User login
The Most Problematic Warts Have No Sure Treatment
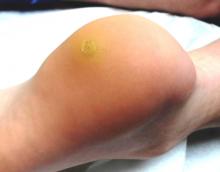
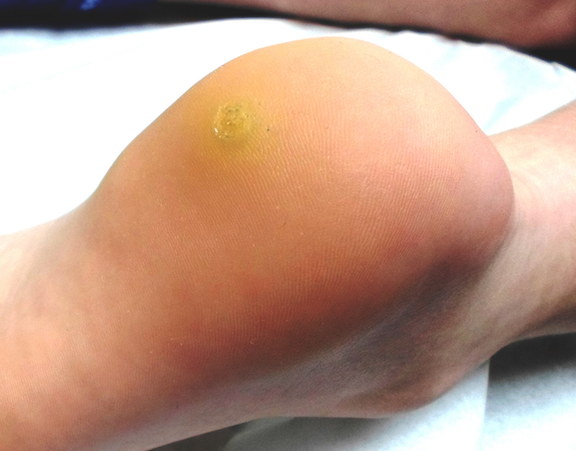
A 23-year-old woman presents with an 18-month history of a lesion on her heel that has persisted despite treatment with an OTC salicylic acid preparation, several attempts with an OTC “freezing unit,” and cryotherapy performed by her primary care provider. The lesion is continually aggravated by weight-bearing.
As a child, she reports, she had several warts on her hands. However, they resolved without treatment.
EXAMINATION
The lesion in question is almost 1 cm in diameter and clearly intradermal in nature. It has a rough, dry feel. On its surface, there are tiny black dots. Normal skin lines flow over the surface of the heel until they reach the lesion; at that point, they curve around its periphery and rejoin on the other side.
DISCUSSION
These features—the black dots, which represent vertically aligned thrombosed capillaries, and the curving skin lines—are diagnostic for plantar warts. This case represents a classic plantar (not “planter”) wart, so named because of its location, not because it has anything to do with planting.
There are good reasons for distinguishing plantar from ordinary warts. For one thing, the outer layer of skin on the sole (the stratum lucidum) is avascular and quite thick, allowing the wart not only to become relatively deep but also to escape detection by the immune system. Since they are almost always on the weight-bearing surface of the sole, even small warts can cause considerable discomfort as they grow.
These same features—the depth and location of the wart—also get in the way of successful treatment, since it may or may not reach the deep margin of the lesion without undue pain and scarring. As in other areas of medicine, we in dermatology strive to avoid treatments that are worse than the disease.
While this is especially true with children, many adults are intolerant of the usual liquid nitrogen treatment (cryotherapy), not only because of the pain associated with the initial application but also because the blistering and pain can persist for days afterward. Perhaps worst of all, no treatment modality is a “sure thing,” so the patient may go through the process and get very little in return.
This combination of issues is why, in dermatology, the first thing we do is to discuss the situation thoroughly with the patient (and parents). My typical conversation starts like this: “You know, you’ve brought us a very difficult problem to treat. This is an infection caused by the human papillomavirus (HPV), which can grow deep and does not elicit much of an immune response. We don’t have drugs or shots to kill the virus. And, as if this were not enough of a problem, none of our treatment choices is remotely perfect. They might not work, and most are sure to cause pain.” Then, of course, I review the treatment options one by one.
TREATMENT
If the patient is lucky and the wart is small and shallow, we typically treat with a liquid nitrogen gun, almost always through a 3 to 5 mm speculum to concentrate the spray. We might shave down the surface of the wart with a #10 blade first, to reduce the thickness and increase the likelihood of successful treatment.
In my opinion, based on many years of treating these warts, using a cotton-tipped applicator to apply the liquid nitrogen is a waste of time and pain. Warts on thin-skinned areas such as arms and legs might be the exception.
Often, with small children, I discuss another option with the parents: that of doing nothing. Warts are warts, not dangerous in any way. Virtually all of them will eventually resolve on their own. The trouble is, of course, that we can’t promise when this will happen, or how big the wart might become in the interim.
There are nonpainful treatment choices, albeit ones with little chance of ultimate success. These include the OTC wart treatment products, virtually all of which contain salicylic acid as their main ingredient. Applied two or three times a week, these products can at least hold smaller warts in check, and could result in a cure.
Much the same could be said for products like cantharidin, a chemical derived from blister beetles, which causes nonpainful and slight blistering at the site. Unfortunately, we can’t prescribe it, which dooms the patient to returning to the office every two or three weeks. As with many such treatment options, it is unlikely to result in a cure.
Another treatment option is dinitrochlorobenzene (DNCB) as the main ingredient in a compounded product. DNCB is a potent T-cell stimulator—another way of saying that we can make the patient allergic to the substance, bringing the body’s immune system to bear on the treated area, producing slight blistering and hopefully destroying the wart in the process. It has to be used with caution, lest the substance wind up on unaffected skin. Parents need to understand that DNCB is slow to work (often taking a month or more) and again, by no means a sure thing. Squaric acid is an alternative to DNCB.
Surgical curettage and electrodessication, under local anesthesia, is potentially the most effective treatment we have for plantar warts—but as you might imagine, piercing the sole of a young child’s foot with a 30-gauge needle is rarely our first choice. It’s the method we used before liquid nitrogen was widely available, and it was a nightmare for all involved. Three outcomes were possible, two quite negative: Serious post-procedure pain and scarring were almost certain. But worst of all, the wart could easily return despite all that. The only time I use this is when the plantar wart is totally resistant to treatment and so large as to interfere with walking.
TAKE-AWAY LEARNING POINTS
• The reason there are 20 or more treatments for warts is that none are remotely perfect.
• Plantar warts are a special problem because they develop on weight-bearing portions of the sole, growing inward (endophytic) in a thick skin layer that allows the virus to avoid detection by the immune system. Plantar warts often cause pain, which treatment can worsen.
• Parents/patients need to understand all of this prior to selecting an appropriate treatment choice.
• They also need to understand that warts do not have to be treated. Most will resolve on their own, eventually.
• Terrorizing children is to be avoided if at all possible. Parents may want their child’s warts to be “taken care of,” but they need to understand this may not be possible.
• Consider referral of problematic plantar warts to dermatology.
A 23-year-old woman presents with an 18-month history of a lesion on her heel that has persisted despite treatment with an OTC salicylic acid preparation, several attempts with an OTC “freezing unit,” and cryotherapy performed by her primary care provider. The lesion is continually aggravated by weight-bearing.
As a child, she reports, she had several warts on her hands. However, they resolved without treatment.
EXAMINATION
The lesion in question is almost 1 cm in diameter and clearly intradermal in nature. It has a rough, dry feel. On its surface, there are tiny black dots. Normal skin lines flow over the surface of the heel until they reach the lesion; at that point, they curve around its periphery and rejoin on the other side.
DISCUSSION
These features—the black dots, which represent vertically aligned thrombosed capillaries, and the curving skin lines—are diagnostic for plantar warts. This case represents a classic plantar (not “planter”) wart, so named because of its location, not because it has anything to do with planting.
There are good reasons for distinguishing plantar from ordinary warts. For one thing, the outer layer of skin on the sole (the stratum lucidum) is avascular and quite thick, allowing the wart not only to become relatively deep but also to escape detection by the immune system. Since they are almost always on the weight-bearing surface of the sole, even small warts can cause considerable discomfort as they grow.
These same features—the depth and location of the wart—also get in the way of successful treatment, since it may or may not reach the deep margin of the lesion without undue pain and scarring. As in other areas of medicine, we in dermatology strive to avoid treatments that are worse than the disease.
While this is especially true with children, many adults are intolerant of the usual liquid nitrogen treatment (cryotherapy), not only because of the pain associated with the initial application but also because the blistering and pain can persist for days afterward. Perhaps worst of all, no treatment modality is a “sure thing,” so the patient may go through the process and get very little in return.
This combination of issues is why, in dermatology, the first thing we do is to discuss the situation thoroughly with the patient (and parents). My typical conversation starts like this: “You know, you’ve brought us a very difficult problem to treat. This is an infection caused by the human papillomavirus (HPV), which can grow deep and does not elicit much of an immune response. We don’t have drugs or shots to kill the virus. And, as if this were not enough of a problem, none of our treatment choices is remotely perfect. They might not work, and most are sure to cause pain.” Then, of course, I review the treatment options one by one.
TREATMENT
If the patient is lucky and the wart is small and shallow, we typically treat with a liquid nitrogen gun, almost always through a 3 to 5 mm speculum to concentrate the spray. We might shave down the surface of the wart with a #10 blade first, to reduce the thickness and increase the likelihood of successful treatment.
In my opinion, based on many years of treating these warts, using a cotton-tipped applicator to apply the liquid nitrogen is a waste of time and pain. Warts on thin-skinned areas such as arms and legs might be the exception.
Often, with small children, I discuss another option with the parents: that of doing nothing. Warts are warts, not dangerous in any way. Virtually all of them will eventually resolve on their own. The trouble is, of course, that we can’t promise when this will happen, or how big the wart might become in the interim.
There are nonpainful treatment choices, albeit ones with little chance of ultimate success. These include the OTC wart treatment products, virtually all of which contain salicylic acid as their main ingredient. Applied two or three times a week, these products can at least hold smaller warts in check, and could result in a cure.
Much the same could be said for products like cantharidin, a chemical derived from blister beetles, which causes nonpainful and slight blistering at the site. Unfortunately, we can’t prescribe it, which dooms the patient to returning to the office every two or three weeks. As with many such treatment options, it is unlikely to result in a cure.
Another treatment option is dinitrochlorobenzene (DNCB) as the main ingredient in a compounded product. DNCB is a potent T-cell stimulator—another way of saying that we can make the patient allergic to the substance, bringing the body’s immune system to bear on the treated area, producing slight blistering and hopefully destroying the wart in the process. It has to be used with caution, lest the substance wind up on unaffected skin. Parents need to understand that DNCB is slow to work (often taking a month or more) and again, by no means a sure thing. Squaric acid is an alternative to DNCB.
Surgical curettage and electrodessication, under local anesthesia, is potentially the most effective treatment we have for plantar warts—but as you might imagine, piercing the sole of a young child’s foot with a 30-gauge needle is rarely our first choice. It’s the method we used before liquid nitrogen was widely available, and it was a nightmare for all involved. Three outcomes were possible, two quite negative: Serious post-procedure pain and scarring were almost certain. But worst of all, the wart could easily return despite all that. The only time I use this is when the plantar wart is totally resistant to treatment and so large as to interfere with walking.
TAKE-AWAY LEARNING POINTS
• The reason there are 20 or more treatments for warts is that none are remotely perfect.
• Plantar warts are a special problem because they develop on weight-bearing portions of the sole, growing inward (endophytic) in a thick skin layer that allows the virus to avoid detection by the immune system. Plantar warts often cause pain, which treatment can worsen.
• Parents/patients need to understand all of this prior to selecting an appropriate treatment choice.
• They also need to understand that warts do not have to be treated. Most will resolve on their own, eventually.
• Terrorizing children is to be avoided if at all possible. Parents may want their child’s warts to be “taken care of,” but they need to understand this may not be possible.
• Consider referral of problematic plantar warts to dermatology.
A 23-year-old woman presents with an 18-month history of a lesion on her heel that has persisted despite treatment with an OTC salicylic acid preparation, several attempts with an OTC “freezing unit,” and cryotherapy performed by her primary care provider. The lesion is continually aggravated by weight-bearing.
As a child, she reports, she had several warts on her hands. However, they resolved without treatment.
EXAMINATION
The lesion in question is almost 1 cm in diameter and clearly intradermal in nature. It has a rough, dry feel. On its surface, there are tiny black dots. Normal skin lines flow over the surface of the heel until they reach the lesion; at that point, they curve around its periphery and rejoin on the other side.
DISCUSSION
These features—the black dots, which represent vertically aligned thrombosed capillaries, and the curving skin lines—are diagnostic for plantar warts. This case represents a classic plantar (not “planter”) wart, so named because of its location, not because it has anything to do with planting.
There are good reasons for distinguishing plantar from ordinary warts. For one thing, the outer layer of skin on the sole (the stratum lucidum) is avascular and quite thick, allowing the wart not only to become relatively deep but also to escape detection by the immune system. Since they are almost always on the weight-bearing surface of the sole, even small warts can cause considerable discomfort as they grow.
