User login
Allegations: Current Trends in Medical Malpractice, Part 2
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
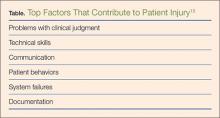
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Allegations: Current Trends in Medical Malpractice, Part 1
We’re lost, but we’re making good time.
-Yogi Berra
As Yogi Berra alludes, it is very easy to get caught up “in the flow” and continue to move along at a good pace, even when one does not know where he or she is ultimately headed. Similarly, in terms of medical malpractice, everyone seems to have an opinion on what should be done to improve the climate of medical malpractice for both providers and patients. Yet, there are many differences in opinions on how to solve these issues, and the “cure” for what “ails” in the system are many—with an undetermined endpoint.
Tort reform is often conjured as the communal fix; yet each state in the Union has its own medical malpractice tort laws, which begs the question of how an issue with so many different facets can be resolved. Additionally, the risk alone of medical malpractice continues to be an important area of concern to emergency physicians (EPs), not only because of the looming threat of malpractice litigation—both real and perceived—but also because of its influence on practice patterns, resource utilization, and patient care in the ED.1,2
Physician Perception
Over the course of a career, an EP faces at least one claim, further perpetuating a common physician perception that the occurrence of a suit is not a condition of “if” but rather of “when.”3 This anxiety and fear among physicians in general are further provoked by the many headlines highlighting massive jury verdicts that dominate the news cycle.4
In addition, the EP’s work and practice are increasingly affected by the impositions of multiple nationally reported quality metrics, institutional throughput goals, and process-improvement efforts. Each of these in turn has the effect of increasing the pace of care and can challenge one’s real-time ability to recognize the dangers of inherent biases, to appreciate and act upon subtle clinical clues, and to rescue patient-experience misadventures. Accordingly, medical malpractice is a frequent topic of discussion for policy proposals among physicians and legislators.
Defensive Medicine and Tort Reform
As spending on health care in the United States topped $3 trillion, or 17.5% of the US gross domestic product in 2014, strategies for cost-containment have become a primary concern across all sectors of the health-care industry.5,6 With defensive medicine proposed by some as a substantial driver of health-care costs, many physicians have focused on tort reform as an avenue to curb defensive testing. This has resulted in substantial policy shifts in a number of jurisdictions.7,8 Some of the policy changes that have taken place over the past few decades have included state-imposed caps on medical malpractice awards and noneconomic damages, caps on attorney fees, and shortened statutes of limitations that require more timely filing of malpractice suits.
Defining Malpractice and Imposing Caps
In 2003, Texas changed its definition of the medical malpractice standard to “willful and wanton negligence”; in Georgia (2005) and South Carolina (2005) the definition was changed to “gross negligence.” Both of these revised definitions are essentially synonymous in a legal sense and are intended to protect physicians working in a high-risk, limited-information, high-intensity environment (eg, the ED) by raising the plaintiff’s responsibility to prove that the defendant physician was aware of the likelihood of serious injury but proceeded with “conscious indifference.”9
It seems, however, that such efforts have been not been entirely effective in reigning in costs of care, decreasing insurance costs, and limiting defensive medicine, particularly in the ED.9 A study by Paik et al10 on the effect of caps on malpractice claims and payouts found that in states with caps, both claims and payouts were effectively reduced, with a large impact on payout per physician and a drop in claims for those cases with larger payouts. While stricter caps had larger effects, the authors did not examine the impact of caps on “defensive medicine.”10 Furthermore, many physicians, health systems, and patient advocacy groups have been exploring and implementing alternative models of claim resolution outside of the legal process.11
Alternative Compensation Models
In the state legislatures of Georgia and Florida, alternative patient-compensation models are currently under proposal. Both models are designed to eliminate the current medical tort system and replace it with an administrative system to compensate patients for medical errors that have caused them harm.12 These proposals are similar to the existing Birth-Related Neurological Injury Compensation Programs (BRNICP) in effect in both Florida and Virginia. The BRNICP in each of these states serves as an administrative system to provide monetary compensation to patients who have clearly suffered only birth-related medical injuries, thus keeping this type of liability out of the court system.
