User login
Dump Truck Dermis
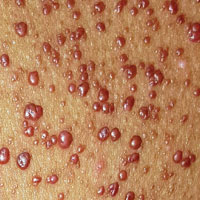
Accompanied by family, a 68-year-old man presents for evaluation of changes on the left side of his face. His relatives, who have not seen him in years, find the changes quite alarming; the patient, however, is quite sure he has “looked this way for a while.” In any case, he has no associated symptoms.
He does have numerous other health problems, including hypertension, heart disease, and a 50–pack-year history of smoking. He has spent a great deal of time in the sun over the years, particularly when he drove a dump truck for work.
EXAMINATION
The left side of the patient’s face is covered with open and closed comedones superimposed on thickened, yellowed skin. Poikilodermatous changes and multiple telangiectasias can also be seen. The right side of his face demonstrates minor skin changes relative to the left.

What is the diagnosis?
DISCUSSION
These changes represent Favre-Racouchot syndrome (FRS). First described by Favre in 1932, the syndrome was refined in 1951 when Favre and Racouchot noticed its prevalence in truck drivers who also smoked. In France at that time, more than 80% of truck drivers were smokers—and they got the most sun exposure on the left sides of their faces. The condition was later identified in fishermen and other outdoor workers.
Studies in the US show that FRS affects nearly 6% of white adults (usually men) older than 60. Radiation therapy (eg, for squamous cell carcinoma) can produce similar effects.
Needless to say, smoking cessation is advisable. Beyond that, treatment involves preventing further sun damage and applying retinoid preparations, such as tretinoin or adapalene. Depending on the desired level of improvement, comedones may need to be surgically ablated.
TAKE-HOME LEARNING POINTS
• Favre-Racouchot syndrome (FRS) manifests with collections of open and closed comedones on sun-damaged facial skin.
• Most FRS patients are white male smokers older than 60.
• FRS is usually unilateral, resulting from overexposure to sunlight through a vehicle’s driver-side window; however, people working outdoors (eg, fishermen) can develop it over the whole face.
Accompanied by family, a 68-year-old man presents for evaluation of changes on the left side of his face. His relatives, who have not seen him in years, find the changes quite alarming; the patient, however, is quite sure he has “looked this way for a while.” In any case, he has no associated symptoms.
He does have numerous other health problems, including hypertension, heart disease, and a 50–pack-year history of smoking. He has spent a great deal of time in the sun over the years, particularly when he drove a dump truck for work.
EXAMINATION
The left side of the patient’s face is covered with open and closed comedones superimposed on thickened, yellowed skin. Poikilodermatous changes and multiple telangiectasias can also be seen. The right side of his face demonstrates minor skin changes relative to the left.

What is the diagnosis?
DISCUSSION
These changes represent Favre-Racouchot syndrome (FRS). First described by Favre in 1932, the syndrome was refined in 1951 when Favre and Racouchot noticed its prevalence in truck drivers who also smoked. In France at that time, more than 80% of truck drivers were smokers—and they got the most sun exposure on the left sides of their faces. The condition was later identified in fishermen and other outdoor workers.
Studies in the US show that FRS affects nearly 6% of white adults (usually men) older than 60. Radiation therapy (eg, for squamous cell carcinoma) can produce similar effects.
Needless to say, smoking cessation is advisable. Beyond that, treatment involves preventing further sun damage and applying retinoid preparations, such as tretinoin or adapalene. Depending on the desired level of improvement, comedones may need to be surgically ablated.
TAKE-HOME LEARNING POINTS
• Favre-Racouchot syndrome (FRS) manifests with collections of open and closed comedones on sun-damaged facial skin.
• Most FRS patients are white male smokers older than 60.
• FRS is usually unilateral, resulting from overexposure to sunlight through a vehicle’s driver-side window; however, people working outdoors (eg, fishermen) can develop it over the whole face.
Accompanied by family, a 68-year-old man presents for evaluation of changes on the left side of his face. His relatives, who have not seen him in years, find the changes quite alarming; the patient, however, is quite sure he has “looked this way for a while.” In any case, he has no associated symptoms.
He does have numerous other health problems, including hypertension, heart disease, and a 50–pack-year history of smoking. He has spent a great deal of time in the sun over the years, particularly when he drove a dump truck for work.
EXAMINATION
The left side of the patient’s face is covered with open and closed comedones superimposed on thickened, yellowed skin. Poikilodermatous changes and multiple telangiectasias can also be seen. The right side of his face demonstrates minor skin changes relative to the left.

What is the diagnosis?
DISCUSSION
These changes represent Favre-Racouchot syndrome (FRS). First described by Favre in 1932, the syndrome was refined in 1951 when Favre and Racouchot noticed its prevalence in truck drivers who also smoked. In France at that time, more than 80% of truck drivers were smokers—and they got the most sun exposure on the left sides of their faces. The condition was later identified in fishermen and other outdoor workers.
Studies in the US show that FRS affects nearly 6% of white adults (usually men) older than 60. Radiation therapy (eg, for squamous cell carcinoma) can produce similar effects.
Needless to say, smoking cessation is advisable. Beyond that, treatment involves preventing further sun damage and applying retinoid preparations, such as tretinoin or adapalene. Depending on the desired level of improvement, comedones may need to be surgically ablated.
TAKE-HOME LEARNING POINTS
• Favre-Racouchot syndrome (FRS) manifests with collections of open and closed comedones on sun-damaged facial skin.
• Most FRS patients are white male smokers older than 60.
• FRS is usually unilateral, resulting from overexposure to sunlight through a vehicle’s driver-side window; however, people working outdoors (eg, fishermen) can develop it over the whole face.
15 and Going Gray
ANSWER
The correct answer is seborrheic dermatitis (choice “d”).
Psoriasis (choice “a”) can manifest in a similar fashion but would also appear elsewhere (eg, the elbows, knees, or nails). The scaling seen with psoriasis is usually white on a salmon-colored base and much coarser.
Vitiligo (choice “b”) presents with total, porcelain-white depigmentation and is not scaly at all; this patient’s loss of pigment was only partial.
Rashes like this are often thought to be fungal, but a fungal infection (choice “c”) is rarely seen on the face and would not demonstrate this exact pattern.
DISCUSSION
Seborrheic dermatitis (SD) is an extremely common papulosquamous skin condition that manifests primarily in oil-rich areas, such as the central face, scalp (dandruff), and in and behind the ears. On white skin, it yields a pinkish-brown scaly rash, but on darker skin, SD causes partial depigmentation—sometimes to an alarming extent. The distribution in this case is typical, with nasolabial, glabellar, ear, and brow involvement.
SD might be caused by a number of factors, some related to climate or genetics. One prevailing theory is that it involves an inflammatory reaction resulting from commensal yeast organisms (Malassezia furfur) feeding on sebum. In this case, the contribution of stress was clear.
TREATMENT/PROGNOSIS
Treatment comprised daily use of ketoconazole shampoo on the scalp and face and a topical ketoconazole cream. The condition cleared within two weeks. Although the chances of a recurrence are quite high, the patient is now armed with information and products to avoid the worst effects.
ANSWER
The correct answer is seborrheic dermatitis (choice “d”).
Psoriasis (choice “a”) can manifest in a similar fashion but would also appear elsewhere (eg, the elbows, knees, or nails). The scaling seen with psoriasis is usually white on a salmon-colored base and much coarser.
Vitiligo (choice “b”) presents with total, porcelain-white depigmentation and is not scaly at all; this patient’s loss of pigment was only partial.
Rashes like this are often thought to be fungal, but a fungal infection (choice “c”) is rarely seen on the face and would not demonstrate this exact pattern.
DISCUSSION
Seborrheic dermatitis (SD) is an extremely common papulosquamous skin condition that manifests primarily in oil-rich areas, such as the central face, scalp (dandruff), and in and behind the ears. On white skin, it yields a pinkish-brown scaly rash, but on darker skin, SD causes partial depigmentation—sometimes to an alarming extent. The distribution in this case is typical, with nasolabial, glabellar, ear, and brow involvement.
SD might be caused by a number of factors, some related to climate or genetics. One prevailing theory is that it involves an inflammatory reaction resulting from commensal yeast organisms (Malassezia furfur) feeding on sebum. In this case, the contribution of stress was clear.
TREATMENT/PROGNOSIS
Treatment comprised daily use of ketoconazole shampoo on the scalp and face and a topical ketoconazole cream. The condition cleared within two weeks. Although the chances of a recurrence are quite high, the patient is now armed with information and products to avoid the worst effects.
ANSWER
The correct answer is seborrheic dermatitis (choice “d”).
Psoriasis (choice “a”) can manifest in a similar fashion but would also appear elsewhere (eg, the elbows, knees, or nails). The scaling seen with psoriasis is usually white on a salmon-colored base and much coarser.
Vitiligo (choice “b”) presents with total, porcelain-white depigmentation and is not scaly at all; this patient’s loss of pigment was only partial.
Rashes like this are often thought to be fungal, but a fungal infection (choice “c”) is rarely seen on the face and would not demonstrate this exact pattern.
DISCUSSION
Seborrheic dermatitis (SD) is an extremely common papulosquamous skin condition that manifests primarily in oil-rich areas, such as the central face, scalp (dandruff), and in and behind the ears. On white skin, it yields a pinkish-brown scaly rash, but on darker skin, SD causes partial depigmentation—sometimes to an alarming extent. The distribution in this case is typical, with nasolabial, glabellar, ear, and brow involvement.
SD might be caused by a number of factors, some related to climate or genetics. One prevailing theory is that it involves an inflammatory reaction resulting from commensal yeast organisms (Malassezia furfur) feeding on sebum. In this case, the contribution of stress was clear.
TREATMENT/PROGNOSIS
Treatment comprised daily use of ketoconazole shampoo on the scalp and face and a topical ketoconazole cream. The condition cleared within two weeks. Although the chances of a recurrence are quite high, the patient is now armed with information and products to avoid the worst effects.