These same features—the depth and location of the wart—also get in the way of successful treatment, since it may or may not reach the deep margin of the lesion without undue pain and scarring. As in other areas of medicine, we in dermatology strive to avoid treatments that are worse than the disease.
While this is especially true with children, many adults are intolerant of the usual liquid nitrogen treatment (cryotherapy), not only because of the pain associated with the initial application but also because the blistering and pain can persist for days afterward. Perhaps worst of all, no treatment modality is a “sure thing,” so the patient may go through the process and get very little in return.
This combination of issues is why, in dermatology, the first thing we do is to discuss the situation thoroughly with the patient (and parents). My typical conversation starts like this: “You know, you’ve brought us a very difficult problem to treat. This is an infection caused by the human papillomavirus (HPV), which can grow deep and does not elicit much of an immune response. We don’t have drugs or shots to kill the virus. And, as if this were not enough of a problem, none of our treatment choices is remotely perfect. They might not work, and most are sure to cause pain.” Then, of course, I review the treatment options one by one.
TREATMENT
If the patient is lucky and the wart is small and shallow, we typically treat with a liquid nitrogen gun, almost always through a 3 to 5 mm speculum to concentrate the spray. We might shave down the surface of the wart with a #10 blade first, to reduce the thickness and increase the likelihood of successful treatment.
In my opinion, based on many years of treating these warts, using a cotton-tipped applicator to apply the liquid nitrogen is a waste of time and pain. Warts on thin-skinned areas such as arms and legs might be the exception.
Often, with small children, I discuss another option with the parents: that of doing nothing. Warts are warts, not dangerous in any way. Virtually all of them will eventually resolve on their own. The trouble is, of course, that we can’t promise when this will happen, or how big the wart might become in the interim.
There are nonpainful treatment choices, albeit ones with little chance of ultimate success. These include the OTC wart treatment products, virtually all of which contain salicylic acid as their main ingredient. Applied two or three times a week, these products can at least hold smaller warts in check, and could result in a cure.
Much the same could be said for products like cantharidin, a chemical derived from blister beetles, which causes nonpainful and slight blistering at the site. Unfortunately, we can’t prescribe it, which dooms the patient to returning to the office every two or three weeks. As with many such treatment options, it is unlikely to result in a cure.
Another treatment option is dinitrochlorobenzene (DNCB) as the main ingredient in a compounded product. DNCB is a potent T-cell stimulator—another way of saying that we can make the patient allergic to the substance, bringing the body’s immune system to bear on the treated area, producing slight blistering and hopefully destroying the wart in the process. It has to be used with caution, lest the substance wind up on unaffected skin. Parents need to understand that DNCB is slow to work (often taking a month or more) and again, by no means a sure thing. Squaric acid is an alternative to DNCB.
Surgical curettage and electrodessication, under local anesthesia, is potentially the most effective treatment we have for plantar warts—but as you might imagine, piercing the sole of a young child’s foot with a 30-gauge needle is rarely our first choice. It’s the method we used before liquid nitrogen was widely available, and it was a nightmare for all involved. Three outcomes were possible, two quite negative: Serious post-procedure pain and scarring were almost certain. But worst of all, the wart could easily return despite all that. The only time I use this is when the plantar wart is totally resistant to treatment and so large as to interfere with walking.
TAKE-AWAY LEARNING POINTS
• The reason there are 20 or more treatments for warts is that none are remotely perfect.
• Plantar warts are a special problem because they develop on weight-bearing portions of the sole, growing inward (endophytic) in a thick skin layer that allows the virus to avoid detection by the immune system. Plantar warts often cause pain, which treatment can worsen.
• Parents/patients need to understand all of this prior to selecting an appropriate treatment choice.
• They also need to understand that warts do not have to be treated. Most will resolve on their own, eventually.
• Terrorizing children is to be avoided if at all possible. Parents may want their child’s warts to be “taken care of,” but they need to understand this may not be possible.
• Consider referral of problematic plantar warts to dermatology.
The Truth About Poison Ivy
Picture it: It’s 1948. You’re 12, and you’re itching. Then a rash develops. Your mother says you probably have poison ivy—and sure enough, you’ve been thrashing about in the woods where they told you not to go (but you didn’t listen). It never hurt you before, but now the blisters are coming, in long streaks, on your legs and arms. There’s no sleeping and no holding still, not even in church. The itching is so bad, and vinegar and the pink stuff they put on you don’t help at all; they only call more attention to your rash. Everyone, even your own family, is giving you a wide berth, because they all believe poison ivy is contagious.
Six weeks later, the rash and itching are finally gone—but not the memory of this common condition, for which no effective treatment will exist until topical corticosteroids are introduced in 1951.
All these years later, many myths about poison ivy persist. Some are such powerful misconceptions that many people cannot be swayed from them, even by facts. For example, poison ivy is not in the least contagious. Nor is it caused by any kind of “poison.”
The culprit is an oleoresin known as urushiol. This oily resin is contained in the stems, leaves, and flowers of plants from the Toxicodendron genus, which includes poison ivy (by far the most common source), poison oak (found almost exclusively west of the Rockies) and poison sumac (found in limited areas of the southeastern United States). Similar reactions can be caused by exposure to other botanicals, including ficus, fern, fig, mango, and Japanese lacquer trees. (Another member of the Toxicodendron family is the Rhus tree, found mostly in Australia, where it is notorious for causing rashes.)
A history of recent exposure to the great outdoors can therefore usually be obtained, although exposure can also occur through contact with pets or with the clothing of family members who have been exposed. A live plant is not necessary. Many a victim has acquired poison ivy from clearing brush or handling firewood in the dead of winter. (The antigen can also be acquired through an airborne route, such as from the smoke generated by burning brush—even at a considerable distance.) Repeated exposure to poison ivy over several years’ time is required, which explains why children and city-dwelling adults may appear to be immune.
Typically, the blisters begin to appear within 12 to 48 hours of exposure (with some notable exceptions). Much to the consternation of the patient and family, new lesions can continue to manifest for up to two weeks after initial exposure, which is probably why so many people think poison ivy is contagious. The truth is, there is no urushiol in the fluid from the blisters, nor is the antigen “poison” in any way. In short, poison ivy cannot be transmitted from one person to another.
Poison ivy rashes manifest in several different ways. The most common is a type IV delayed hypersensitivity reaction, with pathognomic linear streaks of erythematous patches of edematous, blistery skin. Figure 1 shows a classic linear lesion on the face of a 69-year-old woman who had cleaned out her fence line a few days previously. This particular patient had a similar rash on her chest.
Figure 2 shows a more atypical form of poison ivy, entirely lacking linear lesions or even blisters. The patient’s rash was widespread, but concentrated on popliteal and antecubital areas and medial thighs. It comprised large sheets of highly erythematous skin, in the centers of which were targetoid reddish blue patches. This is a variant of erythema multiforme, which is by definition a secondary condition usually triggered by bugs (strep, herpes simplex virus) or drugs (sulfa, tetracycline, aspirin, penicillin) but occasionally by an exaggerated reaction to antigens such as poison ivy. In this case, this 185-pound 47-year-old woman and her family acquired poison ivy while picking wildflowers in wet weeds—bringing a rapid end to the family vacation.
The most effective treatment for severe, symptomatic poison ivy is the use of systemic glucocorticoids (eg, prednisone) and/or intramuscular injection of a corticosteroid (eg, triamcinolone). Patient 2’s condition was so severe that she couldn’t sleep, eat, or even drive a car. (Interestingly enough, she was the only one who sought medical evaluation. The rest of her family was content to clean out the local pharmacy’s supply of calamine lotion and diphenhydramine capsules.) Severity of this nature demands serious medication—in this case, a two-week taper of prednisone (from 60 mg down to 20 mg) plus an IM injection of triamcinolone (60 mg).
We made this treatment decision with the knowledge that such doses might produce adverse effects, including an increase in appetite, fluid accumulation, irritability, and sleeplessness. Before prescribing these medications, the potential effects were thoroughly discussed with the patient and a history was taken to rule out antecedent diabetes, severe hypertension, intercurrent infection, peptic ulcer disease, or bipolar affective disorder, all of which could be worsened by the use of corticosteroids.
So-called “dosepaks” of corticosteroids are far too weak for such a serious condition, and topical medications—even the most powerful—will be of little benefit. I gave Patient 2 one more thing: a prescription for hydroxyzine hydrochloride (25 mg tablets, to be taken at bedtime), both for sedative and antipruritic effects. For milder cases of poison ivy, I often advise no treatment except topical because the one thing that can be depended on is that poison ivy will resolve on its own, eventually.
I also educate patients about the appearance of the poison ivy plant (see Figure 3). In my part of the country (Oklahoma), where poison ivy is found in virtually every fence line, every creek bank, and every backyard, most people don’t really know what it looks like. Part of that confusion results from the fact that it can take a number of forms, including a vine, often wrapped around trees, a small tree, or even a root, coursing along the ground. Its distinguishing features include the “leaves of three” in typical shapes (darts, with notches, or “thumbs” along the leaf margins), a shiny surface, and white flowers turning into berries.
TAKE-AWAY LEARNING POINTS
• Poison ivy is predominantly found east of the Rocky Mountains and poison oak almost exclusively to the west of them. Poison sumac is limited to the southeastern United States.
• Poison ivy is also known as a form of phytodermatitis, with other botanical sources such as ficus, fig, fern, mango, rhus, and Japanese lacquer trees.
• Poison ivy can grow in the form of a bush, a vine, or even a small tree. However, it also demonstrates the “leaves of three.”
• Linear blisters on an erythematous base is the classic description of a poison ivy reaction, but it can also present in a more diffuse form that concentrates on the popliteal areas and medial thighs.
• Poison ivy is not “poison.” It is the quintessential contact dermatitis, a type IV delayed hypersensitivity reaction to the oil contained in the plant.
• Poison ivy is not contagious and cannot be spread on the patient’s body or to anyone else.
Picture it: It’s 1948. You’re 12, and you’re itching. Then a rash develops. Your mother says you probably have poison ivy—and sure enough, you’ve been thrashing about in the woods where they told you not to go (but you didn’t listen). It never hurt you before, but now the blisters are coming, in long streaks, on your legs and arms. There’s no sleeping and no holding still, not even in church. The itching is so bad, and vinegar and the pink stuff they put on you don’t help at all; they only call more attention to your rash. Everyone, even your own family, is giving you a wide berth, because they all believe poison ivy is contagious.
Six weeks later, the rash and itching are finally gone—but not the memory of this common condition, for which no effective treatment will exist until topical corticosteroids are introduced in 1951.
All these years later, many myths about poison ivy persist. Some are such powerful misconceptions that many people cannot be swayed from them, even by facts. For example, poison ivy is not in the least contagious. Nor is it caused by any kind of “poison.”
The culprit is an oleoresin known as urushiol. This oily resin is contained in the stems, leaves, and flowers of plants from the Toxicodendron genus, which includes poison ivy (by far the most common source), poison oak (found almost exclusively west of the Rockies) and poison sumac (found in limited areas of the southeastern United States). Similar reactions can be caused by exposure to other botanicals, including ficus, fern, fig, mango, and Japanese lacquer trees. (Another member of the Toxicodendron family is the Rhus tree, found mostly in Australia, where it is notorious for causing rashes.)
A history of recent exposure to the great outdoors can therefore usually be obtained, although exposure can also occur through contact with pets or with the clothing of family members who have been exposed. A live plant is not necessary. Many a victim has acquired poison ivy from clearing brush or handling firewood in the dead of winter. (The antigen can also be acquired through an airborne route, such as from the smoke generated by burning brush—even at a considerable distance.) Repeated exposure to poison ivy over several years’ time is required, which explains why children and city-dwelling adults may appear to be immune.
Typically, the blisters begin to appear within 12 to 48 hours of exposure (with some notable exceptions). Much to the consternation of the patient and family, new lesions can continue to manifest for up to two weeks after initial exposure, which is probably why so many people think poison ivy is contagious. The truth is, there is no urushiol in the fluid from the blisters, nor is the antigen “poison” in any way. In short, poison ivy cannot be transmitted from one person to another.