Program Structure
Compensation programs such as the BRNICP in Florida and Virginia would replace traditional tort law. In this system, physicians would pay annually into a compensation fund (as do the physicians in Virginia and Florida), with amounts prorated to liability risk based on practice specialty. A patient harmed by a claimed medical injury that was allegedly caused by the proximate treatment rendered, would apply to the patient compensation system via a designated patient advocate. The advocate would initiate the claim process on behalf of the patient, after which the claim would be reviewed by a panel of medical experts in the appropriate field. If the panel finds the injury was preventable or avoidable, the case would then proceed to a compensation committee to render payment to the injured individual.
This compensation model not only eliminates the need for legal counsel for the patient, but also the need for medical malpractice liability insurance and defense counsel for the physician. Unlike traditional tort law, this alternate process encourages a system of transparency that supports appropriate disclosure of medical error rather than delaying late discovery of error and increased angst both for the patient and the physician.
Potential Benefits
One would anticipate that an alternate compensation model such as the BRNCIP that eliminates the fear of a lawsuit (ie, if patients no longer sued physicians for medical malpractice) would have a significant impact on defensive medicine and its associated costs. A study conducted by Emory University concluded that as much as $7 billion in the state of Georgia could be saved each year if such a program was enacted.13 In addition to the financial benefits, the care of all patients would improve through increased efficiency and better appropriation of finite resources. Moreover, patients harmed in a medical mishap would have a more direct, expedited, and less expensive mechanism of compensation compared to traditional tort systems.
The alternate compensation model would also benefit patients by negating the need for legal counsel. In the current tort system, many cases go unaddressed either because the patient does not have the means to hire counsel or the case seems too inconsequential for a lawyer to accept it. The compensation system would improve access for patients with valid claims, from egregious high impact errors to the lower impact errors, which are still significant.
There are also public health benefits to the alternate compensation model, including advances in patient safety as a result of the transparency of medical error and addressing medical mishaps in a timelier manner, providing an opportunity to improve knowledge and system gaps closer to real-time events. No longer would a patient have to forge an adversarial offensive on a physician. The panel of experts, who becomes the peer of the physician, can fairly assess the conditions of the case and bring forth an impartial recommendation to either reimburse or not reimburse the patient.
By eliminating the punitive nature of tort law upon the physician, and because this system compensates through a state-based compensation program, there is no indelible report made naming the physician to the National Practitioner Data Bank. Further, if a provider is identified as a significant risk to the public, the panel of medical experts can report that physician to the state licensing board immediately, which would prove more effective and efficient than the traditional method of data collection and referral currently in place in most states.
Challenges
Challenges to these bills include resistance from those who may be adversely affected by such legislation—mainly medical malpractice trial lawyers (both plaintiff and defendant) and medical malpractice insurance companies.
Conclusion
In consideration of innovative solutions to medical malpractice reform, the efforts in the states of Georgia and Florida clearly think outside the box. Neither of these proposed solutions is currently operational, but certainly if they become state statutes, they will create a very interesting environment to observe while the effects of such systems play out. The operations of the birth-related injury funds have been successful in states that have already implemented such programs. In the meantime, pending such changes in policy and legislation, EPs can mitigate malpractice risk by maintaining board certification and specialty training requirements, and by employing the following:
Follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for;
Maintain open communication with patients—a paramount component in reducing the risk of a malpractice allegation;
Ensure that all members of the care team engender an environment that is focused on patient safety, including open communication with nursing staff and technical support;
Be aware of inherent biases in medical decision-making, which helps to maintain mindfulness in the routine practice of emergency medicine (EM);
Make sure departmental policies and procedures are designed to identify and address all late resulting laboratory results, radiology reading discrepancies and culture results in a timely and uniform manner; and
Provide clear and concise at-home care instructions to patients—prior to discharge—and in a manner the patient can understand.
Part 2 will discuss each of these recommendations in detail and will consider recent trends in medical malpractice as they relate to EM, explore areas of risk, and discuss strategies to reduce medical malpractice risk in the ED.
- Charles SC. Coping with a medical malpractice suit. West J Med. 2001;174(1): 55-58.
- Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6): 525-533.
- Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011; 365(7):629-636.
- Moran B. $6.41 million verdict in Temple malpractice lawsuit. Philadelphia Inquirer. 2012, June 2. http://articles.philly.com/2012-06-02/news/31960243_1_million-verdict-malpractice-massive-heart-attack. Accessed March 1, 2016.