A 15-year-old African-American boy is brought in by his family for evaluation of a condition that began several months ago. Despite multiple attempts at treatment, the uniform but partial depigmentation of the skin around his nose persists. It is made obvious by his type V skin, extending up into the glabellar area and into both eyebrows.
Fine but definite scaling is confined to the depigmented areas. There is heavier white to gray scaling on his frontal scalp, and light scaling in and behind both ears. His elbows, knees, and nails appear normal. He is asymptomatic and in excellent health otherwise, but he considers his condition “unsightly and embarrassing.”
More history-taking reveals that around the time this problem manifested, he was facing the threat of a one-year suspension from school for disciplinary reasons.
Wart's That Lesion?
A 10-year-old girl is referred to dermatology for evaluation of an asymptomatic “wart” that manifested on her thigh several years ago. At first, the lesion grew rapidly, but it has since stabilized. It remains unaffected despite multiple treatments with liquid nitrogen.
According to her parents (with confirmation from her medical record), the patient is otherwise quite healthy.
EXAMINATION
A spindle-shaped, pinkish red, 1.2 x 0.7-cm nodule with a smooth surface and rounded borders is located on the patient’s distal left anterior thigh. The lesion itself is quite firm but nontender to the touch, and its long axis is parallel to transverse local skin tension lines. The patient’s type II skin is otherwise unremarkable.

After consultation with the patient and her family, the lesion is excised under local anesthesia with 5-mm margins in an elliptical pattern to yield favorable lines of closure. The sample is sent to pathology.
What is the diagnosis?
DISCUSSION
The pathology report showed both epithelioid and spindle cells with scattered apoptotic cells seen at the dermoepidermal junction, with no atypia. The margins were clear. Such findings are consistent with a diagnosis of Spitz nevus.
Prior to the 1950s, lesions with these clinical and histologic features were believed to be melanoma and therefore termed juvenile melanoma. But their unique morphologic and histologic architecture—and a lack of signs of progressive or metastatic disease in affected patients—prompted suspicion that they were not really malignant. A pathologist named Sophie Spitz conducted a retrospective study that revealed no cancerous activity in any of the patients. Her findings, on a superficial level, eventually led to the elimination of the term “juvenile melanoma”—but more importantly, they eradicated a great deal of unnecessary, and often mutilating, surgery.
The features of the case patient’s lesion—color, texture, shape, and initial rapid growth —are typical of Spitz nevi, as are the location and the age of the patient. However, the range of morphologic presentations includes darker lesions (some almost black) and those of varying vertical depth and appearance (ie, intradermal, compound, junctional).
A note of caution, however: Although Spitz nevi are benign, true melanomas can present with “Spitzoid” morphologic and histologic features (they’re even called “Spitzoid melanomas”). Key distinguishing features can only be identified via microscopic examination of the lesion’s full vertical structure. So, for safety’s sake, the standard of care for Spitz nevi is to excise them totally, with clear, deep, wide margins, whenever possible.
The case patient had her sutures removed 10 days after surgery. Her ongoing care will include a biannual check for signs of recurrence.
TAKE-HOME LEARNING POINTS
• Until the mid-1950s, what we now refer to as Spitz nevi were called “juvenile melanoma” and were treated as such, with radical and often disfiguring surgeries.
• Spitz nevi are usually seen in children. They can be red, pink, or even black, and often have a history of recent growth and an elliptiform shape.
• Excision with totally clear margins is the correct approach, along with pathologic examination.
• Spitz nevi have histologic features suggestive of melanoma, and some melanomas have “Spitzoid” features. Therefore, all cases must be handled with great care.
A 10-year-old girl is referred to dermatology for evaluation of an asymptomatic “wart” that manifested on her thigh several years ago. At first, the lesion grew rapidly, but it has since stabilized. It remains unaffected despite multiple treatments with liquid nitrogen.
According to her parents (with confirmation from her medical record), the patient is otherwise quite healthy.
EXAMINATION
A spindle-shaped, pinkish red, 1.2 x 0.7-cm nodule with a smooth surface and rounded borders is located on the patient’s distal left anterior thigh. The lesion itself is quite firm but nontender to the touch, and its long axis is parallel to transverse local skin tension lines. The patient’s type II skin is otherwise unremarkable.

