User login
Brazil sees first live birth from deceased-donor uterus transplant
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
FROM THE LANCET
Obesity meds used by just over half of pediatric obesity programs
NASHVILLE, TENN. –
Programs that didn’t offer pharmacotherapy for children and adolescents with obesity cited a variety of reasons in responses to a survey of 33 multicomponent pediatric weight management programs (PWMPs).
Simply not being in favor of using pharmacotherapy for obesity treatment was the most frequently cited reason, named by seven PWMPs that didn’t prescribe obesity medications.
The second most common response to the survey, cited by six programs, was a lack of knowledge about prescribing medications for obesity, and concerns about insurance coverage were noted by five programs, said Claudia Fox, MD, and her colleagues in a poster presentation at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “Despite recommendations, few youth with severe obesity are treated with medications.”
Of the programs that did offer pharmacotherapy, 14 prescribed topiramate, and 13 prescribed phentermine. Metformin was used by 11 programs, and orlistat by eight. Six programs prescribed the fixed-dose combination of topiramate and phentermine.
Lorcaserin, naltrexone/bupropion, liraglutide, phendimetrazine, and naltrexone alone all were used by fewer than five programs each.
The national Pediatric Obesity Weight Evaluation Registry (POWER) “was established in 2013 to identify and promote effective intervention strategies for pediatric obesity,” wrote Dr. Fox and her colleagues
Of the 33 POWER PWMPs who were invited to participate, 30 completed a program profile survey. Of these, 16 programs (53%) offered pharmacotherapy, wrote Dr. Fox, the codirector of the University of Minnesota’s Center for Pediatric Obesity Medicine, Minneapolis, and her colleagues in the POWER work group.
In addition to not being in favor of prescribing obesity medication for pediatric patients, lack of knowledge, and insurance concerns, one program cited limited outcome studies for pediatric obesity pharmacotherapy. One other program’s response noted that patients couldn’t be seen frequently enough to assess the safety of obesity medications.
Taken together, the POWER sites had 7,880 patients. Just 5% were aged 2- 5 years, 48% were aged 6-11 years, and 47% were aged 12-18 years. Just over half (53%) were female.
At baseline, about a quarter of patients (26.4%) had class 1 obesity, defined as a body mass index of at least the 95th age- and sex-adjusted percentile. Children and adolescents with class 2 obesity (BMI of at least 1.2-1.4 times the 95th percentile) made up 35.3% of patients; 38.3% had class 3 obesity, with BMIs greater than 1.4 times the 95th percentile.
In 2017, the Endocrine Society published updated clinical practice guidelines for the assessment, treatment, and prevention of pediatric obesity (J Clin Endocrin Metab. 2017 Mar;102:3;709-57). The guidelines for pediatric obesity treatment recommend intensive lifestyle modifications including dietary, physical activity, and behavioral interventions. Pharmacotherapy is suggested “only after a formal program of intensive lifestyle modification has failed to limit weight gain or to ameliorate comorbidities.” Additionally, say the guidelines, Food and Drug Administration–approved pharmacotherapy should be used only “with a concomitant lifestyle modification program of the highest intensity available and only by clinicians who are experienced in the use of anti-obesity agents and are aware of the potential for adverse reactions.”
“Most commonly prescribed medications are not FDA approved for indication of obesity in pediatrics,” noted Dr. Fox and her coauthors. “Further research is needed to evaluate efficacy of pharmacotherapy in the pediatric population and to understand factors impacting prescribing practices.”
Dr. Fox reported no outside sources of funding and had no relevant financial disclosures.
NASHVILLE, TENN. –
Programs that didn’t offer pharmacotherapy for children and adolescents with obesity cited a variety of reasons in responses to a survey of 33 multicomponent pediatric weight management programs (PWMPs).
Simply not being in favor of using pharmacotherapy for obesity treatment was the most frequently cited reason, named by seven PWMPs that didn’t prescribe obesity medications.
The second most common response to the survey, cited by six programs, was a lack of knowledge about prescribing medications for obesity, and concerns about insurance coverage were noted by five programs, said Claudia Fox, MD, and her colleagues in a poster presentation at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “Despite recommendations, few youth with severe obesity are treated with medications.”
Of the programs that did offer pharmacotherapy, 14 prescribed topiramate, and 13 prescribed phentermine. Metformin was used by 11 programs, and orlistat by eight. Six programs prescribed the fixed-dose combination of topiramate and phentermine.
Lorcaserin, naltrexone/bupropion, liraglutide, phendimetrazine, and naltrexone alone all were used by fewer than five programs each.
The national Pediatric Obesity Weight Evaluation Registry (POWER) “was established in 2013 to identify and promote effective intervention strategies for pediatric obesity,” wrote Dr. Fox and her colleagues
Of the 33 POWER PWMPs who were invited to participate, 30 completed a program profile survey. Of these, 16 programs (53%) offered pharmacotherapy, wrote Dr. Fox, the codirector of the University of Minnesota’s Center for Pediatric Obesity Medicine, Minneapolis, and her colleagues in the POWER work group.
In addition to not being in favor of prescribing obesity medication for pediatric patients, lack of knowledge, and insurance concerns, one program cited limited outcome studies for pediatric obesity pharmacotherapy. One other program’s response noted that patients couldn’t be seen frequently enough to assess the safety of obesity medications.
Taken together, the POWER sites had 7,880 patients. Just 5% were aged 2- 5 years, 48% were aged 6-11 years, and 47% were aged 12-18 years. Just over half (53%) were female.
At baseline, about a quarter of patients (26.4%) had class 1 obesity, defined as a body mass index of at least the 95th age- and sex-adjusted percentile. Children and adolescents with class 2 obesity (BMI of at least 1.2-1.4 times the 95th percentile) made up 35.3% of patients; 38.3% had class 3 obesity, with BMIs greater than 1.4 times the 95th percentile.
In 2017, the Endocrine Society published updated clinical practice guidelines for the assessment, treatment, and prevention of pediatric obesity (J Clin Endocrin Metab. 2017 Mar;102:3;709-57). The guidelines for pediatric obesity treatment recommend intensive lifestyle modifications including dietary, physical activity, and behavioral interventions. Pharmacotherapy is suggested “only after a formal program of intensive lifestyle modification has failed to limit weight gain or to ameliorate comorbidities.” Additionally, say the guidelines, Food and Drug Administration–approved pharmacotherapy should be used only “with a concomitant lifestyle modification program of the highest intensity available and only by clinicians who are experienced in the use of anti-obesity agents and are aware of the potential for adverse reactions.”
“Most commonly prescribed medications are not FDA approved for indication of obesity in pediatrics,” noted Dr. Fox and her coauthors. “Further research is needed to evaluate efficacy of pharmacotherapy in the pediatric population and to understand factors impacting prescribing practices.”
Dr. Fox reported no outside sources of funding and had no relevant financial disclosures.
NASHVILLE, TENN. –
Programs that didn’t offer pharmacotherapy for children and adolescents with obesity cited a variety of reasons in responses to a survey of 33 multicomponent pediatric weight management programs (PWMPs).
Simply not being in favor of using pharmacotherapy for obesity treatment was the most frequently cited reason, named by seven PWMPs that didn’t prescribe obesity medications.
The second most common response to the survey, cited by six programs, was a lack of knowledge about prescribing medications for obesity, and concerns about insurance coverage were noted by five programs, said Claudia Fox, MD, and her colleagues in a poster presentation at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “Despite recommendations, few youth with severe obesity are treated with medications.”
Of the programs that did offer pharmacotherapy, 14 prescribed topiramate, and 13 prescribed phentermine. Metformin was used by 11 programs, and orlistat by eight. Six programs prescribed the fixed-dose combination of topiramate and phentermine.
Lorcaserin, naltrexone/bupropion, liraglutide, phendimetrazine, and naltrexone alone all were used by fewer than five programs each.
The national Pediatric Obesity Weight Evaluation Registry (POWER) “was established in 2013 to identify and promote effective intervention strategies for pediatric obesity,” wrote Dr. Fox and her colleagues
Of the 33 POWER PWMPs who were invited to participate, 30 completed a program profile survey. Of these, 16 programs (53%) offered pharmacotherapy, wrote Dr. Fox, the codirector of the University of Minnesota’s Center for Pediatric Obesity Medicine, Minneapolis, and her colleagues in the POWER work group.
In addition to not being in favor of prescribing obesity medication for pediatric patients, lack of knowledge, and insurance concerns, one program cited limited outcome studies for pediatric obesity pharmacotherapy. One other program’s response noted that patients couldn’t be seen frequently enough to assess the safety of obesity medications.
Taken together, the POWER sites had 7,880 patients. Just 5% were aged 2- 5 years, 48% were aged 6-11 years, and 47% were aged 12-18 years. Just over half (53%) were female.
At baseline, about a quarter of patients (26.4%) had class 1 obesity, defined as a body mass index of at least the 95th age- and sex-adjusted percentile. Children and adolescents with class 2 obesity (BMI of at least 1.2-1.4 times the 95th percentile) made up 35.3% of patients; 38.3% had class 3 obesity, with BMIs greater than 1.4 times the 95th percentile.
In 2017, the Endocrine Society published updated clinical practice guidelines for the assessment, treatment, and prevention of pediatric obesity (J Clin Endocrin Metab. 2017 Mar;102:3;709-57). The guidelines for pediatric obesity treatment recommend intensive lifestyle modifications including dietary, physical activity, and behavioral interventions. Pharmacotherapy is suggested “only after a formal program of intensive lifestyle modification has failed to limit weight gain or to ameliorate comorbidities.” Additionally, say the guidelines, Food and Drug Administration–approved pharmacotherapy should be used only “with a concomitant lifestyle modification program of the highest intensity available and only by clinicians who are experienced in the use of anti-obesity agents and are aware of the potential for adverse reactions.”
“Most commonly prescribed medications are not FDA approved for indication of obesity in pediatrics,” noted Dr. Fox and her coauthors. “Further research is needed to evaluate efficacy of pharmacotherapy in the pediatric population and to understand factors impacting prescribing practices.”
Dr. Fox reported no outside sources of funding and had no relevant financial disclosures.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Just over half of pediatric weight management programs prescribed obesity medications.
Major finding: Of 30 programs responding, 16 (53%) prescribed obesity medication.
Study details: Survey of 33 programs in the Pediatric Obesity Weight Evaluation Registry (POWER).
Disclosures: Dr. Fox reported no outside sources of funding and no conflicts of interest.
Dietary sodium still in play as a potential MS risk factor
BERLIN – Among a host of potential risk factors for multiple sclerosis (MS), one emerging risk factor – dietary sodium – has accumulating evidence, bolstered by new imaging techniques and emerging research about the mediating effect of the gut microbiome.
“The word is still out on salt – there’s still some work to do; we are not where we stand with smoking or obesity” and the association with MS, said Ralf Linker, MD, speaking at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
For all potential emerging risk factors for MS, there’s an attractive hypothesis and, often, epidemiologic data, Dr. Linker said. “There are probably good [epidemiologic] data in multiple sclerosis for vitamin D, smoking, obesity, and probably also alcohol,” he said. “The therapeutic consequence, however, is much less clear, the best example of that being, of course, vitamin D.”
“The attractive risk factor is not enough to be a hypothesis, although some people seem to believe that nowadays,” said Dr. Linker, chair of the department of neurology at Friedrich-Alexander University, Erlangen, Germany. “Probably it’s better to start with some basic science and some experimental data to get an idea of the mechanism.”
“Today, we need clear associations with clear markers, well-defined cohorts, and proper epidemiological data telling us whether this is a real risk factor. ... If you look at the clinicians – and there are many among us in the room here – your ultimate goal, of course, is to use this as an intervention.”
For salt intake, there’s a clear overlap between high salt consumption in Westernized diets and increasing incidence of MS. The association also holds for many other autoimmune diseases, Dr. Linker added.
“The next step is experimental evidence,” Dr. Linker said. In a rodent model of experimental autoimmune encephalomyelitis (EAE), rats with high salt intake had a worse clinical course, compared with control rats fed a usual diet (Nature. 2013 Apr 25;496[7446]:518-22).
“There were a lot of follow-up studies on that,” with identification of multiple immune cells that are up- or down-regulated via distinct pathways in a high-salt environment, Dr. Linker said.
More recently, Dr. Linker was a coinvestigator in work showing that healthy humans placed on a high-salt diet had significant increases in T-helper 17 (Th17) cells after just 2 weeks of an additional 6 g of table salt daily over a baseline 2-4 g/day (Nature. 2017 Nov 30;551[7682]:585-9).
“You can also translate it to a more realistic setting,” where individuals who ate fast food four or more times weekly had significantly higher Th17 cell counts than did those who ate less fast food, he noted in reference to unpublished data.
Looking specifically at MS, a single-center study found that increased sodium intake correlated with increased MS clinical disease activity, with the highest sodium intake (more than 4.8 g/day) associated with higher incidence of MS exacerbations. Those in the highest tier of sodium intake also had a higher lesion load, with 3.65 more T2 lesions seen on MRI scans for each gram of salt consumed above average amounts of 2-4.8 g/day (J Neurol Neurosurg Psychiatry. 2015 Jan;86[1]:26-31).