- Martin AB, Hartman M, Benson J, Catlin A; National Health Expenditure Accounts Team. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2015;35(1):150-160.
- Emanuel E, Tanden N, Altman S, et al. A systemic approach to containing health care spending. N Engl J Med. 2012;367(10):949-954.
- Jost TS. Health care reform requires law reform. Health Aff (Millwood). 2009; 28(5): w761-w769.
- Roslund G. The medical malpractice rundown: a state-by-state report card. Emerg Phys Monthly. 2014;July 21. Available at http://epmonthly.com/article/the-medical-malpractice-rundown-a-state-by-state-report-card/. Accessed March 1, 2016.
- Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
- Paik M, Black BS, Hyma DA. The receding tide of medical malpractice litigation part 2: effect of damage caps. J Empirical Leg Stud. 2013;10(4):639-669.
- Stamm JA, Korzick KA, Beech K, Wood KE. Medical malpractice: reform for today’s patients and clinicians. Am J Med. 2016;129(1):20-25.
- Segal J. Finally: an end to malpractice litigation? Medscape. Available at http://www.medscape.com/viewarticle/840337_1. March 5,2015. Accessed March 1, 2016.
- Shinkman R. Patient compensation system could replace malpractice torts. Fierce Health Finance Web site. November 9, 2014. Available at http://www.fiercehealthfinance.com/story/patient-compensation-system-could-replace-malpractice-torts/2014-11-09. Accessed March 1, 2016.
We’re lost, but we’re making good time.
-Yogi Berra
As Yogi Berra alludes, it is very easy to get caught up “in the flow” and continue to move along at a good pace, even when one does not know where he or she is ultimately headed. Similarly, in terms of medical malpractice, everyone seems to have an opinion on what should be done to improve the climate of medical malpractice for both providers and patients. Yet, there are many differences in opinions on how to solve these issues, and the “cure” for what “ails” in the system are many—with an undetermined endpoint.
Tort reform is often conjured as the communal fix; yet each state in the Union has its own medical malpractice tort laws, which begs the question of how an issue with so many different facets can be resolved. Additionally, the risk alone of medical malpractice continues to be an important area of concern to emergency physicians (EPs), not only because of the looming threat of malpractice litigation—both real and perceived—but also because of its influence on practice patterns, resource utilization, and patient care in the ED.1,2
Physician Perception
Over the course of a career, an EP faces at least one claim, further perpetuating a common physician perception that the occurrence of a suit is not a condition of “if” but rather of “when.”3 This anxiety and fear among physicians in general are further provoked by the many headlines highlighting massive jury verdicts that dominate the news cycle.4
In addition, the EP’s work and practice are increasingly affected by the impositions of multiple nationally reported quality metrics, institutional throughput goals, and process-improvement efforts. Each of these in turn has the effect of increasing the pace of care and can challenge one’s real-time ability to recognize the dangers of inherent biases, to appreciate and act upon subtle clinical clues, and to rescue patient-experience misadventures. Accordingly, medical malpractice is a frequent topic of discussion for policy proposals among physicians and legislators.
Defensive Medicine and Tort Reform
As spending on health care in the United States topped $3 trillion, or 17.5% of the US gross domestic product in 2014, strategies for cost-containment have become a primary concern across all sectors of the health-care industry.5,6 With defensive medicine proposed by some as a substantial driver of health-care costs, many physicians have focused on tort reform as an avenue to curb defensive testing. This has resulted in substantial policy shifts in a number of jurisdictions.7,8 Some of the policy changes that have taken place over the past few decades have included state-imposed caps on medical malpractice awards and noneconomic damages, caps on attorney fees, and shortened statutes of limitations that require more timely filing of malpractice suits.