After consultation with the patient and her family, the lesion is excised under local anesthesia with 5-mm margins in an elliptical pattern to yield favorable lines of closure. The sample is sent to pathology.
What is the diagnosis?
DISCUSSION
The pathology report showed both epithelioid and spindle cells with scattered apoptotic cells seen at the dermoepidermal junction, with no atypia. The margins were clear. Such findings are consistent with a diagnosis of Spitz nevus.
Prior to the 1950s, lesions with these clinical and histologic features were believed to be melanoma and therefore termed juvenile melanoma. But their unique morphologic and histologic architecture—and a lack of signs of progressive or metastatic disease in affected patients—prompted suspicion that they were not really malignant. A pathologist named Sophie Spitz conducted a retrospective study that revealed no cancerous activity in any of the patients. Her findings, on a superficial level, eventually led to the elimination of the term “juvenile melanoma”—but more importantly, they eradicated a great deal of unnecessary, and often mutilating, surgery.
The features of the case patient’s lesion—color, texture, shape, and initial rapid growth —are typical of Spitz nevi, as are the location and the age of the patient. However, the range of morphologic presentations includes darker lesions (some almost black) and those of varying vertical depth and appearance (ie, intradermal, compound, junctional).
A note of caution, however: Although Spitz nevi are benign, true melanomas can present with “Spitzoid” morphologic and histologic features (they’re even called “Spitzoid melanomas”). Key distinguishing features can only be identified via microscopic examination of the lesion’s full vertical structure. So, for safety’s sake, the standard of care for Spitz nevi is to excise them totally, with clear, deep, wide margins, whenever possible.
The case patient had her sutures removed 10 days after surgery. Her ongoing care will include a biannual check for signs of recurrence.
TAKE-HOME LEARNING POINTS
• Until the mid-1950s, what we now refer to as Spitz nevi were called “juvenile melanoma” and were treated as such, with radical and often disfiguring surgeries.
• Spitz nevi are usually seen in children. They can be red, pink, or even black, and often have a history of recent growth and an elliptiform shape.
• Excision with totally clear margins is the correct approach, along with pathologic examination.
• Spitz nevi have histologic features suggestive of melanoma, and some melanomas have “Spitzoid” features. Therefore, all cases must be handled with great care.
A 10-year-old girl is referred to dermatology for evaluation of an asymptomatic “wart” that manifested on her thigh several years ago. At first, the lesion grew rapidly, but it has since stabilized. It remains unaffected despite multiple treatments with liquid nitrogen.
According to her parents (with confirmation from her medical record), the patient is otherwise quite healthy.
EXAMINATION
A spindle-shaped, pinkish red, 1.2 x 0.7-cm nodule with a smooth surface and rounded borders is located on the patient’s distal left anterior thigh. The lesion itself is quite firm but nontender to the touch, and its long axis is parallel to transverse local skin tension lines. The patient’s type II skin is otherwise unremarkable.

After consultation with the patient and her family, the lesion is excised under local anesthesia with 5-mm margins in an elliptical pattern to yield favorable lines of closure. The sample is sent to pathology.
What is the diagnosis?
DISCUSSION
The pathology report showed both epithelioid and spindle cells with scattered apoptotic cells seen at the dermoepidermal junction, with no atypia. The margins were clear. Such findings are consistent with a diagnosis of Spitz nevus.
Prior to the 1950s, lesions with these clinical and histologic features were believed to be melanoma and therefore termed juvenile melanoma. But their unique morphologic and histologic architecture—and a lack of signs of progressive or metastatic disease in affected patients—prompted suspicion that they were not really malignant. A pathologist named Sophie Spitz conducted a retrospective study that revealed no cancerous activity in any of the patients. Her findings, on a superficial level, eventually led to the elimination of the term “juvenile melanoma”—but more importantly, they eradicated a great deal of unnecessary, and often mutilating, surgery.
The features of the case patient’s lesion—color, texture, shape, and initial rapid growth —are typical of Spitz nevi, as are the location and the age of the patient. However, the range of morphologic presentations includes darker lesions (some almost black) and those of varying vertical depth and appearance (ie, intradermal, compound, junctional).
A note of caution, however: Although Spitz nevi are benign, true melanomas can present with “Spitzoid” morphologic and histologic features (they’re even called “Spitzoid melanomas”). Key distinguishing features can only be identified via microscopic examination of the lesion’s full vertical structure. So, for safety’s sake, the standard of care for Spitz nevi is to excise them totally, with clear, deep, wide margins, whenever possible.
The case patient had her sutures removed 10 days after surgery. Her ongoing care will include a biannual check for signs of recurrence.
TAKE-HOME LEARNING POINTS
• Until the mid-1950s, what we now refer to as Spitz nevi were called “juvenile melanoma” and were treated as such, with radical and often disfiguring surgeries.
• Spitz nevi are usually seen in children. They can be red, pink, or even black, and often have a history of recent growth and an elliptiform shape.
• Excision with totally clear margins is the correct approach, along with pathologic examination.
• Spitz nevi have histologic features suggestive of melanoma, and some melanomas have “Spitzoid” features. Therefore, all cases must be handled with great care.
His & Hers Hair Loss
A 29-year-old woman and her 40-year-old husband present together for evaluation of similar problems: One month ago, they both experienced sudden hair loss—the wife in two spots on her scalp, the husband in his beard. In both cases, the hair came out suddenly, without any symptoms. Neither has had this problem before. Both patients are otherwise healthy, but they admit to being under a great deal of stress in the weeks prior to onset of the condition.
Before consulting dermatology, they were seen in an urgent care clinic, where they were diagnosed with “ringworm.” Twice-daily application of nystatin cream was prescribed—to no good effect.
EXAMINATION
On each side of the woman’s parietal scalp is a round, completely hairless patch with exceptionally well-defined margins. The sites are otherwise unremarkable, free of redness, edema, or scaling. Each lesion measures about 3.5 cm in diameter. No lymph nodes are palpable in the adjacent neck.
On the man’s left jawline is a solitary, round, 4-cm, hairless patch. It is also free of edema, erythema, or epidermal disturbance of any kind. There are no palpable lymph nodes in the drainage area.

What is the diagnosis?
DISCUSSION
Sudden, asymptomatic, complete, well-marginated hair loss in any hair-bearing area is likely to be alopecia areata (AA). AA is an autoimmune process in which hair follicles are immobilized and unable to grow new hair until the process stops, which usually happens within weeks to months.
Because stress and AA have a suspected correlation, the patients’ histories of recent stress corroborate the diagnosis. Other features that bolster this impression are the lack of epidermal disturbance (eg, scaling, redness, edema) or palpable nodes in the area. The unusual factor in this case was the simultaneous appearance of the condition in husband and wife—for which I have no good explanation.
There are many items in the differential for localized hair loss, including discoid lupus, lichen planopilaris, and tinea capitis. However, these almost always manifest with frank inflammation characterized by epidermal disturbance.
Treatments such as intralesional steroid injection can promote modest hair growth but are generally ineffective for long-term recovery; unless the procedure is repeated, the hair will continue to fall out. These patients were offered treatment but declined, and they recovered in a short period of time.
TAKE-HOME LEARNING POINTS
• Alopecia areata (AA) typically displays as acute, asymptomatic, complete hair loss in one or more hair-bearing locations, usually in a round, well-defined configuration.
• AA is an autoimmune process that immobilizes hair follicles, causing them to fall out and not be replaced until the process ceases. This can take months, and the condition does not respond well to treatment.
• AA can affect the scalp, beard, brows, or even genital hair.
• The differential for localized hair loss includes tinea capitis, discoid lupus, lichen planopilaris, and lues; however, these all involve disruption of the overlying skin with scaling, redness, or edema.
A 29-year-old woman and her 40-year-old husband present together for evaluation of similar problems: One month ago, they both experienced sudden hair loss—the wife in two spots on her scalp, the husband in his beard. In both cases, the hair came out suddenly, without any symptoms. Neither has had this problem before. Both patients are otherwise healthy, but they admit to being under a great deal of stress in the weeks prior to onset of the condition.
Before consulting dermatology, they were seen in an urgent care clinic, where they were diagnosed with “ringworm.” Twice-daily application of nystatin cream was prescribed—to no good effect.
EXAMINATION
On each side of the woman’s parietal scalp is a round, completely hairless patch with exceptionally well-defined margins. The sites are otherwise unremarkable, free of redness, edema, or scaling. Each lesion measures about 3.5 cm in diameter. No lymph nodes are palpable in the adjacent neck.
On the man’s left jawline is a solitary, round, 4-cm, hairless patch. It is also free of edema, erythema, or epidermal disturbance of any kind. There are no palpable lymph nodes in the drainage area.