On the other hand, Dr. Linker said, “There have been recent very well-conducted studies in very well-defined cohorts casting doubt on this translation to multiple sclerosis.” In particular, an examination of data from over 70,000 participants in the Nurse’s Health Study showed no association between MS risk and dietary salt assessed by a nutritional questionnaire (Neurology. 2017 Sep 26;89[13]:1322-9). “There was no hint that the diagnosis was linked in any way with salt exposure,” Dr. Linker said.
In the BENEFIT study, both a spot urine sample and a food questionnaire were used, and patients were grouped into quintiles of sodium intake. For demyelinating events and MS diagnosis, the curves for all quintiles were “completely overlapping,” with no sign of increased risk of MS with higher sodium intake (Ann Neurol. 2017;82:20-9).
An important caveat to the null findings in these analyses is the known poor agreement between self-report of salt intake and actual sodium load, Dr. Linker noted. Renal sodium excretion can vary widely despite fixed salt intake, so spot urine and even 24-hour urine collection don’t guarantee accuracy, he said, citing studies from space travel emulations that show wide day-to-day excursions in sodium excretion with a fixed diet.
A promising tool for accurate assessment of sodium load may be sodium-23 skin spectroscopy using MRI, because skin tissue binds sodium in a stable, nonosmotic fashion. Dr. Linker and his colleagues have recently found that skin sodium levels, measured at the calf, are higher in individuals with relapsing-remitting MS. “Indeed, the sodium level in the skin of the MS patients was significantly higher than in the controls” who did not have MS, he said of the study that matched 20 patients with MS with 20 healthy controls. The MRI studies were assessed by radiologists blinded to the disease status of participants.
The increase is seen in only free sodium and seen in skin, but not muscle tissue, Dr. Linker said.
Using MRI spectroscopy with a powerful 7-Tesla magnet, Dr. Linker and his colleagues returned to the rodent EAE model, also finding increased sodium in the skin. Mass spectrometry findings were similar in other rodent autoimmune models, he said. The differences were not seen for sodium in other organs, or for potassium levels in the skin.
“The most difficult point,” Dr. Linker said, is “can we use this therapeutically somehow? Of course, you can put your patients on a salt-free or very low-salt diet, but it’s not very tasty, of course, and adherence would be probably very, very low.”
The microbiome may play a modulating role that adds to the sodium-MS story and provides a potential therapeutic option. In mice, a high-salt diet was associated with marked and rapid depletion of Lactobacillus species in the mouse gut microbiome. In healthy humans as well, the drop in lactobacilli was quick and profound when 6 g/day of salt was added to the diet, Dr. Linker said (P = .0053 versus the control diet of 2-4 g sodium/day).
Working backward with the same healthy cohort, repletion of Lactobacillus by probiotic supplementation normalized systolic blood pressure, which had become elevated with increased dietary sodium. Further, Lactobacillus repletion downregulated Th17 cells to levels seen before the high-sodium diet, even when dietary sodium stayed high.
“This was even transferred to multiple sclerosis,” in work recently published by another group, Dr. Linker said. For patients with MS who consumed a Lactobacillus-containing probiotic, investigators could “clearly show, besides effects on the microbiome itself, that there were effects on antigen-presenting cells in MS patients.” Intermediate monocytes decreased, as did dendritic cells, in the small study that involved both healthy controls and MS patients who received a probiotic and then underwent a washout period. Stool and blood samples were collected in both groups to compare values with and without probiotic administration.
A question from the audience looked back at historic data: 100 or more years ago, salt was used extensively for food preservation in many parts of the world, so dietary sodium intake is thought to have been higher. The incidence of MS, though, was lower then. Dr. Linker pointed out that food preservation practices varied widely, and that a host of other variables make assessment of past or present associations difficult. “It’s hard to argue that salt is the one and only risk factor; I would strongly doubt that.”
Still, he said, this early work invites more study, with a target of establishing whether probiotic supplementation could be used as “add-on therapy to established immune drugs.”
Dr. Linker has received honoraria and research support from Bayer, Biogen, Genzyme, Merck Serono, Novartis, and TEVA.
SOURCE: Linker R. ECTRIMS 2018, Scientific Session 7.
BERLIN – Among a host of potential risk factors for multiple sclerosis (MS), one emerging risk factor – dietary sodium – has accumulating evidence, bolstered by new imaging techniques and emerging research about the mediating effect of the gut microbiome.
“The word is still out on salt – there’s still some work to do; we are not where we stand with smoking or obesity” and the association with MS, said Ralf Linker, MD, speaking at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
For all potential emerging risk factors for MS, there’s an attractive hypothesis and, often, epidemiologic data, Dr. Linker said. “There are probably good [epidemiologic] data in multiple sclerosis for vitamin D, smoking, obesity, and probably also alcohol,” he said. “The therapeutic consequence, however, is much less clear, the best example of that being, of course, vitamin D.”
“The attractive risk factor is not enough to be a hypothesis, although some people seem to believe that nowadays,” said Dr. Linker, chair of the department of neurology at Friedrich-Alexander University, Erlangen, Germany. “Probably it’s better to start with some basic science and some experimental data to get an idea of the mechanism.”
“Today, we need clear associations with clear markers, well-defined cohorts, and proper epidemiological data telling us whether this is a real risk factor. ... If you look at the clinicians – and there are many among us in the room here – your ultimate goal, of course, is to use this as an intervention.”
For salt intake, there’s a clear overlap between high salt consumption in Westernized diets and increasing incidence of MS. The association also holds for many other autoimmune diseases, Dr. Linker added.
“The next step is experimental evidence,” Dr. Linker said. In a rodent model of experimental autoimmune encephalomyelitis (EAE), rats with high salt intake had a worse clinical course, compared with control rats fed a usual diet (Nature. 2013 Apr 25;496[7446]:518-22).
“There were a lot of follow-up studies on that,” with identification of multiple immune cells that are up- or down-regulated via distinct pathways in a high-salt environment, Dr. Linker said.
More recently, Dr. Linker was a coinvestigator in work showing that healthy humans placed on a high-salt diet had significant increases in T-helper 17 (Th17) cells after just 2 weeks of an additional 6 g of table salt daily over a baseline 2-4 g/day (Nature. 2017 Nov 30;551[7682]:585-9).
“You can also translate it to a more realistic setting,” where individuals who ate fast food four or more times weekly had significantly higher Th17 cell counts than did those who ate less fast food, he noted in reference to unpublished data.
Looking specifically at MS, a single-center study found that increased sodium intake correlated with increased MS clinical disease activity, with the highest sodium intake (more than 4.8 g/day) associated with higher incidence of MS exacerbations. Those in the highest tier of sodium intake also had a higher lesion load, with 3.65 more T2 lesions seen on MRI scans for each gram of salt consumed above average amounts of 2-4.8 g/day (J Neurol Neurosurg Psychiatry. 2015 Jan;86[1]:26-31).
On the other hand, Dr. Linker said, “There have been recent very well-conducted studies in very well-defined cohorts casting doubt on this translation to multiple sclerosis.” In particular, an examination of data from over 70,000 participants in the Nurse’s Health Study showed no association between MS risk and dietary salt assessed by a nutritional questionnaire (Neurology. 2017 Sep 26;89[13]:1322-9). “There was no hint that the diagnosis was linked in any way with salt exposure,” Dr. Linker said.
In the BENEFIT study, both a spot urine sample and a food questionnaire were used, and patients were grouped into quintiles of sodium intake. For demyelinating events and MS diagnosis, the curves for all quintiles were “completely overlapping,” with no sign of increased risk of MS with higher sodium intake (Ann Neurol. 2017;82:20-9).
An important caveat to the null findings in these analyses is the known poor agreement between self-report of salt intake and actual sodium load, Dr. Linker noted. Renal sodium excretion can vary widely despite fixed salt intake, so spot urine and even 24-hour urine collection don’t guarantee accuracy, he said, citing studies from space travel emulations that show wide day-to-day excursions in sodium excretion with a fixed diet.
A promising tool for accurate assessment of sodium load may be sodium-23 skin spectroscopy using MRI, because skin tissue binds sodium in a stable, nonosmotic fashion. Dr. Linker and his colleagues have recently found that skin sodium levels, measured at the calf, are higher in individuals with relapsing-remitting MS. “Indeed, the sodium level in the skin of the MS patients was significantly higher than in the controls” who did not have MS, he said of the study that matched 20 patients with MS with 20 healthy controls. The MRI studies were assessed by radiologists blinded to the disease status of participants.
The increase is seen in only free sodium and seen in skin, but not muscle tissue, Dr. Linker said.
Using MRI spectroscopy with a powerful 7-Tesla magnet, Dr. Linker and his colleagues returned to the rodent EAE model, also finding increased sodium in the skin. Mass spectrometry findings were similar in other rodent autoimmune models, he said. The differences were not seen for sodium in other organs, or for potassium levels in the skin.
“The most difficult point,” Dr. Linker said, is “can we use this therapeutically somehow? Of course, you can put your patients on a salt-free or very low-salt diet, but it’s not very tasty, of course, and adherence would be probably very, very low.”
The microbiome may play a modulating role that adds to the sodium-MS story and provides a potential therapeutic option. In mice, a high-salt diet was associated with marked and rapid depletion of Lactobacillus species in the mouse gut microbiome. In healthy humans as well, the drop in lactobacilli was quick and profound when 6 g/day of salt was added to the diet, Dr. Linker said (P = .0053 versus the control diet of 2-4 g sodium/day).
Working backward with the same healthy cohort, repletion of Lactobacillus by probiotic supplementation normalized systolic blood pressure, which had become elevated with increased dietary sodium. Further, Lactobacillus repletion downregulated Th17 cells to levels seen before the high-sodium diet, even when dietary sodium stayed high.
“This was even transferred to multiple sclerosis,” in work recently published by another group, Dr. Linker said. For patients with MS who consumed a Lactobacillus-containing probiotic, investigators could “clearly show, besides effects on the microbiome itself, that there were effects on antigen-presenting cells in MS patients.” Intermediate monocytes decreased, as did dendritic cells, in the small study that involved both healthy controls and MS patients who received a probiotic and then underwent a washout period. Stool and blood samples were collected in both groups to compare values with and without probiotic administration.
A question from the audience looked back at historic data: 100 or more years ago, salt was used extensively for food preservation in many parts of the world, so dietary sodium intake is thought to have been higher. The incidence of MS, though, was lower then. Dr. Linker pointed out that food preservation practices varied widely, and that a host of other variables make assessment of past or present associations difficult. “It’s hard to argue that salt is the one and only risk factor; I would strongly doubt that.”
Still, he said, this early work invites more study, with a target of establishing whether probiotic supplementation could be used as “add-on therapy to established immune drugs.”
Dr. Linker has received honoraria and research support from Bayer, Biogen, Genzyme, Merck Serono, Novartis, and TEVA.
SOURCE: Linker R. ECTRIMS 2018, Scientific Session 7.
BERLIN – Among a host of potential risk factors for multiple sclerosis (MS), one emerging risk factor – dietary sodium – has accumulating evidence, bolstered by new imaging techniques and emerging research about the mediating effect of the gut microbiome.
“The word is still out on salt – there’s still some work to do; we are not where we stand with smoking or obesity” and the association with MS, said Ralf Linker, MD, speaking at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
For all potential emerging risk factors for MS, there’s an attractive hypothesis and, often, epidemiologic data, Dr. Linker said. “There are probably good [epidemiologic] data in multiple sclerosis for vitamin D, smoking, obesity, and probably also alcohol,” he said. “The therapeutic consequence, however, is much less clear, the best example of that being, of course, vitamin D.”
“The attractive risk factor is not enough to be a hypothesis, although some people seem to believe that nowadays,” said Dr. Linker, chair of the department of neurology at Friedrich-Alexander University, Erlangen, Germany. “Probably it’s better to start with some basic science and some experimental data to get an idea of the mechanism.”
“Today, we need clear associations with clear markers, well-defined cohorts, and proper epidemiological data telling us whether this is a real risk factor. ... If you look at the clinicians – and there are many among us in the room here – your ultimate goal, of course, is to use this as an intervention.”
For salt intake, there’s a clear overlap between high salt consumption in Westernized diets and increasing incidence of MS. The association also holds for many other autoimmune diseases, Dr. Linker added.
“The next step is experimental evidence,” Dr. Linker said. In a rodent model of experimental autoimmune encephalomyelitis (EAE), rats with high salt intake had a worse clinical course, compared with control rats fed a usual diet (Nature. 2013 Apr 25;496[7446]:518-22).
“There were a lot of follow-up studies on that,” with identification of multiple immune cells that are up- or down-regulated via distinct pathways in a high-salt environment, Dr. Linker said.