Defining Malpractice and Imposing Caps
In 2003, Texas changed its definition of the medical malpractice standard to “willful and wanton negligence”; in Georgia (2005) and South Carolina (2005) the definition was changed to “gross negligence.” Both of these revised definitions are essentially synonymous in a legal sense and are intended to protect physicians working in a high-risk, limited-information, high-intensity environment (eg, the ED) by raising the plaintiff’s responsibility to prove that the defendant physician was aware of the likelihood of serious injury but proceeded with “conscious indifference.”9
It seems, however, that such efforts have been not been entirely effective in reigning in costs of care, decreasing insurance costs, and limiting defensive medicine, particularly in the ED.9 A study by Paik et al10 on the effect of caps on malpractice claims and payouts found that in states with caps, both claims and payouts were effectively reduced, with a large impact on payout per physician and a drop in claims for those cases with larger payouts. While stricter caps had larger effects, the authors did not examine the impact of caps on “defensive medicine.”10 Furthermore, many physicians, health systems, and patient advocacy groups have been exploring and implementing alternative models of claim resolution outside of the legal process.11
Alternative Compensation Models
In the state legislatures of Georgia and Florida, alternative patient-compensation models are currently under proposal. Both models are designed to eliminate the current medical tort system and replace it with an administrative system to compensate patients for medical errors that have caused them harm.12 These proposals are similar to the existing Birth-Related Neurological Injury Compensation Programs (BRNICP) in effect in both Florida and Virginia. The BRNICP in each of these states serves as an administrative system to provide monetary compensation to patients who have clearly suffered only birth-related medical injuries, thus keeping this type of liability out of the court system.
Program Structure
Compensation programs such as the BRNICP in Florida and Virginia would replace traditional tort law. In this system, physicians would pay annually into a compensation fund (as do the physicians in Virginia and Florida), with amounts prorated to liability risk based on practice specialty. A patient harmed by a claimed medical injury that was allegedly caused by the proximate treatment rendered, would apply to the patient compensation system via a designated patient advocate. The advocate would initiate the claim process on behalf of the patient, after which the claim would be reviewed by a panel of medical experts in the appropriate field. If the panel finds the injury was preventable or avoidable, the case would then proceed to a compensation committee to render payment to the injured individual.
This compensation model not only eliminates the need for legal counsel for the patient, but also the need for medical malpractice liability insurance and defense counsel for the physician. Unlike traditional tort law, this alternate process encourages a system of transparency that supports appropriate disclosure of medical error rather than delaying late discovery of error and increased angst both for the patient and the physician.
Potential Benefits
One would anticipate that an alternate compensation model such as the BRNCIP that eliminates the fear of a lawsuit (ie, if patients no longer sued physicians for medical malpractice) would have a significant impact on defensive medicine and its associated costs. A study conducted by Emory University concluded that as much as $7 billion in the state of Georgia could be saved each year if such a program was enacted.13 In addition to the financial benefits, the care of all patients would improve through increased efficiency and better appropriation of finite resources. Moreover, patients harmed in a medical mishap would have a more direct, expedited, and less expensive mechanism of compensation compared to traditional tort systems.
The alternate compensation model would also benefit patients by negating the need for legal counsel. In the current tort system, many cases go unaddressed either because the patient does not have the means to hire counsel or the case seems too inconsequential for a lawyer to accept it. The compensation system would improve access for patients with valid claims, from egregious high impact errors to the lower impact errors, which are still significant.
There are also public health benefits to the alternate compensation model, including advances in patient safety as a result of the transparency of medical error and addressing medical mishaps in a timelier manner, providing an opportunity to improve knowledge and system gaps closer to real-time events. No longer would a patient have to forge an adversarial offensive on a physician. The panel of experts, who becomes the peer of the physician, can fairly assess the conditions of the case and bring forth an impartial recommendation to either reimburse or not reimburse the patient.
By eliminating the punitive nature of tort law upon the physician, and because this system compensates through a state-based compensation program, there is no indelible report made naming the physician to the National Practitioner Data Bank. Further, if a provider is identified as a significant risk to the public, the panel of medical experts can report that physician to the state licensing board immediately, which would prove more effective and efficient than the traditional method of data collection and referral currently in place in most states.
Challenges
Challenges to these bills include resistance from those who may be adversely affected by such legislation—mainly medical malpractice trial lawyers (both plaintiff and defendant) and medical malpractice insurance companies.