Poison ivy rashes manifest in several different ways. The most common is a type IV delayed hypersensitivity reaction, with pathognomic linear streaks of erythematous patches of edematous, blistery skin. Figure 1 shows a classic linear lesion on the face of a 69-year-old woman who had cleaned out her fence line a few days previously. This particular patient had a similar rash on her chest.
Figure 2 shows a more atypical form of poison ivy, entirely lacking linear lesions or even blisters. The patient’s rash was widespread, but concentrated on popliteal and antecubital areas and medial thighs. It comprised large sheets of highly erythematous skin, in the centers of which were targetoid reddish blue patches. This is a variant of erythema multiforme, which is by definition a secondary condition usually triggered by bugs (strep, herpes simplex virus) or drugs (sulfa, tetracycline, aspirin, penicillin) but occasionally by an exaggerated reaction to antigens such as poison ivy. In this case, this 185-pound 47-year-old woman and her family acquired poison ivy while picking wildflowers in wet weeds—bringing a rapid end to the family vacation.
The most effective treatment for severe, symptomatic poison ivy is the use of systemic glucocorticoids (eg, prednisone) and/or intramuscular injection of a corticosteroid (eg, triamcinolone). Patient 2’s condition was so severe that she couldn’t sleep, eat, or even drive a car. (Interestingly enough, she was the only one who sought medical evaluation. The rest of her family was content to clean out the local pharmacy’s supply of calamine lotion and diphenhydramine capsules.) Severity of this nature demands serious medication—in this case, a two-week taper of prednisone (from 60 mg down to 20 mg) plus an IM injection of triamcinolone (60 mg).
We made this treatment decision with the knowledge that such doses might produce adverse effects, including an increase in appetite, fluid accumulation, irritability, and sleeplessness. Before prescribing these medications, the potential effects were thoroughly discussed with the patient and a history was taken to rule out antecedent diabetes, severe hypertension, intercurrent infection, peptic ulcer disease, or bipolar affective disorder, all of which could be worsened by the use of corticosteroids.
So-called “dosepaks” of corticosteroids are far too weak for such a serious condition, and topical medications—even the most powerful—will be of little benefit. I gave Patient 2 one more thing: a prescription for hydroxyzine hydrochloride (25 mg tablets, to be taken at bedtime), both for sedative and antipruritic effects. For milder cases of poison ivy, I often advise no treatment except topical because the one thing that can be depended on is that poison ivy will resolve on its own, eventually.
I also educate patients about the appearance of the poison ivy plant (see Figure 3). In my part of the country (Oklahoma), where poison ivy is found in virtually every fence line, every creek bank, and every backyard, most people don’t really know what it looks like. Part of that confusion results from the fact that it can take a number of forms, including a vine, often wrapped around trees, a small tree, or even a root, coursing along the ground. Its distinguishing features include the “leaves of three” in typical shapes (darts, with notches, or “thumbs” along the leaf margins), a shiny surface, and white flowers turning into berries.
TAKE-AWAY LEARNING POINTS
• Poison ivy is predominantly found east of the Rocky Mountains and poison oak almost exclusively to the west of them. Poison sumac is limited to the southeastern United States.
• Poison ivy is also known as a form of phytodermatitis, with other botanical sources such as ficus, fig, fern, mango, rhus, and Japanese lacquer trees.
• Poison ivy can grow in the form of a bush, a vine, or even a small tree. However, it also demonstrates the “leaves of three.”
• Linear blisters on an erythematous base is the classic description of a poison ivy reaction, but it can also present in a more diffuse form that concentrates on the popliteal areas and medial thighs.
• Poison ivy is not “poison.” It is the quintessential contact dermatitis, a type IV delayed hypersensitivity reaction to the oil contained in the plant.
• Poison ivy is not contagious and cannot be spread on the patient’s body or to anyone else.
Picture it: It’s 1948. You’re 12, and you’re itching. Then a rash develops. Your mother says you probably have poison ivy—and sure enough, you’ve been thrashing about in the woods where they told you not to go (but you didn’t listen). It never hurt you before, but now the blisters are coming, in long streaks, on your legs and arms. There’s no sleeping and no holding still, not even in church. The itching is so bad, and vinegar and the pink stuff they put on you don’t help at all; they only call more attention to your rash. Everyone, even your own family, is giving you a wide berth, because they all believe poison ivy is contagious.
Six weeks later, the rash and itching are finally gone—but not the memory of this common condition, for which no effective treatment will exist until topical corticosteroids are introduced in 1951.
All these years later, many myths about poison ivy persist. Some are such powerful misconceptions that many people cannot be swayed from them, even by facts. For example, poison ivy is not in the least contagious. Nor is it caused by any kind of “poison.”
The culprit is an oleoresin known as urushiol. This oily resin is contained in the stems, leaves, and flowers of plants from the Toxicodendron genus, which includes poison ivy (by far the most common source), poison oak (found almost exclusively west of the Rockies) and poison sumac (found in limited areas of the southeastern United States). Similar reactions can be caused by exposure to other botanicals, including ficus, fern, fig, mango, and Japanese lacquer trees. (Another member of the Toxicodendron family is the Rhus tree, found mostly in Australia, where it is notorious for causing rashes.)
A history of recent exposure to the great outdoors can therefore usually be obtained, although exposure can also occur through contact with pets or with the clothing of family members who have been exposed. A live plant is not necessary. Many a victim has acquired poison ivy from clearing brush or handling firewood in the dead of winter. (The antigen can also be acquired through an airborne route, such as from the smoke generated by burning brush—even at a considerable distance.) Repeated exposure to poison ivy over several years’ time is required, which explains why children and city-dwelling adults may appear to be immune.
Typically, the blisters begin to appear within 12 to 48 hours of exposure (with some notable exceptions). Much to the consternation of the patient and family, new lesions can continue to manifest for up to two weeks after initial exposure, which is probably why so many people think poison ivy is contagious. The truth is, there is no urushiol in the fluid from the blisters, nor is the antigen “poison” in any way. In short, poison ivy cannot be transmitted from one person to another.
Poison ivy rashes manifest in several different ways. The most common is a type IV delayed hypersensitivity reaction, with pathognomic linear streaks of erythematous patches of edematous, blistery skin. Figure 1 shows a classic linear lesion on the face of a 69-year-old woman who had cleaned out her fence line a few days previously. This particular patient had a similar rash on her chest.
Figure 2 shows a more atypical form of poison ivy, entirely lacking linear lesions or even blisters. The patient’s rash was widespread, but concentrated on popliteal and antecubital areas and medial thighs. It comprised large sheets of highly erythematous skin, in the centers of which were targetoid reddish blue patches. This is a variant of erythema multiforme, which is by definition a secondary condition usually triggered by bugs (strep, herpes simplex virus) or drugs (sulfa, tetracycline, aspirin, penicillin) but occasionally by an exaggerated reaction to antigens such as poison ivy. In this case, this 185-pound 47-year-old woman and her family acquired poison ivy while picking wildflowers in wet weeds—bringing a rapid end to the family vacation.
The most effective treatment for severe, symptomatic poison ivy is the use of systemic glucocorticoids (eg, prednisone) and/or intramuscular injection of a corticosteroid (eg, triamcinolone). Patient 2’s condition was so severe that she couldn’t sleep, eat, or even drive a car. (Interestingly enough, she was the only one who sought medical evaluation. The rest of her family was content to clean out the local pharmacy’s supply of calamine lotion and diphenhydramine capsules.) Severity of this nature demands serious medication—in this case, a two-week taper of prednisone (from 60 mg down to 20 mg) plus an IM injection of triamcinolone (60 mg).
We made this treatment decision with the knowledge that such doses might produce adverse effects, including an increase in appetite, fluid accumulation, irritability, and sleeplessness. Before prescribing these medications, the potential effects were thoroughly discussed with the patient and a history was taken to rule out antecedent diabetes, severe hypertension, intercurrent infection, peptic ulcer disease, or bipolar affective disorder, all of which could be worsened by the use of corticosteroids.
So-called “dosepaks” of corticosteroids are far too weak for such a serious condition, and topical medications—even the most powerful—will be of little benefit. I gave Patient 2 one more thing: a prescription for hydroxyzine hydrochloride (25 mg tablets, to be taken at bedtime), both for sedative and antipruritic effects. For milder cases of poison ivy, I often advise no treatment except topical because the one thing that can be depended on is that poison ivy will resolve on its own, eventually.
I also educate patients about the appearance of the poison ivy plant (see Figure 3). In my part of the country (Oklahoma), where poison ivy is found in virtually every fence line, every creek bank, and every backyard, most people don’t really know what it looks like. Part of that confusion results from the fact that it can take a number of forms, including a vine, often wrapped around trees, a small tree, or even a root, coursing along the ground. Its distinguishing features include the “leaves of three” in typical shapes (darts, with notches, or “thumbs” along the leaf margins), a shiny surface, and white flowers turning into berries.
TAKE-AWAY LEARNING POINTS
• Poison ivy is predominantly found east of the Rocky Mountains and poison oak almost exclusively to the west of them. Poison sumac is limited to the southeastern United States.
• Poison ivy is also known as a form of phytodermatitis, with other botanical sources such as ficus, fig, fern, mango, rhus, and Japanese lacquer trees.
• Poison ivy can grow in the form of a bush, a vine, or even a small tree. However, it also demonstrates the “leaves of three.”
• Linear blisters on an erythematous base is the classic description of a poison ivy reaction, but it can also present in a more diffuse form that concentrates on the popliteal areas and medial thighs.
• Poison ivy is not “poison.” It is the quintessential contact dermatitis, a type IV delayed hypersensitivity reaction to the oil contained in the plant.
• Poison ivy is not contagious and cannot be spread on the patient’s body or to anyone else.
Lifelong Problem Has Caused Embarrassment
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.

Since the fourth grade, this 22-year-old African-American man has had facial lesions that, although constantly present, worsen in the summer. The problem is so severe that it has greatly affected his quality of life: In school and in his neighborhood, he has been subjected to rumors that his condition might be contagious. Despite numerous treatment attempts—including topical and oral anti-acne medications, topical and oral antifungal medications, and oral antibiotics—the condition has persisted. Once, at his mother’s urging, the patient even sought the assistance of a faith healer at a religious revival. Initially seen by a primary care provider at a free clinic, he was then referred to a dermatology clinician at the same facility. History taking reveals that the lesions are asymptomatic and appear in additional locations (eg, arms, ears, and neck). The patient denies any family history of similar problems, as well as persistent fever, cough, or shortness of breath. Lab studies obtained by his primary care provider, including a complete blood count and chem screen, were within normal limits. Most of the lesions on the patient’s face are round areas of slightly erythematous erosion covered by eschar. They range in size from 3 mm to more than 1 cm. Focal postinflammatory hyperpigmentation is noted (a common finding in those with type V/VI skin). Focal hyperpigmentation is also seen on both ears, in some cases with scaling and faint erosion on the surface. A KOH prep is performed with scale collected from perilesional skin; results are negative for fungal elements. There are no palpable nodes in the adjacent nodal locations. Two punch biopsies are done, with samples taken from the active margins of the lesions. One is submitted for routine H&E (hematoxylin and eosin) handling and the other in saline for bacterial, acid-fast bacilli (AFB), and fungal cultures. The biopsy shows hyperkeratosis, follicular plugging, and epidermal atrophy. Marked vacuolar degeneration of the dermoepidermal junction is also noted, along with mucin deposition. Stains for bacteria, AFB, and fungi yield negative results.
An Itch for Which OTC Creams Fail
A 50-year-old man self-refers to dermatology for an acute-onset, very itchy rash on the bottom of his foot. The rash appeared a week ago and is so symptomatic that he is unable to sleep. The patient tried applying OTC hydrocortisone 0.5% cream, but it only seemed to worsen his condition.
The patient denies any other significant health concerns. There is no personal or family history of skin problems; no one else in his household has been affected by this outbreak. He has not traveled internationally or domestically in the recent past. The only thing new in his life is a kitten that was rescued from a local animal shelter and given to his teenage daughter by a friend.
EXAMINATION
The rash, confined to the right instep, is composed of tiny, low vesicles surrounded by peripheral scaling. No overt inflammation is noted, although several of the vesicles (which appear to be drying up) have a slightly inflamed appearance. No rash is observed between the toes or elsewhere on the feet.