What is the diagnosis?
DISCUSSION
Sudden, asymptomatic, complete, well-marginated hair loss in any hair-bearing area is likely to be alopecia areata (AA). AA is an autoimmune process in which hair follicles are immobilized and unable to grow new hair until the process stops, which usually happens within weeks to months.
Because stress and AA have a suspected correlation, the patients’ histories of recent stress corroborate the diagnosis. Other features that bolster this impression are the lack of epidermal disturbance (eg, scaling, redness, edema) or palpable nodes in the area. The unusual factor in this case was the simultaneous appearance of the condition in husband and wife—for which I have no good explanation.
There are many items in the differential for localized hair loss, including discoid lupus, lichen planopilaris, and tinea capitis. However, these almost always manifest with frank inflammation characterized by epidermal disturbance.
Treatments such as intralesional steroid injection can promote modest hair growth but are generally ineffective for long-term recovery; unless the procedure is repeated, the hair will continue to fall out. These patients were offered treatment but declined, and they recovered in a short period of time.
TAKE-HOME LEARNING POINTS
• Alopecia areata (AA) typically displays as acute, asymptomatic, complete hair loss in one or more hair-bearing locations, usually in a round, well-defined configuration.
• AA is an autoimmune process that immobilizes hair follicles, causing them to fall out and not be replaced until the process ceases. This can take months, and the condition does not respond well to treatment.
• AA can affect the scalp, beard, brows, or even genital hair.
• The differential for localized hair loss includes tinea capitis, discoid lupus, lichen planopilaris, and lues; however, these all involve disruption of the overlying skin with scaling, redness, or edema.
A 29-year-old woman and her 40-year-old husband present together for evaluation of similar problems: One month ago, they both experienced sudden hair loss—the wife in two spots on her scalp, the husband in his beard. In both cases, the hair came out suddenly, without any symptoms. Neither has had this problem before. Both patients are otherwise healthy, but they admit to being under a great deal of stress in the weeks prior to onset of the condition.
Before consulting dermatology, they were seen in an urgent care clinic, where they were diagnosed with “ringworm.” Twice-daily application of nystatin cream was prescribed—to no good effect.
EXAMINATION
On each side of the woman’s parietal scalp is a round, completely hairless patch with exceptionally well-defined margins. The sites are otherwise unremarkable, free of redness, edema, or scaling. Each lesion measures about 3.5 cm in diameter. No lymph nodes are palpable in the adjacent neck.
On the man’s left jawline is a solitary, round, 4-cm, hairless patch. It is also free of edema, erythema, or epidermal disturbance of any kind. There are no palpable lymph nodes in the drainage area.

What is the diagnosis?
DISCUSSION
Sudden, asymptomatic, complete, well-marginated hair loss in any hair-bearing area is likely to be alopecia areata (AA). AA is an autoimmune process in which hair follicles are immobilized and unable to grow new hair until the process stops, which usually happens within weeks to months.
Because stress and AA have a suspected correlation, the patients’ histories of recent stress corroborate the diagnosis. Other features that bolster this impression are the lack of epidermal disturbance (eg, scaling, redness, edema) or palpable nodes in the area. The unusual factor in this case was the simultaneous appearance of the condition in husband and wife—for which I have no good explanation.
There are many items in the differential for localized hair loss, including discoid lupus, lichen planopilaris, and tinea capitis. However, these almost always manifest with frank inflammation characterized by epidermal disturbance.
Treatments such as intralesional steroid injection can promote modest hair growth but are generally ineffective for long-term recovery; unless the procedure is repeated, the hair will continue to fall out. These patients were offered treatment but declined, and they recovered in a short period of time.
TAKE-HOME LEARNING POINTS
• Alopecia areata (AA) typically displays as acute, asymptomatic, complete hair loss in one or more hair-bearing locations, usually in a round, well-defined configuration.
• AA is an autoimmune process that immobilizes hair follicles, causing them to fall out and not be replaced until the process ceases. This can take months, and the condition does not respond well to treatment.
• AA can affect the scalp, beard, brows, or even genital hair.
• The differential for localized hair loss includes tinea capitis, discoid lupus, lichen planopilaris, and lues; however, these all involve disruption of the overlying skin with scaling, redness, or edema.
As Girl Grows, Lesions Follow Suit
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.

Since shortly after birth, a now 12-year-old African-American girl has had lesions on her trunk. She has never been given a diagnosis and has always been told she would “outgrow the problem.” Instead, the number and distribution of lesions continues to increase, and her pediatrician finally refers her to dermatology for evaluation.
About 150 to 200 nearly identical lesions scatter around the patient’s body, clustered mostly on the left upper back but also on the abdomen and bilateral upper thighs. The fleshy, reddish brown, mushroom-like papules range in size from 2 to 4 mm and exhibit no central umbilication. Two brown spots (each measuring 2 mm) are seen in the iris of the patient’s left eye.
There are no other apparent medical problems to report and no visual deficits. Aside from being unsightly, the lesions are asymptomatic. A shave biopsy of one of them is performed.
A Severe Sitchuation
This 49-year-old man was first diagnosed with Darier disease at age 8. It has been contained, for the most part, by topical medications and acitretin. But the itching on his legs is especially severe, making it difficult for him to leave them alone.
EXAMINATION
Both legs have heavy scaling and lichenification from the lateral aspects of the knees down to the ankles. There is modest erythema but no suppurative signs. Other areas of scaling are seen on his chest and back, but these are less coarse and rough than the leg rash.
What is the diagnosis?
DISCUSSION
Lichen simplex chronicus (LSC) is the term given to this phenomenon. LSC is always secondary to a primary trigger, which can be dry skin, eczema, psoriasis, or even a bug bite. Excessive scratching induces more itching, and before the patient realizes it, he has jumped aboard the itch-scratch-itch train—a vicious cycle that can be hard to break.
The skin reacts to all this attention by thickening and becoming rough; on a microscopic level, the nerves become more sensitive. The urge to scratch becomes so irresistible that some patients fantasize about giving in.
The first goal of treating LSC is to stop the itching by helping the patient avoid contact with the site. High-potency topical steroids can be effective for this, especially if used under occlusion, which not only potentiates the steroid but also provides a barrier to protect the area from the patient’s fingernails (or hairbrush). Once the condition improves, steroids can be slowly withdrawn.
A biopsy, if it had been necessary, would have shown hypertrophic epidermis and acanthotic changes.
TAKE-HOME LEARNING POINTS
• Lichen simplex chronicus (LSC) is secondary to an inciting condition such as eczema, xerosis, psoriasis, or Darier disease.
• The manifestation of the itch-scratch-itch cycle leads to thickening and lichenification of the skin. The itch of LSC is so compelling that scratching is hard to resist.
• Despite treatment and patient education, recurrences are quite common.
This 49-year-old man was first diagnosed with Darier disease at age 8. It has been contained, for the most part, by topical medications and acitretin. But the itching on his legs is especially severe, making it difficult for him to leave them alone.
EXAMINATION
Both legs have heavy scaling and lichenification from the lateral aspects of the knees down to the ankles. There is modest erythema but no suppurative signs. Other areas of scaling are seen on his chest and back, but these are less coarse and rough than the leg rash.
What is the diagnosis?
DISCUSSION
Lichen simplex chronicus (LSC) is the term given to this phenomenon. LSC is always secondary to a primary trigger, which can be dry skin, eczema, psoriasis, or even a bug bite. Excessive scratching induces more itching, and before the patient realizes it, he has jumped aboard the itch-scratch-itch train—a vicious cycle that can be hard to break.
The skin reacts to all this attention by thickening and becoming rough; on a microscopic level, the nerves become more sensitive. The urge to scratch becomes so irresistible that some patients fantasize about giving in.
The first goal of treating LSC is to stop the itching by helping the patient avoid contact with the site. High-potency topical steroids can be effective for this, especially if used under occlusion, which not only potentiates the steroid but also provides a barrier to protect the area from the patient’s fingernails (or hairbrush). Once the condition improves, steroids can be slowly withdrawn.
A biopsy, if it had been necessary, would have shown hypertrophic epidermis and acanthotic changes.
TAKE-HOME LEARNING POINTS
• Lichen simplex chronicus (LSC) is secondary to an inciting condition such as eczema, xerosis, psoriasis, or Darier disease.
• The manifestation of the itch-scratch-itch cycle leads to thickening and lichenification of the skin. The itch of LSC is so compelling that scratching is hard to resist.
• Despite treatment and patient education, recurrences are quite common.
This 49-year-old man was first diagnosed with Darier disease at age 8. It has been contained, for the most part, by topical medications and acitretin. But the itching on his legs is especially severe, making it difficult for him to leave them alone.
EXAMINATION
Both legs have heavy scaling and lichenification from the lateral aspects of the knees down to the ankles. There is modest erythema but no suppurative signs. Other areas of scaling are seen on his chest and back, but these are less coarse and rough than the leg rash.
What is the diagnosis?
DISCUSSION
Lichen simplex chronicus (LSC) is the term given to this phenomenon. LSC is always secondary to a primary trigger, which can be dry skin, eczema, psoriasis, or even a bug bite. Excessive scratching induces more itching, and before the patient realizes it, he has jumped aboard the itch-scratch-itch train—a vicious cycle that can be hard to break.
The skin reacts to all this attention by thickening and becoming rough; on a microscopic level, the nerves become more sensitive. The urge to scratch becomes so irresistible that some patients fantasize about giving in.
The first goal of treating LSC is to stop the itching by helping the patient avoid contact with the site. High-potency topical steroids can be effective for this, especially if used under occlusion, which not only potentiates the steroid but also provides a barrier to protect the area from the patient’s fingernails (or hairbrush). Once the condition improves, steroids can be slowly withdrawn.
A biopsy, if it had been necessary, would have shown hypertrophic epidermis and acanthotic changes.
TAKE-HOME LEARNING POINTS
• Lichen simplex chronicus (LSC) is secondary to an inciting condition such as eczema, xerosis, psoriasis, or Darier disease.
• The manifestation of the itch-scratch-itch cycle leads to thickening and lichenification of the skin. The itch of LSC is so compelling that scratching is hard to resist.
• Despite treatment and patient education, recurrences are quite common.
Picking at a Problem
An 80-year-old woman bitterly complains of itching and discomfort on the left side of her face that began several weeks ago. Her primary care provider initially diagnosed contact dermatitis and prescribed a class 6 topical steroid cream. This helped a bit with the itching but had no effect on appearance.
When a friend suggested the itch might be the result of a bug bite, the patient went directly to the emergency department and was given a two-week taper of prednisone (40 mg/d for a week, then 20 mg/d for a week). This eased the redness, but the itching returned as soon as the course was finished. Finally, she was referred to dermatology.
The patient, who has been a widow for many years, was recently “forced out” of her home of more than 50 years and into an assisted living facility; her family seldom visits, so her friend accompanies her to your office today.
EXAMINATION
Extensive honey-colored crusting on an erythematous base is confined to the left side of the patient’s face. No nodes are palpable in the area. Her friend confirms that she has been picking at the skin.