Conclusion
In consideration of innovative solutions to medical malpractice reform, the efforts in the states of Georgia and Florida clearly think outside the box. Neither of these proposed solutions is currently operational, but certainly if they become state statutes, they will create a very interesting environment to observe while the effects of such systems play out. The operations of the birth-related injury funds have been successful in states that have already implemented such programs. In the meantime, pending such changes in policy and legislation, EPs can mitigate malpractice risk by maintaining board certification and specialty training requirements, and by employing the following:
Follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for;
Maintain open communication with patients—a paramount component in reducing the risk of a malpractice allegation;
Ensure that all members of the care team engender an environment that is focused on patient safety, including open communication with nursing staff and technical support;
Be aware of inherent biases in medical decision-making, which helps to maintain mindfulness in the routine practice of emergency medicine (EM);
Make sure departmental policies and procedures are designed to identify and address all late resulting laboratory results, radiology reading discrepancies and culture results in a timely and uniform manner; and
Provide clear and concise at-home care instructions to patients—prior to discharge—and in a manner the patient can understand.
Part 2 will discuss each of these recommendations in detail and will consider recent trends in medical malpractice as they relate to EM, explore areas of risk, and discuss strategies to reduce medical malpractice risk in the ED.
We’re lost, but we’re making good time.
-Yogi Berra
As Yogi Berra alludes, it is very easy to get caught up “in the flow” and continue to move along at a good pace, even when one does not know where he or she is ultimately headed. Similarly, in terms of medical malpractice, everyone seems to have an opinion on what should be done to improve the climate of medical malpractice for both providers and patients. Yet, there are many differences in opinions on how to solve these issues, and the “cure” for what “ails” in the system are many—with an undetermined endpoint.
Tort reform is often conjured as the communal fix; yet each state in the Union has its own medical malpractice tort laws, which begs the question of how an issue with so many different facets can be resolved. Additionally, the risk alone of medical malpractice continues to be an important area of concern to emergency physicians (EPs), not only because of the looming threat of malpractice litigation—both real and perceived—but also because of its influence on practice patterns, resource utilization, and patient care in the ED.1,2
Physician Perception
Over the course of a career, an EP faces at least one claim, further perpetuating a common physician perception that the occurrence of a suit is not a condition of “if” but rather of “when.”3 This anxiety and fear among physicians in general are further provoked by the many headlines highlighting massive jury verdicts that dominate the news cycle.4
In addition, the EP’s work and practice are increasingly affected by the impositions of multiple nationally reported quality metrics, institutional throughput goals, and process-improvement efforts. Each of these in turn has the effect of increasing the pace of care and can challenge one’s real-time ability to recognize the dangers of inherent biases, to appreciate and act upon subtle clinical clues, and to rescue patient-experience misadventures. Accordingly, medical malpractice is a frequent topic of discussion for policy proposals among physicians and legislators.
Defensive Medicine and Tort Reform
As spending on health care in the United States topped $3 trillion, or 17.5% of the US gross domestic product in 2014, strategies for cost-containment have become a primary concern across all sectors of the health-care industry.5,6 With defensive medicine proposed by some as a substantial driver of health-care costs, many physicians have focused on tort reform as an avenue to curb defensive testing. This has resulted in substantial policy shifts in a number of jurisdictions.7,8 Some of the policy changes that have taken place over the past few decades have included state-imposed caps on medical malpractice awards and noneconomic damages, caps on attorney fees, and shortened statutes of limitations that require more timely filing of malpractice suits.
Defining Malpractice and Imposing Caps
In 2003, Texas changed its definition of the medical malpractice standard to “willful and wanton negligence”; in Georgia (2005) and South Carolina (2005) the definition was changed to “gross negligence.” Both of these revised definitions are essentially synonymous in a legal sense and are intended to protect physicians working in a high-risk, limited-information, high-intensity environment (eg, the ED) by raising the plaintiff’s responsibility to prove that the defendant physician was aware of the likelihood of serious injury but proceeded with “conscious indifference.”9
It seems, however, that such efforts have been not been entirely effective in reigning in costs of care, decreasing insurance costs, and limiting defensive medicine, particularly in the ED.9 A study by Paik et al10 on the effect of caps on malpractice claims and payouts found that in states with caps, both claims and payouts were effectively reduced, with a large impact on payout per physician and a drop in claims for those cases with larger payouts. While stricter caps had larger effects, the authors did not examine the impact of caps on “defensive medicine.”10 Furthermore, many physicians, health systems, and patient advocacy groups have been exploring and implementing alternative models of claim resolution outside of the legal process.11
Alternative Compensation Models
In the state legislatures of Georgia and Florida, alternative patient-compensation models are currently under proposal. Both models are designed to eliminate the current medical tort system and replace it with an administrative system to compensate patients for medical errors that have caused them harm.12 These proposals are similar to the existing Birth-Related Neurological Injury Compensation Programs (BRNICP) in effect in both Florida and Virginia. The BRNICP in each of these states serves as an administrative system to provide monetary compensation to patients who have clearly suffered only birth-related medical injuries, thus keeping this type of liability out of the court system.