Scale is carefully collected (with a #10 blade) from the periphery of the site, as well as the dried roofs of some of the old vesicles. KOH examination shows abundant hyphae.
With his condition thus diagnosed as fungal in origin, the patient is given a written prescription for oxiconazole cream. But when he takes the script to his pharmacy, he discovers his insurance will not cover the cost. With advice from the pharmacist, he buys tolnaftate cream and applies it twice a day.
Despite the use of this product, his symptoms continue unabated throughout the intervening weekend. Very distressed, the patient calls in bright and early on Monday morning to complain. He is able to come in and get samples of the originally prescribed oxiconazole cream, which clears the problem within a week.
DISCUSSION
While “athlete’s foot” is a common problem, neither diagnosis nor treatment is always as simple as one might think. First of all, there are three types of tinea pedis—although interdigital is, by far, the most common. Almost always caused by Trichophyton rubrum, it manifests with a white, macerated look between the fourth and fifth toes (occasionally the third and fourth).
Although heredity may play a significant role in terms of susceptibility, sweat and heat are the major factors in the acquisition of tinea pedis. Persistent sweating (and the wearing of shoes, such as boots, that encourage it) often results in a chronic condition that is unlikely to be “cured.”
Almost any imidazole cream (eg econazole, oxiconazole, or clotrimazole) will at least control it, as will allylamine topical preparations (eg, terbinafine and naftin). Patients should understand that, no matter how earnestly the TV pitchman promotes an antifungal cream as “fast actin’,” nothing will change the fact that tolnaftate is ineffective compared to the medications mentioned above.
The second-most common type is moccasin-variety tinea pedis, which is usually asymptomatic and chronic, presenting with a powdery white fine scale that covers the sides and bottoms of both feet. It rarely needs treatment, in part because it’s asymptomatic but also because most affected patients don’t complain about it. This is a good thing, because a cure is virtually impossible.
This brings us to our case patient, who has the most unusual type of tinea pedis: the inflammatory type, which can be anthropophilic or zoophilic (contracted from man or animal). As this case illustrates, it is usually of acute origin, affects the instep, and is highly symptomatic. Unlike the other types, it manifests with inflammatory vesicles, from which peripheral scaling spreads as the lesions resolve. Abundant hyphae are reliably found in the roofs of resolved vesicles, confirming the diagnosis—although this relatively thick skin may take time to be digested by the alkaline KOH.
Trichophyton mentagrophytes, a common pathogen shed in cat hair, can be difficult to treat. Had this case been more severe, oral terbinafine (250 mg/d for two weeks) might have been added to the oxiconazole to clear the problem. The good news is that this type of tinea pedis tends to be episodic and not chronic. The bad news? If the cat is the culprit (by no means is this certain), the condition may recur.
The differential for this condition includes dyshidrotic eczema, contact dermatitis, and scabies.
TAKE-AWAY LEARNING POINTS
• The least common form of tinea pedis is the inflammatory type, which tends to be of acute onset and highly symptomatic (itchy), typically affects the instep, and presents with vesicles.
• KOH prep must be performed to diagnose this condition; it will reveal large numbers of obvious hyphae. The richest source of sample material is the roof of dried vesicles.
• The hydrocortisone the patient used probably made the fungal infection worse.
• Tolnaftate cream, available OTC, is a relatively ineffective treatment for tinea pedis, compared to the imidazoles and allylamines (no matter what John Madden says).
• Inflammatory tinea pedis is often of zoophilic origin, with cats being a common source.
A 50-year-old man self-refers to dermatology for an acute-onset, very itchy rash on the bottom of his foot. The rash appeared a week ago and is so symptomatic that he is unable to sleep. The patient tried applying OTC hydrocortisone 0.5% cream, but it only seemed to worsen his condition.
The patient denies any other significant health concerns. There is no personal or family history of skin problems; no one else in his household has been affected by this outbreak. He has not traveled internationally or domestically in the recent past. The only thing new in his life is a kitten that was rescued from a local animal shelter and given to his teenage daughter by a friend.
EXAMINATION
The rash, confined to the right instep, is composed of tiny, low vesicles surrounded by peripheral scaling. No overt inflammation is noted, although several of the vesicles (which appear to be drying up) have a slightly inflamed appearance. No rash is observed between the toes or elsewhere on the feet.
Scale is carefully collected (with a #10 blade) from the periphery of the site, as well as the dried roofs of some of the old vesicles. KOH examination shows abundant hyphae.
With his condition thus diagnosed as fungal in origin, the patient is given a written prescription for oxiconazole cream. But when he takes the script to his pharmacy, he discovers his insurance will not cover the cost. With advice from the pharmacist, he buys tolnaftate cream and applies it twice a day.
Despite the use of this product, his symptoms continue unabated throughout the intervening weekend. Very distressed, the patient calls in bright and early on Monday morning to complain. He is able to come in and get samples of the originally prescribed oxiconazole cream, which clears the problem within a week.
DISCUSSION
While “athlete’s foot” is a common problem, neither diagnosis nor treatment is always as simple as one might think. First of all, there are three types of tinea pedis—although interdigital is, by far, the most common. Almost always caused by Trichophyton rubrum, it manifests with a white, macerated look between the fourth and fifth toes (occasionally the third and fourth).
Although heredity may play a significant role in terms of susceptibility, sweat and heat are the major factors in the acquisition of tinea pedis. Persistent sweating (and the wearing of shoes, such as boots, that encourage it) often results in a chronic condition that is unlikely to be “cured.”
Almost any imidazole cream (eg econazole, oxiconazole, or clotrimazole) will at least control it, as will allylamine topical preparations (eg, terbinafine and naftin). Patients should understand that, no matter how earnestly the TV pitchman promotes an antifungal cream as “fast actin’,” nothing will change the fact that tolnaftate is ineffective compared to the medications mentioned above.
The second-most common type is moccasin-variety tinea pedis, which is usually asymptomatic and chronic, presenting with a powdery white fine scale that covers the sides and bottoms of both feet. It rarely needs treatment, in part because it’s asymptomatic but also because most affected patients don’t complain about it. This is a good thing, because a cure is virtually impossible.
This brings us to our case patient, who has the most unusual type of tinea pedis: the inflammatory type, which can be anthropophilic or zoophilic (contracted from man or animal). As this case illustrates, it is usually of acute origin, affects the instep, and is highly symptomatic. Unlike the other types, it manifests with inflammatory vesicles, from which peripheral scaling spreads as the lesions resolve. Abundant hyphae are reliably found in the roofs of resolved vesicles, confirming the diagnosis—although this relatively thick skin may take time to be digested by the alkaline KOH.
Trichophyton mentagrophytes, a common pathogen shed in cat hair, can be difficult to treat. Had this case been more severe, oral terbinafine (250 mg/d for two weeks) might have been added to the oxiconazole to clear the problem. The good news is that this type of tinea pedis tends to be episodic and not chronic. The bad news? If the cat is the culprit (by no means is this certain), the condition may recur.
The differential for this condition includes dyshidrotic eczema, contact dermatitis, and scabies.
TAKE-AWAY LEARNING POINTS
• The least common form of tinea pedis is the inflammatory type, which tends to be of acute onset and highly symptomatic (itchy), typically affects the instep, and presents with vesicles.
• KOH prep must be performed to diagnose this condition; it will reveal large numbers of obvious hyphae. The richest source of sample material is the roof of dried vesicles.
• The hydrocortisone the patient used probably made the fungal infection worse.
• Tolnaftate cream, available OTC, is a relatively ineffective treatment for tinea pedis, compared to the imidazoles and allylamines (no matter what John Madden says).
• Inflammatory tinea pedis is often of zoophilic origin, with cats being a common source.
A 50-year-old man self-refers to dermatology for an acute-onset, very itchy rash on the bottom of his foot. The rash appeared a week ago and is so symptomatic that he is unable to sleep. The patient tried applying OTC hydrocortisone 0.5% cream, but it only seemed to worsen his condition.
The patient denies any other significant health concerns. There is no personal or family history of skin problems; no one else in his household has been affected by this outbreak. He has not traveled internationally or domestically in the recent past. The only thing new in his life is a kitten that was rescued from a local animal shelter and given to his teenage daughter by a friend.
EXAMINATION
The rash, confined to the right instep, is composed of tiny, low vesicles surrounded by peripheral scaling. No overt inflammation is noted, although several of the vesicles (which appear to be drying up) have a slightly inflamed appearance. No rash is observed between the toes or elsewhere on the feet.
Scale is carefully collected (with a #10 blade) from the periphery of the site, as well as the dried roofs of some of the old vesicles. KOH examination shows abundant hyphae.
With his condition thus diagnosed as fungal in origin, the patient is given a written prescription for oxiconazole cream. But when he takes the script to his pharmacy, he discovers his insurance will not cover the cost. With advice from the pharmacist, he buys tolnaftate cream and applies it twice a day.
Despite the use of this product, his symptoms continue unabated throughout the intervening weekend. Very distressed, the patient calls in bright and early on Monday morning to complain. He is able to come in and get samples of the originally prescribed oxiconazole cream, which clears the problem within a week.
DISCUSSION
While “athlete’s foot” is a common problem, neither diagnosis nor treatment is always as simple as one might think. First of all, there are three types of tinea pedis—although interdigital is, by far, the most common. Almost always caused by Trichophyton rubrum, it manifests with a white, macerated look between the fourth and fifth toes (occasionally the third and fourth).
Although heredity may play a significant role in terms of susceptibility, sweat and heat are the major factors in the acquisition of tinea pedis. Persistent sweating (and the wearing of shoes, such as boots, that encourage it) often results in a chronic condition that is unlikely to be “cured.”
Almost any imidazole cream (eg econazole, oxiconazole, or clotrimazole) will at least control it, as will allylamine topical preparations (eg, terbinafine and naftin). Patients should understand that, no matter how earnestly the TV pitchman promotes an antifungal cream as “fast actin’,” nothing will change the fact that tolnaftate is ineffective compared to the medications mentioned above.
The second-most common type is moccasin-variety tinea pedis, which is usually asymptomatic and chronic, presenting with a powdery white fine scale that covers the sides and bottoms of both feet. It rarely needs treatment, in part because it’s asymptomatic but also because most affected patients don’t complain about it. This is a good thing, because a cure is virtually impossible.
This brings us to our case patient, who has the most unusual type of tinea pedis: the inflammatory type, which can be anthropophilic or zoophilic (contracted from man or animal). As this case illustrates, it is usually of acute origin, affects the instep, and is highly symptomatic. Unlike the other types, it manifests with inflammatory vesicles, from which peripheral scaling spreads as the lesions resolve. Abundant hyphae are reliably found in the roofs of resolved vesicles, confirming the diagnosis—although this relatively thick skin may take time to be digested by the alkaline KOH.
Trichophyton mentagrophytes, a common pathogen shed in cat hair, can be difficult to treat. Had this case been more severe, oral terbinafine (250 mg/d for two weeks) might have been added to the oxiconazole to clear the problem. The good news is that this type of tinea pedis tends to be episodic and not chronic. The bad news? If the cat is the culprit (by no means is this certain), the condition may recur.
The differential for this condition includes dyshidrotic eczema, contact dermatitis, and scabies.
TAKE-AWAY LEARNING POINTS
• The least common form of tinea pedis is the inflammatory type, which tends to be of acute onset and highly symptomatic (itchy), typically affects the instep, and presents with vesicles.
• KOH prep must be performed to diagnose this condition; it will reveal large numbers of obvious hyphae. The richest source of sample material is the roof of dried vesicles.
• The hydrocortisone the patient used probably made the fungal infection worse.
• Tolnaftate cream, available OTC, is a relatively ineffective treatment for tinea pedis, compared to the imidazoles and allylamines (no matter what John Madden says).
• Inflammatory tinea pedis is often of zoophilic origin, with cats being a common source.
Unusual Cause for Asymptomatic Rash
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.
Is Man Balding “Just Like Dad”?
ANSWER
The correct answer is alopecia areata (choice “d”), the causes of which are discussed below. It typically manifests with sudden-onset complete hair loss in a well-defined area or areas.