What is the diagnosis?
DISCUSSION
This condition is impetigo—in this case “non-bullous” impetigo, a rash that almost always begins with a breach in normal skin integrity. This opens the skin to superficial invasion by staph and strep organisms, mostly emitting from the nasal passages. In this case, the patient had been picking at seborrheic keratosis (an extremely common phenomenon in someone her age) on her face.
The inclination to scratch and pick—and the inability to manage nasal secretions—make children the most likely candidates for impetigo. It is especially common in those with atopic dermatitis, who not only have poor barrier function (which manifests as eczema) but also constant nasal drainage from seasonal allergies.
The differential includes herpes simplex or zoster, eczema and contact dermatitis. But the location of the rash, the honey-colored crust on an erythematous base, and the history of skin breaches all point directly to impetigo. Lymph nodes are often palpable in the drainage area; their presence corroborates the diagnosis.
Luckily, this type of impetigo is relatively easy to treat: The patient was advised to wash the area with soap and water and apply mupirocin ointment three times a day. She was also prescribed cephalexin (500 mg tid for a week), which cleared the condition aside from a faint bit of postinflammatory pinkness.
TAKE-HOME LEARNING POINTS
• Impetigo is a superficial bacterial infection, usually on or near the face, caused by staph and strep organisms that seed the area from the nasal passages.
• These organisms generally require a break in the skin to gain entrance, often caused by picking or scratching.
• Honey-colored crust on an erythematous base, plus or minus enlarged local nodes, help to confirm the diagnosis.
• Symptoms of impetigo include itching and mild discomfort but not pain.
• Treatment can be as simple as cleaning with soap and water and applying topical mupirocin ointment. A short course of oral antibiotics may be needed to speed the clearance process.
An 80-year-old woman bitterly complains of itching and discomfort on the left side of her face that began several weeks ago. Her primary care provider initially diagnosed contact dermatitis and prescribed a class 6 topical steroid cream. This helped a bit with the itching but had no effect on appearance.
When a friend suggested the itch might be the result of a bug bite, the patient went directly to the emergency department and was given a two-week taper of prednisone (40 mg/d for a week, then 20 mg/d for a week). This eased the redness, but the itching returned as soon as the course was finished. Finally, she was referred to dermatology.
The patient, who has been a widow for many years, was recently “forced out” of her home of more than 50 years and into an assisted living facility; her family seldom visits, so her friend accompanies her to your office today.
EXAMINATION
Extensive honey-colored crusting on an erythematous base is confined to the left side of the patient’s face. No nodes are palpable in the area. Her friend confirms that she has been picking at the skin.

What is the diagnosis?
DISCUSSION
This condition is impetigo—in this case “non-bullous” impetigo, a rash that almost always begins with a breach in normal skin integrity. This opens the skin to superficial invasion by staph and strep organisms, mostly emitting from the nasal passages. In this case, the patient had been picking at seborrheic keratosis (an extremely common phenomenon in someone her age) on her face.
The inclination to scratch and pick—and the inability to manage nasal secretions—make children the most likely candidates for impetigo. It is especially common in those with atopic dermatitis, who not only have poor barrier function (which manifests as eczema) but also constant nasal drainage from seasonal allergies.
The differential includes herpes simplex or zoster, eczema and contact dermatitis. But the location of the rash, the honey-colored crust on an erythematous base, and the history of skin breaches all point directly to impetigo. Lymph nodes are often palpable in the drainage area; their presence corroborates the diagnosis.
Luckily, this type of impetigo is relatively easy to treat: The patient was advised to wash the area with soap and water and apply mupirocin ointment three times a day. She was also prescribed cephalexin (500 mg tid for a week), which cleared the condition aside from a faint bit of postinflammatory pinkness.
TAKE-HOME LEARNING POINTS
• Impetigo is a superficial bacterial infection, usually on or near the face, caused by staph and strep organisms that seed the area from the nasal passages.
• These organisms generally require a break in the skin to gain entrance, often caused by picking or scratching.
• Honey-colored crust on an erythematous base, plus or minus enlarged local nodes, help to confirm the diagnosis.
• Symptoms of impetigo include itching and mild discomfort but not pain.
• Treatment can be as simple as cleaning with soap and water and applying topical mupirocin ointment. A short course of oral antibiotics may be needed to speed the clearance process.
An 80-year-old woman bitterly complains of itching and discomfort on the left side of her face that began several weeks ago. Her primary care provider initially diagnosed contact dermatitis and prescribed a class 6 topical steroid cream. This helped a bit with the itching but had no effect on appearance.
When a friend suggested the itch might be the result of a bug bite, the patient went directly to the emergency department and was given a two-week taper of prednisone (40 mg/d for a week, then 20 mg/d for a week). This eased the redness, but the itching returned as soon as the course was finished. Finally, she was referred to dermatology.
The patient, who has been a widow for many years, was recently “forced out” of her home of more than 50 years and into an assisted living facility; her family seldom visits, so her friend accompanies her to your office today.
EXAMINATION
Extensive honey-colored crusting on an erythematous base is confined to the left side of the patient’s face. No nodes are palpable in the area. Her friend confirms that she has been picking at the skin.