Program Structure
Compensation programs such as the BRNICP in Florida and Virginia would replace traditional tort law. In this system, physicians would pay annually into a compensation fund (as do the physicians in Virginia and Florida), with amounts prorated to liability risk based on practice specialty. A patient harmed by a claimed medical injury that was allegedly caused by the proximate treatment rendered, would apply to the patient compensation system via a designated patient advocate. The advocate would initiate the claim process on behalf of the patient, after which the claim would be reviewed by a panel of medical experts in the appropriate field. If the panel finds the injury was preventable or avoidable, the case would then proceed to a compensation committee to render payment to the injured individual.
This compensation model not only eliminates the need for legal counsel for the patient, but also the need for medical malpractice liability insurance and defense counsel for the physician. Unlike traditional tort law, this alternate process encourages a system of transparency that supports appropriate disclosure of medical error rather than delaying late discovery of error and increased angst both for the patient and the physician.
Potential Benefits
One would anticipate that an alternate compensation model such as the BRNCIP that eliminates the fear of a lawsuit (ie, if patients no longer sued physicians for medical malpractice) would have a significant impact on defensive medicine and its associated costs. A study conducted by Emory University concluded that as much as $7 billion in the state of Georgia could be saved each year if such a program was enacted.13 In addition to the financial benefits, the care of all patients would improve through increased efficiency and better appropriation of finite resources. Moreover, patients harmed in a medical mishap would have a more direct, expedited, and less expensive mechanism of compensation compared to traditional tort systems.
The alternate compensation model would also benefit patients by negating the need for legal counsel. In the current tort system, many cases go unaddressed either because the patient does not have the means to hire counsel or the case seems too inconsequential for a lawyer to accept it. The compensation system would improve access for patients with valid claims, from egregious high impact errors to the lower impact errors, which are still significant.
There are also public health benefits to the alternate compensation model, including advances in patient safety as a result of the transparency of medical error and addressing medical mishaps in a timelier manner, providing an opportunity to improve knowledge and system gaps closer to real-time events. No longer would a patient have to forge an adversarial offensive on a physician. The panel of experts, who becomes the peer of the physician, can fairly assess the conditions of the case and bring forth an impartial recommendation to either reimburse or not reimburse the patient.
By eliminating the punitive nature of tort law upon the physician, and because this system compensates through a state-based compensation program, there is no indelible report made naming the physician to the National Practitioner Data Bank. Further, if a provider is identified as a significant risk to the public, the panel of medical experts can report that physician to the state licensing board immediately, which would prove more effective and efficient than the traditional method of data collection and referral currently in place in most states.
Challenges
Challenges to these bills include resistance from those who may be adversely affected by such legislation—mainly medical malpractice trial lawyers (both plaintiff and defendant) and medical malpractice insurance companies.
Conclusion
In consideration of innovative solutions to medical malpractice reform, the efforts in the states of Georgia and Florida clearly think outside the box. Neither of these proposed solutions is currently operational, but certainly if they become state statutes, they will create a very interesting environment to observe while the effects of such systems play out. The operations of the birth-related injury funds have been successful in states that have already implemented such programs. In the meantime, pending such changes in policy and legislation, EPs can mitigate malpractice risk by maintaining board certification and specialty training requirements, and by employing the following:
Follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for;
Maintain open communication with patients—a paramount component in reducing the risk of a malpractice allegation;
Ensure that all members of the care team engender an environment that is focused on patient safety, including open communication with nursing staff and technical support;
Be aware of inherent biases in medical decision-making, which helps to maintain mindfulness in the routine practice of emergency medicine (EM);
Make sure departmental policies and procedures are designed to identify and address all late resulting laboratory results, radiology reading discrepancies and culture results in a timely and uniform manner; and
Provide clear and concise at-home care instructions to patients—prior to discharge—and in a manner the patient can understand.