Androgenetic alopecia (choice “a”) is incorrect, since its onset is remarkably gradual and the areas it affects are patterned differently from those seen with alopecia areata.
Kerion (choice “b”) is the name of an edematous, inflamed mass in the scalp triggered by fungal infection (tinea capitis) and is almost always accompanied by broken skin and palpable lymph nodes in the area.
Lichen planopilaris (choice “c”) is lichen planus of the scalp and hair follicles, an inflammatory condition that can involve hair loss of variable size and shape, but not in the same well-defined pattern seen here.
DISCUSSION
There are dermatologists who specialize in diseases of the scalp, especially those resulting in hair loss. In addition to the differential diagnoses mentioned, they see conditions such as lupus, trichotillomania, and reactions to hair care products.
Alopecia areata (AA) seldom needs the attention of these specialists, except in atypical cases. The total hair loss in these well-defined, oval-to-round areas presents fairly acutely, with obviously excessive hair loss noted not only in the scalp but also in the comb, brush, or sink. Although AA is quite common (and thus well known to barbers and hairdressers), it is still often a total and very distressing mystery to the patient. Stress is one of the factors theorized to trigger it—but unfortunately, the more stressed the patient is about the hair loss, the worse it gets.
In the vast majority of cases, the condition resolves, the hair returns, and the grateful patient breathes a sigh of relief. Recurrences, however, are not at all uncommon. A tiny percentage of AA patients go on to lose all the hair in their scalp (alopecia totalis), and an even smaller percentage of those patients go on to lose every hair on their body, permanently (alopecia universalis).
Much has been reported about the cause, which appears to be autoimmune in nature, with an apparent hereditary predisposition. About 10% to 20% of affected patients have a positive family history of AA, and those with severe AA have a positive family history about 16% to 18% of the time.
The theory of an autoimmune basis is also strongly supported by the significantly increased incidence of other autoimmune diseases (especially thyroid disease and vitiligo) in AA patients and their families. But T-cells almost certainly play a role too: Reductions in their number are usually followed by resolution of AA, while increases have the opposite effect. Increased antibodies to various portions of the hair shaft and related structures have now been tied to AA episodes, but these may be epiphenomenal and not causative.
One constant is the perifollicular lymphocytic infiltrate surrounding anagen phase follicles of AA patients. When corticosteroids are administered (eg, by intralesional injection, orally, or systemically), it is this infiltrate that is thereby dissipated, promoting at least temporary hair regrowth. Topically applied steroid preparations are not as helpful, and no known treatment has a positive effect on the ultimate outcome.
Fortunately, most cases of AA resolve satisfactorily with minimal or no treatment. Numerous treatments have been tried for AA, including minoxidil, topical sensitizers (eg, squaric acid, dintrochlorobenzene), and several types of phototherapy. Studies of the efficacy of the various treatments is complicated by the self-limiting nature of the problem.
Predictors of potentially poor outcomes include youth, atopy, extent of involvement, and the presence of ophiasis, a term used to describe extensive involvement of the periphery of the scalp.
ANSWER
The correct answer is alopecia areata (choice “d”), the causes of which are discussed below. It typically manifests with sudden-onset complete hair loss in a well-defined area or areas.
Androgenetic alopecia (choice “a”) is incorrect, since its onset is remarkably gradual and the areas it affects are patterned differently from those seen with alopecia areata.
Kerion (choice “b”) is the name of an edematous, inflamed mass in the scalp triggered by fungal infection (tinea capitis) and is almost always accompanied by broken skin and palpable lymph nodes in the area.
Lichen planopilaris (choice “c”) is lichen planus of the scalp and hair follicles, an inflammatory condition that can involve hair loss of variable size and shape, but not in the same well-defined pattern seen here.
DISCUSSION
There are dermatologists who specialize in diseases of the scalp, especially those resulting in hair loss. In addition to the differential diagnoses mentioned, they see conditions such as lupus, trichotillomania, and reactions to hair care products.
Alopecia areata (AA) seldom needs the attention of these specialists, except in atypical cases. The total hair loss in these well-defined, oval-to-round areas presents fairly acutely, with obviously excessive hair loss noted not only in the scalp but also in the comb, brush, or sink. Although AA is quite common (and thus well known to barbers and hairdressers), it is still often a total and very distressing mystery to the patient. Stress is one of the factors theorized to trigger it—but unfortunately, the more stressed the patient is about the hair loss, the worse it gets.
In the vast majority of cases, the condition resolves, the hair returns, and the grateful patient breathes a sigh of relief. Recurrences, however, are not at all uncommon. A tiny percentage of AA patients go on to lose all the hair in their scalp (alopecia totalis), and an even smaller percentage of those patients go on to lose every hair on their body, permanently (alopecia universalis).
Much has been reported about the cause, which appears to be autoimmune in nature, with an apparent hereditary predisposition. About 10% to 20% of affected patients have a positive family history of AA, and those with severe AA have a positive family history about 16% to 18% of the time.
The theory of an autoimmune basis is also strongly supported by the significantly increased incidence of other autoimmune diseases (especially thyroid disease and vitiligo) in AA patients and their families. But T-cells almost certainly play a role too: Reductions in their number are usually followed by resolution of AA, while increases have the opposite effect. Increased antibodies to various portions of the hair shaft and related structures have now been tied to AA episodes, but these may be epiphenomenal and not causative.
One constant is the perifollicular lymphocytic infiltrate surrounding anagen phase follicles of AA patients. When corticosteroids are administered (eg, by intralesional injection, orally, or systemically), it is this infiltrate that is thereby dissipated, promoting at least temporary hair regrowth. Topically applied steroid preparations are not as helpful, and no known treatment has a positive effect on the ultimate outcome.
Fortunately, most cases of AA resolve satisfactorily with minimal or no treatment. Numerous treatments have been tried for AA, including minoxidil, topical sensitizers (eg, squaric acid, dintrochlorobenzene), and several types of phototherapy. Studies of the efficacy of the various treatments is complicated by the self-limiting nature of the problem.
Predictors of potentially poor outcomes include youth, atopy, extent of involvement, and the presence of ophiasis, a term used to describe extensive involvement of the periphery of the scalp.
ANSWER
The correct answer is alopecia areata (choice “d”), the causes of which are discussed below. It typically manifests with sudden-onset complete hair loss in a well-defined area or areas.
Androgenetic alopecia (choice “a”) is incorrect, since its onset is remarkably gradual and the areas it affects are patterned differently from those seen with alopecia areata.
Kerion (choice “b”) is the name of an edematous, inflamed mass in the scalp triggered by fungal infection (tinea capitis) and is almost always accompanied by broken skin and palpable lymph nodes in the area.
Lichen planopilaris (choice “c”) is lichen planus of the scalp and hair follicles, an inflammatory condition that can involve hair loss of variable size and shape, but not in the same well-defined pattern seen here.
DISCUSSION
There are dermatologists who specialize in diseases of the scalp, especially those resulting in hair loss. In addition to the differential diagnoses mentioned, they see conditions such as lupus, trichotillomania, and reactions to hair care products.
Alopecia areata (AA) seldom needs the attention of these specialists, except in atypical cases. The total hair loss in these well-defined, oval-to-round areas presents fairly acutely, with obviously excessive hair loss noted not only in the scalp but also in the comb, brush, or sink. Although AA is quite common (and thus well known to barbers and hairdressers), it is still often a total and very distressing mystery to the patient. Stress is one of the factors theorized to trigger it—but unfortunately, the more stressed the patient is about the hair loss, the worse it gets.
In the vast majority of cases, the condition resolves, the hair returns, and the grateful patient breathes a sigh of relief. Recurrences, however, are not at all uncommon. A tiny percentage of AA patients go on to lose all the hair in their scalp (alopecia totalis), and an even smaller percentage of those patients go on to lose every hair on their body, permanently (alopecia universalis).
Much has been reported about the cause, which appears to be autoimmune in nature, with an apparent hereditary predisposition. About 10% to 20% of affected patients have a positive family history of AA, and those with severe AA have a positive family history about 16% to 18% of the time.
The theory of an autoimmune basis is also strongly supported by the significantly increased incidence of other autoimmune diseases (especially thyroid disease and vitiligo) in AA patients and their families. But T-cells almost certainly play a role too: Reductions in their number are usually followed by resolution of AA, while increases have the opposite effect. Increased antibodies to various portions of the hair shaft and related structures have now been tied to AA episodes, but these may be epiphenomenal and not causative.
One constant is the perifollicular lymphocytic infiltrate surrounding anagen phase follicles of AA patients. When corticosteroids are administered (eg, by intralesional injection, orally, or systemically), it is this infiltrate that is thereby dissipated, promoting at least temporary hair regrowth. Topically applied steroid preparations are not as helpful, and no known treatment has a positive effect on the ultimate outcome.
Fortunately, most cases of AA resolve satisfactorily with minimal or no treatment. Numerous treatments have been tried for AA, including minoxidil, topical sensitizers (eg, squaric acid, dintrochlorobenzene), and several types of phototherapy. Studies of the efficacy of the various treatments is complicated by the self-limiting nature of the problem.
Predictors of potentially poor outcomes include youth, atopy, extent of involvement, and the presence of ophiasis, a term used to describe extensive involvement of the periphery of the scalp.

A 39-year-old man presents with a two-month history of focal hair loss that has not responded to treatment. His primary care provider prescribed first an antifungal topical cream (clotrimazole/betamethasone bid for two weeks), then an oral antibiotic (cephalexin 500 mg qid for 10 days). Neither helped. His scalp is asymptomatic in the affected area (as well as elsewhere), but the hair loss is extremely upsetting to the patient. He is convinced (and has been told by family members) that he is merely going bald “just like his father.” The onset of his hair loss was rather sudden. It began with increased hair found in his sink and shower, followed by comments from family and coworkers. One friend loaned the patient his minoxidil solution, but twice-daily application for a week failed to slow the rate of hair loss. In general, the patient’s health is excellent; he does not require any maintenance medications. Neither he nor any family members have had any serious illnesses (eg, thyroid disease, lupus, vitiligo) that he could recall. The patient’s hair loss, affecting an approximately 10 x 8–cm area, is confined to the right parietal scalp and has a sharply defined border and strikingly oval shape. The hair loss within this area is complete, with no epidermal disturbance of the involved scalp skin noted on inspection or palpation. No nodes are palpable in the surrounding head or neck. No other areas of hair loss can be seen in hair-bearing areas.
What Actually Qualifies as a “Boil”?
A 49-year-old man self-refers to dermatology for evaluation of new, painful nodules confined to his left axilla. He has never experienced anything like this, although he’s had the occasional “boil” on his legs and trunk in the past two years.
His medical history includes a coronary artery bypass three years ago and a recent follow-up arteriogram, performed in the hospital. It was shortly after this procedure that his axillary lesions appeared.
EXAMINATION
The patient is afebrile but in no distress. His fairly impressive lesions—red, fluctuant, and pus-filled—are confined to the left axilla. There are about 10, each averaging more than a centimeter in diameter. Each lesion is discrete, but none display a central comedone. The right axilla is unaffected.
One of the lesions is incised, releasing a modest amount of pus that is collected and submitted for bacterial culture. With a presumptive diagnosis of methicillin-resistant Staphylococcus aureus (MRSA), the patient is started on trimethoprim/sulfamethoxazole (double strength, bid for a month).
DISCUSSION
This case was clinically consistent with mild furunculosis caused by MRSA—an impression borne out by the bacterial culture and sensitivity. To be more precise, this patient had community-acquired MRSA (CA-MRSA), a relatively minor problem compared to more serious variants such as hospital-acquired MRSA; the latter usually requires hospitalization for delivery of IV antibiotics. (To further confuse the situation, I had to explain to the patient that, although he probably had CA-MRSA, he easily could have acquired it at the hospital where he had his arteriogram.)
The word boil is commonly used by the public to refer to almost any new, red, fluctuant mass. Inflamed epidermal cysts—which don’t usually involve infection—are classic examples of how the term is misused. But what the medical world terms a boil entails skin infection, and two common types of such lesions are furuncles and carbuncles.