More recently, Dr. Linker was a coinvestigator in work showing that healthy humans placed on a high-salt diet had significant increases in T-helper 17 (Th17) cells after just 2 weeks of an additional 6 g of table salt daily over a baseline 2-4 g/day (Nature. 2017 Nov 30;551[7682]:585-9).
“You can also translate it to a more realistic setting,” where individuals who ate fast food four or more times weekly had significantly higher Th17 cell counts than did those who ate less fast food, he noted in reference to unpublished data.
Looking specifically at MS, a single-center study found that increased sodium intake correlated with increased MS clinical disease activity, with the highest sodium intake (more than 4.8 g/day) associated with higher incidence of MS exacerbations. Those in the highest tier of sodium intake also had a higher lesion load, with 3.65 more T2 lesions seen on MRI scans for each gram of salt consumed above average amounts of 2-4.8 g/day (J Neurol Neurosurg Psychiatry. 2015 Jan;86[1]:26-31).
On the other hand, Dr. Linker said, “There have been recent very well-conducted studies in very well-defined cohorts casting doubt on this translation to multiple sclerosis.” In particular, an examination of data from over 70,000 participants in the Nurse’s Health Study showed no association between MS risk and dietary salt assessed by a nutritional questionnaire (Neurology. 2017 Sep 26;89[13]:1322-9). “There was no hint that the diagnosis was linked in any way with salt exposure,” Dr. Linker said.
In the BENEFIT study, both a spot urine sample and a food questionnaire were used, and patients were grouped into quintiles of sodium intake. For demyelinating events and MS diagnosis, the curves for all quintiles were “completely overlapping,” with no sign of increased risk of MS with higher sodium intake (Ann Neurol. 2017;82:20-9).
An important caveat to the null findings in these analyses is the known poor agreement between self-report of salt intake and actual sodium load, Dr. Linker noted. Renal sodium excretion can vary widely despite fixed salt intake, so spot urine and even 24-hour urine collection don’t guarantee accuracy, he said, citing studies from space travel emulations that show wide day-to-day excursions in sodium excretion with a fixed diet.
A promising tool for accurate assessment of sodium load may be sodium-23 skin spectroscopy using MRI, because skin tissue binds sodium in a stable, nonosmotic fashion. Dr. Linker and his colleagues have recently found that skin sodium levels, measured at the calf, are higher in individuals with relapsing-remitting MS. “Indeed, the sodium level in the skin of the MS patients was significantly higher than in the controls” who did not have MS, he said of the study that matched 20 patients with MS with 20 healthy controls. The MRI studies were assessed by radiologists blinded to the disease status of participants.
The increase is seen in only free sodium and seen in skin, but not muscle tissue, Dr. Linker said.
Using MRI spectroscopy with a powerful 7-Tesla magnet, Dr. Linker and his colleagues returned to the rodent EAE model, also finding increased sodium in the skin. Mass spectrometry findings were similar in other rodent autoimmune models, he said. The differences were not seen for sodium in other organs, or for potassium levels in the skin.
“The most difficult point,” Dr. Linker said, is “can we use this therapeutically somehow? Of course, you can put your patients on a salt-free or very low-salt diet, but it’s not very tasty, of course, and adherence would be probably very, very low.”
The microbiome may play a modulating role that adds to the sodium-MS story and provides a potential therapeutic option. In mice, a high-salt diet was associated with marked and rapid depletion of Lactobacillus species in the mouse gut microbiome. In healthy humans as well, the drop in lactobacilli was quick and profound when 6 g/day of salt was added to the diet, Dr. Linker said (P = .0053 versus the control diet of 2-4 g sodium/day).
Working backward with the same healthy cohort, repletion of Lactobacillus by probiotic supplementation normalized systolic blood pressure, which had become elevated with increased dietary sodium. Further, Lactobacillus repletion downregulated Th17 cells to levels seen before the high-sodium diet, even when dietary sodium stayed high.
“This was even transferred to multiple sclerosis,” in work recently published by another group, Dr. Linker said. For patients with MS who consumed a Lactobacillus-containing probiotic, investigators could “clearly show, besides effects on the microbiome itself, that there were effects on antigen-presenting cells in MS patients.” Intermediate monocytes decreased, as did dendritic cells, in the small study that involved both healthy controls and MS patients who received a probiotic and then underwent a washout period. Stool and blood samples were collected in both groups to compare values with and without probiotic administration.
A question from the audience looked back at historic data: 100 or more years ago, salt was used extensively for food preservation in many parts of the world, so dietary sodium intake is thought to have been higher. The incidence of MS, though, was lower then. Dr. Linker pointed out that food preservation practices varied widely, and that a host of other variables make assessment of past or present associations difficult. “It’s hard to argue that salt is the one and only risk factor; I would strongly doubt that.”
Still, he said, this early work invites more study, with a target of establishing whether probiotic supplementation could be used as “add-on therapy to established immune drugs.”
Dr. Linker has received honoraria and research support from Bayer, Biogen, Genzyme, Merck Serono, Novartis, and TEVA.
SOURCE: Linker R. ECTRIMS 2018, Scientific Session 7.
EXPERT ANALYSIS FROM ECTRIMS 2018
Breastfeeding with MS: Good for mom, too
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
REPORTING FROM ECTRIMS 2018
True postbariatric hyperinsulinemic hypoglycemia is rare
based on a decade’s worth of experience from the Mayo Clinic, Rochester, Minn.
Of 2,386 patients who had bariatric surgery at Mayo, 60 (2.6%) had a postsurgical diagnosis code associated with hypoglycemia in their medical record. However, just five of them (0.25%) had documentation meeting the criteria for Whipple’s Triad, which consists of low blood glucose levels, symptoms associated with the low glucose levels, and symptom resolution when glucose levels are corrected, Tiffany Cortes, MD, reported in an oral presentation at Obesity Week, which is presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery .
“Postbariatric hypoglycemia is an infrequent occurrence among patients who present with suspicious symptoms,” said Dr. Cortes, an endocrinology fellow at the clinic.
Post–bariatric surgery hypoglycemia is characterized by neuroglycopenia with a documented plasma glucose of less than 54 mg/dL with symptom resolution after a rise in glucose levels; neuroglycopenia that occurs 1-3 hours after a meal; and symptom onset more than 6 months after bariatric surgery, said Dr. Cortes.
Previous work had found that the overall prevalence of post–bariatric surgery hyperinsulinemic hypoglycemia ranged from 17%-34%, with severe symptoms seen in fewer than 1% of surgery recipients.
Bariatric surgery, especially Roux-en-Y gastric bypass (RYGB), may result in wide postprandial blood glucose excursions, with a spike occurring about 30 minutes after eating. For symptomatic individuals, this postprandial glucose peak will prompt an insulin surge followed by a rapid and steep decline in serum glucose.
Looking at Mayo Clinic medical records from mid-2008 to the end of 2017, Dr. Cortes and her colleagues wanted to determine the prevalence of hyperinsulinemic hypoglycemia in the bariatric surgery population.
Additionally, the researchers wanted to see how patients who presented with symptoms suspicious for the syndrome were evaluated and to understand the efficacy of treatments.
Patients who had a diagnosis of type 1 diabetes mellitus and those who were on insulin or sulfonylureas were excluded from the retrospective chart review.
Of the 60 patients evaluated in the endocrinology clinic for symptoms suspicious for hyperinsulinemic hypoglycemia, 51 (85%) were female, and 14 had a diagnosis of diabetes before surgery. Mean patient age at surgery was 43 years.
These symptomatic patients had a mean presurgical body mass index (BMI) of 42.8 kg/m2 (range, 38.6-49.3 kg/m2). Their mean time to maximal weight loss was 1.3 years after surgery, with symptoms beginning at 1.4 years after surgery. Patients lost a mean 37.4% of their body mass to reach a mean nadir BMI of 26.2.
Overall, about two-thirds of the surgeries performed were RYGB. Of patients with hypoglycemic symptoms, 73.3% had an RYGB. Revision of gastric bypass was the next most common surgery, at 21.8% overall; these patients constituted 15% of the hypoglycemic symptom group.
Of the patients with symptoms, 80% noted symptoms only after eating, with half of patients describing symptoms coming on 1-3 hours after eating. A little over a third of the patients didn’t describe the exact timing of symptoms.
Just 20 patients had a complete hypoglycemia work up bundle documented in their medical record, said Dr. Cortes. This consisted of measures of serum glucose, insulin, and C-peptide levels. Of the 20 patients, 5 met Whipple’s Triad criteria, and 4 of these patients received a diagnosis of hyperinsulinemic hypoglycemia.
Two patients had a 72-hour fast, and neither of them met diagnostic criteria. Seventeen patients had a mixed meal tolerance test, with one individual meeting diagnostic criteria for and receiving a diagnosis of hypoinsulinemic hyperglycemia.
Of the five patients meeting diagnostic criteria (0.20% of surgical population), all had received RYGB, and two had previous weight loss procedures, said Dr. Cortes. For four of the patients, the surgical indication was weight loss; the other patient had an indication of gastroesophageal reflux disease (GERD).
“Dietary interventions are the most effective treatment” for post–bariatric surgery hyperinsulinemic hypoglycemia in the Mayo Clinic experience, said Dr. Cortes.
Turning to the investigators’ examination of treatment recommendations for the 60 patients who reported hypoglycemic symptoms, most (95%) received an initial recommendation to manage symptoms by diet changes.
Most patients (77%) had at least one follow-up visit, with over half of these patients (61%) reporting improvement in symptoms, and seven patients (16%) reporting resolution. Twelve patients (27%) either remained the same or had not had a recurrence of symptoms.
Medication was prescribed for 12 patients; of them, 8 received the alpha glucosidase inhibitor acarbose and 7 responded, according to the record review. No one reported worsening of symptoms on acarbose.
Other individual patients were prescribed octreotide alone, or octreotide, pasireotide, or diazoxide in combination with acarbose, with variable results.
Dr. Cortes reported no conflicts of interest and no external sources of funding.
SOURCE: Cortes T et al. Obesity Week 2018, Abstract T-OR-2015.
based on a decade’s worth of experience from the Mayo Clinic, Rochester, Minn.
Of 2,386 patients who had bariatric surgery at Mayo, 60 (2.6%) had a postsurgical diagnosis code associated with hypoglycemia in their medical record. However, just five of them (0.25%) had documentation meeting the criteria for Whipple’s Triad, which consists of low blood glucose levels, symptoms associated with the low glucose levels, and symptom resolution when glucose levels are corrected, Tiffany Cortes, MD, reported in an oral presentation at Obesity Week, which is presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery .
“Postbariatric hypoglycemia is an infrequent occurrence among patients who present with suspicious symptoms,” said Dr. Cortes, an endocrinology fellow at the clinic.
Post–bariatric surgery hypoglycemia is characterized by neuroglycopenia with a documented plasma glucose of less than 54 mg/dL with symptom resolution after a rise in glucose levels; neuroglycopenia that occurs 1-3 hours after a meal; and symptom onset more than 6 months after bariatric surgery, said Dr. Cortes.
Previous work had found that the overall prevalence of post–bariatric surgery hyperinsulinemic hypoglycemia ranged from 17%-34%, with severe symptoms seen in fewer than 1% of surgery recipients.
Bariatric surgery, especially Roux-en-Y gastric bypass (RYGB), may result in wide postprandial blood glucose excursions, with a spike occurring about 30 minutes after eating. For symptomatic individuals, this postprandial glucose peak will prompt an insulin surge followed by a rapid and steep decline in serum glucose.
Looking at Mayo Clinic medical records from mid-2008 to the end of 2017, Dr. Cortes and her colleagues wanted to determine the prevalence of hyperinsulinemic hypoglycemia in the bariatric surgery population.
Additionally, the researchers wanted to see how patients who presented with symptoms suspicious for the syndrome were evaluated and to understand the efficacy of treatments.
Patients who had a diagnosis of type 1 diabetes mellitus and those who were on insulin or sulfonylureas were excluded from the retrospective chart review.
Of the 60 patients evaluated in the endocrinology clinic for symptoms suspicious for hyperinsulinemic hypoglycemia, 51 (85%) were female, and 14 had a diagnosis of diabetes before surgery. Mean patient age at surgery was 43 years.
These symptomatic patients had a mean presurgical body mass index (BMI) of 42.8 kg/m2 (range, 38.6-49.3 kg/m2). Their mean time to maximal weight loss was 1.3 years after surgery, with symptoms beginning at 1.4 years after surgery. Patients lost a mean 37.4% of their body mass to reach a mean nadir BMI of 26.2.
Overall, about two-thirds of the surgeries performed were RYGB. Of patients with hypoglycemic symptoms, 73.3% had an RYGB. Revision of gastric bypass was the next most common surgery, at 21.8% overall; these patients constituted 15% of the hypoglycemic symptom group.
Of the patients with symptoms, 80% noted symptoms only after eating, with half of patients describing symptoms coming on 1-3 hours after eating. A little over a third of the patients didn’t describe the exact timing of symptoms.
