychosom Med 2010; 72:570–577.
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension 2010; 55:1026–1032.
- Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J 2010; 31:1065–1070.
- Kubzansky LD, Park N, Peterson C, Vokonas P, Sparrow D. Healthy psychological functioning and incident coronary heart disease. Arch Gen Psychiatry 2000; 68:400–408.
- Dusek JA, Out HH, Wohlhueter AL, et al Genomic counterstress changes induced by the relaxation response. PLoS One 2008; 3:e2576.
- Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: current research and future directions. Psychosom Med 2010; 72:842–854.