Furuncles are red follicular pustules that develop around a hair. Usually of acute onset, furuncles are almost always bright red and often uncomfortable, if not painful. Staph, as in this case, is the most common cause, but not all furunculosis is associated with MRSA. More often, it is caused by relatively trivial normal flora, such as staph epidermidis, by pseudomonas (as in hot tub folliculitis), or even by a yeast-like fungus called Malassezia furfur. Bacterial culture is indicated when furunculosis is significant.
When furuncles coalesce, forming a single large, pus-filled mass in the skin, they are called carbuncles. Common on the neck, groin, and axillae, carbuncles are treated by liberating the contents (incision and drainage) and sometimes are packed to encourage continued drainage. Culture and sensitivity of the contents can guide rational treatment.
As far as the differential, cysts—even inflamed ones—can be of apocrine derivation, especially in the axillae. They can manifest singly or in multiples; one common condition, hidradenitis supprativa, manifests during puberty/menarche with multiple inflamed cysts in intertriginous (skin on skin) locations. There are typically multiple comedones on the surfaces of these lesions. Other types of cysts include pilar cysts (scalp), keratinous cysts (trunk and extremities), digital mucous cysts (fingers and occasionally toes), and ganglion cysts (overlying tendons).
Most cysts have organized, well-defined walls—a useful feature in distinguishing them from furuncles, carbuncles, and abscesses. The last are collections of pus usually associated with inflammation but not with hair follicles. As a result, they are able to form anywhere on the body (most notably, in the mouth). Some abscesses are sterile, such as those caused by heroin or medication injected accidentally into extravascular tissue. Incision and drainage, culture and sensitivity of the contents, and packing of the space are still indicated.
TAKE-HOME LEARNING POINTS
1) Furuncles are collections of pus associated with a hair follicle and are often caused by staph infection.
2) Carbuncles are composed of multiple furuncles that coalesce into a single larger pus-filled lesion, which is often called a “boil.”
3) MRSA is a form of furunculosis caused by Staphylococcus aureus.
4) Cysts can be inflamed but are almost never infected. Cysts have organized walls, a feature that helps distinguish them from furuncles and carbuncles.
5) Abscesses are collections of pus, often associated with inflammation but not with hair follicles.
6) Abscesses can be sterile, or they can be caused by anaerobic bacteria (eg, dental abscesses).
A 49-year-old man self-refers to dermatology for evaluation of new, painful nodules confined to his left axilla. He has never experienced anything like this, although he’s had the occasional “boil” on his legs and trunk in the past two years.
His medical history includes a coronary artery bypass three years ago and a recent follow-up arteriogram, performed in the hospital. It was shortly after this procedure that his axillary lesions appeared.
EXAMINATION
The patient is afebrile but in no distress. His fairly impressive lesions—red, fluctuant, and pus-filled—are confined to the left axilla. There are about 10, each averaging more than a centimeter in diameter. Each lesion is discrete, but none display a central comedone. The right axilla is unaffected.
One of the lesions is incised, releasing a modest amount of pus that is collected and submitted for bacterial culture. With a presumptive diagnosis of methicillin-resistant Staphylococcus aureus (MRSA), the patient is started on trimethoprim/sulfamethoxazole (double strength, bid for a month).
DISCUSSION
This case was clinically consistent with mild furunculosis caused by MRSA—an impression borne out by the bacterial culture and sensitivity. To be more precise, this patient had community-acquired MRSA (CA-MRSA), a relatively minor problem compared to more serious variants such as hospital-acquired MRSA; the latter usually requires hospitalization for delivery of IV antibiotics. (To further confuse the situation, I had to explain to the patient that, although he probably had CA-MRSA, he easily could have acquired it at the hospital where he had his arteriogram.)
The word boil is commonly used by the public to refer to almost any new, red, fluctuant mass. Inflamed epidermal cysts—which don’t usually involve infection—are classic examples of how the term is misused. But what the medical world terms a boil entails skin infection, and two common types of such lesions are furuncles and carbuncles.
Furuncles are red follicular pustules that develop around a hair. Usually of acute onset, furuncles are almost always bright red and often uncomfortable, if not painful. Staph, as in this case, is the most common cause, but not all furunculosis is associated with MRSA. More often, it is caused by relatively trivial normal flora, such as staph epidermidis, by pseudomonas (as in hot tub folliculitis), or even by a yeast-like fungus called Malassezia furfur. Bacterial culture is indicated when furunculosis is significant.
When furuncles coalesce, forming a single large, pus-filled mass in the skin, they are called carbuncles. Common on the neck, groin, and axillae, carbuncles are treated by liberating the contents (incision and drainage) and sometimes are packed to encourage continued drainage. Culture and sensitivity of the contents can guide rational treatment.
As far as the differential, cysts—even inflamed ones—can be of apocrine derivation, especially in the axillae. They can manifest singly or in multiples; one common condition, hidradenitis supprativa, manifests during puberty/menarche with multiple inflamed cysts in intertriginous (skin on skin) locations. There are typically multiple comedones on the surfaces of these lesions. Other types of cysts include pilar cysts (scalp), keratinous cysts (trunk and extremities), digital mucous cysts (fingers and occasionally toes), and ganglion cysts (overlying tendons).
Most cysts have organized, well-defined walls—a useful feature in distinguishing them from furuncles, carbuncles, and abscesses. The last are collections of pus usually associated with inflammation but not with hair follicles. As a result, they are able to form anywhere on the body (most notably, in the mouth). Some abscesses are sterile, such as those caused by heroin or medication injected accidentally into extravascular tissue. Incision and drainage, culture and sensitivity of the contents, and packing of the space are still indicated.
TAKE-HOME LEARNING POINTS
1) Furuncles are collections of pus associated with a hair follicle and are often caused by staph infection.
2) Carbuncles are composed of multiple furuncles that coalesce into a single larger pus-filled lesion, which is often called a “boil.”
3) MRSA is a form of furunculosis caused by Staphylococcus aureus.
4) Cysts can be inflamed but are almost never infected. Cysts have organized walls, a feature that helps distinguish them from furuncles and carbuncles.
5) Abscesses are collections of pus, often associated with inflammation but not with hair follicles.
6) Abscesses can be sterile, or they can be caused by anaerobic bacteria (eg, dental abscesses).
A 49-year-old man self-refers to dermatology for evaluation of new, painful nodules confined to his left axilla. He has never experienced anything like this, although he’s had the occasional “boil” on his legs and trunk in the past two years.
His medical history includes a coronary artery bypass three years ago and a recent follow-up arteriogram, performed in the hospital. It was shortly after this procedure that his axillary lesions appeared.
EXAMINATION
The patient is afebrile but in no distress. His fairly impressive lesions—red, fluctuant, and pus-filled—are confined to the left axilla. There are about 10, each averaging more than a centimeter in diameter. Each lesion is discrete, but none display a central comedone. The right axilla is unaffected.
One of the lesions is incised, releasing a modest amount of pus that is collected and submitted for bacterial culture. With a presumptive diagnosis of methicillin-resistant Staphylococcus aureus (MRSA), the patient is started on trimethoprim/sulfamethoxazole (double strength, bid for a month).
DISCUSSION
This case was clinically consistent with mild furunculosis caused by MRSA—an impression borne out by the bacterial culture and sensitivity. To be more precise, this patient had community-acquired MRSA (CA-MRSA), a relatively minor problem compared to more serious variants such as hospital-acquired MRSA; the latter usually requires hospitalization for delivery of IV antibiotics. (To further confuse the situation, I had to explain to the patient that, although he probably had CA-MRSA, he easily could have acquired it at the hospital where he had his arteriogram.)
The word boil is commonly used by the public to refer to almost any new, red, fluctuant mass. Inflamed epidermal cysts—which don’t usually involve infection—are classic examples of how the term is misused. But what the medical world terms a boil entails skin infection, and two common types of such lesions are furuncles and carbuncles.
Furuncles are red follicular pustules that develop around a hair. Usually of acute onset, furuncles are almost always bright red and often uncomfortable, if not painful. Staph, as in this case, is the most common cause, but not all furunculosis is associated with MRSA. More often, it is caused by relatively trivial normal flora, such as staph epidermidis, by pseudomonas (as in hot tub folliculitis), or even by a yeast-like fungus called Malassezia furfur. Bacterial culture is indicated when furunculosis is significant.
When furuncles coalesce, forming a single large, pus-filled mass in the skin, they are called carbuncles. Common on the neck, groin, and axillae, carbuncles are treated by liberating the contents (incision and drainage) and sometimes are packed to encourage continued drainage. Culture and sensitivity of the contents can guide rational treatment.
As far as the differential, cysts—even inflamed ones—can be of apocrine derivation, especially in the axillae. They can manifest singly or in multiples; one common condition, hidradenitis supprativa, manifests during puberty/menarche with multiple inflamed cysts in intertriginous (skin on skin) locations. There are typically multiple comedones on the surfaces of these lesions. Other types of cysts include pilar cysts (scalp), keratinous cysts (trunk and extremities), digital mucous cysts (fingers and occasionally toes), and ganglion cysts (overlying tendons).
Most cysts have organized, well-defined walls—a useful feature in distinguishing them from furuncles, carbuncles, and abscesses. The last are collections of pus usually associated with inflammation but not with hair follicles. As a result, they are able to form anywhere on the body (most notably, in the mouth). Some abscesses are sterile, such as those caused by heroin or medication injected accidentally into extravascular tissue. Incision and drainage, culture and sensitivity of the contents, and packing of the space are still indicated.
TAKE-HOME LEARNING POINTS
1) Furuncles are collections of pus associated with a hair follicle and are often caused by staph infection.
2) Carbuncles are composed of multiple furuncles that coalesce into a single larger pus-filled lesion, which is often called a “boil.”
3) MRSA is a form of furunculosis caused by Staphylococcus aureus.
4) Cysts can be inflamed but are almost never infected. Cysts have organized walls, a feature that helps distinguish them from furuncles and carbuncles.
5) Abscesses are collections of pus, often associated with inflammation but not with hair follicles.
6) Abscesses can be sterile, or they can be caused by anaerobic bacteria (eg, dental abscesses).
The Truth About Melanoma
Much energy is expended—by patients, parents, publishers, and providers—in obsessing over, looking for, and preventing malignant melanoma. A day rarely goes by without a story in the media purporting to inform the reader about this dreaded cancer.
On the one hand, who can argue with the provision of information that has the potential to save lives and reduce suffering? The answer is: I can.
What I see in the popular media is a veritable cornucopia of misinformation—often rehashed myths, vast generalizations, and the like—that all too often serves to confuse, obfuscate, and generally perpetuate the most dangerous misconceptions. Many of them lead to totally unnecessary deaths.
I know this not only because I read these articles but also because I see the worried patients who’ve read them. They come in to “get their moles checked,” for example, since they’ve been told “that’s where melanomas come from.” As with all myths, there is a grain of truth in that concept, but it is dangerously misleading, as is much of the other information passed on in these pieces.
Unfortunately, many medical providers are as influenced by these reports as the general public. And while I can’t reach the general public, I can reach a few hundred thousand medical professionals with some facts that have the potential to save lives (maybe even their own).
MYTH # 1: MELANOMAS COME FROM MOLES
Easily the most common “melanoma myth,” this is possibly the most dangerous. While patients are busy watching their “moles,” the melanoma is on its way to killing them.
The problem, of course, is the word mole, which means different things to different people. Most patients who use this word mean the raised, fleshy, often hair-bearing papule or nodule on their face, arm, or back, that can be present without changing for years. When that is the case, there is little or no potential for these lesions—usually compound versus intradermal nevi—to undergo malignant transformation. No physical event (trauma, chemicals, or sun exposure) can turn a benign nevus into a cancer.
What we as medical professionals are looking for in any lesion is a history of change: growth, color, elevation, erosion/ulceration. When these are present, our course is clear: We remove the lesion and send it for pathologic evaluation. Just because malignant transformation of a nevus is unlikely doesn’t mean it can’t happen.
MYTH # 2: SUN CAUSES MELANOMA, SO LESIONS ON NON–SUN-EXPOSED SKIN CAN’T BE MELANOMAS
The truth is that about 80% of melanomas are found in areas normally covered by clothing, such as legs, abdomens, thighs, and even the bottoms of the feet, in the scalp, and on genitals. Yes, sun is unquestionably the cause, but the sun does not necessarily have to strike the affected area.
