User login
A 47-year-old man with eruptions on his trunk
A 47-year-old white male came to the hospital emergency department complaining of chest pain. At admission, it was noted that the patient had numerous lesions on his buttocks, abdomen, back, and all extremities (FIGURES 1 AND 2). These lesions had been there for approximately 5 months—they developed after he discontinued his cholesterol medication due to lapsed insurance coverage. He had a similar eruption when he went off cholesterol medication on another occasion.
The patient’s medical history included type 2 diabetes mellitus, hypertension, coronary artery disease, and hyperlipidemia. He has had multiple heart catheterizations with stent placement, most recently 2 years ago. His mother also had diabetes mellitus, and she died at age 58 from a myocardial infarction.
On examination, his lesions were painless and nonpruritic. He had numerous yellow papules on his buttocks, abdomen, back, and upper and lower extremities. He had no lesions on his face. The rest of the physical exam showed no abnormal results.
FIGURE 1
Nodular lesions on back
The patient had yellow nodular lesions covering his entire trunk and all 4 extremities.
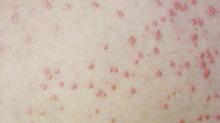
FIGURE 2
Close-up
What is your diagnosis?
What laboratory tests should be done to help make the diagnosis?
DIAGNOSIS: Eruptive xanthomas
This patient has eruptive xanthomas secondary to hypertriglyceridemia. His type IV hyperlipidemia has been worsened by long-standing, poorly controlled type 2 diabetes.
Xanthomas are lipid deposits in the skin and tendons that occur secondarily to a lipid abnormality. These lipid deposits are yellow and frequently firm.1 Although certain types of xanthomas are characteristic of particular lipid abnormalities, none is totally specific because the same form of xanthomas occurs in many different diseases.2
Xanthomas occur in various metabolic disorders and can also be associated with neoplasms. They may be associated with familial or acquired disorders resulting in hyperlipidemia or may be present with no underlying disorder.3
Types of xanthomas. Xanthomas are classified into 5 types based on clinical appearance. Tuberous and tendinous xanthomas both occur on the extensors of fingers and Achilles tendon. They appear as yellow nodules. Plane xanthomas are associated with biliary disease and appear as linear yellow lesions. Xanthelasmas appear as yellow plaques on the eyelids. Eruptive xanthomas are yellow papules that appear and disappear according to variations in lipid levels, especially triglycerides.3 As in this case, eruptive xanthomas usually appear over the buttocks, shoulders, back, and extensor surfaces of the extremities.4
Laboratory tests helpful in making the diagnosis
The patient’s tests on hospital admission showed normal cardiac enzymes and a normal electrocardiogram (ECG). His electrolytes were within normal limits except for a pseudohyponatremia of 133 mEq/dL due to an elevated glucose of 549 mg/dL.
A lipid profile the following morning revealed a triglyceride level of 1976 mg/dL, a total cholesterol level of 323 mg/dL, and a high-density lipoprotein (HDL) cholesterol level of 24 mg/dL. The low-density lipoprotein (LDL) cholesterol could not be calculated due to the high triglyceride level.
Differential diagnosis
Neurofibromas may have an appearance similar to eruptive xanthomas, but would usually be less numerous and less symptomatic. Prurigo nodularis would be another condition to be considered; however, this patient did not have any excoriations. Primary milia can also appear as keratinfilled cysts; however, these are much smaller and usually located on the face.
TREATMENT: Control the lipids and triglycerides
Patients may be prescribed HMG-CoA reductase inhibitors (statins) and fibric acid derivatives for control of lipid and triglyceride abnormalities. Further, counseling should involve diet modification, exercise, smoking cessation, and stringent control of diabetes.5 As a general rule, high doses of statins should not be given to patients who are taking fibrates.6 The combination of a statin and fibric acid derivative is not without risks: it may increase the risk of myopathy and rhabdomyolysis.
We started this patient on fenofibrate (Tricor) along with rosuvastatin (Crestor). When given in combination with any statin medication, fenofibrate resulted in fewer reports of rhabdomyolysis and myopathy than the older fibrate gemfibrozil (Lopid). It is believed that fenofibrate undergoes a different pathway of glucuronidation than gemfibrozil. Most statins undergo glucuronidation in the same family of enzymes as gemfibrozil, which could cause competition in converting the statin to a form that undergoes liver metabolism. Thus, metabolism of the statin is decreased and adverse effects such as rhabdomyolysis and myopathy occurs.7
Outcome
The patient started on rosuvastatin 10 mg once a day and fenofibrate 145 mg once a day. The patient’s xanthomas improved dramatically within a month (FIGURES 3 AND 4). His cholesterol, on the therapy described above, improved dramatically. His triglycerides decreased to 363 mg/dL. His total cholesterol was now 138 mg/dL, with an HDL of 34 mg/dL and an LDL of 31 mg/dL.