Just 20 patients had a complete hypoglycemia work up bundle documented in their medical record, said Dr. Cortes. This consisted of measures of serum glucose, insulin, and C-peptide levels. Of the 20 patients, 5 met Whipple’s Triad criteria, and 4 of these patients received a diagnosis of hyperinsulinemic hypoglycemia.
Two patients had a 72-hour fast, and neither of them met diagnostic criteria. Seventeen patients had a mixed meal tolerance test, with one individual meeting diagnostic criteria for and receiving a diagnosis of hypoinsulinemic hyperglycemia.
Of the five patients meeting diagnostic criteria (0.20% of surgical population), all had received RYGB, and two had previous weight loss procedures, said Dr. Cortes. For four of the patients, the surgical indication was weight loss; the other patient had an indication of gastroesophageal reflux disease (GERD).
“Dietary interventions are the most effective treatment” for post–bariatric surgery hyperinsulinemic hypoglycemia in the Mayo Clinic experience, said Dr. Cortes.
Turning to the investigators’ examination of treatment recommendations for the 60 patients who reported hypoglycemic symptoms, most (95%) received an initial recommendation to manage symptoms by diet changes.
Most patients (77%) had at least one follow-up visit, with over half of these patients (61%) reporting improvement in symptoms, and seven patients (16%) reporting resolution. Twelve patients (27%) either remained the same or had not had a recurrence of symptoms.
Medication was prescribed for 12 patients; of them, 8 received the alpha glucosidase inhibitor acarbose and 7 responded, according to the record review. No one reported worsening of symptoms on acarbose.
Other individual patients were prescribed octreotide alone, or octreotide, pasireotide, or diazoxide in combination with acarbose, with variable results.
Dr. Cortes reported no conflicts of interest and no external sources of funding.
SOURCE: Cortes T et al. Obesity Week 2018, Abstract T-OR-2015.
based on a decade’s worth of experience from the Mayo Clinic, Rochester, Minn.
Of 2,386 patients who had bariatric surgery at Mayo, 60 (2.6%) had a postsurgical diagnosis code associated with hypoglycemia in their medical record. However, just five of them (0.25%) had documentation meeting the criteria for Whipple’s Triad, which consists of low blood glucose levels, symptoms associated with the low glucose levels, and symptom resolution when glucose levels are corrected, Tiffany Cortes, MD, reported in an oral presentation at Obesity Week, which is presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery .
“Postbariatric hypoglycemia is an infrequent occurrence among patients who present with suspicious symptoms,” said Dr. Cortes, an endocrinology fellow at the clinic.
Post–bariatric surgery hypoglycemia is characterized by neuroglycopenia with a documented plasma glucose of less than 54 mg/dL with symptom resolution after a rise in glucose levels; neuroglycopenia that occurs 1-3 hours after a meal; and symptom onset more than 6 months after bariatric surgery, said Dr. Cortes.
Previous work had found that the overall prevalence of post–bariatric surgery hyperinsulinemic hypoglycemia ranged from 17%-34%, with severe symptoms seen in fewer than 1% of surgery recipients.
Bariatric surgery, especially Roux-en-Y gastric bypass (RYGB), may result in wide postprandial blood glucose excursions, with a spike occurring about 30 minutes after eating. For symptomatic individuals, this postprandial glucose peak will prompt an insulin surge followed by a rapid and steep decline in serum glucose.
Looking at Mayo Clinic medical records from mid-2008 to the end of 2017, Dr. Cortes and her colleagues wanted to determine the prevalence of hyperinsulinemic hypoglycemia in the bariatric surgery population.
Additionally, the researchers wanted to see how patients who presented with symptoms suspicious for the syndrome were evaluated and to understand the efficacy of treatments.
Patients who had a diagnosis of type 1 diabetes mellitus and those who were on insulin or sulfonylureas were excluded from the retrospective chart review.
Of the 60 patients evaluated in the endocrinology clinic for symptoms suspicious for hyperinsulinemic hypoglycemia, 51 (85%) were female, and 14 had a diagnosis of diabetes before surgery. Mean patient age at surgery was 43 years.
These symptomatic patients had a mean presurgical body mass index (BMI) of 42.8 kg/m2 (range, 38.6-49.3 kg/m2). Their mean time to maximal weight loss was 1.3 years after surgery, with symptoms beginning at 1.4 years after surgery. Patients lost a mean 37.4% of their body mass to reach a mean nadir BMI of 26.2.
Overall, about two-thirds of the surgeries performed were RYGB. Of patients with hypoglycemic symptoms, 73.3% had an RYGB. Revision of gastric bypass was the next most common surgery, at 21.8% overall; these patients constituted 15% of the hypoglycemic symptom group.
Of the patients with symptoms, 80% noted symptoms only after eating, with half of patients describing symptoms coming on 1-3 hours after eating. A little over a third of the patients didn’t describe the exact timing of symptoms.
Just 20 patients had a complete hypoglycemia work up bundle documented in their medical record, said Dr. Cortes. This consisted of measures of serum glucose, insulin, and C-peptide levels. Of the 20 patients, 5 met Whipple’s Triad criteria, and 4 of these patients received a diagnosis of hyperinsulinemic hypoglycemia.
Two patients had a 72-hour fast, and neither of them met diagnostic criteria. Seventeen patients had a mixed meal tolerance test, with one individual meeting diagnostic criteria for and receiving a diagnosis of hypoinsulinemic hyperglycemia.
Of the five patients meeting diagnostic criteria (0.20% of surgical population), all had received RYGB, and two had previous weight loss procedures, said Dr. Cortes. For four of the patients, the surgical indication was weight loss; the other patient had an indication of gastroesophageal reflux disease (GERD).
“Dietary interventions are the most effective treatment” for post–bariatric surgery hyperinsulinemic hypoglycemia in the Mayo Clinic experience, said Dr. Cortes.
Turning to the investigators’ examination of treatment recommendations for the 60 patients who reported hypoglycemic symptoms, most (95%) received an initial recommendation to manage symptoms by diet changes.
Most patients (77%) had at least one follow-up visit, with over half of these patients (61%) reporting improvement in symptoms, and seven patients (16%) reporting resolution. Twelve patients (27%) either remained the same or had not had a recurrence of symptoms.
Medication was prescribed for 12 patients; of them, 8 received the alpha glucosidase inhibitor acarbose and 7 responded, according to the record review. No one reported worsening of symptoms on acarbose.
Other individual patients were prescribed octreotide alone, or octreotide, pasireotide, or diazoxide in combination with acarbose, with variable results.
Dr. Cortes reported no conflicts of interest and no external sources of funding.
SOURCE: Cortes T et al. Obesity Week 2018, Abstract T-OR-2015.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Less than 1% of bariatric surgery patients had hyperinsulinemic hypoglycemia.
Major finding: When strict diagnostic criteria were used, 0.20% received the diagnosis.
Study details: Single-center retrospective chart review of 2,386 patients receiving bariatric surgery.
Disclosures: Dr. Cortes reported no outside sources of funding and no conflicts of interest.
Source: Cortes T et al. Obesity Week 2018, Abstract T-OR-2015.
Heart disease remains the leading cause of death in U.S.
The 10 leading causes of death in the United States remained unchanged over the past year, according to a new report from the Centers for Disease Control (CDC). Though life expectancy at birth decreased to 78.6 years in 2017, down from 78.7 years in 2016, that change was driven primarily by suicide and drug overdose.
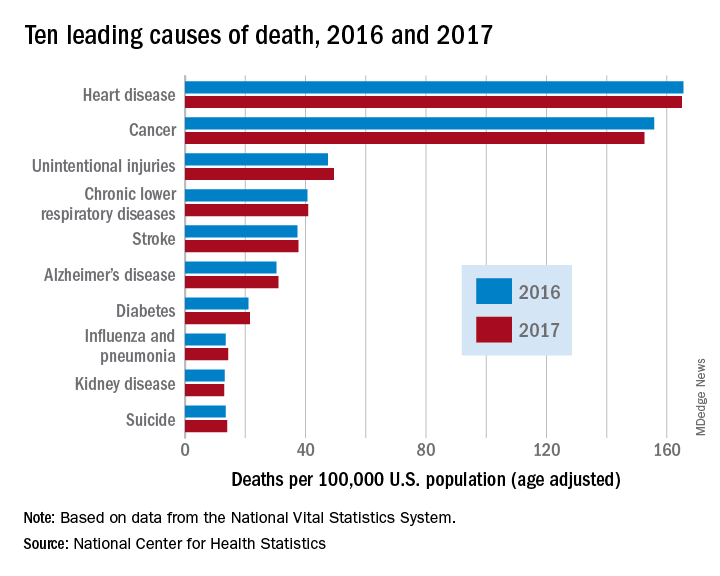
However, heart disease remains the leading cause of death in the United States, at 165 deaths per 100,000 individuals in 2017. This represents a slight, statistically nonsignificant, decrease from the 165.5 deaths per 100,000 caused by heart disease in the previous year.
Other diseases related to cardiometabolic health saw increases. Stroke and diabetes each caused a small but significant increase in deaths in 2017, which saw a 1-year increase to 37.6 from 37.3 stroke deaths per 100,000 people. Diabetes deaths increased to 21.5 from 21 per 100,000 the previous year. Stroke was the fifth and diabetes the seventh most common cause of death, according to the data brief published by the CDC’s National Center for Health Statistics (NCHS).
Alzheimer’s disease deaths also increased significantly, from 30.3 per 100,000 in 2016 to 31 per 100,000 in 2017. Although Alzheimer’s exact etiology remains under study, cardiovascular disease factors and Alzheimer’s disease share many risk factors and are often comorbid .
“With a slight decrease in deaths from heart disease in 2017 and a slight increase in deaths from stroke, this lack of any major movement in these areas has been a trend we’ve seen the last couple of years,” said Ivor Benjamin, MD, president of the American Heart Association, in a press release. “It is discouraging after experiencing decades when heart disease and stroke death rates both dropped more dramatically.”
Infant deaths from congenital malformations decreased from 2016 to 2017, from 122.1 to 118.8 deaths per 100,000 live births. “While the report doesn’t specify death rates for specific types of congenital malformations, this is heartening news as it could reflect fewer deaths from congenital heart defects,” said the AHA in its release.
According to the CDC, the 10 leading causes of death together account for about three quarters of United States deaths. Cancer caused nearly as many deaths as heart disease – 152.5 per 100,000. This represented a significant decrease from the 155.8 cancer deaths per 100,000 seen in 2016. The remaining top 10 causes of death, in decreasing order, were unintentional injuries, chronic lower respiratory diseases, influenza and pneumonia, kidney disease, and suicide.
The 10 leading causes of death in the United States remained unchanged over the past year, according to a new report from the Centers for Disease Control (CDC). Though life expectancy at birth decreased to 78.6 years in 2017, down from 78.7 years in 2016, that change was driven primarily by suicide and drug overdose.
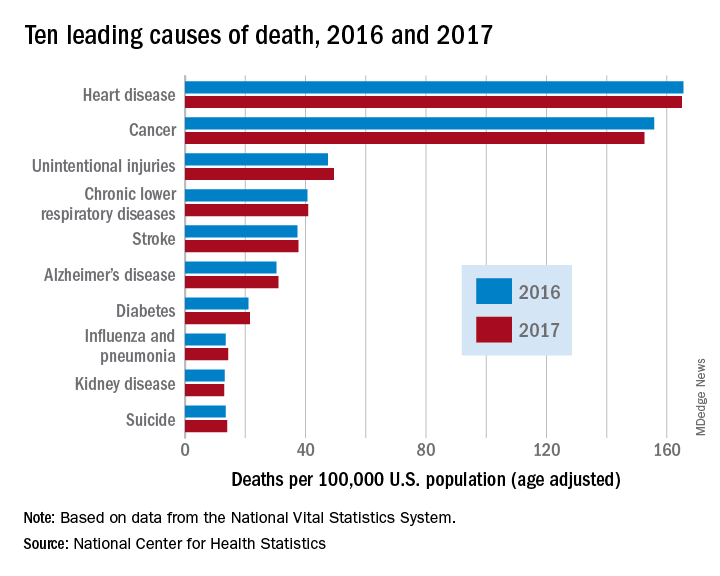
However, heart disease remains the leading cause of death in the United States, at 165 deaths per 100,000 individuals in 2017. This represents a slight, statistically nonsignificant, decrease from the 165.5 deaths per 100,000 caused by heart disease in the previous year.
Other diseases related to cardiometabolic health saw increases. Stroke and diabetes each caused a small but significant increase in deaths in 2017, which saw a 1-year increase to 37.6 from 37.3 stroke deaths per 100,000 people. Diabetes deaths increased to 21.5 from 21 per 100,000 the previous year. Stroke was the fifth and diabetes the seventh most common cause of death, according to the data brief published by the CDC’s National Center for Health Statistics (NCHS).
Alzheimer’s disease deaths also increased significantly, from 30.3 per 100,000 in 2016 to 31 per 100,000 in 2017. Although Alzheimer’s exact etiology remains under study, cardiovascular disease factors and Alzheimer’s disease share many risk factors and are often comorbid .