This is only one of a number of seeming contradictions about melanoma. It’s important to understand and accept this fact even if it makes no sense, because lives are in the balance. Many tragic deaths have occurred because of a failure to understand and accept this reality.
MYTH # 3: MELANOMAS MANIFEST AS RAISED LUMPS ON THE SKIN
Dermatology providers see and hear this all day, every day. Seborrheic keratoses typify this misperception. However, they also serve as a terrific example of the benignancy of most epidermal lesions (ie, ones that are “stuck on” the outer layer of skin and thus easily peeled off), which are usually warty, rough and colored brown, tan, gray, or a combination of these colors. They’re usually present in multiples, another good sign (in general), but they are the source of endless worry for patients and providers.
The truth is that at least 80% of melanomas are essentially macular (flat) enough to be difficult to palpate, and they almost never appear in multiples. Having said this, I should note that melanomas can certainly be raised on the skin—but these are in the minority of cases. Again, change is the key thing to watch for/ask about, but not change that occurs overnight or from known trauma.
Much energy is expended—by patients, parents, publishers, and providers—in obsessing over, looking for, and preventing malignant melanoma. A day rarely goes by without a story in the media purporting to inform the reader about this dreaded cancer.
On the one hand, who can argue with the provision of information that has the potential to save lives and reduce suffering? The answer is: I can.
What I see in the popular media is a veritable cornucopia of misinformation—often rehashed myths, vast generalizations, and the like—that all too often serves to confuse, obfuscate, and generally perpetuate the most dangerous misconceptions. Many of them lead to totally unnecessary deaths.
I know this not only because I read these articles but also because I see the worried patients who’ve read them. They come in to “get their moles checked,” for example, since they’ve been told “that’s where melanomas come from.” As with all myths, there is a grain of truth in that concept, but it is dangerously misleading, as is much of the other information passed on in these pieces.
Unfortunately, many medical providers are as influenced by these reports as the general public. And while I can’t reach the general public, I can reach a few hundred thousand medical professionals with some facts that have the potential to save lives (maybe even their own).
MYTH # 1: MELANOMAS COME FROM MOLES
Easily the most common “melanoma myth,” this is possibly the most dangerous. While patients are busy watching their “moles,” the melanoma is on its way to killing them.
The problem, of course, is the word mole, which means different things to different people. Most patients who use this word mean the raised, fleshy, often hair-bearing papule or nodule on their face, arm, or back, that can be present without changing for years. When that is the case, there is little or no potential for these lesions—usually compound versus intradermal nevi—to undergo malignant transformation. No physical event (trauma, chemicals, or sun exposure) can turn a benign nevus into a cancer.
What we as medical professionals are looking for in any lesion is a history of change: growth, color, elevation, erosion/ulceration. When these are present, our course is clear: We remove the lesion and send it for pathologic evaluation. Just because malignant transformation of a nevus is unlikely doesn’t mean it can’t happen.
MYTH # 2: SUN CAUSES MELANOMA, SO LESIONS ON NON–SUN-EXPOSED SKIN CAN’T BE MELANOMAS
The truth is that about 80% of melanomas are found in areas normally covered by clothing, such as legs, abdomens, thighs, and even the bottoms of the feet, in the scalp, and on genitals. Yes, sun is unquestionably the cause, but the sun does not necessarily have to strike the affected area.
This is only one of a number of seeming contradictions about melanoma. It’s important to understand and accept this fact even if it makes no sense, because lives are in the balance. Many tragic deaths have occurred because of a failure to understand and accept this reality.
MYTH # 3: MELANOMAS MANIFEST AS RAISED LUMPS ON THE SKIN
Dermatology providers see and hear this all day, every day. Seborrheic keratoses typify this misperception. However, they also serve as a terrific example of the benignancy of most epidermal lesions (ie, ones that are “stuck on” the outer layer of skin and thus easily peeled off), which are usually warty, rough and colored brown, tan, gray, or a combination of these colors. They’re usually present in multiples, another good sign (in general), but they are the source of endless worry for patients and providers.
The truth is that at least 80% of melanomas are essentially macular (flat) enough to be difficult to palpate, and they almost never appear in multiples. Having said this, I should note that melanomas can certainly be raised on the skin—but these are in the minority of cases. Again, change is the key thing to watch for/ask about, but not change that occurs overnight or from known trauma.
Much energy is expended—by patients, parents, publishers, and providers—in obsessing over, looking for, and preventing malignant melanoma. A day rarely goes by without a story in the media purporting to inform the reader about this dreaded cancer.
On the one hand, who can argue with the provision of information that has the potential to save lives and reduce suffering? The answer is: I can.
What I see in the popular media is a veritable cornucopia of misinformation—often rehashed myths, vast generalizations, and the like—that all too often serves to confuse, obfuscate, and generally perpetuate the most dangerous misconceptions. Many of them lead to totally unnecessary deaths.
I know this not only because I read these articles but also because I see the worried patients who’ve read them. They come in to “get their moles checked,” for example, since they’ve been told “that’s where melanomas come from.” As with all myths, there is a grain of truth in that concept, but it is dangerously misleading, as is much of the other information passed on in these pieces.
Unfortunately, many medical providers are as influenced by these reports as the general public. And while I can’t reach the general public, I can reach a few hundred thousand medical professionals with some facts that have the potential to save lives (maybe even their own).
MYTH # 1: MELANOMAS COME FROM MOLES
Easily the most common “melanoma myth,” this is possibly the most dangerous. While patients are busy watching their “moles,” the melanoma is on its way to killing them.
The problem, of course, is the word mole, which means different things to different people. Most patients who use this word mean the raised, fleshy, often hair-bearing papule or nodule on their face, arm, or back, that can be present without changing for years. When that is the case, there is little or no potential for these lesions—usually compound versus intradermal nevi—to undergo malignant transformation. No physical event (trauma, chemicals, or sun exposure) can turn a benign nevus into a cancer.
What we as medical professionals are looking for in any lesion is a history of change: growth, color, elevation, erosion/ulceration. When these are present, our course is clear: We remove the lesion and send it for pathologic evaluation. Just because malignant transformation of a nevus is unlikely doesn’t mean it can’t happen.
MYTH # 2: SUN CAUSES MELANOMA, SO LESIONS ON NON–SUN-EXPOSED SKIN CAN’T BE MELANOMAS
The truth is that about 80% of melanomas are found in areas normally covered by clothing, such as legs, abdomens, thighs, and even the bottoms of the feet, in the scalp, and on genitals. Yes, sun is unquestionably the cause, but the sun does not necessarily have to strike the affected area.
This is only one of a number of seeming contradictions about melanoma. It’s important to understand and accept this fact even if it makes no sense, because lives are in the balance. Many tragic deaths have occurred because of a failure to understand and accept this reality.
MYTH # 3: MELANOMAS MANIFEST AS RAISED LUMPS ON THE SKIN
Dermatology providers see and hear this all day, every day. Seborrheic keratoses typify this misperception. However, they also serve as a terrific example of the benignancy of most epidermal lesions (ie, ones that are “stuck on” the outer layer of skin and thus easily peeled off), which are usually warty, rough and colored brown, tan, gray, or a combination of these colors. They’re usually present in multiples, another good sign (in general), but they are the source of endless worry for patients and providers.
The truth is that at least 80% of melanomas are essentially macular (flat) enough to be difficult to palpate, and they almost never appear in multiples. Having said this, I should note that melanomas can certainly be raised on the skin—but these are in the minority of cases. Again, change is the key thing to watch for/ask about, but not change that occurs overnight or from known trauma.
Not Just Another Groin Rash
ANSWER
The correct answer is fungal infection (choice “a”). If this condition had been fungal, it would have responded to one or more of the medications used to treat it. In this case, treatment failure demanded consideration of alternate diagnostic possibilities.
Lichen simplex chronicus (choice “b”), also known as neurodermatitis, was a good possibility, since it is the consequence of chronic rubbing or scratching in response to the itching caused by, for example, eczema.
Psoriasis (choice “c”) usually has adherent white scale on its surface, unless it’s in an intertriginous (skin on skin) area where scale gets rubbed off by friction.
The patient’s actual diagnosis, however, turned out to be Paget’s disease (choice “d”). See the Discussion for relevant details.
DISCUSSION
Biopsy showed changes consistent with a type of skin cancer called extramammary Paget’s disease (EMPD), an intradermal adenocarcinoma that tends to develop in areas where apocrine glands are found (eg, the anogenital and axillary areas).
The majority of EMPD cases represent adenocarcinoma in situ with extension from adnexal structures. Intraepidermal metastasis from noncutaneous adenocarcinomas (via local or lymphatic routes) accounts for a significant minority of cases (< 25%). Urogenital and colorectal carcinomas are the most common.
EMPD is more common in women and is rare before age 40. In addition to the usual intertriginous areas, other sites in which it may be found include eyelids and ears. The lesions typically itch but rarely hurt; they do, however, inevitably grow larger and more extensive.
The histologic changes of EMPD are identical to those seen in mammary Paget’s disease, though the latter virtually always involves the areola and nipple. It also signals the presence of an underlying intraductal breast cancer.
The main teaching point to be gleaned from this case is the concept of “cancer presenting as a rash,” of which there are several examples: cutaneous T-cell lymphoma, B-cell lymphoma, metastatic breast cancer, superficial basal cell carcinoma, and intraepidermal squamous cell carcinoma (Bowen’s disease).
EMPD is especially prone to being overlooked, not only because groin rashes are so common but also because most skin cancers are “lesional” (ie, they take the form of a papule or nodule). Any rash that proves to be unresponsive to ordinary treatment should be either referred to dermatology or biopsied.
TREATMENT
This patient was prescribed imiquimod 5% cream, to be applied three times a week, which has a good chance of clearing the condition (but only after three to four months of application). If this fails, the patient will be referred for Mohs surgery.
Even so, recurrences are common. About 25% of EMPD patients with underlying malignancies eventually die of their disease. For these reasons, the patient was referred back to his primary care provider for workup for a possible underlying malignancy.
ANSWER
The correct answer is fungal infection (choice “a”). If this condition had been fungal, it would have responded to one or more of the medications used to treat it. In this case, treatment failure demanded consideration of alternate diagnostic possibilities.
Lichen simplex chronicus (choice “b”), also known as neurodermatitis, was a good possibility, since it is the consequence of chronic rubbing or scratching in response to the itching caused by, for example, eczema.
Psoriasis (choice “c”) usually has adherent white scale on its surface, unless it’s in an intertriginous (skin on skin) area where scale gets rubbed off by friction.
The patient’s actual diagnosis, however, turned out to be Paget’s disease (choice “d”). See the Discussion for relevant details.
DISCUSSION
Biopsy showed changes consistent with a type of skin cancer called extramammary Paget’s disease (EMPD), an intradermal adenocarcinoma that tends to develop in areas where apocrine glands are found (eg, the anogenital and axillary areas).
The majority of EMPD cases represent adenocarcinoma in situ with extension from adnexal structures. Intraepidermal metastasis from noncutaneous adenocarcinomas (via local or lymphatic routes) accounts for a significant minority of cases (< 25%). Urogenital and colorectal carcinomas are the most common.
EMPD is more common in women and is rare before age 40. In addition to the usual intertriginous areas, other sites in which it may be found include eyelids and ears. The lesions typically itch but rarely hurt; they do, however, inevitably grow larger and more extensive.
The histologic changes of EMPD are identical to those seen in mammary Paget’s disease, though the latter virtually always involves the areola and nipple. It also signals the presence of an underlying intraductal breast cancer.
The main teaching point to be gleaned from this case is the concept of “cancer presenting as a rash,” of which there are several examples: cutaneous T-cell lymphoma, B-cell lymphoma, metastatic breast cancer, superficial basal cell carcinoma, and intraepidermal squamous cell carcinoma (Bowen’s disease).
EMPD is especially prone to being overlooked, not only because groin rashes are so common but also because most skin cancers are “lesional” (ie, they take the form of a papule or nodule). Any rash that proves to be unresponsive to ordinary treatment should be either referred to dermatology or biopsied.
TREATMENT
This patient was prescribed imiquimod 5% cream, to be applied three times a week, which has a good chance of clearing the condition (but only after three to four months of application). If this fails, the patient will be referred for Mohs surgery.