What is the diagnosis?
DISCUSSION
This condition is impetigo—in this case “non-bullous” impetigo, a rash that almost always begins with a breach in normal skin integrity. This opens the skin to superficial invasion by staph and strep organisms, mostly emitting from the nasal passages. In this case, the patient had been picking at seborrheic keratosis (an extremely common phenomenon in someone her age) on her face.
The inclination to scratch and pick—and the inability to manage nasal secretions—make children the most likely candidates for impetigo. It is especially common in those with atopic dermatitis, who not only have poor barrier function (which manifests as eczema) but also constant nasal drainage from seasonal allergies.
The differential includes herpes simplex or zoster, eczema and contact dermatitis. But the location of the rash, the honey-colored crust on an erythematous base, and the history of skin breaches all point directly to impetigo. Lymph nodes are often palpable in the drainage area; their presence corroborates the diagnosis.
Luckily, this type of impetigo is relatively easy to treat: The patient was advised to wash the area with soap and water and apply mupirocin ointment three times a day. She was also prescribed cephalexin (500 mg tid for a week), which cleared the condition aside from a faint bit of postinflammatory pinkness.
TAKE-HOME LEARNING POINTS
• Impetigo is a superficial bacterial infection, usually on or near the face, caused by staph and strep organisms that seed the area from the nasal passages.
• These organisms generally require a break in the skin to gain entrance, often caused by picking or scratching.
• Honey-colored crust on an erythematous base, plus or minus enlarged local nodes, help to confirm the diagnosis.
• Symptoms of impetigo include itching and mild discomfort but not pain.
• Treatment can be as simple as cleaning with soap and water and applying topical mupirocin ointment. A short course of oral antibiotics may be needed to speed the clearance process.
A Creepy Crawly Anomaly
ANSWER
The correct answer is dermatofibroma (choice “c”), based on the classic histologic picture and the lack of supportive findings for other items in the differential. These include seborrheic keratosis, granular cell tumor, basal cell carcinoma, and sweat duct cancer.
DISCUSSION
This is a perfect example of one of the most common benign tumors, seen daily in dermatology offices worldwide. Alternately referred to as superficial benign fibrous histiocytomas, dermatofibromas (DFs) typically manifest on lower extremities, are about twice as common in women as in men, and usually affect patients in their early 40s.
DFs appear most commonly as low, firm, round to ovoid, pinkish brown papules that dimple with lateral digital pressure. Though not pathognomic, the “dimple sign” is highly suggestive of this diagnosis. DF lesions can also manifest as firm, convex papules or nodules (as in this case) with the same coloring but without the dimple sign.
For years, DFs were believed to be a reaction to trauma (eg, bug bite). While this theory still has its adherents, more recent studies suggest these are true tumors composed of skin fibroblasts. Their ability to occur internally, even in bone, provides further evidence against their putatively reactive nature.
Histologically, the typical DF shows whorling fascicles of a fibroblastic spindle cell proliferation in the dermis. By contrast, the most dangerous item in the differential, the rare but greatly feared malignant dermatofibrosarcoma protuberans, is characterized by a storiform (cartwheel-shaped) pattern of spindle cells.
DFs are often subject to trauma from shaving and therefore surgically removed. However, since this was not the case for this patient, she chose to leave her lesion in place.
ANSWER
The correct answer is dermatofibroma (choice “c”), based on the classic histologic picture and the lack of supportive findings for other items in the differential. These include seborrheic keratosis, granular cell tumor, basal cell carcinoma, and sweat duct cancer.
DISCUSSION
This is a perfect example of one of the most common benign tumors, seen daily in dermatology offices worldwide. Alternately referred to as superficial benign fibrous histiocytomas, dermatofibromas (DFs) typically manifest on lower extremities, are about twice as common in women as in men, and usually affect patients in their early 40s.
DFs appear most commonly as low, firm, round to ovoid, pinkish brown papules that dimple with lateral digital pressure. Though not pathognomic, the “dimple sign” is highly suggestive of this diagnosis. DF lesions can also manifest as firm, convex papules or nodules (as in this case) with the same coloring but without the dimple sign.
For years, DFs were believed to be a reaction to trauma (eg, bug bite). While this theory still has its adherents, more recent studies suggest these are true tumors composed of skin fibroblasts. Their ability to occur internally, even in bone, provides further evidence against their putatively reactive nature.
Histologically, the typical DF shows whorling fascicles of a fibroblastic spindle cell proliferation in the dermis. By contrast, the most dangerous item in the differential, the rare but greatly feared malignant dermatofibrosarcoma protuberans, is characterized by a storiform (cartwheel-shaped) pattern of spindle cells.
DFs are often subject to trauma from shaving and therefore surgically removed. However, since this was not the case for this patient, she chose to leave her lesion in place.
ANSWER
The correct answer is dermatofibroma (choice “c”), based on the classic histologic picture and the lack of supportive findings for other items in the differential. These include seborrheic keratosis, granular cell tumor, basal cell carcinoma, and sweat duct cancer.
DISCUSSION
This is a perfect example of one of the most common benign tumors, seen daily in dermatology offices worldwide. Alternately referred to as superficial benign fibrous histiocytomas, dermatofibromas (DFs) typically manifest on lower extremities, are about twice as common in women as in men, and usually affect patients in their early 40s.
DFs appear most commonly as low, firm, round to ovoid, pinkish brown papules that dimple with lateral digital pressure. Though not pathognomic, the “dimple sign” is highly suggestive of this diagnosis. DF lesions can also manifest as firm, convex papules or nodules (as in this case) with the same coloring but without the dimple sign.
For years, DFs were believed to be a reaction to trauma (eg, bug bite). While this theory still has its adherents, more recent studies suggest these are true tumors composed of skin fibroblasts. Their ability to occur internally, even in bone, provides further evidence against their putatively reactive nature.
Histologically, the typical DF shows whorling fascicles of a fibroblastic spindle cell proliferation in the dermis. By contrast, the most dangerous item in the differential, the rare but greatly feared malignant dermatofibrosarcoma protuberans, is characterized by a storiform (cartwheel-shaped) pattern of spindle cells.
DFs are often subject to trauma from shaving and therefore surgically removed. However, since this was not the case for this patient, she chose to leave her lesion in place.

A 48-year-old woman is referred to dermatology for examination of a lesion on her ankle. Although the patient is certain that it has remained unchanged for years, she takes her primary care provider’s recommendation and agrees to be seen. She says the lesion occasionally itches and has a “crawly” feeling to it, but its size remains consistent.
Located on the lateral aspect of her left ankle is a brownish red, firm, round, intradermal nodule. It measures 8.5 mm and has a faint brown macular halo around it. Biopsy shows multiple round fascicles of spindle cells proliferating in the dermis. Special stains rule out the possibility of dermatofibrosarcoma protuberans, the most serious item in the differential.
The patient’s medical history includes breast cancer and a significant family history of skin cancer.
"I Got Blisters On My Fingers!"
The stubborn focal eruption on this 6-year-old boy’s left fourth finger remains unaffected after a one-week course of oral cephalexin, so his pediatrician refers him to dermatology. The problem initially manifested as a cluster of tiny blisters, which tingled a bit but didn’t hurt. When redness developed around it, the patient’s mother brought him for evaluation.
The boy experienced the same problem in the same location almost exactly a year ago. It was treated the same way and within a week or two had resolved.
The child is otherwise reasonably healthy, despite being allergy-prone. He has a history of seasonal allergies and is susceptible to skin infections, such as staph.
EXAMINATION
On the dorsal aspect of his finger are grouped vesicles on an erythematous base, measuring about 1 cm altogether. Several of these demonstrate central umbilication, and several are filled with pus. The erythema is minimal, and there is no tenderness on palpation. Palpation of the epitrochlear area reveals a tiny, nontender node.