“With a slight decrease in deaths from heart disease in 2017 and a slight increase in deaths from stroke, this lack of any major movement in these areas has been a trend we’ve seen the last couple of years,” said Ivor Benjamin, MD, president of the American Heart Association, in a press release. “It is discouraging after experiencing decades when heart disease and stroke death rates both dropped more dramatically.”
Infant deaths from congenital malformations decreased from 2016 to 2017, from 122.1 to 118.8 deaths per 100,000 live births. “While the report doesn’t specify death rates for specific types of congenital malformations, this is heartening news as it could reflect fewer deaths from congenital heart defects,” said the AHA in its release.
According to the CDC, the 10 leading causes of death together account for about three quarters of United States deaths. Cancer caused nearly as many deaths as heart disease – 152.5 per 100,000. This represented a significant decrease from the 155.8 cancer deaths per 100,000 seen in 2016. The remaining top 10 causes of death, in decreasing order, were unintentional injuries, chronic lower respiratory diseases, influenza and pneumonia, kidney disease, and suicide.
The 10 leading causes of death in the United States remained unchanged over the past year, according to a new report from the Centers for Disease Control (CDC). Though life expectancy at birth decreased to 78.6 years in 2017, down from 78.7 years in 2016, that change was driven primarily by suicide and drug overdose.
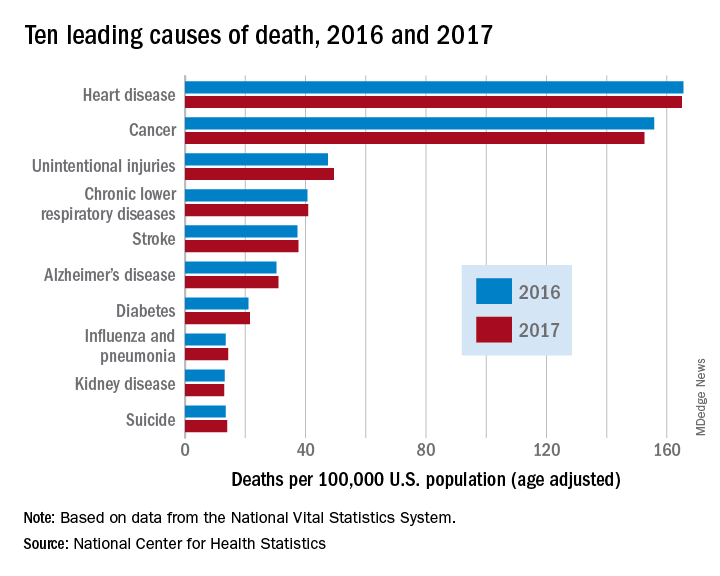
However, heart disease remains the leading cause of death in the United States, at 165 deaths per 100,000 individuals in 2017. This represents a slight, statistically nonsignificant, decrease from the 165.5 deaths per 100,000 caused by heart disease in the previous year.
Other diseases related to cardiometabolic health saw increases. Stroke and diabetes each caused a small but significant increase in deaths in 2017, which saw a 1-year increase to 37.6 from 37.3 stroke deaths per 100,000 people. Diabetes deaths increased to 21.5 from 21 per 100,000 the previous year. Stroke was the fifth and diabetes the seventh most common cause of death, according to the data brief published by the CDC’s National Center for Health Statistics (NCHS).
Alzheimer’s disease deaths also increased significantly, from 30.3 per 100,000 in 2016 to 31 per 100,000 in 2017. Although Alzheimer’s exact etiology remains under study, cardiovascular disease factors and Alzheimer’s disease share many risk factors and are often comorbid .
“With a slight decrease in deaths from heart disease in 2017 and a slight increase in deaths from stroke, this lack of any major movement in these areas has been a trend we’ve seen the last couple of years,” said Ivor Benjamin, MD, president of the American Heart Association, in a press release. “It is discouraging after experiencing decades when heart disease and stroke death rates both dropped more dramatically.”
Infant deaths from congenital malformations decreased from 2016 to 2017, from 122.1 to 118.8 deaths per 100,000 live births. “While the report doesn’t specify death rates for specific types of congenital malformations, this is heartening news as it could reflect fewer deaths from congenital heart defects,” said the AHA in its release.
According to the CDC, the 10 leading causes of death together account for about three quarters of United States deaths. Cancer caused nearly as many deaths as heart disease – 152.5 per 100,000. This represented a significant decrease from the 155.8 cancer deaths per 100,000 seen in 2016. The remaining top 10 causes of death, in decreasing order, were unintentional injuries, chronic lower respiratory diseases, influenza and pneumonia, kidney disease, and suicide.
FROM A CDC DATA BRIEF
U.S. life expectancy down; drug overdose, suicide up sharply
Average life expectancy fell in the United States fell from 78.7 years to 78.6 years from 2016 to 2017, according to a new report on the nation’s health. The decrease is primarily attributable to increases in suicide and drug overdose rates, according to new data from the Centers for Disease Control (CDC).
“The latest CDC data show that the U.S. life expectancy has declined over the past few years. Tragically, this troubling trend is largely driven by deaths from drug overdose and suicide,” said CDC Director Robert Redfield, MD, in a statement.
Two subreports that looked specifically at suicide mortality and drug overdose deaths mapped out where, when, and for whom the sharpest increases in mortality are being seen.
For suicide, though rates have increased by 33% overall for both men and women since 1999, the greatest annual increases in suicide rates have happened since 2006, according to a new report from the CDC’s National Center for Health Statistics (NCHS).
Overall, suicide rates have climbed from 10.5 to 14.0 per 100,000 individuals, with statistically significant increases in suicide rates among all age groups except those aged 75 years and older.
Suicide rates rose more steeply in the most rural counties. The age-adjusted increase in the most rural counties was 53%, compared with an increase of 16% in suicide rates for the nation’s most urban counties over the 1999-2017 time period.
Over the entire period studied, men were more likely than women to experience suicide, as rates rose among most age groups. For example, the rates of suicide for men aged 15-24 years rose from 16.8 to 22.7 per 100,000; for women in that age group, suicide rates went from 3.0 to 5.8 per 100,000.
Though suicide has remained the 10th leading cause of death overall in the United States, suicide was the second leading cause of death for adolescents and young adults (aged 10-34) in 2016, and the fourth leading cause of death for those aged 35-54 in that year.
These increases come despite a goal set by the CDC and a national coalition of health partners to reduce suicide rates to 10.2 per 100,000 by 2020, as part of the Healthy People 2020 initiative, noted Molly Hedegaard, MD, of NCHS, and her coauthors, in the suicide mortality data briefing.
Drug overdoses increased by nearly 10% in one year, with the highest rates seen in adults aged 25-54 years, according to a second CDC data briefing.
The number of people who died of drug overdoses in the United States in 2017 was 70,237. This represents a year-over-year age-adjusted increase of 9.6%, from 19.8 to 21.7 per 100,000 individuals, said Dr. Hedegaard and the coauthors of the drug overdose mortality report.
Reflecting known national trends in opioid use disorder, age-adjusted drug overdose deaths were highest in the states of West Virginia, Ohio, and Pennsylvania, where rates were 57.8, 46.3, and 44.3 per 100,000 residents, respectively. The District of Columbia had the fourth-highest age adjusted drug overdose death rate, at 44 per 100,000.
Twenty states, clustered primarily in the Eastern half of the United States, “had age-adjusted drug overdose death rate that were statistically higher than the national rate,” wrote Dr. Hedegaard and her coauthors.
Compared with 1999, more than six times as many adults in older midlife (aged 55-64 years) died from drug overdoses in 2017 (4.2 versus 28 per 100,000).
Adults aged 25-34 years, 35-44 years, and 45-54 years also had significant increases in drug overdose rates; in 2017, rates were 38.4, 29, and 37.7 per 100,000, respectively. Adolescent and young adults died from drug overdoses at a rate of 12.6 per 100,000, and those over 65 years old had a death rate of 6.9 per 100,000.
Deaths attributable to synthetic opioid use, excluding methadone, rose by 45% in just one year, going from 6.2 to 9.0 per 100,000 nationally. In 1999, synthetic opioids other than methadone were implicated in just 0.3 per 100,000 deaths. Synthetic opioids include fentanyl and fentanyl analogs, such as carfentanyl.
Deaths involving heroin remained stable from 2016 to 2017, at 4.9 per 100,000. Deaths attributable to natural and semisynthetic prescription opioids, such as oxycodone and hydrocodone, also were the same in 2017 as 2016, at 4.4 per 100,000.
Looking at trends over time since 1999, the rate of increase in drug overdose deaths had risen slowly since 1999 and stabilized in the mid-2000s. However, beginning in 2012, rates have increased steeply, particularly for males.
“Male rates were significantly higher than female rates for all years,” reported Dr. Hedegaard and her coauthors (P less than .05). Though female drug overdose death rates have climbed from 3.9 to 14.4 per 100,000 since 1999, the male death rate has gone from 8.2 to 29.1 per 100,000 during the study period.
“Life expectancy gives us a snapshot of the nation’s overall health and these sobering statistics are a wakeup call that we are losing too many Americans, too early and too often, to conditions that are preventable. CDC is committed to putting science into action to protect U.S. health, but we must all work together to reverse this trend and help ensure that all Americans live longer and healthier lives,” said Dr. Redfield.
Average life expectancy fell in the United States fell from 78.7 years to 78.6 years from 2016 to 2017, according to a new report on the nation’s health. The decrease is primarily attributable to increases in suicide and drug overdose rates, according to new data from the Centers for Disease Control (CDC).
“The latest CDC data show that the U.S. life expectancy has declined over the past few years. Tragically, this troubling trend is largely driven by deaths from drug overdose and suicide,” said CDC Director Robert Redfield, MD, in a statement.
Two subreports that looked specifically at suicide mortality and drug overdose deaths mapped out where, when, and for whom the sharpest increases in mortality are being seen.
For suicide, though rates have increased by 33% overall for both men and women since 1999, the greatest annual increases in suicide rates have happened since 2006, according to a new report from the CDC’s National Center for Health Statistics (NCHS).
Overall, suicide rates have climbed from 10.5 to 14.0 per 100,000 individuals, with statistically significant increases in suicide rates among all age groups except those aged 75 years and older.
Suicide rates rose more steeply in the most rural counties. The age-adjusted increase in the most rural counties was 53%, compared with an increase of 16% in suicide rates for the nation’s most urban counties over the 1999-2017 time period.
Over the entire period studied, men were more likely than women to experience suicide, as rates rose among most age groups. For example, the rates of suicide for men aged 15-24 years rose from 16.8 to 22.7 per 100,000; for women in that age group, suicide rates went from 3.0 to 5.8 per 100,000.
Though suicide has remained the 10th leading cause of death overall in the United States, suicide was the second leading cause of death for adolescents and young adults (aged 10-34) in 2016, and the fourth leading cause of death for those aged 35-54 in that year.
These increases come despite a goal set by the CDC and a national coalition of health partners to reduce suicide rates to 10.2 per 100,000 by 2020, as part of the Healthy People 2020 initiative, noted Molly Hedegaard, MD, of NCHS, and her coauthors, in the suicide mortality data briefing.
Drug overdoses increased by nearly 10% in one year, with the highest rates seen in adults aged 25-54 years, according to a second CDC data briefing.
The number of people who died of drug overdoses in the United States in 2017 was 70,237. This represents a year-over-year age-adjusted increase of 9.6%, from 19.8 to 21.7 per 100,000 individuals, said Dr. Hedegaard and the coauthors of the drug overdose mortality report.
Reflecting known national trends in opioid use disorder, age-adjusted drug overdose deaths were highest in the states of West Virginia, Ohio, and Pennsylvania, where rates were 57.8, 46.3, and 44.3 per 100,000 residents, respectively. The District of Columbia had the fourth-highest age adjusted drug overdose death rate, at 44 per 100,000.
Twenty states, clustered primarily in the Eastern half of the United States, “had age-adjusted drug overdose death rate that were statistically higher than the national rate,” wrote Dr. Hedegaard and her coauthors.
Compared with 1999, more than six times as many adults in older midlife (aged 55-64 years) died from drug overdoses in 2017 (4.2 versus 28 per 100,000).
Adults aged 25-34 years, 35-44 years, and 45-54 years also had significant increases in drug overdose rates; in 2017, rates were 38.4, 29, and 37.7 per 100,000, respectively. Adolescent and young adults died from drug overdoses at a rate of 12.6 per 100,000, and those over 65 years old had a death rate of 6.9 per 100,000.
Deaths attributable to synthetic opioid use, excluding methadone, rose by 45% in just one year, going from 6.2 to 9.0 per 100,000 nationally. In 1999, synthetic opioids other than methadone were implicated in just 0.3 per 100,000 deaths. Synthetic opioids include fentanyl and fentanyl analogs, such as carfentanyl.
Deaths involving heroin remained stable from 2016 to 2017, at 4.9 per 100,000. Deaths attributable to natural and semisynthetic prescription opioids, such as oxycodone and hydrocodone, also were the same in 2017 as 2016, at 4.4 per 100,000.