FIGURE 3
After treatment
FIGURE 4
Close-up
The patient reported no adverse effects from the medications. It was recommended that he continue on his present therapy indefinitely with the proper laboratory follow-up. We have not increased his dose of either medication, since his admission and no side effects have been encountered. We will continue to monitor his liver function tests and adjust the dose of his medications as needed.
CORRESPONDENCE
Jay Shubrook, DO, Parks Hall, Ohio University College of Medicine, Athens, OH 45701.
1. Damjanov I, Linder J. Diseases of the skin and connective tissues. In: Anderson’s Pathology. 10th ed. St Louis, Mo: Mosby, 1996:2454-2455.
2. Habif T. Xanthomas and dyslipoproteinemia. In: Clinical Dermatology. 4th ed. St Louis, Mo: Mosby, 2004:902-904.
3. Kumar V, Abbas A, Fausto N. Diseases of organ systems. In: Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders, 2005:1248.
4. Freedberg I, Eisen A, Wolff K, et al. Xanthomatoses and lipoprotein disorders. In: Fitzpatrick’s Dermatology in General Medicine. 5th ed. New York: McGraw-Hill, 1999:1804-1809.
5. Braunwald E, Fauci A, Kasper D, Hauser S, Longo D, Jameson J. Disorders of lipoprotein metabolism. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill, 2001:2245-2256.
6. Knopp RH. Drug treatment of lipid disorders. N Engl J Med 1999;341:498-511.
7. Corsini A, Bellosta S, Davidson MH. Pharmacokinetic interactions between statins and fibrates. Am J Cardiol 2005;96(9A):44K–49K; 34K-35K. Epub 2005 Oct 21.
A 47-year-old white male came to the hospital emergency department complaining of chest pain. At admission, it was noted that the patient had numerous lesions on his buttocks, abdomen, back, and all extremities (FIGURES 1 AND 2). These lesions had been there for approximately 5 months—they developed after he discontinued his cholesterol medication due to lapsed insurance coverage. He had a similar eruption when he went off cholesterol medication on another occasion.
The patient’s medical history included type 2 diabetes mellitus, hypertension, coronary artery disease, and hyperlipidemia. He has had multiple heart catheterizations with stent placement, most recently 2 years ago. His mother also had diabetes mellitus, and she died at age 58 from a myocardial infarction.
On examination, his lesions were painless and nonpruritic. He had numerous yellow papules on his buttocks, abdomen, back, and upper and lower extremities. He had no lesions on his face. The rest of the physical exam showed no abnormal results.
FIGURE 1
Nodular lesions on back
The patient had yellow nodular lesions covering his entire trunk and all 4 extremities.
FIGURE 2
Close-up
What is your diagnosis?
What laboratory tests should be done to help make the diagnosis?
DIAGNOSIS: Eruptive xanthomas
This patient has eruptive xanthomas secondary to hypertriglyceridemia. His type IV hyperlipidemia has been worsened by long-standing, poorly controlled type 2 diabetes.
Xanthomas are lipid deposits in the skin and tendons that occur secondarily to a lipid abnormality. These lipid deposits are yellow and frequently firm.1 Although certain types of xanthomas are characteristic of particular lipid abnormalities, none is totally specific because the same form of xanthomas occurs in many different diseases.2
Xanthomas occur in various metabolic disorders and can also be associated with neoplasms. They may be associated with familial or acquired disorders resulting in hyperlipidemia or may be present with no underlying disorder.3
Types of xanthomas. Xanthomas are classified into 5 types based on clinical appearance. Tuberous and tendinous xanthomas both occur on the extensors of fingers and Achilles tendon. They appear as yellow nodules. Plane xanthomas are associated with biliary disease and appear as linear yellow lesions. Xanthelasmas appear as yellow plaques on the eyelids. Eruptive xanthomas are yellow papules that appear and disappear according to variations in lipid levels, especially triglycerides.3 As in this case, eruptive xanthomas usually appear over the buttocks, shoulders, back, and extensor surfaces of the extremities.4
Laboratory tests helpful in making the diagnosis
The patient’s tests on hospital admission showed normal cardiac enzymes and a normal electrocardiogram (ECG). His electrolytes were within normal limits except for a pseudohyponatremia of 133 mEq/dL due to an elevated glucose of 549 mg/dL.
A lipid profile the following morning revealed a triglyceride level of 1976 mg/dL, a total cholesterol level of 323 mg/dL, and a high-density lipoprotein (HDL) cholesterol level of 24 mg/dL. The low-density lipoprotein (LDL) cholesterol could not be calculated due to the high triglyceride level.
Differential diagnosis
Neurofibromas may have an appearance similar to eruptive xanthomas, but would usually be less numerous and less symptomatic. Prurigo nodularis would be another condition to be considered; however, this patient did not have any excoriations. Primary milia can also appear as keratinfilled cysts; however, these are much smaller and usually located on the face.