What is the diagnosis?
DISCUSSION
Herpetic whitlow (HW), while uncommon, is far from rare. Essentially a cold sore occurring away from the usual labial/facial location, HW presents with premonitory symptoms of itch, tingle, and slight pain, followed by the appearance of grouped vesicles on an erythematous base. The vesicles are often umbillicated, as with most herpetic conditions. And, like most herpes simplex–related outbreaks, HW tends to recur in the same location—an extremely useful piece of information.
Its appearance on unusual areas can cause confusion, but herpes simplex can manifest almost anywhere: toes, legs, nipples, the tips of ears, and even the eye. On the thicker skin of fingers, these vesicles may be a bit harder to recognize than they would be on a penis or lip.
Because it is often assumed that pus designates a bacterial infection, its presence in this situation can be puzzling. But pus is really just a collection of dead white cells, often seen in conditions unrelated to bacteria (eg, psoriasis).
One additional factor played a role in the diagnosis of this condition. Atopic children (with seasonal allergies, asthma, eczema, and other related phenomena) are exceptionally susceptible to skin infections of all kinds, including bacterial, viral, and fungal. Further evaluation revealed that this child had a history of molluscum contagiosum and impetigo.
If the nature of this outbreak had been unclear, it could have been cultured (though it could take a week or two to get results) or even biopsied. The latter option would have shown the cytopathic effects of the virus.
No treatment was possible, nor was it necessary. HW has to be treated within the first day or two of the outbreak to be effective. Since this patient’s outbreaks only occur once a year, he does not need prophylactic treatment. Over time, as he and his immune system mature, he can be expected to have fewer attacks.
In terms of contagion, he represents no more threat to others than a child with a cold sore or a wart.
TAKE-HOME LEARNING POINTS
• Herpetic whitlow (HW), although commonly found on fingers, can occur almost anywhere.
• The causative organism is herpes simplex; each episode begins with premonitory symptoms, followed within a few days by the appearance of grouped vesicles on an erythematous base. After a week or two, the episode resolves.
• Herpes infections of all kinds in immunocompetent patients tend to recur in the same places repeatedly.
• Atopy predisposes to skin infections of all kinds.
• Pus is not necessarily an indication of bacterial infection; it is often seen in viral infections.
The stubborn focal eruption on this 6-year-old boy’s left fourth finger remains unaffected after a one-week course of oral cephalexin, so his pediatrician refers him to dermatology. The problem initially manifested as a cluster of tiny blisters, which tingled a bit but didn’t hurt. When redness developed around it, the patient’s mother brought him for evaluation.
The boy experienced the same problem in the same location almost exactly a year ago. It was treated the same way and within a week or two had resolved.
The child is otherwise reasonably healthy, despite being allergy-prone. He has a history of seasonal allergies and is susceptible to skin infections, such as staph.
EXAMINATION
On the dorsal aspect of his finger are grouped vesicles on an erythematous base, measuring about 1 cm altogether. Several of these demonstrate central umbilication, and several are filled with pus. The erythema is minimal, and there is no tenderness on palpation. Palpation of the epitrochlear area reveals a tiny, nontender node.

What is the diagnosis?
DISCUSSION
Herpetic whitlow (HW), while uncommon, is far from rare. Essentially a cold sore occurring away from the usual labial/facial location, HW presents with premonitory symptoms of itch, tingle, and slight pain, followed by the appearance of grouped vesicles on an erythematous base. The vesicles are often umbillicated, as with most herpetic conditions. And, like most herpes simplex–related outbreaks, HW tends to recur in the same location—an extremely useful piece of information.
Its appearance on unusual areas can cause confusion, but herpes simplex can manifest almost anywhere: toes, legs, nipples, the tips of ears, and even the eye. On the thicker skin of fingers, these vesicles may be a bit harder to recognize than they would be on a penis or lip.
Because it is often assumed that pus designates a bacterial infection, its presence in this situation can be puzzling. But pus is really just a collection of dead white cells, often seen in conditions unrelated to bacteria (eg, psoriasis).
One additional factor played a role in the diagnosis of this condition. Atopic children (with seasonal allergies, asthma, eczema, and other related phenomena) are exceptionally susceptible to skin infections of all kinds, including bacterial, viral, and fungal. Further evaluation revealed that this child had a history of molluscum contagiosum and impetigo.
If the nature of this outbreak had been unclear, it could have been cultured (though it could take a week or two to get results) or even biopsied. The latter option would have shown the cytopathic effects of the virus.
No treatment was possible, nor was it necessary. HW has to be treated within the first day or two of the outbreak to be effective. Since this patient’s outbreaks only occur once a year, he does not need prophylactic treatment. Over time, as he and his immune system mature, he can be expected to have fewer attacks.
In terms of contagion, he represents no more threat to others than a child with a cold sore or a wart.
TAKE-HOME LEARNING POINTS
• Herpetic whitlow (HW), although commonly found on fingers, can occur almost anywhere.
• The causative organism is herpes simplex; each episode begins with premonitory symptoms, followed within a few days by the appearance of grouped vesicles on an erythematous base. After a week or two, the episode resolves.
• Herpes infections of all kinds in immunocompetent patients tend to recur in the same places repeatedly.
• Atopy predisposes to skin infections of all kinds.
• Pus is not necessarily an indication of bacterial infection; it is often seen in viral infections.
The stubborn focal eruption on this 6-year-old boy’s left fourth finger remains unaffected after a one-week course of oral cephalexin, so his pediatrician refers him to dermatology. The problem initially manifested as a cluster of tiny blisters, which tingled a bit but didn’t hurt. When redness developed around it, the patient’s mother brought him for evaluation.
The boy experienced the same problem in the same location almost exactly a year ago. It was treated the same way and within a week or two had resolved.
The child is otherwise reasonably healthy, despite being allergy-prone. He has a history of seasonal allergies and is susceptible to skin infections, such as staph.
EXAMINATION
On the dorsal aspect of his finger are grouped vesicles on an erythematous base, measuring about 1 cm altogether. Several of these demonstrate central umbilication, and several are filled with pus. The erythema is minimal, and there is no tenderness on palpation. Palpation of the epitrochlear area reveals a tiny, nontender node.