Looking at trends over time since 1999, the rate of increase in drug overdose deaths had risen slowly since 1999 and stabilized in the mid-2000s. However, beginning in 2012, rates have increased steeply, particularly for males.
“Male rates were significantly higher than female rates for all years,” reported Dr. Hedegaard and her coauthors (P less than .05). Though female drug overdose death rates have climbed from 3.9 to 14.4 per 100,000 since 1999, the male death rate has gone from 8.2 to 29.1 per 100,000 during the study period.
“Life expectancy gives us a snapshot of the nation’s overall health and these sobering statistics are a wakeup call that we are losing too many Americans, too early and too often, to conditions that are preventable. CDC is committed to putting science into action to protect U.S. health, but we must all work together to reverse this trend and help ensure that all Americans live longer and healthier lives,” said Dr. Redfield.
Average life expectancy fell in the United States fell from 78.7 years to 78.6 years from 2016 to 2017, according to a new report on the nation’s health. The decrease is primarily attributable to increases in suicide and drug overdose rates, according to new data from the Centers for Disease Control (CDC).
“The latest CDC data show that the U.S. life expectancy has declined over the past few years. Tragically, this troubling trend is largely driven by deaths from drug overdose and suicide,” said CDC Director Robert Redfield, MD, in a statement.
Two subreports that looked specifically at suicide mortality and drug overdose deaths mapped out where, when, and for whom the sharpest increases in mortality are being seen.
For suicide, though rates have increased by 33% overall for both men and women since 1999, the greatest annual increases in suicide rates have happened since 2006, according to a new report from the CDC’s National Center for Health Statistics (NCHS).
Overall, suicide rates have climbed from 10.5 to 14.0 per 100,000 individuals, with statistically significant increases in suicide rates among all age groups except those aged 75 years and older.
Suicide rates rose more steeply in the most rural counties. The age-adjusted increase in the most rural counties was 53%, compared with an increase of 16% in suicide rates for the nation’s most urban counties over the 1999-2017 time period.
Over the entire period studied, men were more likely than women to experience suicide, as rates rose among most age groups. For example, the rates of suicide for men aged 15-24 years rose from 16.8 to 22.7 per 100,000; for women in that age group, suicide rates went from 3.0 to 5.8 per 100,000.
Though suicide has remained the 10th leading cause of death overall in the United States, suicide was the second leading cause of death for adolescents and young adults (aged 10-34) in 2016, and the fourth leading cause of death for those aged 35-54 in that year.
These increases come despite a goal set by the CDC and a national coalition of health partners to reduce suicide rates to 10.2 per 100,000 by 2020, as part of the Healthy People 2020 initiative, noted Molly Hedegaard, MD, of NCHS, and her coauthors, in the suicide mortality data briefing.
Drug overdoses increased by nearly 10% in one year, with the highest rates seen in adults aged 25-54 years, according to a second CDC data briefing.
The number of people who died of drug overdoses in the United States in 2017 was 70,237. This represents a year-over-year age-adjusted increase of 9.6%, from 19.8 to 21.7 per 100,000 individuals, said Dr. Hedegaard and the coauthors of the drug overdose mortality report.
Reflecting known national trends in opioid use disorder, age-adjusted drug overdose deaths were highest in the states of West Virginia, Ohio, and Pennsylvania, where rates were 57.8, 46.3, and 44.3 per 100,000 residents, respectively. The District of Columbia had the fourth-highest age adjusted drug overdose death rate, at 44 per 100,000.
Twenty states, clustered primarily in the Eastern half of the United States, “had age-adjusted drug overdose death rate that were statistically higher than the national rate,” wrote Dr. Hedegaard and her coauthors.
Compared with 1999, more than six times as many adults in older midlife (aged 55-64 years) died from drug overdoses in 2017 (4.2 versus 28 per 100,000).
Adults aged 25-34 years, 35-44 years, and 45-54 years also had significant increases in drug overdose rates; in 2017, rates were 38.4, 29, and 37.7 per 100,000, respectively. Adolescent and young adults died from drug overdoses at a rate of 12.6 per 100,000, and those over 65 years old had a death rate of 6.9 per 100,000.
Deaths attributable to synthetic opioid use, excluding methadone, rose by 45% in just one year, going from 6.2 to 9.0 per 100,000 nationally. In 1999, synthetic opioids other than methadone were implicated in just 0.3 per 100,000 deaths. Synthetic opioids include fentanyl and fentanyl analogs, such as carfentanyl.
Deaths involving heroin remained stable from 2016 to 2017, at 4.9 per 100,000. Deaths attributable to natural and semisynthetic prescription opioids, such as oxycodone and hydrocodone, also were the same in 2017 as 2016, at 4.4 per 100,000.
Looking at trends over time since 1999, the rate of increase in drug overdose deaths had risen slowly since 1999 and stabilized in the mid-2000s. However, beginning in 2012, rates have increased steeply, particularly for males.
“Male rates were significantly higher than female rates for all years,” reported Dr. Hedegaard and her coauthors (P less than .05). Though female drug overdose death rates have climbed from 3.9 to 14.4 per 100,000 since 1999, the male death rate has gone from 8.2 to 29.1 per 100,000 during the study period.
“Life expectancy gives us a snapshot of the nation’s overall health and these sobering statistics are a wakeup call that we are losing too many Americans, too early and too often, to conditions that are preventable. CDC is committed to putting science into action to protect U.S. health, but we must all work together to reverse this trend and help ensure that all Americans live longer and healthier lives,” said Dr. Redfield.
Physical activity may count more for women who keep the pounds off
NASHVILLE – , according to new analysis of a small study.
Physical activity is a key component in successful maintenance of weight loss, but differential effects of physical activity between men and women had not been well explored, Ann Caldwell, PhD, said in an interview at Obesity Week 2018, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Caldwell and her colleagues at the University of Colorado Anschutz Medical Campus, Aurora, conducted a secondary analysis of case-control data of individuals with healthy weight, overweight, or obesity, and those who had successfully maintained weight loss. They compared total daily energy expenditure (TDEE) and physical activity energy expenditure (PAEE), looking at men and women in all three groups separately.
The study included 20 women and 5 men who had successfully maintained a weight loss of at least 13.6 kg for at least 1 year. These were matched with 20 women and 7 men with a body mass index within the healthy range, as controls for the weight loss maintainers at their post–weight loss BMI.
Another group of 22 women and 6 men with BMIs in the overweight or obese category served as controls for the weight loss maintainers at their pre–weight loss BMI.
For all participants, TDEE was measured using the doubly labeled water method for 7 days. This method tracks elimination of a set quantity of ingested water made up of two uncommon isotopes (hydrogen-2 and oxygen-18) to measure energy expenditure. Since the oxygen is lost both as water and carbon dioxide as a result of metabolism, the presence of less oxygen-18 over time indicates a higher total energy expenditure.
Indirect calorimetry was used to measure resting energy expenditure (REE), and energy expenditure related to physical activity was calculated by subtracting REE and a 10% fraction of TDEE (to account for the thermic effect of feeding) from total TDEE.
“There were significant sex-group interactions for TDEE, PAEE, and PAEE/TEE,” said Dr. Caldwell. She explained that the cutoff for statistical significance for the investigators’ analysis was set at P = .1, since sample sizes were so small for men.
For women who were weight-loss maintainers, both PAEE and PAEE/TDEE ratios were higher than for the female healthy-BMI and high-BMI control participants: PAEE was 822 kcal/day for the maintainers, 536 kcal/day for the healthy-BMI, and 669 kcal/day for the high-BMI controls (P less than .01 for both comparisons).
Dr. Caldwell and her colleagues saw no difference when comparing the PAEE/TDEE ratio for women in each of the control groups.
For men, by contrast, PAEE was highest for those with healthy BMIs, at 815 kcal/day, and lowest for those in the high-BMI control group, at 506 kcal/day. Men who were weight loss maintainers fell in the middle, at 772 kcal/day of PAEE. The PAEE/TDEE ratio was significantly higher for both weight loss maintainers and normal-BMI participants than for the high-BMI participants (P less than .07).
“These cross-sectional data suggest potential sex differences in the importance of [physical activity] for successful weight loss maintenance that should be explored further with objective measures,” wrote Dr. Caldwell and her coauthors.
The investigators are planning further work that incorporates objective physical activity data via actigraphy, and that will include a larger sample of men. Through a prospective study that overcomes the limitation of the present study, they hope to develop a clearer picture of sex differences in weight loss maintenance.
The National Institutes of Health supported the study. Dr. Caldwell reported no relevant conflicts of interest.
SOURCE: Caldwell A et al. Obesity Week 2018, Abstract TP-3233.
NASHVILLE – , according to new analysis of a small study.
Physical activity is a key component in successful maintenance of weight loss, but differential effects of physical activity between men and women had not been well explored, Ann Caldwell, PhD, said in an interview at Obesity Week 2018, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Caldwell and her colleagues at the University of Colorado Anschutz Medical Campus, Aurora, conducted a secondary analysis of case-control data of individuals with healthy weight, overweight, or obesity, and those who had successfully maintained weight loss. They compared total daily energy expenditure (TDEE) and physical activity energy expenditure (PAEE), looking at men and women in all three groups separately.
The study included 20 women and 5 men who had successfully maintained a weight loss of at least 13.6 kg for at least 1 year. These were matched with 20 women and 7 men with a body mass index within the healthy range, as controls for the weight loss maintainers at their post–weight loss BMI.
Another group of 22 women and 6 men with BMIs in the overweight or obese category served as controls for the weight loss maintainers at their pre–weight loss BMI.
For all participants, TDEE was measured using the doubly labeled water method for 7 days. This method tracks elimination of a set quantity of ingested water made up of two uncommon isotopes (hydrogen-2 and oxygen-18) to measure energy expenditure. Since the oxygen is lost both as water and carbon dioxide as a result of metabolism, the presence of less oxygen-18 over time indicates a higher total energy expenditure.
Indirect calorimetry was used to measure resting energy expenditure (REE), and energy expenditure related to physical activity was calculated by subtracting REE and a 10% fraction of TDEE (to account for the thermic effect of feeding) from total TDEE.
“There were significant sex-group interactions for TDEE, PAEE, and PAEE/TEE,” said Dr. Caldwell. She explained that the cutoff for statistical significance for the investigators’ analysis was set at P = .1, since sample sizes were so small for men.
For women who were weight-loss maintainers, both PAEE and PAEE/TDEE ratios were higher than for the female healthy-BMI and high-BMI control participants: PAEE was 822 kcal/day for the maintainers, 536 kcal/day for the healthy-BMI, and 669 kcal/day for the high-BMI controls (P less than .01 for both comparisons).
Dr. Caldwell and her colleagues saw no difference when comparing the PAEE/TDEE ratio for women in each of the control groups.
For men, by contrast, PAEE was highest for those with healthy BMIs, at 815 kcal/day, and lowest for those in the high-BMI control group, at 506 kcal/day. Men who were weight loss maintainers fell in the middle, at 772 kcal/day of PAEE. The PAEE/TDEE ratio was significantly higher for both weight loss maintainers and normal-BMI participants than for the high-BMI participants (P less than .07).
“These cross-sectional data suggest potential sex differences in the importance of [physical activity] for successful weight loss maintenance that should be explored further with objective measures,” wrote Dr. Caldwell and her coauthors.
The investigators are planning further work that incorporates objective physical activity data via actigraphy, and that will include a larger sample of men. Through a prospective study that overcomes the limitation of the present study, they hope to develop a clearer picture of sex differences in weight loss maintenance.
The National Institutes of Health supported the study. Dr. Caldwell reported no relevant conflicts of interest.
SOURCE: Caldwell A et al. Obesity Week 2018, Abstract TP-3233.
NASHVILLE – , according to new analysis of a small study.
Physical activity is a key component in successful maintenance of weight loss, but differential effects of physical activity between men and women had not been well explored, Ann Caldwell, PhD, said in an interview at Obesity Week 2018, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Caldwell and her colleagues at the University of Colorado Anschutz Medical Campus, Aurora, conducted a secondary analysis of case-control data of individuals with healthy weight, overweight, or obesity, and those who had successfully maintained weight loss. They compared total daily energy expenditure (TDEE) and physical activity energy expenditure (PAEE), looking at men and women in all three groups separately.
The study included 20 women and 5 men who had successfully maintained a weight loss of at least 13.6 kg for at least 1 year. These were matched with 20 women and 7 men with a body mass index within the healthy range, as controls for the weight loss maintainers at their post–weight loss BMI.
Another group of 22 women and 6 men with BMIs in the overweight or obese category served as controls for the weight loss maintainers at their pre–weight loss BMI.
For all participants, TDEE was measured using the doubly labeled water method for 7 days. This method tracks elimination of a set quantity of ingested water made up of two uncommon isotopes (hydrogen-2 and oxygen-18) to measure energy expenditure. Since the oxygen is lost both as water and carbon dioxide as a result of metabolism, the presence of less oxygen-18 over time indicates a higher total energy expenditure.