TREATMENT: Control the lipids and triglycerides
Patients may be prescribed HMG-CoA reductase inhibitors (statins) and fibric acid derivatives for control of lipid and triglyceride abnormalities. Further, counseling should involve diet modification, exercise, smoking cessation, and stringent control of diabetes.5 As a general rule, high doses of statins should not be given to patients who are taking fibrates.6 The combination of a statin and fibric acid derivative is not without risks: it may increase the risk of myopathy and rhabdomyolysis.
We started this patient on fenofibrate (Tricor) along with rosuvastatin (Crestor). When given in combination with any statin medication, fenofibrate resulted in fewer reports of rhabdomyolysis and myopathy than the older fibrate gemfibrozil (Lopid). It is believed that fenofibrate undergoes a different pathway of glucuronidation than gemfibrozil. Most statins undergo glucuronidation in the same family of enzymes as gemfibrozil, which could cause competition in converting the statin to a form that undergoes liver metabolism. Thus, metabolism of the statin is decreased and adverse effects such as rhabdomyolysis and myopathy occurs.7
Outcome
The patient started on rosuvastatin 10 mg once a day and fenofibrate 145 mg once a day. The patient’s xanthomas improved dramatically within a month (FIGURES 3 AND 4). His cholesterol, on the therapy described above, improved dramatically. His triglycerides decreased to 363 mg/dL. His total cholesterol was now 138 mg/dL, with an HDL of 34 mg/dL and an LDL of 31 mg/dL.
FIGURE 3
After treatment
FIGURE 4
Close-up
The patient reported no adverse effects from the medications. It was recommended that he continue on his present therapy indefinitely with the proper laboratory follow-up. We have not increased his dose of either medication, since his admission and no side effects have been encountered. We will continue to monitor his liver function tests and adjust the dose of his medications as needed.
CORRESPONDENCE
Jay Shubrook, DO, Parks Hall, Ohio University College of Medicine, Athens, OH 45701.
A 47-year-old white male came to the hospital emergency department complaining of chest pain. At admission, it was noted that the patient had numerous lesions on his buttocks, abdomen, back, and all extremities (FIGURES 1 AND 2). These lesions had been there for approximately 5 months—they developed after he discontinued his cholesterol medication due to lapsed insurance coverage. He had a similar eruption when he went off cholesterol medication on another occasion.
The patient’s medical history included type 2 diabetes mellitus, hypertension, coronary artery disease, and hyperlipidemia. He has had multiple heart catheterizations with stent placement, most recently 2 years ago. His mother also had diabetes mellitus, and she died at age 58 from a myocardial infarction.
On examination, his lesions were painless and nonpruritic. He had numerous yellow papules on his buttocks, abdomen, back, and upper and lower extremities. He had no lesions on his face. The rest of the physical exam showed no abnormal results.
FIGURE 1
Nodular lesions on back
The patient had yellow nodular lesions covering his entire trunk and all 4 extremities.
FIGURE 2
Close-up
What is your diagnosis?
What laboratory tests should be done to help make the diagnosis?
DIAGNOSIS: Eruptive xanthomas
This patient has eruptive xanthomas secondary to hypertriglyceridemia. His type IV hyperlipidemia has been worsened by long-standing, poorly controlled type 2 diabetes.
Xanthomas are lipid deposits in the skin and tendons that occur secondarily to a lipid abnormality. These lipid deposits are yellow and frequently firm.1 Although certain types of xanthomas are characteristic of particular lipid abnormalities, none is totally specific because the same form of xanthomas occurs in many different diseases.2
Xanthomas occur in various metabolic disorders and can also be associated with neoplasms. They may be associated with familial or acquired disorders resulting in hyperlipidemia or may be present with no underlying disorder.3
Types of xanthomas. Xanthomas are classified into 5 types based on clinical appearance. Tuberous and tendinous xanthomas both occur on the extensors of fingers and Achilles tendon. They appear as yellow nodules. Plane xanthomas are associated with biliary disease and appear as linear yellow lesions. Xanthelasmas appear as yellow plaques on the eyelids. Eruptive xanthomas are yellow papules that appear and disappear according to variations in lipid levels, especially triglycerides.3 As in this case, eruptive xanthomas usually appear over the buttocks, shoulders, back, and extensor surfaces of the extremities.4
Laboratory tests helpful in making the diagnosis
The patient’s tests on hospital admission showed normal cardiac enzymes and a normal electrocardiogram (ECG). His electrolytes were within normal limits except for a pseudohyponatremia of 133 mEq/dL due to an elevated glucose of 549 mg/dL.