Even so, recurrences are common. About 25% of EMPD patients with underlying malignancies eventually die of their disease. For these reasons, the patient was referred back to his primary care provider for workup for a possible underlying malignancy.
ANSWER
The correct answer is fungal infection (choice “a”). If this condition had been fungal, it would have responded to one or more of the medications used to treat it. In this case, treatment failure demanded consideration of alternate diagnostic possibilities.
Lichen simplex chronicus (choice “b”), also known as neurodermatitis, was a good possibility, since it is the consequence of chronic rubbing or scratching in response to the itching caused by, for example, eczema.
Psoriasis (choice “c”) usually has adherent white scale on its surface, unless it’s in an intertriginous (skin on skin) area where scale gets rubbed off by friction.
The patient’s actual diagnosis, however, turned out to be Paget’s disease (choice “d”). See the Discussion for relevant details.
DISCUSSION
Biopsy showed changes consistent with a type of skin cancer called extramammary Paget’s disease (EMPD), an intradermal adenocarcinoma that tends to develop in areas where apocrine glands are found (eg, the anogenital and axillary areas).
The majority of EMPD cases represent adenocarcinoma in situ with extension from adnexal structures. Intraepidermal metastasis from noncutaneous adenocarcinomas (via local or lymphatic routes) accounts for a significant minority of cases (< 25%). Urogenital and colorectal carcinomas are the most common.
EMPD is more common in women and is rare before age 40. In addition to the usual intertriginous areas, other sites in which it may be found include eyelids and ears. The lesions typically itch but rarely hurt; they do, however, inevitably grow larger and more extensive.
The histologic changes of EMPD are identical to those seen in mammary Paget’s disease, though the latter virtually always involves the areola and nipple. It also signals the presence of an underlying intraductal breast cancer.
The main teaching point to be gleaned from this case is the concept of “cancer presenting as a rash,” of which there are several examples: cutaneous T-cell lymphoma, B-cell lymphoma, metastatic breast cancer, superficial basal cell carcinoma, and intraepidermal squamous cell carcinoma (Bowen’s disease).
EMPD is especially prone to being overlooked, not only because groin rashes are so common but also because most skin cancers are “lesional” (ie, they take the form of a papule or nodule). Any rash that proves to be unresponsive to ordinary treatment should be either referred to dermatology or biopsied.
TREATMENT
This patient was prescribed imiquimod 5% cream, to be applied three times a week, which has a good chance of clearing the condition (but only after three to four months of application). If this fails, the patient will be referred for Mohs surgery.
Even so, recurrences are common. About 25% of EMPD patients with underlying malignancies eventually die of their disease. For these reasons, the patient was referred back to his primary care provider for workup for a possible underlying malignancy.

A 60-year-old man is referred to dermatology for evaluation of a somewhat itchy, unilateral groin rash. For several years, it has waxed and waned, never completely resolving. Recently, the rash has grown in size, and the itching has intensified, causing the patient to lose sleep. The patient has tried several OTC and prescription topical medications for this problem: creams containing clotrimazole, tolnaftate, 1% hydrocortisone, and betamethasone/clotrimazole, as well as triple-antibiotic ointment and several different moisturizing creams and lotions. He also tried a two-week course of oral terbinafine (250 mg/d). Additional questioning reveals a history of atopy, eczema, and asthma as a child. There is a strong family history of similar problems. This strikingly red, blistery-appearing rash is palm-sized and confined to the right groin. It has a fairly well–defined, scaly border that is KOH-negative on microscopic examination. Within the borders of this lesion are several focal, shiny, somewhat atrophic areas in which no epidermal adnexae (pores, follicles, hair, skin lines) can be seen.
A Compulsion to Scratch, But Is There an Itch?
ANSWER
The correct answer is neurotic excoriations (choice “d”), a chronic condition thought to be a psychologic process with dermatologic manifestations, consciously created by repetitive scratching and rubbing. Focally, it can manifest with skin alterations very similar to lichen simplex chronicus (choice “a”; also known as neurodermatitis), but the latter refers to very limited, localized processes and does not involve the psychiatric overlay seen with neurotic excoriations.
Patients with dermatitis artefacta (choice “b”; formerly called factitial dermatitis) consciously create their lesions for secondary gain, often using sharp objects such as nail files, kitchen utensils, or even shards of broken glass. Dermatitis artefacta lesions, which are relatively sparse and bizarre in appearance, can also be created by the application of caustic chemicals, or even by injection of foreign substances.
The differential rightly includes any number of skin conditions such as bullous pemphigoid (choice “c”). However, this was effectively ruled out by the biopsy and also by the morphology and extended chronicity of the patient’s complaint.
DISCUSSION
Neurotic excoriations (NE) are usually created by unconscious picking, scratching, or rubbing. There may be a precipitating minor skin pathology (eg, insect bite, folliculitis or acne), but it can develop independent of any such process. Its origins can often be tied to upsetting life events, such as divorce, death, or early dementia.
More history taking from this patient and her family revealed that her skin problems began after her husband died in an accident, after which, according to her children, “she has never been the same.” Her picking accelerated when she moved to an assisted living setting.
Because patients create neurotic excoriations, their lesions have the quality of an “outside job,” with clean linear erosions, crusts, and scars that can be hypopigmented or hyperpigmented, depending on the patient’s skin type. Similar in size and shape, the lesions tend to be bilaterally and symmetrically distributed and confined to areas within easy reach, such as the extensor surfaces of the arms and the upper part of the back.
The vast majority of NE patients are adult women, though it is also seen in children as a manifestation of comorbid psychopathology or other psychosocial stressor.
TREATMENT
As one might expect, treatment of NE is difficult, particularly since many patients find it impossible to accept the role their mental state plays in the creation and perpetuation of their condition. In the best of all possible scenarios, the patient would be seen and followed by a psychiatrist, who would probably prescribe psychoactive medication.
Failing that—or even in addition to that treatment—one could, at a minimum, find ways to distract the patient, trim her nails as much as possible, and/or place barriers between the offending nails and the skin in question.
Topical medications, such as steroid creams, are of very limited usefulness, as are oral antibiotics and antihistamines.
ANSWER
The correct answer is neurotic excoriations (choice “d”), a chronic condition thought to be a psychologic process with dermatologic manifestations, consciously created by repetitive scratching and rubbing. Focally, it can manifest with skin alterations very similar to lichen simplex chronicus (choice “a”; also known as neurodermatitis), but the latter refers to very limited, localized processes and does not involve the psychiatric overlay seen with neurotic excoriations.
Patients with dermatitis artefacta (choice “b”; formerly called factitial dermatitis) consciously create their lesions for secondary gain, often using sharp objects such as nail files, kitchen utensils, or even shards of broken glass. Dermatitis artefacta lesions, which are relatively sparse and bizarre in appearance, can also be created by the application of caustic chemicals, or even by injection of foreign substances.
The differential rightly includes any number of skin conditions such as bullous pemphigoid (choice “c”). However, this was effectively ruled out by the biopsy and also by the morphology and extended chronicity of the patient’s complaint.
DISCUSSION
Neurotic excoriations (NE) are usually created by unconscious picking, scratching, or rubbing. There may be a precipitating minor skin pathology (eg, insect bite, folliculitis or acne), but it can develop independent of any such process. Its origins can often be tied to upsetting life events, such as divorce, death, or early dementia.
More history taking from this patient and her family revealed that her skin problems began after her husband died in an accident, after which, according to her children, “she has never been the same.” Her picking accelerated when she moved to an assisted living setting.
Because patients create neurotic excoriations, their lesions have the quality of an “outside job,” with clean linear erosions, crusts, and scars that can be hypopigmented or hyperpigmented, depending on the patient’s skin type. Similar in size and shape, the lesions tend to be bilaterally and symmetrically distributed and confined to areas within easy reach, such as the extensor surfaces of the arms and the upper part of the back.
The vast majority of NE patients are adult women, though it is also seen in children as a manifestation of comorbid psychopathology or other psychosocial stressor.
TREATMENT
As one might expect, treatment of NE is difficult, particularly since many patients find it impossible to accept the role their mental state plays in the creation and perpetuation of their condition. In the best of all possible scenarios, the patient would be seen and followed by a psychiatrist, who would probably prescribe psychoactive medication.
Failing that—or even in addition to that treatment—one could, at a minimum, find ways to distract the patient, trim her nails as much as possible, and/or place barriers between the offending nails and the skin in question.
Topical medications, such as steroid creams, are of very limited usefulness, as are oral antibiotics and antihistamines.
ANSWER
The correct answer is neurotic excoriations (choice “d”), a chronic condition thought to be a psychologic process with dermatologic manifestations, consciously created by repetitive scratching and rubbing. Focally, it can manifest with skin alterations very similar to lichen simplex chronicus (choice “a”; also known as neurodermatitis), but the latter refers to very limited, localized processes and does not involve the psychiatric overlay seen with neurotic excoriations.
Patients with dermatitis artefacta (choice “b”; formerly called factitial dermatitis) consciously create their lesions for secondary gain, often using sharp objects such as nail files, kitchen utensils, or even shards of broken glass. Dermatitis artefacta lesions, which are relatively sparse and bizarre in appearance, can also be created by the application of caustic chemicals, or even by injection of foreign substances.
The differential rightly includes any number of skin conditions such as bullous pemphigoid (choice “c”). However, this was effectively ruled out by the biopsy and also by the morphology and extended chronicity of the patient’s complaint.
DISCUSSION
Neurotic excoriations (NE) are usually created by unconscious picking, scratching, or rubbing. There may be a precipitating minor skin pathology (eg, insect bite, folliculitis or acne), but it can develop independent of any such process. Its origins can often be tied to upsetting life events, such as divorce, death, or early dementia.
More history taking from this patient and her family revealed that her skin problems began after her husband died in an accident, after which, according to her children, “she has never been the same.” Her picking accelerated when she moved to an assisted living setting.
Because patients create neurotic excoriations, their lesions have the quality of an “outside job,” with clean linear erosions, crusts, and scars that can be hypopigmented or hyperpigmented, depending on the patient’s skin type. Similar in size and shape, the lesions tend to be bilaterally and symmetrically distributed and confined to areas within easy reach, such as the extensor surfaces of the arms and the upper part of the back.
The vast majority of NE patients are adult women, though it is also seen in children as a manifestation of comorbid psychopathology or other psychosocial stressor.
TREATMENT
As one might expect, treatment of NE is difficult, particularly since many patients find it impossible to accept the role their mental state plays in the creation and perpetuation of their condition. In the best of all possible scenarios, the patient would be seen and followed by a psychiatrist, who would probably prescribe psychoactive medication.
Failing that—or even in addition to that treatment—one could, at a minimum, find ways to distract the patient, trim her nails as much as possible, and/or place barriers between the offending nails and the skin in question.
Topical medications, such as steroid creams, are of very limited usefulness, as are oral antibiotics and antihistamines.

At her daughters’ insistence, this 69-year-old woman requests referral to dermatology for a skin condition that has been present for at least 20 years. During that time, she has seen many medical providers (including dermatologists) and has tried many different treatments (eg, creams, oral antibiotics, oral steroids, and antihistamines). While some of these helped a bit, most did not help at all—nor did the constant nagging at the patient by family and caregivers. Nonetheless, her daughters feel strongly that their mother is perpetuating the problem with her “scratching and picking.” They have observed that when she is able to leave her arms alone, the improvement in her skin is dramatic. For example, years ago, she broke her wrist and was placed in a cast for six weeks; when it was removed, the affected arm was completely clear (except for multiple old scars). Everyone, including the patient, was ecstatic—but a week later, the lesions returned. The extensor aspects of both arms and hands are covered with linear excoriations, scars, and scabs, with focal hyperpigmentation in many of the excoriated areas. Overall, the skin in these areas is re-markably thickened and focally shiny. Her skin elsewhere—such as her palms and the volar aspects of her arms—is relatively clear. Throughout the examination, the patient’s hands never stop rubbing and scratching her arms, even as she weakly denies doing so. “Whatever happens, I’m not going to see a shrink,” she says. Clearly, a biopsy is in order, with a sample taken from a typical section of her forearm. The results show minimal changes but demonstrate hyperkeratosis. Blood work, including a complete metabolic profile and complete blood count, fail to show any evidence of systemic disease.