Indirect calorimetry was used to measure resting energy expenditure (REE), and energy expenditure related to physical activity was calculated by subtracting REE and a 10% fraction of TDEE (to account for the thermic effect of feeding) from total TDEE.
“There were significant sex-group interactions for TDEE, PAEE, and PAEE/TEE,” said Dr. Caldwell. She explained that the cutoff for statistical significance for the investigators’ analysis was set at P = .1, since sample sizes were so small for men.
For women who were weight-loss maintainers, both PAEE and PAEE/TDEE ratios were higher than for the female healthy-BMI and high-BMI control participants: PAEE was 822 kcal/day for the maintainers, 536 kcal/day for the healthy-BMI, and 669 kcal/day for the high-BMI controls (P less than .01 for both comparisons).
Dr. Caldwell and her colleagues saw no difference when comparing the PAEE/TDEE ratio for women in each of the control groups.
For men, by contrast, PAEE was highest for those with healthy BMIs, at 815 kcal/day, and lowest for those in the high-BMI control group, at 506 kcal/day. Men who were weight loss maintainers fell in the middle, at 772 kcal/day of PAEE. The PAEE/TDEE ratio was significantly higher for both weight loss maintainers and normal-BMI participants than for the high-BMI participants (P less than .07).
“These cross-sectional data suggest potential sex differences in the importance of [physical activity] for successful weight loss maintenance that should be explored further with objective measures,” wrote Dr. Caldwell and her coauthors.
The investigators are planning further work that incorporates objective physical activity data via actigraphy, and that will include a larger sample of men. Through a prospective study that overcomes the limitation of the present study, they hope to develop a clearer picture of sex differences in weight loss maintenance.
The National Institutes of Health supported the study. Dr. Caldwell reported no relevant conflicts of interest.
SOURCE: Caldwell A et al. Obesity Week 2018, Abstract TP-3233.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Women who kept weight off burned more calories in physical activity than did normal or high-BMI controls.
Major finding: In women, the ratio of physical activity energy expenditure to total daily energy expenditure was higher for successful weight-loss maintainers (P less than .01).
Study details: Secondary analysis of case-control study enrolling 80 individuals.
Disclosures: The National Institutes of Health funded the study. Dr. Caldwell reported no conflicts of interest.
Source: Caldwell A et al. Obesity Week 2018, abstract TP-3233.
Fatigue in MS: Common, often profound, tough to treat
BERLIN – In addition to the pain, motor and sensory impairments, and cognitive dysfunction that can stalk multiple sclerosis (MS) patients, for many, there’s also the challenge of an invisible, tough-to-quantify entity: fatigue.
“Approximately 80% of patients suffer from fatigue, so it’s an immense problem in MS. There’s no real clear relationship with disease severity,” Vincent de Groot, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. “Despite what a lot of people think, there’s no clear or strong relationship between fatigue and the amount of physical activity people undertake daily,” he noted.
“Patients all know what we are talking about when we ask about fatigue,” but there are a variety of definitions of fatigue used in research, a fact that has limited progress in the field, said Dr. de Groot.
Primary fatigue is related to the pathophysiology of MS itself, while secondary fatigue can result from MS symptoms, such as poor sleep from spasms. Secondary fatigue can also be a side effect of MS medications; baclofen, used for spasticity, is a good example, said Dr. de Groot. “We must not underestimate how many problems these drugs can give people.”
What’s the mechanism by which MS causes primary fatigue? “The simple answer is that we do not know,” said Dr. de Groot, a physiatrist and researcher at Vrije University, Amsterdam.
Though immune-mediated fatigue had been proposed as a factor for patients with MS, Dr. de Groot said that his own lab’s work has not found any connection between fatigue levels and any immune-related biomarkers. “So I don’t think the immune hypothesis has a lot of evidence.”
Similarly, though there might be mechanistic reasons to suspect the hypothalamic-pituitary-adrenal (HPA) axis as a culprit for MS fatigue, no consistent association has been found between any markers for HPA axis disruption and fatigue ratings, Dr. de Groot said.
Newer theories center on MS-related disruptions in brain connectivity, with imaging studies now able to detect some of these disruptions in functional connectivity that correlate with fatigue. “Right now, I think this is the hypothesis to bet money on,” Dr. de Groot said.
Many factors come into play, including environmental and psychological factors, he said.
“What can we do to treat MS-related fatigue?” Though several drugs have been used, “if you carefully look at the systematic reviews, the evidence is very, very disappointing,” Dr. de Groot said. For both amantadine and modafinil, “there is no evidence that these drugs are effective,” he said, citing a systematic review and meta-analysis that found a pooled effect size of 0.07 (95% confidence interval, –0.22 to 0.37) for medications (Mult Scler Int. 2014 May; doi: 10.1155/2014/798285).
Only two trials have looked at multidisciplinary rehabilitation for MS-related fatigue, Dr. de Groot said. Two studies that looked at multidisciplinary strategies that pulled in a variety of disciplines to help develop tailored fatigue management strategies saw no between-group effect when the multidisciplinary intervention was compared with nurse-provided information or with non–fatigue-related rehabilitation.
In an effort to determine whether MS-related fatigue is truly refractory to treatment, Dr. de Groot said that he and his colleagues decided to take “three steps back” to look at the individual interventions that make up a multidisciplinary approach to tackling fatigue. “So, we looked at exercise therapy, energy conservation management, and cognitive-behavioral therapy,” beginning with a literature review, he said.
Members of his research group found that effect sizes ranged from small to moderate for the three approaches, but there were methodologic problems with many of the studies; in the case of cognitive-behavioral therapy (CBT), the effect size waned over time, Dr. de Groot said. A newer randomized, controlled trial showed a relatively robust effect size of 0.52 for Internet-delivered CBT, which may provide a promising and practical approach (J Neurol Neurosurg Psychiatry. 2018 Sep;89[9]:970-6. doi: 10.1136/jnnp-2017-317463).
Looking at fatigue and societal participation, Dr. de Groot and his colleagues examined what effect aerobic training, energy conservation management, and CBT had on the two outcome measures. The three interventions were studied in three stand-alone trials, he said.
Patients were assessed at baseline, and at 8, 16, 26, and 52 weeks. The assessments were performed by a blinded researcher and were the same across trials: For fatigue, researchers used the Checklist Individual Strength–fatigue (CIS20R-fatigue), and for societal participation, they administered the Impact on Participation and Autonomy (IPA).
Each trial included 90 patients, randomized 1:1 to receive high- or low-intensity treatment. Patients had to have MS with no exacerbations within the prior 6 months and an Expanded Disability Status Scale score of 6 or less. However, the included patients had severe fatigue, with a CIS20R-fatigue subscore of 35 or higher, and the fatigue could not be attributable to such secondary causes as infection, depression, or thyroid or sleep problems. Finally, patients could not have been treated for fatigue in the 3 months prior to enrollment.
Those in the high-intensity treatment group received 12 sessions focused on the particular intervention over 4 months, provided by an expert therapist. Each type of intervention had a treatment protocol that was followed over the 4 months. Patients receiving low-intensity treatment saw an MS-specialized nurse three times over 4 months.
The aerobic training intervention had patients performing high-intensity exercise on a cycle ergometer for 30 minutes, three times weekly for 16 weeks. In addition to the 12 supervised sessions, patients also completed 36 home-based sessions. The level of intensity for each patient was personalized based on their baseline cardiopulmonary exercise test, Dr. de Groot said.
At the end of 1 year, patients in the high-intensity group and those in the low-intensity group reported virtually the same fatigue scores. Though there was an initial drop in fatigue for those in the high-intensity group, compared with baseline and with the low-intensity participants, values on the CIS20R never dropped below 35, the “severe fatigue” cutoff.
And, Dr. de Groot said, there was no effect on societal participation or in other fatigue scores. In sum, the effect size was barely significant at –0.54 (95% CI, –1.00 to –0.06), with a number needed to treat of 9.
Adherence to attempting the workouts was fairly good for participants in the high-intensity group; 74% completed the sessions, with 71% doing so at the prescribed workload. The median rate of perceived exertion on a 1-20 scale was 14.
However, the thrice-weekly exercise bouts didn’t improve aerobic fitness parameters: Neither V02peak, V02peak adjusted for body mass, nor anaerobic threshold changed for those in the high-intensity group. Peak power did increase by 11.7 watts (P = .048).
Energy conservation education, whether delivered in high- or low-intensity format, had almost no effect on fatigue scores, with a number needed to treat of 158 – a figure that is “neither significant nor clinically meaningful,” Dr. de Groot said. Other fatigue scores and societal participation levels also went unchanged.
However, CBT delivered in a series of 10 modules to address various beliefs and coping mechanisms about MS, fatigue, pain, and activity regulation did have a positive effect on fatigue. Here, the effect size was –0.79 (95% CI, –1.26 to –0.32). The number needed to treat was 3, and CIS20R values did dip below the “severe fatigue” threshold during treatment. A similar effect, Dr. de Groot said, was seen for other fatigue and quality of life measures, though societal participation scores didn’t change. No significant improvement was seen for the low-intensity CBT group.
“Severe MS-related fatigue can be reduced effectively with CBT in the short term. More research is needed on how to maintain this effect in the long term,” Dr. de Groot said. Still, “it’s currently the best treatment option,” he said.
The fact that patients reverted to their preintervention fatigue levels regardless of the intervention shows that effective treatment for MS-related fatigue should probably be ongoing, viewed more as a process than an occurrence, Dr. de Groot said.
To that end, Dr. de Groot and his colleagues are conducting a randomized, controlled trial that includes 166 MS patients with fatigue. The study has two arms: The first is a noninferiority trial comparing face-to-face CBT with e-learning delivery of the content, and the second looks at the efficacy of ongoing booster sessions after initial CBT.
An online database of randomized, controlled trials of rehabilitation for MS patients can be found at www.appeco.net.
The study was funded by Fonds NutsOhra, a private Dutch foundation. Dr. de Groot reported no relevant conflicts of interest.
SOURCE: de Groot V. Mult Scler. 2018;24(S2):83, Abstract 225.
BERLIN – In addition to the pain, motor and sensory impairments, and cognitive dysfunction that can stalk multiple sclerosis (MS) patients, for many, there’s also the challenge of an invisible, tough-to-quantify entity: fatigue.
“Approximately 80% of patients suffer from fatigue, so it’s an immense problem in MS. There’s no real clear relationship with disease severity,” Vincent de Groot, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. “Despite what a lot of people think, there’s no clear or strong relationship between fatigue and the amount of physical activity people undertake daily,” he noted.
“Patients all know what we are talking about when we ask about fatigue,” but there are a variety of definitions of fatigue used in research, a fact that has limited progress in the field, said Dr. de Groot.
Primary fatigue is related to the pathophysiology of MS itself, while secondary fatigue can result from MS symptoms, such as poor sleep from spasms. Secondary fatigue can also be a side effect of MS medications; baclofen, used for spasticity, is a good example, said Dr. de Groot. “We must not underestimate how many problems these drugs can give people.”
What’s the mechanism by which MS causes primary fatigue? “The simple answer is that we do not know,” said Dr. de Groot, a physiatrist and researcher at Vrije University, Amsterdam.
Though immune-mediated fatigue had been proposed as a factor for patients with MS, Dr. de Groot said that his own lab’s work has not found any connection between fatigue levels and any immune-related biomarkers. “So I don’t think the immune hypothesis has a lot of evidence.”
Similarly, though there might be mechanistic reasons to suspect the hypothalamic-pituitary-adrenal (HPA) axis as a culprit for MS fatigue, no consistent association has been found between any markers for HPA axis disruption and fatigue ratings, Dr. de Groot said.
Newer theories center on MS-related disruptions in brain connectivity, with imaging studies now able to detect some of these disruptions in functional connectivity that correlate with fatigue. “Right now, I think this is the hypothesis to bet money on,” Dr. de Groot said.
Many factors come into play, including environmental and psychological factors, he said.
“What can we do to treat MS-related fatigue?” Though several drugs have been used, “if you carefully look at the systematic reviews, the evidence is very, very disappointing,” Dr. de Groot said. For both amantadine and modafinil, “there is no evidence that these drugs are effective,” he said, citing a systematic review and meta-analysis that found a pooled effect size of 0.07 (95% confidence interval, –0.22 to 0.37) for medications (Mult Scler Int. 2014 May; doi: 10.1155/2014/798285).
Only two trials have looked at multidisciplinary rehabilitation for MS-related fatigue, Dr. de Groot said. Two studies that looked at multidisciplinary strategies that pulled in a variety of disciplines to help develop tailored fatigue management strategies saw no between-group effect when the multidisciplinary intervention was compared with nurse-provided information or with non–fatigue-related rehabilitation.
In an effort to determine whether MS-related fatigue is truly refractory to treatment, Dr. de Groot said that he and his colleagues decided to take “three steps back” to look at the individual interventions that make up a multidisciplinary approach to tackling fatigue. “So, we looked at exercise therapy, energy conservation management, and cognitive-behavioral therapy,” beginning with a literature review, he said.