A lipid profile the following morning revealed a triglyceride level of 1976 mg/dL, a total cholesterol level of 323 mg/dL, and a high-density lipoprotein (HDL) cholesterol level of 24 mg/dL. The low-density lipoprotein (LDL) cholesterol could not be calculated due to the high triglyceride level.
Differential diagnosis
Neurofibromas may have an appearance similar to eruptive xanthomas, but would usually be less numerous and less symptomatic. Prurigo nodularis would be another condition to be considered; however, this patient did not have any excoriations. Primary milia can also appear as keratinfilled cysts; however, these are much smaller and usually located on the face.
TREATMENT: Control the lipids and triglycerides
Patients may be prescribed HMG-CoA reductase inhibitors (statins) and fibric acid derivatives for control of lipid and triglyceride abnormalities. Further, counseling should involve diet modification, exercise, smoking cessation, and stringent control of diabetes.5 As a general rule, high doses of statins should not be given to patients who are taking fibrates.6 The combination of a statin and fibric acid derivative is not without risks: it may increase the risk of myopathy and rhabdomyolysis.
We started this patient on fenofibrate (Tricor) along with rosuvastatin (Crestor). When given in combination with any statin medication, fenofibrate resulted in fewer reports of rhabdomyolysis and myopathy than the older fibrate gemfibrozil (Lopid). It is believed that fenofibrate undergoes a different pathway of glucuronidation than gemfibrozil. Most statins undergo glucuronidation in the same family of enzymes as gemfibrozil, which could cause competition in converting the statin to a form that undergoes liver metabolism. Thus, metabolism of the statin is decreased and adverse effects such as rhabdomyolysis and myopathy occurs.7
Outcome
The patient started on rosuvastatin 10 mg once a day and fenofibrate 145 mg once a day. The patient’s xanthomas improved dramatically within a month (FIGURES 3 AND 4). His cholesterol, on the therapy described above, improved dramatically. His triglycerides decreased to 363 mg/dL. His total cholesterol was now 138 mg/dL, with an HDL of 34 mg/dL and an LDL of 31 mg/dL.
FIGURE 3
After treatment
FIGURE 4
Close-up
The patient reported no adverse effects from the medications. It was recommended that he continue on his present therapy indefinitely with the proper laboratory follow-up. We have not increased his dose of either medication, since his admission and no side effects have been encountered. We will continue to monitor his liver function tests and adjust the dose of his medications as needed.
CORRESPONDENCE
Jay Shubrook, DO, Parks Hall, Ohio University College of Medicine, Athens, OH 45701.
1. Damjanov I, Linder J. Diseases of the skin and connective tissues. In: Anderson’s Pathology. 10th ed. St Louis, Mo: Mosby, 1996:2454-2455.
2. Habif T. Xanthomas and dyslipoproteinemia. In: Clinical Dermatology. 4th ed. St Louis, Mo: Mosby, 2004:902-904.
3. Kumar V, Abbas A, Fausto N. Diseases of organ systems. In: Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders, 2005:1248.
4. Freedberg I, Eisen A, Wolff K, et al. Xanthomatoses and lipoprotein disorders. In: Fitzpatrick’s Dermatology in General Medicine. 5th ed. New York: McGraw-Hill, 1999:1804-1809.
5. Braunwald E, Fauci A, Kasper D, Hauser S, Longo D, Jameson J. Disorders of lipoprotein metabolism. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill, 2001:2245-2256.
6. Knopp RH. Drug treatment of lipid disorders. N Engl J Med 1999;341:498-511.
7. Corsini A, Bellosta S, Davidson MH. Pharmacokinetic interactions between statins and fibrates. Am J Cardiol 2005;96(9A):44K–49K; 34K-35K. Epub 2005 Oct 21.
1. Damjanov I, Linder J. Diseases of the skin and connective tissues. In: Anderson’s Pathology. 10th ed. St Louis, Mo: Mosby, 1996:2454-2455.
2. Habif T. Xanthomas and dyslipoproteinemia. In: Clinical Dermatology. 4th ed. St Louis, Mo: Mosby, 2004:902-904.
3. Kumar V, Abbas A, Fausto N. Diseases of organ systems. In: Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders, 2005:1248.
4. Freedberg I, Eisen A, Wolff K, et al. Xanthomatoses and lipoprotein disorders. In: Fitzpatrick’s Dermatology in General Medicine. 5th ed. New York: McGraw-Hill, 1999:1804-1809.
5. Braunwald E, Fauci A, Kasper D, Hauser S, Longo D, Jameson J. Disorders of lipoprotein metabolism. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill, 2001:2245-2256.
6. Knopp RH. Drug treatment of lipid disorders. N Engl J Med 1999;341:498-511.
7. Corsini A, Bellosta S, Davidson MH. Pharmacokinetic interactions between statins and fibrates. Am J Cardiol 2005;96(9A):44K–49K; 34K-35K. Epub 2005 Oct 21.