What is the diagnosis?
DISCUSSION
Herpetic whitlow (HW), while uncommon, is far from rare. Essentially a cold sore occurring away from the usual labial/facial location, HW presents with premonitory symptoms of itch, tingle, and slight pain, followed by the appearance of grouped vesicles on an erythematous base. The vesicles are often umbillicated, as with most herpetic conditions. And, like most herpes simplex–related outbreaks, HW tends to recur in the same location—an extremely useful piece of information.
Its appearance on unusual areas can cause confusion, but herpes simplex can manifest almost anywhere: toes, legs, nipples, the tips of ears, and even the eye. On the thicker skin of fingers, these vesicles may be a bit harder to recognize than they would be on a penis or lip.
Because it is often assumed that pus designates a bacterial infection, its presence in this situation can be puzzling. But pus is really just a collection of dead white cells, often seen in conditions unrelated to bacteria (eg, psoriasis).
One additional factor played a role in the diagnosis of this condition. Atopic children (with seasonal allergies, asthma, eczema, and other related phenomena) are exceptionally susceptible to skin infections of all kinds, including bacterial, viral, and fungal. Further evaluation revealed that this child had a history of molluscum contagiosum and impetigo.
If the nature of this outbreak had been unclear, it could have been cultured (though it could take a week or two to get results) or even biopsied. The latter option would have shown the cytopathic effects of the virus.
No treatment was possible, nor was it necessary. HW has to be treated within the first day or two of the outbreak to be effective. Since this patient’s outbreaks only occur once a year, he does not need prophylactic treatment. Over time, as he and his immune system mature, he can be expected to have fewer attacks.
In terms of contagion, he represents no more threat to others than a child with a cold sore or a wart.
TAKE-HOME LEARNING POINTS
• Herpetic whitlow (HW), although commonly found on fingers, can occur almost anywhere.
• The causative organism is herpes simplex; each episode begins with premonitory symptoms, followed within a few days by the appearance of grouped vesicles on an erythematous base. After a week or two, the episode resolves.
• Herpes infections of all kinds in immunocompetent patients tend to recur in the same places repeatedly.
• Atopy predisposes to skin infections of all kinds.
• Pus is not necessarily an indication of bacterial infection; it is often seen in viral infections.
Of Cell Phones & Skin Damage
A 54-year-old man is seen for evaluation of various skin problems, none of which he believes to be serious. His concern primarily stems from his job of 30 years, which keeps him outdoors most days with minimal protection from the sun.
In addition to the generally weathered skin on his sun-exposed arms and face, his wife has noticed redness around his neck and chest that is slowly worsening with time.
He denies any discomfort with the changes in his neck skin. He has a history of diabetes and smoking.
EXAMINATION
There is well-defined redness around his neck, especially in the front, that spills down onto his chest. Strangely, instead of matching the scoop neckline of the t-shirts he always wears, the chest redness is asymmetrical. It veers off to the patient’s left, sparing the midline chest. The erythema is partially blanchable with digital pressure but totally macular with no increased warmth.
What is the diagnosis?
DISCUSSION
This patient’s condition is poikiloderma of Civatte (PC), an increase in surface vasculature etched into the skin by chronic overexposure to the sun. PC usually follows a very predictable pattern, mirroring the patient’s usual attire. This made the asymmetry in this patient’s case striking and puzzling. Speculation included uneven sunscreen application or use of clothing such as overalls, which tend to shift during wearing, but the cause remained a mystery—that is, until the patient got dressed.
After putting his shirt back on, he placed his large, heavy cell phone in the left pocket, effectively pulling his shirt down and to the left. This exposed more skin on that side, covering up the right side of the chest. He confirmed that he carried the cell phone in his shirt pocket constantly during his waking hours, at home and on the job.
This conundrum needed to be solved in order to rule out other possible conditions. There’s no rule that prevents a person from having two adjacent diagnoses at the same time, such as PC and Bowen disease (a superficial form of squamous cell carcinoma). In this case, the patient’s skin changes were all consistent with one diagnosis.
TAKE-HOME LEARNING POINTS
• Poikiloderma of Civatte (PC) is the term given to a particular pattern of chronic overexposure to UV rays, typically affecting the neck and upper chest.
• PC is often caused by occupational sun exposure.
• Unless treated with a laser, PC changes are permanent but harmless. They do, however, identify the patient as being at risk for sun-caused skin cancer.
• Atypical presentations of what appear to be common problems may need a bit of investigation to rule out other items in the differential.
A 54-year-old man is seen for evaluation of various skin problems, none of which he believes to be serious. His concern primarily stems from his job of 30 years, which keeps him outdoors most days with minimal protection from the sun.
In addition to the generally weathered skin on his sun-exposed arms and face, his wife has noticed redness around his neck and chest that is slowly worsening with time.
He denies any discomfort with the changes in his neck skin. He has a history of diabetes and smoking.
EXAMINATION
There is well-defined redness around his neck, especially in the front, that spills down onto his chest. Strangely, instead of matching the scoop neckline of the t-shirts he always wears, the chest redness is asymmetrical. It veers off to the patient’s left, sparing the midline chest. The erythema is partially blanchable with digital pressure but totally macular with no increased warmth.
What is the diagnosis?
DISCUSSION
This patient’s condition is poikiloderma of Civatte (PC), an increase in surface vasculature etched into the skin by chronic overexposure to the sun. PC usually follows a very predictable pattern, mirroring the patient’s usual attire. This made the asymmetry in this patient’s case striking and puzzling. Speculation included uneven sunscreen application or use of clothing such as overalls, which tend to shift during wearing, but the cause remained a mystery—that is, until the patient got dressed.
After putting his shirt back on, he placed his large, heavy cell phone in the left pocket, effectively pulling his shirt down and to the left. This exposed more skin on that side, covering up the right side of the chest. He confirmed that he carried the cell phone in his shirt pocket constantly during his waking hours, at home and on the job.
This conundrum needed to be solved in order to rule out other possible conditions. There’s no rule that prevents a person from having two adjacent diagnoses at the same time, such as PC and Bowen disease (a superficial form of squamous cell carcinoma). In this case, the patient’s skin changes were all consistent with one diagnosis.
TAKE-HOME LEARNING POINTS
• Poikiloderma of Civatte (PC) is the term given to a particular pattern of chronic overexposure to UV rays, typically affecting the neck and upper chest.
• PC is often caused by occupational sun exposure.
• Unless treated with a laser, PC changes are permanent but harmless. They do, however, identify the patient as being at risk for sun-caused skin cancer.
• Atypical presentations of what appear to be common problems may need a bit of investigation to rule out other items in the differential.
A 54-year-old man is seen for evaluation of various skin problems, none of which he believes to be serious. His concern primarily stems from his job of 30 years, which keeps him outdoors most days with minimal protection from the sun.
In addition to the generally weathered skin on his sun-exposed arms and face, his wife has noticed redness around his neck and chest that is slowly worsening with time.
He denies any discomfort with the changes in his neck skin. He has a history of diabetes and smoking.
EXAMINATION
There is well-defined redness around his neck, especially in the front, that spills down onto his chest. Strangely, instead of matching the scoop neckline of the t-shirts he always wears, the chest redness is asymmetrical. It veers off to the patient’s left, sparing the midline chest. The erythema is partially blanchable with digital pressure but totally macular with no increased warmth.
What is the diagnosis?
DISCUSSION
This patient’s condition is poikiloderma of Civatte (PC), an increase in surface vasculature etched into the skin by chronic overexposure to the sun. PC usually follows a very predictable pattern, mirroring the patient’s usual attire. This made the asymmetry in this patient’s case striking and puzzling. Speculation included uneven sunscreen application or use of clothing such as overalls, which tend to shift during wearing, but the cause remained a mystery—that is, until the patient got dressed.
After putting his shirt back on, he placed his large, heavy cell phone in the left pocket, effectively pulling his shirt down and to the left. This exposed more skin on that side, covering up the right side of the chest. He confirmed that he carried the cell phone in his shirt pocket constantly during his waking hours, at home and on the job.
This conundrum needed to be solved in order to rule out other possible conditions. There’s no rule that prevents a person from having two adjacent diagnoses at the same time, such as PC and Bowen disease (a superficial form of squamous cell carcinoma). In this case, the patient’s skin changes were all consistent with one diagnosis.
TAKE-HOME LEARNING POINTS
• Poikiloderma of Civatte (PC) is the term given to a particular pattern of chronic overexposure to UV rays, typically affecting the neck and upper chest.
• PC is often caused by occupational sun exposure.
• Unless treated with a laser, PC changes are permanent but harmless. They do, however, identify the patient as being at risk for sun-caused skin cancer.
• Atypical presentations of what appear to be common problems may need a bit of investigation to rule out other items in the differential.