Part 2 will discuss each of these recommendations in detail and will consider recent trends in medical malpractice as they relate to EM, explore areas of risk, and discuss strategies to reduce medical malpractice risk in the ED.
- Charles SC. Coping with a medical malpractice suit. West J Med. 2001;174(1): 55-58.
- Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6): 525-533.
- Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011; 365(7):629-636.
- Moran B. $6.41 million verdict in Temple malpractice lawsuit. Philadelphia Inquirer. 2012, June 2. http://articles.philly.com/2012-06-02/news/31960243_1_million-verdict-malpractice-massive-heart-attack. Accessed March 1, 2016.
- Martin AB, Hartman M, Benson J, Catlin A; National Health Expenditure Accounts Team. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2015;35(1):150-160.
- Emanuel E, Tanden N, Altman S, et al. A systemic approach to containing health care spending. N Engl J Med. 2012;367(10):949-954.
- Jost TS. Health care reform requires law reform. Health Aff (Millwood). 2009; 28(5): w761-w769.
- Roslund G. The medical malpractice rundown: a state-by-state report card. Emerg Phys Monthly. 2014;July 21. Available at http://epmonthly.com/article/the-medical-malpractice-rundown-a-state-by-state-report-card/. Accessed March 1, 2016.
- Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
- Paik M, Black BS, Hyma DA. The receding tide of medical malpractice litigation part 2: effect of damage caps. J Empirical Leg Stud. 2013;10(4):639-669.
- Stamm JA, Korzick KA, Beech K, Wood KE. Medical malpractice: reform for today’s patients and clinicians. Am J Med. 2016;129(1):20-25.
- Segal J. Finally: an end to malpractice litigation? Medscape. Available at http://www.medscape.com/viewarticle/840337_1. March 5,2015. Accessed March 1, 2016.
- Shinkman R. Patient compensation system could replace malpractice torts. Fierce Health Finance Web site. November 9, 2014. Available at http://www.fiercehealthfinance.com/story/patient-compensation-system-could-replace-malpractice-torts/2014-11-09. Accessed March 1, 2016.
- Charles SC. Coping with a medical malpractice suit. West J Med. 2001;174(1): 55-58.
- Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6): 525-533.
- Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011; 365(7):629-636.
- Moran B. $6.41 million verdict in Temple malpractice lawsuit. Philadelphia Inquirer. 2012, June 2. http://articles.philly.com/2012-06-02/news/31960243_1_million-verdict-malpractice-massive-heart-attack. Accessed March 1, 2016.
- Martin AB, Hartman M, Benson J, Catlin A; National Health Expenditure Accounts Team. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2015;35(1):150-160.
- Emanuel E, Tanden N, Altman S, et al. A systemic approach to containing health care spending. N Engl J Med. 2012;367(10):949-954.
- Jost TS. Health care reform requires law reform. Health Aff (Millwood). 2009; 28(5): w761-w769.
- Roslund G. The medical malpractice rundown: a state-by-state report card. Emerg Phys Monthly. 2014;July 21. Available at http://epmonthly.com/article/the-medical-malpractice-rundown-a-state-by-state-report-card/. Accessed March 1, 2016.
- Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
- Paik M, Black BS, Hyma DA. The receding tide of medical malpractice litigation part 2: effect of damage caps. J Empirical Leg Stud. 2013;10(4):639-669.
- Stamm JA, Korzick KA, Beech K, Wood KE. Medical malpractice: reform for today’s patients and clinicians. Am J Med. 2016;129(1):20-25.
- Segal J. Finally: an end to malpractice litigation? Medscape. Available at http://www.medscape.com/viewarticle/840337_1. March 5,2015. Accessed March 1, 2016.
- Shinkman R. Patient compensation system could replace malpractice torts. Fierce Health Finance Web site. November 9, 2014. Available at http://www.fiercehealthfinance.com/story/patient-compensation-system-could-replace-malpractice-torts/2014-11-09. Accessed March 1, 2016.