Members of his research group found that effect sizes ranged from small to moderate for the three approaches, but there were methodologic problems with many of the studies; in the case of cognitive-behavioral therapy (CBT), the effect size waned over time, Dr. de Groot said. A newer randomized, controlled trial showed a relatively robust effect size of 0.52 for Internet-delivered CBT, which may provide a promising and practical approach (J Neurol Neurosurg Psychiatry. 2018 Sep;89[9]:970-6. doi: 10.1136/jnnp-2017-317463).
Looking at fatigue and societal participation, Dr. de Groot and his colleagues examined what effect aerobic training, energy conservation management, and CBT had on the two outcome measures. The three interventions were studied in three stand-alone trials, he said.
Patients were assessed at baseline, and at 8, 16, 26, and 52 weeks. The assessments were performed by a blinded researcher and were the same across trials: For fatigue, researchers used the Checklist Individual Strength–fatigue (CIS20R-fatigue), and for societal participation, they administered the Impact on Participation and Autonomy (IPA).
Each trial included 90 patients, randomized 1:1 to receive high- or low-intensity treatment. Patients had to have MS with no exacerbations within the prior 6 months and an Expanded Disability Status Scale score of 6 or less. However, the included patients had severe fatigue, with a CIS20R-fatigue subscore of 35 or higher, and the fatigue could not be attributable to such secondary causes as infection, depression, or thyroid or sleep problems. Finally, patients could not have been treated for fatigue in the 3 months prior to enrollment.
Those in the high-intensity treatment group received 12 sessions focused on the particular intervention over 4 months, provided by an expert therapist. Each type of intervention had a treatment protocol that was followed over the 4 months. Patients receiving low-intensity treatment saw an MS-specialized nurse three times over 4 months.
The aerobic training intervention had patients performing high-intensity exercise on a cycle ergometer for 30 minutes, three times weekly for 16 weeks. In addition to the 12 supervised sessions, patients also completed 36 home-based sessions. The level of intensity for each patient was personalized based on their baseline cardiopulmonary exercise test, Dr. de Groot said.
At the end of 1 year, patients in the high-intensity group and those in the low-intensity group reported virtually the same fatigue scores. Though there was an initial drop in fatigue for those in the high-intensity group, compared with baseline and with the low-intensity participants, values on the CIS20R never dropped below 35, the “severe fatigue” cutoff.
And, Dr. de Groot said, there was no effect on societal participation or in other fatigue scores. In sum, the effect size was barely significant at –0.54 (95% CI, –1.00 to –0.06), with a number needed to treat of 9.
Adherence to attempting the workouts was fairly good for participants in the high-intensity group; 74% completed the sessions, with 71% doing so at the prescribed workload. The median rate of perceived exertion on a 1-20 scale was 14.
However, the thrice-weekly exercise bouts didn’t improve aerobic fitness parameters: Neither V02peak, V02peak adjusted for body mass, nor anaerobic threshold changed for those in the high-intensity group. Peak power did increase by 11.7 watts (P = .048).
Energy conservation education, whether delivered in high- or low-intensity format, had almost no effect on fatigue scores, with a number needed to treat of 158 – a figure that is “neither significant nor clinically meaningful,” Dr. de Groot said. Other fatigue scores and societal participation levels also went unchanged.
However, CBT delivered in a series of 10 modules to address various beliefs and coping mechanisms about MS, fatigue, pain, and activity regulation did have a positive effect on fatigue. Here, the effect size was –0.79 (95% CI, –1.26 to –0.32). The number needed to treat was 3, and CIS20R values did dip below the “severe fatigue” threshold during treatment. A similar effect, Dr. de Groot said, was seen for other fatigue and quality of life measures, though societal participation scores didn’t change. No significant improvement was seen for the low-intensity CBT group.
“Severe MS-related fatigue can be reduced effectively with CBT in the short term. More research is needed on how to maintain this effect in the long term,” Dr. de Groot said. Still, “it’s currently the best treatment option,” he said.
The fact that patients reverted to their preintervention fatigue levels regardless of the intervention shows that effective treatment for MS-related fatigue should probably be ongoing, viewed more as a process than an occurrence, Dr. de Groot said.
To that end, Dr. de Groot and his colleagues are conducting a randomized, controlled trial that includes 166 MS patients with fatigue. The study has two arms: The first is a noninferiority trial comparing face-to-face CBT with e-learning delivery of the content, and the second looks at the efficacy of ongoing booster sessions after initial CBT.
An online database of randomized, controlled trials of rehabilitation for MS patients can be found at www.appeco.net.
The study was funded by Fonds NutsOhra, a private Dutch foundation. Dr. de Groot reported no relevant conflicts of interest.
SOURCE: de Groot V. Mult Scler. 2018;24(S2):83, Abstract 225.
BERLIN – In addition to the pain, motor and sensory impairments, and cognitive dysfunction that can stalk multiple sclerosis (MS) patients, for many, there’s also the challenge of an invisible, tough-to-quantify entity: fatigue.
“Approximately 80% of patients suffer from fatigue, so it’s an immense problem in MS. There’s no real clear relationship with disease severity,” Vincent de Groot, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. “Despite what a lot of people think, there’s no clear or strong relationship between fatigue and the amount of physical activity people undertake daily,” he noted.
“Patients all know what we are talking about when we ask about fatigue,” but there are a variety of definitions of fatigue used in research, a fact that has limited progress in the field, said Dr. de Groot.
Primary fatigue is related to the pathophysiology of MS itself, while secondary fatigue can result from MS symptoms, such as poor sleep from spasms. Secondary fatigue can also be a side effect of MS medications; baclofen, used for spasticity, is a good example, said Dr. de Groot. “We must not underestimate how many problems these drugs can give people.”
What’s the mechanism by which MS causes primary fatigue? “The simple answer is that we do not know,” said Dr. de Groot, a physiatrist and researcher at Vrije University, Amsterdam.
Though immune-mediated fatigue had been proposed as a factor for patients with MS, Dr. de Groot said that his own lab’s work has not found any connection between fatigue levels and any immune-related biomarkers. “So I don’t think the immune hypothesis has a lot of evidence.”
Similarly, though there might be mechanistic reasons to suspect the hypothalamic-pituitary-adrenal (HPA) axis as a culprit for MS fatigue, no consistent association has been found between any markers for HPA axis disruption and fatigue ratings, Dr. de Groot said.
Newer theories center on MS-related disruptions in brain connectivity, with imaging studies now able to detect some of these disruptions in functional connectivity that correlate with fatigue. “Right now, I think this is the hypothesis to bet money on,” Dr. de Groot said.
Many factors come into play, including environmental and psychological factors, he said.
“What can we do to treat MS-related fatigue?” Though several drugs have been used, “if you carefully look at the systematic reviews, the evidence is very, very disappointing,” Dr. de Groot said. For both amantadine and modafinil, “there is no evidence that these drugs are effective,” he said, citing a systematic review and meta-analysis that found a pooled effect size of 0.07 (95% confidence interval, –0.22 to 0.37) for medications (Mult Scler Int. 2014 May; doi: 10.1155/2014/798285).
Only two trials have looked at multidisciplinary rehabilitation for MS-related fatigue, Dr. de Groot said. Two studies that looked at multidisciplinary strategies that pulled in a variety of disciplines to help develop tailored fatigue management strategies saw no between-group effect when the multidisciplinary intervention was compared with nurse-provided information or with non–fatigue-related rehabilitation.
In an effort to determine whether MS-related fatigue is truly refractory to treatment, Dr. de Groot said that he and his colleagues decided to take “three steps back” to look at the individual interventions that make up a multidisciplinary approach to tackling fatigue. “So, we looked at exercise therapy, energy conservation management, and cognitive-behavioral therapy,” beginning with a literature review, he said.
Members of his research group found that effect sizes ranged from small to moderate for the three approaches, but there were methodologic problems with many of the studies; in the case of cognitive-behavioral therapy (CBT), the effect size waned over time, Dr. de Groot said. A newer randomized, controlled trial showed a relatively robust effect size of 0.52 for Internet-delivered CBT, which may provide a promising and practical approach (J Neurol Neurosurg Psychiatry. 2018 Sep;89[9]:970-6. doi: 10.1136/jnnp-2017-317463).
Looking at fatigue and societal participation, Dr. de Groot and his colleagues examined what effect aerobic training, energy conservation management, and CBT had on the two outcome measures. The three interventions were studied in three stand-alone trials, he said.
Patients were assessed at baseline, and at 8, 16, 26, and 52 weeks. The assessments were performed by a blinded researcher and were the same across trials: For fatigue, researchers used the Checklist Individual Strength–fatigue (CIS20R-fatigue), and for societal participation, they administered the Impact on Participation and Autonomy (IPA).
Each trial included 90 patients, randomized 1:1 to receive high- or low-intensity treatment. Patients had to have MS with no exacerbations within the prior 6 months and an Expanded Disability Status Scale score of 6 or less. However, the included patients had severe fatigue, with a CIS20R-fatigue subscore of 35 or higher, and the fatigue could not be attributable to such secondary causes as infection, depression, or thyroid or sleep problems. Finally, patients could not have been treated for fatigue in the 3 months prior to enrollment.
Those in the high-intensity treatment group received 12 sessions focused on the particular intervention over 4 months, provided by an expert therapist. Each type of intervention had a treatment protocol that was followed over the 4 months. Patients receiving low-intensity treatment saw an MS-specialized nurse three times over 4 months.
The aerobic training intervention had patients performing high-intensity exercise on a cycle ergometer for 30 minutes, three times weekly for 16 weeks. In addition to the 12 supervised sessions, patients also completed 36 home-based sessions. The level of intensity for each patient was personalized based on their baseline cardiopulmonary exercise test, Dr. de Groot said.
At the end of 1 year, patients in the high-intensity group and those in the low-intensity group reported virtually the same fatigue scores. Though there was an initial drop in fatigue for those in the high-intensity group, compared with baseline and with the low-intensity participants, values on the CIS20R never dropped below 35, the “severe fatigue” cutoff.
And, Dr. de Groot said, there was no effect on societal participation or in other fatigue scores. In sum, the effect size was barely significant at –0.54 (95% CI, –1.00 to –0.06), with a number needed to treat of 9.
Adherence to attempting the workouts was fairly good for participants in the high-intensity group; 74% completed the sessions, with 71% doing so at the prescribed workload. The median rate of perceived exertion on a 1-20 scale was 14.
However, the thrice-weekly exercise bouts didn’t improve aerobic fitness parameters: Neither V02peak, V02peak adjusted for body mass, nor anaerobic threshold changed for those in the high-intensity group. Peak power did increase by 11.7 watts (P = .048).
Energy conservation education, whether delivered in high- or low-intensity format, had almost no effect on fatigue scores, with a number needed to treat of 158 – a figure that is “neither significant nor clinically meaningful,” Dr. de Groot said. Other fatigue scores and societal participation levels also went unchanged.
However, CBT delivered in a series of 10 modules to address various beliefs and coping mechanisms about MS, fatigue, pain, and activity regulation did have a positive effect on fatigue. Here, the effect size was –0.79 (95% CI, –1.26 to –0.32). The number needed to treat was 3, and CIS20R values did dip below the “severe fatigue” threshold during treatment. A similar effect, Dr. de Groot said, was seen for other fatigue and quality of life measures, though societal participation scores didn’t change. No significant improvement was seen for the low-intensity CBT group.
“Severe MS-related fatigue can be reduced effectively with CBT in the short term. More research is needed on how to maintain this effect in the long term,” Dr. de Groot said. Still, “it’s currently the best treatment option,” he said.
The fact that patients reverted to their preintervention fatigue levels regardless of the intervention shows that effective treatment for MS-related fatigue should probably be ongoing, viewed more as a process than an occurrence, Dr. de Groot said.
To that end, Dr. de Groot and his colleagues are conducting a randomized, controlled trial that includes 166 MS patients with fatigue. The study has two arms: The first is a noninferiority trial comparing face-to-face CBT with e-learning delivery of the content, and the second looks at the efficacy of ongoing booster sessions after initial CBT.
An online database of randomized, controlled trials of rehabilitation for MS patients can be found at www.appeco.net.
The study was funded by Fonds NutsOhra, a private Dutch foundation. Dr. de Groot reported no relevant conflicts of interest.
SOURCE: de Groot V. Mult Scler. 2018;24(S2):83, Abstract 225.
EXPERT ANALYSIS FROM ECTRIMS 2018
Bariatric surgery ups risk of suicide, self-harm
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Bariatric surgery patients have an elevated risk for suicide or self-harm.
Major finding: The odds ratio for suicide or self-harm was 1.69 after bariatric surgery.
Study details: Meta-analysis of 28 studies of bariatric surgery patients.
Disclosures: The authors reported no conflicts of interest and no outside sources of funding.
Source: Roberts D et al. Obesity Week 2018, Poster A433.